Effect of Early Skin-to-Skin Contact on Mother-Preterm Infant Interaction Through 18 Months: Randomized Controlled Trial
High quality mother-infant interaction, particularly during the formative first year, is positively associated with intelligence quotient and school performance in the child's later life (Kelly et al., 1996). However, premature birth exposes both infants and their mothers to an array of different interactions and to a range of developmental risks. Preterm infants look less at their caregivers and respond poorly to sounds, smiles, and levels of play activity (Beckwith & Cohen, 1990; Gerner, 1999); and are less adaptable and more intense (Medoff-Cooper, 1986). Mothers of preterm infants are also stressed by preterm birth (Miles et al., 1992) and perceive a loss and feel guilty about the early abrupt termination of their pregnancies (Affonso et al., 1992).
Skin-to-skin contact (SSC), also known as kangaroo care (KC) or kangaroo mother care (KMC), was originally developed in Bogotá, Colombia in 1978 in response to the shortage of incubators needed to care for low-birth-weight infants (Charpak et al., 2005; Rey & Martinez, 1983). The term KMC is reserved for care given almost continuously and mostly by the mother to facilitate lactation and successful breastfeeding. Until recently, the focus of SSC studies was on physiological measurements of adaptation in preterm infants. These include, such as, temperature, respiration, heart rate, oxygen saturation, weight gain, breastfeeding status, mortality, and morbidity (Bergman & Jurisoo, 1994; Bergman et al., 2004; Cattaneo et al., 1998; Ludington-Hoe et al., 2004; Suman et al., 2008) and on sleep organization (Ludington-Hoe et al., 2006). Results of these studies have shown that SSC promotes beneficial physiological conditions such as increased quiet sleep state and more stable thermoregulation, heart rate, respiratory rate, and higher oxygen saturation.
Effects of SSC on mothers of preterm infants
When mothers of preterm infants were studied, the focus was on the psychological response of the mother to her SSC experience. With a sample of Swedish mothers, Affonso et al. (1989) were the first to report the effect of SSC on maternal feelings toward their infants during and after SSC. In a subsequent study, Affonso et al. (1993) examined the effect of SSC on the reaction of American mothers to stable, very-low- and low-birth-weight preterm infants in a tertiary level intensive care nursery. These researchers found that SSC provided a way for mothers to know their infants, to develop strong positive feelings towards them, and to reconcile their feelings about having a premature birth, so that emotional healing could take place. In another qualitative study, Roller (2005) interviewed 10 mothers who experienced SSC with their preterm infants. Interviews occurred after the infants were discharged from the hospital. Two essential themes that emerged from the SSC experience were “kept from knowing” her infant and “getting to know” her preterm infant. In short, mothers felt that SSC (termed KC in this study) provided an opportunity for them to get to know more about their infants during a stressful time.
Similar positive psychological responses were also found in mothers of intubated preterm infants. Gale et al. (1993) and Neu (1999) both found that after experiencing SSC, parents (mostly mothers) reported stronger identification with and knowledge of their preterm infants. Most recently, Johnson (2007) interviewed a group of 18 primiparous mothers who experienced 60 minutes of SSC with their preterm infants three times in the first two weeks post-birth. These infants were either receiving ventilator support or oxygen therapy. After SSC, mothers expressed their feelings as “heart-warming,” “being needed,” and “having confidence in knowing” how to care for her infant.
Long-term effects of SSC on mother-preterm infant interaction
In a Cochrane review, Moore, Anderson, and Bergman (2007) reported more maternal affectionate touching and attachment behaviors at follow-up in randomized controlled trials (RCTs) with mothers of fullterm infants who experienced SSC. However, only one RCT has been conducted (Charpak, Ruis-Pelaez, Figueroa, & Charpak, 1997) in which long-term effects of SSC on mother-preterm infant interaction (MPI) have been reported (Tessier et al., 1998). In this RCT (N = 488) which was conducted in Bogota, Colombia, 488 mothers were encouraged to provide KMC for their infants 24 hours a day. An objective instrument, Nursing Child Assessment Feeding Scale, was used to measure maternal perception and the state of each mother’s readiness to respond to her infant’s needs at 41 weeks post-conception. KMC dyads had higher scores on maternal sensitivity (a subscale of the feeding scale) than controls (p = .05).
Positive effects of SSC on MPI and infant and family health were also reported in three publications from a matched-control study conducted with 146 preterm infants in two hospitals in Jerusalem, Israel. Feldman, Eidelman et al. (2002) reported that at 37 weeks’ gestation, SSC mothers were less depressed and had more positive affect, touch, adaptation to infant cues, and perception of their infants. At three months SSC parents were more sensitive and provided a better home environment and SSC infants scored higher on the Bayley Mental and Motor Developmental Indices. Feldman, Weller et al. (2002) found that at hospital discharge SSC infants had more mature state distribution and organized sleep-wake cycle and at three months SSC infants were more tolerant to negative maternal emotion, displayed less negative affect, and their parents were more sensitive and less intrusive. SSC parents also demonstrated more affectionate touching of their infants and of each other, and more often held their infants in a position conducive to mutual gaze and touch. At six months, SSC mother-infant dyads shared attention, and infants’ sustained exploration of their environment began sooner and lasted longer. Feldman, Weller et al. (2003) found that SSC had a positive impact on mother-infant interaction, father-infant interaction, and the spousal relationship. Feldman and Eidelman (2003) then conducted a prospective case-control study in one hospital with 70 very-low- and low-birth-weight preterm infants. The 35 infants who experienced SSC for at least one hour a day for 14 days had significantly more rapid maturation of vagal tone between 32 and 37 weeks' gestation and better behavioral organization (e.g., longer periods of quiet sleep and alert wakefulness, and shorter periods of active sleep).
In a historical-control study with healthy low-birth-weight infants, Ohgi et al. (2002) found that SSC infants scored higher than controls on behavioral organization during the neonatal period and on the Bayley Developmental Indices at 12 months. In a comparison study in Italy, Tallandini and Scalembra (2006) examined the effects of KMC on very-low-birth-weight preterm infants and their mothers. Control dyads (n = 21) received routine care and KMC dyads (n = 19), who experienced SSC for at least one hour per day for a mean of 24.37 days (SD = 11.06). KMC mothers wee were less emotionally stressed while in the hospital, and mother-infant interaction was better 38 gestational weeks.
The above review supports the beneficial effects of SSC on mother-preterm infant interaction. However, the focus of most of these was on subjective self-report of maternal feelings during or shortly after SSC. When an objective measure was used, follow-up data were collected only once at 41 weeks’ gestation (Tessier et al., 1998) or once right after hospital discharge (Tallandini & Scalembra, 2006), or the study was not an RCT (Feldman & Eidelman, 2003; Feldman, Eidelman et al., 2002; Feldman, Weller et al., 2002, 2003; Ohgi et al., 2002; Tallandini & Scalembra).
Inspired by the early work of Ourth and Brown (1961), Kennell et al. (1974), and Klaus et al. (1972), the Mutual Caregiving Model was developed by the second author (1972, 1977, 1989). Briefly stated, beginning with birth, the ideal habitat (ecological niche) for each newborn infant is the specific and relatively familiar milieu provided by its mother. Although human infants are born with the skills needed to survive and be nourished in a self-regulatory fashion, this can only happen optimally if infants remain with their mothers in this habitat and in skin-to-skin contact. This experience promotes a broad parasympathetic (vagal) response (e.g., glandular secretion), which is physiologically beneficial and comforting for both mother and infant and would logically promote bonding and attachment. Similar conceptualizations have been set forth by others (e.g., Bergman et al., 2004; Labbok & Krasovec, 1990; Uvnäs-Moberg, 1998; Widström et al., 1987; Winberg, 2005). Thus, an RCT was conducted to further examine the effects of early SSC on the health of preterm infants and their mothers during their hospital stay and through 18 months. Two publications have resulted from this RCT to date. Anderson et al. (2003) reported mother-infant contact information during the first two days’ postbirth, and Hake-Brooks & Anderson (2008) focused on breastfeeding duration and exclusivity of mother-infant dyads in the hospital and through 18 months. The purpose of the report presented here was to examine the effect of SSC on mother-preterm infant interaction at 6, 12, and 18 months.
