Abstract
Background
For women, who are more likely to live in poverty, defining the clinical and economic impact of socioeconomic factors may aid in defining redistributive policies to improve healthcare quality.
Methods
The NIH-NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE) enrolled 819 women referred for clinically indicated coronary angiography. This study's primary end point was to evaluate the independent contribution of socioeconomic factors on the estimation of time to cardiovascular death or myocardial infarction (MI) (n = 79) using Cox proportional hazards models. Secondary aims included an examination of cardiovascular costs and quality of life within socioeconomic subsets of women.
Results
In univariable models, socioeconomic factors associated with an elevated risk of cardiovascular death or MI included an annual household income <$20,000 (p = 0.0001), <9th grade education (p = 0.002), being African American, Hispanic, Asian, or American Indian (p = 0.016), on Medicaid, Medicare, or other public health insurance (p < 0.0001), unmarried (p = 0.001), unemployed or employed part-time (p < 0.0001), and working in a service job (p = 0.003). Of these socioeconomic factors, income (p = 0.006) remained a significant predictor of cardiovascular death or MI in risk-adjusted models that controlled for angiographic coronary disease, chest pain symptoms, and cardiac risk factors. Low-income women, with an annual household income <$20,000, were more often uninsured or on public insurance (p < 0.0001) yet had the highest 5-year hospitalization and drug treatment costs (p < 0.0001). Only 17% of low-income women had prescription drug coverage (vs. ≥50% of higher-income households, p < 0.0001), and 64% required ≥2 anti-ischemic medications during follow-up (compared with 45% of those earning ≥$50,000, p < 0.0001).
Conclusions
Economic disadvantage prominently affects cardiovascular disease outcomes for women with chest pain symptoms. These results further support a profound intertwining between poverty and poor health. Cardiovascular disease management strategies should focus on policies that track unmet healthcare needs and worsening clinical status for low-income women.
Introduction
Socioeconomic status is inversely related to cardiovascular outcome, with lower strata patients having worse cardiac risk factor profiles and higher case fatality rates.1–6 Although age, ethnicity, and gender are significant covariates acting within this association of socioeconomic status to outcome, research among women has largely focused on the impact of social support, networks, and strain on patient well-being.7–10 For women, measurement of the impact of socioeconomic factors on estimation of cardiovascular prognosis and quality of life is important for the design of sex-specific focused interventions for people in lower socioeconomic strata.11 Limited data are available in female cohorts about the interplay among socioeconomic factors, including income, education, employment status, and health insurance coverage, and their impact on adverse cardiovascular outcomes, including quality of life and resource consumption patterns.2,12
Thus, the aim of the current report was to explore the relative contribution of multiple socioeconomic factors as estimators of major cardiovascular events and quality of life in 819 women prospectively enrolled in the NIH-NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE). A secondary aim was to evaluate cardiovascular costs across socioeconomic subsets of WISE women.
Materials and Methods
Patient entry criteria
The WISE study methods were reported previously.13,14 In brief, women enrolled in WISE included those seeking evaluation of chest pain symptoms and referred for clinically indicated coronary angiography. All women had signs and symptoms suggestive of myocardial ischemia prior to enrollment in WISE. Of a consecutive series of 7603 women, 936 were enrolled in the WISE. Reporting of income was voluntary and was not available for 117 women; clinical characteristics for those without income data were similar to those of the 819 women included herein. All study procedures and follow-up methodologies were approved by each center's investigational review board.
Baseline evaluation
Detailed demographic and medical history characteristics were collected (Table 1), and blood pressure and heart rate were recorded at study entry. Other cardiovascular risk marker data were collected, including lipid measurements and body mass index (BMI).
Table 1.
A Comparison of Baseline Clinical History and Socioeconomic Measurements by Annual Income Levels
| <$20,000 (n = 308) | $20,000–$49,999 (n = 352) | $50,000–$99,999 (n = 124) | ≥$100,000 (n = 35) | p value | |
|---|---|---|---|---|---|
| Age (in years), mean ± SD (range) | 58.6 ± 11 (21–83) | 58.6 ± 12 (27–86) | 56.2 ± 11 (33–82) | 55.6 ± 9 (40–79) | 0.096 |
| Post-Menopausea | 78% | 73% | 72% | 66% | 0.70 |
| Cardiac risk factors and cardiometabolic syndrome | |||||
| Hypertension | 66% | 61% | 44% | 31% | <0.0001 |
| Diabetes | 32% | 23% | 18% | 9% | <0.0001 |
| Current smoker | 26% | 17% | 15% | 6% | 0.021 |
| Body mass index (kg/m2) | 31 ± 7 | 30± 7 | 28± 6 | 29± 6 | 0.006 |
| Metabolic syndromeb | 55% | 44% | 37% | 33% | 0.009 |
| Comorbid conditions | |||||
| Cerebrovascular disease | 15% | 8% | 4% | 6% | 0.001 |
| Renal dysfunction | 5% | 2% | 1% | 0% | 0.014 |
| Depression requiring treatment | 32% | 21% | 17% | 26% | 0.002 |
| Alcohol use | 8% | 16% | 21% | 26% | <0.0001 |
| Presenting cardiac symptoms | |||||
| Typical angina | 35% | 26% | 33% | 20% | 0.050 |
