Abstract
Background and Purpose
Psychosocial stress has been widely studied as a risk factor for stroke and coronary heart disease (CHD) but little is known about the differential effects of stress on stroke and CHD risk by race and sex. Caregiving for a disabled spouse has been associated with increased mortality and CHD risk, but the association of caregiving strain with stroke and CHD risk across race and sex is unknown.
Methods
Participants in the REasons for Geographic and Racial Differences in Stroke (REGARDS) study who were providing in-home caregiving to a disabled spouse reported on caregiving strain (high, some, or none), depressive symptoms, social network, education, and age. Caregiving strain groups were compared on the Framingham Stroke Risk Score (N=716) and Framingham CHD Risk Score (N=607), which estimate the projected 10-year risk of incident stroke and ischemic heart disease, respectively.
Results
High caregiving strain was associated with a 23% higher covariate-adjusted estimated stroke risk (11.06% for caregivers with no strain versus 13.62% risk for high strain caregivers). This association was stronger in men, particularly African American men with high caregiving strain (26.95% estimated 10 year stroke risk). Caregiving strain was not associated with CHD risk scores.
Conclusions
Caregiving strain is significantly associated with higher estimated stroke risk, with greatest effects for men, particularly African American men, providing caregiving to their wives. Male spouse caregivers may need special caregiving support. Prospective longitudinal studies should examine how sex and race may moderate the impact of stress on stroke and CHD risk.
Keywords: Psych & Behavior, Risk Factors, Women & Minorities, Stress, Family caregiving, Stroke risk, Epidemiological studies, Caregiving stress
Psychosocial stress has been widely studied as a risk factor for cardiovascular disorders, including CHD and stroke. A review of the relationship between psychosocial stress and cardiovascular disease1 concluded that a top priority for future research should be examining whether psychosocial stress is a differential risk factor by race. This is particularly important given the widely documented racial differences in both CHD and stroke2, and indications that psychosocial stress may be particularly important risk factor for African Americans1.
Among the psychosocial risk factors that have been studied to date, one important factor is family caregiving stress. This is a common stressor, with about 12% of Americans over age 45 reporting family caregiving responsibilities3. High caregiving stress has been associated with poor physical and psychological health in a large number of studies3–5 and with increased mortality among spouse caregivers in one study6.
We have identified two studies examining the relationship between family caregiving stress and risk for CHD, but no such studies focusing on risk for stroke. Both projects utilized data from the Nurses Health Study. One found increased risk of CHD onset or death among spouse caregivers7. Another study found increased risk of CHD onset or death among caregivers of grandchildren and children8. Neither study examined race as a predictor variable, and sex could not be examined because the Nurses Health Study focused only on women.
Besides caregiving stress, several other psychosocial risk and protective factors have been studied as risk factors for CHD and stroke. Depressive symptoms, lack of social support, and low socioeconomic status have been widely shown to predict risk of CHD1,9–11. However there are fewer studies of these risk factors in stroke12–14, and some critics have suggested the increased risk of stroke related to socioeconomic factors may be explained by traditional risk factors15.
One reason that it has been difficult to study the differential impact of stress by race is that there have been few large, racially diverse samples on which there are measures of psychosocial stress and risk for stroke and CHD. The REasons for Geographic and Racial Differences in Stroke (REGARDS) study is an ongoing epidemiologic study of stroke and CHD incidence and mortality using a large national sample of African American and White adults over 45 years of age. The REGARDS baseline telephone interview included key questions about caregiving responsibilities and caregiving strain, as well as important factors that should be examined as covariates. Thus, we have the capacity to identify caregivers, including the subgroup of caregivers who report high strain, and to compare these variables to stroke and CHD risk scores.
