Abstract
Objective
To explore the quality of life changes in methadone maintenance treatment (MMT) clinic outpatients in the first 3 months of treatment.
Methods
A cohort study was conducted in 5 MMT clinics over 3 months, and the Quality of Life (QOL) of outpatients was measured by the QOL instrument for drug addicts (QOL-DA) at days 1, 30, and 90 to explore quality of life changes. Repeated measurement analysis method was used for data analysis.
Results
172 outpatients in five MMT clinics were recruited, and 142 (82.65%) remained in treatment at day 90. The Cronbach α coefficient of the QOL instrument for drug addicts used in our study is 0.96, with a range of 0.74–0.94 for all subscales. The QOL scores of drug addicts improved from day 1 to day 30 (X̄beginning =51.92, X̄first month =74.83, P < 0.01), and all subscale scores improved significantly (P < 0.01). However, quality of life improved little from day 30 to day 90, (X̄ first month =74.83, X̄ third month =75.99, P < 0.01). Physical health and mental health third month improved significantly during the 2nd and 3rd month, while all other subscale scores did not (P > 0.05).
Conclusion
Methadone maintenance treatment is helpful in improving the quality of life of outpatients in MMT clinics in China.
Keywords: Quality of life, Addiction outpatient, Methadone Maintenance Treatment, China
INTRODUCTION
Drug addiction resurged in China in the early 1980s, and spread quickly in the 1990s. From 1990 to 2000, the numbers of registered drug abusers increased more than 11-fold from 70,000 to 860,000[1]. There were 957,000 registered drug abusers in 2007[2]; however, the real number of drug abusers is estimated to be much higher. Heroin remains the major drug of abuse (78%) in China, and nearly three-quarters (72.5%) of heroin users are injecting drug users (IDUs) [2] and 40% percent of IDUs are estimated to share needles or syringes[3]
Drug abuse is a complex issue and is linked to many social, economic, criminal and health challenges facing different societies, one of which is HIV/AIDS. Globally, IDUs account for approximately 10% of the estimated 4.3 million new HIV infections that occur each year[4]. Of the estimated 700,000 HIV people living with HIV/AIDS (PLWHA) in China in 2007, approximately 38.1% (266,700) were infected via injecting drug use[3]. Although sexual intercourse is now the main HIV/AIDS transmission route in China, injecting drug use is still a major HIV transmission route and accounted for 42% of new HIV cases in 2007[3].
In terms of the reduction of heroin use, criminal activity, and protection against HIV infection, methadone maintenance treatment (MMT) has been proven an effective therapy for heroin abuse [5–7]. After initial trials, MMT clinics were established by the Chinese government in 2004. According to an evaluation of the effectiveness of the first eight pilot MMT clinics in 2007[8], from baseline to 6 months, the proportion of drug use by clinical patients dropped rapidly (69.1% vs. 8.9%), injection frequency was reduced (90 times vs. twice per month), and self-reported criminal activities decreased sharply (20.7% vs. 3.6%). In addition, 95.9% of outpatients were satisfied with clinical services provided. Later studies of MMT in China have found results consistent to the evaluation of the 8 pilot MMT clinics [9–12]. Consequently, MMT is being scaled up rapidly in China and by the end of 2007, there were 503 clinics providing treatment for more than 50,000 outpatients per day.
In order to improve the effectiveness of MMT clinics, it was suggested that MMT clinics provide comprehensive services to outpatients in addition to MMT, such as providing free HIV and hepatitis C virus (HCV) testing. Although a comprehensive services model has not been developed, all MMT clinics provide at least one of the following services in China: anti-retroviral therapy for eligible clients, psychological counseling, rehabilitation programs with social support, life skills and employment skills training [13, 14].
In order to determine the impact of MMT on the lives of MMT clinic outpatients in China, a culturally appropriate quality of life instrument for drug addicts [15] was used to assess quality of life changes of MMT clinic outpatients during the first 3 months of treatment.
