Abstract
Introduction
A growing body of literature suggests atypical cerebral asymmetry and interhemispheric interaction in ADHD. A common means of assessing lateralized brain function in clinical populations has been to examine the relative proportion of EEG alpha activity (8– 12 Hz) in each hemisphere (i.e., alpha asymmetry). Increased rightward alpha asymmetry has been associated with ADHD-like traits such as reduced reward responsiveness, a lack of inhibition toward aversive experience, and increased approach behaviors, and previous work has indicated increased rightward alpha asymmetry in children with ADHD. The current study explores whether increased rightward alpha asymmetry is also evident in adults with ADHD.
Method
We assessed low (8– 10 Hz) and high (10– 12 Hz) alpha asymmetry in adults with ADHD (n = 29) versus controls (n = 62) during baseline and cognitive activation conditions for nine homologous electrode pairs along the anterior–posterior axis.
Result
Seven results emerged (p < .05) showing increased rightward alpha asymmetry in adults with ADHD. This occurred in three specific electrode pairs across two testing conditions, and five of six results occurred in the lower alpha band. Finally, post hoc analysis indicated that increased rightward alpha asymmetry was generally associated with greater numbers of ADHD symptoms—with a possible parietal association for inattentive and a fronto-temporal association for hyperactivity symptoms.
Conclusions
Increased rightward alpha asymmetry previously observed in children with ADHD appears to be a developmentally persistent feature of ADHD.
Keywords: Laterality, Attention, Hemisphere, EEG, States, ADHD, Alpha
1. Introduction
Attention deficit hyperactivity disorder (ADHD) is thought to represent an extreme on a normal continuum of liability with multiple genetic and environmental influences implicated as etiologic factors. A growing body of research suggests that atypical brain laterality (ABL) may be a common trait influencing ADHD risk along this continuum (Fassbender & Schweitzer, 2006; Hale, Bookheimer, McGough, Phillips, & McCracken, 2007; Hale et al., 2005; Hale, Zaidel, McGough, Phillips, & McCracken, 2006; Smalley, Loo, Yang, & Cantor, 2005; Stefanatos & Wasserstein, 2001). ABL was first suggested by the observation that ADHD-like symptoms occurred in some patients with right-sided brain damage (Heilman, Voeller, & Nadeau, 1991) and by the observation that brain systems important for attention and arousal regulation, implicated in ADHD pathology, seemed to be right-lateralized (Aston-Jones, Foote, & Bloom, 1984; Corbetta, Miezin, Shulman, & Petersen, 1993; Pardo & Raichle, 1991). From this, a ‘right hemisphere’ (RH) deficit model in ADHD has been considered (for review see Stefanatos & Wasserstein, 2001).
Subsequent neurocognitive and brain-imaging studies have supported abnormal RH contribution, however, the nature of this abnormality has not yet been characterized. Impoverished RH function is sometimes assumed due to the association of ADHD-like symptoms with right-sided brain damage or abnormal brain structure, but it is also possible that such circumstance could lead to a loss of inhibition and dysregulated and/or increased RH activation (for review see Mesulam, 1988). Likewise, reports of ADHD deficits on tasks thought to tap RH specialized functions (for review see Stefanatos & Wasserstein, 2001) cannot by themselves rule out whether poor LH function also contributed to poor task performance. Finally, brain-imaging studies of ADHD have clearly demonstrated abnormal structure and function in both hemispheres (for review see Durston, 2003; Giedd, Blumenthal, Molloy, & Castellanos, 2001; Seidman, Valera, & Makris, 2005; Valera, Faraone, Murray, & Seidman, 2006), as well as smaller corpus callosum volumes and abnormal left–right EEG coherence (Barry, Clarke, McCarthy, Selikowitz, & Johnstone, 2005; Chabot & Serfontein, 1996; Clarke et al., 2007). In short, the nature of putative abnormal RH function in ADHD remains unclear, and the notion of a strictly lateralized deficit does not account for additional suggested abnormalities of both LH and interhemispheric function. Thus, characterization of putative ABL in ADHD requires continued research.
A common means of assessing lateralized brain function in clinical populations has been to examine the relative proportion of EEG alpha activity (8– 12 Hz) in each hemisphere (i.e., alpha asymmetry). Alpha asymmetry appears to be a relatively stable trait with good internal consistency and test–re-test reliability (Tomarken, Davidson, Wheeler, & Kinney, 1992). Approximately 60% of variance is estimated to reflect a trait component, and 40% a state component (Hagemann, Naumann, Thayer, & Bartussek, 2002). Moreover, abnormalities in alpha asymmetry have been demonstrated with multiple forms of psychopathology such as depression (Bruder et al., 1997), anxiety (Bruder et al., 1997), bipolar disorder (Harmon-Jones et al., 2008), schizophrenia (Strelets, Garakh, Novototskii-Vlasov, & Magomedov, 2006), and autism (Stroganova et al., 2007) highlighting its importance for clinical research and demonstrating that ABL may be a shared feature of brain dysfunction impacting multiple psychiatric disorders (Smalley et al., 2005).
EEG studies of ADHD have consistently demonstrated anomalous alpha activity (for review see Barry, Clarke, & Johnstone, 2003), while medication studies have shown that increased alpha activity may be an important feature of ADHD methylphenidate response (Loo, Hopfer, Teale, & Reite, 2004; Song, Shin, Jon, & Ha, 2005). Also, increased rightward alpha asymmetry has been generally associated with ADHD-like traits such as reduced reward responsiveness, a lack of inhibition toward aversive experience, and increased approach behaviors (Davidson, 1992). Yet to our knowledge, only two studies have directly examined alpha asymmetry in ADHD. Baving, Laucht, and Schmidt (1999) reported increased rightward alpha asymmetry in 4–8-year-old boys with ADHD during an eyes-open resting condition. (Chabot and Serfontein, 1996) also reported increased rightward alpha asymmetry in large sample of 6–16-year-old ADHD male and female children during an eyes-closed resting condition.
The current study is the first to explore the hypothesis that increased rightward alpha asymmetry is also present in adults with ADHD. To do this, we assess alpha asymmetry in adults with ADHD versus healthy controls during two baseline conditions and one cognitive activation condition. Additionally, in our asymmetry analysis we examine upper (10– 12 Hz) and lower (8– 10 Hz) aspects of the alpha frequency band. Low alpha has been postulated to reflect diffuse attentional and brain-state phenomenon, while high alpha is postulated to reflect more localized and task-specific cognition (for review see Klimesch, 1999; Pfurtscheller, Neuper, & Krausz, 2000).
