Abstract
Background
Physical activity (PA) is an important component of weight loss programs and may be encouraged for severely obese patients undergoing bariatric surgery. However, few studies have determined the amount and intensity of activities undertaken preoperatively by bariatric surgery patients using objective measures.
Methods
Using RT3 tri-axial accelerometers, this study compared 38 bariatric surgery candidates and 20 normal-weight controls on: 1) activity counts/hour; 2) minutes/day spent in moderate-to-vigorous intensity PA (MVPA) and vigorous intensity PA (VPA); and 3) level of compliance with national recommendations to accumulate 150 minutes/week of MVPA in bouts ≥ 10 minutes.
Results
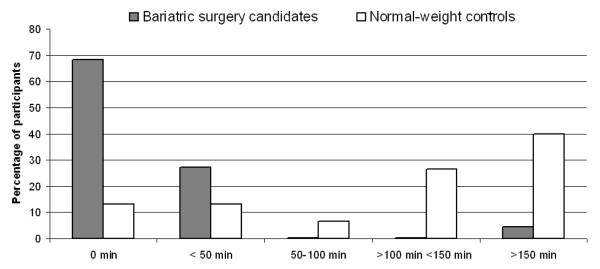
Surgery candidates, compared to controls, recorded significantly (Ps < 0.01) fewer activity counts/hour (13799 ± 3758 vs 19462 ± 4259) and spent fewer minutes/day engaged in MVPA (26.4 ± 23.0 vs 52.4 ± 24.7) and VPA (1.2 ± 3.4 vs 11.8 ± 9.0). More than two-thirds (68%) of surgery candidates versus 13% of NW did not accumulate any MVPA in bouts ≥ 10 minutes and only 4.5% of Ob met the weekly MVPA recommendation compared to 40% of NW.
Conclusion
Bariatric surgery candidates have low PA levels and rarely engage in PA bouts of sufficient duration and intensity to maintain and improve health. Additional research is needed to determine how best to increase PA in bariatric surgery candidates.
Keywords: physical activity, accelerometers, bariatric surgery, severe obesity, controls
Introduction
Recent trends in obesity prevalence among U.S. adults reveal a sub-epidemic, indicated by disproportionate growth in the most extreme weight categories [1]. The rapid rise of severe obesity and its resistance to conventional weight loss approaches has led to burgeoning demand for bariatric surgery. Across all procedures, bariatric surgery patients lose approximately 39 kg or 56% of their excess body weight [2]. However, not all patients achieve weight loss success [3]. Efforts to identify non-surgical factors underlying suboptimal weight loss have largely focused on patient behaviors given their amenability to change.
Bariatric surgery patients’ physical activity (PA) behaviors might contribute to variability in weight loss success. Recent prospective findings suggest that failure of patients with low PA preoperatively to substantially increase their PA postoperatively can undermine weight loss outcomes [4]. Given that the preoperative period may serve as a “teachable moment” to initiate or increase engagement in PA, accurate determination of PA at this juncture is critical to informing development of appropriate interventions.
However, most studies have assessed PA in bariatric surgery patients using self-report questionnaires. While these measures are inexpensive, easy to administer, and impose relatively little burden on participants, obese individuals often over-report their PA [5, 6]. Indeed, the accuracy of such measures is dependent on participants’ perceptions of PA intensity and their ability to remember information about the types and patterns of PA that they perform [7]. To overcome these limitations, accelerometers (motion sensors) which provide minute-by-minute data on activity patterns under free-living conditions, have increasingly been used to objectively quantify PA [8]. Recently, accelerometers have been used to assess: validity of a subjective PA measure [9], compliance with PA recommendations in weight loss maintainer and always normal-weight groups [10], PA energy expenditure during behavioral weight loss intervention [11], and the effectiveness of behavioral interventions to increase PA [12].
Yet, only one study has used accelerometers to assess PA in bariatric surgery patients [13]. Bariatric surgery candidates in the Longitudinal Assessment of Bariatric Surgery (LABS) study wore a biaxial, ankle-mounted accelerometer that recorded steps per minute. Findings demonstrated a wide range of activity levels among the sample, although most (80%) participants were either inactive or insufficiently active (i.e. < 10,000 steps/day).
