Abstract
Congenital adrenal hyperplasia (CAH) describes a group of genetic, autosomal recessive conditions, where there is a block in cortisol biosynthesis. Approximately 95 percent of cases are due to 21-hydroxylase deficiency, which is discussed in this article. Patients with the severe or classic form of CAH have epinephrine deficiency in addition to cortisol deficiency. Both epinephrine and cortisol are important counterregulatory hormones and help prevent hypoglycemia during physical stress. This is the first prospective study to evaluate the incidence of hypoglycemia during acute illness in children with classic CAH. Our objective was to examine blood glucose levels and symptoms of these children during the physical stressor of a typical acute illness managed at home.
Twenty patients, ages 3 to 10 years with classic CAH participated. Parents were instructed regarding management of illnesses, home blood glucose monitoring and questionnaire completion. Over 29 months, 20 patients completed questionnaires and 6 patients performed home blood glucose monitoring. A blood glucose of <60mg/dL was documented in 3 out of 8 monitored acute illness episodes, and in 2 out of 6 of monitored children. The acute illness episodes with documented blood glucose <60mg/dL were not associated with vomiting.
Our data suggest that children with classic CAH may experience lowering of blood glucose during illnesses, and patient education regarding the management of common childhood illness should include glucose supplementation.
Introduction
Classic congenital adrenal hyperplasia (CAH) due to 21-hydroxylase deficiency is a genetic disorder that results in impaired biosynthesis of cortisol, with and without aldosterone and epinephrine deficiency. The genetic frequency of classic CAH is approximately 1 in 15,000. The clinical spectrum ranges from the most severe to mild forms, depending on the degree of 21-hydroxylase activity. There are three main phenotypes: classic salt-wasting, classic simple-virilizing, and nonclassic. In the classic forms, epinephrine deficiency occurs because adrenocortical secretion of cortisol is necessary for adrenomedullary organogenesis and adrenomedullary epinephrine synthesis (Merke et al., 2000). Both cortisol and epinephrine are counterregulatory hormones and play an essential role in the regulation of blood glucose. The standard treatment for classic CAH due to 21-hydroxylase deficiency is glucocorticoid (replaces cortisol) and fludrocortisone (replaces aldosterone), given daily. There is no known effective treatment for the epinephrine deficiency.
Both cortisol and epinephrine are counterregulatory hormones and play an important role in preventing hypoglycemia. However, epinephrine has a greater overall effect on glucose levels during acute stress (Shamoon, Hendler, & Sherwin, 1981; Weise et al., 2004). Previously, we evaluated epinephrine reserve in children with CAH using a standardized exercise test. Exercise is a powerful natural stimulus of the adrenal medulla and normally results in a brisk increase in epinephrine secretion. In these prior studies, we found that children with classic CAH receiving standard glucocorticoid replacement had significantly lower epinephrine levels and the normal exercise-induced rise in blood glucose was blunted when compared to controls. Doubling of the usual hydrocortisone dose did not influence glucose levels, supporting the concept that epinephrine, rather than cortisol, is the major regulator of short-term blood glucose levels (Weise et al., 2004).
Febrile illness is a natural stressor and a powerful stimulus of both the adrenal medulla and cortex. Normally with fever or other significant physical illness the body responds by producing more cortisol; however patients affected with CAH are unable to produce cortisol so the glucocorticoid replacement dose must be increased when a fever or illness occurs. Severe complications have been reported in patients with CAH, and overall approximately 8 to 9 percent of these patients have been reported to experience episodes of hypoglycemia (Donaldson et al., 1994; Jaaskelainen & Voutilainen, 2000; Pinto et al., 2003), which typically occurs in young children with significant illness evaluated in an emergency setting. The aim of this study was to prospectively determine the frequency of hypoglycemia in children with classic CAH during common childhood illnesses managed at home.