2. Methods and materials
2.1. Participants
The sample consisted of 91 adults (62 controls and 29 ADHD) recruited from an ongoing UCLA ADHD family genetics study (Smalley et al., 2000). Participation in this study required that families had at least 2 ADHD affected offspring. Thus, all subjects in the current study (cases and controls) were the biological parents of children with ADHD. After receiving verbal and written explanations of study requirements participants provided written informed consent approved by the UCLA Institutional Review Board. Through the UCLA ADHD Genetics Study all subjects were screened for ADHD and other psychiatric disorders via direct interviews using the Schedule for Affective Disorders and Schizophrenia – Lifetime Version (SADS-LAR; (Fyer, Endicott, Mannuzza, & Klein (1995)) supplemented with the Behavioral Disorders supplement from the Kiddie Schedule for Affective Disorders and Schizophrenia – Present and Lifetime Version (KSADS-PL; Kaufman et al., 1997). All interviews were conducted by clinical psychologists or highly trained interviewers with extensive experience in psychiatric diagnoses. Childhood ADHD status and number of ADHD symptoms were assessed by self-report using the Behavioral Disorders section of the KSADS-PL. ‘Best estimate’ diagnoses were determined after individual review of diagnoses, symptoms, and impairment level by senior clinicians (Leckman, Sholomskas, Thompson, Belanger, & Weissman, 1982). Inter-rater reliabilities were computed with a mean weighted kappa of 0.84 across all diagnoses with a greater than 5% occurrence in the sample. Handedness was assessed with a shortened version of the Edinburgh Handedness Inventory (Oldfield, 1971). Subjects were excluded if there was a documented neurological disorder, significant head injury resulting in concussion, a diagnosis of schizophrenia or autism, or an estimated full scale IQ < 80. Inclusion criteria for the present study required a current diagnosis of ADHD, and for non-ADHD controls, no evidence of past or current ADHD (i.e., showing 4 or fewer past or current ADHD symptoms). Subject demographics, including co-morbidity and medication status, are presented in Table 1.
Table 1.
Study demographics.
| Clinical variables | Controls N = 62 | ADHD N = 29 | Statistic |
|---|---|---|---|
| Estimated full IQ | X̄ = 117, std = 13.7 | X̄ = 116.8, std = 12.2 | t = .15, p = .88 |
| Age | X̄ = 44.4, std = 6.2 | X̄ = 45.2, std = 5.6 | t = −.54, p = .60 |
| ADHD type | n/a | 13C, 13I, 2H | n/a |
| Sex | 28F, 34M | 17F, 12M | χ2 = 1.4, p = .23 |
| Non-right handed | 5 NR, 57 R | 4 NR, 25 R | fe p = .31 |
| Anxiety | 2 affected | 6 affected | fe p = .01 |
| Mood | 4 affected | 6 affected | fe p = .05 |
| Medication | 3 subjects^ | 4 subjects^ |
Estimated Full IQ: estimated from block-design and vocabulary subtest of WAIS-R; ADHD type: C = combined, I = inattentive, H= hyperactive; NR = non-right-handed: R = right-handed; χ2 = chi-square test; fe = Fisher’s exact test; Anxiety/Mood reflect definite diagnosis of anxiety or mood disorder as assessed by direct interview using SADS-LAR(see text for reference); ĉontrol subjects on medication during EEG recording (1 Wellbutrin, 1 Celexa, 1 Lexapro), ADHD subjects on medication during EEG recording (2 Ritalin, 1 Paxil, 1 Celexa).
2.2. Electrophysiologic measures
EEG recording was carried out using 40 silver chloride electrodes using the International 10/20 locations and was referenced to linked ears. Eye movements were monitored by electrodes placed on the outer canthus of each eye for horizontal movements and by electrodes above the eye for vertical eye movements. EEG recording consisted of 2 baseline conditions lasting 5 min each [eyes open (EO) and eyes closed (EC)] and a cognitive activation condition, the Conners’ Continuous Performance test lasting 14 min (CPT) (Conners, 1994). The CPT test requires subjects to monitor a computer screen while single letters are sequentially and centrally presented with varying interstimulus intervals. Subjects must press the space bar with every letter presentation except for the letter X.
Continuous EEG data were subjected to automatic artifact detection via MAN-SCAN software (SAM Technology, Inc., San Francisco, CA, http://www.manscaneeg.com) designed to identify dead and bad channels, vertical and horizontal eye movements, saturation, muscle and movement artifact, and line frequency interference. Subsequent to this automated procedure, all data were visually inspected by an experienced EEG technician and any residual contaminants were identified. Next, continuous EEG was broken into 1-s epochs, and artifact-containing epochs were removed on a channel specific basis. Remaining artifact free epochs were then fast four transformed (FFT) and averaged for each condition (EC, EO, CPT). Lastly, EEG power (µv2) was exported in 1 Hz bins from 1 to 20 Hz. Technicians involved in the EEG recording and processing were blind to ADHD diagnostic status.
Absolute power of 8– 10 Hz frequency bands were averaged for each electrode composing a ‘low alpha’ measure. Absolute power of 10– 12 Hz frequency bands were averaged for each electrode composing a ‘high alpha’ measure. Laterality indices (LIs) were generated for nine homologous left/right electrode pairs (AF4-AF3, F4-F3, F8-F7, FT8-FT7, T8-T7, TP8-TP7, P4-P3, P8-P7, O2-O1) using to the following calculation (R − L/R + L × 1000).
2.3. Statistical analysis
For each condition (EC, EO, CPT), SPSS 15.0 general linear model univariate procedure was used to assess for group differences in high and low alpha for the nine LIs. Age, sex, and medication status were co-varied in all analyses. Age and sex are understood to impact brain laterality (Toga & Thompson, 2003; Zaidel, Aboitiz, Clarke, Kaiser, & Matteson, 1995) and previous work in our group has suggested a possible differential effect of age on lateralized brain function in ADHD versus control subjects. Co-varying for medication status was used to adjust for possible effects of four ADHD and three control subjects who were on medication during testing (see Table 1). Furthermore, all reported results of interest were re-tested with medicated subjects removed. Lastly, all reported results of interest were re-tested to assess for possible effects of co-morbid anxiety, mood, and handedness (see Section 3.3).
3. Results
Seven group differences emerged, all of which indicated increased rightward alpha asymmetry in adults with ADHD. These results occurred only during the CPT and EC conditions, and only in three laterality indices (F8-F7, FT8-FT7, P4-P3). Moreover, five of seven group differences occurred in low alpha. Medication status (entered as a covariate along with age and sex) did not approach significance in any analysis (for example, p-values for the covariate ‘medication status’ in the seven reported findings were .79, .73, .87, .55, .42, .97, .43). The covariate for age showed a significant effect for two analyses: high and low alpha at FT8-FT7 during the CPT task (p = .031, and p = .035). The covariate for sex showed one effect: high alpha at F8-F7 during the CPT task (p = .021).
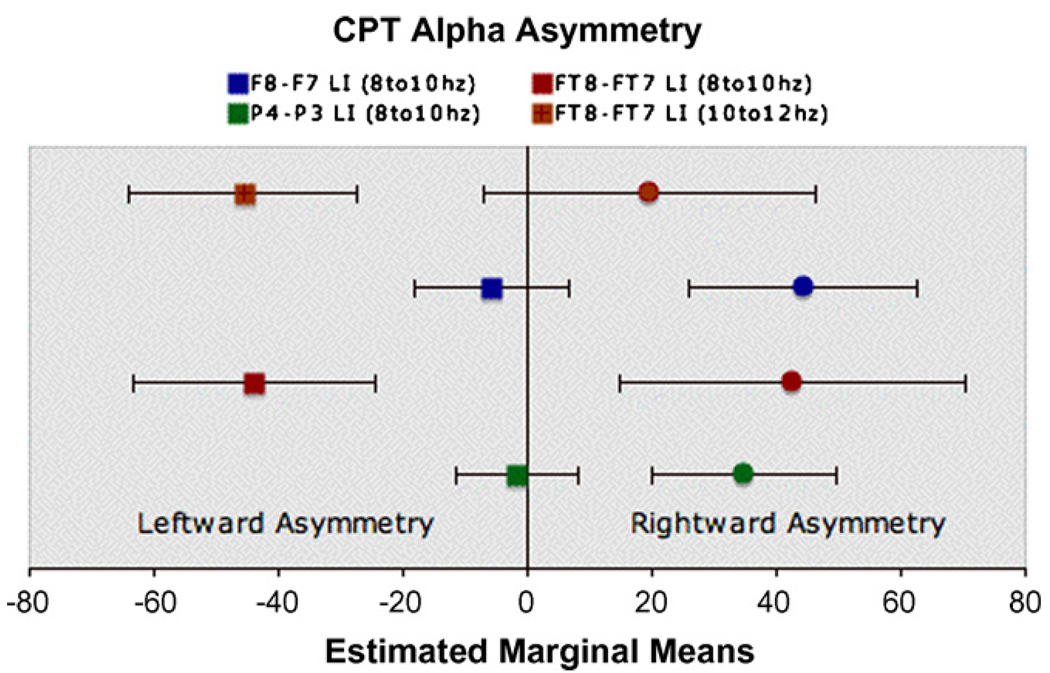
3.1. The Continuous Performance Task
During the CPT tasks, adults with ADHD showed increased rightward alpha asymmetry for low alpha at: F8-F7 [F(1, 84) = 5.0, p = .028], FT8-FT7 [F(1, 84) = 6.2, p = .015], P4-P3 [F(1, 86) = 4.25, p = .042], and high alpha at: FT8-FT7 [F(1, 84) = 3.98, p = .049] and one trend: F4-F3 high alpha [F(1, 84) = 3.6, p = .06] (see Fig. 1).