The purpose of the current study was to use accelerometers to obtain additional information concerning bariatric surgery candidates’ engagement in different intensities of PA, relative to normal-weight controls. Delineating the areas of PA in which bariatric surgery candidates and normal-weight controls differ may be helpful in developing suitable recommendations for increasing PA during the preoperative period. Therefore, we compared these groups on total volume of PA (accelerometer activity counts/hour) and time (min/day) spent in moderate-to-vigorous intensity PA (MVPA) and vigorous-intensity PA (VPA). In addition, we assessed whether they differed on level of adherence to national PA recommendations to accumulate 150 min/wk of MVPA in bouts ≥ 10 min [14].
Methods
Participants and procedures
Severely obese (BMI > 35 kg/m2) candidates for bariatric surgery and normal-weight controls (BMI < 25 kg/m2) who were similar in sex and age characteristics were studied. Bariatric surgery candidates were recruited from one of three clinics in Providence, Rhode Island. During a preoperative consultation visit, candidates were given a flyer describing the study. Interested patients were asked to sign the flyer, thereby granting permission to be contacted by telephone to learn more about the study and be screened for eligibility. Of 469 patients who granted permission to be contacted, 408 patients either chose not to participate, did not yet have a scheduled surgery date, or were found ineligible. Of 63 bariatric surgery candidates deemed eligible, 53 attended the research laboratory to complete study procedures.
Normal-weight controls were recruited from a network of Rhode Island hospitals via an internal online advertisement that provided a number to call to receive more information about the study and be screened for eligibility. Of 75 individuals who contacted research staff, 52 either refused to participate or were ineligible. Of the 23 individuals found eligible, 21 attended the research laboratory to complete study procedures.
Eligible surgery and control participants, who were aged 18-65 years, non-smokers, and ambulatory, visited the research laboratory where they provided informed consent and had their height and weight measured using a stadiometer and electronic scale according to standard procedures. Normal-weight participants’ BMI was confirmed to be below 25.0 kg/m2 at this time. Demographic information was provided via questionnaire. Participants received an accelerometer to wear for the next 7 consecutive days, a daily log to report when the device was clipped on and removed, and a postage-paid envelope to return the device. Participants were compensated $15 for their participation. The study protocol was approved by the Miriam Hospital Institutional Review Board, Providence RI, USA.
Physical activity (PA) measurement
PA was assessed using the RT3 triaxial accelerometer (Stayhealthy, Inc, Monrovia, CA). The RT3 is a battery operated device about the size of a pager which uses an integrated computer chip to measure activity in three individual planes: vertical, horizontal, and anterior-posterior. The RT3 detects accelerations for each of the 3 planes across 1-min intervals and converts these data into activity counts. Greater acceleration over a given period yields greater activity counts. The RT3 possesses adequate reliability [15] and provides a valid assessment of treadmill walking and non-structured PA against the criterion of oxygen consumption [16].
In the current study, each RT3 accelerometer was programmed with the participant’s personal data (sex, age, height, and weight). The device was clipped to the participant’s waistline on the right side and activated to start recording PA data. Participants were instructed to wear the device during all waking hours (except for bathing) for 7 consecutive days while maintaining their regular level of PA. Upon mail receipt, data from the device was downloaded and stored on a desktop computer using proprietary software.