METHODS
Study Sites
Xi’an, the capital city of Shannxi province, has 8.2 million citizens, of which approximately 9,000 are registered drug addicts and 69 are PLWHA. There are 5 MMT clinics in Xi’an, 4 of which were established one month prior to study commencement. These 5 MMT clinics offer HIV/HCV testing and psychological counseling provided by doctors from these clinics.
Participant Recruitment, Informed Consent and Confidentiality
Participants were outpatients from the 5 MMT Clinics in Xi’an, who began treatment between November 15 and December 15, 2006. To be eligible, participants must: be 20 years or above; have at least primary school education; can self-administer the questionnaire; and do not have a serious mental illness. The participant criteria was given to the Chief Medical Officer of each clinic, who then checked all patient records and made a list of eligible potential participants (N = 176). All eligible potential participants were approached by the Chief Medical Officer to see if they were interested in participating in the study. The purpose and processes of the study, and the potential risks and benefits were explained by the researcher to each participant. It was emphasized that participation was confidential and their daily treatment would not be affected whether or not they participated in the study. All except four outpatients (2.2%) agreed to participate and verbal informed consent was obtained.
Quality of Life Instrument
The quality of life instrument for drug addicts (QOL-DA) used in our study was developed by Lin Xiao and colleagues in 2006. The instrument was developed to test the quality of life of drug addicts, and is composed of 61 items covering six dimensions: physical health, mental health, family relationships & social support, living condition (economic status and ability to participate in various social activities), drug dependence, and satisfaction with life. The Cronbach α coefficient was 0.958, test-retest reliability was 0.917, and half-split reliability was 0.844. Six dimensions accounted for 53.68% of variance. The loading of each item on expected factors was 0.433–0.853. The comparative fit index (CFI) was 0.95 and the standardized root mean residual (SRMR) was 0.07. In addition, the instrument had good content validity when tested on drug addicts using a cognitive study, indicating each item is perceived by drug addicts and the instrument designer as having a similar meaning. Therefore the QOL-DA has robust psychometric properties[15].
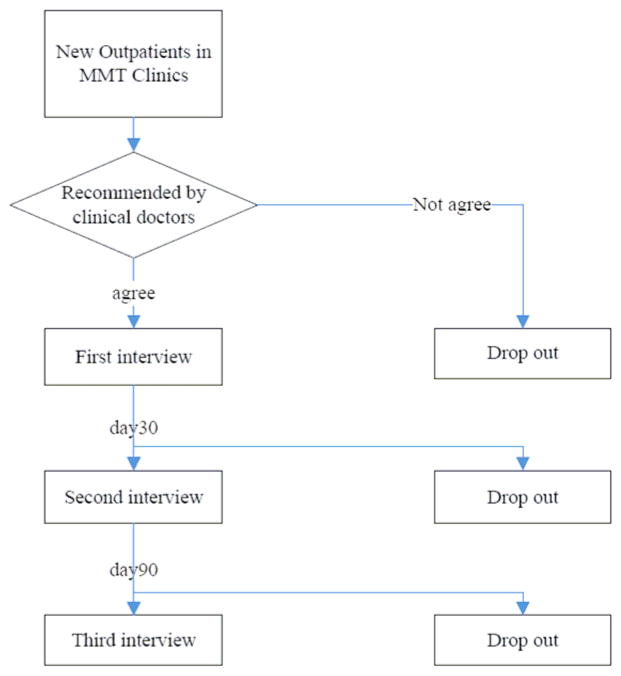
Study Design
A cohort study was conducted. Outpatients in MMT clinics were followed for 3 months (Figure 1). After informed consent was obtained, quality of life scores of outpatients were measured by the quality of life instrument for drug addicts at treatment day 1, day 30 and day 90.
Figure 1.
Study Design Flowchart
Permission to undertake the study was granted by the Institutional Review Board of the National Center for STD/AIDS Control and Prevention, Chinese Center for Disease Control and Prevention.
Interview
After informed consent was given, a self-administered questionnaire was completed by participants in a separate, private room. The researcher responded to interviewees’ questions and checked the integrity of the completed questionnaires. If any missed item was unintentional, this was immediately corrected.