Methods
Design and Sample
This two-group RCT was conducted at University Hospitals of Cleveland, Cleveland, Ohio, a large urban teaching and research hospital and Kadlec Medical Center, Richland, Washington, a regional hospital in a somewhat rural setting. Approval from the Institutional Review Board was obtained at each site. Eligibility was established and informed consent was obtained during early labor. Inclusion and exclusion criteria are delineated elsewhere (Anderson et al., 2003). After birth, mothers and their preterm infants who remained eligible were randomized using minimization to either SSC or control group.
Results of a pilot RCT by Syfrett (1993) were used for sample size estimation. With a power of .8, alpha of .01 (two tailed), and a medium-sized effect, a sample of 33 dyads per group were needed. To protect possible attrition during the follow-up phase, 50 dyads per group were recruited. Between 1997 and 2000, 75 dyads were randomized at the midwestern hospital and 25 at the northwestern hospital.
Instrumentation
The computerized minimization program contains an algorithm for minimizing between-group imbalance of potential confounding factors (Conlon & Anderson, 1990; Zeller et al., 1997). This program was developed using principles introduced by Pocock and Simon (1975). Researchers can choose only factors already known (e.g., delivery method) because this information must be entered into the computer before the minimization program can be run. Thirteen prognostic factors were chosen for randomization: maternal factors (socioeconomic status, race, parity, smoking, feeding intent, MgSO4 use, epidural use, delivery method, dexamethosone use) and infant factors (gender, NICU or not, gestational age, and birth time).
To avoid potential selection bias for the first 10 dyads, one investigator (GCA) created an abbreviated permuted block sequence with randomly selected blocks of six and then four. First 10 envelopes were labeled 1 to 10. Then 6 papers (3 labeled SSC and 3 Control), were tightly folded, placed into a bag, and vigorously stirred. Next one paper was randomly selected and placed, still folded, in Envelope 1 which was then sealed. Envelopes 2 to 6 were filled in the same manner. This procedure was repeated with 4 additional papers (2 SSC; 2 Control) and Envelopes 7 to 10. This process also minimized the history threat to internal validity because group size increased at a relatively balanced yet unpredictable rate until the minimization program could begin.
The Nursing Child Assessment Satellite Training Program (NCAST) Feeding and Teaching scales (Sumner & Spietz, 1994a, b) were used to measure MPI. The feeding scale has a possible 76 points and the teaching scale has 73. The feeding scale can be used with infants from birth to one year, the teaching scale with infants from birth to 3 years. Both scales consist of six subscales to assess mother-infant interaction: sensitivity to cues, response to infant distress, social-emotional growth fostering, cognitive growth fostering, clarity of cues, and responsiveness of the child to the caregiver. Each subscale lists a series of caregiver and infant behaviors that the evaluator observes during a routine feeding session and a teaching session. In the teaching session, the mother teaches her infant a task she thinks the infant will not know how to do. The scales consist of binary (yes/no) items. All items rated yes are summed. A higher score indicates an interaction that is richer in positive affect, sensitivity, synchronicity, vocalization, and reciprocity. The feeding and teaching scales have established validity and reliability (Sumner & Spietz, 1994a, b).
Before starting the MPI assessment, several research team members, including the first author, received training from an NCAST certified instructor to reach at least 85% accuracy in scoring standardized reliability videotapes of feeding and teaching sessions. After each follow-up, interactions were scored by the first author and other members of the research team who were masked to group assignment. Then, 10% of randomly selected tapes were scored for interrater reliability, which was maintained at 90% throughout the scoring period.
In-Hospital Procedure and Intervention
Informed consent was obtained during early labor. On the day of delivery, after the infants were born and as soon as continuing eligibility was established, mother-infant dyads were randomly assigned to either the SSC or control group. Dyads in both groups received routine care from hospital staff. Control dyads were cared for in incubators, warmer beds, or bassinettes and were held wrapped in blankets. In addition, SSC dyads were encouraged to begin experiencing SSC as early, as often, and for as long each time as possible.
For those dyads who were able to begin SSC immediately following birth, infants were placed prone between their mother’s breasts and covered across the back with a large warming blanket folded in half and tucked slightly under the mother on both sides. Infants wore a cap that often became damp and was then replaced with a dry one. If SSC began later mothers held their infants between their breasts with either their hospital gown or their own clothing and a blanket folded across the infant's back for warmth. Infants wore a small diaper and often, a cap.
Mothers in both groups were contacted frequently for data collection by the researchers, who also provided brief support if needed or requested at these times. The presence of the nurse researchers was approximately equal in both groups because of the identical and numerous data collection points in the protocol. Details of recruitment, randomization, intervention, and in-hospital data collection are in Anderson et al. (2003) and Hake-Brooks & Anderson (2008).
Follow-up Procedure
Follow-up assessment of MPI occurred when infants reached 6, 12 and 18 months corrected age. Before each follow-up, a member of the research team arranged the visit at a meeting time convenient for mother and infant. Many follow-up visits were done on weekends. Transportation was provided by taxi as needed. At the Ohio site, when mothers returned for follow-up visits, a research member greeted each mother and her infant at the entrance to the hospital lobby and escorted them to a private room in a clinic. The clinic, used primarily for research studies, was well lighted and quiet. Similar procedures were carried out at the Washington site, except that mothers and infants returned for follow-up to an outpatient clinic. During these visits each dyad was videotaped during a feeding session at 6 and 12 months and during a teaching session at 6, 12, and 18 months. Mothers also completed several sets of questionnaires, and infants were assessed for growth and development using the Bayley Scale of Infant Development II (Bayley, 1993) by trained research staff. Although the members who contacted mothers to make follow-up arrangements were aware of the group assignment of each mother-infant dyad, the research staff involved in follow-up assessments were not aware of group assignment. At the completion of each visit, remuneration was provided. All follow-up assessments were completed by the end of 2001.
Results
In-Hospital Sample
Of the 491 women approached during a period of four years, 229 (47%) declined to participate. Reasons provided fell into two main categories: study too complicated and not interested in research. Of the 262 women (53%) who consented, 100 (38%) were studied; 52 were randomized to the SSC group and 48 to the control group (Figure 1). During the in-hospital phase, five dyads (2 SSC; 3 controls) withdrew. Reasons were: three mothers (2 SSC; 1 control) did not want their infant connected to a monitor; one control mother did not provide a reason; and one control mother wanted to have SSC with her infant.
Figure 1.
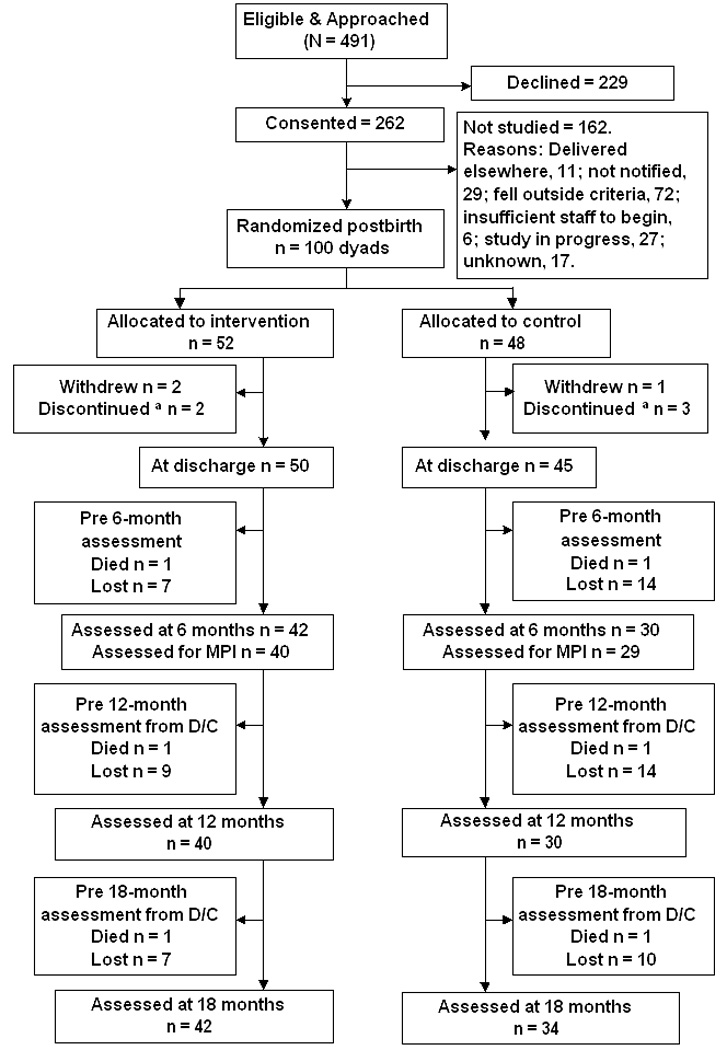
CONSORT diagram of all possible and actual dyads returned for mother-preterm infant interaction (MPI) assessment at follow-up.
aDyads who discontinued their in-hospital participation agreed to participate during follow-up. D/C = discharge.
