Abstract
Despite progress in identifying homogeneous subphenotypes of obsessive compulsive disorder (OCD) through factor analysis of the Yale-Brown Obsessive Compulsive Scale Symptom Checklist (YBOCS-SC), prior solutions have been limited by a reliance on presupposed symptom categories rather than discrete symptoms. Furthermore, there have been only limited attempts to evaluate the familiality of OCD symptom dimensions. The purpose of this study was to extend prior work by this collaborative group in category-based dimensions by conducting the first-ever exploratory dichotomous factor analysis using individual OCD symptoms, comparing these results to a refined category-level solution, and testing the familiality of derived factors. Participants were 485 adults in the six-site OCD Collaborative Genetics Study, diagnosed with lifetime OCD using semi-structured interviews. YBOCS-SC data were factor analyzed at both the individual item and symptom category levels. Factor score intraclass correlations were calculated using a subsample of 145 independent affected sib pairs. The item- and category-level factor analyses yielded nearly identical 5-factor solutions. While significant sib-sib associations were found for 4 of the 5 factors, Hoarding and Taboo Thoughts were the most robustly familial (rICC ≥ 0.2). This report presents considerable converging evidence for a 5-factor structural model of OCD symptoms, including separate factor analyses employing individual symptoms and symptom categories, as well as sibling concordance. The results support investigation of this multidimensional model in OCD genetic linkage studies.
Keywords: obsessive compulsive disorder, symptoms, factors, familial, genetics
1. Introduction
Obsessive compulsive disorder (OCD) is a chronic illness associated with substantial distress and functional impairment. Twin studies suggest OCD is heritable, with concordance rates higher in monozygotic (80–87%) than dizygotic twins (47–50%) (Carey and Gottesman, 1981). Family studies find relatives of cases affected substantially more often than relatives of controls (Pauls et al., 1995; Nestadt et al., 2000). Obsessions and compulsions are remarkably diverse and are expressed with great variability across patients with OCD (Rasmussen and Eisen, 1988). Phenotypic heterogeneity significantly complicates research on OCD pathophysiology, etiology, and the search for vulnerability genes.
Factor analytic approaches have been used to derive useful phenotypic dimensions in other heterogeneous conditions, including schizophrenia (Liddle et al., 1992; Andreasen et al., 1995) and bipolar disorder (Cassidy et al., 1998). Similarly, in the last decade, at least ten factor analyses (total N<2,000) have delineated clinically meaningful OCD symptom dimensions (see Mataix-Cols et al., 2005). While fairly similar in content, the number of factors reported ranges from three to six.
A major weakness of existing factor analytically-derived OCD dimensions is that they depend on the a priori structure of the field’s primary symptom measure, the Yale Brown Obsessive Compulsive Scale Symptom Checklist (YBOCS-SC) (Goodman et al., 1989). This comprehensive list classifies obsessions and compulsions into 13 categories, based on the symptoms’ overt similarities. Most factorial studies to date, including a recent report from this collaborative group (Hasler et al., 2007), have used composite scores on these a priori categories rather than individual symptoms (Mataix-Cols et al., 2005). However, category-level factor analyses are biased since they assume the validity of these symptom groupings (Summerfeldt et al., 1999), restrict the number of items available for analysis, and limit the symptom dimensions that can emerge (Denys et al., 2004). It is not surprising that an item-level confirmatory factor analysis (Summerfeldt et al., 1999) failed to empirically support the YBOCS-SC categories. Moreover, the published 3-factor (Baer, 1994) and 4-factor (Leckman et al., 1997) models, both derived from these categories, were not confirmed at the item-level. While adequate fit was found for the 4-factor model at the second-order (or category) level, parameter estimates showed within-factor heterogeneity and overlap between factors (Summerfeldt et al., 1999). Despite these significant weaknesses, category-level factor analyses have been applied to the YBOCS-SC for practical reasons (e.g., fewer variables to manage; smaller samples required for power than item-level analyses).