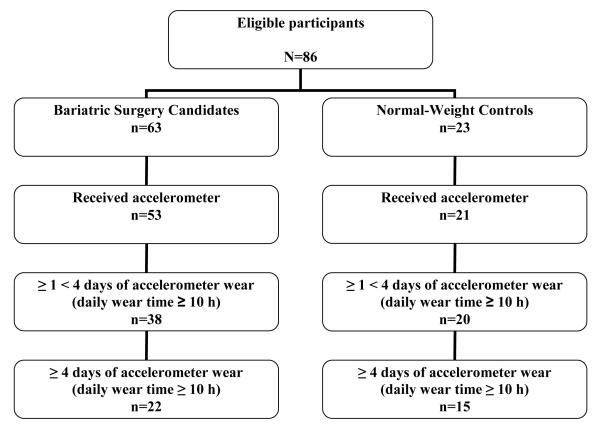
RT3 vector magnitude activity counts, calculated as the square root of the sum of squared accelerations of the three planes, were used to represent PA. For accelerometer data to be valid for this study, a minimum of 4 days in which the device was worn ≥ 10 hours/day was required. The device was considered not to be worn if there were > 30 min in which the RT3 did not record any activity counts. These RT3 wear time requirements have been shown to result in reasonable estimation of MVPA and MVPA occurring in bouts ≥ 10 min among obese adults [17]. In the event that participants did not meet these requirements, battery power of the device expired before receipt, or the device malfunctioned, participants were asked to wear the device again. As shown in Figure 1, of the 86 eligible participants, 74 visited the laboratory and were given an accelerometer. Of these initial 74, 16 RT3 recordings were excluded (n = 8 with 0 days of wear that met the criteria of ≥ 10 hours/day of wear time and 8 with battery power or device failure). Of the remaining 58 participants, 21 (16 bariatric surgery candidates and 5 normal-weight controls) had at least 1 but fewer than 4 days with ≥ 10 hours of RT3 wear and thus were excluded from primary analyses. This left a sample of 37 participants (22 bariatric surgery candidates and 15 normal-weight controls) who met the ≥ 10 hours/day wear requirement on ≥ 4 days.
Figure 1.
Flowchart of number of accelerometers received and participants who met different accelerometer wear time criteria
Data were analyzed to determine: 1) activity counts/hour, representing total volume of PA; and 2) min/day spent in ≥ 1 min bouts of MVPA and VPA. RT3 activity count cut points of ≥ 984 activity counts/min and ≥ 2341 activity counts/min were used to identify min/day spent in MVPA and VPA, respectively. In a previous study [16], these activity count thresholds were shown to correspond to moderate (3 METs) and vigorous (6 METs) intensity activity. Time spent in PA at each of level of intensity was determined by totaling the minutes in each day during which activity counts met the corresponding minimum activity counts threshold. Weekly minutes spent performing MVPA in bouts ≥ 10 min were summed to determine level of compliance with national PA recommendations to accumulate 150 min/wk of MVPA in bouts ≥ 10 min [14].
Statistical analyses
Statistical analyses were conducted using the Statistical Package for Social Sciences, version 14.0 (SPSS for Windows, SPSS, Chicago, IL). Descriptive statistics were generated for all variables. Examination of differences between groups on demographic and anthropometric variables was performed using χ2 analyses for categorical variables and independent t-tests for continuous variables. Analyses of covariance (ANCOVA) were used to compare the groups on accelerometer counts/hour and min/day spent in MVPA and VPA, adjusting for marginal group differences in race and level of education. Zero values were inserted for participants who had no PA that met the defined intensity criteria. Chi-square tests were used to compare the groups on level of compliance with the national PA recommendation to accumulate 150 min/wk of MVPA in bouts ≥ 10 min [14]. Similar to the procedures above, zero values were inserted for participants who did not accumulate any MVPA in bouts ≥ 10 min. All tests were two-tailed and statistical significance was set at p < 0.05.
Results
Participants
Baseline characteristics of the 22 bariatric surgery candidates and 15 normal-weight controls who met valid RT3 wear requirements are presented in Table 1. The groups were similar on age (47.6 ± 9.1 years), gender (84% female), and marital status (59% married). There were non-significant (p’s < 0.09) trends for bariatric surgery candidates to differ from normal controls on race (68% vs. 100% Caucasian) and educational level (48% vs. 79% with ≥ 4 years of college). Per design, bariatric surgery candidates had greater weight (131.6 ± 27.9 vs. 61.5 ± 8.9 kg) and BMI (49.3 ± 8.4 vs. 22.8 ± 1.3 kg/m2) values. Analyses conducted across and within the surgery and control groups showed no significant (p > 0.30) differences in demographics between participants who did and did not meet valid RT3 wear requirements, with the exception that within the surgery group, those who met requirements were more likely to be married (73% vs. 44%; p < 0.047).
Table 1.