In this paper, we examine the relationship of caregiving strain to well-validated indices of stroke and CHD risk. We focused on a highly stressed subgroup of caregivers, those caring for and co-residing with spouses, since previous research has documented that this is a very high risk caregiving group6,7. In addition, we examined the role of depressive symptoms, social network, education, and age which are also potential predictors of risk. While women have been found to show more psychological distress with caregiving than men16, and African Americans sometimes report less psychological distress than Whites17, there are few studies examining differential impact of sex and race on the impact of stress on physical health indicators.
Materials and Methods
Participants
Potential participants for the REGARDS study were randomly selected from a commercially available nationwide list, using a stratified random sampling design. Approximately half of the sample was obtained from "stroke belt" region (the states of AL, AR, GA, LA, MS, NC, SC, and TN) and the remaining half from other areas throughout the 48 contiguous states, with an effort to include about half African American and half White, as well as half male and half female. After mail contact, a subsequent telephone contact was attempted. Respondents were briefly screened for eligibility and then invited to participate. Exclusion criteria included age less than 45, self-identified race other than African American or White, previous diagnosis of cancer requiring chemotherapy, inability to communicate in English, or residence in or on a waiting list for a nursing home. Anyone not excluded by these criteria was eligible for enrollment. The cooperation rate (the proportion of known eligible participants who agreed to be interviewed) was over 60%18. The sampling, recruitment, and telephone interviewing procedures for REGARDS have been described in more detail elsewhere18.
Enrollment began in January of 2003 and ended in October of 2007. A total of 30,239 participants completed the initial telephone interview and home visit and provided valid race, sex, and age data. Of these, 30,186 (99.9%) answered the interview questions about caregiving status and, if relevant, caregiving strain (see below). A subgroup of 837 individuals was identified who were spouse caregivers and who co-resided with their spouse, the group of interest here, which is at highest risk for negative health outcomes due to caregiving6. In addition, for the analyses focusing on stroke risk, participants with a previous history of stroke were excluded, and for the analyses focusing on risk for CHD risk individuals with a history of CHD were excluded, consistent with the requirements for these two risk scores. A total of 70 spouse caregivers had a history of both stroke and CHD, resulting in 767 total participants for these analyses. This included 716 spouse caregivers for the analysis of stroke risk scores, and 607 spouse caregivers for the analysis of CHD risk scores.
Procedures
Trained interviewers contacted potential participants and established eligibility for participation, and obtained verbal informed consent. A computer-assisted telephone interview was then administered that obtained information on demographic variables, medical history, depressive symptoms, and caregiving. Education was included as a measure of socioeconomic status and was coded into four ordinal categories (less than high school graduate, high school graduate, some college, college graduate or more).
After completing the telephone interview, a home visit was arranged to obtain physical measures such as blood pressure, to gather blood and urine samples, and to perform electrocardiograms (ECGs). The procedures used to collect these measures are described in greater detail elsewhere19.
Instruments
Depressive Symptoms
The 4-item short form of the Center for Epidemiological Studies-Depression scale (CESD-4) was used to assess depressive symptoms20. Participants indicated how many days during the past week they felt depressed, lonely, sad, or had crying spells. Response options included less than 1 day, 1–2 days, 3–4 days, or 5 or more days. Total scores ranged from 0 to 12, with a score of 4 or more suggestive of significant psychological distress. The reliability and validity of the CESD-4 have been shown to be sufficient in comparison with the full 20-item CESD20.
Social Network
A single item indicator, a report of how many friends and relatives that the participant sees at least once per month, was used to indicate size of the social network.
Stroke Risk
The Framingham Stroke Risk Score (FSRS) was developed to predict 10-year risk of stroke based on data from the Framingham study21,22. The profile uses the following variables: age, systolic blood pressure (SBP), antihypertensive medication, current cigarette smoking, diabetes, history of cardiovascular disease, atrial fibrillation, and left ventricular hypertrophy (LVH) as indicated by a 7-lead ECG for the first 25% of the participants and a 12-lead ECG for the remaining 75% of the participants.
