Abstract
Objectives
(1) Quantify at which carious lesion depths dentists intervene surgically for cases of varying caries penetration and caries risk; (2) Identify characteristics that are associated with surgical intervention.
Methods
Dentists in a practice-based research network who reported doing at least some restorative dentistry were surveyed. Dentists were asked to indicate whether they would surgically intervene in a series of cases depicting occlusal caries. Each case included a photograph of an occlusal surface displaying typical characteristics of caries penetration, and a written description of a patient at a specific level of caries risk. Using logistic regression, we analyzed associations of surgical treatment with dentist and practice characteristics, and patient caries risk levels.
Results
519 DPBRN practitioner-investigators responded, of whom 63% indicated that they would surgically restore lesions located on inner enamel surfaces, and 90% of lesions located in outer dentin surfaces in a low caries risk individual. Regarding individuals at high caries risk, 77% reported that they would surgically restore inner enamel lesions and 94% reported restoring lesions located on the outer dentin surface. Dentists who did not assess caries risk were more likely to intervene on dentin lesions (p=.004). Practitioner-investigators who were in private practice were significantly more likely to intervene surgically on enamel lesions, compared to dentists from large group practices (p<.001).
Conclusion
Most dentists chose to provide some treatment to lesions that were within the enamel surface. Decisions to intervene surgically in the caries process differ by caries lesion depth, patient caries risk, assessment of caries risk, type of practice model, and percent of patients who self-pay.
Keywords: caries diagnosis, treatment threshold, organized dentistry, practice model, private practice, large group practice, public health, risk assessment
Introduction
The diagnosis and treatment of primary dental caries are common procedures in general dental practice and are topics of extensive research. 1,2,3,4 Small-scale studies have shown that substantial variation exists among clinicians in restorative treatment thresholds. 6,7,8,9,10 Not all of the thresholds can be appropriate; some may be too conservative and some too aggressive, but the “right” threshold has not been identified. At present, the only thresholds that can be definitely identified as not appropriate are those that call for surgical treatment when caries is confined to enamel, due to the potential for enamel lesions to arrest or reverse.11 Enamel-based thresholds for surgical treatment have become more of an issue as recent attention to risk assessment and development of diagnostic systems focus more attention on enamel lesions, alternatives to surgical treatment are shown to be effective,12,13 and long-term consequences of surgical treatment are considered.14,15,16,17,18
Two consequences merit particular consideration. First, the decision to place a restoration in an un-restored tooth will affect the prognosis of the tooth and the cost of treatment over its lifetime. Teeth with restorations are more likely to require additional restorations and other related treatments.19 Second, because future assessments of patients' risk of caries are often based on the number of existing restorations,20,16, 21,22 placing an initial restoration may alter a patient's risk profile, which in turn may alter future restorative decisions. Therefore, the profession needs to examine the extent to which clinicians employ enamel-based thresholds for surgical treatment and begin to formulate approaches to minimize their use.
This study has begun that process by determining the distribution of thresholds for surgical treatment and exploring the extent to which dentists' personal and practice characteristics are associated with enamel-based thresholds. The study was based in The Dental Practice-Based Research Network (DPBRN), which has a broad representation of practice types, treatment philosophies, and patient populations, including a substantial diversity in race, ethnicity, socio-economic status, geography and rural/urban area of residence among both its practitioner-investigators and the patients whom they serve. Our objectives were to: (1) quantify at which carious lesion depths dentists intervene surgically for cases of varying caries penetration and caries risk; (2) identify characteristics that are associated with surgical intervention.
Materials and Methods
The study design was cross-sectional, consisting of a single administration of a questionnaire to all DPBRN dentist practitioner-investigators who indicated on their enrollment questionnaire that they do at least some restorative dentistry in their practices (n=901). The study was approved by the respective Institutional Review Board (IRB) of all participating regions. Participants indicated their selection of treatment from among options for cases presented in the questionnaire. Three cases consisted of a clinical photograph of the occlusal surface of a mandibular first molar, together with a description of the patient. The treatment decision (how the dentist would treat the patient) for the case was requested under two different caries risk conditions; first, where the patient has minimal risk factors (the patient has no other teeth with dental restorations or dental caries and is not missing any teeth); and second, where the patient is clearly at high risk for caries (the patient has 12 teeth with existing dental restorations, heavy plaque and calculus, multiple Class V white spot lesions, and is missing five teeth). The photographs showed occlusal surfaces with increasing caries severity. Case 1 had a white or discolored enamel surface. Case 2 had brown discoloration in about half of the occlusal surface. Case 3 had brown discoloration in most of the fissures in the occlusal surface and had no cavitation. Cases 1 and 2 were considered lesions located in the outer and inner enamel, respectively. Case 3 was considered a dentin lesion located in the outer 1/3 of the dentin (Figure 1).23, 24, 25 For each case and each scenario the respondent provided treatment codes in a “check all that apply” format (see Figure 1). Options were then classified into the following categories: 1) no treatment, 2) minimally-invasive treatment, 3) preventive treatment, and 4) restorative treatment. Practitioner-investigators were also asked if they assessed caries risk for individual patients as part of their treatment plan.
Figure 1.
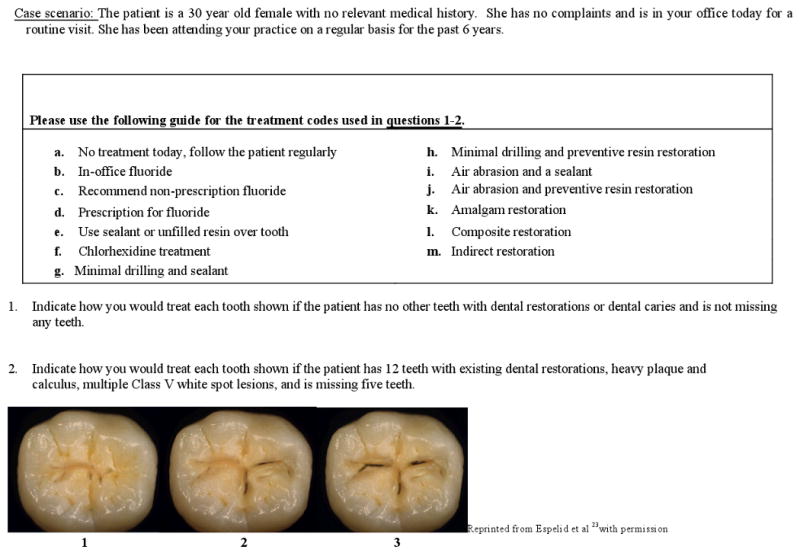
Questions asked of participating dentists:
Information regarding dentists' demographics and practice characteristics (Table 2) was already gathered through an enrollment questionnaire (www.dentalpbrn.org/users/related_links/default.asp), and results from this questionnaire suggest that DPBRN dentists have much in common with dentists at large.26
Table 2.