Subjects and Methods
Participants
Patients with classic CAH who were enrolled in a long-term clinical trial at NIH and were ten years old or less were invited to participate in the study. Twenty children (12 males, 8 females; median age 6 years, age range 3 to 10 years) were studied prospectively (Table 1). All patients had been previously genotyped. Twelve of the 20 children had a history of salt-wasting adrenal crises and 16 had a genotype typically associated with the more severe type of classic CAH (salt-wasting). Patients with more severe form of classic CAH (salt -wasting) have an increased risk for adrenal crisis during acute illness. In addition since children with the severe form of classic CAH have inadequate epinephrine production, they may be at increased risk for hypoglycemia with acute illness. The remaining 4 children had a slightly milder form of CAH known as classic simple-virilizing. All children had adrenal insufficiency due to their CAH and were receiving hydrocortisone and fludrocortisone treatment. The two groups were similar in age and were taking similar glucocorticoid replacement doses; a majority had the severe salt-wasting form of CAH. The National Institute of Child Health and Human Development institutional review board approved the study. Written informed consent was obtained from a parent, and children gave their assent.
Table 1. Clinical characteristics of CAH patients: Blood glucose monitored vs unmonitored.
| Blood glucose monitored | Blood glucose not monitored | |
|---|---|---|
| Children with CAH | 6 | 14 |
| Females | 2 | 6 |
| Males | 4 | 8 |
| Mean Age (years ± std dev) | 6.2 ± 2 | 6.2 ± 2.5 |
| Severe type of CAH (salt wasters) | 5 | 11 |
| Receiving flutamide/testolactone treatment | 0 | 7 |
| Hydrocortisone (mg/m2/day ± std dev) | 13.2 ± 2.7 | 10.5 ± 4.5 |
| Fludrocortisone (ug/day ± std dev) | 67 ± 20 | 117± 37 |
| Illness episodes | 8 | 32 |
| IM Solu-Cortef® | 0 | 9 |
| Recent serum metanephrine (pg/mL ± std dev) | 17.8 ± 12.5 | 17.3 ± 9.2 |
| History of hospitalization/ER visit(s) for adrenal crisis | 5 | 9 |
Procedures and Instruments
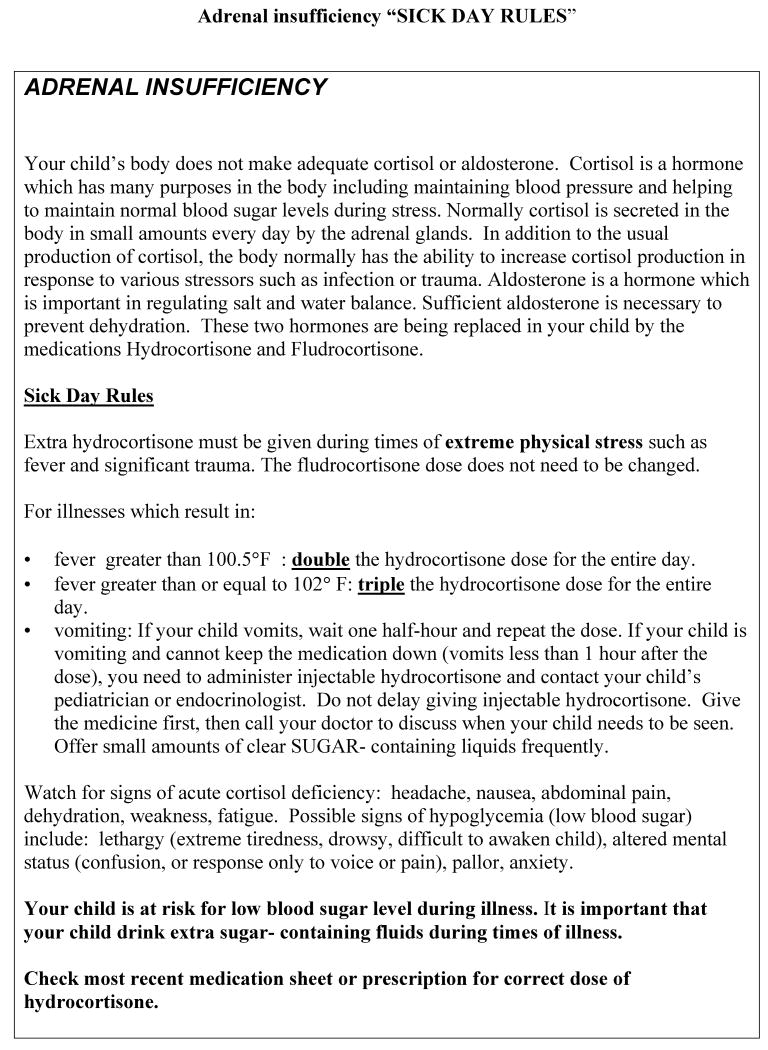
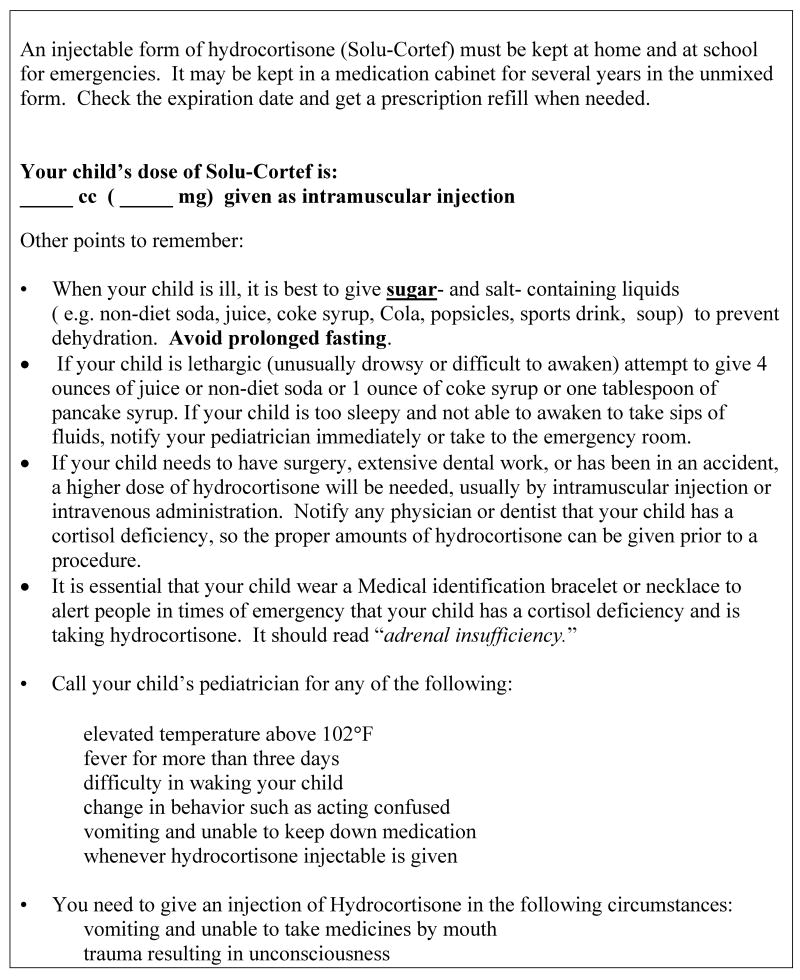
Parents of children with CAH were provided with written instructions and supplies needed for data collection during their routine NIH visit. Pediatric endocrine nurses reviewed symptoms of adrenal insufficiency with the parent(s) and gave written instructions regarding management of acute illness including glucocorticoid stress dose guidelines (“sick day rules”) (Figure 1). Parents were taught by the nursing staff how to perform home blood glucose monitoring (i.e. finger sticks, use of a glucometer) using demonstration and written materials. Competence to perform the blood glucose testing was assessed by a pediatric endocrine nurse with return demonstration of the technique by the parent.
Figure 1. Adrenal insufficiency “SICK DAY RULES”.