Five dyads (3 SSC; 2 controls) discontinued their in-hospital participation but agreed to participate during follow-up. Reasons for discontinuation included infant on ventilator support (1 SSC; 1 control), hospital transfer (1 control), not wanting infant connected to the monitor (1 SSC), and maternal illness (1 SSC). At hospital discharge, 95 dyads were eligible for follow-up. No demographic between-group differences were found (Table 1). Two of the 50 SSC dyads did not experience SSC because the infants required ventilator support. The remaining 48 dyads first experienced SSC at a mean of 9.9 hours (SD: 11.3, range: 0.5 to 42.1), for an average 11.6 times (SD: 5.2, range: 1 to 25), and for an average 1.3 hours each time (SD: 0.5, range: 0.5 to 2.5). Seven dyads (14.6%) experienced SSC during the first hour postbirth and 41 (85.4%) within the first 24 hours. During the study duration (ranging from 2 to 5 days), these dyads spent 17.7% (SD: 13.3, range: 3 to 63%) in SSC holding.
Table 1.
Selected Demographics of All Possible Dyads by Group at Discharge (N = 95)
| SSC (n = 50) |
Control (n = 45) |
||||
|---|---|---|---|---|---|
| Variables | M | SD | M | SD | p |
| Maternal age at delivery (year) | 25.0 | 6.3 | 24.4 | 5.8 | .63 |
| 1-minute APGAR | 7.4 | 1.4 | 7.6 | 1.4 | .59 |
| 5-minute APGAR | 8.6 | 0.8 | 8.6 | 0.6 | .90 |
| Birth weight (g) | 2257 | 426 | 2211 | 394 | .59 |
| Gestational age (wk) | 34.4 | 1.6 | 34.6 | 1.4 | .54 |
| n | % | n | % | ||
| Gestational age | |||||
| Moderately preterm (32–33) | 17 | 34 | 13 | 30 | .59 |
| Late preterm (34 -< 37) | 33 | 66 | 32 | 71 | |
| Delivery method | |||||
| Vaginal | 39 | 78 | 34 | 76 | .78 |
| Cesarean section | 11 | 22 | 11 | 24 | |
| Marital status | |||||
| Single | 29 | 58 | 28 | 62 | .68 |
| Married | 21 | 42 | 17 | 38 | |
| Maternal race | |||||
| Non-White | 30 | 60 | 28 | 62 | .82 |
| White | 20 | 40 | 17 | 38 | |
| Parity | |||||
| Primipara | 25 | 50 | 19 | 42 | .45 |
| Multipara | 25 | 50 | 26 | 58 | |
| Insurance status | |||||
| Public | 21 | 42 | 20 | 44 | .81 |
| Private | 29 | 58 | 25 | 56 | |
| Feeding Intent | |||||
| Bottle | 14 | 32 | 16 | 36 | .43 |
| Breast | 36 | 68 | 29 | 64 | |
| Child’s sex | |||||
| Female | 23 | 46 | 26 | 58 | .25 |
| Male | 27 | 54 | 19 | 42 | |
| NICU admission | |||||
| Yes | 34 | 68 | 30 | 67 | .89 |
| No | 16 | 32 | 15 | 33 | |
| Ventilator supporta | |||||
| Yes | 9 | 18 | 5 | 11 | .34 |
| No | 41 | 82 | 40 | 89 | |
SSC did not begin until infants were no longer receiving ventilator support.
Follow-Up Sample
Before the six-month follow-up, two female infants (1 SSC; 1 control) died due to Sudden Infant Death Syndrome. The SSC infant was born at 32 weeks gestation to a 20-year-old Hispanic mother and died at 5 months of age. The control infant was born at 34 weeks gestation to a 25-year-old African American mother and died before 3 months of age. Demographics for these two infants were included in the lost to follow-up columns for analysis purposes (Table 2).
Table 2.
Comparison of Maternal/Infant Demographics of Returned to Lost Dyads at 6, 12, and 18-Month Follow-ups
| 6 Months | 12 Months | 18 Months | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Returned (n = 72) |
Lost (n = 23) |
Returned (n = 70) |
Lost (n = 25) |
Returned (n = 76) |
Lost (n = 19) |
||||||||||
| Variable | M | SD | M | SD | p | M | SD | M | SD | p | M | SD | M | SD | p |
| Maternal age (yr) | 25.3 | 6.1 | 23.0 | 5.7 | .11 | 25.1 | 6.3 | 23.5 | 5.0 | .24 | 25.0 | 6.2 | 23.5 | 5.3 | .33 |
| 1 minute APGAR | 7.5 | 1.3 | 7.4 | 1.7 | .57 | 7.6 | 1.3 | 7.2 | 1.6 | .30 | 7.6 | 1.3 | 7.1 | 1.7 | .26† |
| 5 minute APGAR | 8.6 | 0.7 | 8.4 | 0.8 | .16 | 8.7 | 0.6 | 8.3 | 0.8 | .03† | 8.6 | .63 | 8.3 | .89 | .16† |
| Birth weight (g) | 2277 | 405 | 2104 | 402 | .08 | 2262 | 416 | 2162 | 389 | .30 | 2266 | 415 | 2115 | 373 | .15 |
| Gestation (wk) | 34.6 | 1.5 | 34.0 | 1.4 | .10 | 34.6 | 1.5 | 34.1 | 1.4 | .21 | 34.6 | 1.5 | 33.8 | 1.4 | .04 |
| n | % | n | % | n | % | n | % | n | % | n | % | ||||
| Group assignment | |||||||||||||||
| SSC | 42 | 58 | 8 | 35 | .05 | 40 | 57 | 10 | 40 | .14 | 42 | 55 | 8 | 42 | .30 |
| Control | 30 | 42 | 15 | 65 | 30 | 43 | 15 | 60 | 34 | 45 | 11 | 58 | |||
| Delivery method | |||||||||||||||
| Vaginal | 53 | 74 | 20 | 87 | .19 | 20 | 29 | 2 | 8 | .04 | 56 | 74 | 17 | 90 | .14 |
| Cesarean section | 19 | 26 | 3 | 13 | 50 | 71 | 23 | 92 | 20 | 26 | 2 | 11 | |||
| Marital status | |||||||||||||||
| Single | 37 | 51 | 20 | 87 | .002 | 36 | 51 | 21 | 84 | .004 | 43 | 57 | 14 | 74 | .17 |
| Married | 35 | 49 | 3 | 13 | 34 | 49 | 4 | 16 | 33 | 43 | 5 | 26 | |||
| Maternal race | |||||||||||||||
| Non-White | 40 | 56 | 18 | 78 | .05 | 38 | 54 | 20 | 80 | .02 | 44 | 58 | 14 | 74 | .21 |
| White | 32 | 44 | 5 | 22 | 32 | 46 | 5 | 20 | 32 | 42 | 5 | 26 | |||
| Parity | |||||||||||||||
| Primipara | 35 | 49 | 9 | 39 | .43 | 36 | 51 | 8 | 32 | .09 | 37 | 49 | 7 | 37 | .35 |
| Multipara | 37 | 51 | 14 | 61 | 34 | 49 | 17 | 68 | 39 | 51 | 12 | 63 | |||
| Insurance status | |||||||||||||||
| Public | 27 | 38 | 14 | 61 | .05 | 28 | 40 | 13 | 52 | .30 | 31 | 41 | 10 | 53 | .35 |
| Private | 45 | 63 | 9 | 39 | 42 | 60 | 12 | 48 | 45 | 59 | 9 | 47 | |||
| Feeding Intent | |||||||||||||||
| Bottle | 24 | 33 | 6 | 26 | .52 | 20 | 29 | 10 | 40 | .29 | 25 | 33 | 5 | 26 | .58 |
| Breast | 48 | 67 | 17 | 74 | 50 | 71 | 15 | 60 | 51 | 67 | 14 | 74 | |||
| Child’s sex | |||||||||||||||
| Female | 36 | 50 | 13 | 57 | .59 | 37 | 53 | 12 | 48 | .68 | 41 | 54 | 8 | 42 | .36 |
| Male | 36 | 50 | 10 | 44 | 33 | 47 | 13 | 52 | 35 | 46 | 11 | 58 | |||
| NICU admission | |||||||||||||||
| Yes | 46 | 64 | 18 | 78 | .20 | 25 | 36 | 6 | 24 | .28 | 51 | 67 | 13 | 68 | .91 |
| No | 26 | 36 | 5 | 22 | 45 | 64 | 19 | 76 | 25 | 33 | 6 | 32 | |||
| Ventilator support | |||||||||||||||
| Yes | 11 | 15 | 3 | 13 | .79 | 12 | 83 | 2 | 92 | .27 | 12 | 84 | 2 | 11 | .56 |
| No | 61 | 85 | 20 | 87 | 58 | 17 | 23 | 8 | 64 | 16 | 17 | 90 | |||
Note. Percents are column percents. Percents do not always add to 100 because of rounding.