| Dyspnea on presentation | 70% | 48% | 53% | 49% | <0.0001 |
| Prior stress resting, anti-ischemic therapy use, and angiographic results | |||||
| Positive stress test | 36% | 50% | 56% | 57% | <0.0001 |
| Nitroglycerin use | 59% | 40% | 37% | 36% | <0.0001 |
| Angiographic CAD | 0.032 | ||||
| No 50% Stenosis | 59% | 61% | 66% | 71% | |
| 1 vessel | 19% | 15% | 13% | 27% | |
| 2–3 Vessel | 23% | 24% | 21% | 2% | |
| Socioeconomic factors | |||||
| Ethnicity | <0.0001 | ||||
| Black | 31% | 13% | 3% | 6% | |
| Hispanic, Asian, or Indianc | 1% | 1% | 3% | 0% | |
| White | 68% | 86% | 95% | 91% | |
| Marital status | <0.0001 | ||||
| Never Married | 8% | 5% | 0% | 0% | |
| Divorced/separated | 29% | 13% | 4% | 0% | |
| Widowed | 27% | 16% | 3% | 0% | |
| Married | 32% | 65% | 90% | 100% | |
| Living in a marriage-like relationship | 4% | 3% | 3% | 0% | |
| Education | <0.0001 | ||||
| <High school diploma | 38% | 11% | 3% | 0% | |
| High school diploma | 38% | 47% | 31% | 17% | |
| Some college/vocational training | 19% | 31% | 32% | 34% | |
| College graduate or higher | 5% | 11% | 34% | 49% | |
| Health insurance | |||||
| Medicare | 44% | 24% | 22% | 0% | |
| Other publicd | 18% | 5% | 2% | 9% | |
| Private | 25% | 69% | 76% | 91% | |
| None/self-pay | 13% | 2% | 0% | 0% | |
| Employment statuse | |||||
| Full-time | 14% | 31% | 38% | 43% | <0.0001 |
| Part-time | 5% | 8% | 13% | 14% | <0.0001 |
| Retired | 33% | 32% | 26% | 20% | <0.0001 |
| Disablede | 31% | 14% | 6% | 0% | <0.0001 |
Postnenopause was defined by at least 12 months of amenorrhea or prior bilateral salpingo-oophorectomy.
Metabolic syndrome defined as any three of the following: waist circumference >35 inches, triglycerides ≥150 mg/dL, HDL cholesterol <50 mg/dL, hypertension, and fasting glucose ≥110 mg/dL.
Precise definition for ethnicity includes Hispanic, Asian or Pacific Islander, American Indian or Alaskan Native.
Other public insurance, Medicaid or Civilian Health and Medical Program of the Uniformed Services (CHAMPUS).
Subsets within Employment status are not exclusive; affirmative responses may be included within multiple categories. Within these categories is the term disabled, which is defined as those receiving Social Security disability benefits.
Quality of life measurements
Data on patients' self-reported quality of life, satisfaction, and well-being were collected.15 Functional disability was scored using the Duke Activity Status Index (DASI) estimated metabolic equivalents (METs).16 The DASI is a 12-item questionnaire that documents patient's self-reported difficulties in routine activities of daily living (e.g., vacuuming), self-care (e.g., bathing), ability to ambulate, and recreational activities.
Socioeconomic status
Socioeconomic factors collected were ethnicity, marital status, highest level of education, retirement status, employment and vocational status, disability status, income, and health insurance coverage.17 Health insurance coverage included primary and supplemental plans. Household income was categorized as <$20,000 (n = 308), $20,000–$49,999 (n = 352), $50,000–$99,999 (n = 124), and ≥$100,000 (n = 35). For comparative purposes, low-income women are defined as those with an annual household income of <$20,000 vs. higher-income women.
For education, the three groups included post-high school vocational or college education (n = 360), 9th–12th grade or general equivalency diploma (n = 489), or <9th grade (n = 51). Within WISE, 739 women were Caucasian, non-Hispanic, 161 were black or African American, and 11 were Hispanic, Asian, American Indian, or Alaskan Native. Marital status included married (n = 523), divorced, separated, widowed, living in a marriagelike situation (n = 337), or never married (n = 47).
Angiography core laboratory
The extent of coronary disease was defined as the number of vessels with ≥50% stenosis.18
Follow-up outcomes
Patients were contacted at 6 weeks and then yearly for 5 years of follow-up. During contact, a scripted interview was used to ascertain cardiovascular hospitalizations or death. Death certificates or medical records were independently reviewed to determine causality. Data on medication use, office or community health clinic visits, and cardiac procedures were collected.
Collection of cardiovascular costs
The WISE cost methodology has been published previously.19 Briefly, total cardiovascular costs were summed using standard approaches including 5% annual discount rate and inflation correction based on the U.S. medical service sector estimate (city average) of the consumer price index (for urban wage earners and clerical workers).19 Five-year costs for cardiovascular hospitalizations, emergency department visits, coronary revascularization and angiography, outpatient testing, and visits to generalist, specialists, nurse practitioners/physician's assistant, or community clinics were summed. Indirect cost data were estimated based on hours lost from work for healthcare, reduced productivity hours, transportation costs to the doctor or hospital, and out-of-pocket costs for drugs, medical devices (e.g., glucometer), and alternative therapies (e.g., vitamins).
Statistical analysis
Descriptive statistics included comparisons of categorical variables by chi-square statistic or continuous variables using analysis of variance (ANOVA) techniques. Quality of life measurements were compared by socioeconomic subsets using a chi-square statistic. The DASI was compared using ANOVA techniques. The mean ± standard deviation (SD) DASI METs were plotted over time using a trendline fitted with a polynomial function.