Dental Practice Characteristics Tested for their Association with Decision to Restore
| Practice Setting | Patient Population | Dental Procedure Characteristics | Dentist's Individual Characteristics |
|---|---|---|---|
| Practice busynessa | Dental insurance coverage | Percent of time each day doing restorative workb | Year of graduation from dental school |
| Waiting time for restorative dentistry | Practice charges by payment source | Percent of time each day doing esthetic workb | Race of dentist |
| Age distribution | Percent of time each day doing extractionsc | Gender of dentist | |
| Racial/ethnic distribution |
1=too busy to treat all people requesting appointments, 2=provided care to all who requested appointments, but the practice was overburdened; 3= provided care to all who requested appointments, and the practice was not overburdened; 4= not busy enough-the practice could have treated more patients
0=none; 1=1-30% of the time; 2=31 to 50% of the time; 3=more than 50% of the time.
0=none; 1=1-20% of the time; 2=21 to 30% of the time; 3=more than 30% of the time.
Data collection process
A pilot version of the questionnaire was submitted to 16 practitioner-investigators throughout the network. The pilot-testing assessed the feasibility and comprehension of each questionnaire item. A subsequent pre-testing phase finalized documentation of comprehension of questionnaire items and quantified test-retest reliability of questionnaire items, which involved 35 DPBRN dentists. Items had to meet a test-retest reliability of kappa > 0.7 to be considered sufficiently reliable for inclusion in the final version of the questionnaire. The lapse in time between test and retest was 15 days. The results of pilot and pre-testing were not included in the final results.
Pre-printed survey form packages were sent by the Coordinating Center to each regional office. These forms had the practitioner's self-checking identification number preprinted on each page of each form. Practitioner-investigators were asked to complete the questionnaire by hand and return to the assigned Regional Coordinator in a pre-addressed envelope. Upon receipt, the regional coordinator reviewed the questionnaire for completeness and sent it to the Coordinating Center.
Practitioners were remunerated after they had returned a completed questionnaire and had responded to possible queries from the Regional Coordinator having to do with verifying illegible or unclear responses.
Practitioner-investigators were requested to return the questionnaire within three weeks. A reminder letter was sent after the third week to clinicians who had not returned the questionnaire. After an additional three weeks, a second reminder was sent. After a final three-week waiting period, if a practitioner had not returned the questionnaire, it was assumed that he or she was not interested in participating.
Study Population
This study queried dentists working in outpatient dental practices who have affiliated with DPBRN to investigate research questions and to share experiences and expertise (n=1166). DPBRN comprises five regions: AL/MS: Alabama/Mississippi, FL/GA: Florida/Georgia, MN: dentists employed by HealthPartners (http://www.healthpartners.com/) and private practitioners in Minnesota, PDA: Permanente Dental Associates (http://permanentedental.kpnw.org/) in cooperation with Kaiser Permanente's Center for Health Research, and SK: Denmark, Norway, and Sweden.27 DPBRN dentists can also be characterized by “type of practice”, for which we categorized each dentist as being in either: (1) a solo or small group private practice (SGP); (2) a large group practice (LGP); or (3) a public health practice (PHP). “Small” practices were defined as those that had 3 or fewer dentists. Public health practices were defined as those that receive the majority of their funding from public sources. In the AL/MS and FL/GA regions, 99% of practitioner-investigators were in SGP and 1% were in PHP. In the MN region, 87% were in LGP and 13% were in SGP. In the PDA region, all were in LGP. In the SK region, 55% were in SGP and 45% were in PHP.
Participants of the DPBRN were recruited through continuing education courses and mass mailings to licensed dentists from the participating regions. As part of enrollment in DPBRN, all practitioner-investigators complete an enrollment questionnaire about their practice characteristics and themselves. The enrollment questionnaire26 and other details about DPBRN are provided at http://www.DentalPBRN.org.
Variable Selection
To identify characteristics that may be associated with inappropriate treatment threshold, explanatory variables were identified based on extant literature related to theoretical models of factors associated with dentists' treatment decisions and treatment received by patients. 28,29,30 The variables included in bivariate analyses of association were: gender and race/ethnicity of dentist, years since graduation from dental school, region of practice, type of practice, payment source from patients, practice busyness, time devoted to restorative dentistry, time devoted to esthetic dentistry, time devoted to extractions, and age distribution of patients seen in the practice. Additionally a logistic regression model was tested which included: type of practice, time devoted to restorative dentistry, assessment of caries risk, age distribution of patients, busyness of the practice, patients who self-pay, time devoted esthetic dentistry, and time devoted to extractions.
Statistical Analysis
Data were analyzed using SAS software version 9.1 (Cary, N.C.). Power analyses revealed that a sample size of 200 practitioners was deemed necessary to provide 90% power. A p-value of 0.05 or less was considered statistically significant. Before commencing analysis, a data conditioning step was conducted to create an overall treatment recommendation for each case within each scenario from the four variables that summarized treatment codes (no treatment, minimally-invasive treatment, preventive treatment, and restorative treatment). The overall variable had values with the following definitions: 1) no treatment – if the “no treatment” option was endorsed, 2) preventive only – if only the prevention option was endorsed, 3) preventive and minimally-invasive – if the prevention and minimally-invasive treatment options were endorsed, 4) preventive and restorative – if the prevention and restorative were the only options endorsed, 5) minimally-invasive treatment – if the minimally-invasive and restorative options were the only options endorsed, 6) restorative only – if the restoration option was solely endorsed.
An outcome variable was defined based on whether or not study participants recommended restorative treatment. Bivariate analyses of restorative outcome examined associations between the explanatory variables for low and high caries risk individuals. Chi-square tests were used for bivariate analysis when explanatory variables were categorical; t-tests were used when explanatory variables were continuous. Fisher's exact test was used for bivariate testing of categorical data in the case of sparse cell sizes. McNemar's test, appropriate for testing marginal homogeneity between paired categorical data, was used to determine if dentists reported the decision to restore differently for two caries risk scenarios. To simultaneously examine the effect of an explanatory variable on outcome after adjusting for the effect of other explanatory variables, logistic regressions were performed. Variables that were significant at the 0.10 level were included in logistic regression models. Due to the multicollinearity of region and “type of practice” and “race”, only the type of practice variable was tested in the logistic regression model.
Results
Of 901 mailed questionnaires, 519 (58%) were returned. Among the eligible participants who decided to participate, there were no differences by gender, area of specialty, or years since dental school graduation when compared to practitioners who chose not to participate. Among respondents, not all practitioners answered all the questions; consequently, some questions have different sample sizes.