CHD Risk
The Framingham CHD Risk Score was developed to predict 10-year risk of onset of CHD or CHD death based on data from the Framingham study23. The score uses the following variables: age, total cholesterol, HDL cholesterol, SBP, diabetes, and current cigarette smoking.
Caregiving Variables
Each participant was asked: "Are you currently providing care on an on-going basis to a family member with a chronic illness or disability? This would include any kind of help such as watching your family member, dressing or bathing this person, arranging care, or providing transportation." Respondents who answered affirmatively to this question were categorized as “caregivers” and subsequently asked 1) how they were related to their care recipient, 2) whether they lived in the same residence with the care recipient, and 3) how much of a mental or emotional strain it was on them to provide this care. Response options for the caregiving strain question were the same as those used by Schulz and Beach6 and included "no strain," "some strain," or "a lot of strain."
Statistical analyses
Multiple regression analyses were conducted using SAS PROC Reg and SAS PROC GLM to identify the unique predictors of Framingham stroke risk and CHD risk scores. The independent or predictor variables were age, sex, race, education, depressive symptoms, social network, and caregiving strain. Age was centered by subtracting out the mean age of 68 years for these 767 spouse caregivers. In our multiple regression models, we first estimated models with these main effects and then added interaction effects for sex*race, sex*caregiving strain, race*caregiving strain, and sex*race*caregiving strain to determine if any caregiving strain main effects were differentially moderated by sex or race subgroups.
Results
Table 1 summarizes the descriptive information for the 767 participants included in our analyses, including 716 for whom stroke risk scores could be calculated and 607 participants for whom CHD risk scores could be calculated. Men were older, had lower depression scores, and were less likely to report high caregiving strain than women but there were no significant race difference on these items. African Americans also had lower educational attainment than Whites, an effect that was stronger for men than women. Because of race and sex differences on many of the variables in Table 1 and previous research suggesting associations between these factors and stroke and CHD risk, these variables were used as covariates in our analyses.
Table 1.
Descriptive Information for Caregivers by Race and Sex
| White Females (N = 257) |
White Males (N = 225) |
African American Females (N = 165) |
African American Males (N = 120) |
Total Sample (N = 767) |
|
|---|---|---|---|---|---|
| Age | |||||
| M | 66.65 | 70.21 | 65.79 | 69.35 | 67.93 |
| SD | 8.88 | 9.25 | 8.25 | 9.96 | 9.21 |
| Education | |||||
| Less than HS | 29 (11%) | 17 (8%) | 28 (17%) | 32 (27%) | 106 (14%) |
| HS | 78 (30%) | 53 (23%) | 48 (29%) | 30 (25%) | 209 (27%) |
| Some college | 71 (28%) | 60 (27%) | 49 (30%) | 25 (21%) | 205 (27%) |
| College graduate | 79 (31%) | 95 (42%) | 40 (24%) | 33 (27%) | 247 (32%) |
| Social Network | |||||
| M | 7.71 | 6.87 | 6.91 | 7.16 | 7.20 |
| SD | 7.67 | 7.41 | 7.60 | 7.89 | 7.61 |
| CESD-4 | |||||
| M | 1.69 | 1.00 | 1.47 | 1.37 | 1.39 |
| SD | 2.57 | 1.89 | 2.37 | 2.44 | 2.33 |
| Caregiver Strain | |||||
| None | 59 (23%) | 88 (39%) | 46 (28%) | 54 (45%) | 246 (32%) |
| Medium | 139 (54%) | 105 (47%) | 85 (51%) | 51 (43%) | 380 (50%) |
| High | 59 (23%) | 32 (14%) | 34 (21%) | 15 (12%) | 141 (18%) |
| Framingham Stroke Risk Score (N = 716) |
|||||
| M | 8.90 | 12.85 | 9.55 | 17.14 | 11.46 |
| SD | 9.51 | 10.32 | 9.39 | 14.96 | 11.08 |
| Framingham CHD Risk Score (N = 607) |
|||||
| M | 6.91 | 15.84 | 7.13 | 17.72 | 10.85 |
| SD | 8.14 | 11.62 | 6.38 | 11.43 | 10.44 |
Note: HS=High School; CESD=Center for Epidemiological Studies Depression; CHD = Coronary Heart Disease.