Our prognostic modeling was performed in several stages. We first evaluated the univariable prediction of various socioeconomic factors. Our next step was to consider the independent contribution of socioeconomic factors above and beyond clinical variables, including chest pain symptoms, angiographic coronary disease, cardiac risk factors, and BMI. Our final evaluation included a stepwise model to provide some inference about the relative importance or rank of socioeconomic factors in relation to clinical variables (including chest pain symptoms, angiographic coronary disease, cardiac risk factors, and BMI). The specifics of our statistical analyses are as follows: Time to cardiovascular death or myocardial infarction (MI) was estimated using univariable and multivariable Cox proportional hazard models. From the Cox model, unadjusted survival curves were plotted. Risk-adjusted models included socioeconomic variables plus the following clinical covariates: angiographic coronary disease, cardiac risk factors, symptoms, and BMI. Model overfitting procedures were considered by limiting the number of variables included in any given model to only 1 for every 10 outcomes. Moreover, the proportional hazards assumption was met for all survival analyses. Relative risk ratios (95% confidence intervals [CI]) were calculated. Stepwise Cox regression modeling was employed to identify the single greatest socioeconomic estimator of outcome. This latter model included socioeconomic and clinical variables within the risk-adjusted model described.
Costs were compared for women by income subsets using general linear modeling techniques adjusted by the DASI estimate of METs as a surrogate for disability. Further risk adjustment by including age or angiographic coronary disease did not influence the results presented herein.
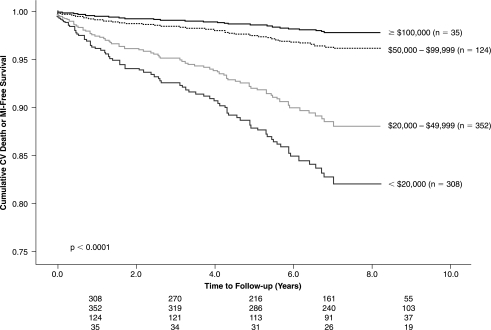
A post-hoc sample size calculation revealed that there was sufficient power to detect differences in survival across income subsets (β ≥ 0.80, α = 0.05, 2-tailed) (Power and Precision,™ v. 2.0). We specifically compared cardiovascular event-free survival, defined as cardiovascular death or nonfatal MI (Fig. 2), for women with an annual household income of ≥$50,000 as compared with those in the low income strata of <$20,000.
FIG. 2.
Survival free from cardiovascular (CV) death or nonfatal myocardial infarction (MI) by annual household income of <$20,000, $20,000–$49,999, $50,000–$99,999, and ≥$100,000, respectively.
Results
Clinical characteristics of WISE women by household income
Women earning <$20,000 per year (i.e., low income) had a greater degree of comorbidity and symptom burden, including more typical angina (p = 0.050) and angiographic coronary disease (p = 0.032) (Table 1).
Fewer women from low-income households were married compared with women with a household income of ≥$50,000 (p < 0.0001). Additionally, approximately 1 in 3 low-income women were black, whereas less than 1 in 10 higher-income women were non-Caucasian (p < 0.0001). Additionally, 24% of women earning <$20,000 per year, as compared with nearly 7 of 10 women earning ≥$50,000 per year, had post-high school training or education (p < 0.0001). Full-time employment was reported in 14%, 31%, 38%, and 43% of women reporting incomes of <$20,000, $20,000–$49,999, $50,000–$99,999, and ≥$100,000, respectively (p < 0.0001).
Quality of life measurements by household income
Women from low-income households more often perceived their health as fair/poor (p < 0.0001) and had a reduced perceived quality of life (p < 0.0001) (Table 2). Finally, nearly half of low-income women were living alone, whereas none of the women in higher household income strata (i.e., >$20,000) lived alone (p = 0.0003).
Table 2.
Quality of Life Measurements at Study Entry by Household Income
| <$20,000 (n = 308) | $20,000–$49,999 (n = 352) | $50,000–$99,999 (n = 124) | ≥$100,000 (n = 35) | p value | |
|---|---|---|---|---|---|
| Functional disability, defined as estimated DASI METsa <4.7 | 31% | 13% | 6% | 0% | <0.0001 |
| Fair/poor perceived health | 57% | 34% | 21% | 12% | <0.0001 |
| Low perceived quality of lifeb | 10% | 6% | 4% | 3% | <0.0001 |
| Health impairs work or lost days from work due to health | 81% | 77% | 40% | 60% | 0.023 |
| History of psychosocial stress | 34% | 31% | 33% | 49% | 0.204 |
| Living alone at 5 years of follow-up | 45% | 0% | 0% | 0% | 0.003 |
DASI METs, Duke Activity Status Index estimate of metabolic equivalents.
Perceived quality of life ranged from 0 to 3 out of 10, with 10 being excellent.
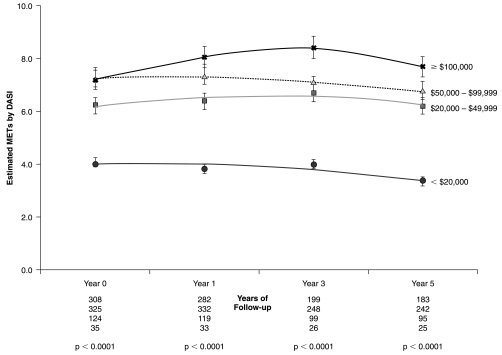
Low-income women had reduced physical functioning (as measured by decreased DASI estimated METs) (Fig. 1) (p < 0.0001). The DASI score was approximately 3 METs lower for women with an annual income <$20,000 compared with those earning <$50,000 per year (p < 0.0001). Nearly half of low-income women stated that they had trouble walking one to two blocks on level ground (p < 0.0001), and 80% noted difficulties in climbing a flight of stairs or walking uphill (p < 0.0001).
FIG. 1.
