Abstract
In this article, we use age of immigration as a proxy for the developmental context for understanding the association between immigration experiences and mental health. Generation defines the context under which immigrants arrive in the United States. We drew data from the National Latino and Asian American Study (N = 2,095), the first ever study conducted on the mental health of a national sample of Asian Americans. Our findings reveal that age of immigration is linked to lifetime and 12-month rates of psychiatric disorder: Immigrants who arrive earlier in life are more likely to have both lifetime and 12-month disorders. U.S. born and immigrants who arrive as children are much more likely to have a mental disorder in their lifetimes than other immigrant generations.
Cumulative disadvantage and acculturation or cultural assimilation hypotheses are often invoked when considering the association between immigration and mental health. Time, which plays a central part in both hypotheses, gauges the change and adjustment of immigrants in their new communities. The acculturation hypothesis posits that the longer one resides in a location, the more familiar and integrated the person becomes with the language, lifestyle, and culture of the new place (Chun, Organista, & Marin, 2002; Salent & Lauderdale, 2003). Any social or health disadvantages immigrants may experience on arrival will be substantially reduced or eliminated over time. Immigrants become integrated into the mainstream of society and can take advantage of social and community resources to reduce the impact of stressors and to seek care before serious emotional and psychological problems arise. The cumulative disadvantage hypothesis suggests the opposite: Over time, the social or health disadvantages will actually increase the longer immigrants reside in a new location (Rumbaut, 1999; Rumbaut & Weeks, 1996; Shuval, 1982). Because of discrimination and other social factors, immigrants do not become fully integrated in American society. They also learn, over time, the unhealthy habits and lifestyles that are associated with poor health in American society. Whereas this time variable assumes that people change or learn about a new culture at the same pace, time of residence is commonly used to assess the association between adaptation and mental health outcomes. The available evidence has not supported a uniform pattern across various immigrant groups (Escobar & Vega, 2000; Landale, Oropesa, & Gorman, 2000; Williams & Collins, 1995).
Whereas length of residence provides a measure of adaptation and adjustment, prior studies on immigration and mental health have often ignored another vital time dimension: the age when an immigrant arrives in a new country. A few studies have demonstrated that age of immigration can be an important correlate of mental health. In a national study of older adults, for example, Angel, Buckley, and Sakamoto (2001) found that late-life immigrants experience higher levels of emotional distress than U.S.-born individuals. Childhood immigrants were statistically indistinguishable from the U.S. born in levels of emotional distress. Another study focusing on Chinese Americans in Los Angeles, California came to different conclusions and found that immigrants who came as children were more likely to suffer from major depression than immigrants who came as adults (Hwang, Chun, Takeuchi, Myers, & Siddarth, 2005). Breslau and Chang (2006) also found the significantly lower risk for mood, anxiety, and substance-abuse disorders for Asian Americans who immigrated during adolescence or adulthood (age 14 or older) compared to U.S. born and immigrants who arrived as children (age 13 or younger). Beyond immigration per se, the age when Asians immigrate to the United States is strongly associated with major depression. Chinese immigrants, for example, who arrive after their 20th birthday are nearly 1.5 to 3.0 times more likely to have had major depression than those who arrive before they reach 20 years of age (Takeuchi et al., 1998). Some of the discrepancies in past studies may be attributed to different sampling frames, varying measures of mental health, and the inclusion of different ethnic groups. The essential point is that age of immigration can be an important determinant of emotional health, albeit in different ways.
One of the difficulties in studying age of immigration and mental health is that the variable is often treated as a risk factor devoid of any conceptual underpinnings. In this article, we suggest that research on this variable can be enhanced by seeing age of immigration as a proxy for the developmental context of a person’s experiences at the time of their arrival in the United States. When seen in this light, it has the potential to be a powerful factor in understanding how a person negotiates life in a new country and different culture. The context when people immigrate help shape language ability and usage, density and heterogeneity of friendship networks, place of residence, and exposure to risky behaviors and stressful environments. In this study, we used the construct of generation that defines the context under which immigrants arrive in the United States. In our analyses, we assess how generation helps explain the association between immigration and psychiatric disorder. We used data drawn from the National Latino and Asian American Study (NLAAS), which is the first ever study conducted on the mental health of a national sample of Asian Americans.
BACKGROUND
Immigrant generation is defined by age and life stage when a person immigrates into a new society and has unique opportunities and challenges during discrete developmental periods. Immigrant generation may lead to different life-course trajectories because the social institutions in a new society affect immigrants’ lives in different ways by age of immigration (Fuligni, 2004; Rumbaut, 2004). Different social institutions provide access to unique types of social networks and relationships. Social networks are specific sets of concrete intermediary linkages that provide a mechanism in which macrostructural phenomena exert influence on individuals (Granovetter, 1973; Laumann & Pappi, 1976). Social networks can be seen as opportunity structures because when a person’s social ties have access to societal resources and opportunities, the person has greater access to those resources and opportunities. The number of social groups and institutions (e.g., schools, clubs, friendship networks, and family ties) geared toward teaching the child about the new society is far greater than those available for adults. These social groups, in turn, provide children with a greater access to the opportunity structures in a new culture. Conversely, given the larger set of social groups available for immigrant children, there may also be a greater amount of negative stressors and influences that can lead to detrimental social and health outcomes as the child matures.
Although an important developmental distinction is between immigrants who arrive as children or adults, this distinction may too broad and obscures some critical processes unique to children and adolescents or between young adults and older adults. Rumbaut (2004) provided a more refined typology of immigrant generations that highlights some of the opportunities and challenges at each developmental stage. The generation categories provide a novel frame to understand the association between immigration and mental health (Fuligni, 2004). Immigrants who arrive in the United States during adulthood (18 years and older) are the 1.0 generation. In the making more refined distinctions in immigrant developmental processes, we break from convention and separate the 1.0 generation into two categories: (a) immigrants who arrive between 18 and 40 years old (1.0a generation) and (b) immigrants who arrive in the United States after the age of 41 years old (1.0b generation). The 1.0a generation receives all of their elementary and secondary schooling in another country. They may have difficulties speaking English, and their important social networks may be with coethnics who come from the same country. If they received their college education in the United States, they are likely to accrue the same economic and social economic rewards as U.S.-born individuals. The 1.0b generation receives all of their schooling in another country and is likely to experience difficulties with English. Even if they have a college education and advanced degrees, they may not be able to accrue the same rewards from their investment as their U.S.-born counterparts (Zeng & Xie, 2004). Their social networks are likely to be comprised of coethnics, and they may have difficulties finding jobs that match their areas of interests and expertise.
