Abstract
Background:
Asthma and COPD are characterized by substantial racial disparities in morbidity and mortality. We hypothesized that because African-American patients with these conditions experience greater mortality and morbidity than their white counterparts, they would use more health-care resources when no difference in health insurance exists.
Methods:
A retrospective, population-based cohort study was conducted using Maryland Medicaid Managed Care patient encounter data. We compared health services utilization and cost outcomes in both African-American and white patients with COPD, asthma, or coexisting COPD and asthma.
Results:
The study population consisted of 9,131 patients with COPD, asthma, or both conditions. Of the total population, 52% were African American (n = 4,723), and 44% were white (n = 4,021); all other races were combined into the “unknown race” category to account for the remaining 4% (n = 387). After controlling for age, gender, cohort allocation, and comorbidities, we found that African-American adults with COPD, asthma, or coexisting COPD and asthma actually used fewer medical services and accounted for lower medical costs than white adults.
Conclusions:
Lower health services utilization and medical costs among African-American patients with COPD and asthma may provide a possible explanation for the racial disparities in outcomes of patients with these conditions.
Racial disparities in health-care utilization and outcomes are known for a number of diseases; heretofore, COPD has been considered1,2 a disease that disproportionately affects white men. However, some data3,4 show that COPD fatality rates have risen faster in African Americans than in whites. The trends in the prevalence of COPD and its associated mortality and morbidity3,4 may reflect the patterns of smoking that existed some 30 to 50 years ago. Smoking among minorities, especially African Americans, has increased more rapidly than among whites, and the prevalence of COPD in the former has risen accordingly.3
Data collected by the Centers for Disease Control and Prevention, National Center for Health Statistics,5–9 show that racial and ethnic differences in asthma prevalence, health-care utilization, and mortality exist; however, few studies3 have addressed racial disparities in COPD care. Our previous work10 has shown that medical resource utilization varies between COPD and asthma patients. Even after adjusting for demographics and comorbidities, we found that patients with COPD had the highest health-care utilization, followed by patients with both COPD and asthma.
In the current study, we focused on possible differences in health-care utilization by race. Because of the reported greater prevalence of COPD and asthma morbidity and mortality among African Americans, we hypothesized that these patients would tend to use more health-care services than their white counterparts. We selected a population of Medicaid patients in order to minimize the differences in economic barriers of access to health-care facilities across the study population.
Materials and Methods
Design
This study used a retrospective patient encounters database, and the study period was 36 months, from January 1, 2001, to December 31, 2003. The study population was selected from the larger (> 400,000) pool of all Maryland Medicaid Managed Care beneficiaries. The race variable was drawn directly from encounter files in Medicaid data. African-American patients accounted for about half of the study population, with female beneficiaries constituting > 60%, and beneficiaries ≥ 17 years of age constituting approximately 50%.
Patients enrolled in the study were adults between 40 and 64 years of age as of January 1, 2001, and who had undergone follow-up for at least 360 days from their first medical claim. Patients with COPD were identified on the basis of claims with International Classification of Diseases, ninth revision,11,12 codes 491.xx, 492.xx, and 496.xx, and patients with asthma on the basis of code 493.xx in the primary, secondary, or tertiary diagnosis fields. Complete pharmacy information was required for all patients to ensure that they were undergoing treatment. Patients who were dually eligible for Medicare were excluded to avoid missing claims and variables, as we only were able to track patient activity through Medicaid. We defined the following three cohorts: asthma; COPD; and comorbid COPD and asthma. Patients with only asthma or only COPD in the first 30 months (ie, from January 1, 2001, to June 30, 2003) were assigned to the corresponding asthma or COPD cohort. Claims information on either diagnosis was continuously collected until the first claim for the other diagnosis was reported. Patients who had both asthma and COPD in the first 30 months were assigned to the comorbid COPD and asthma cohort. Claims information was collected until December 31, 2003.
Patients who were < 40 or > 65 years of age were excluded. The younger cutoff was to exclude patients who were more likely to have asthma than COPD. The older cutoff corresponds to the age at which many patients are dually eligible for Medicare and, thus, were excluded from this study as described previously.
Health-care and medical health services utilization was defined as all procedures, tests, and services performed by each point of service (ie, inpatient, outpatient, and physician), and the type of expenditure was determined by the point of service. Outpatient point of service was defined as within a hospital practice yet not admitted to the hospital (inpatient). Physician point of service was defined as a practice outside of a hospital. Costs were imputed based on Medicaid fee schedules.