Fig. 1.
Alpha asymmetry in adults with ADHD versus controls during the Continuous Performance Task. Caption: circles = mean asymmetry scores for ADHD group; squares = mean asymmetry scores for control group; LI = laterality index; note: ADHD group shows increased rightward alpha asymmetry at three laterality indices with group differences occurring for both high and low alpha at FT8-FT7.
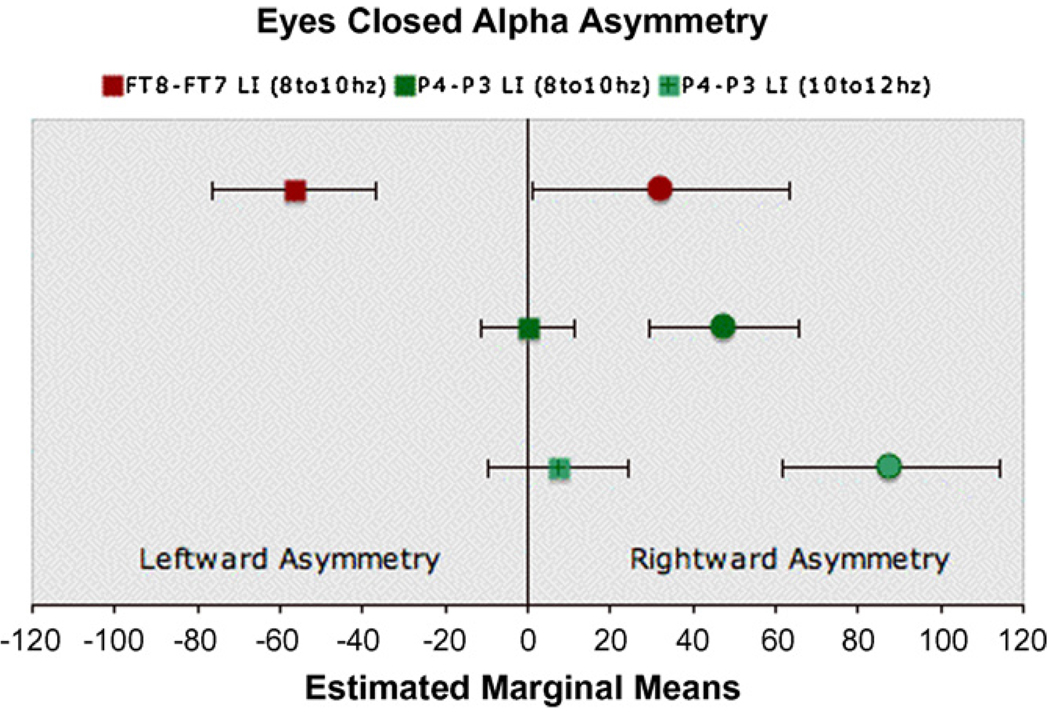
3.2. The eyes-closed condition
During the EC condition adults with ADHD showed increased rightward alpha asymmetry for low alpha at: FT8-FT7 [F(1, 82) = 5.26, p = .024], P4-P3 [F(1, 81) = 4.73, p = .03], and high alpha at: P4-P3 [F(1, 81) = 5.8, p = .02] (Fig. 2).
Fig. 2.
Alpha asymmetry in adults with ADHD versus controls during the eyes-closed condition. Caption: circles = mean asymmetry scores for ADHD group; squares = mean asymmetry scores for control group; LI = laterality index; note: ADHD group shows increased rightward alpha asymmetry at two laterality indices with group differences occurring for both high and low alpha at P4-P3.
3.3. Secondary analyses: adjusting for possible confounds
As stated, primary analyses indicated no effect whatsoever of medication status, however, as an additional assessment, results of interest were re-tested with medicated subjects removed (removal of medicated subjects reduces ADHD sample size by 14% [4 of 29 subjects]—with the associated loss of statistical power). Furthermore, effects of anxiety and mood disorder, as well as handedness, were evaluated by re-testing results of interests with each of these factors entered as covariates in separate analyses along with sex, age, and medication status.
The overall pattern of results was not altered by these adjustments. However, four group differences did emerge as being particularly robust, surviving all adjustments at p < .05. These results were F8-F7 and FT8-FT7 for low alpha during the CPT task, and P4-P3 in both low and high alpha during the EC condition. Table 2 summarizes adjusted p-values for these analyses.
Table 2.
Summary of adjusted p-values.
| Measures | Primary | Med. subs removed | Adjusted for handeness | Adjusted for anxiety | Adjusted for mood |
|---|---|---|---|---|---|
| CPT low alpha | |||||
| F8-7* | .028 | .043 | .032 | .041 | .034 |
| FT8-7* | .015 | .035 | .027 | .021 | .024 |
| P4-3 | .042 | .074 | .043 | .057 | .034 |
| CPT high alpha | |||||
| FT8-7 | .049 | .074 | .069 | .053 | .10 |
| EC low alpha | |||||
| FT8-7 | .024 | .069 | .022 | .009 | .02 |
| P4-3* | .033 | .044 | .024 | .044 | .038 |
| EC high alpha | |||||
| P4-3* | .019 | .027 | .015 | .027 | .027 |
Primary = original analyses adjusted for age, sex, and medication status; med. subs removed = analyses adjusted for age and sex with medicated subjects removed (4 adhd, 3 control subjects); adjusted for … handedness, anxiety, and mood = separate analyses with these factors added as covariates along with age, sex, and medication status.
LIs that survived all adjustments at p < .05.
3.4. Post hoc analysis
We used linear regression analysis to examine the association of EEG alpha asymmetry measures reported above (i.e., those suggestive of ADHD/control group differences) with inattentive and hyperactive symptom severity across the whole group (n = 91) (see Table 3). This assesses whether these LI measures in certain regions are associated with ADHD symptoms regardless of ADHD/control diagnostic status. EEG alpha asymmetry measures were predictors and modeled along with covariates age, sex, and medication status. The number of ADHD symptoms for inattentive and hyperactive–impulsive domains were used as outcome variables in separate analyses. Results suggest increased rightward alpha asymmetry is generally associated with greater ADHD symptoms. Moreover, they indicate a possible differential association between fronto-temporal and superior parietal alpha asymmetry measures for inattentive versus hyperactive symptoms. Specifically, hyperactive symptoms may be associated with fronto-temporal asymmetry, while parietal asymmetries may be associated with inattentive symptoms.