indicates the result of separate variance t-tests
Although 95 dyads were eligible for the 6-month follow-up at hospital discharge, assessment measures for MPI were not in place until Dyad 7. Therefore, only 69 of the 72 dyads who returned for the 6-month follow-up could be assessed. At the 12-month follow-up, 71 dyads returned. One SSC dyad did not complete the feeding session because the infant was hungry and was fed just before arriving for follow-up. The other SSC infant was brought to follow-up by her foster mother, not her biological mother, so feeding and teaching assessments were not done and the infant was considered lost to follow-up. Therefore, 69 dyads were assessed for feeding interactions and 70 for teaching interactions. At 18 months, 76 dyads returned for follow-up and all had teaching sessions.
Among the five dyads that discontinued in-hospital participation, two SSC dyads returned for all follow-up visits. The other three dyads (1 SSC; 2 controls) returned at 12 and 18-months. Reasons for attrition included having one’s phone disconnected, not responding to request for follow-up, moving without leaving a forwarding address, moving out of the state, not coming to a scheduled follow-up, and no longer having custody of the infant. A CONSORT diagram of the number of all possible dyads for all follow-ups is presented in Figure 1.
Analyses for demographic variables were conducted between dyads who returned for follow-up and completed MPI assessment and those who did not at 6, 12, and 18 months (Table 2). At 6-months, married mothers were significantly more likely to return compared to single mothers (p = .002). At 12-months, married, White mothers, or infants born vaginally were more likely to return compared to single (p = .004), non-white (p = .02) mothers, or infants born by cesarean (p = .04). Infants who returned had higher 5-minute APGAR scores (p = .03). At 18-months, infants who returned had a slightly longer gestation (p = .04). All comparisons are presented in Table 2. No differences were found when demographics were further examined based on group assignment (Table 3, Table 4, & Table 5).
Table 3.
Maternal and Infant Characteristics of Returned Dyads by Group at 6-month Follow-up (N = 69)
| Variables |
SSC (n = 40) M ± SD |
Control (n = 29) M ± SD |
p |
|---|---|---|---|
| Maternal age at delivery (yr) | 26.1 ± 6.3 | 24.2 ± 5.9 | .22 |
| 1-minute APGAR | 7.5 ± 1.4 | 7.6 ± 1.3 | .88 |
| 5-minute APGAR | 8.6 ± 0.7 | 8.7 ± 0.6 | .85 |
| Birthweight (g) | 2288 ± 385 | 2262 ± 438 | .62 |
| Gestational age (wk) | 34.6 ± 1.5 | 34.7 ± 1.4 | .70 |
| n (%) | n (%) | ||
| Gestational age | |||
| Moderately preterm (32–33) | 12 (30) | 9 (31) | .93 |
| Late preterm (34 -< 37) | 28 (70) | 20 (69) | |
| Delivery method | |||
| Vaginal | 31 (78) | 19 (66) | .27 |
| Cesarean section | 9 (23) | 10 (35) | |
| Martial status | |||
| Single | 20 (50) | 15 (52) | .89 |
| Married | 20 (50) | 14 (48) | |
| Maternal race | |||
| Non-white | 23 (58) | 15 (52) | .63 |
| White | 17 (43) | 14 (48) | |
| Parity | |||
| Primipara | 18 (45) | 15 (52) | .58 |
| Multipara | 22 (55) | 14 (48) | |
| Insurance | |||
| Public | 15 (38) | 10 (35) | .80 |
| Private | 25 (63) | 19 (66) | |
| Feeding Intent | |||
| Bottle | 11 (28) | 11 (38) | .36 |
| Breast | 29 (73) | 18 (62) | |
| Child’s sex | |||
| Female | 18 (45) | 18 (62) | .16 |
| Male | 22 (55) | 11 (38) | |
| NICU admission | |||
| Yes | 27 (68) | 17 (59) | .45 |
| No | 13 (33) | 12 (41) | |
| Ventilator support | |||
| Yes | 7 (17) | 4 (13) | .70 |
| No | 35 (83) | 26 (87) | |
Note. Percents are column percents. Percents do not always add to 100 because of rounding.
Table 4.
Maternal and Infant Characteristics of Returned Dyads by Group at 12-month Follow-up (N = 70)
| Variables |
SSC (n = 40) M ± SD |
Control (n = 30) M ± SD |
p |
|---|---|---|---|
| Maternal age at delivery (yr) | 25.3 ± 6.4 | 24.9 ± 6.3 | .80 |
| 1-minute APGAR | 7.5 ± 1.3 | 7.7 ± 1.3 | .54 |
| 5-minute APGAR | 8.7 ± 0.7 | 8.7 ± 0.6 | .96 |
| Birthweight (g) | 2247 ± 429 | 2281 ± 404 | .73 |
| Gestational age (wk) | 34.4 ± 1.6 | 34.8 ± 1.3 | .35 |
| n (%) | n (%) | ||
| Gestational age | |||
| Moderately preterm (32–33) | 14 (35) | 7(23) | .29 |
| Late preterm (34 -< 37) | 26 (65) | 23 (77) | |
| Delivery method | |||
| Vaginal | 30 (75) | 20 (67) | .45 |
| Cesarean section | 10 (25) | 10 (33) | |
| Martial status | |||
| Single | 20 (50) | 16 (53) | .78 |
| Married | 20 (50) | 14 (47) | |
| Maternal race | |||
| Non-white | 22 (55) | 16 (53) | .89 |
| White | 18 (45) | 14 (47) | |
| Parity | |||
| Primipara | 21 (53) | 15 (50) | .84 |
| Multipara | 19 (48) | 15 (50) | |
| Insurance | |||
| Public | 16 (40) | 12 (40) | 1.0 |
| Private | 24 (60) | 18 (60) | |
| Feeding Intent | |||
| Bottle | 9 (23) | 11 (37) | .19 |
| Breast | 31 (78) | 19 (63) | |
| Child’s sex | |||
| Female | 19 (48) | 18 (60) | .30 |
| Male | 21 (53) | 12 (40) | |
| NICU admission | |||
| Yes | 27 (68) | 18 (60) | .52 |
| No | 13 (33) | 12 (40) | |
| Ventilator support | |||
| Yes | 8 (21) | 4 (13) | .46 |
| No | 32 (80) | 26 (87) | |
Note. Percents are column percents. Percents do not always add to 100 because of rounding.