Table 3 shows the distributions of treatment recommendations (based on the overall treatment variable) when the cases described the patient as having minimal risk factors. For Case 1, depicting a lesion in the outer enamel, the majority of dentists (69%) recommended no treatment, while 17% recommended preventive treatment only, and 14% recommended some form of surgical treatment. For Case 2, portraying a lesion in the inner enamel, 24% of respondents recommended no treatment, 13% recommended preventive treatment alone, and a majority of respondents (63%) recommended surgical treatment. For Case 3, which represented a lesion into the dentin, 90% of respondents recommended surgical treatment. The nature of the surgical treatment differed across the cases, with minimally invasive treatment without an accompanying preventive intervention comprising 65% (46/71), 65% (207/319), and 41% (191/466) of recommendations for Cases 1, 2, and 3 respectively.
Table 3.
Distribution of treatment options chosen by dentists for Cases 1 through 3 for a low caries risk individual (question 1)
| Number of responses | Case 1 n=512 |
Case 2 n=509 |
Case 3 n=514 |
|---|---|---|---|
| No treatment | 352 (69%) | 124 (24%) | 34 (7%) |
| Preventive only | 89 (17%) | 66 (13%) | 14 (3%) |
| Surgical Treatment* | 71 (14%) | 319 (63%) | 466 (90%) |
| Preventive and minimally-invasive | 23 | 69 | 92 |
| Preventive and restorative | 0 | 9 | 44 |
| Minimally-invasive | 46 | 207 | 191 |
| Restorative only | 2 | 34 | 139 |
The area highlighted in gray shows a frequency breakdown of the surgical treatment options.
Table 4 shows recommended treatment distributions (based on the overall treatment variable) when the cases described the patient as being at high risk for caries. Here the patterns seen in the low risk cases were repeated, but with larger proportions of recommendations involving surgical treatment. A quarter of dentists recommended surgical treatment for Case 1, 77% for Case 2, and 94% for Case 3. Again, the nature of the surgical treatment differed across the cases, with minimally invasive treatment without an accompanying preventive intervention comprising 40% (51/129), 34% (135/394), and 16% (78/482) of recommendations for Cases 1, 2, and 3 respectively.
Table 4.
Distribution of treatment options chosen by dentists for Cases 1 through 3 for a high caries risk individual (question 2)
| Number of responses | Case 1 n=514 |
Case 2 n=514 |
Case 3 n=514 |
|---|---|---|---|
| No treatment | 206 (40%) | 52 (10%) | 15 (3%) |
| Preventive only | 179 (35%) | 68 (13%) | 17 (3%) |
| Surgical* | 129 (25%) | 394 (77%) | 482 (94%) |
| Preventive and minimally-invasive | 65 | 155 | 117 |
| Preventive and restorative | 5 | 36 | 127 |
| Minimally-invasive | 51 | 135 | 78 |
| Restorative only | 8 | 68 | 160 |
The area highlighted in gray shows a frequency breakdown of the surgical treatment option.
For the sake of brevity, only Cases 2 and 3 were illustrated in Tables 5 and 6, which show distributions for explanatory variables among those recommending surgical treatment in low and high caries risk individuals, respectively. Significant differences were found for the participating practices according to region (Case 2: low risk, p=.0015, high risk, p<.001; Case 3: low risk, p<.001, high risk, p<.001). In the low caries risk scenario (Table 5), practitioner-investigators from the FL/GA, MN, PDA, and SK regions were less likely to recommend intervening surgically on enamel lesions than practitioner-investigators from the AL/MS region. The same pattern held in a high caries risk scenario (Table 6). Practitioner-investigators from the PDA region were less likely to intervene surgically on caries in the outer 1/3 of the dentin.
Table 5.
Dentists and practice characteristics of dentists, by whether they recommended surgical treatment for Case 2 and Case 3 based on a scenario for a low caries risk individual.
| Characteristics Overall (517**) | Percent who recommended restoration for Case 2 N=509 9% | p-value | Percent who recommended restoration for Case 3 N=514 41% | p-value |
|---|---|---|---|---|
| Gender | ||||
| Male (424) | 10% | 0.166 | 42% | 0.205 |
| Female (93) | 6% | 35% | ||
| Race | ||||
| White (461) | 9% | 0.461 | 41% | 0.534 |
| Hispanic (12) | 8% | 25% | ||
| Black (18) | 17% | 50% | ||
| Other (22) | 13% | 35% | ||
| Years since graduation from dental school | ||||
| mean (SD) recommend | 20 (11) | 0.960 | 19 (10) | 0.228 |
| mean (SD) did not recommend | 20 (10) | 20 (10) | ||
| Region | ||||
| AL/MS (296) | 14% | 0.0015* | 52% | <0.001* |
| FL/GA (102) | 5% | 36% | ||
| MN (31) | 6% | 19% | ||
| PDA (50) | 0% | 14% | ||
| SK (38) | 3% | 16% | ||
| Type of practice | ||||
| LGP (77) | 1% | 0.007* | 14% | <0.001* |
| SGP (419) | 11% | 46% | ||
| PHP (21) | 0% | 29% | ||
| Percent of patients who self-pay | ||||
| 0 % (15) | 0% | 0.600 | 13% | <0.001* |
| 1-30% (242) | 10% | 41% | ||
| 31-50% (127) | 11% | 54% | ||
| >50% (107) | 10% | 31% | ||
| Percent of patients who are under 19 | ||||
| 0-10% (200) | 8% | .132 | 41% | .707 |
| 11-20% (161) | 8% | 43% | ||
| >20% (140) | 14% | 38% | ||
| Time devoted to restorative dentistry | ||||
| 0-50% (202) | 12% | .280 | 41% | .506 |
| 51-80% (264) | 8% | 43% | ||
| >80% (45) | 9% | 33% | ||
| Time devoted to esthetic dentistry | ||||
| 0 % (8) | 0% | .797 | 13% | .408 |
| 1-30% (418) | 9% | 41% | ||
| 31-50% (50) | 8% | 42% | ||
| >50% (22) | 13% | 45% | ||
| Time devoted to extractions | ||||
| 0% (11) | 0% | .204 | 27% | .647 |
| 1-20% (447) | 9% | 41% | ||
| >20% (36) | 17% | 42% | ||
| Practice busyness | ||||
| Too busy to treat (55) | 11% | .436 | 33% | .258 |
| Overburdened (90) | 11% | 41% | ||
| Not overburdened (277) | 8% | 40% | ||
| Not busy enough (79) | 13% | 49% | ||
| Assessment of caries risk | ||||
| Yes (358) | 9% | 0.469 | 39% | 0.064 |
| No (135) | 11% | 48% |
Overall sample size for table, n=517, is the number of dentists who responded to surgical intervention question for Case 2 or Case 3
statistical significance from t-test (numerical variable) and chi-square tests (categorical variables) or Fisher's exact tests (when chi-square test assumptions violated)
Table 6.