Statistical Analysis
In order to ascertain whether or not socio-demographic characteristics were confounders in the comparison of quality of life for drug addicts, chi-square test and ANOVA were used to compare the socio-demographic characteristics of participants on day 1, day 30 and day 90. The reliability of the quality of life measurement was calculated. ANOVA for repeated measurement data was used to analyze the difference between drug addicts’ quality of life scores on day 1, day 30 and day 90. If the data didn’t accord with Feldt-Huynh condition, Greenhouse-Geisser adjusted result was used.
RESULTS
Socio-demographic Characteristics of Participants
One-hundred and seventy-two outpatients were recruited. On day 30, 163 (94.77%) outpatients remained and this dropped to 142 (82.56%) outpatients on day 90. During the course of the study most participants were male (~ 85%), unemployed (~ 76%), Han Chinese (~ 90%), intravenous drug users (~ 76%) and HCV positive (~ 73%). The socio-demographic characteristics of participants at each data collection time point are listed in Table 1.
Table 1.
Socio-demographic Characteristics of Participants
| Variables | Day 1 (172) | Day 30 (163) | Day 90 (142) |
|---|---|---|---|
| Gender (%) | |||
| Male | 146 (84.9) | 138(84.7) | 121(85.2) |
| Female | 26 (15.1) | 25(15.3) | 21(14.8) |
| Age (year) | 38.0±5.43 | 37.8±5.39 | 37.9±5.25 |
| Marital Status (%) | |||
| Single | 67(39.0) | 65(39.9) | 59(41.5) |
| Married | 80(46.5) | 75(46.0) | 63(44.4) |
| Divorced | 24(14.0) | 22(13.5) | 20(14.1) |
| Widow/Widower | 1(0.6) | 1(0.6) | 0(0.0) |
| Employment | |||
| Unemployed | 133(77.3) | 124(76.1) | 108(76.1) |
| Farmer | 4(2.3) | 4(2.5) | 2(1.4) |
| Employer | 12(7.0) | 12(7.4) | 11(7.7) |
| Laborer | 12(7.0) | 12(7.4) | 11(7.7) |
| Waiter | 8(4.7) | 8(4.9) | 7(4.9) |
| Office clerk | 3(1.7) | 3(1.8) | 3(2.1) |
| Ethnicity | |||
| Han | 154(89.5) | 147(90.2) | 126(88.7) |
| Hui | 17(9.9) | 15(9.2) | 15(12.6) |
| Zhuang | 1(0.6) | 1(0.6) | 1(0.7) |
| Education (%) | |||
| Primary school & illiterate | 17(9.9) | 17(10.4) | 14(9.9) |
| Junior high school | 96(55.8) | 91(55.8) | 80(56.3) |
| Senior high school | 51(29.7) | 47(28.8) | 40(28.2) |
| College and | 8(4.7) | 8(4.9) | 8(5.6) |
| Drug use (year) | 9.6±4.881 | 9.7±4.86 | 9.59±4.724 |
| Drug administration method (%) | |||
| Inhaled | 39(22.7) | 36(22.1) | 31(21.8) |
| Intravenous injection | 131(76.2) | 125(76.7) | 109(76.8) |
| Muscular injection | 1(0.6) | 1(0.6) | 1(0.7) |
| Mixed | 1(0.6) | 1(0.6) | 1(0.7) |
| HIV (%) | |||
| Yes | 0(0.0) | 0(0.0) | 0(0.0) |
| No | 161(93.6) | 157(96.3) | 137(96.5) |
| Unknown | 11(6.4) | 6(3.7) | 5(3.5) |
| HCV (%) | |||
| Yes | 122(70.9) | 119(73.0) | 106(74.6) |
| No | 39(22.7) | 38(23.3) | 31(21.8) |
| Unknown | 11(6.4) | 6(3.7) | 5(3.5) |
The socio-demographic characteristics of participants at day 1, day 30 and day 90 were compared, and no significant difference was found between the different time points (P > 0.05). Thus, socio-demographic characteristics were not confounders for comparison of the quality of life scores for drug addicts between day 1, day 30 and day 90.