Table 5.
Maternal and Infant Characteristics of Returned Dyads by Group at 18-month Follow-up (N = 76)
| Variables |
SSC (n = 42) M ± SD |
Control (n = 34) M ± SD |
p |
|---|---|---|---|
| Maternal age at delivery (yr) | 25.1 ± 6.2 | 24.9 ± 6.2 | .91 |
| 1-minute APGAR | 7.5 ± 1.3 | 7.7 ± 1.3 | .62 |
| 5-minute APGAR | 8.6 ± 0.7 | 8.6 ± 0.6 | .86 |
| Birthweight (g) | 2260 ± 427 | 2273 ± 406 | .90 |
| Gestational age (wk) | 34.5 ± 1.6 | 34.8 ± 1.3 | .33 |
| n (%) | n (%) | ||
| Gestational age | |||
| Moderately preterm (32–33) | 14 (33) | 8 (24) | .35 |
| Late preterm (34 -< 37) | 28 (67) | 26 (77) | |
| Delivery method | |||
| Vaginal | 32 (76) | 24 (71) | .58 |
| Cesarean section | 10 (24) | 10 (29) | |
| Martial status | |||
| Single | 23 (55) | 20 (59) | .72 |
| Married | 19 (45) | 14 (41) | |
| Maternal race | |||
| Non-white | 25 (60) | 19 (56) | .75 |
| White | 17 (41) | 15 (44) | |
| Parity | |||
| Primipara | 22 (52) | 15 (44) | .47 |
| Multipara | 20 (48) | 19 (56) | |
| Insurance | |||
| Public | 18 (43) | 13 (38) | .68 |
| Private | 24 (57) | 21 (62) | |
| Feeding Intent | |||
| Bottle | 12 (29) | 13 (38) | .37 |
| Breast | 30 (71) | 21 (62) | |
| Child’s sex | |||
| Female | 19 (45) | 22 (65) | .09 |
| Male | 23 (55) | 12 (35) | |
| NICU admission | |||
| Yes | 30 (71) | 21 (62) | .37 |
| No | 12 (29) | 13 (39) | |
| Ventilator support | |||
| Yes | 8 (19) | 4 (12) | .39 |
| No | 34 (81) | 30 (88) | |
Note. Percents are column percents. Percents do not always add to 100 because of rounding.
Mother-Infant Interaction
Descriptive statistics (mean and standard deviation) and intention-to-treat analysis were used to describe and analyze data related to mother-infant interaction. Between-group differences in feeding and teaching scores were examined using student t-tests. To avoid inflating a Type 1 error, total teaching and feeding scores were first compared at each follow-up, followed by comparisons of the Mother Total and Child Total scores. SSC mothers and infants had higher total feeding scores at 6 and 12 months. When examining mothers and infants separately, SSC mothers had slightly higher Mother Total feeding scores at 6 and 12-months. SSC and control infants had comparable Infant Total feeding scores (Table 6). Total Teaching scores were similar between groups throughout follow-up. SSC mothers had consistently higher Mother Total scores at all three follow-ups. In contrast, SSC infants had lower Infant Total scores at 6 months (p = .001) but not at 12- and 18-months. Upon further analysis, at 6-month follow-up, control infants had higher scores on the Child’s Response to Caregiver sub-scale (p = .001) (Table 7).
Table 6.
Six and 12-Month Feeding Scores by Group
| 6-Month | 12-Month | |||||
|---|---|---|---|---|---|---|
| SSC n = 40 |
Control n = 29 |
SSC n = 39 |
Control n = 30 |
|||
| Feeding Scalesa | M (SD) | M (SD) | p | M (SD) | M (SD) | p |
| Mother | ||||||
| Sensitivity to cues (16) | 13.1 (1.8) | 12.9 (2.0) | .74 | 12.5 (1.6) | 12.1 (2.1) | .40 |
| Responses to distress (11) | 9.7 (1.2) | 9.6 (1.5) | .73 | 9.6 (1.5) | 9.7 (1.5) | .72 |
| Social-emotional growth fostering (14) | 11.6 (1.6) | 11.4 (1.6) | .66 | 11.7 (1.6) | 11.1 (1.9) | .16 |
| Cognitive fostering (9) | 6.8 (1.6) | 6.6 (1.7) | .49 | 7.6 (1.4) | 7.3 (1.5) | .38 |
| Mother total score (50) | 41.2 (3.9) | 40.4 (4.9) | .46 | 41.2 (3.9) | 40 (5.2) | .29 |
| Infant | ||||||
| Clarity of cues (15) | 12.8 (1.5) | 13.0 (1.7) | .63 | 12.9 (1.7) | 13 (1.9) | .78 |
| Response to mother (11) | 7.4 (1.5) | 7.6 (1.8) | .66 | 7.6 (1.3) | 7.5 (2) | .85b |
| Infant total score (26) | 20.2 (2.8) | 20.5 (3.1) | .61 | 20.5 (2.4) | 20.5 (3.4) | .96 |
| Total feeding score (76) | 61.4 (6.0) | 60.9 (6.9) | .79 | 61.5 (5.2) | 60.5 (7.7) | .57b |
Numbers in parentheses in this column indicate maximum scores for each scale.
Indicates the result of separate variance t-tests.
Table 7.
Six, 12-, and 18-Month Teaching Scores by Group
| 6-Month |
12-Month |
18-Month |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| SSC n = 40 |
Control n = 29 |
SSC n = 40 |
Control n = 30 |
SSC n = 42 |
Control n = 34 |
||||
| M (SD) | M (SD) | p | M (SD) | M (SD) | p | M ± SD | M ± SD | p | |
| Teaching Scalesa | |||||||||
| Mother | |||||||||
| Sensitivity to cues (11) | 8.9 (1.1) | 8.5 (1.2) | .16 | 8.9 (1.2) | 8.3 (1.2) | .05 | 8.6 (1.6) | 8.2 (1.4) | .36 |
| Responses to distress (11) | 10.0 (1.1) | 9.6 (1.3) | .17 | 9.4 (1.7) | 9.3 (1.5) | .72 | 9.4 (1.9) | 9.2 (1.7) | .57 |
| Social-emotional growth fostering (11) | 8.1 (1.4) | 8.1 (1.0) | .97 | 8.3 (1.4) | 8 (1.5) | .39 | 8.3 (1.4) | 8.6 (1.2) | .35 |
| Cognitive fostering (17) | 11.4 (2.5) | 11.1 (2.9) | .68 | 11.9 (2.3) | 11.5 (2.4) | .49 | 12.5 (2.6) | 12.4 (2.5) | .90 |
| Mother total (50) | 38.3 (4.4) | 37.3 (4.5) | .34 | 38.3 (4.8) | 37.1 (4.7) | .29 | 35.5 (13.3) | 34.2 (14.4) | .68 |
| Infant | |||||||||
| Clarity of cues (10) | 8.3 (1.2) | 8.7 (0.7) | .07 | 9.0 (0.9) | 9.2 (1.0) | .37 | 9.1 (.8) | 9.3 (.7) | .29 |
| Response to mother (13) | 8.4 (2.3) | 10.0 (1.6) | .001 | 9.0 (2.0) | 9.6 (2.5) | .29 | 8.7 (1.8) | 9.4 (2.5) | .20 |
| Infant total (23) | 16.7 (3.2) | 18.8 (1.8) | .001 | 18.0 (2.4) | 18.8 (3.3) | .26 | 17.8 (2.2) | 18.7 (2.9) | .17 |
| Total teaching score (73) | 55.1 (6.6) | 56.0 (5.0) | .51 | 56.5 (5.1) | 55.2 (5.7) | .32 | 56.7 (5.4) | 56.7 (4.9) | .97 |
Numbers in parentheses in this column indicate maximum scores for each scale.