Predictors of Stroke Risk Scores
Significant main effects for predicting stroke risk scores are summarized in Table 2. Higher stroke risk scores were associated with greater age, male sex, African American race, less education, greater depressive symptoms, and high caregiving strain. When we applied the regression results, the model-predicted stroke risk score (or covariate-adjusted stroke risk mean score) for the high strain caregivers was 13.62%, which represents a 23% increase over the 11.06% model-predicted stroke risk score for the no strain caregivers.
Table 2.
Regression Model Predicting Framingham Stroke Risk Scores in Spouse Caregivers
| Predictor | Estimate | SE | Std. estimate | P |
|---|---|---|---|---|
| Intercept | 14.55 | 1.28 | --- | <0.0001 |
| Age – 68 | 0.65 | 0.04 | 0.53 | <0.0001 |
| Sex (F = 1, M = 0) | −3.33 | 0.72 | −0.15 | <0.0001 |
| Race (AA = 1, W = 0) | 2.44 | 0.73 | 0.11 | 0.0009 |
| Education: < High School | --- | --- | --- | --- |
| High School | −2.69 | 1.18 | −0.11 | 0.02 |
| Some College | −3.56 | 1.19 | −0.14 | 0.003 |
| College Graduate | −4.53 | 1.17 | −0.19 | 0.0001 |
| Depressive Symptoms | 0.33 | 0.16 | 0.07 | 0.04 |
| Social Network | 0.03 | 0.05 | 0.02 | 0.50 |
| Caregiving Strain: None | --- | --- | --- | --- |
| Some | −0.12 | 0.80 | −0.01 | 0.88 |
| High | 2.56 | 1.09 | 0.09 | 0.02 |
Note: F=Female; M=Male; AA=African American; W=White
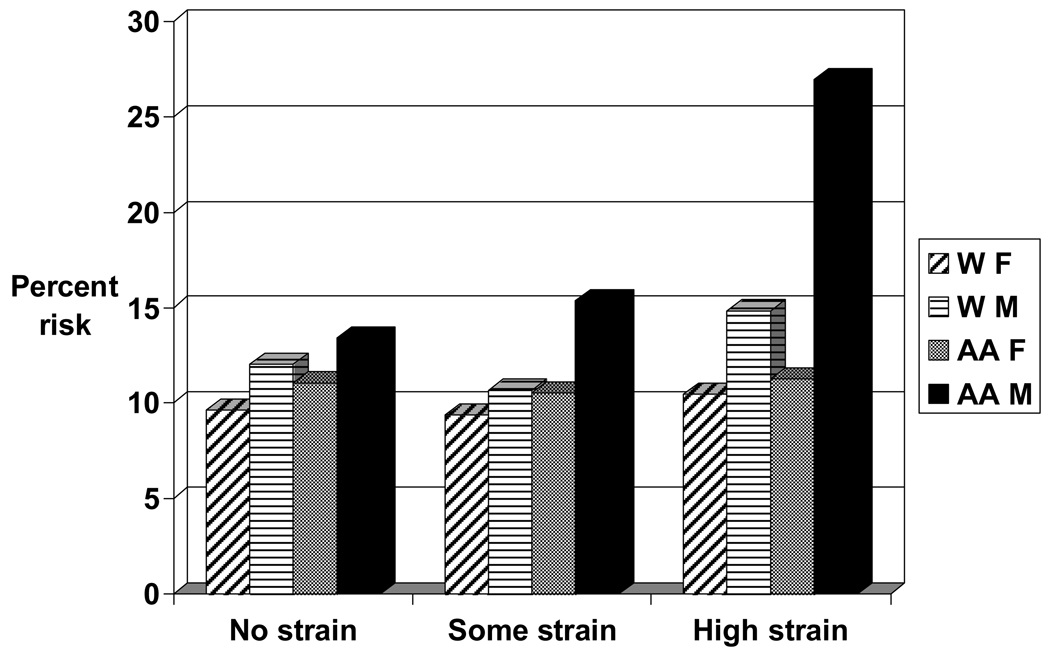
The subsequent model including interaction effects revealed two statistically significant 2-way interactions for sex*race [F(1, 677) = 8.77, p = .003], and for sex*caregiver strain [F(2, 677) = 6.38, p=.002]. Both of these 2-way interactions were embedded in a statistically significant 3-way interaction for sex*race*caregiving strain [F(2,677) = 3.17, p = .04]. The 3-way interaction and embedded 2-way interactions are illustrated in Figure 1, where it is evident that the high strain African American male caregivers had by far the highest covariate-adjusted stroke risk score of 26.95%. This adjusted stroke risk score was more than 10 points higher than that for any other race-sex group.