A comprehensive model of OCD symptom structure requires exploratory factor analysis of individual YBOCS-SC items to identify symptom clusters empirically. Three such item-level analyses have been reported (Hantouche and Lancrenon, 1996; Feinstein et al., 2003; Denys et al., 2004). All were limited by low subjects-to-items ratios (4–9 subjects per item) and the use of principal components analysis. When used with dichotomous (present versus absent), non-normally distributed data, as are obtained with the YBOCS-SC, traditional factor analysis procedures, like principal components analysis, can be misleading since commonly endorsed items cluster separately from less commonly endorsed items, even when all measure the same latent variable, yielding factors that reflect similarity in item prevalence rather than strength of association (Nunnally and Bernstein, 1994). An appropriate statistical alternative is dichotomous factor analysis (DFA) (Christoffersen, 1975), which explicitly accounts for the dichotomous, non-normal distribution of these data. Only one study (Cullen et al., 2007) has applied DFA to YBOCS-SC data but that attempt was at the category-level.
Despite prior findings of OCD’s heritability, there have been few attempts to evaluate the familiality of OCD symptom dimensions. The first two such studies used the 4-factor model developed by Leckman et al. (1997). Alsobrook et al. (1999) reported that the recurrence risk of OCD among first-degree relatives of probands with high scores on either the obsessions/checking or symmetry/ordering factors was much higher than the recurrence risk among relatives of probands with low scores on these factors. In a segregation analysis, Leckman et al. (2003) yielded significant correlations between siblings and mother-child pairs for the same two factors in a sample of Tourette Syndrome affected sibpairs and relatives. Cullen et al. (2007) examined affected sibling similarity on four DFA-derived category-based factors in the Johns Hopkins OCD Family Study. Significant intrafamilial sib-sib correlations were found for the symmetry/ordering and hoarding factors despite limited power. Finally, in a category-based principal components analysis of affected sibling pairs from the OCD Collaborative Genetics Study (OCGS), Hasler et al. (2007) derived the same factor structure as in Leckman et al. (1997). All four factors showed statistically significant sib-sib correlations, with hoarding and obsessions/checking demonstrating the strongest familiality. Further and more consistent evidence of the familiality of symptom dimensions is needed to support the use of factor scores as quantitative traits in genetic linkage studies (Baer, 1994; Miguel et al., 2005).
The present study extends the work of Hasler et al. (2007) by re-analyzing YBOCS-SC data in the OCGS and applying the first-ever exploratory DFA of individual OCD symptoms. Results of this item-level analysis were compared to a refined category-level solution (see Data Analysis) from the same sample. We also examined affected sibling similarity on the derived symptom dimensions via intraclass sibling correlations as in Korszun et al. (2004). We expected the highest familial correlation for the hoarding factor based on clinical impressions, prior analyses by this group in the OCGS (Hasler et al., 2007), and findings from the Johns Hopkins OCD Family Study (Samuels et al., 2002; Cullen et al., 2007), a precursor to the OCGS.
2. Method
2.1. Subjects
Data were collected between 2001 and 2004 as part of the OCGS (Samuels et al., 2006). The OCGS is a federally-funded collaboration among six sites in the United States: Johns Hopkins University (JHU) School of Medicine [lead site], Butler Hospital/Brown University, Columbia University, Massachusetts General Hospital/Harvard Medical School, National Institute of Mental Health (NIMH), and University of California–Los Angeles. The study targeted families with OCD-affected sibling pairs, and extended these when possible through affected first- and second-degree relatives. Probands were included if their first onset of obsessions and/or compulsions occurred before the age of 18 years because of the greater familial risk in early-onset cases (Nestadt et al., 2000). Exclusion criteria for probands, intended to reduce the heterogeneity of the sample, included lifetime schizophrenia, severe mental retardation, Tourette Syndrome, or OCD which occurred exclusively in the context of depression (“secondary OCD”).
While the overall OCGS sample included both children and adults with lifetime DSM-IV OCD (n = 624), the current sample is restricted to the 485 adult participants (age > 18 years) with lifetime OCD because it is not clear, at present, whether the symptom structure of child/adolescent OCD is comparable to adult OCD. Two recent category-based principal components analyses (McKay et al., 2006; Stewart et al., 2007) and an item-based cluster analysis (Ivarsson and Valderhaug, 2006), suggest some differences in the content of OCD symptom factors in affected children/adolescents as compared to adults. While McKay et al. (2006) was likely underpowered (n = 137), Stewart et al. (2007) (n = 231) still derived somewhat different factors than previous adult category-level analyses, including a factor in which contamination/cleaning loaded with the aggressive and somatic categories. Despite similarities to adult cluster analyses of OCD symptoms (Calamari et al., 1999, 2004), Ivarsson and Valderhaug (2006) (n = 213) noted important differences in their child/adolescent cluster analysis such as the absence of subgroups for hoarding and symmetry/ordering. The authors speculated that these discrepancies might be due to developmental differences in OCD phenomenology and clinical course in children/adolescents as compared with adults (Jaisoorya et al., 2003; Stewart et al., 2004).