The 1.25 generation arrives in the United States between 13 and 17 years of age. They receive a portion of their schooling in another country and often, have difficulties learning the English language. The 1.25 generation is often referred to as a group caught between two cultures: the American and their ethnic culture. They may be different from their American-born peers in terms of their values, knowledge of American culture, and lifestyles. Immigrants who arrive at the age of 12 years or below are considered the 1.50 generation. Schools are the principal socialization institution outside of the family, and in fact, the 1.50 generation receives most of its schooling in the United States. Because they come to the United States as children, they are able to grasp American culture and values and speak English at a quicker pace than older generations. Compared to other generational categories, they are more likely to have similar opportunities for mobility and opportunities to engage in risky behavior as their U.S.-born counterparts.
Generation may be associated with mental disorders in at least three distinct ways. First, the onset for many psychiatric disorders, especially the most prevalent ones such as affective, anxiety, and substance use, occurs in adolescent or early adulthood (American Psychiatric Association, 1994). Immigrants coming in at earlier ages, especially at childhood, have the longest period of time during this risk period. Immigrants who come at earlier ages also may be at risk for problems such as substance abuse because they have the potential to be involved in social networks that may have greater access and opportunity to engage in these behaviors. Because the 1.50 generation is most similar to U.S.-born individuals among the different generation of immigrants, we would expect that these two groups would have similar rates of different mental disorders.
Second, and related to the first, the construct of generation provides a period marker when mental disorders are likely to occur. Immigration to a new country is a major transition that involves leaving one’s established community, social networks and support, and social position; encountering unfair treatment as an outsider; and learning a new language and culture. It’s reasonable to suggest that the period shortly after immigration represents a critical risk period for immigrants in which multiple stressors associated with these transitions can lead to serious mental health problems. In this article, we investigate whether the critical risk is true for all immigrant generations or whether it is more likely to occur for certain ones, in particular, immigrants who arrive as children and adolescents.
Finally, it is often assumed that different facets of immigration are associated with psychological health and psychiatric disorders. However, it is possible that immigrants come with a preexisting psychiatric disorder. Few studies have taken this into account when they have assessed the association with immigration and psychiatric disorders. Because psychiatric disorders are more likely to occur in adolescence or early adulthood, it is likely that older immigrants generations 1.0a and 1.0b, have a higher proportion of psychiatric disorders prior to their arrival in the United States. Given our unique data set, we examine this issue by testing whether psychiatric disorders are more likely to occur before or after immigration and how these patterns vary by generations. The associations between generation and different psychiatric disorders may vary by gender, as men and women differ in rates and types of psychiatric disorders. Women are more likely to have depression, anxiety, and somatic complaints than men, whereas men are more likely to experience alcohol dependence and antisocial personality disorder than women (Gater et al., 1998; Kessler et al., 1994; Linzer et al., 1996; Piccinelli & Homen, 1997; World Health Organization, n.d.).
In sum, the construct of generation provides an innovative frame for examining how age of immigration is associated with psychiatric disorders. More than in previous studies, we can address the following questions: (a) Is generation associated with psychiatric disorders? (b) How is generation linked to specific psychiatric disorders, and do these patterns vary for men and women?, and (c) Are some generations more likely to have a psychiatric disorder prior to their arrival in the United States?
METHOD
We drew data for this study from the NLAAS. The NLAAS core sampling procedure resulted in a nationally representative household sample of Latino and Asian Americans. This study is based on data from the sample of Asian Americans in the NLAAS project. A detailed description of the NLAAS protocol and sampling methods has been previously documented (Alegría, Takeuchi, et al., 2004; Pennell et al., 2004; Heeringa et al., 2004). Following is a brief description of the NLAAS sampling design and study procedure.
Sampling Design
Participants in the NLAAS were recruited using one of three sampling methods. First, participants in the core sample were recruited with a multistage stratified area probability sampling design. Primary sampling units (PSUs), defined as metropolitan statistical areas (MSAs) or county units, and secondary sampling units (SSUs), formed from contiguous grouping of census blocks, were selected using probability proportionate to size (PPS), from which households were sampled. One member of the household was selected using standard Kish methods (Kish, 1965; Pennell et al., 2004).
Second, participants in the NLAAS high-density supplemental sample were recruited using a 5% density criterion, in which Latino or Asian target ancestry groups representing at least 5% of total households in a census block were oversampled. Individuals who were Latino or Asian and did not belong to the target ancestry group under which these geographical areas were classified were still eligible to participate. For example, Chinese individuals living in a Filipino high-density census block were eligible for recruitment into the NLAAS. Therefore, individuals living in high-density areas had two opportunities for recruitment: first through the NLAAS core sampling strategy and second through the NLAAS high-density sampling strategy.
Third, in addition to core and high-density sampling methods, second respondents were recruited from households in which one participant had already been interviewed. Second respondent sampling was utilized to increase the total sample of participants and to reduce study expenses. The three components of the NLAAS sampling design resulted in the construction of weighting corrections to take into account joint probabilities of selection.
Study Procedure
Interviewers with linguistic and cultural backgrounds concordant with those of the target population administered the NLAAS questionnaire. Interviewers underwent rigorous training and were tested by an independent service to assess bilingual language fluency and proficiency with all NLAAS materials. Participants were initially contacted with an introductory letter and study brochure followed by screening, scheduling, and interviewing. Interviews were conducted in the preferred language indicated by the respondent using computer-assisted interviewing software. The questionnaire was administered face-to-face to participants in the NLAAS core and high-density samples unless the respondent specifically requested a telephone interview or if a face-to-face interview was prohibitive. Interviews were conducted via telephone to second respondents. As a measure of quality control, a random sample of participants with completed interviews was recontacted to validate the data. The average duration of each interview was 2.6 hours. A $50.00 incentive was initially provided to participants, but was later increased up to $150.00 to reduce nonresponse. Written informed consent was obtained for all participants, and all study procedures and protocols were approved by Institutional Review Boards (IRB) at University of Washington, Cambridge Health Alliance, Harvard University, and the University of Michigan.
