Abstract
Background
The worksite represents a promising venue in which to address the issue of obesity.
Design
Pair-matched, cluster-RCT. Data were collected from 2005 to 2008 and analyzed in 2008.
Setting/Participants
A random sample of 806 employees was selected to represent the workforce of six hospitals in central Massachusetts.
Intervention
The 2-year ecologic intervention sought to prevent weight gain through changes in worksite weight-related norms using strategies targeted at the organization, interpersonal environment and employees.
Main outcome measures
The primary outcome was change in BMI at 12- and 24-month follow-up. Change in perceptions of organizational commitment to employee health and normative coworker behaviors were secondary outcomes.
Results
There was no intervention impact on change in BMI from baseline to 12 (β=0.272; 95% CI= −0.271–0.782) or 24 months (β=0.276; 95% CI= −0.338, 0.890) in intention-to-treat analysis. Using intervention exposure (scale=0 to 100) as the independent variable, there was a decrease of 0.012 BMI units (95% CI= −0.025–0.001) for each unit increase in intervention participation at 24-month follow-up. Employees in intervention sites reported significantly greater improvements in perceptions of organizational commitment to employee health at 12 and 24 months compared to control sites, but there was no impact on perceptions of normative coworker behaviors.
Conclusions
The intervention had a dose–response relationship with BMI, with positive effects proportional to extent of participation. While the intervention was successful at changing organizational perceptions, successfully improving changes in actual and perceived social norms may be required to achieve population-level impact in complex worksite organizations.
Introduction
The overweight/obesity epidemic is resulting in profound health consequences.1,2,3,4 Approximately two thirds of U.S. adults are overweight or obese,5 with an alarming increase in rate over recent decades.6 Most U.S. adults gain 1 to 2 pounds per year.7 Curbing this gradual increase could hinder the continually climbing overweight/obesity prevalence,8 with tremendous public health impact.
Numerous weight loss and weight gain prevention interventions have been developed. Psychosocial and cognitive–behavioral strategies targeted at individuals have had limited success in reaching large segments of the population and sustaining long-term outcomes.9,10 Ecologic frameworks emphasize that behavior is influenced by psychological and cognitive factors and its environmental context.11,12 Interventions incorporating multilevel strategies guided by ecologic frameworks are increasingly common and hold promise for reducing the obesity epidemic.13,14
The worksite is a promising setting for weight gain prevention interventions.15,16 These may be attractive to employers17 hoping to reduce direct medical care and health insurance costs, absenteeism and disability claims, and to improve productivity.18–24 Most working age adults spend the majority of most days at work, allowing large segments of the population to be reached.25 Common systems for communication, education and support present opportunities for the introduction, adoption and maintenance of healthy behaviors.26
Recognizing the potential of worksite-based weight gain prevention interventions, the National Heart Lung and Blood Institute (NHLBI) launched a special initiative Overweight and Obesity Control at Worksites.27 It funded seven worksite projects nationwide to test the effectiveness of ecologically based interventions at preventing and reducing overweight and obesity. This paper describes the results of one of these projects, the Step Ahead trial, which tested the effectiveness of a multilevel intervention on weight gain prevention among hospital employees. This study also investigates the relationship of participation in intervention activities with weight gain prevention and the effectiveness of the intervention on change in measures of the ecologic conceptual framework.
Methods
Objectives and Hypotheses
The study goal was to test the effectiveness of a worksite intervention on weight gain prevention. The hypothesis was that the intervention would prevent weight gain among employees at intervention hospitals, while employees at control hospitals would gradually gain weight at a rate consistent with the national adult population. The trial was designed with 80% power to detect a minimum difference of .5 BMI units between employees in the intervention site and those in the control site at a two-sided alpha level of .05, accounting for number of clusters.
Study Design
The study was conducted at six member hospitals of the largest healthcare system in central Massachusetts. The study used a cluster-randomized design in which the unit of randomization was the hospital and the unit of analysis was the individual employee. Hospitals were matched into pairs according to size and level of service. Within each matched pair, one site was randomized as an intervention site and one as a control. Overall, 6,910 employees worked at the six hospitals at least 20 hours per week in January, 2005. The study received approval from the University of Massachusetts Medical School IRB, covering all participating hospitals. Data collection occurred from 2005 to 2008. The intervention was implemented from 2006 to 2008. Analyses were conducted in 2008.
Study Cohort and Recruitment
An employee cohort was selected to determine the effectiveness of the site-based intervention at the individual level. The cohort was intended to represent the employee population. Random samples from human resources records of each hospital were drawn, stratified by gender and minority status. A random sample was selected from each stratum, with oversampling of male and minority employees, ensuring the ability to perform subgroup analysis by gender and race/ethnicity in a predominantly female and non-Hispanic white workforce.
A study invitation letter signed by the Principal Investigator and the hospital president was sent to targeted employees' work addresses. Letters in both Spanish and English were sent to employees listed as Hispanic in human resources records. The letter invited participation in a study to test ways of preventing weight gain in employees, described how they were selected and provided telephone and e-mail contact information to set up an initial visit, ask questions or refuse participation. Enrollment was completed in scheduled drop-in sessions or individual appointments. IRB approval required that project staff attempt additional contact only by work telephone, pager or mail following a standardized protocol. To enroll housekeeping employees, who lacked work mailboxes and telephones, invitations were distributed at time clocks during shift change and study staff made an informational presentation at a staff meeting. Enrollment visits were conducted at all hours of the day/night at the employee's convenience. No special efforts were made to encourage evaluation cohort members to participate in intervention activities.
Cohort members were screened to meet these inclusion criteria: (1) aged 18–65 years, (2) able to understand and communicate in English or Spanish, (3) not planning to leave employment in the next 2 years, (4) working at least 20 hours per week, (5) not working in more than one participating hospital, (6) no impediment to being weighed and measured and (7) not pregnant. A 6-month washout period following study enrollment was included. Employees were excluded if no longer eligible at this time point (e.g., left employment) or they dropped out of the study.