Dentists and practice characteristics of dentists, by whether they recommended surgical treatment for Case 2 and Case 3 based on a scenario for a high caries risk individual.
| Characteristic Overall | Percent who recommended restoration for Case 2 | p-value | Percent who recommended restoration for Case 3 | p-value |
|---|---|---|---|---|
| (517**) | 22% | 60% | ||
| Gender | ||||
| Male (424) | 24% | 0.046* | 60% | 0.904 |
| Female (93) | 14% | 61% | ||
| Race | ||||
| White (461) | 22% | 0.470 | 60% | 0.284 |
| Hispanic (12) | 8% | 50% | ||
| Black (18) | 17% | 78% | ||
| Other (22) | 32% | 50% | ||
| Years since graduation from dental school | ||||
| mean (SD) recommend | 19 (11) | 0.550 | 20 (10) | 0.331 |
| mean (SD) did not recommend | 20 (10) | 21 (10) | ||
| Region | ||||
| AL/MS (296) | 30% | <0.001* | 73% | <0.001* |
| FL/GA (102) | 17% | 61% | ||
| MN (31) | 10% | 48% | ||
| PDA (50) | 4% | 16% | ||
| SK (38) | 8% | 29% | ||
| Type of practice | ||||
| LGP (77) | 5% | <0.001* | 27% | <0.001* |
| SGP (419) | 26% | 68% | ||
| PHP (21) | 10% | 38% | ||
| Percent of patients who self-pay | ||||
| 0 % (15) | 0% | 0.089 | 27% | <0.001* |
| 1-30% (242) | 22% | 60% | ||
| 31-50% (127) | 27% | 77% | ||
| >50% (107) | 19% | 48% | ||
| Percent of patients who are under 19 | ||||
| 0-10% (200) | 18% | .133 | 57% | .090 |
| 11-20% (161) | 24% | 59% | ||
| >20% (140) | 26% | 68% | ||
| Time devoted to restorative dentistry | ||||
| 0-50% (202) | 24% | .330 | 62% | .239 |
| 51-80% (264) | 23% | 62% | ||
| >80% (45) | 14% | 49% | ||
| Time devoted to esthetic dentistry | ||||
| 0 % (8) | 0% | .337 | 38% | .446 |
| 1-30% (418) | 23% | 61% | ||
| 31-50% (50) | 20% | 66% | ||
| >50% (22) | 14% | 67% | ||
| Time devoted to extractions | ||||
| 0% (11) | 9% | .151 | 45% | .336 |
| 1-20% (447) | 22% | 61% | ||
| >20% (36) | 33% | 69% | ||
| Practice busyness | ||||
| Too busy to treat (55) | 11% | .088 | 55% | .234 |
| Overburdened (90) | 22% | 59% | ||
| Not overburdened (277) | 22% | 60% | ||
| Not busy enough (79) | 29% | 71% | ||
| Assessment of caries risk | ||||
| Yes (358) | 21% | 0.124 | 57% | 0.004* |
| No (137) | 27% | 71% | ||
Overall sample size for table, n=517, is the number of dentists who responded to surgical intervention question for Case 2 or Case 3
statistical significance from t-test (numerical variable) and chi-square tests (categorical variables) or Fisher's exact tests (when chi-square test assumptions violated)
Additionally, significant differences were found according to the type of practice (Case 2: low risk, p=.0015, high risk, p<.001; Case 3: low risk, p<.001, high risk, p<.001). In the low caries risk scenario (Table 5), practitioner-investigators who work in LGP practices were less likely to recommend intervening surgically on enamel lesions than practitioner-investigators who work in SGP practices. In a high-risk scenario (Table 6), practitioner-investigators from LGP and PHP models were less likely to recommend intervening surgically on enamel lesions, as compared to practitioner-investigators in the SGP model.
In a high caries risk scenario (Table 6), male practitioner-investigators intervened more frequently on enamel lesions (Case 2) than female practitioner-investigators.
Seventy-two percent of dentists (n=358) reported that they assess patients' caries risk. From these only eighteen percent (n=63) use a special form for caries risk assessment. Dentists from PDA (100%), SK (94%), and MN (93%) regions reported assessing caries risk significantly more often than dentists from AL/MS (65%) and FL/GA (63%) regions. McNemar's test was used to determine if dentists reported the decision to restore differently for the two caries risk scenarios. Significant differences (p<.001) were found on both Case 2 and Case 3 regarding the caries risk scenario. For Case 2, 9% decided to intervene in the low risk scenario compared to 22% in the high risk scenario. For Case 3, 40% decided to intervene in the low risk scenario compared to 60% in the high risk scenario. Practitioner-investigators who assessed caries risk were less likely to intervene on dentin caries in the outer 1/3.
Regardless of the caries risk scenario, practices that have a smaller percent of patients who self-pay were less likely to intervene on dentin lesions (Case 3) on both caries risk scenarios (Table 5 and Table 6).
The dental insurance variable had these categories: covered by a private insurance program that pays for some or all of their dental care; covered by a public program that pays for some or all of their dental care; not covered by any third party and pay their own bills; not covered by any third party and receive free care or for a fee that you reduce substantially. For respondents to the Assessment of Caries Diagnosis and Treatment Questionnaire, 58% of patients were covered by private insurance; 15% by public insurance; 27% not covered by any program (Makhija et al. Gen Dent, 2009).
In Case 3, low caries risk scenario, type of practice and payment source from patients were significantly related to surgical treatment and included in a logistic regression model. Significant ORs were: SGP vs. LGP, OR=7.2 (95% CI: [3.4,15.7]); 1%-30% self-pay vs. greater than 50%, OR=2.3 (95% CI: [1.4,3.8]); and 31%-50% self-pay vs. greater than 50% self-pay OR=2.6 (95% CI: [1.5,4.4]).
In Case 2, high caries risk scenario, type of practice, payment source from patients, and gender were included in the logistic regression model. The only significant OR was SGP vs. LGP, OR=15.6 (95% CI: [3.7,66.0]). In Case 3, high caries risk scenario, type of practice, payment source from patients, and assessment were included in the logistic regression model. Significant ORs were: SGP vs. LGP, OR=9.2 (95% CI: [4.6,18.3]); 1%-30% self-pay vs. greater than 50%, OR=2.9 (95% CI: [1.7,4.8]); and 31%-50% self-pay vs. greater than 50% self-pay, OR=3.5 (95% CI: [2.0,6.3]).