Discussion
Mother-infant interaction is a complex phenomenon. Positive impact of SSC on feelings of mothers of preterm infants has been reported in several studies (e.g., Affonso et al., 1989, 1993; Dombrowski et al., 2000; Moran et al., 1999; Neu, 1999; Roller, 2005; Roller et al., 1999; Swinth et al., 2000). In most recent publications, SSC mothers were more sensitive and less intrusive, and their infants showed less negative emotion and more dyadic reciprocity (Feldman & Eidelman, 2003; Feldman, Eidelman et al., 2002; Feldman, Weller et al., 2002; Feldman, Weller et al., 2003; Tallandini & Scalembra, 2006).
Although other SSC study findings appeared similar at first, more careful examination revealed dissimilarities between studies to allow valid comparisons, such as study design (Feldman, Weller et al., 2003) and infant populations (Sloan et al., 1994; Rojas et al., 2003). Other examples include Tallandini and Scalembra (2006) who used the same instrument but their study was not a randomized trial and follow-up was done shortly after discharge. Findings most similar to our study are by Tessier et al. (1998) in terms of study design (RCT) and one instrument (NCAST feeding scale) used to measure MPI. Reporting on follow-up outcomes from the RCT conducted by Charpak et al. (1997) in which only the NCAST feeding scale was used, these researchers found that the SSC experience was not directly related to MPI in 488 preterm infants at 41 weeks’ post-conception age. Although they found that SSC mothers were more sensitive than controls to needs of their infants during a feeding session, the difference was very small. Results of our study were similar. SSC and control mother-preterm infant dyads had similar mother-infant interactions. In addition, SSC mothers, compared to controls, demonstrated consistently slightly higher scores in both feeding and teaching interactions throughout follow-ups. The strength of our study compared to Tessier’s study is that we, in addition to the NCAST feeding scale, used the NCAST teaching scale to assess MPI.
In our study SSC infants often scored lower than control infants, especially at the 6-month teaching session, in which SSC infants were significantly less likely to respond to their caregiver’s cues. The fact that this difference was not apparent at 12 and 18 months suggests that SSC infants might have been at a qualitatively different developmental stage than the controls at 6 months (cf. Lewis & Ramsey, 1995). However we have no data to support this suggestion and can only recommend that such data be collected in future studies.
Several other possible explanations merit consideration effects of SSC on MPI. First, attrition may have contributed to results. In our study, the SSC group had a higher return rate than the control group at all three follow-up visits. In addition, dyads who did not return were more likely to be mothers who were single or non-white. Attrition raises the possibility that the returning dyads had more positive interaction than dyads who did not return. Although some demographic differences were found between returning and non-returning dyads, whatever possible influences these differences, and the directions thereof, might have had on the measurement of mother-infant interaction is unclear.
Second, heterogeneity of the study infants is another possible reason. During the in-hospital phase of this study, subject recruitment was much slower because, by the time the study was funded, the primary study hospital was competing with secondary level hospitals that had established small NICUs to increase market share. Most of the pregnant women admitted into the primary study hospital were at higher risk than expected, as were their preterm infants after birth. As a result, many preterm infants did not meet the inclusion criteria and expansion of inclusion criteria to permit recruitment of higher-risk dyads was needed. Thus, about 70% of the preterm infants in the study were admitted into the NICU and several of these infants also required ventilator support. Dyads admitted to the NICU and/or needing ventilator support could not begin SSC as early or for as long due to infant care needs. The heterogeneity of this sample may have increased individual differences in terms of the dependent variable, thereby inflating the error variance and decreasing the chance of detecting a significant intervention effect (Stewart & Archbold, 1992). In addition, possible intervention diffusion cannot be ignored. Although our study only studied one dyad at a time, some SSC infants stayed in the NICU after the study ended. Parents of the control infants could have observed other parents experiencing SSC and initiated SSC themselves. This information, however, was not obtained at the time of follow-up visits.
Finally, the instruments chosen for this study may not reflect the essence of mother-infant interaction after experiencing SSC. Gross et al. (1993) reported that the NCAST Teaching Scale measures the cognitive experience, rather than affective feeling, of the mother. In addition, each item on the feeding and teaching scales was rated as a dichotomous response (presence or absence). As soon as ae behavior occurred the item was scored “yes” regardless of how often the behavior occurred thereafter. Then all items scored yes were added to obtain a sum score. Thus, the quantity of each behavior (e.g. kissing, caressing, and touching) was not measured. For these reasons, these two scales might not be sensitive enough to capture any between-group difference in changes resulting from the intervention.
Recommendations for Future Studies
Based on the experience of conducting this study, we recommend that researchers of future studies consider the following factors when assessing mother-infant interaction in dyads who experience SSC. Internal validity can be strengthened by consistent and more homogenous inclusion criteria, a higher return rate, and documentation of SSC experience throughout follow-ups. The feasibility of achieving these suggestions will also require careful evaluation.
Methodological triangulation with multiple measurement tools should be considered to better understand the effect of SSC on mother-infant interaction. One such tool is the Parent Child Early Relational Assessment (PC-ERA) in which observations of interactions are made during a play session. Based on our experience of conducting follow-ups, we learned that by the time the mother-infant dyads arrived, some infants and their mothers had already become tired from preparing for and making the trip. Thus, a play session that would be more comfortable for the dyads might help elicit a more familiar interaction pattern between infants and mothers. In addition, a subjective (qualitative) measure needs to be collected regarding mothers’ perceptions of connectedness to their infants.
Confounding variables should also be identified and measured concurrently or in advance. For example, shorter maternal leaves are associated with an increase in infants’ internalized behaviors (Berger et al., 2005) and more negative affect/behaviors in maternal-infant interactions (Clark et al., 1997). Other examples are parenting stress (Holditch-Davis & Miles, 2000; Jarvis & Creasey, 1991) and lack of a support system (Kotch et al., 1997).
Although definitive conclusions regarding the long-term effects of SSC on mother-infant interaction cannot be made at this time, it is important to note that no adverse effects were found. Based on positive findings from current literature about mother-infant interaction during and after SSC, all new mothers, if they are able and whether or not they ask to do SSC, should be encouraged to experience SSC and assured that they will have additional support from hospital staff. The longer term effects of SSC on mother-infant interaction, however, merit further testing
What is already known about this topic?
Mother-infant interaction is positively associated with child development.
Skin-to-skin contact elicits positive subjective responses from mothers of preterm infants.
Skin-to-skin contact promotes beneficial physiological conditions in preterm infants such as increased quiet sleep state, and more stable thermoregulation, heart rate, respiratory rate, and oxygen saturation.
Skin-to-skin contact also promotes longer breastfeeding duration and exclusivity.
What this paper adds:
This is the first study to assess mother-preterm infant interaction throughout 18 months in a randomized controlled trial of very early skin-to-skin contact. In addition the infant participants were predominantly (68%) late-preterm infants.
Mother-preterm infant dyads in both groups had similar interactions during feeding and teaching sessions, except that skin-skin contact infants were less likely to respond to their mothers’ teaching cues at 6 months.
Acknowledgements
We thank the Project Coordinators Francesca Pagliotti, Joan Swinth, Mary Alice Dombrowski, Meghan Moran Collins, & Cathy Santori; the study participants; and the nursing, hospital, and clinic staffs of both sites; and Diane Pacella from the General Clinical Research Center at University Hospitals for their contributions to this follow-up research.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Sheau-Huey Chiu, College of Nursing, University of Florida, Gainesville, FL, USA.
Gene Cranston Anderson, Case Western Reserve University; and Professor Emerita, University of Florida and Courtesy Faculty, College of Nursing, University of Florida, Gainesville, FL, USA.