Intervention
People's behavior is influenced by how other members of their cultural and social networks behave and their perceptions of this behavior.28 The intervention was designed to promote organizational and social norms related to healthy eating and physical activity in the worksite. Ecologic frameworks posit that sociocultural and physical environments and individual characteristics influence an individual's behaviors.11,29,30 the intervention targeted organizational and interpersonal norms. At the hospital level, intervention strategies targeted organizational leadership, climate, culture and capacity to promote an environment supportive of weight control and associated behaviors.31 Interpersonal-level intervention strategies focused on work-based relationships and aimed to promote an environment supportive of physical activity and healthy eating within existing social networks.32 Intervention messages aimed to improve employee knowledge, self-efficacy, behavioral capabilities and outcome expectancies, consistent with Social Cognitive Theory.33 The control condition received no intervention.
The intervention was refined based on formative research.34 Intervention hospital employee and leadership advisory committees helped develop site-tailored strategies. Each strategy lasted the entire 2-year period.
A social marketing campaign integrated all program activities using common logos, themes and messages. Primary sources of project information were a weekly newsletter, a website and an information center with print materials centrally located in each hospital.
Environmental strategies promoting physical activity included stairway signs using messages from CDC's StairWELL campaign35 and additional messages unique to Step Ahead. Signs were placed at elevator waiting areas, stairwell entrances and every stairway landing. Indoor (10 minutes/.5 mile) and outdoor (20 minutes/1 mile) walking routes and maps with mileage and step counts were developed at each site. “Walks with the President” were held whereby groups of employees could take a 20-minute walk on the walking route with the president to meet and chat.
Environmental strategies promoting healthy eating included cafeteria signs noting nutritional information of most food and beverage items. The project dietitian worked with food services staff to provide healthy menu options, defined as whole grains, low saturated fat, lean protein (focusing on fish, chicken, legumes and eggs) and fruits and vegetables. Special cafeteria events were held to coincide with other Step Ahead activities. For example, during a 6-week virtual walk around the Mediterranean Sea (described below), weekly healthy entrees highlighting cuisine of different countries were offered. At two intervention hospitals, a weekly seasonal Farmers' Market was held. Permission for a Farmers' Market was not obtained from hospital leadership at the third intervention site.
Strategies promoting interpersonal support included periodic campaigns and challenges targeting physical activity, healthy eating and weight maintenance and loss. For one, a virtual walk around the Mediterranean Sea, groups/individuals submitted time or total number of steps taken, on a paper log or by email, weekly for 6 weeks. These were converted into miles, and hospital-wide progress was mapped and displayed at the Step Ahead information center, described below. Group and individual prizes were given. Interpersonal support and group activity also were promoted by toolkits for Walking Groups and Healthy Potlucks.
A display and workshop series, a weekly newsletter, recipe books and other print materials were developed as strategies targeting individual knowledge, skills and behaviors. Displays were set up at least weekly at each hospital cafeteria and lobbies during meals and between shifts, at the Farmers' Market and at events for hospital employees, such as benefits fairs and immunization clinics. Each display focused on one topic, such as “Quick and Healthy Dinners”, “Moving Indoors” and “Healthy Holidays”. A 30-minute workshop focusing on strength training was conducted monthly. A simple 10-minute routine with an illustrated handout and a resistance band were provided. A weekly one-page newsletter was distributed by e-mail, on the website and at information centers. It included an article on a healthy weight-related topic, a recipe and a quick tip on incorporating healthy eating and physical activity into daily routines. Seasonal recipe books and print handouts were available on the website, at information centers and at workshops and displays.
Data Sources and Measures
Employee cohort members completed assessments at baseline, 12-month follow-up and 24-month follow-up. Assessments occurred in meeting rooms or private offices at worksites before or after work, or during scheduled breaks. Assessments were conducted at all day/night hours to accommodate all shifts. Data sources included human resources records, anthropometric measurements, and a 30-minute self-administered survey which was either completed at the time of anthropometric measurements or returned via mail. Employees received a $20 giftcard for completing each measurement time point. No efforts were made to contact those no longer working at the hospitals at follow-up.
The primary outcome measure was change in BMI. Weight measurements were taken by trained staff using portable digital scales with readings to the nearest 2/10th pound. Heights were measured to the nearest 1/8th inch using portable stadiometers. Weight and height were converted to metric scale and BMI calculated as weight in kilograms divided by height in meters squared (kg/m2). A secondary outcome measure included a dichotomous indicator of weight gain prevention from baseline to 24-month follow-up (change of 0 kg/m2 or less vs >0 kg/m2.)
Measures of the ecologic conceptual framework were included as potential intervention mediators.36 Employee perception of organizational commitment to employee health was measured by the 4-item subscale of the Worksite Health Climate survey (WHC) (α=88).37 Respondents rated each item on a 5-point scale ranging from strongly disagree to strongly agree. The scale was computed as an average of items. Modified versions of the WHC subscales for health norms measured employee perceptions of eating and physical activity behaviors of coworkers.37 Items were selected and adapted to focus on at-work behavior. Four items asked about coworkers' physical activity behaviors at work and five about coworkers' eating habits at work. Seven response categories (almost none to almost all) estimated the proportion of coworkers who practiced specific behaviors. Negative items were reverse-coded, with higher scores corresponding to healthier behaviors. Each scale was computed as an average. Psychometric testing indicated strong internal consistency (α=78, healthy eating; α=74, physical activity).
Employee characteristics were assessed as potential intervention modifiers. Demographic factors included gender, age group, education, annual household income and race/ethnicity. Job characteristics included shift usually worked and whether the employee's occupation involved direct patient care, a marker of job flexibility. Baseline BMI was categorized as normal weight (BMI <25.0 kg/m2), overweight (BMI 25.0–29.9 kg/m2) or obese (BMI >= 30.0 kg/m2).
At the two follow-up assessment points, a survey was administered to intervention site participants assessing participation in Step Ahead activities. Ten major intervention strategies were assessed: stairway signs, cafeteria signs, Farmers' Markets, walking groups, challenges, workshops and educational displays, newsletters, project website, project information center and print materials. For each, participants were asked if they were aware of the strategy and if so, how often they used it on a 5-point scale. Individual measures were summed across study years, giving each a range of 0–10. A summary variable of intervention participation was created by summing the individual measures. The variable had a possible range of 0 to 100, with higher scores indicating greater participation.