DISCUSSION
Occlusal fissures of the first permanent molar are generally the first sites in the permanent dentition to develop caries.31,32 Therefore, it is the most critical area when deciding on treatment of dental caries (shown in Cases 1, 2, and 3). In the current study, most dentists, irrespective of patient's caries risk, chose not to restore an enamel lesion in the absence of dark brown pigmentation (as shown in Case 1). However, a substantial minority of dentists readily changed their treatment option to surgical treatment if some minor brown pigmentation was present on enamel as illustrated in Case 2. A study by Thylstrup and Qvist 33 (1987) reported no presence of bacteria in dentinal tubules on active enamel carious lesions with minor cavitations, despite the appearance of brown discoloration. Minimal intervention treatment including tracing pit and fissure with extremely small bur and air abrasion techniques causes less destruction of tooth structure than conventional surgical techniques. 34,35,36,37 However, it is still a surgical treatment procedure and should only be used to access caries that cannot be remineralized. In recent years, there has been pronounced change in the epidemiology and disease pattern of dental caries. 39, 40, 41 Progression of enamel caries is now slower, and allows preventive intervention before the stage of irreversible destruction of the tooth is reached. There is also a pronounced reduction in lesion development on smooth surfaces accessible to fluoride. 42, 43, 44 Therefore, current expert opinion suggests that surgical treatment for non-cavitated lesions is inappropriate.45 The study found that fewer practitioners recommended preventive treatment where the lesion was more severe (Table 3). This fact was observed irrespective of patient's caries risk. Dentists seem to approach carious lesions as a separate entity and not as a consequence of the disease process. Extensive literature suggests that the “cure” for the caries disease does not rely on the placement of a restoration, but on patient education and individual assessment of caries risk followed by a change in the environment of this multi-factorial disease.46,47
A photograph cannot replicate all the nuances that can be perceived in a real tooth and therefore we cannot state with certainty that the decision making context provided by this questionnaire entirely duplicated the real-world clinical context. Also, it is possible that respondents may have misinterpreted the severity of the lesions depicted in the photographs. Nonetheless, it is unlikely that such misinterpretation could occur differentially by the explanatory variables examined in this study. Thus, the differences in willingness to intervene surgically are likely reflections of true differences in dentists' beliefs about what represents the appropriate point in lesion progression to initiate such treatment.
We used the occlusal photograph caries model23 in this questionnaire to see how dentists' responses varied given the same stimulus. The results of reliability tests suggested that the clinical photographs were an instructive method to meet the stated objectives of the study. It is common when quantifying test/re-test reliability for the time elapsed to be only three days. In this study, the time for the reliability test was extended to 15 days so that respondents would be less likely to remember their responses.
The sample used in this manuscript seems to be generalizable to dentists who meet the eligibility requirements. There were no significant differences between enrolled U.S. DPBRN respondents and general practitioners who participated in the ADA survey to which they were compared, based on these characteristics: gender; number of offices at which the dentist practices; insurance coverage by patients in the practice, number of operatories, patient visits per week, number of days waiting for a new patient examination, and number of minutes waiting in the waiting room (Makhija et al. Gen Dent, 2009)[this should be converted to a superscript]. The only significant difference observed was that DPBRN practitioner-investigators are more likely to be recent graduates. Region and practice type can almost be used interchangeably in this analysis because the regions participating in DPBRN are mainly differentiated by their practice type, as detailed in the Methods section. Although some dentists reported not routinely using caries risk assessment, this did not seem crucial to how dentists treatment plan patients, based on their responses to low and high caries risk scenarios. McNemar's Test showed significant differences on how dentists approach the treatment threshold based on caries risk, regardless of whether they routinely assess caries risk. A possible explanation for this finding is that although dentists may not formally assess patients caries risk, intrinsically they rationalize findings from the data collection and incorporate them into their decision to restore according to different caries risk. In other words, some sort of assessment of patients' caries risk is done indirectly.
Dentists in Scandinavia chose not to restore lesions that were limited to enamel; restorative treatment was indicated predominantly for occlusal surfaces that involved dentin. Other studies in Scandinavia have reported similar findings. 48,49 In Scandinavian dental schools, preventive and restorative dentistry have been integrated in the undergraduate curriculum as one subject, “cariology”. Current treatment strategy in Scandinavia is based on diagnosis of caries activity, identification of the main causal and predisposing factors in the individual case, and assessment of the actual caries risk.50 In contrast, in North American dental schools this concept has been introduced relatively recently. 51,52 Additionally, Scandinavian dental practices have changed the clinical criteria for intervention in the caries process. More restrictive criteria for placement of the first restoration are currently in place53 as a result of studies that have successfully monitored interproximal enamel lesions. 7, 8. The criteria for placement of the first restoration may decrease over-treatment54 and consequently reduce the cost of care.
Patient's cultural background may be an important predictor of oral health. 55,56,57 The patient population of the Scandinavian region is substantially different from the US patient population. The recall frequency by Scandinavian patients is more predictable, so Scandinavian dentists are more comfortable with monitoring initial lesions and the governments are more involved in health management in Scandinavia. In fact, the Norwegian Public Oral Health Act of 1983 (http://www.lovdata.no/all/nl-19830603-054.htm) states that prevention must be attempted before treatment. Prevention is promoted extensively through health promoting activities which even included sugar-free sports events. Lill Karin Wendt in Sweden has presented a model of preventing dental caries in small children by using fancy bottles with fresh water instead of sugary drinks.58 A cohort epidemiological study done in Sweden from 1973 through 2003 shows an overall improvement in oral health over the 30-year period.59 Half of participating DPBRN practices in Scandinavia are public health practices supported by the government.
It is not clear whether the proportion of patients who have no dental insurance (percent self-pay) is also a factor influencing determining decisions to intervene surgically. This variable entered the regression models largely because of the effect of 15 respondents who indicated that there were no self-pay patients in their practices. These practices were markedly different than practices in all other categories of self pay, one of which was practices with 30% or fewer of such patients. Further, there was no “dose-response” effect across the remaining three categories of self pay patients. It is more likely that the entrance of this variable represents an outlier effect due to differences in these 15 practices than it does a more generalized relationship between the presence of self-pay patients in dental practices after practice type has been accounted for.
Regarding surgical treatment in the outer dentin (Case 3), large differences were evident in the recommendations made by practitioner-investigators from the AL/MS and FL/GA regions when compared to practitioner-investigators from the other regions. Both the AL/MS and FL/GA regions are composed of private practitioners who are generally graduates of Southeast and Northeast dental schools, with a good mix of rural/urban patient populations and some diversity among dentists and patients regarding race/ethnicity. Patient socio-economic status and demographics have been previously recognized as being important factors in the restorative dentistry decision making process.29 Treatment choices can also be influenced by patient preferences and third party payments reimbursement. Additionally, except for the Scandinavia region, the regional differences are more reflective of practice type (e.g., “private” versus “large group practice”) than geographical location. The participating practices from the AL/MS and FL/GA regions were mostly private practitioners with a few practitioners working in public health settings. In private practice, the cost of practicing and revenue are a function of the number and type of procedures being done and amount of time used to deliver the services. In private practice, dentists also direct the dental care with individual practice philosophies and diagnostic criteria. Operational and management considerations direct and influence the treatment choices. Therefore, the individual dentist is responsible for all decisions and outcomes.