Reliability of the Quality of Life Instrument
In our study, the reliability of the quality of life of instrument was calculated, and the results are as follows: Cronbach α coefficient was 0.96 for the overall instrument, and was 0.91 for physical health, 0.94 for mental health, 0.86 for family relationship & social support, 0.74 for living condition, 0.81 for drug dependence, and 0.86 for satisfaction with life. The Spearman-Brown split-half reliability coefficient was 0.86 overall, and was 0.83 for physical health, 0.89 for mental health, 0.82 for family relationship & social support, 0.72 for living condition, 0.83 for drug dependence, and 0.83 for satisfaction with life. According to Fayer & Hays, reliabilities of an instrument exceeding 0.70 are acceptable for group comparison, and should be larger than 0.8 for individual evaluation[16]. This indicates the quality of life instrument used in this study has sufficient reliability.
Quality of Life for Outpatients Receiving MMT
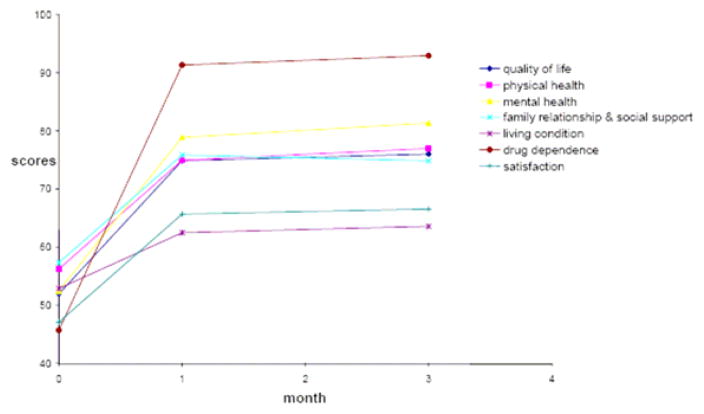
Table 2 and Figure 2 show the changes of quality of life score and subscale scores of outpatients receiving MMT at treatment initiation, day 30 and day 90.
Table 2.
Quality Of Life of 142 Outpatients at day 1, day 30, and day 90
| Day 1 (x̄± s) | Day 30 (x̄± s) | Day 90 (x̄± s) | |
|---|---|---|---|
| Quality of life | 51.92 ± 10.893 | 74.83 ±8.786 | 75.99 ± 8.635 |
| Physical health | 56.17 ± 14.286 | 74.91 ± 11.220 | 76.94 ± 12.260 |
| Mental health | 52.46 ± 16.134 | 78.85 ± 13.833 | 81.33 ± 13.492 |
| Family relationship & social support | 57.31 ± 16.172 | 75.82 ± 15.203 | 74.82 ± 14.882 |
| Living condition | 52.85 ± 10.146 | 62.45 ± 10.632 | 63.55 ± 10.346 |
| Drug dependence | 45.65 ± 14.893 | 91.31 ± 9.275 | 92.92 ± 8.780 |
| Satisfaction with life | 47.06 ± 13.335 | 65.65 ± 13.102 | 66.50 ± 12.701 |
Figure 2.
Changes of quality of life and subscale scores
As the ANOVA for repeated measurement data indicates, quality of life scores of outpatients in MMT clinics differed between days 1, 30 and 90 (F = 469.15, P < 0.05). The quality of life score on day 30 was higher than day 1 (F = 550.44, P < 0.05), and only a minor increase was measured from day 30 to day 90 (F = 191.34, P = 0.05). This indicates MMT is helpful in improving the quality of life of outpatients in clinics, especially in the first month.
Physical health
The physical health subscale score increased from day 1 to day 30 (F = 191.71, P < 0.05), and from day 30 to day 90 (F = 6.32, P < 0.05) indicating that the physical health of outpatients receiving MMT improved gradually over the three month period.