Statistical Analysis
Data were analyzed using survey procedures in Stata version 10.1 (College Station, Texas). All analyses were weighted to reflect the workforce population with respect to age, gender, race/ethnicity and occupation, accounting for the probability sampling design and probability of participants being retained at the 12- and 24-month follow-ups due to loss to follow-up. Survey linear regression models were used to estimate the effect of the intervention on BMI, employee perception of organizational commitment to employee health, and employee perceptions of coworker normative physical activity and dietary behaviors, while accounting for the complex sampling design. For all outcomes, both time-specific and annualized intervention effects were determined. The intervention effect was estimated for the overall study population and subgroups. Intervention effects across subgroups were compared. Models adjusted for gender, age, race/ethnicity, education, occupation, shift, and hours worked per week.
Classification and regression tree (CART) analysis38–40 was used to compare rates of weight gain prevention across segments of the workforce that were unique, mutually exclusive and exhaustive with respect to intervention participation among employees in intervention sites. Stopping rules imposed include a minimum Gini improvement measure of .001, a maximum of independent variables per terminal node of 5 and a minimum of 200 employees (of the total workforce) per terminal node. The 10 intervention participation measures were considered as independent variables. SPSS Answer Tree 2.0 software was used. The CART groups identified were then compared according to employee characteristics using contingency tables and chi-square statistics.
Results
Enrollment and Retention Rates
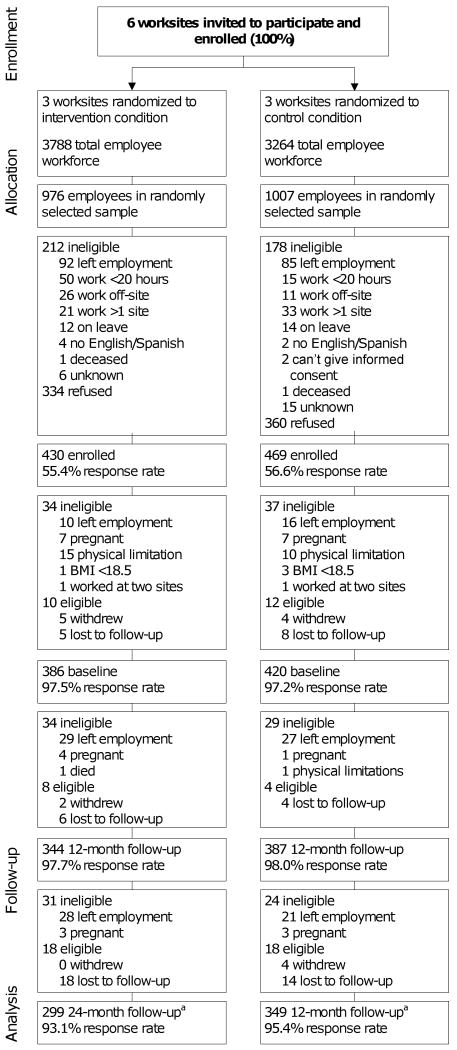
Figure 1 presents study enrollment and retention. All six invited hospitals participated. The baseline response rate was 56% of eligible participants. Compared to participants, nonparticipants were more likely to be physicians (35.1% vs 58.1% for all other occupations) and men (51.1% vs 59.3% for women). Reasons given for not participating were lack of interest (56.3% of refusers), no time (19.4%) and personal health or family obligations (2.0%), with 22.4% giving no reason. The 24-month retention rate was 80% among all enrolled participants (648/806). The primary reason for loss to follow-up was no longer being employed (105/158). The 24-month retention rate among those who remained eligible was 94% (648/688). There were no significant differences between conditions in response or retention rates.
Figure 1.
Trial flowchart
a 4 were to lost to follow-up at 12 months, but completed the 24-month follow-up.
Study Population
A description of the employee cohort is presented in Table 1. The majority was female, non-Hispanic white and overweight or obese. Compared to control sites, intervention site employees were more likely to be male, to have a graduate degree, to have a household income greater than $75,000 per year and to work second or third shift.
Table 1. Description of employee characteristics by intervention statusa.
| Characteristic | Total Population | Intervention Site Employees | Control Site Employees | P-value |
|---|---|---|---|---|
| (n=806) | (n=386) | (n=420) | ||
| Gender | <.0001 | |||
| Female | 81.0% | 78.3% | 84.2% | |
| Male | 19.0% | 21.7% | 15.8% | |
| Age | .65 | |||
| 18–40 | 35.2% | 35.2% | 35.3% | |
| 41–50 | 33.4% | 31.8% | 35.2% | |
| 51+ | 31.4% | 33.0% | 29.5% | |
| Race/Ethnicity | .18 | |||
| Asian/Other | 1.4% | 1.7% | 1.1% | |
| Hispanic | 5.3% | 5.9% | 4.7% | |
| Non-Hispanic black | 4.7% | 4.1% | 4.8% | |
| Non-Hispanic white | 88.8% | 88.3% | 88.3% | |
| Education | .04 | |||
| High school or less | 13.0% | 10.8% | 15.6% | |
| 1–3 years post high school | 46.3% | 45.5% | 47.4% | |
| College degree | 26.6% | 25.8% | 27.5% | |
| Graduate degree | 14.1% | 17.9% | 9.5% | |
| Annual Household Income | <.0001 | |||
| < $45,000 | 21.6% | 22.1% | 21.0% | |
| $45,000–75,000 | 21.5% | 22.8% | 19.9% | |
| $75,000-$100,000 | 19.3% | 15.3% | 23.9% | |
| ≥ $100,000 | 37.7% | 39.8% | 35.2% | |
| Shift | .05 | |||
| First/Split | 71.8% | 69.0% | 75.1% | |
| Second | 11.6% | 10.7% | 12.6% | |
| Third/Mixed | 16.6% | 20.3% | 12.3% | |
| Patient care–based occupation | .48 | |||
| Yes | 63.7% | 64.8% | 62.4% | |
| No | 36.3% | 35.2% | 37.6% | |
| Baseline BMI | .47 | |||
| < 25.0 kg/m2 | 34.5% | 36.9% | 31.6% | |
| 25.0–29.9 kg/m2 | 31.0% | 30.1% | 32.0% | |
| ≥ 30.0 kg/m2 | 34.6% | 33.0% | 36.4% |
Weighted to represent the hospital workforce population.
Intervention Participation
As reported in Table 2, the most commonly utilized activities were stairway and cafeteria signs and weekly newsletters, while the project website and participation in project challenges and walking groups were least frequently utilized.