Characteristics of bariatric surgery candidates and normal-weight controls (mean ± SD)
| Bariatric surgery candidates |
Normal-weight controls |
P value | |
|---|---|---|---|
| Age (years) | 48.4 ± 9.4 | 46.4 ± 9.0 | 0.542 |
| Sex (%) | |||
| Female | 81.8 | 86.7 | |
| Male | 18.2 | 13.3 | 0.476 |
| Race (%) | |||
| Caucasian | 68.2 | 100 | |
| African American | 13.6 | 0 | |
| Hispanic | 18.2 | 0 | 0.053 |
| Marital Status | |||
| Married | 57.8 | 60.0 | |
| Not married | 42.2 | 40.0 | 0.417 |
| Education level (%) | |||
| High school or vocational training | 23.8 | 0 | |
| < 4 years of college | 28.6 | 21.4 | |
| ≥ 4 years of college | 47.6 | 78.6 | 0.089 |
| Weight (kg) | 131.6 ± 27.9 | 61.5 ± 8.9 | 0.0001 |
| BMI (kg/m2) | 49.3 ± 8.4 | 22.8 ± 1.3 | 0.0001 |
Physical activity (PA)
Bariatric surgery candidates compared to normal-weight controls recorded significantly fewer activity counts/hour (13798 ± 3758 vs. 19462.0 ± 4258, p = 0.001), indicating less engagement in overall PA. Moreover, as shown in Figure 2, although bariatric surgery candidates exhibited a wide range of activity levels, nearly 60% (59.2) recorded fewer than 15,000 counts/hour, or approximately 8,000 steps/day [18], compared to 6.7% of controls. Secondary analyses comparing bariatric surgery candidates (n = 38) and controls (n = 20) who met the criterion of 10 hours/day of wear time on ≥ 1 days produced similar findings (data not shown).
Figure 2.
Accelerometer activity counts per hour in bariatric surgery candidates and normal-weight controls.
With respect to time (minutes/day) spent in ≥ 1 min periods of MVPA and VPA, bariatric surgery candidates on average spent less than a half hour per day in MVPA compared to almost an hour for normal weight controls (26.4 ± 23.0 vs. 52.4 ± 24.7 min/day, p = 0.009). Similarly, bariatric surgery participants spent markedly less time in VPA than controls (1.2 ± 3.4 vs. 11.8 ± 9.0 min/day, p <.0001). Again, secondary analyses comparing bariatric surgery candidates (n = 38) and controls (n = 20) who had ≥ 1 days of valid accelerometer wear did not change the pattern of findings (data not shown)
Figure 3 shows large group differences in weekly accumulation of MVPA in bouts of at least 10 minutes. More than two-thirds (68.2) of bariatric surgery candidates did not have any MVPA bouts ≥ 10 min, compared to 13.3% of normal-weight controls. In addition, only 1 of 22 (4.5%) bariatric surgery candidates met the national recommendation to accumulate 150 min/wk of MVPA in bouts ≥ 10 min, versus 6 of 15 (40%) controls (p = 0.011) [18]. Similar results were produced with secondary analyses of participants who wore the RT3 for 7 days and met the ≥ 10 hours/day wear requirement on at least 1 of these days (0% of 26 bariatric surgery candidates vs. 50% of 16 controls, p < 0.0001).
Figure 3.
Weekly accumulation of moderate-to-vigorous intensity physical activity in bouts of at least 10 minutes in bariatric surgery candidates and normal-weight controls
Discussion
This study used objective data obtained from accelerometers to compare bariatric surgery candidates and normal-weight controls on total PA and PA performed at different intensities in bouts of varying duration. Bariatric surgery candidates performed less PA overall and spent fewer minutes per day in MVPA and VPA compared to controls. More than two-thirds (68%) of bariatric surgery candidates had no MVPA in bouts ≥ 10 min compared to only 13% of controls. Furthermore, only 4.5% of bariatric surgery candidates met national PA guidelines to accumulate ≥ 150 min/wk of MVPA in bouts ≥ 10 min [14], compared to 40% of controls. Taken together, these findings suggest that when compared to normal-weight individuals, most bariatric surgery candidates move less throughout the day and are less likely to participate in PA of a sufficient intensity and duration to improve and maintain health and manage body weight [14, 19].