Both PDA and MN have a preponderance of graduates of Northwest and Midwest dental schools, and primarily comprise large group practices or “health maintenance organizations” (HMO). The MN region is composed primarily of dentists who are associated with HealthPartners Dental Group (HP). PDA is a professional corporation operated by 110 general dentists which contracts with Kaiser Foundation Health Plan, to treat Kaiser Permanente patients in the Northwest Region. Both HP and PDA are prepaid, multi-specialty dental groups that operate as part of a comprehensive health care organization. The delivery of care is based on evidence-based dentistry with a focus on management of the caries disease process through risk assessment, risk reduction, and preservation of hard and soft tissue. Dentists participating in HP and PDA have a fixed base salary and annual individual incentive programs. Therefore, dentists are not solely reimbursed based on the number of procedures. Actually, dentists in the PDA region are reimbursed based on applying evidence-based principles into their clinical practices such as placement of sealants and individual preventive treatments. This level of organization might enable HP and PDA dentists to use standardized training and diagnostic tools more consistently than dentists in solo or small group private practices. Additionally, PDA and the HP dental group in the MN region have both independently developed their own manual for caries risk assessment, which have specific recommendations for the assessment of caries risk and identify protocols for the radiographic and clinical diagnosis of dental caries.
The current study did not query whether or not participating dentists regularly attend Continuing Education courses on minimally invasive dentistry techniques. However, non-surgical treatment for non-cavitated lesions has been validated through publication and national consensus. Despite this fact, some dentists still choose to treat incipient caries lesions surgically. Significant differences were evident between SGP and LGP models. Part of the explanation for this difference may be related to the pace at which new information is translated into practice. This pace might be faster in group practices than in more-isolated solo practices. In general, the translation of research into clinical practice has been a slow process. It is estimated that only 14 percent of new science enters daily clinical practice, and that process takes an estimated average of 17 years.60
Conclusion
Dentists' responses were quite varied regarding when to intervene surgically in the caries process. Most dentists chose to provide some treatment to lesions that were within the inner part of the enamel. Almost all dentists chose to surgically restore dentin lesions.
Decisions to intervene surgically in the caries process differ by caries lesion depth, patient caries risk, assessment of caries risk, type of practice model, and percent of patients who self-pay.
Table 1.
The treatment options provided for restoring Cases 1 through Case 3
| Treatment Option | Treatment Description |
|---|---|
| No treatment | No treatment should be delivered |
| Preventive treatment only | In-office fluoride, non-prescription fluoride, prescription of fluoride, sealant, chlorhexidine treatment |
| Surgical treatment | Minimally-invasive treatment only, done through either 1) minimal drilling and sealant, 2) minimal drilling and preventive resin restoration, 3) air abrasion and sealant, or 4) air abrasion and preventive resin restoration |
| Restorative treatment only, done through either 1) amalgam restoration, 2) composite restoration, or 3) indirect restoration | |
| Preventive treatment option combined with minimally-invasive treatment | |
| Preventive treatment option combined with restorative treatment |
Acknowledgments
The authors would like to thank Dr. Ivar Mjör, who served as a consultant during the planning phase of the research project, and all DPBRN practitioner-investigators who responded to the questionnaire. Furthermore, the authors would like to acknowledge grants U01-DE-16746 and U01-DE-16747 from NIDCR-NIH. Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. The informed consent of all human subjects who participated in this investigation was obtained after the nature of the procedures had been explained fully.
Footnotes
The DPBRN Collaborative Group comprises practitioner-investigators, faculty investigators, and staff investigators who contributed to this DPBRN activity. A list of these persons is at http://www.dpbrn.org/users/publications/Default.aspx
Clinical Significance: The threshold for surgical treatment of caries lesions depends on various factors, including the type of dental practice model.
Contributor Information
Dr. Valeria V Gordan, College of Dentistry, Department of Operative Dentistry at University of Florida, Gainesville, Florida, USA.
Dr. James D Bader, School of Dentistry, Department of Operative Dentistry at the University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, USA.
Dr. Cynthia W Garvan, College of Education, University of Florida, Gainesville, Florida, USA.
Dr. Joshua S Richman, Preventive Medicine and Biostatistics, University of Alabama at Birmingham, Birmingham, Alabama, USA.
Dr Odont Vibeke Qvist, Department of Cariology and Endodontics, School of Dentistry, Faculty of Health Sciences, University of Copenhagen, Copenhagen, Denmark.
Dr. Jeffrey L Fellows, Center for Health Research, Kaiser Permanente Northwest, Portland, Oregon, USA.
Dr. D. Brad Rindal, HealthPartners, Minneapolis, Minnesota, USA.
Dr. Gregg H Gilbert, Department of General Dental Sciences, School of Dentistry, University of Alabama at Birmingham, Birmingham, Alabama, USA.
References
- 1.Pitts NB. Diagnostic tools and measurements – impact on appropriate care. Community Dent Oral Epidemiol. 1997;25:24–35. doi: 10.1111/j.1600-0528.1997.tb00896.x. [DOI] [PubMed] [Google Scholar]
- 2.Pitts NB, Stamm JW, editors. Proceedings from the international consensus workshop on caries clinical trials. J Dent Res. 2004;83 doi: 10.1177/154405910408301s27. Spec Issue C. [DOI] [PubMed] [Google Scholar]