The 485 participants comprised 218 multiply affected OCD families; no sporadic (i.e., nonfamilial) cases were included. The sample (69.7% female; 97.1% Caucasian) was recruited from psychiatric treatment settings, referrals from clinicians in the community, web sites, advertisements, self-help groups, and the Obsessive Compulsive Foundation (OCF). Mean age for this sample at assessment was 41.8 years (range = 19–95; SD = 14.5) and mean age at OCD onset was 14.0 years (range = 3–58; SD=9.2). The protocol was approved by the institutional review board at each site. After complete description of the study to the subjects, written informed consent was obtained. For more information on OCGS procedures and site-specific recruitment strategies, see Samuels et al (2006).
2.2. Clinical Assessment
Experienced doctoral-level interviewers conducted diagnostic assessments and participated in regular case conferences under the supervising clinician at each site. OCD was diagnosed using an adaptation of the Schedule for Affective Disorders and Schizophrenia – Lifetime Version Modified for Anxiety Disorders (SADS-LA-R) (Mannuzza et al., 1986). Interviewers administered the YBOCS-SC to enumerate participants’ lifetime obsessive-compulsive symptoms. Additional clinical information was obtained from informant interviews, using the Family Informant Schedule and Criteria (Mannuzza et al., 1985), and review of previous psychiatric treatment records, if available. Interviewers created a narrative formulation for each case and completed the JHU Diagnostic Assignment Checklist to indicate the presence/absence of specific diagnostic criteria. The diagnostic checklist presents logical algorithms with specified rules, allowing assignment of definite, probable, absent, or unknown for each disorder. (Only definite OCD-affected adults and sib pairs were included in the current sample.) Two expert diagnosticians reviewed cases independently at each site, followed by review of diagnostic assignment at JHU. The inter-rater reliability (kappa) values for OCD and its clinical symptoms were: 0.81 for OCD, 0.81 for obsessions, and 0.88 for compulsions (Samuels et al., 2006).
2.3. Data Analysis
For the item-level analysis, an exploratory DFA was conducted using Mplus Version 3 (Muthén and Muthén, 1998–2004). To maximize the subjects-to-items ratio, the 10 open-ended (i.e., ‘other’) items and 20 miscellaneous items were excluded, leaving a total of 44 specified YBOCS-SC items. Symptoms present at the time of interview and/or in the past (i.e., lifetime symptoms) were coded 1; those never present as 0. The inputs for the DFA are tetrachoric inter-item correlations (rather than Pearson correlations), which assume normally distributed latent response variables. Criteria for retention of factors were Cattell’s scree test, pattern of factor loadings, and factor interpretability. Kaiser’s criterion (eigenvalues greater than 1) was not used because of the large number of variables involved. Mplus also provides estimates of the Root Mean Square Error of Approximation (RMSEA) fit index (Steiger and Lind, 1980), which has been recommended as a reliable criterion for determining the number of factors to include in a model (Fabrigar et al., 1999). RMSEA values less than 0.05 constitute good fit (Browne and Cudeck, 1992). A factor rotation that required the resultant solutions to be orthogonal (varimax) was selected. An oblique (promax) rotation yielded the same solution. Loadings ≥ 0.45 were considered statistically significant.