Figure 1.
10 year probability of stroke risk (FSRS) by race, sex, and caregiving strain, adjusted for depression, education, and age.
Note: W=White; AA=African American; F=Female; M=Male; FSRS=Framingham Stroke Risk Score
Predictors of CHD Risk Scores
Significant main effects from the multiple regression analysis predicting CHD risk scores are summarized in Table 3. Higher CHD risk scores were associated with greater age, male sex, and greater depressive symptoms. Race, number in the social network, and caregiving strain were not found to be related to CHD risk scores. A college education was associated with somewhat reduced CHD risk compared to participants with less than a high school education. The expanded model that included 2-way and 3-way interactions for caregiving strain indicated that none of the interaction effects were statistically significant.
Table 3.
Regression Model Predicting Framingham CHD Risk Scores in Spouse Caregivers
| Predictor | Estimate | SE | Std. estimate | P |
|---|---|---|---|---|
| Intercept | 18.00 | 1.35 | --- | <0.0001 |
| Age – 68 | 0.29 | 0.04 | 0.26 | <0.0001 |
| Sex (F = 1, M = 0) | −8.52 | 0.78 | −0.41 | <0.0001 |
| Race (AA = 1, W = 0) | 0.35 | 0.77 | 0.02 | 0.65 |
| Education: < High School | --- | --- | --- | --- |
| High School | −0.89 | 1.28 | −0.04 | 0.49 |
| Some College | −2.31 | 1.30 | −0.10 | 0.08 |
| College Graduate | −3.08 | 1.27 | −0.14 | 0.02 |
| Depressive Symptoms | 0.42 | 0.17 | 0.10 | 0.01 |
| Social Network | 0.00 | 0.05 | 0.00 | 0.97 |
| Caregiving Strain: None | --- | --- | --- | --- |
| Some | −1.08 | 0.85 | −0.05 | 0.20 |
| High | −1.21 | 1.18 | −0.05 | 0.30 |
Note: CHD=Coronary Heart Disease; F=Female; M=Male; AA=African American; W=White
Supplemental analyses
In order to better understand the significant relationship between caregiving strain and stroke risk scores, we examined the relationship between caregiving strain and each of the component variables that comprise the stroke risk score. We conducted univariate analyses of variance or chi-square tests to ascertain whether any of these components of the stroke risk score were significantly associated with caregiving strain. Of the eight components, only age was significantly associated with caregiving strain [F(2,713) = 4.46, p = .01], with high strain caregivers (M = 65.8 years) being significantly younger than moderate strain (M = 68.4 years) and no strain (M = 68.5 years) caregivers. Thus, by including age as a covariate in our multiple regression models and examining age-adjusted stroke risk scores, this allowed the caregiving strain relationship with estimated stroke risk scores to emerge as statistically significant.
We used education as our primary indicator of SES because it better reflects lifelong socioeconomic status than income among older, largely retired populations, and because there was more missing data on income than on education. Supplemental analyses using income as a covariate replicated the findings reported above.