Our findings are similar to those from recent studies suggesting low levels of PA in bariatric surgery patients preoperatively. In a study of 190 RYGB patients, nearly two-thirds (64%) were inactive, defined as self-reported accumulation of < 200 min/wk of MVPA including walking in ≥ 10 min bouts [4]. King and colleagues [13] showed a variety of PA levels among 757 bariatric surgery candidates from the LABS study, although most (80%) were either inactive or insufficiently active based on objective step counts (i.e. <10,000 steps/day). Consistent with the findings of King et al., bariatric surgery candidates in the present study exhibited a wide range of PA levels, although most were inactive or insufficiently active based on accelerometer activity counts/hour and time (min/wk) accumulated in MVPA bouts ≥ 10 min. Indeed, 91% of the bariatric surgery candidates recorded fewer than 18,972 accelerometer activity counts/hour, a cut-off roughly equivalent to 10,000 steps/day [18], and 95% failed to meet the national recommendation to accumulate 150 weekly minutes of MVPA in ≥ 10 min bouts [14].
Similar to previous studies that have compared PA levels in obese and non-obese individuals using accelerometers [20-23], we found that severely obese individuals preparing to undergo bariatric surgery engage in less PA of at least a moderate intensity than their normal-weight counterparts. Bariatric surgery candidates spent 50% less time each day in MVPA, compared to controls (26 vs 52 min/day). In addition, more than two-thirds (68%) of bariatric surgery candidates did not accumulate any MVPA in bouts ≥ 10 min versus 13% of controls. These findings are consistent with those from a recent population-based study showing that higher BMI and larger waist circumference are associated with lower levels of accelerometer-determined MVPA occurring in bouts ≥ 10 min [23].
Finally, the finding that only 1 of the 22 bariatric surgery candidates in this study met the recommended 150 minutes of MVPA in bouts ≥ 10 min is striking. Moreover, the majority of bariatric surgery candidates were not even close to meeting these criteria—15 (68%) had no MVPA bouts ≥ 10 min and 21 (95%) accumulated less than 50 min/wk of MVPA in ≥ 10 min bouts. These findings support previous research showing lower objective adherence to recommended PA levels in non-severely obese versus normal-weight individuals [20, 21] and strongly suggest that meeting existing PA guidelines geared towards the general population may be too challenging from a physical and/or motivational standpoint for many bariatric surgery patients preoperatively. Consequently, interventions to increase PA in bariatric surgery candidates may be most effective when a variety of strategies are employed, such as: shaping PA behavior through goals that promote gradual increases in PA amount and intensity [24]; encouraging accumulation of daily PA in multiple short bouts versus a long single bout [25]; prescribing slower walking on a flat surface to minimize adverse biomechanical effects of severe obesity [26]; reducing sedentary behaviors to increase number of opportunities for lifestyle and structured PA [27]; and teaching other techniques such as self-reinforcement and stimulus control to increase low PA motivation and commitment [24].
This study is the first to: 1) use the RT3 accelerometer, a device used in large scale observational and treatment studies [10, 17], in a bariatric surgery patient population; 2) objectively determine time spent by bariatric surgery candidates performing PA at different levels of intensity and in MVPA bouts ≥ 10 minutes, relative to normal weight controls; and 3) compare these groups on objective adherence to national physical activity recommendations. These strengths and novel aspects advance previous PA research involving bariatric surgery patients, which has largely relied on self-report measures to assess PA and not directly compared PA in this group with that of normal-weight individuals.