The Charlson comorbidity index (CCI)13 was used to adjust for the severity of comorbid illness of each patient. Asthma and COPD scores were removed from the CCI to avoid double counting the burden of these conditions. Figure 1 illustrates the cohort selection process.
Figure 1.
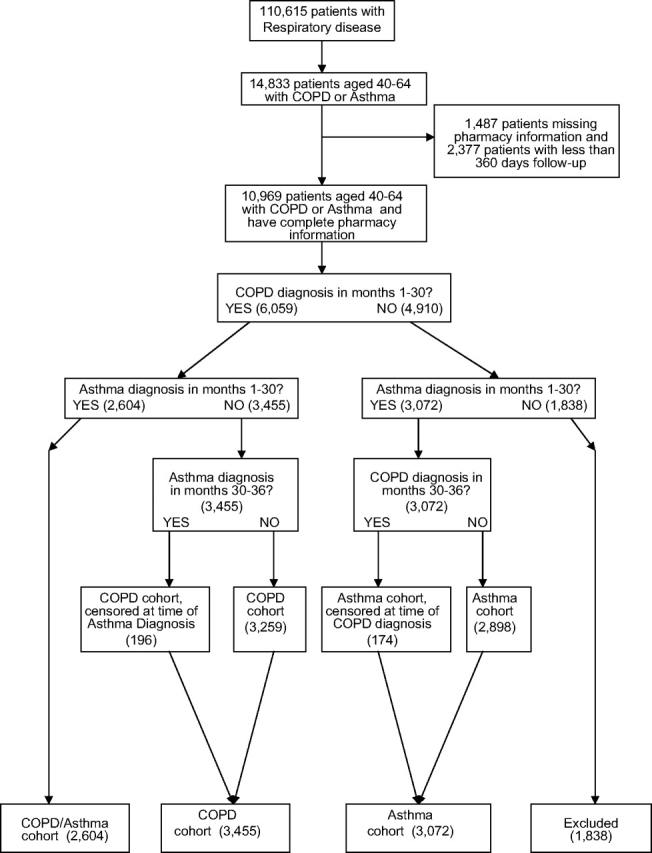
Flow chart of cohort selection.
This study used deidentified claims data, with no option for informed consent. The study qualified as exempt by the University of Maryland Internal Review Board, protocol exemption No. H-23480.
Statistical Analysis
Health-care and medical health services utilization was examined by combining all COPD-specific or asthma-specific utilization data and identifying the type of medical utilization, including physician office visits and outpatient services. All health services utilization was annualized (annual counts of all services), and the corresponding annualized costs (the sum of all services) were calculated on the basis of the average unit cost for each type of service, as derived from Medicaid fee schedules. Multivariate analyses were conducted, using logistic regression models, to predict utilization patterns and costs. Costs were analyzed by comparing the top 25th percentile of medical utilization with the lower 75th percentile. Other factors controlled for in the multivariate analyses were race, age, gender, CCI, and cohort allocation. The incremental burden of COPD was calculated by subtracting the costs of the asthma cohort from the costs of the comorbid COPD and asthma cohort. Bivariate analysis was used to compare utilization and costs by race, age, gender, and comorbidity.
Results
Table 1 shows the demographic characteristics of the three study cohorts. The total study population consisted of 9,131 patients with COPD, asthma, or both conditions. Of the total population, 52% were African American (n = 4,723), and 44% were white (n = 4,021); all other races were combined into an “unknown race” category to account for the remaining 4% of the population (n = 387).
Table 1.
Demographic Characteristics of Study Cohorts
| Characteristics | All Patients | Asthma Cohort | COPD Cohort | Comorbid COPD and Asthma Cohort | p Value |
|---|---|---|---|---|---|
| Sample size | 9,131 (100) | 3,072 (33.64) | 3,455 (37.84) | 2,604 (28.52) | |
| Race | |||||
| White | 4,021 (44) | 959 (31) | 1,747 (51) | 1,315 (51) | < 0.0001 |
| African American | 4,723 (52) | 1,946 (63) | 1,579 (46) | 1,198 (46) | |
| Other | 387 (4) | 167 (5) | 129 (4) | 91 (3) | |
| Age group | |||||
| 40–49 yr | 4,273 (47) | 1,942 (63) | 1,231 (36) | 1,100 (42) | < 0.0001 |
| 50–64 yr | 4,858 (53) | 1,130 (37) | 2,224 (64) | 1,504 (58) | |
| Gender | |||||
| Women | 6,398 (70) | 2,557 (83) | 1,868 (54) | 1,973 (76) | < 0.0001 |
| Men | 2,733 (30) | 515 (17) | 1,587 (46) | 631 (24) |
Values are given as No. (%), unless otherwise indicated.