Sample
Participants in this study were noninstitutionalized people of Asian ancestry who were 18 years of age or older and resided in any of the 50 states and Washington, DC. Three Asian national origin groups targeted for the Asian American sample were Chinese, Filipino, or Vietnamese in addition to individuals of “other” Asian ancestry. A total of 2,095 Asian American participants were recruited between May 2002 and November 2003 as part of the larger NLAAS survey. The final weighted response rate for the NLAAS Asian American sample was 69.3% for first respondents and 73.6% for second respondents. The combined weighted response rate for Asian American participants was 65.6%. Detailed sample characteristics are reported in other NLAAS studies (Alegría, Takeuchi, et al., 2004; Pennell et al., 2004).
Measures
In addition to English, the NLAAS battery was available in Spanish, Chinese, Tagalog, and Vietnamese. The NLAAS instrument was translated using standard translation and back-translation techniques based on a comprehensive model focusing on five dimensions of cultural equivalence (Alegría, Vila, et al., 2004). The NLAAS instruments were not available in other Asian languages.
Generation and age of immigration
Respondents were categorized into different immigrant generations based on the age when they arrive in the United States: (a) Generation 1.50 or individuals who immigrated at 0 to 12 years of age, (b) Generation 1.25 (13–17 years), (c) Generation 1.0a (18–40 years), and (d) Generation 1.0b (41+ years). We also included respondents born in the United States in some of our analyses. Age of immigration is measured as a continuous variable using the item “How old were you when you first came to this country?”
Diagnostic measures
The primary diagnostic instrument included in the NLAAS questionnaire was the World Mental Health Survey Initiative version of the World Health Organization Composite International Diagnostic Interview (WMH–CIDI; World Mental Health Survey Consortium, 2004). The questionnaire included 22 diagnostic sections and 4 sections assessing functioning and physical comorbidity. The WMH–CIDI was used to assess lifetime and 12-month psychiatric disorder using the Diagnostic and Statistical Manual of Mental Disorders (4th ed. [DSM–IV]; American Psychiatric Association, 1994). The WMH–CIDI is a fully structured diagnostic instrument that may be administered by trained lay interviewers. Diagnostic assessments using earlier English versions of the CIDI have been found to be concordant with those of trained clinical interviewers (Wittchen, 1994). However, the validity of the Chinese, Tagalog, and Vietnamese versions of the WMH–CIDI developed for this study has not been assessed. “Any” disorder was based on the diagnosis of at least one disorders in any of the following four categories: (a) affective disorders (major depression or dysthymia), (b) anxiety disorders (panic disorder, agoraphobia, social phobia, generalized anxiety disorder, or posttraumatic stress disorder), (c) substance disorders (alcohol abuse, alcohol dependence, drug abuse, or drug dependence), and/or (d) other disorders (panic attack, bulimia, or anorexia). We focus on lifetime, the presence of a disorder in one’s lifetime, and current or 12-month disorder—the presence of a disorder within a year of the interview—as the primary outcome variables.
Control variables
We included gender, age of the respondent, and length of residence in the United States as control variables. Gender was coded as a dummy variable, with women given a score of “1.” Age of respondent was a continuous variable that begins from 18 years old. Length of residence is also a continuous variable we computed using age of respondent and age of immigration.
Analyses
We computed the lifetime and 12-month prevalence rates for any affective, any anxiety, any substance abuse, and any disorder for the total sample and for immigrants. We report weighted percentages, means, and standard errors, and we used the SUDAAN software system version 9.0 (RTI International, 2004) to adjust for sample weights and sample design effects.
We employed survival analyses to examine the associations between age at immigration and mental disorders, which reduced the bias associated with the age distribution of the sample (Cox & Oakes, 1984; Lee, 1992; StatSoft, Inc., 2006). We used Cox proportional hazard regression to calculate the hazard ratio (HR) for experiencing lifetime mental disorders (any affective, any anxiety, any substance abuse, and any disorder). We estimated the parameters in the Cox model by the maximum likelihood methods using the PHREG procedure of SAS version 9.1. We present the results in terms of estimated HRs or relative risks and their p values. Because we are examining how age of immigration influence on psychiatric disorders, we excluded U.S.-born respondents from these analyses. Age at immigration is the main predictor variable in the Cox model, and the control variables are gender (women = 1) and length of residence in the United States. Because age and length of residence were highly correlated (r = .43, p < .0001), we replaced age with length of residence and ran the same regression models. The findings on age of immigration remained consistent when using length of residence instead of age. We used length of residence as a time-varying covariate, as each respondent has a different effective length of residence at each different time in their life. We used logistic regression to examine the associations between age at immigration and 12-month mental disorders because 12-month disorders behave like binary outcome variables, which do not occur over continuous time with no censored data (incomplete observations of the survival time). As for survival analysis data, some individuals may not be observed for the full time until an event occurs (e.g., because of termination of the study). We conducted logistic regression analyses using the SUDAAN software system to adjust for sample weights and sample design effects.
Using the life table survival analysis method, we plotted hazard rates to show the risk of initiating major psychiatric disorders across the developmental life stages—childhood (0–12 years old), adolescence (13–17), young adulthood (18–40), middle adulthood (41–54), and late adulthood (55–65)—for those among whom initiation had not occurred previously. We conducted these analyses separately by gender and controlled for the age of respondent to compensate for the age distributions of the generational samples and to correct for the possibility that older respondents have more time to develop a psychiatric disorder. These analyses include both U.S.-born and immigrant samples.