Table 3.
Association of alpha asymmetry and ADHD symptoms.
| SADS inattentive | SADS hyperactive | |||||
|---|---|---|---|---|---|---|
| SB | t | p | SB | t | p | |
| Eyes closed | ||||||
| FT8-7 LA | .17 | 1.5 | .14 | .23 | 2.1 | .038 |
| P4-3 LA | .25 | 2.3 | .027 | .066 | .6 | .55 |
| P4-3 HA | .21 | 1.8 | .075 | .13 | 1.2 | .25 |
| CPT | ||||||
| F8-7 LA | .18 | 1.7 | .098 | .24 | 2.3 | .026 |
| FT8-7 LA | .12 | 1.1 | .28 | .25 | 2.4 | .018 |
| P4-3 LA | .20 | 1.9 | .06 | .15 | 1.4 | .16 |
| FT8-7 HA | .07 | .65 | .52 | .20 | 1.9 | .065 |
Regression analysis was used to test the association of alpha asymmetry measures on SADS inattentive and hyperactive symptom scales in the whole sample (ADHD & controls combine n = 91). LA = low alpha; HA = high alpha; bold values = results with p < .05; italicised values = trends p < .07; SB = standardized beta coefficient.
4. Discussion
This study sought to determine whether rightward alpha asymmetry previously observed in child ADHD samples was also present in adults with ADHD. We compared EEG alpha asymmetry of adults with ADHD to controls during baseline (EC, EO) and cognitive challenge (CPT) conditions. Group differences were assessed with nine homologous electrode pairs for low (8– 10 Hz) and high (10– 12 Hz) alpha frequency bands. Seven results emerged all demonstrating increased rightward alpha asymmetry in adults with ADHD. These findings replicate previous reports of increased rightward alpha asymmetry in children with ADHD (Baving et al., 1999; Chabot & Serfontein, 1996) and support our a priori hypothesis. Moreover, they demonstrate a clear and conceptually coherent pattern of findings: (1) all results showed increased rightward asymmetry for ADHD, (2) all results occurred in two specific brain regions (fronto-temporal [F8-F7, FT8-FT7], superior parietal [P4-P3]) across two testing conditions (EC, CPT), and (3) five of seven results occurred in the lower alpha band. Given this clear pattern of findings aligned with our a priori hypothesis we feel it is unlikely that the current results reflect random false positive errors. Still, the important issue of multiple testing is discussed in further detail below (see Section 5). Finally, post hoc analysis of the whole group (controls and ADHD together) suggested that these specific alpha asymmetry measures more generally index ADHD symptomatology with increasing rightward asymmetry predicting greater numbers of symptoms. More specifically, they suggest a possible parietal association for inattentive symptoms and a fronto-temporal association for hyperactivity symptoms.
The previous reports of increased rightward alpha in ADHD were in children (Baving et al., 1999; Chabot & Serfontein, 1996). Our study demonstrates that this may be a developmentally stable trait that is observable in adults. This finding is consistent with multiple reports of ABL in adult ADHD samples from both structural and functional imaging (for review see Durston, 2003; Giedd et al., 2001; Seidman et al., 2005; Valera et al., 2006) and behavioral laterality testing (Campbell et al., 1996; Cohen et al., 1996; Hale et al., 2005; Hale et al., 2006; Malone, Kershner, & Siegel, 1988). Recent work in our group has indicated that rightward alpha asymmetry increases across development among ADHD children who have a parent diagnosed with ADHD but not in children without a similarly diagnosed parent. These results suggest a familial contribution to rightward shifting alpha asymmetry only in families with an ADHD affected parent. If true, this suggests that increased rightward alpha asymmetry may be associated with ADHD persistence and be an especially salient feature of adults who continue to meet diagnostic criteria for ADHD.
Rightward alpha asymmetry in ADHD may be state and frequency specific as it was observed during EC and CPT conditions, but not during an EO recording, and was most prominent for the lower alpha band. As mentioned, low alpha activity (8– 10 Hz) has been associated with diffuse attentional processing whereas high alpha activity (10– 12 Hz) is thought to reflect localized and task-specific processing (Klimesch, 1999; Pfurtscheller et al., 2000). According to this, our findings in low alpha suggest that increased rightward alpha asymmetry in ADHD reflects abnormal brain-state orientation during EC and CPT conditions more than localized processing. Sensory processing during the EO condition might have produced excessive brain state variability that overrode or masked any asymmetry effects in this condition.
Indeed, a more stable pattern of laterality findings in ADHD may occur during rest or simple forms of processing that involve limited variability in brain-state orientation. For example, functional imaging during executive operations has produced mixed results with regards to brain laterality in ADHD (for review see Durston, 2003; Giedd et al., 2001; Seidman et al., 2005; Valera et al., 2006), however, those studies measuring brain activity at rest or during simple (i.e., non-executive function) tasks appear to show a more consistent pattern of reduced left hemisphere (LH) (Ernst, Zametkin, Matochik, Jons, & Cohen, 1998; Seig, Gaffney, Preston, & Jellings, 1995; Zametkin et al., 1993; Zametkin et al., 1990) and/or increased RH Baving et al., 1999; Chabot & Serfontein, 1996; Hale et al., 2007; Swartwood, Swartwood, Lubar, & Timmermann, 2003) activation. Moreover, a recent fMRI study compared adults with ADHD and controls during simple and complex levels of task processing and found that increased RH activation in ADHD only occurred with simple processing (Hale et al., 2007). Lastly, a recent model by Sonuga-Barke and Castellanos (2007) has suggested that ADHD may involve maladaptive increased switching into a ‘default’ or ‘baseline’ brain state during active cognition, and points out that this may be associated with excessive response variability observed in ADHD (Klein, Wendling, Huettner, Ruder, & Peper, 2006). In short, our results may reflect dysregulation of baseline versus active brain states in ADHD, and highlight that this may involve increased rightward alpha asymmetry.
Rightward alpha asymmetry in adult ADHD subjects was topographically specific. Group differences were found for three electrode pairs only (F8-F7, FT8-FT7, P4-P3), with FT8-FT7 and P4-P3 showing effects in both EC and CPT conditions. Although spatial resolution of surface EEG is limited, these electrodes pairs generally reflect brain activity in fronto-temporal (possibly involving anterior–temporal lobes) (F8-F7, FT8-FT7), and superior parietal (P4-P3) regions. These regions have been associated with abnormal brain function in ADHD with various tasks including response inhibition and working memory challenges (Bush, Valera, & Seidman, 2005; Durston, 2003; Giedd et al., 2001; Hale et al., 2007). Rightward alpha asymmetry in these regions may reflect a default brain-state orientation that is maladaptive for active goal-directed or executive function operations. Moreover, post hoc analyses (with all subjects combined) suggested parietal association with inattentive symptoms and fronto-temporal association with hyperactive symptoms. This may be consistent with research showing superior parietal association with directing attention (Corbetta et al., 1993), and frontal–temporal association with social–emotional processing that likely play a role in mediating social constraints on behavior (for review see Olson, Plotzker, & Ezzyat, 2007).