References
- Affonso DD, Bosque E, Wahlberg V, Brady JP. Reconciliation and healing for mothers through skin-to-skin contact provided in an American tertiary level intensive care nursery. Neonatal Network. 1993;12(3):25–32. [PubMed] [Google Scholar]
- Affonso DD, Hurst L, Mayberry LJ, Haller L, Yost K, Lynch MI. Stressors reported by mothers of hospitalized premature infants. Neonatal Network. 1992;11(6):63–70. [PubMed] [Google Scholar]
- Affonso DD, Wahlberg V, Persson B. Exploration of mothers’ reactions to the kangaroo method of prematurity care. Neonatal Network. 1989;7(6):43–51. [PubMed] [Google Scholar]
- Anderson GC. Unpublished masters thesis. Madison: University of Wisconsin; 1972. Self-regulatory mother-infant interaction deprivation: A theoretical framework. [Google Scholar]
- Anderson GC. The mother and her newborn: Mutual caregivers. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 1977;6(5):50–57. doi: 10.1111/j.1552-6909.1977.tb02181.x. [DOI] [PubMed] [Google Scholar]
- Anderson GC. Risk in mother-infant separation postbirth. Image, Journal of Nursing Scholarship. 1989;21(4):196–199. doi: 10.1111/j.1547-5069.1989.tb00142.x. [DOI] [PubMed] [Google Scholar]
- Anderson GC, Chiu SH, Dombrowski MAS, Swinth JY, Albert J, Wada N. Mother-infant contact in a randomized trial of kangaroo (skin-to-skin) care. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2003;32:604–611. doi: 10.1177/0884217503256616. [DOI] [PubMed] [Google Scholar]
- Bayley N. Bayley scale of infant development. 2nd ed. Lutz, FL: Psychological Assessment Resources; 1993. [Google Scholar]
- Beckwith L, Cohen SE. Social interaction with the parent during infancy and later intellectual competence in children born preterm. In: Honig AS, editor. Early Parenting and Later Child Achievement. New York: Gordon and Breach; 1990. pp. 25–40. [Google Scholar]
- Berger LM, Hill J, Waldfogel J. Maternity leave, early maternal employment and child health and development in the US. The Economic Journal. 2005;115(501):F29–F47. [Google Scholar]
- Bergman NJ, Jurisoo LA. The 'kangaroo-method' for treating low birth weight babies in a developing country. Tropical Doctor. 1994;24:57–60. doi: 10.1177/004947559402400205. [DOI] [PubMed] [Google Scholar]
- Bergman NJ, Linley LL, Fawcus SR. Randomized controlled trial of skin-to-skin contact from birth versus conventional incubator for physiological stabilization in 1200- to 2199-gram newborns. Acta Paediatrica. 2004;93:779–785. doi: 10.1111/j.1651-2227.2004.tb03018.x. [DOI] [PubMed] [Google Scholar]
- Cattaneo A, Davanzo R, Worku B, Surjono A, Echeverria M, Bedri A, Haksari E, Haksari E, Osorno L, Gudetta B, Setyowireni D, Quintero S, Tamburlini G. Kangaroo mother care for low birthweight infants: A randomized controlled trial in different settings. Acta Paediatrica. 1998;87:976–985. doi: 10.1080/080352598750031653. [DOI] [PubMed] [Google Scholar]
- Charpak N, Ruiz-Pelaez JG, Figueroa Z, Charpak Y. Kangaroo mother versus traditional care for newborn infants ≤ 2000 grams: A randomized, controlled trial. Pediatrics. 1997;100:682–688. doi: 10.1542/peds.100.4.682. [DOI] [PubMed] [Google Scholar]
- Charpak N, Ruiz JG, Zupan J, Cattaneo A, Figueroa Z, Tessier R, Cristo M, Anderson G, Ludington S, Mendoza S, Mokhachane M, Worku B. Kangaroo Mother Care: 25 years after. Acta Paediatrica. 2005;94:514–522. doi: 10.1111/j.1651-2227.2005.tb01930.x. [DOI] [PubMed] [Google Scholar]
- Clark R, Hyde JS, Essex MJ, Klein MH. Length of maternity leave and quality of mother-infant interactions. Child Development. 1997;68(2):364–383. doi: 10.1111/j.1467-8624.1997.tb01945.x. [DOI] [PubMed] [Google Scholar]
- Conlon M, Anderson GC. Three methods of random assignment: Comparison of balance achieved on potentially confounding variables. Nursing Research. 1990;39:386–379. [PubMed] [Google Scholar]
- Dombrowski MAS, Anderson GC, Santori C, Roller CG, Pagliotti F, Dowling D. Kangaroo (skin-to-skin) care for premature twins and their adolescent parents. MCN, American Journal of Maternal-Child Nursing. 2000;25(2):92–94. doi: 10.1097/00005721-200003000-00009. [DOI] [PubMed] [Google Scholar]
- Feldman R, Eidelman AI, Sirota L, Weller A. Comparison of skin-to-skin (kangaroo) and traditional care: Parenting outcomes and preterm infant development. Pediatrics. 2002;110:16–26. doi: 10.1542/peds.110.1.16. [DOI] [PubMed] [Google Scholar]
- Feldman R, Eidelman AI. Skin-to-skin contact (kangaroo care) accelerates autonomic and neurobehavioural maturation in preterm infants. Developmental Medicine of Child Neurology. 2003;45(4):274–281. doi: 10.1017/s0012162203000525. [DOI] [PubMed] [Google Scholar]
- Feldman R, Weller A, Sirota L, Eidelman AI. Skin-to-skin contact (kangaroo care) promotes self-regulation in premature infants: Sleep-wake cyclicity, arousal modulation, and sustained exploration. Developmental Psychology. 2002;38:194–207. doi: 10.1037//0012-1649.38.2.194. [DOI] [PubMed] [Google Scholar]
- Feldman R, Weller A, Sirota L, Eidelman AI. Testing a family intervention hypothesis: The contribution of mother-infant skin-to-skin contact (kangaroo care) to family interaction, proximity, and touch. Journal of Family Psychology. 2003;17:94–107. [PubMed] [Google Scholar]
- Gale G, Franck L, Lund C. Skin-to-skin (kangaroo) holding of the intubated premature infant. Neonatal Network. 1993;12(6):49–57. [PubMed] [Google Scholar]
- Gerner EM. Emotional interaction in a group of preterm infants at 3 and 6 months of corrected age. Infant and Child Development. 1999;8:117–128. [Google Scholar]
- Gross D, Conrad B, Fogg L, Millis L, Garvey C. What does the NCATS measure? Nursing Research. 1993;42:260–265. [PubMed] [Google Scholar]
- Hake-Brooks SJ, Anderson GC. Kangaroo care and breastfeeding of mother-preterm infant dyads 0–18 months: A randomized, controlled trial. Neonatal Network. 2008;27:151–159. doi: 10.1891/0730-0832.27.3.151. [DOI] [PubMed] [Google Scholar]
- Holditch-Davis D, Miles MS. Mothers' stories about their experiences in the neonatal intensive care unit. Neonatal Network. 2000;19(3):13–21. doi: 10.1891/0730-0832.19.3.13. [DOI] [PubMed] [Google Scholar]
- Jarvis P, Creasey G. Parental stress, coping, and attachment in families with an 18-month-old infant. Infant Behavior and Development. 1991;14:383–395. [Google Scholar]
- Johnson AN. The maternal experience of kangaroo holding. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2007;36:568–573. doi: 10.1111/j.1552-6909.2007.00187.x. [DOI] [PubMed] [Google Scholar]
- Kennell JH, Jerauld R, Wolfe H, Chesler D, Kreger NC, McAlpine W. Maternal behavior one year after early and extended post-partum contact. Developmental Medicine and Child Neurology. 1974;16:172–179. doi: 10.1111/j.1469-8749.1974.tb02738.x. [DOI] [PubMed] [Google Scholar]
- Klaus M, Jerauld R, Kreger N, McAlpine W, Steffa M, Kennell J. Maternal attachment: Importance of the first postpartum days. New England Journal of Medicine. 1972;286:460–463. doi: 10.1056/NEJM197203022860904. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Morisset CE, Barnard KE, Hammond MA, Booth CL. The influence of early mother-child interaction on preschool cognitive/linguistic outcomes in a high-social risk group. Infant Mental Health Journal. 1996;17:310–321. [Google Scholar]