In addition, parents were instructed to give a specific liquid amount of one of the following liquids if the blood glucose was less than 60mg.dL: 4 ounces of juice or non-diet soda (13 to 17 gm carbohydrate CHO), 1 ounce of coke syrup (21 to 24 gm CHO), or 1 tablespoon of maple/pancake syrup (13 to 15gm CHO). These liquids were chosen because they contain a high concentration of sugar in a small volume. After 30 minutes the parent was instructed to re-check the blood glucose and record symptoms. ‘Illness report forms,’ were given for the parents to record blood glucose, symptoms, and treatments. If the child's blood glucose remained <60mg/dL after interventions, the parent was advised to seek professional help. Parents were also instructed to offer small amounts of clear liquids that contain CHO as well as sodium, such as Gatorade® (7gm CHO and 55mg sodium per 4 ounces), Pedialyte® (3 gm CHO and 125mg sodium per four ounces), or non-diet juice or soda (3.5 gm CHO and 10mg sodium per four ounces), frequently during the acute illness to prevent/treat dehydration.
For the purpose of this study, hypoglycemia was defined as blood glucose < 60mg/dl, since our intent was to capture all significant lowering of blood glucose, not just severe drops. The One Touch Fast Take Blood Glucose Monitoring System (Lifescan, Inc., Milpitas, CA) was used because Lifescan, Inc., provided data that demonstrated the accuracy of the One Touch monitor with low glucose levels (<50mg/dL) (J.Telford, Lifescan Inc., personal communication, December 7, 2000). Fever was defined as a temperature of 100.5° Fahrenheit or greater (orally) and illness was defined as an episode of fever, vomiting, diarrhea, respiratory infection, and/or lethargy. Adrenal crisis was defined as life-threatening adrenal insufficiency due to insufficient glucocorticoid and includes symptoms of shock, dehydration, and/or alterations in serum sodium and potassium levels.
At six-month intervals, the ‘Illness report’ forms were collected and a single practitioner reviewed results with the parent. For parents who did not monitor blood glucose during an acute illness, information regarding any illnesses in the past six months, including the child's symptoms and use of stress dose(s) of hydrocortisone, was collected retrospectively, based on parental recall and/or home records. Serum free metanephrine values, a measure of epinephrine stores in the adrenal medulla, were obtained from prior medical records (within 6 months). The most recent value recorded was used as an estimate of adrenomedullary function.
Results
Over a period of 29 months, 20 patients completed the study and 6 patients performed blood glucose monitoring at home. Patients who completed blood glucose monitoring were similar in age and other clinical characteristics when compared to patients who did not complete blood glucose monitoring (Table 1). A blood glucose of <60mg/dL was documented in 3 of the 8 monitored acute illness episodes, (in 2 of the 6 children who had blood glucose monitored) (Table 2). The acute illness episodes with documented blood glucose <60mg/dL were not associated with vomiting, which is unusual since prior reports in the literature note that hypoglycemia in young children typically occurs with gastrointestinal illnesses, malnutrition, and/or infection with a bacterial pathogen. Lack of oral intake places the patient at higher risk for hypoglycemia.
Table 2. CAH patients with monitored illness episodes.
| Patient | Age/sex | Genotype | Clinical Phenotype | Number illness episodes | Number episodes monitored | Lowest blood glucose | Illness symptoms |
|---|---|---|---|---|---|---|---|
| 1 | 4yr male | In2/In2 | Severe form of CAH | 4 | 1 | 108 | Vomiting, lethargy |
| 2 | 3yr female | In2/unknown | Severe form of CAH | 3 | 1 | 48 | Fever (101.8°F, lethargy Strep throat |
| 3 | 8yr male | P30L/large deletion | Milder form of CAH | 1 | 1 | 76 | Fever (102.3°F, nausea, lethargy |
| 4 | 6yr male | In2/unknown | Severe form of CAH | 2 | 2 | 78 | Fever (101.8°F, lethargy, headache |
| 5 | 5yr female | In2/large deletion | Milder form of CAH | 7 | 2 | 44 | Lethargy |
| 6 | 7yr male | In2/In2 | Severe form of CAH | 2 | 1 | 118 | Fever (102.5°F, lethargy |
| KEY to Table 2 | |||||||
| Genotypes associated with: | |||||||
Severe form of CAH (salt-waster):
|
Milder forms of CAH (simple-virilizer or non-classic)
|
||||||
The most common symptoms during illness in the 20 patients were fever (41 percent), vomiting (37 percent), and lethargy (12 percent). Lethargy was reported in all episodes with documented hypoglycemia. All children were appropriately managed with oral stress dose(s) of hydrocortisone and antipyretics (see Figure 1). No child in this study required overnight hospitalization for management of an acute illness episode.