Estimated metabolic equivalents (METs) (average ± SD) by the Duke Activity Status Index (DASI) at baseline through 5 years of follow-up by household income <$20,000, $20,000–$49,999, $50,000–$99,999, and ≥$100,000, respectively. The line of best-fit between baseline and through 5 years of follow-up was fit with a polynomial function.
The average MET value for low-income women started at 4.1, declining to 3.3 at 5 years of follow-up (Fig. 1). At baseline and throughout follow-up, higher-income women achieved greater DASI estimated METs (p < 0.0001). For women with an annual household income of ≥$50,000, DASI scores ranged from 6.8 to 8.4 METs during follow-up.
Univariable estimators of outcome
At 5.0 ± 2.6 years of follow-up, 79 women died secondary to cardiovascular disease or were hospitalized for an acute MI. Female subsets at highest risk (i.e., significant univariable estimators) included women with annual household income <$20,000 (p < 0.0001), employed less than full time (p < 0.0001), on publically funded health insurance (p < 0.0001), <9th grade education (p = 0.002), in service positions (p = 0.006), being African American, Hispanic, Asian, or American Indian (p = 0.008), or unmarried (p = 0.022) (Table 3).
Table 3.
Socioeconomic Factors Predictive of Cardiovascular Death or Nonfatal Myocardial Infarction in Unadjusted and Risk-Adjusteda Cox Proportional Hazards Models
| Unadjusted Relative risk (95% CI) | Unadjusted model Chi-square, p value | Risk-adjusted Relative risk (95% CI0 p value | |
|---|---|---|---|
| Income level | 4.91 | 23, <0.0001 | 4.76 (1.68–13.45) |
| <$20,000 vs. ≥$50,000 | (2.11–11.44) | p = 0.006 | |
| Employment | 4.33 | 16, <0.0001 | 3.98 (1.59–9.97) |
| part-time employment, or unemployed vs. full-time employment | (2.00–9.35) | p = 0.001 | |
| Education | 3.51 | 12, 0.002 | 2.84 (1.33–6.06) |
| 9th–12th grade, GED,b or <9th grade vs. post-high schoolc | (1.76–6.99) | p = 0.017 | |
| Ethnicity | 1.77 | 10, 0.008 | 1.49 (0.90–2.51) |
| Black, Hispanic, Asian/Pacific Islander, or American Indian/Alaskan Native vs. Caucasian non-Hispanic | (1.13–2.77) | p = 0.13 | |
| Insurance status | 3.27 | 16, <0.0001 | 2.13 (1.0–4.52) |
| Publicd or no health insurance vs. private HMO/PPO | (1.72–6.21) | p = 0.054 | |
| Marital status | 2.51 | 8, 0.022 | 2.41 (1.12–5.20) |
| Divorced, separated, living in a marriage-like situation, or never married vs. married | (1.23–5.14) | p = 0.06 | |
| Retired | 1.62 | 5, 0.023 | 1.46 (0.91–2.35) |
| Retired vs. not retired | (1.07–2.44) | p = 0.213 | |
| Vocation | |||
| Service job | 1.79 | 8, 0.006 | 1.51 (0.94–2.41) |
| Service vs. non-service job | (1.18–2.71) | p = 0.06 | |
| Nontechnical job | 1.93 | 4, 0.037 | 2.13 (0.98–4.67) |
| Nontechnical vs. technical job | (1.03–3.62) | p = 0.086 | |
| Nonmanagerial job | 1.60 | 3, 0.071 | 1.43 (0.80–2.52) |
| Nonmanagerial vs. managerial job | (0.95–2.67) | p = 0.244 | |
Risk-adjusted by angiographic CAD extent, cardiac symptoms, cardiac risk factors (smoking, age, hypertension, hyperlipidemia, and diabetes), and body mass index.
GED, General Educational Development Diploma; HMO, health maintenance organization; PPO, preferred provider organization.
Post-high school, vocational training, classes toward or completion of an associate's or baccalaureate degree or higher.
Public insurance, Medicare, Medicaid, or Civilian Health and Medical Program of the Uniformed Services (CHAMPUS).
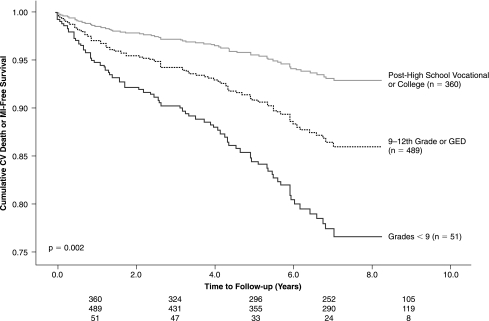
Cardiovascular event-free survival at 5 years was 99%, 97%, 87%, and 82%, respectively, for household income levels of ≥$100,000, $50,000–$99,999, $20,000–$49,999, and <$20,000 (Fig. 2) (p = 0.001). For women with varying educational backgrounds, those at greatest risk included women who did not enter high school, with 77% cardiovascular event-free survival at 5 years (Fig. 3) (p = 0.002). Women with some post-high school education, including college coursework or vocational training, had a 5-year cardiovascular event-free survival of 94%. Higher cardiovascular event-free survival was reported for women working fulltime compared with those unemployed or working part-time (98% vs. 90%, p < 0.0001).
FIG. 3.
Survival free from cardiovascular (CV) death or nonfatal myocardial infarction (MI) by education, including women attending school prior to high school, those having some high school education, and those having some post-high school training, respectively. GED, General Educational Development diploma.
Risk-adjusted prognostic models
In a multivariable model evaluating socioeconomic factors, income (p = 0.001) and education (p = 0.012) were the greatest predictors of cardiovascular death or MI. The relative risk ratio was 4.91-fold higher for women with an annual household income of <$20,000 compared with those in the higher income strata (Table 3) (p < 0.0001). Moreover, the relative risk ratio for women without any post-high school training or education was elevated 3.51-fold as compared with women with at least some education or training beyond high school (Table 3)(p = 0.002).