A number of study limitations should also be considered. Although accelerometers are able to overcome certain limitations of questionnaires such as over-reporting, types of exercise and non-exercise related activities performed cannot be determined. Additional studies are needed to evaluate the extent to which the RT3 provides a valid assessment of different structured activities (e.g., walking, cycling, etc.) performed by bariatric surgery patients. Accuracy of the RT3 in detecting vertical movement may have been limited in bariatric surgery candidates as a result of monitor tilting due to excess adiposity and abnormal walking or gait abnormalities [8]. Further research is required to understand how these and other physical limitations affect performance and measurement of lifestyle and structured activities. The activity count thresholds that were used to define MVPA and VPA are based on a younger and leaner sample [16], which may affect the accuracy of these classifications in our sample. Bariatric surgery candidates in this study were ambulatory and controls were homogeneous to race which may limit generalizability of our findings to the respective populations. Overall, the sample was relatively small and self-selected. It is possible that participants, particularly controls, were more physically active than individuals who were unmotivated to participate. We did not collect specific information concerning occupation or socioeconomic status (SES) level, although analyses adjusting for education level (a common proxy of SES) did not change our pattern of findings. Nonetheless, additional studies are needed to examine whether occupation, length of work day and related sitting time contribute to differences in PA between bariatric surgery patients and normal-weight individuals on work and non-work days. Finally, less than two-thirds (64%; 48% of surgery candidates and 75% of controls) of participants who wore an accelerometer from which data could be retrieved met the wear requirement on ≥ 4 days, although analyses including all participants with at least 1 day of valid wear did not alter the pattern of findings. Future research is needed to determine an appropriate balance between accelerometer wear time and participant burden, particularly among bariatric surgery patients.
In summary, the present study is the first to use accelerometers to compare PA in bariatric surgery candidates and normal-weight controls. Compared to controls, bariatric surgery candidates moved less throughout the day and spent less time in PA of at least a moderate intensity. Moreover, less than 5% of bariatric surgery candidates met the national PA recommendation to accumulate 150 weekly minutes of MVPA in bouts lasting at least 10 minutes, compared to 40% of controls. Future research is needed to determine how best to increase PA in bariatric surgery candidates and the effects of accelerometer-determined PA patterns and intensity on postoperative weight and health-related outcomes.
Acknowledgements
Appreciation is expressed to Angelica Adams, B.S., and Jennifer Trautvetter, B.A., for their assistance with data collection and Michael McDermott, M.S. who prepared and organized the accelerometer data for analysis under the auspices of the University of Pittsburgh Obesity and Nutrition Research Center (ONRC) (P30DK046204). This research was funded by grants from the Warren Alpert Medical School of Brown University’s Center of Excellence in Women’s Health and the National Institute of Diabetes and Digestive and Kidney Diseases (grant K01 DK083438-01) awarded to Drs. Wing and Bond, respectively.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sturm R. Increases in morbid obesity in the USA: 2000-2005. Public Health. 2007;121:492–6. doi: 10.1016/j.puhe.2007.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Buchwald H, Estok R, Fahrbach K, et al. Weight and types 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122:248–65. doi: 10.1016/j.amjmed.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 3.Snyder B, Nguyen A, Scarbourough T, Yu S, Wilson E. Comparison of those who succeed in losing significant excessive weight after bariatric surgery and those who fail. Surg Endosc. 2009 doi: 10.1007/s00464-008-0322-1. doi: 10.1007/s00464-008-3221-1. [DOI] [PubMed] [Google Scholar]
- 4.Bond DS, Phelan S, Wolfe LG, et al. Becoming physically active after bariatric surgery is associated with improved weight loss and health-related quality of life. Obesity. 2009;17:78–83. doi: 10.1038/oby.2008.501. [DOI] [PubMed] [Google Scholar]