Table 2.
Participation in intervention strategies among intervention condition employees (n=806).
| Participation in intervention strategies in the past 12 months | Time point | |
|---|---|---|
| 12 months (%) | 24 months (%) | |
| How often read stairway signs | ||
| Never noticed | 22.3 | 21.9 |
| Read never or occasionally | 5.8 | 6.9 |
| Read sometimes | 22.5 | 24.0 |
| Read frequently | 49.5 | 47.4 |
| How often read cafeteria signs | ||
| Never noticed | 32.1 | 26.3 |
| Read never or occasionally | 23.9 | 18.8 |
| Read sometimes | 23.7 | 28.4 |
| Read frequently | 20.2 | 26.5 |
| How often attended Farmers' Market | ||
| Never | 60.6 | 56.3 |
| Once per month or less | 33.2 | 20.6 |
| More than once per month | 17.3 | 23.2 |
| Ever participated in a walking group | ||
| No | 86.9 | 85.8 |
| Yes | 13.1 | 14.2 |
| Ever participated in a challenges or contests | ||
| No | 89.1 | 84.5 |
| Yes | 10.9 | 15.5 |
| Number of workshops and displays attended | ||
| Never | 46.8 | 47.6 |
| 1–2 | 21.7 | 22.2 |
| 3–4 | 17.8 | 14.3 |
| 5+ | 13.7 | 15.9 |
| How often read newsletter | ||
| Not familiar | 46.1 | 35.7 |
| Less than monthly | 19.9 | 18.0 |
| ≥ Monthly, < weekly | 16.2 | 26.3 |
| Weekly | 17.7 | 20.0 |
| How often visited project website | ||
| Not familiar | 73.5 | 59.2 |
| Less than monthly | 14.4 | 26.4 |
| ≥ Monthly, < weekly | 3.9 | 4.5 |
| Weekly or more often | 8.1 | 9.9 |
| How often visited project information center | ||
| Not familiar | 38.1 | 26.2 |
| Less than monthly | 47.8 | 41.9 |
| ≥ Monthly, < weekly | 9.3 | 19.0 |
| Weekly or more often | 4.8 | 12.9 |
| How often read project print materials | ||
| Not familiar | 38.1 | 26.2 |
| Less than monthly | 47.8 | 41.9 |
| ≥ Monthly, < weekly | 9.3 | 19.0 |
| Weekly or more often | 4.8 | 12.9 |
| Mean intervention participation score (SE) | 15.8 (.76) | 18.1 (.86) |
| Median intervention participation score (IQR) | 14 (8–23) | 16 (9–26) |
Effect of the Intervention on Weight Gain Prevention
There was no intervention impact on change in BMI. The estimated group difference in change in BMI was .272 (95% CI= −.271–.782) from baseline to 12 months and .276 (95% CI= −.338–.890) from baseline to 24 months (Table 3). Average adjusted BMI in the intervention and control conditions were 28.4 and 29.0 at baseline, 28.7 and 29.1 at 12 months and 28.9 and 29.4 at 24 months, respectively. There were also no differences observed in each of the modifying variables examined (data not shown).
Table 3. Difference between intervention and control conditions in change in BMI (n=806)a,b.
| 12-month | 24-month | |||||||
|---|---|---|---|---|---|---|---|---|
| Change per unit (t-score) | 95% CI | Change per unit (t-score) | 95% CI | |||||
| Lower | Upper | P-value | Lower | Upper | P-value | |||
| Group difference in change in BMI (intention-to-treat analysis) | .272 (0.98) | −.271 | .816 | .33 | .276 (0.88) | −.338 | .890 | .38 |
| Intervention participation (per unit: range 0–100) (Dose–response analysis) | −.013 (−1.27) | −.032 | .007 | .21 | −.012 (−1.81) | −.025 | .001 | .06 |
Adjusted for gender, age, race/ethnicity, education, job category, shift, and hours worked per week.
Weighted to represent the hospital workforce population.
Analysis examining the association of extent of intervention participation with change in BMI suggested a relationship. For each unit increase in intervention participation (range: 0–100), there was a decrease of .012 BMI units (95% CI= −.025–.001; p=.06) from baseline to 24 months. The threshold of intervention participation associated with weight gain prevention was computed by dividing .5 (the hypothesized detectable BMI unit) by the observed regression coefficient of .012, which equals 41.7 (data not shown). This indicated that in order to achieve the intervention weight gain prevention benefits, an individual would need an intervention participation score of 41.7 or greater, of a possible 100 (mean sum of 12- and 24-month scores=33). This was reported by approximately 27% of the workforce.
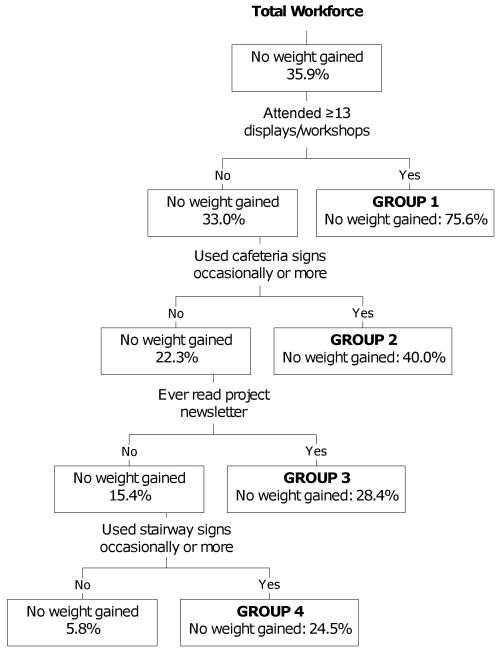
The CART analysis among intervention condition employees found five patterns of intervention participation associated with likelihood of no weight gain at 24 months (Figure 2). The five patterns, from those most likely to prevent weight gain to those least likely to prevent weight gain were (1) frequent utilizers of displays and workshops (6.9% of the workforce), (2) frequent readers/users of cafeteria nutritional signs and information (56.4% of the workforce), (3) reading study newsletters (19.7% of the workforce), (4) frequent readers/users of stairway signs (8.7% of workforce) and (5) infrequent users of each intervention strategy (8.3%). There were significant differences among the five CART groups on all demographic and work-related measures (Table 4). The group most likely to prevent weight gain (group 1) was characterized by a higher proportion of employees who were non-Hispanic white, aged >50 years, of higher educational and income level, obese, worked first shift and had no patient care responsibilities. The group least likely to prevent weight gain (group 5) included a higher proportion of employees who were nonwhite, middle aged (41–50 years), of lower educational and income level and worked second or third shift.