When controlling for angiographic coronary disease, symptoms, BMI, and risk factors, however, income (p = 0.006) remained a significant predictor of cardiovascular death or MI. As expected, angiographic coronary disease extent was the single greatest predictor of prognosis in a multivariable Cox model that included BMI, symptoms, and cardiac risk factors (p < 0.0001). Income (p = 0.001), however, was the second greatest estimator of cardiovascular death or MI.
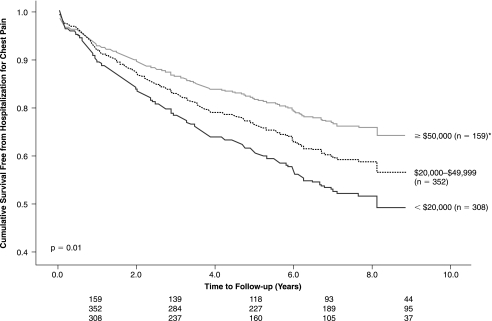
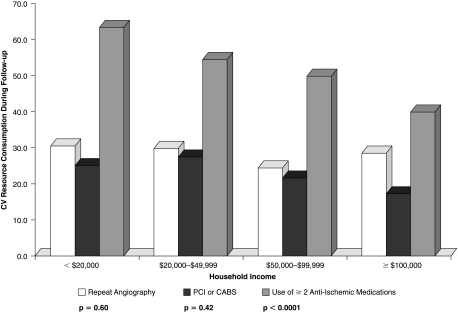
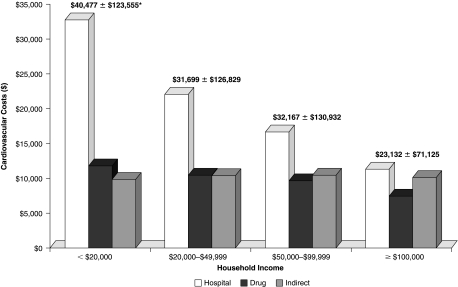
Risk-adjusted cardiovascular costs and resource consumption patterns by household income
Nearly half of women earning <$20,000 were hospitalized for worsening or refractory chest pain symptoms compared with 30%–40% of higher-income women (Fig. 4) (p = 0.01). Despite this, follow-up angiography (p = 0.60) or coronary revascularization (p = 0.42) rates were similar by income (Fig. 5). Because of their greater angina burden, nearly 70% of low-income women required two or more anti-ischemic medications for chest pain symptoms during follow-up compared with only half of higher-income women (p = 0.002). In fact, 18% of low-income women required the use of two or more anti-ischemic medications for 4 of the 5 years of follow-up.
FIG. 4.
Survival free from hospitalization for worsening chest pain symptoms by household income. (Lines for≥$100,000 were superimposed over $50,000–$99,999 lines and were thus merged for this analysis.)
FIG. 5.
Use of cardiac procedures during follow-up, including repeat coronary angiography and coronary revascularization procedures [percutaneous coronary intervention (PCI) or coronary artery bypass surgery (CABS)] and recorded use of two or more anti-ischemic medications during follow-up. CV, cardiovascular.
The result being higher 5-year risk-adjusted costs for low- income women (Fig. 6) (p < 0.0001). For women from low- income households, total 5-year cardiovascular costs exceeded $40,000, with $9,775 being indirect of out-of-pocket costs. This may be compared with 5-year total costs of $23,132 and indirect costs of $10,107 for women with an annual household income of ≥$100,000. Concurrent with the reported greater frequency of medication use, only 17% of women with incomes <$20,000 had prescription drug coverage; this rate increased to nearly half having drug coverage for those earning ≥$20,000 per year (p < 0.0001). Indirect costs were similar across household incomes, averaging $1,827 per year, but represented 18%, 6%, 2%, and 2% of total household incomes for women earning <$20,000, $20,000–$49,999, $50,000–$99,999, and ≥$100,000, respectively (p < 0.0001).
FIG. 6.
Five-year hospital (p < 0.0001) and drug (p < 0.0001) costs by annual household income. Also included are 5-year indirect costs, which were similar across household incomes (p = 0.76). All cost estimates were adjusted for the DASI estimate of MET capacity as a surrogate for disability. Further risk adjustment using age and angiographic coronary disease did not change these results.
Discussion
Women comprise a disproportionate share of those having limited financial means. Our results reveal an intertwining of socioeconomic factors with key subsets at particularly high risk for worsening cardiovascular prognosis, including non-Caucasian, unmarried women with limited education. Of all the socioeconomic factors, however, income was the most prominent and independently contributed to worsening cardiovascular event-free survival. Those at highest risk included women with an annual household income <$20,000, with a 5-year cardiovascular event-free survival rate of 82% compared with 97%–99% survival rates for women earning ≥$50,000 per year. The resulting relative risk ratio was elevated nearly 5-fold for low-income women compared with those with an annual household income of ≥$50,000 (p < 0.0001). Although there are limited data for women, these results are consistent with prior findings noting socioeconomic factors as contributory to greater coronary heart disease risk.20–24
Activities of daily living in low-income women
The current study also examined quality of life in addition to the prognostic findings. From this WISE cohort, more than half of low-income women perceived their health status as fair/poor compared with only 1 in 10 women from higher-income households. Moreover, low-income women reported greater functional disability compared with women from higher-income households. From the yearly DASI questionnaire, low-income women reported their average estimated METs capacity was 4.1 after 1 year of follow-up. Approximately 4–5 METs of physical work capacity is required to perform routine household chores; thus, low-income women were largely incapable of minimal activities of daily living.15 Further deterioration in MET capacity was reported through 5 years of follow-up such that low-income women, on average, were able to perform only 3.3 METs of physical work, whereas women from higher-income households reported functional capabilities in the range of 7–8 METs. The DASI is a simple, 12-item questionnaire by which estimation of METs can provide information on physical work capacity, and the score correlates very well with long-term outcomes in women.15 Thus, the DASI may provide a means to document a patient's limitations in performing routine activities of daily living, with a DASI-estimated METs of ≤4.7 indicating high risk.