The three cohorts were balanced with regard to the number of patients with a study condition, as follows: asthma, 33.6% (n = 3,072); COPD, 37.8% (n = 3,455); and comorbid COPD and asthma, 28.5% (n = 2,604). In the asthma cohort, > 63% of the patients (n = 1,946) were African American, which is about 12% higher than the proportion of African-American patients in the entire study population. White patients comprised 31% of the asthma cohort (n = 959), and other races accounted for the remaining 5% (n = 167). The COPD and comorbid COPD and asthma cohorts had similar racial composition, with African-American patients comprising 46%; whites, 51%; and other races, 3% in each cohort.
Patients were divided into one of two groups by age, as follows: 40 to 49 years of age (47% of the study population) and 50 to 64 years of age (53%). The asthma cohort comprised predominantly younger patients (40-to-49-year-old age group, 63%), whereas the COPD and comorbid COPD and asthma cohorts were dominated by the older patients (50-to-64-year-old age group, 64% and 58%, respectively).
Female patients comprised 70% of the study population. Women were overrepresented in the asthma cohort (83%), underrepresented in the COPD cohort (54%), and relatively well represented in the comorbid COPD and asthma cohort (76%). Although male patients comprised 30% of the study population, they accounted for 17% of the asthma cohort, 46% of the COPD cohort, and 24% of the comorbid COPD and asthma cohort.
The older age group had higher mean health services utilization and higher average medical costs than the younger group. Similar means were found for female and male patients for both health services utilization, including physician visits, hospitalizations, and emergency department visits (average frequencies, 13 and 12, respectively; p = 0.170), and cost ($6,872 and $6,883, respectively; p = 0.984). Patients in the comorbid COPD and asthma cohort had significantly higher cost ($14,914) and health services utilization (average frequency, 26) than patients in the asthma ($2,307; average frequency, 7; p < 0.0001) and COPD ($4,879; average frequency, 8; p < 0.0001) cohorts. The mean medical cost for the COPD cohort was higher than that for the asthma cohort ($4,879 vs $2,307, respectively). There was a significant difference between the COPD and asthma cohorts with respect to the mean annualized medical health services utilization (average frequency, 8 and 7, respectively; p < 0.0001).
Table 2 reports annualized health services utilization, aggregated for all three cohorts by race. On average, annualized health services utilization for white patients was higher than those for African Americans and other races. Further, the mean of health services utilization and number of physician office visits were higher for white patients than for African Americans or all others. Table 3 reports the mean health services utilization costs by race for the comorbid COPD and asthma cohort.
Table 2.
Mean Annualized Resource Utilization by Race
| Resources | White (n = 4,021) | African American (n = 4,723) | Other (n = 387) |
|---|---|---|---|
| All medical utilization | 14 (2; 6; 16) | 12 (1; 5; 13) | 12 (1; 5; 12) |
| Physician office visits | 8 (1; 3; 8) | 6 (1; 2; 7) | 7 (1; 3; 7) |
| Outpatient services | 2 (0; 0; 2) | 2 (0; 0; 2) | 2 (0; 0; 2) |
| Inpatient services | 4 (0; 0; 4) | 4 (0; 0; 0) | 3 (0; 0; 0) |
Values are given as the mean (25th percentile; median; 75th percentile). Mean annualized resource utilization = the mean of the annual counts of all services.
Table 3.
Mean Annualized Cost Related to COPD and Asthma by Race
| Cost Categories | White (n = 4,021), $ | African American (n = 4,723), $ | Other (n = 387), $ |
|---|---|---|---|
| Office visits | 668 (36; 106; 298) | 403 (26; 84; 249) | 421 (29; 105; 312) |
| Outpatient services | 343 (0; 0; 299) | 295 (0; 0; 232) | 247 (0; 0; 176) |
| Inpatient services | 6,601 (0; 0; 2,693) | 5,594 (0; 0; 0) | 5,017 (0; 0; 0) |
| Medical utilization | 7,649 (66; 328; 4,173) | 6,313 (52; 252; 2,158) | 5,706 (51; 290; 1,914) |
Values are given as the mean (25th percentile; median; 75th percentile). Mean annualized cost = the mean of the sum of all services calculated based on the average unit cost for each type of service derived from Medicaid fee schedules.