- 5.Lightman SW, Pirsarska K, Bermann ER, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. New Engl J Med. 1992;327:1893–8. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 6.Jakicic JM, Polley BA, Wing RR. Accuracy of self-reported exercise and the relationship with weight loss in overweight women. Med Sci Sports Exerc. 1998;30:634–8. doi: 10.1097/00005768-199804000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Shephard RJ. Limits to the measurement of habitual physical activity by questionnaires. Br J Sports Med. 2003;37:197–206. doi: 10.1136/bjsm.37.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Corder K, Brage S, Ekelund U. Accelerometers and pedometers: methodology and clinical application. Curr Opin Clin Nutr Metab Care. 2007;10:597–603. doi: 10.1097/MCO.0b013e328285d883. [DOI] [PubMed] [Google Scholar]
- 9.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–8. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 10.Phelan S, Roberts S, Lang W, Wing RR. Empirical evaluation of physical activity recommendations for weight control in women. Med Sci Sports Exerc. 2007;39:1832–6. doi: 10.1249/mss.ob013e31812383c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Polzien KM, Jakicic JM, Tate DF, Otto AD. The efficacy of a technology-based system in a short-term behavioral weight loss intervention. Obesity. 2007;15:825–30. doi: 10.1038/oby.2007.584. [DOI] [PubMed] [Google Scholar]
- 12.Opdenacker J, Boen F, Coorevits N, Delucluse C. Effectiveness of a lifestyle intervention and a structured exercise intervention in older adults. Prev Med. 2008;46:518–24. doi: 10.1016/j.ypmed.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 13.King WC, Belle SH, Eid GM, et al. Physical activity levels of patients undergoing bariatric surgery in the Longitudinal Assessment of Bariatric Surgery study. Surg Obes Relat Dis. 2008;4:721–8. doi: 10.1016/j.soard.2008.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendations for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–34. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 15.Powell SM, Jones DI, Rowlands AV. Technical variability of the RT3 accelerometer. Med Sci Sports Exerc. 2003;35:1773–8. doi: 10.1249/01.MSS.0000089341.68754.BA. [DOI] [PubMed] [Google Scholar]
- 16.Rowlands AV, Thomas PW, Eston RG, Topping R. Validation of the RT3 triaxial accelerometer for the assessment of physical activity. Med Sci Sports Exerc. 2004;36:518–24. doi: 10.1249/01.mss.0000117158.14542.e7. [DOI] [PubMed] [Google Scholar]
- 17.Jerome GJ, Young DR, Laferriere D, Chen C, Vollmer WM. Reliability of RT3 accelerometers among overweight and obese adults. Med Sci Sports Exerc. 2009;41:110–4. doi: 10.1249/MSS.0b013e3181846cd8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.MacFarlane DJ, Chan D, Chan KL, Ho EY, Lee CC. Using three objective criteria to examine pedometer guidelines for free-living individuals. Eur J Appl Physiol. 2008;104:435–44. doi: 10.1007/s00421-008-0789-4. [DOI] [PubMed] [Google Scholar]
- 19.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41:459–71. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 20.Cooper AR, Page A, Fox KR, Misson J. Physical activity patterns in normal, overweight and obese individuals using minute-by-minute accelerometry. Eur J Clin Nutr. 2000;54:887–94. doi: 10.1038/sj.ejcn.1601116. [DOI] [PubMed] [Google Scholar]
- 21.Davis JN, Hodges VA, Gillham MB. Physical activity compliance: differences between overweight/obese and normal-weight adults. Obesity. 2006;14:2259–2265. doi: 10.1038/oby.2006.265. [DOI] [PubMed] [Google Scholar]
- 22.Hemmingsson E, Ekelund U. Is the association between physical activity and body mass index obesity dependent? Int J Obes. 2007;31:663–8. doi: 10.1038/sj.ijo.0803458. [DOI] [PubMed] [Google Scholar]
- 23.Strath SJ, Holleman RG, Ronis DL, Swartz AM, Richardson CR. [Accessed [November 1, 2008]];Objective physical activity accumulation in bouts and nonbouts and relation to markers of obesity in US adults. Prev Chronic Dis. 2008 5(4) http://www.cdc.gov/pcd/issues/2008/oct/07_0158.htm. [PMC free article] [PubMed]
- 24.Jakicic JM. Exercise strategies for the obese patient. Prim Care. 2003;30:393–403. doi: 10.1016/s0095-4543(03)00010-1. [DOI] [PubMed] [Google Scholar]
- 25.Jakicic JM, Wing RR, Butler BA, Robertson BJ. Prescribing exercise in multiple short bouts versus one continuous bout: effects on adherence, cardiorespiratory fitness, and weight loss in overweight women. Int J Obes Relat Metab Disord. 1995;19:893–901. [PubMed] [Google Scholar]
- 26.Browning RC, Kram R. Effects of obesity on the biomechanics of walking at different speeds. Med Sci Sports Exerc. 2007;39:1632–1641. doi: 10.1249/mss.0b013e318076b54b. [DOI] [PubMed] [Google Scholar]
- 27.Epstein LH, Roemmich JN. Reducing sedentary behavior: role in modifying physical activity. Exerc Sport Sci Rev. 2001;29:103–108. doi: 10.1097/00003677-200107000-00003. [DOI] [PubMed] [Google Scholar]