Lastly, all results showed increased R > L asymmetry of alpha power in ADHD. This directionality is consistent with findings in ADHD children (Baving et al., 1999; Chabot & Serfontein, 1996), and with studies showing greater rightward alpha asymmetry with ADHD-like traits such as reduced reward responsiveness, a lack of inhibition toward aversive experience, and increased approach behaviors (Davidson, 1992). Moreover, post hoc analyses suggest that greater rightward alpha asymmetry was generally associated with greater number of ADHD symptoms. However, interpreting this directionality with respect to underlying brain function is not straightforward (see below).
Some recent findings challenge the completeness of the traditional view that alpha activity is inversely related to brain function (Cooper, Croft, Dominey, Burgess, & Gruzelier, 2003; Klimesch, Sauseng, & Hanslmayr, 2007; Palva & Palva, 2007; Shaw, 1996). For instance, simultaneous EEG alpha recording with either fMRI (Goldman, Stern, Engel, & Cohen, 2002; Martinez-Montes, Valdes-Sosa, Miwakeichi, Goldman, & Cohen, 2004) or PET (Sadato et al., 1998; Schreckenberger et al., 2004) imaging has demonstrated both negative and positive associations between alpha activity and brain function. Moreover, increased alpha activity during active and/or cognitively demanding challenges has been reported (the so-called paradoxical alpha response) (Cooper, Burgess, Croft, & Gruzelier, 2006; Cooper et al., 2003; and for review see Klimesch et al., 2007; Palva & Palva, 2007; Shaw, 1996). To account for this, novel theories have suggested that alpha activity may index the proportion of self-directed-intentional (i.e., top-down) versus sensory-directed (bottom-up) processing (Klimesch et al., 2007; Palva & Palva, 2007; Shaw, 1996). Although speculative, this view can theoretically account for discrepant findings.
Given this ongoing work, definitive conclusions regarding the directionality of the current results and underlying brain function are not suggested. However, it is interesting to note that with the more recent view of alpha activity, our results appear to be consistent with imaging studies showing R > L asymmetries of brain function (cited above), behavioral laterality studies indicating increased RH contributions (Campbell et al., 1996; Cohen et al., 1996; Hale et al., 2005; Hale et al., 2006; Malone et al., 1988), and naming speed tasks indicating poor LH function in ADHD (Brock & Christo, 2003; Nigg, Butler, Huang-Pollock, & Henderson, 2002; Rucklidge & Tannock, 2002; Semrud-Clikeman, Guy, Griffin, & Hynd, 2000; Stevens, Quittner, Zuckerman, & Moore, 2002; Tannock, Martinussen, & Frijters, 2000; Weiler, Bernstein, Bellinger, & Waber, 2000; Willcutt, Doyle, Nigg, Faraone, & Pennington, 2005).
Lastly, it is critical to understand that our sample was ascertained through ADHD affected children. This has important implications for the interpretation of our findings when considering a heritable endophenotype of ADHD. Although there are, in theory, non-heritable means by which unaffected parents may have ADHD affected offspring (i.e., de novo mutation, brain injury, or environmental factors), family and twin studies support a multi-factorial model of inheritance (Faraone et al., 2005) and under this model it is more likely that such parents would be elevated on putative ADHD endophenotypes. Moreover, ascertainment through two affected offspring likely increases the chances that affected parents were drawn from more heritable forms of ADHD perhaps making endophenotypes easier to detect in this group. Lastly, two previous studies showing increased rightward alpha asymmetry in ADHD children (Baving et al., 1999; Chabot & Serfontein, 1996) did not assess family loading for ADHD or this asymmetry effect and so cannot help address whether this finding represents an endophenotype. In short, we cannot at this time be certain whether the result of increased rightward alpha asymmetry in ADHD represents an endophenotype or an actual biological surrogate for ADHD itself—both of which could, in theory, be related to an underlying genetic susceptibility.
For instance, the observed result of increased rightward alpha asymmetry in our adult cases could reflect: (a) a difference in the severity of expression of an ADHD endophenotype—even though it is shared and elevated in both groups, (b) a non-genetic biological marker for the full blown syndrome of adult ADHD (perhaps stemming from secondary consequences of having ADHD across the life-span), (c) a unique ADHD endophenotype and etiologic pathway that is specific to parent–offspring affected families, or (d) a unique genetic liability for a biological marker of the full syndrome of ADHD, rather than an endophenotype, that is specific to parent–offspring affected families. (a) and (b) assume groups are elevated for a set of shared ADHD endophenotypes. (c) and (d) assume this as well, but additionally account for the possibility that there may be unique gene-effects in parent–offspring affected families, for instance, gene-effects that are perhaps stronger and/or associated with ADHD persistence. Without a control sample lacking ADHD affected offspring, we cannot distinguish between these possibilities. However, these data suggest that future analysis of these two general models will be important, and could be accomplished by stratifying cases and controls based on the degree of ADHD familial loading. Indeed, this type of study design may prove particularly usefully in uncovering complex but subtle gene-effects in what are likely multigenic disorders such as ADHD.
In sum, increased rightward alpha asymmetry in adults with ADHD is evident during an EC and active cognition state (CPT task) particularly in low versus high alpha, and particularly in ventrolateral frontal and superior parietal regions. This replicates increased rightward alpha asymmetry observed in ADHD children and suggests brain region and condition specificity for this effect. Alpha asymmetry may be a useful endophenotype or an actual biological surrogate for ADHD itself.
5. Limitations
The issue of multiple comparisons is particularly difficult with EEG research as there are multiple sources of measurement (i.e., electrodes), each producing multiple data components (i.e., multi-hertz signal). Adding to this, state-influenced variability in EEG signal can diminish important trait characteristics that are thus less likely to survive corrections for multiple testing. EEG researchers often address this issue by averaging data across electrodes and/or using repeated measures ANOVA analyses. Importantly, each of these tactics brings to bear certain limitations. Averaging discounts the possibility of distinct and meaningful site-specific activations, while repeated measures ANOVA can unduly eliminate valid and informative data. In repeated measures ANOVA data must be present for all levels of each included variable. Thus, for example, a subject missing just 1 of 54 measures in the ANOVA-Group (ADHD, control) × Region (9 LIs- using 18 electrodes) × Condition (EC, EO, CPT), would be entirely eliminated from the analysis, and unfortunately, due to channel specific artifact, this scenario is not uncommon.
Our choice to independently analyze measures of interest across conditions and for both alpha-types was guided by these considerations, as well as the fact that we were testing a very specific a priori hypothesis, and hence, the risk of type 1 error was considerably reduced (Perneger, 1998). Moreover, with this approach we had the advantage of being able examine our results for the presence or absence of a consistent pattern of findings that aligned with our hypothesis—reasoning that such a pattern, if present, would provide reasonably good assurance that findings did not stem from random false positive errors.
As reported, we did find such a pattern and feel confident that the current results, aligned with our a priori hypothesis, did not result from type 1 errors. That being said, the modest strength of the reported group differences does suggest a high degree of variability for these effects. Indeed, it is likely that observed ABL in adults with ADHD represents only one of many contributing and variably expressed etiologic pathways for ADHD. Understanding these multiple sources of ADHD pathology will likely prove critical to devising better treatments.