Illness episodes with blood glucose monitoring
There were 8 episodes of illness requiring stress doses of hydrocortisone in the six children whose parents recorded blood glucose. There were three documented episodes of blood glucose <60mg/dL (Table 2). One child had a blood glucose level of 44mg/dL with symptoms of lethargy, weakness and fatigue (at 8AM, last oral caloric intake had been at bedtime the evening prior). The parent did not check her temperature due to concern about attending to the child's lethargic condition. The child became more alert and responsive after oral juice intake and the parent did not re-check the blood glucose. The primary medical doctor evaluated the child and no further intervention was required.
A second child with symptoms of fever of 101.8°F, abdominal pain and sleepiness, reported initial blood glucose of 48ug/dL. One hour after she received cola, a repeat glucose was 175ug/dl. (Her last oral intake had been four ounces of a fruit drink, one-half hour prior to parent noting fever and subsequent blood glucose test). She subsequently was diagnosed and treated for strep throat infection. The third child had symptoms of lethargy and muscle weakness upon awakening in the morning (no prior illness symptoms, last oral caloric had been at bedtime the evening prior). The initial blood glucose was 56mg/dL, which increased to 163mg/dL after she ate and received her usual dose of oral glucocorticoid.
The average glucocorticoid replacement dose for the patients who had documented hypoglycemia was 14.2 mg/m2/day, which is within the range of recommended glucorticoid replacement dose for children affected with CAH. Insufficient replacement dose of glucocorticoid is associated with an increased risk of adrenal crisis. Patients had adrenal hormone levels (17-hydroxyprogesterone, androstenedione, and plasma renin activity) that were within the therapeutic range at routine evaluations prior to and after the illness episodes, reflecting good control of their CAH and compliance with daily medication. Children with hypoglycemia had prior serum free metanephrine values (estimate of adrenomedullary function) at a prior visit similar to those who had documented normoglycemia (data not shown). Measurement of free metanephrine was not predictive of hypoglycemia or vomiting with illness.
Illness episodes without blood glucose monitoring
There were 32 acute illness episodes that required stress doses of hydrocortisone in the 14 children whose parents did not record blood glucose. In addition, there were 11 episodes of illness that were not monitored in the group of 6 children whose parents performed blood glucose monitoring for other illness episodes. The most common symptoms during illness were fever (55 percent), vomiting (49 percent), and fever and vomiting (28 percent). The most common reason that parents reported for not monitoring blood glucose was inconvenience. Other reasons for not monitoring blood glucose were preoccupation with taking care of the sick child, the illness episode did not occur at home where the blood glucose monitor equipment was kept, or the parent who was present with the child at illness onset was not the parent who received training for blood glucose monitoring. All children were appropriately managed with oral stress dose(s) of hydrocortisone, antipyretics, and oral fluids containing glucose.
Administration of intramuscular hydrocortisone
None of the children who had blood glucose monitoring performed by parents required an intramuscular injection of hydrocortisone. In the acute illness episodes where blood glucose was not monitored, 21% resulted in the child receiving intramuscular hydrocortisone.
Discussion
The aim of this study was to prospectively examine the frequency of hypoglycemia in children with classic CAH during common childhood illnesses managed at home. Our data suggest that children with classic CAH may experience lowering of blood glucose during typical childhood illnesses. Although administration of stress doses of hydrocortisone is crucial to prevent adrenal crisis, based on our findings and the findings of previous retrospective studies that hypoglycemia may occur in approximately 9% of acute illnesses; glucose supplementation is also warranted to prevent hypoglycemia.