Cardiovascular resource consumption and costs in women from low-income households
Low-income women consumed more healthcare resources and had higher cardiovascular healthcare costs during follow-up. This would be expected, given the higher risk status, greater risk factor burden, and more prevalent coronary disease in the women from low-income households. Importantly, cost differences between women of low and high household incomes cause a selection bias. That is, women from low-income households with more angina symptoms and more coronary disease would be expected to have higher costs of care. That being said, the presentation of cost data is meant to define the tremendous financial burden of healthcare for our low-income women.
Prior results have shown that a lack of available financial resources for lower-income patients limits regular healthcare access, causing underuse of preventive services and therapeutic interventions and contributing to worsening outcome.25,26 Within WISE, low-income women with a greater angina burden required more anti-ischemic therapies yet frequently had inadequate health insurance coverage. In fact, out-of-pocket expenses for healthcare encumbered 18% of household incomes for those earning <$20,000 compared with only 2% of higher-income households. The current results are similar to national results noting that nearly 1 in 5 families spend >10% of their annual incomes on healthcare.27 Those at highest risk of incurring hefty healthcare expenses include low-income individuals with chronic medical conditions, similar to our women with angina.
It is likely that a lack of prescription drug coverage had an undocumented influence on medication adherence and refilling.28 This financial burden for low-income women could be even greater with the inclusion of unfilled prescriptions, although this information was unavailable within WISE. Additionally, low-income women reported more sick days and diminished work productivity that further compromise their take-home salary and perhaps led to higher rates of job strain. Prior reports have noted that job strain accelerates coronary disease risk.29
Medical management was often ineffective for low-income women, with nearly half requiring hospitalization for refractory or worsening angina; this suggests unmet healthcare needs. Although there appeared to be more intensive use of anti-ischemic therapies by low-income women, the greater burden of angina and higher risk status suggest an underutilization of invasive, secondary prevention measures. That is, the similar utilization rates for repeat angiography and follow-up coronary revascularization could, in fact, be an underuse of services for the higher-risk, more symptomatic women of low-income households. Several prior reports have documented lower utilization rates for coronary revascularization in lower-income patients.30–35 Consistent with the current data, the literature supports the hypothesis that unmet health needs of low-income patients contributes to worsening prognosis.25–28,30,31,36–41
Study limitations
Poverty status data could not be calculated because of lack of information on regional home location and the number of adult and children living within each household.35,42 Although urban and rural housing data were not available on a patient level basis, the vast majority of patients in the lowest income bracket (i.e., 72%) were enrolled from two centers (Gainesville, Florida, and Birmingham, Alabama, p < 0.0001), perhaps residing in a more rural environment than were other study participants. Although urban vs. rural living data were unavailable, the inclusion of the enrolling center as a marker for regional variation did not change the current results. A significant limitation to this study is the lack of detail about differences in treatment, including the intensity of anti-ischemic therapy use across the participating centers. Across-center differences in patient management and the use of varying physician specialty or generalist care may be confounding the current results. This latter factor may be operational and cause an incorrect assessment of the impact of income and other socioeconomic factors. Specific information on provider training and experience was not available and could have influenced the results. We cannot exclude the possibility that a type I error occurred resulting from the extensive modeling performed within this analysis, although the significance level of income was small, suggesting that the false positive rate for our primary comparisons may be minimal. Finally, as the WISE study is an observational cohort design, no specific causal pathway may be identified within our available socioeconomic, clinical, or quality of life data.
Conclusions
Although prior reports have delineated the health effects of socioeconomic disadvantage,1–4 limited evidence is available about women.7,9 Our data suggest that among a variety of socioeconomic factors, income is the strongest estimator of cardiovascular morbidity and mortality. This evidence indicates that both affordability and accessibility may be operationally limiting our subset of low-income women.
The current results also reveal the complex interrelationship between poverty and poor health. Women from low-income households were not only at heightened risk of cardiovascular events but also required more intensive cardiac resources for management of their symptoms. Higher rates of hospitalization for worsening chest pain along with greater anti-ischemic therapy use revealed their worsening symptom burden, including a greater reliance on medical management. However, similar use patterns for outpatient visits and cardiac procedures coupled with their worsening prognosis signify unmet healthcare needs. For women from low-income households, limited financial means should also be framed within the context of deficiencies in healthcare coverage. Few of our low-income women had group health insurance coverage, and these were patients identified as incurring heavy healthcare expenditures.29 Improved health insurance coverage for women from low-income households has the potential to shift care from out-of-pocket expenses to that covered by group policies. This may reduce global cardiovascular costs by more effective management of low-income women. Thus, redistributive policies targeted toward breaking the cycle of excessive healthcare costs with policies of effective disease management for low-income women should be evaluated. Implications from these results should be a greater targeting of low-income women within the healthcare system and better tracking of drug compliance and prescription filling. Serial evaluation of their symptoms and functional capacities may serve to focus primary care physicians on the women's at-risk status. These results are generalizable to a large cohort of female patients where nearly half of middle-aged to elderly women comprise this lower-income stratum.