In the current study, 4 ADHD and 3 control subjects were on medication during testing. We chose to leave the sample intact for two primary reasons. First, medication status included as a covariate did not approach significance in any reported analysis (p-values for the covariate medication status were uniformly >.4 with a mean of .68). Next, given this lack of association between medication status and alpha asymmetry, the cost of losing 4 of 29 ADHD subjects (14% of ADHD sample) and the associated loss of statistical power did not seem warranted. Also, although studies have shown an affect of methylphenidate on alpha power (2 ADHD subjects in the current study), an impact on alpha asymmetry has not been established; and regarding subjects on SSRI medication (3 controls and 2 ADHD), a recent study has demonstrated no effect on either alpha power or alpha asymmetry (Bruder et al., 2008). Most importantly however, we tested all reported results with medicated subjects removed and found that our pattern of results was unchanged. Three of seven p-values did adjust to .07, but this is not surprising given the loss of statistical power associated with removing 14% of the ADHD sample. In short, given the lack of effect of co-varying for medication status and the fact that our pattern of results were not altered with medicated subjects removed, we feel it unlikely that the current findings stem from the presence of medicated subjects in our samples.
Co-morbid anxiety and mood disorder were present in both ADHD and control samples in the current study. We assessed the effects of these factors for all reported findings and found that the pattern of results was unchanged. We chose to co-vary versus eliminate these subjects because the incidence of mood and anxiety disorder in our samples are representative of typical control and ADHD populations (Biederman et al., 1993). Indeed, it is interesting to consider that because adult ADHD samples consistently contain such co-morbidities it is possible (and perhaps likely) that these conditions share some over-lapping etiologic pathways and that understanding this overlap may help to shed light on ADHD pathology itself.
Lastly, future studies with larger sample sizes should directly examine the impact of gender, handedness, co-morbidity and sub-type on the expression of anomalous EEG alpha asymmetry in ADHD.
Footnotes
This work was funded in part by National Institute of Mental Health Grant MH058277 (Smalley), National Institute of Child Health and Human Development Grant HD40275 (Loo), and National Institute of Mental Health Grant 1K99MH082104 (Hale).
References
- Aston-Jones G, Foote SL, Bloom FE. Anatomy and physiology of locus coeruleus neurons: Functional implication. Frontiers of Clinical Neuroscience. 1984;2:92–116. [Google Scholar]
- Barry RJ, Clarke AR, Johnstone SJ. A review of electrophysiology in attention-deficit/hyperactivity disorder: I. Qualitative and quantitative electroencephalography. Clinical Neurophysiology. 2003;114:171–183. doi: 10.1016/s1388-2457(02)00362-0. [DOI] [PubMed] [Google Scholar]
- Barry RJ, Clarke AR, McCarthy R, Selikowitz M, Johnstone SJ. EEG coherence adjusted for inter-electrode distance in children with attention-deficit/hyperactivity disorder. International Journal of Psychophysiology. 2005;58(1):12–20. doi: 10.1016/j.ijpsycho.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Baving L, Laucht M, Schmidt MH. Atypical frontal brain activation in ADHD: Preschool and elementary school boys and girls. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(11):1363–1371. doi: 10.1097/00004583-199911000-00010. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Spencer T, Wilens T, Norman D, Lapey KA, et al. Patterns of psychiatric comorbidity, cognition, and psychosocial functioning in adults with attention deficit hyperactivity disorder. The American Journal of Psychiatry. 1993;150(12):1792–1798. doi: 10.1176/ajp.150.12.1792. [DOI] [PubMed] [Google Scholar]
- Brock SE, Christo C. Digit naming speed performance among children with attention-deficit/hyperactivity disorder. California School Psychologist. 2003;8:115–125. [Google Scholar]
- Bruder GE, Fong R, Tenke CE, Leite P, Towey JP, Stewart JE, et al. Regional brain asymmetries in major depression with or without an anxiety disorder: A quantitative electroencephalographic study. Biological Psychiatry. 1997;41(9):939–948. doi: 10.1016/S0006-3223(96)00260-0. [DOI] [PubMed] [Google Scholar]
- Bruder GE, Sedoruk JP, Stewart JW, McGrath PJ, Quitkin FM, Tenke CE. Electroencephalographic alpha measures predict therapeutic response to a selective serotonin reuptake inhibitor antidepressant: Pre- and post-treatment findings. Biological Psychiatry. 2008;63(12):1171–1177. doi: 10.1016/j.biopsych.2007.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bush G, Valera EM, Seidman LJ. Functional neuroimaging of attention-deficit/hyperactivity disorder: A review and suggested future directions. Biological Psychiatry. 2005;57(11):1273–1284. doi: 10.1016/j.biopsych.2005.01.034. [DOI] [PubMed] [Google Scholar]
- Campbell L, Malone MA, Kershner JR, Roberts W, Humphries T, Logan WJ. Methylphenidate slows right hemisphere processing in children with attention-deficit/hyperactivity disorder. Journal of Child and Adolescent Psychopharmacology. 1996;6(4):229–239. doi: 10.1089/cap.1996.6.229. [DOI] [PubMed] [Google Scholar]
- Chabot RJ, Serfontein G. Quantitative electroencephalographic profiles of children with attention deficit disorder. Biological Psychiatry. 1996;40:951–963. doi: 10.1016/0006-3223(95)00576-5. [DOI] [PubMed] [Google Scholar]
- Clarke AR, Barry RJ, McCarthy R, Selikowitz M, Johnstone SJ, Hsu CI, et al. Coherence in children with attention-deficit/hyperactivity disorder and excess beta activity in their EEG. Clinical Neurophysiology. 2007;118(7):1472–1479. doi: 10.1016/j.clinph.2007.04.006. [DOI] [PubMed] [Google Scholar]
- Cohen MS, Kosslyn SM, Breiter HC, DiGirolamo GJ, Thompson WL, Bookheimer SY, et al. Changes in cortical activity during mental rotation: Amapping study using functional magnetic resonance imaging. Brain. 1996;119:89–100. doi: 10.1093/brain/119.1.89. [DOI] [PubMed] [Google Scholar]
- Conners CK. The Continuous Performance Test (CPT): Use as a diagnostic tool and measure of treatment outcome. Paper Presented at the American Psychological Association; Los Angeles, CA. 1994. [Google Scholar]
- Cooper NR, Burgess AP, Croft RJ, Gruzelier JH. Investigating evoked and induced electroencephalogram activity in task-related alpha power increases during an internally directed attention task. Neuroreport. 2006;17(2):205–208. doi: 10.1097/01.wnr.0000198433.29389.54. [DOI] [PubMed] [Google Scholar]
- Cooper NR, Croft RJ, Dominey SJJ, Burgess AP, Gruzelier JH. Paradox lost? Exploring the role of alpha oscillations during externally vs. internally directed attention and the implications for idling and inhibition hypotheses. International Journal of Psychophysiology. 2003;47(1):65–74. doi: 10.1016/s0167-8760(02)00107-1. [DOI] [PubMed] [Google Scholar]