In our small prospective study of childhood illnesses in children with CAH, hypoglycemia associated with an acute illness was noted in 3 out of 8 episodes when blood glucose was monitored. Overall, 2 of the 20 (10%) children enrolled in the study had documented hypoglycemia. This is likely an underestimate of the frequency of hypoglycemia since the illness episodes not monitored were more severe according to parental report and many unmonitored illnesses were associated with vomiting and lack of oral intake. All illness episodes were typical childhood illnesses. The most common clinical symptom associated with illnesses with documented hypoglycemia was lethargy.
There are several reports of hypoglycemia in children with CAH associated with acute illness episodes (Mackinnon & Grant, 1977). Pinto (Pinto et al., 2003) reported the follow-up of 68 children with classic CAH, and noted that hypoglycemia occurred 9 times in children between the ages of 1 to 3 years, and resulted in two deaths. Donaldson (Donaldson et al., 1994) reported a 9% incidence of hypoglycemia in young children who were admitted to the hospital for an illness and noted that the incidence was probably an underestimate since blood glucose was only measured in 22% of admissions.
These previous reports of hypoglycemia in patients with CAH are retrospective reports of patients with severe illness who presented for medical evaluation. Overall, in these reports, approximately 8 to 9 percent of patients with CAH experienced hypoglycemia. Our study is the first prospective evaluation of glucose levels in patients with CAH during common childhood illnesses managed at home. Although our sample size was small, our results are consistent with the retrospective hospital- based reports of the incidence of hypoglycemia in children with classic CAH during an acute illness episode. In all of our patients, oral intake of glucose containing fluids (or food) plus stress doses of hydrocortisone successfully increased the blood glucose to the normal range and the parents were able to successfully manage the illness at home.
It has been suggested that higher dose glucocorticoid be used early in life to prevent hypoglycemia, since younger children are at higher risk for hypoglycemia (Pinto et al., 2003). There is no evidence that chronic use of higher doses of glucocorticoid protects against hypoglycemia or life-threatening complications, and epinephrine deficiency may have an important role. Studies of normal preterm infants provide evidence to support the notion that epinephrine rather than glucagon is the major regulator of gluconeogenesis and glyconeogenesis in the counterregulatory response to hypoglycemia in neonates (Jackson, Williams, Burchell, Coughtrie, & Hume, 2004). Our previous finding that stress doses of hydrocortisone were not beneficial in adolescents with CAH undergoing short-term, high-intensity exercise and did not alter glucose levels (Weise et al., 2004), implicates epinephrine as the major player in acute blood sugar regulation in older children. Moreover, excessive glucocorticoid use during the first two years of life has been found to be a risk factor for adult short stature in multiple studies (New, Gertner, Speiser, & del Balzo, 1988; Rasat, Espiner, & Abbott, 1995; Soliman, AlLamki, AlSalmi, & Asfour, 1997; Young & Hughes, 1990) and may lead to risk factors for cardiovascular disease (i.e. obesity, hyperlipidemia). Most likely, epinephrine, glucagon, and cortisol interact synergistically to prevent hypoglycemia, (Shamoon et al., 1981), but epinephrine may be more important in the acute response to a decrease in blood glucose levels. Unfortunately, there is no good way to replace the deficient epinephrine response and glucose supplementation is the best way to prevent and treat the lowering of blood glucose.
The small sample size and lack of a control group of children are limitations of our study. A benefit of home blood glucose monitoring was that parents reported reassurance in knowing the blood glucose and its relevance to their child's symptoms during an acute illness. Hypoglycemia occurring beyond the newborn period in otherwise healthy children is rare; however there is little data available. Most studies report the incidence of hypoglycemia in children with concurrent dehydration (due to vomiting and/or diarrhea), malnutrition, and/or bacterial pathogens (Bennish, Azad, Rahman, & Phillips, 1990; Daral et al., 1985; Glyn-Jones, 1975; Reid, McQuillan, & Losek, 2003). Reid et al., (2003) reported a study of healthy children (under the age of 5 years) with acute gastroenteritis and noted that hypoglycemia (defined as a BG <45mg/dL in infants less than one month age, and < 60mg/dL in children older than one month) was significantly associated with presence of neuroglycopenia (altered mental status); history of having as many or more episodes of vomiting than diarrhea; and female gender.