Figure 2.
Classification tree results
Table 4. Description of employees according to CART group (n=806)a.
| Intervention Utilization Groups Determined by CART Analysis | ||||||
|---|---|---|---|---|---|---|
| Characteristic | Frequent workshop/display attendees (%) | Infrequent workshop/display attendees; Frequent cafeteria sign readers (%) | Infrequent workshop/display attendees and cafeteria sign readers; Frequent newsletter readers (%) | Infrequent workshop/display attendees and cafeteria sign and newsletter readers; Frequent stair sign readers (%) | Infrequent workshop/display attendees and cafeteria sign, newsletter and stair sign readers (%) | p value |
| Gender | <.001 | |||||
| Female | 83.0 | 74.6 | 79.4 | 80.8 | 87.3 | |
| Male | 17.0 | 25.3 | 20.6 | 19.4 | 12.7 | |
| Age | <.001 | |||||
| 18–40 | 6.8 | 33.2 | 47.1 | 24.5 | 29.8 | |
| 41–50 | 23.1 | 34.6 | 26.7 | 21.5 | 46.8 | |
| 51+ | 70.2 | 32.1 | 26.2 | 54.0 | 23.4 | |
| Race/Ethnicity | <.001 | |||||
| Asian/Other | 1.3 | 2.3 | .6 | 1.8 | 2.5 | |
| Hispanic | 5.7 | 5.5 | 6.1 | 2.7 | 9.3 | |
| Non-Hispanic black | 1.3 | 5.2 | 3.2 | 0 | 7.0 | |
| Non-Hispanic white | 91.8 | 87.1 | 90.1 | 95.5 | 81.2 | |
| Education | <.001 | |||||
| High school or less | 1.3 | 10.4 | 10.6 | 18.8 | 13.3 | |
| 1–3 years post high school | 54.7 | 42.4 | 45.0 | 55.3 | 49.6 | |
| College degree | 28.0 | 21.8 | 29.3 | 22.0 | 34.1 | |
| Graduate degree | 16.0 | 25.3 | 15.2 | 3.9 | 3.0 | |
| Annual household income | <.001 | |||||
| < $45,000 | 11.6 | 20.6 | 21.6 | 14.2 | 34.9 | |
| $45,000–75,000 | 43.1 | 20.5 | 16.5 | 38.4 | 9.9 | |
| $75,000-$100,000 | 4.3 | 18.0 | 16.9 | 23.4 | 22.3 | |
| ≥ $100,000 | 40.9 | 40.9 | 45.0 | 24.0 | 32.9 | |
| Shift | <.001 | |||||
| First/Split | 98.7 | 76.3 | 54.6 | 72.1 | 61.3 | |
| Second | 0 | 5.5 | 17.2 | 10.8 | 20.2 | |
| Third/Mixed | 1.3 | 18.2 | 28.2 | 17.1 | 18.5 | |
| Patient care–based occupation | <.001 | |||||
| Yes | 45.3 | 65.5 | 73.2 | 58.9 | 50.1 | |
| No | 54.7 | 34.5 | 26.8 | 41.1 | 49.9 | |
| Baseline BMI | <.001 | |||||
| < 25.0 kg/m2 | 21.2 | 35.0 | 44.3 | 29.7 | 37.8 | |
| 25.0–29.9 kg/m2 | 38.2 | 25.9 | 34.1 | 31.8 | 30.3 | |
| ≥ 30.0 kg/m2 | 40.6 | 39.1 | 21.6 | 38.5 | 32.0 | |
Weighted to represent the hospital workforce population.
Effect of the Intervention on Normative Perceptions
Table 3 reports that the intervention was associated with improved perceptions of organizational commitment to employee health at both 12 months (β=32, 95% CI=.17–.47) and 24 months (β=37; 95% CI=20–.54). There was no effect on employee perceptions of coworker normative physical activity or dietary behaviors.
Discussion
In this study of the effectiveness of an ecologic weight gain prevention intervention at hospital worksites over a 2-year period, no population- or subgroup-level effects on weight gain prevention were observed. The intervention was successful in improving perceptions of organizational commitment but not in changing perceptions of coworker normative behaviors. It is important, however, to consider that changes in normative behavioral practices take time. An example of this is the long history of achieving reduction in tobacco use via individual, social and political processes, which did include numerous worksite initiatives.17 There has been considerable emphasis on weight in mass media. Initiatives are underway in schools and communities, and changes are being made in local community and public policy. 41,42 Education and commitment of the medical community to increase lifestyle change in their patients will also reinforce obesity-related efforts as has happened with other prevention initiatives.25,43 Over time, employer efforts should be an important force in changing normative patterns, as will public policy.41,44,45
A trend was observed toward an association between greater intervention participation and weight gain prevention. The rate of participation was not high enough to result in weight gain prevention at the population level. While employees were aware of Step Ahead branding, notably stairwell and cafeteria strategies, participation rates in more intensive intervention activities were not high. Several reasons may explain this. The study was conducted in a period of intensifying pressure for productivity in hospitals, which may have resulted in high levels of work-related stress and limited freedom to attend intervention activities.17,46 Implementation of hospital wellness programs is challenged by round-the-clock staffing and lack of flexibility in the schedules of clinical workers. People who worked second and third shift were less likely to be frequent attendees of workshops and displays. These were offered at shift change (e.g., 7AM) and at breakfast and dinner hours, but were most frequently offered during lunch hours. Shift workers are also potentially isolated from the prevailing organizational culture and environment. Future interventions specifically targeted at shift workers are important, as shift work is associated with health consequences.47,48 Employees involved in patient care may not have schedule flexibility to participate in some activities, especially in environments promoting efficiency and patient-centered care. For interventions to be successful, employees must have the opportunity to attend.