Discussion
Our results show that, after adjusting for demographic covariates, highly strained spouse caregivers have significantly elevated stroke risk scores on the FSRS compared to spouse caregivers reporting no caregiving strain. This risk was highest for highly stressed caregiving husbands, with highly stressed African American caregiving husbands showing particularly elevated FSRS scores. High caregiving strain showed this significant association with the FSRS after controlling for demographic factors and other indicators of psychosocial stress, including significant associations between stroke risk and age, educational attainment, and depressive symptoms. Supplemental analyses examining the FSRS components individually found that highly stressed caregivers were significantly younger, on average, than less strained caregivers, but there were no caregiving strain differences on SBP, use of antihypertensive medication, diabetes, cigarette smoking status, history of cardiovascular disease, atrial fibrillation, or LVH.
There are a number of possible explanations for this pattern of findings. Highly stressful caregiving can be chronic, and include many difficult and uncontrollable stressors such as witnessing the suffering of a loved one, managing stressful behavior problems, financial strain, social isolation, and providing physically and psychologically demanding personal care tasks24. Caregiving and other psychosocial stressors can have significant effects on the cardiovascular system5,11, although we found no differences on the individual variables comprising the risk score in our supplemental analyses. Because younger spouse caregivers were significantly more likely to report high caregiving strain than older spouse caregivers, it appears that the health benefits of relative youth were eliminated by the counteracting health effects of increased caregiving strain. Caregiving strain can also interfere with other health behaviors such as exercising and getting proper rest5,11. It is not clear why these collective age-adjusted health effects of caregiving strain were observed on measures of stroke risk but not CHD risk. Given the cross-sectional nature of the present findings, it is possible that people high in some stroke risk factors may find caregiving to be more stressful, but then one might expect older caregivers to report more caregiving strain. Prospective research on caregiving strain, incident stroke, and incident coronary events will be critical for further addressing the relationships suggested by these cross-sectional associations.
Highly strained husbands, especially African American husbands, showed the highest estimated stroke risk. Caregiving is traditionally a female gender role, and although many men do take on caregiving responsibilities, role discrepant responsibilities can be increase strain. It is also of interest that, as a whole, husband caregivers were much less likely than wife caregivers to report that their caregiving roles were high strain. Male caregivers have been found to use more paid services, and have more assistance from extended families, than female caregivers16, which can serve to decrease caregiving strain. In our study, husbands as a whole were less likely to report high strain than wives. Perhaps the subgroup of husbands reporting high caregiving strain are lacking the paid and family assistance that many male caregivers receive when coping with highly stressful caregiving roles.
Our results also replicated some widely reported findings. Greater age, male sex, African American race, less education, and greater depressive symptoms were all associated with higher stroke risk scores. Greater age, male sex, and greater depressive symptoms were also associated with higher CHD risk scores. A strength of our study is that we examined caregiving strain even after accounting for the variance associated with these other factors, some of which (such as depression) are associated with caregiving strain.
Because our results examined stroke risk scores, they must be viewed with caution. Future research should study the association of caregiving strain with incident stroke and CHD, which we will eventually have the capacity to examine within REGARDS. When data are available on incident stroke and CHD it will be important to look at how factors such as caregiving strain may interact with depressive symptoms, social network, and other variables, since such interaction effects may be more powerful than main effects25. In addition, the group of highly strained African American males was relatively small, so the very high score in this subgroup should be viewed with caution. It is unclear why caregiving strain was not associated with CHD risk scores, although other demographic and psychosocial risk factors including age, education, and depressive symptoms were associated with CHD risk. There are some different variables included in the CHD and stroke risk scores. For example, the stroke risk score includes atrial fibrillation and LVH, while the CHD score includes total and HDL cholesterol.