- 3.Traebert J, Marcenes W, Kreutz JV, Oliverira R, Piazza CH, Peres MA. Brazilian dentists' restorative treatment decisions. Oral Health Prev Dent. 2005;3:53–60. [PubMed] [Google Scholar]
- 4.Innes NP, Stirrups DR, Evans DJ, Hall N, Leggate M. A novel technique using performed metal crowns for managing carious primary molars in general practice-a retrospective analysis. Br Dent J. 2006;200:451–454. doi: 10.1038/sj.bdj.4813466. [DOI] [PubMed] [Google Scholar]
- 5.Slade GD, Rozier RG, Zeldin LP, Margolis PA. Training pediatric health care providers in prevention of dental decay: results from a randomized controlled trial. BMC Health Serv Res. 2007;7:176. doi: 10.1186/1472-6963-7-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thylstrup A, Bille J, Qvist V. Radiographic and observed tissue changes in approximal carious lesions at the time of operative treatment. Caries Res. 1986;20:75–84. doi: 10.1159/000260923. [DOI] [PubMed] [Google Scholar]
- 7.Mejare I, Sundberg H, Espelid I, Tveit AB. Caries and restorative treatment thresholds by Swedish dentists. Acta Odontol Scand. 1999;57:149–154. doi: 10.1080/000163599428887. [DOI] [PubMed] [Google Scholar]
- 8.Tveit AB, Espelid I, Skodje F. Restorative treatment decisions on approximal caries in Norway. Int Dent J. 1999;49:165–172. doi: 10.1002/j.1875-595x.1999.tb00902.x. [DOI] [PubMed] [Google Scholar]
- 9.Yorty JS, Brown KB. Caries risk assessment/treatment programs in US dental schools. J Dent Educ. 1999;63:745–747. [PubMed] [Google Scholar]
- 10.Clark TD, Mjör IA. Current teaching of cariology in North American dental schools. Oper Dent. 2001;26:412–418. [PubMed] [Google Scholar]
- 11.American Dental Association Council on Scientific Affairs. Professionally applied topical fluoride: evidence-based clinical recommendations. JADA. 2006;137(8):1151–1159. doi: 10.14219/jada.archive.2006.0356. [DOI] [PubMed] [Google Scholar]
- 12.Marinho VC, Higgins JP, Logan S, Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2002;(3):CD002279. doi: 10.1002/14651858.CD002279. [DOI] [PubMed] [Google Scholar]
- 13.Moberg Skold U, Petersson LG, Lith A, Birkhed D. Effect of school-based fluoride varnish programmes on approximal caries in adolescents from different caries risk areas. Caries Res. 2005;39(4):273–279. doi: 10.1159/000084833. [DOI] [PubMed] [Google Scholar]
- 14.Gordan VV. In vitro evaluation of margins of replaced resin based composite restorations. J Esthet Dent. 2000;12:217–223. doi: 10.1111/j.1708-8240.2000.tb00223.x. [DOI] [PubMed] [Google Scholar]
- 15.Gordan VV. Clinical evaluation of replacement of class V resin based composite restorations. J Dent. 2001;29:485–488. doi: 10.1016/s0300-5712(01)00030-6. [DOI] [PubMed] [Google Scholar]
- 16.Anusavice KJ. Clinical decision-making for coronal caries management in the permanent dentition. J Dent Educ. 2001;65:1143–1146. [PubMed] [Google Scholar]
- 17.Anusavice KJ, Benn DK. Is it time to change state and regional dental licensure board exams in response to evidence from caries research? Crit Rev Oral Biol Med. 2001;12:368–372. doi: 10.1177/10454411010120050101. [DOI] [PubMed] [Google Scholar]
- 18.Gordan VV, Mondragon E, Shen C. Evaluation of the cavity design, cavity depth, and shade matching in the replacement of resin based composite restorations. Quintessence Inter. 2002;32:273–278. [PubMed] [Google Scholar]
- 19.Shugars DA, Bader JD. Cost implications of differences in dentists' restorative treatment decisions. J Public Health Dent. 1996;56:219–222. doi: 10.1111/j.1752-7325.1996.tb02439.x. [DOI] [PubMed] [Google Scholar]
- 20.Anusavice KJ. Treatment regimens in preventive and restorative dentistry. J Am Dent Assoc. 1995;126:727–743. doi: 10.14219/jada.archive.1995.0267. [DOI] [PubMed] [Google Scholar]
- 21.Fontana M, Zero DT. Assessing patients' caries risk. J Am Dent Assoc. 2006;137:1231–1239. doi: 10.14219/jada.archive.2006.0380. [DOI] [PubMed] [Google Scholar]
- 22.Featherstone JD, Domejean-Orliaguet S, Jenson L, Wolff M, Young DA. Caries risk assessment in practice for age 6 through adult. J Calif Dent Assoc. 2007;35:703–707. 710–713. [PubMed] [Google Scholar]
- 23.Espelid I, Tveit AB, Mejáre I, Nyvad B. Caries - New knowledge or old truths? The Norwegian Dental Journal. 1997;107:66–74. [Google Scholar]
- 24.Ekstrand KR, Ricketts DN, Kidd EA, Qvist V, Schou L. Detection, diagnosing, monitoring and logical treatment of occlusal caries in relation to lesion activity and severity: An in vivo examination with histological validation. Caries Res. 1998;32:247–54. doi: 10.1159/000016460. [DOI] [PubMed] [Google Scholar]
- 25.Ekstrand KR, Martignon S, Ricketts DNJ, Qvist V. Detection and activity assessment of primary coronal caries lesions: A methodologic study. Operative Dent. 2007;32:225–235. doi: 10.2341/06-63. [DOI] [PubMed] [Google Scholar]
- 26.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ, Qvist V, DPBRN Collaborative Group Dentists in practice-based research networks have much in common with dentists at large: evidence from The Dental PBRN. Gen Dent. 2009;57:270–275. [PMC free article] [PubMed] [Google Scholar]
- 27.Gilbert GH, Williams OD, Rindal DB, Pihlstrom DJ, Benjamin PL, Wallace MA, DPBRN Collaborative Group The creation and development of The Dental Practice-Based Research Network. J Am Dent Assoc. 2008;139:74–81. doi: 10.14219/jada.archive.2008.0024. [DOI] [PubMed] [Google Scholar]
- 28.Bader JD, Shugars DA. What do we know about how dentists make caries-related treatment decisions? Community Dent Oral Epidemiol. 1997;25:97–103. doi: 10.1111/j.1600-0528.1997.tb00905.x. [DOI] [PubMed] [Google Scholar]
- 29.Gilbert GH, Duncan RP, Vogel WB. Determinants of dental care use in dentate adults: six-monthly use during a 24-month period in the Florida Dental Care Study. Soc Sci Med. 1998;47:727–737. doi: 10.1016/s0277-9536(98)00148-8. [DOI] [PubMed] [Google Scholar]
- 30.Gilbert GH, Shewchuk RM, Litaker MS. Effect of dental practice characteristics of racial disparities in patient-specific tooth loss. Med Care. 2006;44:414–420. doi: 10.1097/01.mlr.0000207491.28719.93. [DOI] [PubMed] [Google Scholar]
- 31.Ekstrand KR, Ricketts DN, Kidd EA. Occlusal caries: pathology, diagnosis and logical management. Dent Update. 2001;28:380–387. doi: 10.12968/denu.2001.28.8.380. [DOI] [PubMed] [Google Scholar]