Nurses have a critical role in the education of patients and families of children affected with classic CAH, including the management of acute illnesses. A careful history regarding the child's responses to prior illness episodes will provide important information about whether the child experienced symptom of lethargy, and/or required an emergency room visit or hospitalization. Information obtained from the history of prior illnesses will allow the clinician to determine whether the parent is performing stress-dosing appropriately, and if re-education is indicated. Children who experienced symptoms of lethargy and/or an emergency room visit or hospitalization related to an acute illness should be counseled regarding the risk of hypoglycemia and the importance of glucose supplementation during illness. In addition, the nurse can discuss with the parent the option of home glucose monitoring during illness episodes. Also, since young children with classic CAH are likely to have an increased risk for hypoglycemia with acute illness, it is important for nurses to counsel parents regarding proper choice and amounts of glucose containing fluids for their child during an illness.
Future directions
A limitation of this study is the lack of a control group of children with fever, to compare the incidence of hypoglycemia with acute illness. Future studies should be designed to include a control group, although this may be difficult to implement, since parents may be hesitant to perform fingersticks on a child without a known risk-factor. In addition, it would be beneficial to collect data about the adrenomedullary response during illness episodes (i.e. 24 hour urine for free metanephrine) to help elucidate the role of epinephrine deficiency in hypoglycemia.
Conclusion
In conclusion, our study indicates that children with classic CAH receiving adequate glucocorticoid and mineralcorticoid supplementation are at risk for hypoglycemia during common childhood illnesses. Administration of stress doses of hydrocortisone is undoubtedly crucial during illness; but is probably not sufficient to prevent hypoglycemia. The addition of glucose supplementation to the traditional instructions regarding stress doses of glucocorticoid is essential in preventing potentially life-threatening hypoglycemia, especially in children.
For relevant patient education materials refer to the following web sites: “Facts about CAH” at http://www.cc.nih.gov/ccc/patient_education/pepubs/cah.pdf and “Managing adrenal insufficiency” at http://www.cc.nih.gov/ccc/patient_education/pepubs/mngadrins.pdf
Acknowledgments
This study was supported in part by the intramural program of NICHD, NIH and by the Congenital Adrenal hyperplasia Research, Education and Support (CARES) Foundation No commercial financial support to declare.
The authors thank the patients and their families for participating in this study and the 9 West nursing staff of the NIH Clinical Research Center for their assistance. This research was supported (in part) by the Intramural Research Program of the National Institute of Child Health and Human Development, NIH, and (in part) by the Congenital Adrenal hyperplasia Research, Education and Support (CARES) Foundation.