Mental health
The score of mental health increased significantly from day 1 to day 30 (F = 324.65, P < 0.05), and also did so from day 30 to day 90 (F = 5.77, P < 0.05).
Family relationship & social support
The subscale score for family relationship & social support of outpatients on day 30 improved over day 1 (F = 163.54, P < 0.05). This was the only subscale to register a decrease from day 30 to day 90, although this decrease was not significant (F = 0.85, P > 0.05).
Living condition
The subscale score on day 30 is much higher than that on day 1 (F = 124.34, P < 0.05); however, there was no significant change between day 30 and day 90 (F = 1.55, P > 0.05), indicating that outpatients’ living conditions improved rapidly in the first month and then remained stable for the following 2 months.
Drug dependence
Among all the subscales, scores on this subscale showed the largest improvement in the first month, improving dramatically from 45.65 to 91.31 in the first month (F = 1095.39, P < 0.05). The scores remained stable at this level from day 30 to day 90 (F = 3.44, P > 0.05).
Satisfaction with life
This improved significantly in the first month (F = 226.34, P < 0.05), and there was only a minor improvement between day 30 and day 90 (F = 0.86, P > 0.05).
DISCUSSION
Heroin addiction is not only symptomatic of problems in the lives of drug addicts but it also can introduce serious problems into the lives of such users. More than 70% of drug addicts in China suffer from physical illnesses including gastritis, bacterial infections, cardiovascular diseases, pulmonary disease, hepatitis and HIV/AIDS[17]. In our study, physical health of outpatients improved continuously from day 1 to day 90. This indicates that although some outpatients experienced side-effects from methadone, their physical health improved greatly due to MMT.
In China, drug addicts, and in particular those who use heroin, have poor mental health, such as low self-esteem and high anxiety, compared to non-addicts[18, 19]. The results of our study showed that MMT continually improved outpatients’ mental health from treatment initiation to day 90. This may be because MMT enabled outpatients to feel less stressed after the start of treatment due to being free from the financial burdens of drug addiction, and not needing to worry about being arrested or having an overdose. In addition, there is strong stigma towards drug addicts in China and most outpatients feel ashamed of their addiction to heroin. After treatment initiation, they slowly became independent from heroin addiction, and their self esteem returned as a result[20]. Moreover, the support they received from the MMT doctors and family members may have helped to further improve the mental health of outpatients.
The improved living condition in the first month of MMT might be because most clients receive more financial support from their families compared to before treatment initiation. However, due to most drug addicts lacking suitable employment skills, and combined with the strong discrimination against drug addicts in China, it is extremely difficult for MMT outpatients to gain and maintain meaningful employment. Thus, their living condition score did not improve much. This suggests a need to provide career training programs in MMT clinics and conduct interventions in communities to reduce stigma against drug addicts.
Addicts usually receive less social support than non-addicts[21, 22]. In our study, outpatients in MMT improved relationships with their families and received more social support from day 1 to day 30; however this improvement did not continue from day 30 to day 90, and in fact decreased slightly. This might be due to misunderstanding from family members of the effectiveness with which MMT can assist outpatients to detoxify and be rehabilitated; they may have hoped MMT could solve all problems caused by heroin addiction. Family members may lose heart if the outpatient relapses into drug use or conducts property crime. This suggests the need to provide consulting services for family members, since family is of central importance in Chinese culture and most support for outpatients come from their families as social support services of this nature for drug users are not widely available in China.
Although the provision of comprehensive services using MMT clinics as a platform for delivery needs require expanding, improving and scaling up, the quality of life of outpatients receiving treatment in the existing MMT clinics improved significantly. This result is consistent with studies in western countries[23–25].
It is well know that retention rates are a potential problem for MMT programs, and many studies have investigated this issue [26–29]. In our study, 9 participants dropped out by the end of the first month and the retention rate at day 90 was 82.6%. These results were similar with another study in China, which showed the average retention rate was 93.5% at day 30, and 81.5% at day 90 [30].