- 32.Kidd EAM, Ricketss DNJ, Pitts NB. Occlusal caries diagnosis: a changing challenge for clinicians and epidemiologists. J Dent. 1993;21:323–331. doi: 10.1016/0300-5712(93)90001-7. [DOI] [PubMed] [Google Scholar]
- 33.Ekstrand K, Qvist V, Thylstrup A. Light microscope study of the effect of probing in occlusal surfaces. Caries Res. 1987;21(4):368–74. doi: 10.1159/000261041. [DOI] [PubMed] [Google Scholar]
- 34.Mount GJ, Ngo H. Minimal intervention: a new concept for operative dentistry. Quintessence Int. 2000;31:527–533. [PubMed] [Google Scholar]
- 35.White JM, Eakle WS. Rationale and treatment approach in minimally invasive dentistry. J Am Dent Assoc. 2000;131:13S–19S. doi: 10.14219/jada.archive.2000.0394. [DOI] [PubMed] [Google Scholar]
- 36.Peters MC, McLean ME. Minimally invasive operative care. I. Minimal intervention and concepts for minimally invasive cavity preparations. J Adhes Dent. 2001;3:7–16. [PubMed] [Google Scholar]
- 37.Mandari GJ, Frencken JE, van't Hof MA. Six-year success rates of occlusal amalgam and glass-ionomer restorations placed using three minimal intervention approaches. Caries Res. 2003;37:246–253. doi: 10.1159/000070866. [DOI] [PubMed] [Google Scholar]
- 38.Burke FJT. From extension for prevention to prevention of extension: (Minimal intervention dentistry) Dent Update. 2003;30:492–498. 500–502. doi: 10.12968/denu.2003.30.9.492. [DOI] [PubMed] [Google Scholar]
- 39.Hugoson A, Koch G, Hallonsten AL, Norderyd J, Åberg A. caries prevalence and distribution in 3-20-years-olds in Jönköping, Sweden, in 1973, 1978, 1983, 1993. Community Dent Oral Epidemiol. 2000;28:83–89a. doi: 10.1034/j.1600-0528.2000.028002083.x. [DOI] [PubMed] [Google Scholar]
- 40.Hugoson A, Koch G, Slotte C, Bergendal T, Thorstensson B, Thorstensson H. Caries prevalence and distribution in 20-80-years-olds in Jönköping, Sweden, in 1973, 1983, 1993. Community Dent Oral Epidemiol. 2000;28:90–96b. doi: 10.1034/j.1600-0528.2000.028002090.x. [DOI] [PubMed] [Google Scholar]
- 41.Mathaler TM. Caries status in Europe and predictions of future trends. Caries Res. 1990;24:381–396. doi: 10.1159/000261302. [DOI] [PubMed] [Google Scholar]
- 42.Twesme DA, Firestone AR, Heaven TJ, Feagin FF, Jacobson A. Air-rotor stripping and enamel demineralization in vitro. Am J Orthod Dentofacial Orthop. 1994;105:142–152. doi: 10.1016/S0889-5406(94)70110-5. [DOI] [PubMed] [Google Scholar]
- 43.Sawyer KK, Donly KJ. Remineralization effects of a sodium fluoride bioerodible gel. Am J Dent. 2004;17:245–248. [PubMed] [Google Scholar]
- 44.Donly KJ, Brown DJ. Indetify, protect, restore: emerging issues in approaching children's oral health. Gen Dent. 2005;53:106–110. [PubMed] [Google Scholar]
- 45.National Institutes of Health. Consensus Development Conference Statement. Diagnosis and management of dental caries throughout life. 2001 http://consensus.nih.gov/2001/2001Dentalcaries115html.htm.
- 46.Bader JD, Shugars DA, Bonito AJ. Systematic reviews of selected caries prevention and management methods. Community Dent Oral Epidemiol. 2001;29:399–411. doi: 10.1034/j.1600-0528.2001.290601.x. [DOI] [PubMed] [Google Scholar]
- 47.Young DA, Featherstone JDB, Roth JR. Curing the silent epidemic: Caries management in the 21st century and beyond. Calif Dent Assoc J. 2007;35:681–685. [PubMed] [Google Scholar]
- 48.Lith A, Pettersson LG, Grondahl HG. Radiographic study of approximal restorative treatment in children and adolescents in two Swedish communities differing in caries prevalence. Community Dent Oral Epidemiol. 1995;23:211–6. doi: 10.1111/j.1600-0528.1995.tb00233.x. [DOI] [PubMed] [Google Scholar]
- 49.Lith A, Lindstrand C, Grondahl HG. Caries development in a young population managed by a restrictive attitude to radiography and operative intervention: II. A study at the surface level. Dentomaxillofac Radiol. 2002;31:232–9. doi: 10.1038/sj.dmfr.4600705. [DOI] [PubMed] [Google Scholar]
- 50.Lagerlöf F, Oliveby A. Clinical implications: new strategies for caries treatment. In: Stookey GK, editor. Early detection of dental caries Indianapolis. IN: School of Dentistry, Indiana University; 1996. pp. 297–316. [Google Scholar]
- 51.Ismail AI. Clinical diagnosis of precavitated carious lesions. Community Dent Oral Epidemiol. 1997;25:13–23. doi: 10.1111/j.1600-0528.1997.tb00895.x. [DOI] [PubMed] [Google Scholar]
- 52.Lundeen TF, Roberson TM. Cariology: the lesion, etiology, prevention, and control. In: Sturdevant CM, Roberson TM, Heymann HO, Sturdevant JR, editors. The Art and Science of Operative Dentistry. St Louis, Missouri: Mosby; 1995. pp. 60–128. [Google Scholar]
- 53.Mjor IA, Holst D, Eriksen HM. Caries and restoration prevention. JADA. 2008;139:565–570. doi: 10.14219/jada.archive.2008.0216. [DOI] [PubMed] [Google Scholar]
- 54.Bader JD, Shugars DA. Understanding dentists' restorative treatment decisions. J Public Health Dent. 1992;52:102–110. doi: 10.1111/j.1752-7325.1992.tb02251.x. [DOI] [PubMed] [Google Scholar]
- 55.Gilbert GH, Litaker MS, Makhija SK. Differences in quality between dental practices associated with race and income mix of patients. J Health Care Poor Underserved. 2007;18:847–867. doi: 10.1353/hpu.2007.0095. [DOI] [PubMed] [Google Scholar]
- 56.Dasanayake AP, Li Y, Chhun N, Bronstein JM, Childers NK. Challenges faced by minority children in obtaining dental care. J Health Care Poor Underserved. 2007;18:779–789. doi: 10.1353/hpu.2007.0093. [DOI] [PubMed] [Google Scholar]
- 57.Tilashalski KR, Gilbert GH, Boykin MJ, Litaker MS. Racial differences in treatment preferences: oral health as an example. J Eval Clin Pract. 2007;13:102–108. doi: 10.1111/j.1365-2753.2006.00661.x. [DOI] [PubMed] [Google Scholar]
- 58.Wendt LK. On oral health in infants and toddlers (thesis) Swed Dent J. 1995;106(suppl):62. [PubMed] [Google Scholar]
- 59.Hugoson A, Koch G, Gothberg C, Helkimo AN, Lundin SA, Norderyd O, Sjodin B, Sondell K. Oral health of individuals aged 3-80 years in Jonkoping, Sweden during 30 years (1973-2003). I & II. Review of findings on dental care habits and knowledge of oral health. Swed Dent J. 2005;29:125–138. 139–155. [PubMed] [Google Scholar]
- 60.Boren SA, Balas EA. Evidence-based quality measurement. J Ambul Care Manage. 1999;22:17–23. doi: 10.1097/00004479-199907000-00005. [DOI] [PubMed] [Google Scholar]