Footnotes
Data from this paper was presented at the International Congress of Endocrinology (Lisbon, Portugal in September 2004) and the Pediatric Endocrine Nurses Society Conference (New Orleans, LA in May 2005).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bennish ML, Azad AK, Rahman O, Phillips RE. Hypoglycemia during diarrhea in childhood. Prevalence, pathophysiology, and outcome. N Engl J Med. 1990;322(19):1357–1363. doi: 10.1056/NEJM199005103221905. [DOI] [PubMed] [Google Scholar]
- Daral TS, Singh HP, Sachdev HP, Mohan M, Mathur M, Bhargava SK. Acute dehydrating diarrhea. Clinical profile in neonates & young infants. Indian Pediatr. 1985;22(5):333–338. [PubMed] [Google Scholar]
- Donaldson MD, Thomas PH, Love JG, Murray GD, McNinch AW, Savage DC. Presentation, acute illness, and learning difficulties in salt wasting 21-hydroxylase deficiency. Arch Dis Child. 1994;70(3):214–218. doi: 10.1136/adc.70.3.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glyn-Jones R. Blood sugar in infantile gastro-enteritis. S Afr Med J. 1975;49(36):1474–1476. [PubMed] [Google Scholar]
- Jaaskelainen, Voutilainen R. Long-term outcome of classical 21-hydroxylase deficiency: diagnosis, complications and quality of life. Acta Paediatr. 2000;89(2):183–187. doi: 10.1080/080352500750028807. [DOI] [PubMed] [Google Scholar]
- Jackson L, Williams FL, Burchell A, Coughtrie MW, Hume R. Plasma catecholamines and the counterregulatory responses to hypoglycemia in infants: a critical role for epinephrine and cortisol. J Clin Endocrinol Metab. 2004;89(12):6251–6256. doi: 10.1210/jc.2004-0550. [DOI] [PubMed] [Google Scholar]
- Mackinnon J, Grant DB. Hypoglycaemia in congenital adrenal hyperplasia. Arch Dis Child. 1977;52(7):591–593. doi: 10.1136/adc.52.7.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merke DP, Chrousos GP, Eisenhofer G, Weise M, Keil MF, Rogol AD, et al. Adrenomedullary dysplasia and hypofunction in patients with classic 21-hydroxylase deficiency. N Engl J Med. 2000;343(19):1362–1368. doi: 10.1056/NEJM200011093431903. [DOI] [PubMed] [Google Scholar]
- New MI, Gertner JM, Speiser PW, del Balzo P. Growth and final height in classical and nonclassical 21-hydroxylase deficiency. Acta Paediatr Jpn. 1988;30(Suppl):79–88. [PubMed] [Google Scholar]
- Pinto G, Tardy V, Trivin C, Thalassinos C, Lortat-Jacob S, Nihoul-Fekete C, et al. Follow-up of 68 children with congenital adrenal hyperplasia due to 21-hydroxylase deficiency: relevance of genotype for management. J Clin Endocrinol Metab. 2003;88(6):2624–2633. doi: 10.1210/jc.2002-021433. [DOI] [PubMed] [Google Scholar]
- Rasat R, Espiner EA, Abbott GD. Growth patterns and outcomes in congenital adrenal hyperplasia; effect of chronic treatment regimens. N Z Med J. 1995;108(1005):311–314. [PubMed] [Google Scholar]
- Reid S, McQuillan S, Losek J. Hypoglycemia complicating dehydration due to acute gastroenteritis. Clin Pediatr (Phila) 2003;42(7):641–646. doi: 10.1177/000992280304200711. [DOI] [PubMed] [Google Scholar]
- Shamoon H, Hendler R, Sherwin RS. Synergistic interactions among antiinsulin hormones in the pathogenesis of stress hyperglycemia in humans. J Clin Endocrinol Metab. 1981;52(6):1235–1241. doi: 10.1210/jcem-52-6-1235. [DOI] [PubMed] [Google Scholar]
- Soliman AT, AlLamki M, AlSalmi I, Asfour M. Congenital adrenal hyperplasia complicated by central precocious puberty: linear growth during infancy and treatment with gonadotropin-releasing hormone analog. Metabolism. 1997;46(5):513–517. doi: 10.1016/s0026-0495(97)90186-4. [DOI] [PubMed] [Google Scholar]
- Weise M, Drinkard B, Mehlinger SL, Holzer SM, Eisenhofer G, Charmandari E, et al. Stress dose of hydrocortisone is not beneficial in patients with classic congenital adrenal hyperplasia undergoing short-term, high-intensity exercise. J Clin Endocrinol Metab. 2004;89(8):3679–3684. doi: 10.1210/jc.2003-032051. [DOI] [PubMed] [Google Scholar]
- Young MC, Hughes IA. Response to treatment of congenital adrenal hyperplasia in infancy. Arch Dis Child. 1990;65(4):441–444. doi: 10.1136/adc.65.4.441. [DOI] [PMC free article] [PubMed] [Google Scholar]