- Corbetta M, Miezin F, Shulman G, Petersen S. A PET study of visuospatial attention. The Journal of Neuroscience. 1993;13(3):1202–1226. doi: 10.1523/JNEUROSCI.13-03-01202.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ. Anterior cerebral asymmetry and the nature of emotion. Brain and Cognition. 1992;20(1):125–151. doi: 10.1016/0278-2626(92)90065-t. [DOI] [PubMed] [Google Scholar]
- Durston S. A review of the biological bases of ADHD: What have we learned from imaging studies? Mental Retardation and Developmental Disabilities Research Reviews. 2003;9(3):184–195. doi: 10.1002/mrdd.10079. [DOI] [PubMed] [Google Scholar]
- Ernst M, Zametkin AJ, Matochik JA, Jons PH, Cohen RM. DOPA decarboxylase activity in attention deficit hyperactivity disorder adults. A [fluorine-18] fluorodopa positron emission tomographic study. The Journal of Neuroscience. 1998;18(15):5901–5907. doi: 10.1523/JNEUROSCI.18-15-05901.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, et al. Molecular genetics of attention-deficit/hyperactivity disorder. Biological Psychiatry. 2005;57(11):1313–1323. doi: 10.1016/j.biopsych.2004.11.024. [DOI] [PubMed] [Google Scholar]
- Fassbender C, Schweitzer JB. Is there evidence for neural compensation in attention deficit hyperactivity disorder? A review of the functional neuroimaging literature. Clinical Psychology Review. 2006;26(4):445–465. doi: 10.1016/j.cpr.2006.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fyer AJ, Endicott J, Mannuzza S, Klein DF. The schedule for affective disorders and schizophrenia-lifetime version, modified for the study of anxiety disorder 1985, Updated for DSM-IV (SADS-LA-IV) New York Anxiety Genetics Unit, New York State Psychiatric Institute; 1995. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Blumenthal J, Molloy E, Castellanos FX. Brain imaging of attention deficit/hyperactivity disorder. Annals of New York Academy of Science. 2001;931:33–49. doi: 10.1111/j.1749-6632.2001.tb05772.x. [DOI] [PubMed] [Google Scholar]
- Goldman RI, Stern JM, Engel J, Jr, Cohen MS. Simultaneous EEG and fMRI of the alpha rhythm. Neuroreport. 2002;13(18):2487–2492. doi: 10.1097/01.wnr.0000047685.08940.d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagemann D, Naumann E, Thayer JF, Bartussek D. Does resting electroencephalograph asymmetry reflect a trait? An application of latent state-trait theory. Journal of Personality and Social Psychology. 2002;82(4):619–641. [PubMed] [Google Scholar]
- Hale TS, Bookheimer S, McGough JJ, Phillips JM, McCracken JT. Atypical brain activation during simple & complex levels of processing in adult ADHD: An fMRI Study. Journal of Attention Disorders. 2007;10(4):1–16. doi: 10.1177/1087054706294101. [DOI] [PubMed] [Google Scholar]
- Hale TS, McCracken JT, McGough JJ, Smalley SL, Phillips JM, Zaidel E. Impaired linguistic processing and atypical brain laterality in adults with ADHD. Clinical Neuroscience Research. 2005;5:255–263. [Google Scholar]
- Hale TS, Zaidel E, McGough JJ, Phillips JM, McCracken JT. Aytpical Brain laterality in adults with ADHD during dichotic listening for emotional intonation and words. Neuropsychologia. 2006;44:896–904. doi: 10.1016/j.neuropsychologia.2005.08.014. [DOI] [PubMed] [Google Scholar]
- Harmon-Jones E, Abramson LY, Nusslock R, Sigelman JD, Urosevic S, Turonie LD, et al. Effect of bipolar disorder on left frontal cortical responses to goals differing in valence and task difficulty. Biological Psychiatry. 2008;63(7):693–698. doi: 10.1016/j.biopsych.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Heilman KM, Voeller KK, Nadeau SE. A possible pathophysiological substrate of attention deficit hyperactivity disorder. The Journal of Child Neurology. 1991;6 Supplemental:S76–S81. doi: 10.1177/0883073891006001s09. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Klein C, Wendling K, Huettner P, Ruder H, Peper M. Intra-subject variability in attention-deficit hyperactivity disorder. Biological Psychiatry. 2006;60(10):1088–1097. doi: 10.1016/j.biopsych.2006.04.003. [DOI] [PubMed] [Google Scholar]
- Klimesch W. EEG alpha and theta oscillations reflect cognitive and memory performance: A review and analysis. Brain Research. Brain Research Reviews. 1999;29(2–3):169–195. doi: 10.1016/s0165-0173(98)00056-3. [DOI] [PubMed] [Google Scholar]
- Klimesch W, Sauseng P, Hanslmayr S. EEG alpha oscillations: The inhibition-timing hypothesis. Brain Research Review. 2007;53(1):63–88. doi: 10.1016/j.brainresrev.2006.06.003. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM. Best estimate of lifetime psychiatric diagnosis: A methodological study. Archives of General Psychiatry. 1982;39(8):879–883. doi: 10.1001/archpsyc.1982.04290080001001. [DOI] [PubMed] [Google Scholar]
- Loo SK, Hopfer C, Teale PD, Reite ML. EEG correlates of methylphenidate response in ADHD: Association with cognitive and behavioral measures. Journal of Clinical Neurophysiology. 2004;21(6):457–464. doi: 10.1097/01.wnp.0000150890.14421.9a. [DOI] [PubMed] [Google Scholar]
- Malone MA, Kershner JR, Siegel L. The effects of methylphenidate on levels of processing and laterality in children with attention deficit disorder. Journal of Abnormal Child Psychology. 1988;16(4):379–395. doi: 10.1007/BF00914170. [DOI] [PubMed] [Google Scholar]
- Martinez-Montes E, Valdes-Sosa PA, Miwakeichi F, Goldman RI, Cohen MS. Concurrent EEG/fMRI analysis by multiway Partial Least Squares. Neuroimage. 2004;22(3):1023–1034. doi: 10.1016/j.neuroimage.2004.03.038. [DOI] [PubMed] [Google Scholar]
- Mesulam M-M. Neural substrates of behavior: The effects of brain lesions upon mental state. In: Nicholi AM, editor. The New Harvard guide to psychiatry. Cambridge, MA: Harvard University Press; 1988. pp. 91–128. [Google Scholar]
- Nigg JT, Butler KM, Huang-Pollock CL, Henderson JM. Inhibitory processes in adults with persistent childhood onset ADHD. Journal of Consulting Clinical Psychology. 2002;70(1):153–157. doi: 10.1037//0022-006x.70.1.153. [DOI] [PubMed] [Google Scholar]
- Oldfield RC. Assessment and analysis of handedness: The Edinburgh Inventory. Neuropsychologia. 1971;19:97–113. doi: 10.1016/0028-3932(71)90067-4. [DOI] [PubMed] [Google Scholar]
- Olson IR, Plotzker A, Ezzyat Y. The enigmatic temporal pole: A review of findings on social and emotional processing. Brain. 2007;130(7):1718–1731. doi: 10.1093/brain/awm052. [DOI] [PubMed] [Google Scholar]
- Palva S, Palva JM. New vistas for alpha-frequency band oscillations. Trends in Neurosciences. 2007;30(4):150–158. doi: 10.1016/j.tins.2007.02.001. [DOI] [PubMed] [Google Scholar]
- Pardo JV, Raichle ME. Localization of a human system of sustained attention by Positron Emission Tomography. Nature. 1991;349:61–64. doi: 10.1038/349061a0. [DOI] [PubMed] [Google Scholar]
- Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998;316(7139):1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfurtscheller G, Neuper C, Krausz G. Functional dissociation of lower and upper frequency mu rhythms in relation to voluntary limb movement. Clinical Neurophysiology. 2000;111(10):1873–1879. doi: 10.1016/s1388-2457(00)00428-4. [DOI] [PubMed] [Google Scholar]
- Rucklidge JJ, Tannock R. Neuropsychological profiles of adolescents with ADHD: Effects of reading difficulties and gender. Journal of Child Psychology and Psychiatry. 2002;43(8):988–1003. doi: 10.1111/1469-7610.00227. [DOI] [PubMed] [Google Scholar]
- Sadato N, Nakamura S, Oohashi T, Nishina E, Fuwamoto Y, Waki A, et al. Neural networks for generation and suppression of alpha rhythm: A PET study. Neuroreport. 1998;9(5):893–897. doi: 10.1097/00001756-199803300-00024. [DOI] [PubMed] [Google Scholar]
- Schreckenberger M, Lange-Asschenfeldt C, Lochmann M, Mann K, Siessmeier T, Buchholz HG, et al. The thalamus as the generator and modulator of EEG alpha rhythm: A combined PET/EEG study with lorazepam challenge in humans. Neuroimage. 2004;22(2):637–644. doi: 10.1016/j.neuroimage.2004.01.047. [DOI] [PubMed] [Google Scholar]
- Seidman LJ, Valera EM, Makris N. Structural brain imaging of attention-deficit/hyperactivity disorder. Biological Psychiatry. 2005;57(11):1263–1272. doi: 10.1016/j.biopsych.2004.11.019. [DOI] [PubMed] [Google Scholar]
- Seig KG, Gaffney GR, Preston DF, Jellings JA. SPECT brain imaging abnormalities in attention deficit hyperactivity disorder. Clinical Nuclear Medicine. 1995;20:55–60. doi: 10.1097/00003072-199501000-00014. [DOI] [PubMed] [Google Scholar]
- Semrud-Clikeman M, Guy K, Griffin JD, Hynd GW. Rapid naming deficits in children and adolescents with reading disabilities and attention deficit hyperactivity disorder. Brain and Language. 2000;75(1):70–83. doi: 10.1006/brln.2000.2337. [DOI] [PubMed] [Google Scholar]
- Shaw JC. Intention as a component of the alpha-rhythm response to mental activity. International Journal of Psychophysiology. 1996;24(1–2):7–23. doi: 10.1016/s0167-8760(96)00052-9. [DOI] [PubMed] [Google Scholar]
- Smalley SL, Loo SK, Yang MH, Cantor RM. Toward localizing genes underlying cerebral asymmetry and mental health. American Journal of Medical Genetics B: Neuropsychiatric Genetics. 2005;135(1):79–84. doi: 10.1002/ajmg.b.30141. [DOI] [PubMed] [Google Scholar]
- Smalley SL, McGough JJ, Del’Homme M, NewDelman J, Gordon E, Kim T, et al. Familial clustering of symptoms and disruptive behaviors in multiplex families with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(9):1135–1143. doi: 10.1097/00004583-200009000-00013. [DOI] [PubMed] [Google Scholar]
- Song DH, Shin DW, Jon DI, Ha EH. Effects of methylphenidate on quantitative EEG of boys with attention-deficit hyperactivity disorder in continuous performance test. Yonsei Medical Journal. 2005;46(1):34–41. doi: 10.3349/ymj.2005.46.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonuga-Barke EJ, Castellanos FX. Spontaneous attentional fluctuations in impaired states and pathological conditions: A neurobiological hypothesis. Neuroscience and Biobehavioral Review. 2007;31(7):977–986. doi: 10.1016/j.neubiorev.2007.02.005. [DOI] [PubMed] [Google Scholar]
- Stefanatos GA, Wasserstein J. Attention deficit/hyperactivity disorder as a right hemisphere syndrome: Selective Literature Review and Detailed Neuropsychological Case Studies. Annals of the New York Academy of Sciences. 2001;931(1):172–195. [PubMed] [Google Scholar]
- Stevens J, Quittner AL, Zuckerman JB, Moore S. Behavioral inhibition, self-regulation of motivation, and working memory in children with attention deficit hyperactivity disorder. Developmental Neuropsychology. 2002;21(2):117–139. doi: 10.1207/S15326942DN2102_1. [DOI] [PubMed] [Google Scholar]
- Strelets V, Garakh Z, Novototskii-Vlasov V, Magomedov R. Relationship between EEG power and rhythm synchronization in health and cognitive pathology. Neuroscience and Behavioral Physiology. 2006;36(6):655–662. doi: 10.1007/s11055-006-0070-4. [DOI] [PubMed] [Google Scholar]
- Stroganova TA, Nygren G, Tsetlin MM, Posikera IN, Gillberg C, Elam M, et al. Abnormal EEG lateralization in boys with autism. Clinical Neurophysiology. 2007;118(8):1842–1854. doi: 10.1016/j.clinph.2007.05.005. [DOI] [PubMed] [Google Scholar]
- Swartwood JN, Swartwood MO, Lubar JF, Timmermann DL. EEG differences in ADHD-combined type during baseline and cognitive tasks. Pediatric Neurology. 2003;28(3):199–204. doi: 10.1016/s0887-8994(02)00514-3. [DOI] [PubMed] [Google Scholar]
- Tannock R, Martinussen R, Frijters J. Naming speed performance and stimulant effects indicate effortful, semantic processing deficits in attention-deficit/hyperactivity disorder. Journal of Abnormal Child Psychology. 2000;28(3):237–252. doi: 10.1023/a:1005192220001. [DOI] [PubMed] [Google Scholar]
- Toga AW, Thompson PM. Mapping brain asymmetry. Nature Reviews. Neuroscience. 2003;4(1):37–48. doi: 10.1038/nrn1009. [DOI] [PubMed] [Google Scholar]
- Tomarken AJ, Davidson RJ, Wheeler RE, Kinney L. Psychometric properties of resting anterior EEG asymmetry: Temporal stability and internal consistency. Psychophysiology. 1992;29(5):576–592. doi: 10.1111/j.1469-8986.1992.tb02034.x. [DOI] [PubMed] [Google Scholar]
- Valera EM, Faraone SV, Murray KE, Seidman LJ. Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biological Psychiatry. 2006 doi: 10.1016/j.biopsych.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Weiler MD, Bernstein JH, Bellinger DC, Waber DP. Processing speed in children with attention deficit hyperactivity disorder, inattentive type. Neuropsychology, Development, and Cognition, Section C, Child Neuropsychology. 2000;6(3):218–234. doi: 10.1076/chin.6.3.218.3156. [DOI] [PubMed] [Google Scholar]
- Willcutt EG, Doyle AE, Nigg JT, Faraone SV, Pennington BF. Validity of the executive function theory of attention-deficit/hyperactivity disorder: A meta-analytic review. Biological Psychiatry. 2005;57(11):1336. doi: 10.1016/j.biopsych.2005.02.006. [DOI] [PubMed] [Google Scholar]
- Zaidel E, Aboitiz F, Clarke JM, Kaiser D, Matteson R. Sex differences in interhemispheric relations for language. In: Kitterle F, editor. Hemispheric communication mechanisms and models. Hillsdale, NJ: Erlbaum; 1995. pp. 85–174. [Google Scholar]
- Zametkin AJ, Liebenauer LL, Fitzgerald GA, King AC, Minkunas DV, Her-scovitch P, et al. Brain metabolism in teenagers with attention-deficit hyperactivity disorder. Archives of General Psychiatry. 1993;50(5):333–340. doi: 10.1001/archpsyc.1993.01820170011002. [DOI] [PubMed] [Google Scholar]
- Zametkin AJ, Nordahl TE, Gross M, King AC, Semple WE, Rumsy J, et al. Cerebral glucose metabolism in adults with hyperactivity of childhood onset. New England Journal of Medicine. 1990;323:1361–1366. doi: 10.1056/NEJM199011153232001. [DOI] [PubMed] [Google Scholar]