Table 4 reports the results of multivariate logistic regression on health services utilization and costs related to COPD or asthma. Table 4 shows that African-American patients used 17% fewer medical services, including physician visits, hospitalizations, and emergency department visits, than white patients (odds ratio [OR], 0.83; 95% confidence interval [CI], 0.75 to 0.93). African-American patients showed 18% less utilization of outpatient services than white patients (OR, 0.82; 95% CI, 0.74 to 0.91). Other races also were 26% less likely to use outpatient services than white patients (OR, 0.74; 95% CI, 0.57 to 0.96). African-American patients showed 15% less utilization of inpatient services than white patients (OR, 0.85; 95% CI, 0.76 to 0.94) and costs that were 14% below those of the white group (OR, 0.86; 95% CI, 0.77 to 0.96). There were no detectable differences in the utilization of other health services between whites and others.
Table 4.
Multivariate Logistic Regression on Medical Utilization and Cost Related to COPD and Asthma
| Utilization, Count |
Physician Visits, Count |
Outpatient Services, Count |
Inpatient Services, Count |
Cost Top 25th vs low 75th, $ |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Effects | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Race | ||||||||||
| White (reference) | ||||||||||
| African American | 0.83 | 0.75–0.93 | 0.90 | 0.81–1.00 | 0.82 | 0.74–0.91 | 0.85 | 0.76–0.94 | 0.86 | 0.77–0.96 |
| Other | 0.83 | 0.64–1.09 | 1.03 | 0.8–1.34 | 0.74 | 0.57–0.96 | 0.85 | 0.65–1.11 | 0.92 | 0.71–1.20 |
| Age groups | ||||||||||
| 40–49 yr (reference) | ||||||||||
| 50–64 yr | 1.28 | 1.15–1.43 | 1.39 | 1.25–1.54 | 0.82 | 0.74–0.91 | 1.25 | 1.12–1.38 | 1.29 | 1.17–1.44 |
| Gender | ||||||||||
| Male (reference) | ||||||||||
| Female | 1.06 | 0.94–1.19 | 1.06 | 0.94–1.18 | 1.01 | 0.90–1.14 | 1.18 | 1.05–1.33 | 1.16 | 1.03–1.30 |
| CCI | 1.08 | 1.06–1.10 | 1.01 | 0.99–1.03 | 1.01 | 1.00–1.03 | 1.14 | 1.12–1.16 | 1.13 | 1.11–1.15 |
| Disease cohorts | ||||||||||
| Asthma (reference) | ||||||||||
| COPD | 1.21 | 1.05–1.41 | 1.16 | 1.01–1.34 | 0.40 | 0.35–0.46 | 1.51 | 1.31–1.74 | 1.50 | 1.30–1.74 |
| COPD and asthma | 6.29 | 5.5–7.20 | 5.32 | 4.67–6.07 | 2.39 | 2.12–2.69 | 5.21 | 4.55–5.97 | 5.25 | 4.59–6.02 |
Adjusted multivariate logistic regression results from Table 4 show that patients in the older age group were more likely to have higher overall health services utilization (OR, 1.28; 95% CI, 1.15 to 1.43), physician services (OR, 1.39; 95% CI, 1.25 to 1.54), and inpatient services (OR, 1.25; 95% CI, 1.12 to 1.38). Additionally, they had higher costs (OR, 1.29; 95% CI, 1.17 to 1.44) than the younger group.
The patients who had a higher comorbidity burden, as reflected by their CCI, were more likely to use medical resources, and the cost for using such resources was significantly higher. The comorbid COPD and asthma cohort had significantly higher health services utilization (OR, 6.29; 95% CI, 5.5 to 7.2) and costs (OR, 5.25; 95% CI, 4.59 to 6.02) than the asthma cohort. Patients with COPD also had higher health services utilization (OR, 1.21; 95% CI, 1.05 to 1.41) and costs (OR, 1.50; 95% CI, 1.30 to 1.74) than the reference group (Table 4).