RESULTS
Sample Characteristics and Prevalence Rates of Mental Disorders
Table 1 displays the sample characteristics for the total Asian American sample (N = 2,095) and for those Asian Americans who were immigrants (N = 1,639). Sample sizes for each of the generations, including U.S.-born respondents, were over 100 respondents: The 1.0a generation (18–40 years old) had the largest sample and the l.25 generation, the group of immigrants who arrived as adolescents, had the smallest sample. Table 1 also shows the lifetime and 12-month rates of the different psychiatric disorders. Approximately 18% of the respondents experienced a psychiatric disorder in their lifetime, and half this percentage (9.5%) had experienced the problem within 12 months prior to the interview. Affective and anxiety disorders were the most prevalent in our sample, as has been commonly found in other studies (Kessler, Berglund, et al., 2005; Kessler, Chu, Demler, Merikangas, & Walters, 2005), and substance-abuse disorders had a relatively low prevalence. The rates for the immigrant sample were lower than the overall rates for the total sample, suggesting that immigrants had lower rates of psychiatric disorders than U.S.-born Asian Americans. In fact, U.S.-born Asian Americans and the 1.50 generation had the highest lifetime rate of any disorder (25%), with the other immigrant generations having had similar rates between 13% and 15% (data not shown). This pattern generally held for the specific disorders with the exception of substance-use disorders. U.S.-born respondents had the highest lifetime rate of substance abuse disorders (13%) followed by the 1.50 and the 1.25 generations (4.5% and 5.6%, respectively). The 1.0 generations had the lowest rates of substance abuse disorders, with each prevalence rate below 2%.
TABLE 1.
Distribution of Demographic Characteristics and Rates of Psychiatric Disorders Among Asian Americans in the NLAAS
| Total Sample |
Immigrants Only |
|||||
|---|---|---|---|---|---|---|
| Variable | N | Weighted %/M |
SE | N | Weighted %/M |
SE |
| Gender | ||||||
| Male | 998 | 47.45% | 1.22% | 771 | 46.46% | 1.34% |
| Female | 1,097 | 52.55% | 1.22% | 868 | 53.54% | 1.34% |
| Age (years) | 41.33 | 0.89 | 42.45 | 0.81 | ||
| Generation | ||||||
| U.S. born | 454 | 23.07% | 3.17% | |||
| 1.50 generation (0–12) years | 237 | 12.72% | 1.42% | 237 | 16.53% | 1.79% |
| 1.25 generation (13–17) | 130 | 5.08% | 0.57% | 130 | 6.61% | 0.78% |
| 1.0a generation (18–40) | 1,022 | 47.85% | 2.61% | 1,022 | 62.19% | 1.75% |
| 1.0b generation (41+) | 249 | 11.28% | 1.36% | 249 | 14.66% | 1.64% |
| Missing = 3, 1 | ||||||
| Length of residence (years) | 21.08 | 1.35 | 16.14 | 0.59 | ||
| Age at immigration (years) | 26.32 | 0.74 | ||||
| Lifetime prevalence | ||||||
| Any disorders | 373 | 17.91% | 1.50% | 244 | 15.72% | 1.46% |
| Any affective disorders | 196 | 9.10% | 0.88% | 125 | 8.02% | 0.82% |
| Any anxiety disorders | 198 | 9.82% | 1.23% | 131 | 8.84% | 1.11% |
| Any substance disorders | 85 | 3.96% | 0.69% | 36 | 2.25% | 0.74% |
| 12-month prevalence | ||||||
| Any disorders | 192 | 9.46% | 0.72% | 123 | 8.35% | 0.76% |
| Any affective disorders | 95 | 4.73% | 0.59% | 60 | 4.27% | 0.51% |
| Any anxiety disorders | 117 | 5.75% | 0.71% | 72 | 4.91% | 0.74% |
| Any substance disorders | 28 | 1.30% | 0.27% | 10 | 0.70% | 0.25% |
Note. Total sample N = 2,095; immigrant sample n = 1,639. NLAAS = National Latino and Asian American Study; M = mean; SE = standard error.
Age of Immigration and Lifetime Mental Disorders
Table 2 presents HRs derived from a series of Cox proportional hazard regression analyses estimating the association between age of immigration and lifetime mental disorders (i.e., any affective, any anxiety, any substance abuse, and any disorder), controlling for gender and length of residence. With dichotomous variables such as gender, an HR less than 1 indicates the risk of a psychiatric disorder is lower, and an HR greater than 1 indicates the risk is higher than their counterpart (in this study, the risk for women compared to men). With continuous variables such as age of immigration and length of residence, an HR less than 1.0 indicates a negative association with a psychiatric disorder, and an HR greater than 1.0 indicates a positive association. In this particular study, because we expected immigrants who came as children and adolescents would be at greater risk for psychiatric disorders, we expected the HR for age of immigration to be less than 1. If the p value for any predictor variable was less than .05, it is very unlikely that the estimate occurred by chance.
TABLE 2.
Hazard Regression Estimates of the Effects of Gender, Age at Immigration, and Length of Residence on Different Lifetime Mental Disorders Among Asian American Immigrants (Derived From Cox Hazards Regression Models)
| Any Affective |
Any Anxiety |
Any Substance |
Any Disorder |
|||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | HR | p | HR | p | HR | p | HR | p |
| Gender | 1.293 | .1565 | 0.958 | .8103 | 0.267 | .0010 | 1.019 | .8858 |
| Length of residence | 0.970 | < .1563 | 0.990 | .6333 | 1.039 | .3702 | 1.003 | .8401 |
| Age at immigration | 0.935 | < .0001 | 0.979 | .0194 | 0.962 | .1443 | 0.965 | < .0001 |
Note. HR = hazard ratio.
Results of Cox proportional hazard regression indicate that age at immigration was a significant predictor of any affective, any anxiety, and any disorders and in the hypothesized direction. Immigrants who came at younger ages evidenced greater risk for these mental disorders than those who immigrated at later ages. Specifically, the HR of having any lifetime affective disorder decreased by 6.5% (100% to 93.5%) as age at immigration increased by on year, controlling for gender and length of residence. Similarly, the HR of any lifetime anxiety disorder decreased by 2.1 % (100% to 97.9%) for every 1-year increase in age at immigration. The risk for any lifetime disorders decreased by 3.5% (100% to 96.5%) as age at immigration increased by 1 year.
Gender is a significant predictor only for lifetime substance abuse disorders. The hazard risk of lifetime substance abuse for women was 73.3% (100% to 26.7%) less than men. Length of residence was not a significant predictor of all the psychiatric disorder categories.