Footnotes
This work was supported by contracts from the National Heart, Lung and Blood Institutes, Nos. N01-HV-68161, N01-HV-68162, N01-HV-68163, and N01-HV-68164, grants U0164829, U01 HL649141, and U01 HL649241, a GCRC grant MO1-RR00425 from the National Center for Research Resources, and grants from the Gustavus and Louis Pfeiffer Research Foundation, Denville, New Jersey, The Women's Guild of Cedars-Sinai Medical Center, Los Angeles, California, The Ladies Hospital Aid Society of Western Pennsylvania, Pittsburgh, Pennsylvania, and QMED, Inc., Laurence Harbor, New Jersey.
Disclosure Statement
No competing financial interests exist.
References
- 1.Marmot MG. Shipley MJ. Rose G. Inequalities in death-specific explanations of a general pattern. Lancet. 1984;1:1003–1006. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- 2.Steenland K. Henley J. Calle E. Thun M. Individual- and area-level socioeconomic status variables as predictors of mortality in a cohort of 179,383 persons. Am J Epidemiol. 2004;159:1047–1056. doi: 10.1093/aje/kwh129. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan GA. Keil JE. Socioeconomic factors and cardiovascular disease: A review of the literature. Circulation. 1995;88:1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 4.Feinstein JS. The relationship between socioeconomic status and health: A review of the literature. Milbank Q. 1993;71:279–322. [PubMed] [Google Scholar]
- 5.Syme SL. Berkman LF. Social class, susceptibility and sickness. Am J Epidemiol. 1976;104:1–8. doi: 10.1093/oxfordjournals.aje.a112268. [DOI] [PubMed] [Google Scholar]
- 6.Armstrong DL. Strogatz D. Wang R. United States coronary mortality trends and community services associated with occupational structure, among blacks and whites, 1984–1998. Soc Sci Med. 2004;58:2349–2361. doi: 10.1016/j.socscimed.2003.08.030. [DOI] [PubMed] [Google Scholar]
- 7.Lawlor DA. Davey Smith G. Patel R. Ebrahim S. Life-course socioeconomic position, area deprivation, and coronary heart disease: Findings from the British Women's Heart and Health Study. Am J Public Health. 2005;95:91–97. doi: 10.2105/AJPH.2003.035592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LaCroix AZ. Psychosocial factors and risk of coronary heart disease in women: An epidemiologic perspective. Fertil Steril. 1994;62:133S–139S. [PubMed] [Google Scholar]
- 9.Blom M. Janszky I. Balog P. Orth-Gomer K. Wamala SP. Social relations in women with coronary heart disease: The effects of work and marital stress. J Cardiovasc Risk. 2003;10:201–206. doi: 10.1097/01.hjr.0000065926.57001.e0. [DOI] [PubMed] [Google Scholar]
- 10.Davey Smith G. Patel R. Ebrahim S. Life-course socioeconomic position, area deprivation, and coronary heart disease: Findings from the British Women's Heart and Health Study. Am J Public Health. 2005;95:91–97. doi: 10.2105/AJPH.2003.035592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andersson P. Leppert J. Men of low socio-economic and educational level possess pronounced deficient knowledge about the risk factors related to coronary heart disease. J Cardiovasc Risk. 2001;8:371–377. doi: 10.1177/174182670100800606. [DOI] [PubMed] [Google Scholar]
- 12.Vogels EA. Lagro-Janssen AL. van Weel C. Sex differences in cardiovascular disease: Are women with low socioeconomic status at high risk? Br J Gen Pract. 1999;49:963–966. [PMC free article] [PubMed] [Google Scholar]
- 13.Bairey Merz CN. Kelsey SF. Pepine CJ, et al. The women's ischemia syndrome evaluation (WISE) study: Protocol design, methodology and feasibility report. J Am Coll Cardiol. 1999;33:1453–1461. doi: 10.1016/s0735-1097(99)00082-0. [DOI] [PubMed] [Google Scholar]
- 14.Bairey Merz N. Bonow RO. Sopko G, et al. Women's ischemic syndrome evaluation: Current status and future research directions. A report of the National Heart, Lung and Blood Institute Workshop, October 2–4, 2002, Executive Summary. Circulation. 2004;109:805–807. doi: 10.1161/01.CIR.0000116205.96440.FE. [DOI] [PubMed] [Google Scholar]
- 15.Shaw LJ. Olson MB. Kip K, et al. The value of estimated functional capacity in estimating outcome: Results from the NHLBI-sponsored women's ischemia syndrome evaluation. J Am Coll Cardiol. 2006;47:S36–S43. doi: 10.1016/j.jacc.2005.03.080. [DOI] [PubMed] [Google Scholar]
- 16.Bairey Merz CN. Olson M. McGorray S, et al. Physical activity and functional capacity measurement in women. J Womens Health Gend Based Med. 2000;9:769–777. doi: 10.1089/15246090050147745. [DOI] [PubMed] [Google Scholar]
- 17.Rutledge T. Reis SE. Olson M, et al. Psychosocial variables are associated with atherosclerosis risk factors among women with chest pain: The WISE study. Psychosom Med. 2001;63:282–288. doi: 10.1097/00006842-200103000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Sharaf BL. Pepine CJ. Kerensky RA, et al. Detailed angiographic analysis of women with suspected ischemic chest pain (pilot phase data from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation [WISE] Study Angiographic Core Laboratory) Am J Cardiol. 2001;87:937–941. doi: 10.1016/s0002-9149(01)01424-2. [DOI] [PubMed] [Google Scholar]