The CART analyses highlight that the group with the highest rate of weight gain prevention had high levels of participation in intervention workshops and displays, strategies that required the employee's most active participation. Such participation may be driven by individual motivation, but ecologic models emphasize that motivation is further enhanced within a supportive environment.11 These results support the notion that there is no one-size-fits-all solution for controlling weight. The heterogeneity of the workforce may require that multiple types of strategies be required to achieve the necessary engagement of individuals, despite growing perceptions of commitment and norms.49–51
A growing number of studies have incorporated worksite policy and environmental modifications to promote healthy eating and physical activity. 52–56 Strategies such as point-of-purchase information, pricing strategies and availability on food purchases from cafeterias and vending machines have resulted in improvements in purchase and eating of healthy foods.52,53 With respect to physical activity, ecologic approaches that combine on-site access to fitness facilities with individually targeted outreach efforts, such as educational and behavioral skills training programs, have produced increases in physical activity, compared to access alone.54 Although not specific to worksites, research has demonstrated that providing decisional prompt signage promoting use of stairs over elevators and providing attractive stairway environments, such as carpeting, signage or art, and music can promote physical activity.54–56 Despite the potential of these approaches, they had not previously been studied in relation to weight control outcomes. Previous worksite interventions focusing on weight control have largely included multistrategy approaches, such as didactic education and groups, targeting weight loss among volunteers.109 Overall, these approaches have observed modest short-term success. Prior to NHLBI's Overweight and Obesity Control at Worksites initiative, no previous worksite study examined the long-term impact of ecologic interventions targeting weight gain prevention. The Step Ahead intervention incorporated strategies, such as cafeteria and stairway signage, that had previously shown promise in improving behaviors that are associated with weight control, in addition to other strategies promoting social and organizational normative changes. This approach was effective among only people motivated/able to participate. Recent efforts to promote worksite wellness have called for policy approaches that were not included in the Step Ahead intervention, such as monetary compensation and reduced health insurance rates.26 Inclusion of similar policy approaches in the context of a multicomponent intervention may facilitate greater participation than what was observed in this study.
This study has strengths and limitations. While hospitals pose challenges because of organizational complexity, hospitals across the country share similar missions and organizational structures. The employee population was diverse and similar to the overall U.S. population with respect to educational attainment.57 These factors strengthen generalizability. Hospitals are important intervention targets because workers are potential models of healthy lifestyles for patients and the community. Additional strengths are a strong design, including a representative cohort allowing inference to the worksite population and the high retention rate. Study limitations include the low baseline response rate. However, the BMI distribution of the sample was similar to the U.S. population overall,5 making the direction of any bias difficult to determine. Because there were so many departments and shifts, resources were not available to actively target specific groups with existing interpersonal ties. Instead, the intervention relied on existing groups to take advantage of intervention activities. A similar intervention may have been more effective in smaller worksites. The intervention participation data were collected via self-report, which is subject to social desirability bias.
Conclusion
Study findings suggest that worksite-based ecologic interventions can succeed in preventing weight gain among employees who engage in offered interventions. Future interventions should include strategies to actively facilitate participation of employees who may not be self-motivated as well as organization-wide strategies that demonstrate leadership support for worker health. Increased recognition of social context within worksites and targeting intervention strategies at the interpersonal level to improve actual and perceived social norms may also improve behaviors related to healthy weight, and future interventions should be designed to test this.
Table 5. Difference between intervention and control conditions in change conceptual model measures (n=806)a,b.
| 12-month | 24-month | |||||||
|---|---|---|---|---|---|---|---|---|
| Change per unit (t-score) | 95% CI | Change per unit (t-score) | 95% CI | |||||
| Lower | Upper | P-value | Lower | Upper | P-value | |||
| Perception of organizational commitment to employee health | .32 (4.17) | .17 | .47 | <.0001 | .37 (4.31) | .20 | .54 | <.0001 |
| Perception of employee normative dietary behaviors | .12 (1.23) | −.07 | .30 | .22 | .04 (0.44) | −.15 | .24 | .66 |
| Perception of employee normative physical activity behaviors | −.02 (−0.21) | −.20 | .16 | .83 | .08 (0.75) | −.12 | .27 | .46 |
Adjusted for gender, age, race/ethnicity, education, job category, shift, and hours worked per week.
Weighted to represent the hospital workforce population.
Acknowledgments
Funding came from the National Heart, Lung and Blood Institute (NHLBI), grant 5R01HL079483. NHLBI is not responsible for the content of this article. We thank Walter Ettinger, M.D., John Polanowicz and Patrick Muldoon, presidents of participating hospitals UMassMemorial Medical Center, Marlborough Hospital and HealthAlliance Hospital and their human resources, facilities, food services, information services, marketing, public relations, administrative, and clinical staff who supported this study. We also thank the Public Affairs department at University of Massachusetts Medical School. Thanks to employees who volunteered on Advisory Boards and Committees and to the hundreds of participants in the current evaluation sample. Thanks to Christine Foley who developed and produced materials and assisted with data collection, and to recruiters/data collectors: Betsy Costello, Caroline Cranos, Barbara Glidden, Susan Bakke and Valerie Ugrinow. We thank Denise Jolicoeur for assistance with intervention development and delivery and work with Employee Advisory Boards, and Kathy Leung for data management. Hall-Foushee Communications Inc. provided the overall design of the logos, materials and social marketing campaign.
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Stephenie C. Lemon, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, Massachusetts.
Jane Zapka, Division of Biostatistics and Epidemiology, Medical University of South Carolina, Charleston, South Carolina.
Wenjun Li, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, Massachusetts.
Barbara Estabrook, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, Massachusetts.
Milagros Rosal, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, Massachusetts.
Robert Magner, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, Massachusetts.
Victoria Andersen, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, Massachusetts.
Amy Borg, Division of Preventive and Behavioral Medicine, University of Massachusetts Medical School, Worcester, Massachusetts.
Janet Hale, Graduate School of Nursing, University of Massachusetts Medical School, Worcester, Massachusetts.