Due to good relationships between outpatients and doctors in the MMT clinics, only four qualified potential participants refused to participate in our study. Thus, the results of our study are reliable to reflect upon quality of life changes in literate outpatients in MMT clinics. In our study, all participants were required to administer the questionnaire themselves; therefore illiterate drug addicts were excluded. Illiterate MMT clinic outpatients still need to be studied as their quality of life may be different to that of literate MMT clinic outpatients; the latter of whom may have greater employment opportunities.
CONCLUSION
Methadone maintenance treatment is helpful in improving the quality of life of outpatients in MMT clinics and should be expanded further in China.
Acknowledgments
Thanks go to the staff at Xi’an CDC and the Directors of the 5 Methadone Maintenance Treatment Clinics in Xi’an for their help with this study. The authors would also like to thank Naomi Juniper and Adrian Liau for their assistance in editing the manuscript.
Supported by the International Clinical Operational and Health Services Research and Training Award (ICOHRTA) AIDS/TB, Grant # U2R TW 006917 and U2R TW 006918, funded by the National Institutes of Health, the Fogarty International Center, the National Institute of Drug Abuse and the National Institute of Mental Health.
References
- 1.Tang YL, Zhao D, Zhao C, Cubells JF. Opiate addiction in China: current situation and treatments. Addiction. 2006;101:657–665. doi: 10.1111/j.1360-0443.2006.01367.x. [DOI] [PubMed] [Google Scholar]
- 2.Annual Report on Drug Control in China. Beijing: China National Narcotics Control Committee; 2008. [Google Scholar]
- 3.2007 Update on the HIV/AIDS Epidemic and Response in China. Beijing: Chinese Ministry of Health&Joint United Nations Program on HIV/AIDS WHO; 2007. [Google Scholar]
- 4.Aceijas C, Stimson GV, Hickman M. Global overview of injecting drug use and HIV infection among injecting drug users. AIDS. 2004;18:2295–2303. doi: 10.1097/00002030-200411190-00010. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein A, Herrera J. Heroin addicts and methadone treatment in Albuquerque: a 22-year follow-up. Drug Alcohol Depend. 1995;40:139–150. doi: 10.1016/0376-8716(95)01205-2. [DOI] [PubMed] [Google Scholar]
- 6.Verster ABE. In: Information for policymakers on the effectiveness of substitution treatment for opiate dependence. Euromethwork TN, editor. 2003. [Google Scholar]
- 7.Literature Review: Methadone Maintenance Treatment. Ottawa: Health Canada; 2002. [Google Scholar]
- 8.Pang L, Hao Y, Mi G, Wang C, Luo W, Rou K, et al. Effectiveness of first eight methadone maintenance treatment clinics in China. Aids. 2007;21 (Suppl 8):S103–107. doi: 10.1097/01.aids.0000304704.71917.64. [DOI] [PubMed] [Google Scholar]
- 9.Yang X, Hao C, Ruan Y. Impact of Community-based Methadone Maintenance Treatment on Social Function and Family Relationship among Heroin Addicts. Chinese Journal of Natural Medicine. 2007;9:15–19. [PubMed] [Google Scholar]
- 10.Hao C, Zhang L, Ruan Y. on the Impact of Community-based methadone maintenance treatment Among Drug Addicts. Journal of Preventive Medicine Information. 2006;22:251. [Google Scholar]
- 11.Long Z, Wu Z, Du B. Situation of 538 Heroin Addicts Undertaking Methadone Maintenance Treatment. Chinese Journal of Drug Dependence. 2006;15:38–40. [Google Scholar]
- 12.Liu Y, Deng P, Xiong X. Effective Evaluation on Methadone Maintenance Treatment in Chaoyang District, Beijing. Chinese Journal of Drug Dependence. 2007;16:302–306. [Google Scholar]