Discussion
COPD and asthma present a number of medical, public health, and economic concerns for patients, physicians, and insurers as well as for the community, which often shares the impact of the disease. This study compared health services utilization and cost outcomes in Maryland Medicaid Managed Care adult beneficiaries with COPD, asthma, or coexisting COPD and asthma. We found significant differences by race in health services utilization. Contrary to our expectations across all three study cohorts, African-American patients consistently used fewer overall medical services, outpatient physician visits, and hospitalizations than their white counterparts, which accounted for lower medical costs associated with obstructive lung disease. This finding held true even after adjusting for age, gender, and comorbidities, and in the presence of uniform socioeconomic status. We specifically differentiated among COPD, asthma, and concomitant COPD and asthma because our previous study10 showed differential utilization across these cohorts.
There are few published data regarding racial disparities in the treatment choice of COPD.14 Some literature15–18 on disparities has pointed to the differences in access to health care and quality of care, with African Americans less likely to receive adequate care than whites. Egede and Zheng19 demonstrated that African-American patients are less likely to receive a preventive health-care measure, such as influenza vaccine, than white counterparts with similar health conditions. Our findings show lower utilization of medical care by African Americans, even after controlling for disease, age, gender, and comorbidities.
The finding that lower health-care costs are associated with African Americans than with whites could represent, in addition to other factors, poorer access to care. Because our cohorts represented patients from only one equally insured economic stratum, we do not believe that economic factors played a role in determining access to health care. We have no data that address the possibility that a difference exists in available health-care facilities serving the African-American and white cohorts. Further, we cannot determine whether cultural differences exist with regard to willingness to utilize health-care resources between groups. However, it seems likely that if one cohort was less willing to utilize outpatient resources, it would be more likely to utilize inpatient services, but this was not the case in our study, which showed that African Americans utilized fewer resources for all types of health services. Mortality figures were not available in the database; thus, we cannot say whether lower hospitalization costs represent a differential effect of obstructive lung disease between groups.
Racial differences in health-care utilization could have been due to differences in environmental exposure. For COPD, the prime exposure risk is cigarette smoking, Dransfield3 and Hall13 have documented the differences in smoking rates by race. Further, there may be differences in lag time between the initiation of smoking and the development of respiratory disease, including COPD. Higher health services utilization rates among whites in our study may mimic the early popularity of smoking among this group, now apparent after an attendant lag interval. If this speculation is true, utilization rates among African Americans may show a change in the future. There may be phenotypic differences between African Americans and whites in the response to environmental exposure, which may include different degrees of disease severity for the same degree of disease severity. These factors need to be explored in future studies.
Limitations to this study include those normally associated with retrospective claims analyses. As noted, we could not address differences in smoking behavior of the groups, and accuracy of diagnoses cannot be verified. Our data collection method, using claims data from only one source population (Maryland Medicaid Managed Care) may be subject to selection and channeling bias. There may be reasons that access to Maryland Medicaid Managed Care is easier for white beneficiaries who are worse off clinically than African-American counterparts. Our study used no disease severity indicator within each cohort because that information was lacking in the encounter data, thus limiting our findings regarding health services utilization and cost outcomes. Therefore, one cannot discount the idea that the African-American population in this cohort could be less sick. Future studies exploring racial disparities in health services utilization will have to account for severity of obstructive lung disease (eg, FEV1, symptom scores, and arterial blood gas measurements) as well as severity of environmental exposure (smoking). However, even in the absence of these details, the findings are surprising and bear further investigation, especially with regard to possible racial differences in the willingness to use medical care resources, self-treat, or seek a diagnosis.
We conclude that in a Medicaid population, health-care utilization rates for obstructive lung disease, both outpatient and inpatient, were lower for African-American than white patients. This finding could represent differences in relevant environmental exposure, geographic access to health-care facilities, cultural differences in the willingness to use health-care resources, or phenotypic differences in disease severity or clinical presentation. Future studies should be directed at exploring these factors as indices of mortality and morbidity between these racial groups.
Acknowledgments
Author contributions: All authors participated in the study conception, design, analysis, interpretation of results, and revision of the manuscript, and approved the final version of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to the ACCP that no significant conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Army, the Department of Defense or the US Government.
Abbreviations:
- CCI
Charlson comorbidity index
- CI
confidence interval
- OR
odds ratio
Footnotes
Funding/Support: This research was supported by National Heart, Lung, and Blood Institute Grant HL07441 (S.L.S.).
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal.org/site/misc/reprints.xhtml).