References
- 1.Wyatt SB, Winters KP, Dubbert PM. Overweight and obesity: prevalence, consequences, and causes of a growing public health problem. Am J Med Sci. 2006;331(4):166–74. doi: 10.1097/00000441-200604000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Gregg EW, Cheng YJ, Cadwell BL, Imperatore G, Williams DE, Flegal KM, et al. Secular trends in cardiovascular disease risk factors according to body mass index in U.S. adults. Jama. 2005;293(15):1868–74. doi: 10.1001/jama.293.15.1868. [DOI] [PubMed] [Google Scholar]
- 3.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625–38. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 4.Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293(15):1861–7. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- 5.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the U.S., 1999–2004. JAMA. 2006;295(13):1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 6.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among U.S. adults, 1999–2000. JAMA. 2002;288(14):1723–7. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 7.Lewis CE, Jacobs DR, Jr, McCreath H, Kiefe CI, Schreiner PJ, Smith DE, et al. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 2000;151(12):1172–81. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 8.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science. 2003;299(5608):853–5. doi: 10.1126/science.1079857. [DOI] [PubMed] [Google Scholar]
- 9.Schmitz MK, Jeffery RW. Public health interventions for the prevention and treatment of obesity. Med Clin North Am. 2000;84(2):491–512. viii. doi: 10.1016/s0025-7125(05)70233-9. [DOI] [PubMed] [Google Scholar]
- 10.Jeffery RW. Public health strategies for obesity treatment and prevention. Am J Health Behav. 2001;25(3):252–9. doi: 10.5993/ajhb.25.3.12. [DOI] [PubMed] [Google Scholar]
- 11.Sallis JF, Owen N. Ecological models of health behavior. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research and Practice. 3rd. San Francisco, CA: Jossey-Bass Publishers; 2002. pp. 462–484. [Google Scholar]
- 12.Stokols D. Establishing and maintaining healthy environments. Toward a social ecology of health promotion. Am Psychol. 1992;47(1):6–22. doi: 10.1037//0003-066x.47.1.6. [DOI] [PubMed] [Google Scholar]
- 13.Elder JP, Lytle L, Sallis JF, Young DR, Steckler A, Simons-Morton D, et al. A description of the social-ecological framework used in the trial of activity for adolescent girls (TAAG) Health Educ Res. 2007;22(2):155–65. doi: 10.1093/her/cyl059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Booth SL, Sallis JF, Ritenbaugh C, Hill JO, Birch LL, Frank LD, et al. Environmental and societal factors affect food choice and physical activity: rationale, influences, and leverage points. Nutr Rev. 2001;59:S21–39. doi: 10.1111/j.1753-4887.2001.tb06983.x. discussion S57-65. [DOI] [PubMed] [Google Scholar]
- 15.Schroeder SA. Tobacco control in the wake of the 1998 master settlement agreement. N Engl J Med. 2004;350(3):293–301. doi: 10.1056/NEJMsr031421. [DOI] [PubMed] [Google Scholar]
- 16.Katz DL, O'Connell M, Yeh MC, Nawaz H, Njike V, Anderson LM, et al. Public health strategies for preventing and controlling overweight and obesity in school and worksite settings: a report on recommendations of the Task Force on Community Preventive Services. MMWR Recomm Rep. 2005;54(RR–10):1–12. [PubMed] [Google Scholar]
- 17.McNeely E. The consequences of job stress for nurses' health: time for a check-up. Nurs Outlook. 2005;53(6):291–9. doi: 10.1016/j.outlook.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Wee CC, Phillips RS, Legedza AT, Davis RB, Soukup JR, Colditz GA, et al. Healthcare expenditures associated with overweight and obesity among U.S. adults: importance of age and race. Am J Public Health. 2005;95(1):159–65. doi: 10.2105/AJPH.2003.027946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raebel MA, Malone DC, Conner DA, Xu S, Porter JA, Lanty FA. Health services use and healthcare costs of obese and nonobese individuals. Arch Intern Med. 2004;164(19):2135–40. doi: 10.1001/archinte.164.19.2135. [DOI] [PubMed] [Google Scholar]
- 20.Thorpe KE, Florence CS, Howard DH, Joski P. The impact of obesity on rising medical spending. Health Aff (Millwood) 2004 Web Exclusives:W4-480–6. doi: 10.1377/hlthaff.w4.480. [DOI] [PubMed] [Google Scholar]
- 21.Finkelstein EA, Fiebelkorn IC, Wang G. State-level estimates of annual medical expenditures attributable to obesity. Obes Res. 2004;12(1):18–24. doi: 10.1038/oby.2004.4. [DOI] [PubMed] [Google Scholar]
- 22.Finkelstein E, Fiebelkorn C, Wang G. The costs of obesity among full-time employees. Am J Health Promot. 2005;20(1):45–51. doi: 10.4278/0890-1171-20.1.45. [DOI] [PubMed] [Google Scholar]
- 23.Long DA, Reed R, Lehman G. The cost of lifestyle health risks: obesity. J Occup Environ Med. 2006;48(3):244–51. doi: 10.1097/01.jom.0000201568.73562.a2. [DOI] [PubMed] [Google Scholar]
- 24.Gates DM, Succop P, Brehm BJ, Gillespie GL, Sommers BD. Obesity and presenteeism: the impact of body mass index on workplace productivity. J Occup Environ Med. 2008;50(1):39–45. doi: 10.1097/JOM.0b013e31815d8db2. [DOI] [PubMed] [Google Scholar]
- 25.Bao Y, Duan N, Fox SA. Is some provider advice on smoking cessation better than no advice? An instrumental variable analysis of the 2001 National Health Interview Survey. Health Serv Res. 2006;41(6):2114–35. doi: 10.1111/j.1475-6773.2006.00592.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chapman LS. Reducing obesity in work organizations. Am J Health Promot. 2004;19(1) 1–8 discussion 12. [PubMed] [Google Scholar]
- 27.Pratt CA, Lemon SC, Fernandez ID, Goetzel R, Beresford SA, French SA, et al. Design characteristics of worksite overweight and obesity control interventions supported by the National Heart, Lung, and Blood Institute. Obesity. 2007;15(9):2171–2180. doi: 10.1038/oby.2007.258. [DOI] [PubMed] [Google Scholar]
- 28.Cialdin R, K CA, Reno RR, editors. A focus theory of normative conduct: A theoretical refinement and reevaluation of the role of norms in human behavior. San Diego, CA: Academic Press; 1991. [Google Scholar]
- 29.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 30.Linnan LA, Sorensen G, Colditz G, Klar DN, Emmons KM. Using theory to understand the multiple determinants of low participation in worksite health promotion programs. Health Educ Behav. 2001;28(5):591–607. doi: 10.1177/109019810102800506. [DOI] [PubMed] [Google Scholar]
- 31.Steckler A, Goodman RM, Kegler MC. Mobilizing Organizations for Health Enhancement: Theories of Organizational Change. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education. 3rd. San Francisco: Jossey-Bass; 2002. pp. 335–360. [Google Scholar]
- 32.Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research and Practice. 3rd. San Francisco, CA: Jossey-Bass; 2002. pp. 185–209. [Google Scholar]
- 33.Bandura A. Social Foundation of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 34.Zapka J, Lemon S, Estabrook B, Jolicoeur D. Keeping a Step Ahead—formative phase of a workplace intervention trial to prevent obesity. Obes. 2007;15:27S–36S. doi: 10.1038/oby.2007.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.StairWELL to Better Health: A Worksite Intervention. 2008 website. [cited 2008 December 16, 2008]; Available from: www.cdc.gov/nccdphp/Dnpa/hwi/toolkits/stairwell/index.htm.