- 19.Shaw LJ. Bairey Merz CN. Pepine CJ, et al. for the WISE Investigators. The economic burden of angina in women with suspected ischemic heart disease. Circulation. 2006;114:894–904. doi: 10.1161/CIRCULATIONAHA.105.609990. [DOI] [PubMed] [Google Scholar]
- 20.Williams RB. Barefoot JC. Califf RM, et al. Prognostic importance of social and economic resources among medically treated patients with angiographically documented coronary artery disease. JAMA. 1992;267:520–524. [PubMed] [Google Scholar]
- 21.Diez Roux AV. Detrano R. Jackson S, et al. Acculturation and socioeconomic position as predictors of coronary calcification in a multiethnic sample. Circulation. 2005;112:1557–1565. doi: 10.1161/CIRCULATIONAHA.104.530147. [DOI] [PubMed] [Google Scholar]
- 22.Lawlor DA. Ebrahim S. Davey Smith G. Adverse socioeconomic position across the lifecourse increase coronary heart disease risk cumulatively: Findings from the British women's heart and health study. J Epidemiol Community Health. 2005;59:785–793. doi: 10.1136/jech.2004.029991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lynch J. Kaplan GA. Salonen R. Cohen RD. Salonen JT. Socioeconomic status and carotid atherosclerosis. Circulation. 1995;92:1786–1792. doi: 10.1161/01.cir.92.7.1786. [DOI] [PubMed] [Google Scholar]
- 24.Rose G. Marmot MG. Social class and coronary heart disease. Br Heart J. 1981;45:13–19. doi: 10.1136/hrt.45.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Adler NE. Newman K. Socioeconomic disparities in health: Pathways and policies. Health Affairs. 2002;21:60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- 26.Marmot M. Shipley M. Brunner E. Hemingway H. Relative contribution of early life and adult socioeconomic status to adult morbidity in the Whitehall II study. J Epidemiol Community Health. 2001;55:301–307. doi: 10.1136/jech.55.5.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Banthin JS. Bernard DM. Changes in financial burdens for health care. JAMA. 2006;296:2712–2719. doi: 10.1001/jama.296.22.2712. [DOI] [PubMed] [Google Scholar]
- 28.Stroupe KT. Teal EY. Tu W. Weiner M. Murray MD. Association of refill adherence and health care use among adults with hypertension in an urban health care system. Pharmacotherapy. 2006;26:779–789. doi: 10.1592/phco.26.6.779. [DOI] [PubMed] [Google Scholar]
- 29.Hintsanen M. Kivimaki M. Elovainio M, et al. Job strain and early atherosclerosis. Psychosom Med. 2005;67:740–747. doi: 10.1097/01.psy.0000181271.04169.93. [DOI] [PubMed] [Google Scholar]
- 30.Feder G. Crook AM. Magee P. Banerjee S. Timmis AD. Hemingway H. Ethnic differences in invasive management of coronary disease: Prospective cohort study of patients undergoing coronary angiography. BMJ. 2002;324:511–516. doi: 10.1136/bmj.324.7336.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ford ES. Cooper RS. Racial/ethnic differences in health care utilization of cardiovascular procedures: A review of the evidence. Health Serv Res. 1995;30:237–252. [PMC free article] [PubMed] [Google Scholar]
- 32.Wenneker MB. Epstein AM. Racial inequities in the use of procedures for patients with ischemic heart disease in Massachusetts. JAMA. 1989;261:253–257. [PubMed] [Google Scholar]
- 33.Hannon EL. Kilburn H. O'Donnell JF, et al. Interracial access to selected cardiac procedures for patients hospitalized with coronary artery disease in New York State. Med Care. 1991;29:430–441. doi: 10.1097/00005650-199105000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Goldberg KC. Hartz AJ. Jacobsen SJ, et al. Racial and community factors influencing coronary artery bypass graft surgery rates for all Medicare patients. JAMA. 1992;267:1473–1477. [PubMed] [Google Scholar]
- 35.Ayanian AZ. Udvarhelyi IS. Gatsonis CA, et al. Racial differences in the use of revascularization procedures after coronary angioplasty. JAMA. 1993;269:2642–2646. [PubMed] [Google Scholar]
- 36.Angell M. Privilege and health: What's the connection? N Engl J Med. 1993;329:126–127. doi: 10.1056/NEJM199307083290210. [DOI] [PubMed] [Google Scholar]
- 37.www.cdc.gov/nchs/data/hus/hus98.pdf. [Jun 25;2005 ]. www.cdc.gov/nchs/data/hus/hus98.pdf
- 38.Adler NE. Boyce T. Chesney MA. Folkman S. Syme SL. Socioeconomic inequalities in health: No easy solution. JAMA. 1993;269:3140–3145. [PubMed] [Google Scholar]
- 39.www.ssa.gov/policy/docs/statcomps/income_pop55/2002/sect3.html#table3.1. [Jun 25;2005 ]. www.ssa.gov/policy/docs/statcomps/income_pop55/2002/sect3.html#table3.1
- 40.Backlund E. Sorlie PD. Johnson NJ. A comparison of the relationships of education and income with mortality. Soc Sci Med. 1999;49:1373–1384. doi: 10.1016/s0277-9536(99)00209-9. [DOI] [PubMed] [Google Scholar]
- 41.Reid FDA. Cook DG. Whincup PH. Use of statins in the secondary prevention of coronary heart disease: Is treatment equitable? Heart. 2002;88:15–19. doi: 10.1136/heart.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.www.census.gov/hhes/poverty/threshld/thresh03.html. [Jun 26;2005 ]. www.census.gov/hhes/poverty/threshld/thresh03.html