References
- 1.Murphy RE, Katz S, Massaro DJ, et al. Is emphysema a disease predominantly of the white male? Preliminary report. JAMA. 1962;181:726–727. doi: 10.1001/jama.1962.03050340064016a. [DOI] [PubMed] [Google Scholar]
- 2.Mannino DM, Gagnon RC, Petty TL, et al. Obstructive lung disease and low lung function in adults in the United States: data from the National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2000;160:1683–1689. doi: 10.1001/archinte.160.11.1683. [DOI] [PubMed] [Google Scholar]
- 3.Dransfield MT, Bailey WC. COPD: racial disparities in susceptibility, treatment, and outcomes. Clin Chest Med. 2006;27:463–471. doi: 10.1016/j.ccm.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 4.Chatila WM, Wynkoop WA, Vance G, et al. Smoking patterns in African Americans and whites with advanced COPD. Chest. 2004;125:15–21. doi: 10.1378/chest.125.1.15. [DOI] [PubMed] [Google Scholar]
- 5.McDaniel M, Paxson C, Waldfogel J. Racial disparities in childhood asthma in the United States: evidence from the National Health Interview Survey, 1997 to 2003. Pediatrics. 2006;117:e868–e877. doi: 10.1542/peds.2005-1721. [DOI] [PubMed] [Google Scholar]
- 6.Gupta RS, Carrion-Carire V, Weiss KB. The widening black/white gap in asthma hospitalizations and mortality. J Allergy Clin Immunol. 2006;117:351–358. doi: 10.1016/j.jaci.2005.11.047. [DOI] [PubMed] [Google Scholar]
- 7.Shanawani H. Health disparities and differences in asthma: concepts and controversies. Clin Chest Med. 2006;27:17–28. doi: 10.1016/j.ccm.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 8.Lugogo NL, Kraft M. Epidemiology of asthma. Clin Chest Med. 2006;27:1–15. doi: 10.1016/j.ccm.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 9.Crater DD, Heise S, Perzanowski M, et al. Asthma hospitalization trends in Charleston, South Carolina, 1956 to 1997: twenty-fold increase among black children during a 30-year period. Pediatrics. 2001;108:E97. doi: 10.1542/peds.108.6.e97. [DOI] [PubMed] [Google Scholar]
- 10.Shaya FT, Dongyi D, Akazawa MO, et al. Burden of concomitant asthma and COPD in a Medicaid population. Chest. 2008;134:14–19. doi: 10.1378/chest.07-2317. [DOI] [PubMed] [Google Scholar]
- 11.Howard DL, Hakeem FB, Njue C, et al. Racially disproportionate admission rates for ambulatory care sensitive conditions in North Carolina. Public Health Rep. 2007;122:362–372. doi: 10.1177/003335490712200310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottlieb DJ, Beiser AS, O'Connor GT. Poverty, race, and medication use are correlates of asthma hospitalization rates: a small area analysis in Boston. Chest. 1995;108:28–35. doi: 10.1378/chest.108.1.28. [DOI] [PubMed] [Google Scholar]
- 13.Hall WH, Ramachandran R, Narayan S, et al. An electronic application for rapidly calculating Charlson Comorbidity Score. BMC Cancer. 2004;4:94. doi: 10.1186/1471-2407-4-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foreman MG, Willsie SK. Healthcare disparities in critical illness. Clin Chest Med. 2006;27:473–486. doi: 10.1016/j.ccm.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Cabana MD, Lara M, Shannon J. Racial and ethnic disparities in the quality of asthma care. Chest. 2007;132(suppl):810S–817S. doi: 10.1378/chest.07-1910. [DOI] [PubMed] [Google Scholar]
- 16.Davis AM, Kreutzer R, Lipsett M, et al. Asthma prevalence in Hispanic and Asian American ethnic subgroups: results from the California Healthy Kids Survey. Pediatrics. 2006;118:e363–e370. doi: 10.1542/peds.2005-2687. [DOI] [PubMed] [Google Scholar]
- 17.Lieu TA, Lozano P, Finkelstein JA, et al. Racial/ethnic variation in asthma status and management practices among children in managed Medicaid. Pediatrics. 2002;109:857–865. doi: 10.1542/peds.109.5.857. [DOI] [PubMed] [Google Scholar]
- 18.Jha AK, Shlipak MG, Hosmer W, et al. Racial differences in mortality among men hospitalized in the Veterans Affairs healthcare system. JAMA. 2001;285:297–303. doi: 10.1001/jama.285.3.297. [DOI] [PubMed] [Google Scholar]
- 19.Egede LE, Zheng D. Racial/ethnic differences in influenza vaccination coverage in high-risk adults. Am J Public Health. 2003;93:2074–2078. doi: 10.2105/ajph.93.12.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]