Age of Immigration (Generations) and 12-Month Mental Disorders
A related question is whether age of immigration is associated with current levels of psychiatric disorders. Table 3 presents odds ratios (ORs) derived from a series of logistic regressions that addressed this question. Age of immigration was a significant predictor of a 12-month any affective, any substance abuse, and any disorder. Immigrants who arrived at older ages were significantly less likely to have a 12-month any affective, substance use, and any disorder. Specifically, immigrants who arrived in the United States between 18 and 40 years old (1.0a generation) were significantly less likely to have any affective, any substance abuse, and any disorder than those who arrived between 0 and 12 years old (1.5 generation), controlling for gender and length of residence (OR = 0.28, 0.07, and 0.39, respectively). Immigrants who arrived in the U.S. after the age of 41 years old were significantly less likely to have any affective and any disorder than those who arrived between 0 and 12 years old (1.5 generation; OR = 0.17 and 0.48, respectively). A linear association emerged between age at immigration and any 12-month affective and substance abuse disorder, which indicated that the odds of disorders decreased as the age of immigration increased. Age at immigration was not a significant predictor of 12-month any anxiety disorder. Gender and length of residence were not significant across the different 12-month disorders.
TABLE 3.
Odds Ratio of the Effects of Gender, Age at Immigration, and Length of Residence on Different 12-Month Mental Disorders Among Asian American Immigrants (Derived From Logistic Regression Models)
| Any Affective |
Any Anxiety |
Any Substance |
Any Disorder |
|||||
|---|---|---|---|---|---|---|---|---|
| Characteristic | OR | p | OR | p | OR | p | OR | P |
| Gender | 0.97 | .9282 | 1.02 | .9626 | 0.59 | .4338 | 1.09 | .7613 |
| Length of residence | 0.96 | .0644 | 1.02 | .1452 | 0.98 | .2307 | 1.00 | .8376 |
| Age at immigration (years) | ||||||||
| 0 to 12 (1.5 gen.) | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| 13 to 17 (1.25 gen.) | 0.56 | .3447 | 1.49 | .3585 | 0.15 | .1522 | 0.58 | .2241 |
| 18 to 40 (1.0a gen.) | 0.28 | .0060 | 0.65 | .2638 | 0.07 | .0175 | 0.39 | .0079 |
| 41+ (1.0b gen.) | 0.17 | .0392 | 1.27 | .5030 | — | — | 0.48 | .0237 |
Note. OR = odds ratio; gen. = generation.
Age of Immigration (Generations) and the Occurrence of Mental Disorders
We next examined whether different generations are particularly disadvantaged by mental health problems prior to their arrival in the United States. To address this issue, we compared the age of onset of disorders with the age of immigration as reported by the interviewees. In analyses not shown here, we found a linear association between generation and disorders prior to arrival—the percentage of disorders prior to arrival increased as the age of immigration increased. This pattern was across all disorders with the most distinct differences in any, affective, and substance-abuse disorders. This pattern makes intuitive sense because the age of onset for many major disorders occur during adolescence and early adulthood, but this initial finding does highlight that some immigrant groups disproportionately suffer from mental health problems prior to their arrival in the United States. Moreover, these problems may serve as a significant disadvantage for individuals as they establish social and other types of relationships, find jobs, establish residency, and learn the intricacies of a new lifestyle.
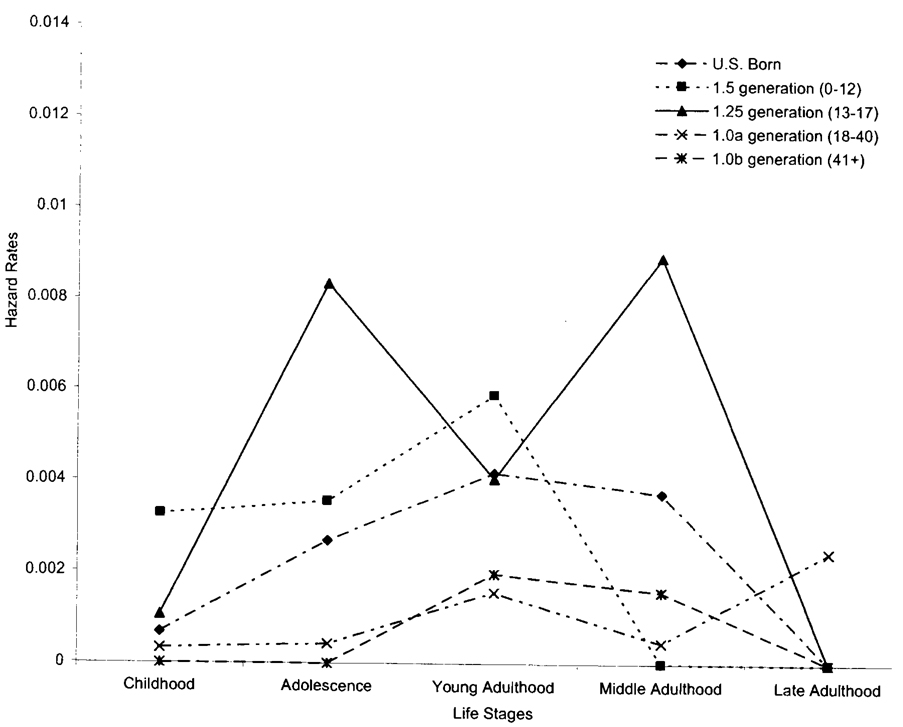