Finally, high caregiving strain has already been shown to be a risk factor for depressive symptoms and early mortality3–6. Highly strained caregivers may benefit from effective caregiver intervention programs, which have been shown to be of similar effectiveness for husbands and wives experiencing highly stressful caregiving26.
Acknowledgments and Funding
The research reported in this paper was supported by investigator-initiated grants (R01 NS045789, David Roth, PI; and R01 HL080477, Monika Safford, PI) and by a cooperative agreement (U01 NS041588) from the National Institute of Neurological Disorders and Stroke (NINDS), National Institutes of Health, Department of Health and Human Services. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NINDS or the National Institutes of Health. Representatives of NINDS have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. The authors acknowledge the participating investigators and institutions of REGARDS for their valuable contributions: The University of Alabama at Birmingham, Birmingham, Alabama (Study PI, Statistical and Data Coordinating Center, Survey Research Unit): George Howard DrPH, Leslie McClure PhD, Virginia Howard PhD, Libby Wagner MA, Virginia Wadley PhD, Rodney Go PhD, Monika Safford MD, Ella Temple PhD, Margaret Stewart MSPH, J. David Rhodes BSN; University of Vermont (Central Laboratory): Mary Cushman MD; Wake Forest University (ECG Reading Center): Ron Prineas MD, PhD; Alabama Neurological Institute (Stroke Validation Center, Medical Monitoring): Camilo Gomez MD, Susana Bowling MD; University of Arkansas for Medical Sciences (Survey Methodology): LeaVonne Pulley PhD; University of Cincinnati (Clinical Neuroepidemiology): Brett Kissela MD, Dawn Kleindorfer MD; Examination Management Services, Incorporated (In-Person Visits): Andra Graham; Medical University of South Carolina (Migration Analysis Center): Daniel Lackland DrPH; Indiana University School of Medicine (Neuropsychology Center): Frederick Unverzagt PhD; National Institute of Neurological Disorders and Stroke, National Institutes of Health (funding agency): Claudia Moy PhD.
Footnotes
Conflicts of Interest: None
References
- 1.Everson-Rose SA, Lewis TT. Psychosocial factors and cardiovascular diseases. Annu Rev Public Health. 2005;26:469–500. doi: 10.1146/annurev.publhealth.26.021304.144542. [DOI] [PubMed] [Google Scholar]
- 2.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–e171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 3.Roth DL, Perkins M, Wadley VG, Temple E, Haley WE. Family caregiving and emotional strain: Associations with psychological health in a national sample of community-dwelling middle-aged and older adults. Qual Life Res. doi: 10.1007/s11136-009-9482-2. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: A meta-analysis. Psychol Aging. 2003;18:250–267. doi: 10.1037/0882-7974.18.2.250. [DOI] [PubMed] [Google Scholar]
- 5.Vitaliano PV, Scanlan JM, Zhang J. Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol Bull. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]
- 6.Schulz R, Beach S. Caregiving as a risk factor for mortality: The caregiver health effects study. JAMA. 1999;282:2215–2219. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 7.Lee S, Colditz GA, Berkman LF, Kawachi I. Caregiving and risk of coronary heart disease in U.S. women: a prospective study. Am J Prev Med. 2003;24:113–119. doi: 10.1016/s0749-3797(02)00582-2. [DOI] [PubMed] [Google Scholar]
- 8.Lee S, Colditz G, Berkman L, Kawachi I. Caregiving to children and grandchildren and risk of coronary heart disease in women. Am J Public Health. 2003;93:1939–1944. doi: 10.2105/ajph.93.11.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thurston RC, Kubzansky LD. Multiple sources of psychosocial disadvantage and risk of coronary heart disease. Psychosom Med. 2007;69:748–755. doi: 10.1097/PSY.0b013e31815772a3. [DOI] [PubMed] [Google Scholar]