- Kotch JB, Browne DC, Ringwalt CL, Dufort V, Ruina E, Stewart PW, Jung JW. Stress, social support, and substantiated maltreatment in the second and third years of life. Child Abuse & Neglect. 1997;21:1025–1037. doi: 10.1016/s0145-2134(97)00063-x. [DOI] [PubMed] [Google Scholar]
- Labbok M, Krasovec K. Toward consistency in breastfeeding definitions. Studies in Family Planning. 1990;21:226–230. [PubMed] [Google Scholar]
- Lewis M, Ramsay DS. Stability and change in cortisol and behavioral responses to stress during the first 18 months of life. Developmental Psychobiology. 1995;28:419–429. doi: 10.1002/dev.420280804. [DOI] [PubMed] [Google Scholar]
- Ludington-Hoe S, Anderson G, Swinth J, Thompson C, Hadeed A. Randomized controlled trial of kangaroo care: Cardiorespiratory and thermal effects on healthy preterm infants. Neonatal Network. 2004;23(3):39–48. doi: 10.1891/0730-0832.23.3.39. [DOI] [PubMed] [Google Scholar]
- Ludington-Hoe S, Johnson M, Morgan K, Lewis T, Gutman J, Wilson P, et al. Neurophysiologic assessment of neonatal sleep organization: Preliminary results of a randomized, controlled trial of skin contact with preterm infants. Pediatrics. 2006;117(5):e909–e923. doi: 10.1542/peds.2004-1422. [DOI] [PubMed] [Google Scholar]
- Medoff-Cooper B. Temperament in very low birth weight infants. Nursing Research. 1986;35(3):139–143. [PubMed] [Google Scholar]
- Miles MS, Funk SG, Kasper MN. The stress responses of mothers and fathers of preterm infants. Research in Nursing and Health. 1992;15(4):261–269. doi: 10.1002/nur.4770150405. [DOI] [PubMed] [Google Scholar]
- Moore ER, Anderson GC, Bergman N. The Cochrane Library, Issue 3. Chichester, UK: John Wiley & Sons; 2007. Early skin-to-skin contact for mothers and their healthy newborn infants. (Cochrane review) [DOI] [PubMed] [Google Scholar]
- Moran M, Radzyminiski SG, Higgins K, Dowling DA, Miller MJ, Anderson GC. Maternal kangaroo (skin-to-skin) care in the NICU beginning 4 hours postbirth. MCN, The American Journal of Maternal-Child Nursing. 1999;24(2):74–79. doi: 10.1097/00005721-199903000-00006. [DOI] [PubMed] [Google Scholar]
- Neu M. Parents’ perception of skin-to-skin care with their preterm infants requiring assisted ventilation. Journal of Obstetric, Gynecologic, Neonatal Nursing. 1999;28:157–164. doi: 10.1111/j.1552-6909.1999.tb01980.x. [DOI] [PubMed] [Google Scholar]
- Ohgi S, Fukuda M, Moriuchi H, Kusumoto T, Akiyama T, Nugent JK, et al. Comparison of kangaroo care and standard care: Behavioral organization, development, and temperament in healthy, low-birth-weight infants through 1 year. Journal of Perinatology. 2002;22:374–379. doi: 10.1038/sj.jp.7210749. [DOI] [PubMed] [Google Scholar]
- Ourth L, Brown KB. Inadequate mothering and disturbance in the neonatal period. Child Development. 1961;32:287–295. doi: 10.1111/j.1467-8624.1961.tb05026.x. [DOI] [PubMed] [Google Scholar]
- Pocock SJ, Simon R. Sequential treatment assignment with balancing for prognostic factors in the controlled clinical trial. Biometrics. 1975;31:103–115. [PubMed] [Google Scholar]
- Rey ES, Martinez HG. Manejo rational de nino premature. Proceeding of the Conferences I Curso de Medicina Fetal y Neonatal; Bogota, Colombia. 1983. pp. 137–151. [Google Scholar]
- Rojas MA, Kaplan M, Quevedo M, Sherwonit E, Foster LB, Ehrenkranz RA, et al. Somatic growth of preterm infants during skin-to-skin care versus traditional holding: A randomized, controlled trial. Journal of Developmental and Behavioral Pediatrics. 2003;24(3):163–168. doi: 10.1097/00004703-200306000-00006. [DOI] [PubMed] [Google Scholar]
- Roller CG. Getting to know you: Mothers’ experiences of kangaroo care. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2005;34:210–217. doi: 10.1177/0884217504273675. [DOI] [PubMed] [Google Scholar]
- Roller GC, Meyer K, Anderson GC. Birth kangaroo (skin-to-skin) care and breastfeeding: An eclamptic women’s story. MCN: American Journal of Maternal-Child Nursing. 1999;24(6):294–295. doi: 10.1097/00005721-199911000-00006. [DOI] [PubMed] [Google Scholar]
- Sloan NL, Camacho LWL, Rojas EP, Stern C Maternidad Isifdro Ayora Study. Kangaroo mother method: Randomized controlled trial of an alternative method of care for stabilised low-birthweight infants. Lancet. 1994;344:782–785. doi: 10.1016/s0140-6736(94)92341-8. [DOI] [PubMed] [Google Scholar]
- Stewart BJ, Archbold PG. Nursing intervention studies require outcome measures that are sensitive to change: Part one. Research in Nursing & Health. 1992;15:477–491. doi: 10.1002/nur.4770150610. [DOI] [PubMed] [Google Scholar]
- Suman RP, Udani R, Nanavati R. Kangaroo mother care for low birth weight infants: A randomized controlled trial. Indian Pediatrics. 2008;45(1):17–23. [PubMed] [Google Scholar]
- Sumner G, Spietz A. NCAST caregiver/parent-child interaction feeding manual. Seattle: NCAST Publications, University of Washington, School of Nursing; 1994a. [Google Scholar]
- Sumner G, Spietz A. NCAST caregiver/parent-child interaction teaching manual. Seattle: NCAST Publications, University of Washington, School of Nursing; 1994b. [Google Scholar]
- Syfrett B. Unpublished masters theses. Gainesville, FL: University of Florida; 1993. Very early and virtually continuous kangaroo care for 34–36 week gestation preterm infants: Effects on temperature, breastfeeding, supplementation, and weight. (AAT 1359163) [Google Scholar]
- Swinth JY, Nelson LE, Hadeed A, Anderson GC. Shared kangaroo care for triplets. MCN, The American Journal of Maternal-Child Nursing. 2000;25(4):214–216. doi: 10.1097/00005721-200007000-00010. [DOI] [PubMed] [Google Scholar]
- Tallandini MA, Scalembra C. Kangaroo mother care and mother-premature infant dyadic interaction. Infant Mental Health Journal. 2006;27(3):251–275. doi: 10.1002/imhj.20091. [DOI] [PubMed] [Google Scholar]
- Tessier R, Cristo M, Velez S, Giron M, de Calume ZF, Ruiz-Palaz, Charpak Y, Charpak N. Kangaroo mother care and the bonding hypothesis. Pediatrics. 1998;102(2):e17–e24. doi: 10.1542/peds.102.2.e17. [DOI] [PubMed] [Google Scholar]
- Uvnäs-Moberg K. Oxytocin may mediate the benefits of positive social interaction and emotions. Psychoneuroendocrinology. 1998;23(8):819–835. doi: 10.1016/s0306-4530(98)00056-0. [DOI] [PubMed] [Google Scholar]
- Winberg J. Mother and newborn baby: Mutual regulation of physiology and behavior – a selective review. Developmental Psychobiology. 2005;47(3):217–229. doi: 10.1002/dev.20094. [DOI] [PubMed] [Google Scholar]
- Widström AM, Ransjö-Arvidson AB, Christensson K, Matthiesen AS, Winberg J, Uvnäs-Moberg K. Gastric suction in healthy newborn infants. Effects on circulation and developing feeding behavior. Acta Paediatrica Scandinavica. 1987;76:566–572. doi: 10.1111/j.1651-2227.1987.tb10522.x. [DOI] [PubMed] [Google Scholar]
- Zeller R, Good M, Anderson GC, Zeller D. Strengthening experimental design by balancing potentially confounding variables across treatment groups. Nursing Research. 1997;46:345–349. doi: 10.1097/00006199-199711000-00009. [DOI] [PubMed] [Google Scholar]