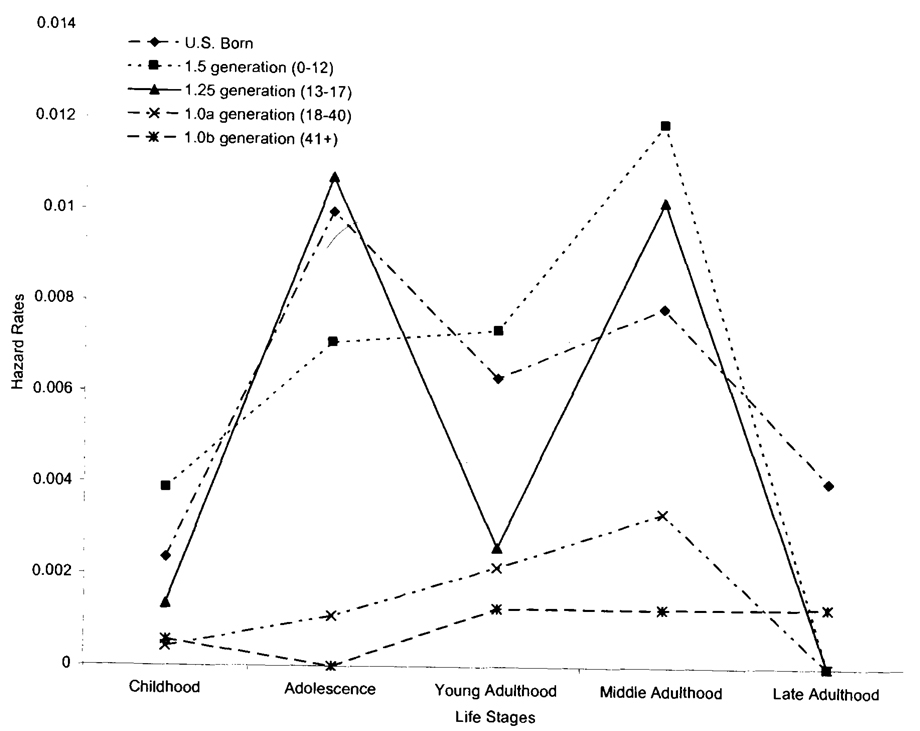
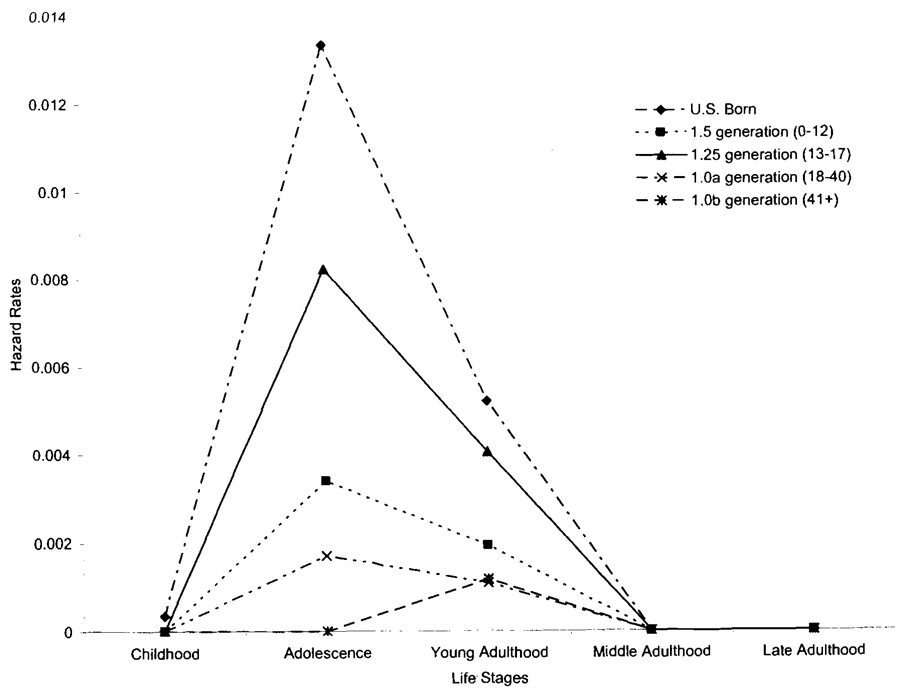
We examined this issue in more detail using the life table survival analysis that shows the hazard rates, defined as the probability that respondents with no prior psychiatric disorders at the beginning of the certain developmental life stage will experience a psychiatric disorder in that life stage (i.e., childhood, adolescence, young adulthood, middle adulthood, or late adulthood). Because we have four different categories of disorders and gender is an important factor in these patterns, there are eight possible graphs to show our findings. We reduced this number to show three figures that capture our major findings. We present the line graphs to show the hazard rates for lifetime affective disorders for men and women and substance disorders for men across the developmental life stages. Findings for the other graphs are similar to the results reported here. The next three figures were constructed by applying the age-specific hazard rates of having a first episode in a given period of time, reducing the bias associated with the respondent’s age.
U.S.-born men show their greatest risk for affective disorders occurring during young and middle adulthood (see Figure 1). One striking observation across immigrant generations is that the risk period for affective disorders occurred at the life stage during or immediately after immigration. The 1.5 generation who came to the United States during childhood have had a higher hazard rate for affective disorders at childhood than the U.S.-born men. Their risks for affective disorders have continued through young adulthood. The 1.25 generation had a high hazard rate during adolescence or during the time of their immigration to the United States. Their risk for affective disorders was lowered in young adulthood but increased dramatically during middle adulthood. The 1.0a generation experienced a high risk for affective disorders at the immigration during young adulthood and then a decreased risk in middle adulthood, and an elevated risk in late adulthood. The 1.0b generation of men had a different pattern for affective disorders. They were the only group of immigrant men to have shown the greatest risk for affective disorder before they immigrated to the United States. This elevated risk was maintained during immigration and was substantially reduced in late adulthood.
FIGURE 1.
Survival analyses for lifetime affective disorders by generation (men).
Figure 2 highlights the hazard rates for affective disorders among women. U.S.-born women were at greatest risk for affective disorders during adolescence and a second risk period during middle adulthood. Like immigrant men, immigrant Asian women showed a greater risk for affective disorders during or shortly after their immigration to the United States. The 1.50 generation of women had a higher risk for affective disorders during childhood. Their risks continued through adolescence and young adulthood and peaked during middle adulthood. Immigrant women who came to the United States as adolescents had their greatest risk for affective disorders during adolescence. They showed a decreased risk in young adulthood and an elevated risk during middle adulthood. The 1.0a generation also had the greatest risk for affective disorders during the period of their immigration. Similar to immigrant men, the 1.0b generation of Asian women was the only generation to have shown a higher risk for affective disorders prior to their immigration to the United States.
FIGURE 2.
Survival analyses for lifetime affective disorders by generation (women).