- 10.Goldston K, Baillie AJ. Depression and coronary heart disease: A review of the epidemiological evidence, explanatory mechanisms and management approaches. Clin Psychol Rev. 2008;28:288–306. doi: 10.1016/j.cpr.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Rozanski A, Blumenthal JA, Davidson KW, Saab PG, Kubzansky L. The epidemiology, pathophysiology, and management of psychosocial risk factors in cardiac practice: The emerging field of behavioral cardiology. J Am Coll Cardiol. 2005;45:637–651. doi: 10.1016/j.jacc.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Liebetrau M, Steen B, Skook I. Depression as a risk factor for the incidence of first-ever stroke in 85-year-olds. Stroke. 2008;39:1960–1965. doi: 10.1161/STROKEAHA.107.490797. [DOI] [PubMed] [Google Scholar]
- 13.Salaycik KJ, Kelly-Hayes M, Beiser A, Nguyen AH, Brady SM, Kase CS, Wolf PA. Depressive symptoms and risk of stroke: The Framingham Study. Stroke. 2007;38:16–21. doi: 10.1161/01.STR.0000251695.39877.ca. [DOI] [PubMed] [Google Scholar]
- 14.Kuper H, Adamin HO, Theorell T, Weiderpass E. The socioeconomic gradient in the incidence of stroke: A prospective study in middle-aged women in Sweden. Stroke. 2007;38:27–33. doi: 10.1161/01.STR.0000251805.47370.91. [DOI] [PubMed] [Google Scholar]
- 15.Hankey GJ. Potential new risk factors for ischemic stroke: What is their potential? Stroke. 2006;37:2181–2188. doi: 10.1161/01.STR.0000229883.72010.e4. [DOI] [PubMed] [Google Scholar]
- 16.Pinquart M, Sörensen S. Gender differences in caregiver stressors, social resources, and health: an updated meta-analysis. J of Gerontol B Psychol Sci Soc Sci. 2006;61B:P33–P45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- 17.Dilworth-Anderson P, Williams IC, Gibson BE. Issues of race, ethnicity, and culture in caregiving research: A 20-year review (1980–2000) Gerontologist. 2002;42:237–272. doi: 10.1093/geront/42.2.237. [DOI] [PubMed] [Google Scholar]
- 18.Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The REasons for Geographic and Racial Differences in Stroke study: Objectives and design. Neuroepidemiology. 2005;25:135–143. doi: 10.1159/000086678. [DOI] [PubMed] [Google Scholar]
- 19.Cushman M, Cantrell RA, McClure LA, Howard G, Prineas RJ, Moy CS, Temple EM, Howard VJ. Estimated 10-year stroke risk by region and race in the United States. Ann Neurol. 2008;64:507–513. doi: 10.1002/ana.21493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Melchior LA, Huba GJ, Brown VB, Reback CJ. A short depression index for women. Educ Psychol Meas. 1993;53:1117–1125. [Google Scholar]
- 21.Wolf PA, D’Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22:312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 22.D’Agostino RB, Wolf PA, Belanger AJ, Kannel WB. Stroke risk profile: adjustment for antihypertensive medication: the Framingham study. Stroke. 1994;25:40–43. doi: 10.1161/01.str.25.1.40. [DOI] [PubMed] [Google Scholar]
- 23.Wilson PWF, D’Agostin RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 24.Schulz R, Hebert RS, Dew MA, Brown SL, Scheier MF, Beach SR, Czaja SJ, Martire LM, Coon D, Langa KM, Gitlin LN, Stevens AB, Nichols L. Patient suffering and caregiver compassion: new opportunities for research, practice, and policy. Gerontologist. 2007;47:4–13. doi: 10.1093/geront/47.1.4. [DOI] [PubMed] [Google Scholar]
- 25.Baune BT. The puzzle of predicting the impact of brain infarcts on cognitive impairment in the aging brain. Stroke. 2009;40:667–669. doi: 10.1161/STROKEAHA.108.534230. [DOI] [PubMed] [Google Scholar]
- 26.Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with Alzheimer’s disease. Neurology. 2006;67:1592–1599. doi: 10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]