- 36.Lemon SC, Zapka J, Li W, Estabrook B, Magner R, Rosal MC. Perceptions of worksite support and employee obesity, activity, and diet. Am J Health Behav. 2009;33(3):299–308. doi: 10.5993/ajhb.33.3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ribisl KM, Reischl TM. Measuring the climate for health at organizations. Development of the worksite health climate scales. J Occup Med. 1993;35(8):812–24. doi: 10.1097/00043764-199308000-00019. [DOI] [PubMed] [Google Scholar]
- 38.Lemon SC, Roy J, Clark MA, Friedmann PD, Rakowski W. Classification and regression tree analysis in public health: Methodologic review and comparison with logistic regression. Ann Behav Med. 2003;26(3):172–181. doi: 10.1207/S15324796ABM2603_02. [DOI] [PubMed] [Google Scholar]
- 39.Zhang H, Singer B. Recursive partitioning in the health sciences. In: Dietz K, Gail M, Krickeberg K, Singer B, editors. Statistics for biology and health. New York NY: Springer-Verlag; 1999. [Google Scholar]
- 40.Breiman L, Friedman JH, Olshen RA, Stone CJ. Classification and regression trees. 2nd. Pacific Grove: Wadsworth; 1984. [Google Scholar]
- 41.CDC. Public Health Strategies for Preventing and Controlling Overweight and Obesity in School and Worksite Settings. A Report on Recommendations of the Task Force on Community Preventive Services MMWR. 2005;54(RR10):1–12. [PubMed] [Google Scholar]
- 42.Jordan KC, Erickson ED, Cox R, Carlson EC, Heap E, Friedrichs M, et al. Evaluation of the Gold Medal Schools program. J Am Diet Assoc. 2008;108(11):1916–20. doi: 10.1016/j.jada.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 43.Halm J, Amoako E. Physical activity recommendation for hypertension management: does healthcare provider advice make a difference? Ethn Dis. 2008;18(3):278–82. [PubMed] [Google Scholar]
- 44.Mello MM, Studdert DM, Brennan TA. Obesity—the new frontier of public health law. N Engl J Med. 2006;354(24):2601–10. doi: 10.1056/NEJMhpr060227. [DOI] [PubMed] [Google Scholar]
- 45.Gostin LO. Law as a tool to facilitate healthier lifestyles and prevent obesity. Jama. 2007;297(1):87–90. doi: 10.1001/jama.297.1.87. [DOI] [PubMed] [Google Scholar]
- 46.Marine A, R J, Serra C, Verbeek J. Preventing occupational stress in healthcare workers. Cochrane Database of Systematic Reviews. 2008;(4) doi: 10.1002/14651858.CD002892.pub2. [DOI] [PubMed] [Google Scholar]
- 47.Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population-based study of 27,485 people. Occup Environ Med. 2001;58(11):747–52. doi: 10.1136/oem.58.11.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tenkanen L, Sjoblom T, Harma M. Joint effect of shift work and adverse life-style factors on the risk of coronary heart disease. Scand J Work Environ Health. 1998;24(5):351–7. doi: 10.5271/sjweh.355. [DOI] [PubMed] [Google Scholar]
- 49.Lemon SC, Rosal MC, Zapka J, Borg A, Andersen V. Contributions of weight perceptions to weight loss attempts: differences by body mass index and gender. Body Image. 2009;6(2):90–6. doi: 10.1016/j.bodyim.2008.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dorsey RR, Eberhardt MS, Ogden CL. Racial/ethnic differences in weight perception. Obesity (Silver Spring) 2009;17(4):790–5. doi: 10.1038/oby.2008.603. [DOI] [PubMed] [Google Scholar]
- 51.Zapka J, Lemon SC, Estabrook B, Rosal MC. Factors related to weight loss behavior in a multiracial/ethnic workforce. Ethn Dis. 2009;19(2):154–60. [PMC free article] [PubMed] [Google Scholar]
- 52.Engbers LH, van Poppel MN, Chin APMJ, van Mechelen W. Worksite health promotion programs with environmental changes: a systematic review. Am J Prev Med. 2005;29(1):61–70. doi: 10.1016/j.amepre.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 53.Seymour JD, Yaroch AL, Serdula M, Blanck HM, Khan LK. Impact of nutrition environmental interventions on point-of-purchase behavior in adults: a review. Prev Med. 2004;39 2:S108–36. doi: 10.1016/j.ypmed.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 54.Kahn EB, Ramsey LT, Brownson RC, Heath GW, Howze EH, Powell KE, et al. The effectiveness of interventions to increase physical activity. A systematic review(1,2) Am J Prev Med. 2002;22(4 Suppl 1):73–107. doi: 10.1016/s0749-3797(02)00434-8. [DOI] [PubMed] [Google Scholar]
- 55.Boutelle KN, Jeffery RW, Murray DM, Schmitz MK. Using signs, artwork, and music to promote stair use in a public building. Am J Public Health. 2001;91(12):2004–6. doi: 10.2105/ajph.91.12.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kerr NA, Yore MM, Ham SA, Dietz WH. Increasing stair use in a worksite through environmental changes. Am J Health Promot. 2004;18(4):312–5. doi: 10.4278/0890-1171-18.4.312. [DOI] [PubMed] [Google Scholar]
- 57.U.S. Bureau of the Census. Washington, DC: U.S. Census; Sep 1, 2008. http://www.census.gov/main/www/citation.html. [Google Scholar]