As indicated earlier, the results for anxiety and any disorders were similar to the findings on affective disorders. Results on substance-abuse disorders showed an entirely different pattern. Because women have low rates of substance-abuse disorders, we only show the findings for Asian American men (Figure 3). It is clear from that the greatest risk for substance abuse disorders for U.S.-born and immigrant men occurred during adolescence. U.S.-born men had the highest risk for substance abuse during adolescence followed by the 1.25 and 1.50 generations, respectively. The risk for the onset of substance-abuse disorders was reduced substantially in young adulthood and was nonexistent in latter stages of life. The older generations, 1.0a and 1.0b, experience the greatest risk for substance abuse in the life stage prior to immigration.
FIGURE 3.
Survival analyses for lifetime substance-abuse disorders by generation (men).
DISCUSSION
Our findings reveal that age of immigration is linked to lifetime and 12-month rates of psychiatric disorder: Immigrants who arrived earlier in life were more likely to have both lifetime and 12-month disorders. U.S. born and immigrants who arrived as children (1.50 generation) were much more likely to have a mental disorder in their lifetimes than other immigrant generations. Equally compelling are the data on the occurrence of these mental disorders among immigrants. Immigrants who arrived as older adults (1.0b) were far more likely to have the onset of their disorders before they arrived in the United States. Finally, immigrants who came as children and adolescents were far more likely to have substance abuse disorders after they arrived in the United States.
A compelling finding is that except for the 1.0b generation, the period during and shortly after immigration were critical times for the onset of different psychiatric disorders. Despite the commonality that they came to the United States prior to their 18th birthday, generations 1.50 and 1.25 showed a slightly different risk for any affective disorders. Generation 1.50 men and women had a greater risk for different psychiatric disorders, with the exception of substance abuse, during childhood than U.S.-born individuals; and, their risk for psychiatric disorders, including substance abuse, increased during adolescence. The 1.25 generation of men and women were especially at risk for all psychiatric disorders during adolescence, a time when they immigrated to the United States. Our analyses are unable to explain why the differences in the onset of psychiatric disorders occurred between generations. Subsequent studies can more directly test how similarities in social status, social relationships, and English speaking abilities mediate or moderate the association between generations and mental health.
Although childhood, adolescence, and early adulthood are important developmental periods for most people, they are especially critical for immigrants who come as children or adolescents. Immigrants who arrive as children may face unique challenges from their school and friendship networks that may be qualitatively different from those presented by their family. For example, they may need to learn and negotiate different social norms, cultural beliefs, and values to adjust to new friendship networks, and at the same time, they must maintain their social and cultural attachments with their families. In addition, early developmental periods are associated with high risk for a range of psychiatric disorders including substance abuse because immigrant children and adolescents have the potential to be involved in social networks that have greater access and opportunity to engage in these behaviors. Certainly more research is needed to identify the social, cultural, and institutional factors that make these periods as risky for psychiatric problems. Moreover, the development of programs targeting the 1.50 and 1.25 generations appears essential to prevent the onset of serious mental disorders.
Our study has several limitations. Although this is the first national study of Asian Americans, we decided to include relatively large samples of certain Asian ethnic groups (e.g., Chinese, Vietnamese, and Filipino). Asian ethnic groups such as Korean, Cambodian, and Indian are included in the other Asian category. This sampling strategy provides a practical means for establishing a national estimate of psychiatric disorders for Asian Americans, but we are unable to do more detailed analyses with the other Asian ethnic category. We are unable to conduct separate sets of life table survival analyses by ethnicity because the sample sizes are too small. Second, we focused primarily on Western expressions of psychiatric disorders as defined by the DSM–IV. Although this strategy provides us with a useful means to compare mental disorders using the same measure, we may be underestimating rates of the problem, especially if immigrants express their problems in unique ways that are not captured by the DSM–IV. Reliance on the DSM–IV also constrains our analyses in that we cannot examine the possible effects of developmental contexts of immigration on more culturally nuanced or culturally specific disorders that may be manifested in Asian American populations (e.g., neurasthenia). Third, the data used in these analyses came from a cross-sectional survey, and we are unable to determine the processes by which immigration reduces or enhances the risk for different mental disorders. Despite these limitations, our analyses on generations suggest that timing and sequencing of events related to immigration are potentially powerful factors in understanding the distribution of mental disorders. Although longitudinal studies can better capture the timing and sequencing of critical events, cross-sectional studies can still do a better job of conceptualizing the factors that enhance the transition from immigration to engagement in a different geographic location.
Much of the work on immigration and mental health has tended to use means or variable-based analyses such as regression analyses. These analyses typically assess whether a particular variable—such as length of residence, ethnicity, or age of immigration—reduces or explains away the difference between immigrants and U.S.-born individuals in mental health outcomes. To complement this approach, it may be useful to incorporate more dynamic analytic models that view age of arrival as an “unfolding” event in which earlier events can prime the causal influence of subsequent events and occurrences (Thoits, 1995). The use of dynamic models will allow one to examine the possibility that immigration may actually lead to the identification of multiple trajectories or pathways. Using developments of an event-centered paradigm coming from historical sociology (Abbott, 1992), human development (Singer & Ryff, 2001), and other fields, researchers may better capture the meaningful events, conditions, and actions that produce well-being or mental illness.
Contributor Information
David T. Takeuchi, University of Washington
Seunghye Hong, University of Washington.
Krista Gile, University of Washington.
Margarita Alegría, Cambridge Health Alliance and Harvard Medical School.