- 13.Zhang C, Chen S. Changes in Copying styles and Social Support of Patients Treated with Methadone Maintenance Combined with Rehabilitation Program. Chinese Journal of Drug Dependence. 2008;17:293–296. [Google Scholar]
- 14.Luo J, Zhang C, Yang G. Explore of Methadone Maintenance Treatment in Drug addicts. Soft Science of Health. 2006;20:41–42. [Google Scholar]
- 15.Xiao L, Wu Z, Li J. Development of Quality of Life Measurement for Drug Addicts. Chinese Mental Health Journal. 2007;21:386–388. [Google Scholar]
- 16.Fayers PHR. Assessing quality of life in clinical trials. New York: Oxford New York: Oxford University Press; 2005. [Google Scholar]
- 17.Zhao C, Liu Z, Zhao D, Liu Y, Liang J, Tang Y, et al. Drug abuse in China. Ann N Y Acad Sci. 2004;1025:439–445. doi: 10.1196/annals.1316.054. [DOI] [PubMed] [Google Scholar]
- 18.Liang J. Psychological characters and influence factors of heroin addicts. Chinese Journal of Drug Abuse Prevention and Treatment. 2004;10:340–342. [Google Scholar]
- 19.Wang L, Luo L, Zhao J. Study of mental health, social, and quality of life for drug addicts. Psychological Science. 2004;27:284–286. [Google Scholar]
- 20.Xiao L, Wu Z, Pang L. Qualitative study on the effectiveness of community-based methadone maintenance treatment among heroin addicts in some regions of China. Chinese Journal of AIDS&STD. 2007;13:195–197. [Google Scholar]
- 21.Yang J, Zheng L, Liu L. Investigation on and analysis of social support system of drug users. Chinese Journal of Drug Dependence. 2008;17:217–219. [Google Scholar]
- 22.Wang P. An investigation on coping style and status of social support system in heroin addicts. Chinese Journal of Drug Abuse Prevention and Treatment. 2004;10:26–28. [Google Scholar]
- 23.Richter D, Eikelmann B, Berger K. Use of the SF-36 in the evaluation of a drug detoxification program. Qual Life Res. 2004;13:907–914. doi: 10.1023/B:QURE.0000025589.07313.46. [DOI] [PubMed] [Google Scholar]
- 24.Puigdollers E, Domingo-Salvany A, Brugal MT, Torrens M, Alvaros J, Castillo C, et al. Characteristics of heroin addicts entering methadone maintenance treatment: quality of life and gender. Subst Use Misuse. 2004;39:1353–1368. doi: 10.1081/ja-120039392. [DOI] [PubMed] [Google Scholar]
- 25.Torrens M, Domingo-Salvany A, Alonso J, Castillo C, San L. Methadone and quality of life. Lancet. 1999;353:1101. doi: 10.1016/S0140-6736(05)76462-X. [DOI] [PubMed] [Google Scholar]
- 26.Greenfield L, Brady JV, Besteman KJ, De Smet A. Patient retention in mobile and fixed-site methadone maintenance treatment. Drug Alcohol Depend. 1996;42:125–131. doi: 10.1016/0376-8716(96)01273-2. [DOI] [PubMed] [Google Scholar]
- 27.Gossop M, Marsden J, Stewart D, Treacy S. Outcomes after methadone maintenance and methadone reduction treatments: two-year follow-up results from the National Treatment Outcome Research Study. Drug Alcohol Depend. 2001;62:255–264. doi: 10.1016/s0376-8716(00)00211-8. [DOI] [PubMed] [Google Scholar]
- 28.Torrens M, Castillo C, Perez-Sola V. Retention in a low-threshold methadone maintenance program. Drug Alcohol Depend. 1996;41:55–59. doi: 10.1016/0376-8716(96)01230-6. [DOI] [PubMed] [Google Scholar]
- 29.Anderson JF, Warren LD. Client retention in the British Columbia Methadone Program, 1996–1999. Can J Public Health. 2004;95:104–109. doi: 10.1007/BF03405776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu E. Factors Influencing Client Retention in Methadone Maintenance Treatment Clinics in China. Los Angeles: University of California Los Angeles; 2008. [Google Scholar]