REFERENCES
- Abbott A. From causes to events. Sociological Research and Methods. 1992;20:428–455. [Google Scholar]
- Alegría M, Takeuchi D, Canino G, Duan N, Shrout P, Meng X-L, et al. Considering context, place and culture: The National Latino and Asian American Study. International Journal of Methods in Psychiatric Research. 2004;13:208–220. doi: 10.1002/mpr.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Vila D, Woo M, Canino G, Takeuchi D, Vera M, et al. Cultural relevance and equivalence in the NLAAS instrument: Integrating etic and emic in the development of cross-cultural measures for a psychiatric epidemiology and services study of Latinos. International Journal of Methods in Psychiatric Research. 2004;13:270–288. doi: 10.1002/mpr.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Angel JL, Buckley CJ, Sakamoto A. Duration or disadvantage? Exploring nativity, ethnicity, and health in midlife. The Journals of Gerontology. 2001;56B:S275–S284. doi: 10.1093/geronb/56.5.s275. [DOI] [PubMed] [Google Scholar]
- Breslau J, Chang D. Psychiatric disorders among foreign-born and US-born Asian Americans in a US national survey [Electronic version] Social Psychiatry and Psychiatric Epidemiology. 2006;127 doi: 10.1007/s00127-006-0119-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chun KM, Organista PB, Marin G, editors. Acculturation: Advances in theory, measurement, and applied research. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- Cox DR, Oakes D. Analysis of survival data. New York: Chapman & Hall; 1984. [Google Scholar]
- Escobar J, Vega W. Mental health and immigration’s AAAs: Where do we go from here? Journal of Nervous & Mental Disease. 2000;188:736–740. doi: 10.1097/00005053-200011000-00003. [DOI] [PubMed] [Google Scholar]
- Fuligni AJ. Convergence and divergence in the developmental contexts of immigrants to the United States. In: Schaie W, Elder G, editors. Historical influences on lives and aging. New York: Springer; 2005. pp. 89–98. [Google Scholar]
- Gater R, Tnasella M, Korten A, Tiemens BG, Mavreas VG, Olatawura MO. Sex differences in the prevalence and detection of depressive and anxiety disorders in general health care settings. Archives of General Psychiatry. 1998;55:405–413. doi: 10.1001/archpsyc.55.5.405. [DOI] [PubMed] [Google Scholar]
- Granovetter M. The strength of weak ties. American Journal of Sociology. 1973;78:1360–1380. [Google Scholar]
- Heeringa SG, Wagner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES) International Journal of Methods in Psychiatric Research. 2004;13:221–240. doi: 10.1002/mpr.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang W, Chun C, Takeuchi D, Myers H, Siddarth P. Age of first onset major depression in Chinese Americans. Cultural Diversity and Ethnic Minority Psychology. 2005;11:16–27. doi: 10.1037/1099-9809.11.1.16. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distribution of DSM–IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM–IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, et al. Lifetime and 12-month prevalence of DSM–III–R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kish L. Survey sampling. New York: Wiley; 1965. [Google Scholar]
- Landale NS, Oropesa RS, Gorman BK. Migration and infant death: Assimilation or selective migration among Puerto Ricans? American Sociological Review. 2000;65:888–909. [Google Scholar]
- Laumann EO, Pappi FU. Networks of collective action: A perspective on community influence systems. New York: Academic; 1976. [Google Scholar]
- Lee ET. Statistical methods for survival data analysis. New York: Wiley; 1992. [Google Scholar]
- Linzer M, Spitzer R, Kroenke K, Williams JB, Hahn S, Brody D, et al. Gender, quality of life and mental disorders in primary care: Results from the PRIME-MD 1000 study. American Journal of Medicine. 1996;101:526–533. doi: 10.1016/s0002-9343(96)00275-6. [DOI] [PubMed] [Google Scholar]
- Pennell BE, Bowers A, Carr D, Chardoul S, Cheung G-Q, Dinkelmann K, et al. The development and implementation of the National Comorbidity Survey Replication, the National Survey of American Life, and the National Latino and Asian American Survey. International Journal of Methods in Psychiatric Research. 2004;13:241–269. doi: 10.1002/mpr.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccinelli M, Homen FG. Geneva, Switzerland: World Health Organization; Gender differences in the epidemiology of affective disorders and schizophrenia. 1997
- Research Triangle Institute (RTI) International. SUDAAN (Version 9.0.0) Research Triangle Park, NC: 2004. [Google Scholar]
- Rumbaut RG. Assimilation and its discontents: Ironies and paradoxes. International Migration Review. 1999;31:923–960. [PubMed] [Google Scholar]
- Rumbaut R. Ages, life stages, and generational cohorts: Decomposing the immigrant first and second generations in the United States. International Migration Review. 2004;38:1160–1205. [Google Scholar]
- Rumbaut RG, Weeks JR. Unraveling a public health enigma: Why do immigrants experience superior perinatal health outcomes? Research in the Sociology of Health Care. 1996;13B:337–391. [Google Scholar]
- Salant T, Lauderdale DS. Measuring culture: A critical review of acculturation and health in Asian immigrant populations. Social Science & Medicine. 2003;57:71–90. doi: 10.1016/s0277-9536(02)00300-3. [DOI] [PubMed] [Google Scholar]
- Shuval J. Migration and stress. In: Golberger L, Breznitz S, editors. Handbook of stress: Theoretical and clinical aspects. New York: Free Press; 1982. pp. 677–691. [Google Scholar]
- Singer BH, Ryff CD. New horizons in health: An integrative approach. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- StatSoft. Inc. Electronic statistics textbook. Tulsa, OK: Statsoft; 2006. Survival/failure time analysis. Retrieved June 9, 2006, from http://www.statsoft.com/textbook/stsurvan.html. [Google Scholar]
- Takeuchi DT, Chung RC, Lin KM, Shen H, Kurasaki K, Chun C, et al. Lifetime and twelve-month prevalence rates of major depressive episodes and dysthymia among Chinese Americans in Los Angeles. American Journal of Psychiatry. 1998;155:1407–1414. doi: 10.1176/ajp.155.10.1407. [DOI] [PubMed] [Google Scholar]
- Thoits P. Stress, coping and social support processes: Where are we? What next? Journal of Health and Social Behavior. 1995;35(Extra Issue):53–79. [PubMed] [Google Scholar]
- Williams DR, Collins C. U.S. socioeconomic and racial differentials in health: Patterns and explanations. Annual Review of Sociology. 1995;21:349–386. [Google Scholar]
- Wittchen HU. Reliability and validity studies of the WHO Composite International Diagnostic Interview (CIDI): A critical review. Journal of Psychiatric Research. 1994;28:57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Department of Mental Health and Substance Dependence; Gender disparities in mental health. (n.d.). Retrieved September 18, 2006, from http://www.who.int/mental_health/media/en/242.pdf.
- World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Journal of American Medical Association. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- Zeng Z, Xie Y. Asian-Americans’ earnings disadvantage reexamined: The role of place of education. The American Journal of Sociology. 2004;109:1075–1108. [Google Scholar]