As a comparison to the item-level solution, an exploratory factor analysis of the YBOCS-SC categories was conducted using the SPSS statistical package, version 11.0 (SPSS, Inc., Chicago). The a priori categories were adjusted according to a method tested by Pinto et al. (in press). Specifically, two of the aggressive obsession items, “fear will harm others because not careful enough” and “fear will be responsible for something terrible happening,” were treated as a separate category (overresponsibility for harm), because these symptoms appear phenomenologically distinct from items targeting fear of aggressive impulses (e.g., “I have violent or horrific images in my mind”) and, in fact, did not correlate with the other aggressive obsessions in two prior item-level factor analyses (Summerfeldt et al., 1997; Denys et al., 2004). When these adjusted categories were subjected to principal components analysis in Pinto et al. (in press), the resulting factor structure corresponded to that of prior item-level analyses. To maximize comparability to prior category-level factorial studies (e.g., Leckman et al., 1997; Mataix-Cols et al., 1999; Pinto et al., in press), the two “miscellaneous” categories were excluded from the present category-level analysis. Scores were computed for each of 14 categories as the number of symptoms endorsed divided by the number of symptoms in that category, as in Pinto et al. (in press). We used an interval scoring system for the categories, rather than a dichotomous (present/absent) (Cullen et al., 2007) or a three-point ordinal rating (Mataix-Cols et al., 1999), to increase the range of category scores and to maximize the variance in our dataset. Proportions, unlike the symptom counts used in Leckman et al. (1997), do not give undue weight to categories composed of numerous items. Criteria for retention of factors were Kaiser’s criterion, Cattell’s scree test, pattern of factor loadings, and factor interpretability. For consistency with all prior category-level analyses, the initial factors were extracted using the principal components method, followed by varimax rotation. Promax rotation yielded the same solution. Loadings ≥ 0.45 were considered statistically significant. Category-level factor scores were standardized, with mean 0 and standard deviation 1.
To identify the significance of the familial effect, SPSS 11.0 was used to calculate intraclass correlations (rICC) between the category-level factor scores of affected adult siblings (both individuals in each pair were adults and met criteria for definite lifetime DSM-IV OCD), with one sib pair chosen randomly from each OCGS family with siblings who met the age and definite status criteria (n = 145 independent sib pairs). An rICC provides a ratio of between versus within sib pair variance (Haggard, 1958), with a statistically significant rICC indicating sibling resemblance (Rovine, 1994). Significance level was set at P < 0.05.
3. Results
3.1. Dichotomous Factor Analysis of YBOCS-SC Items
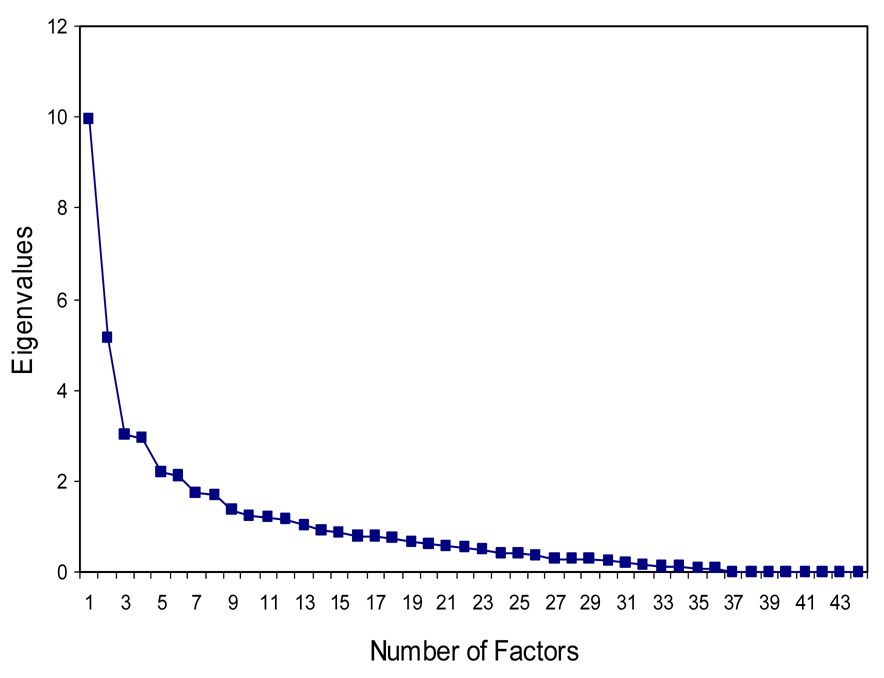
Table 1 displays frequencies of the 44 individual YBOCS-SC items (lifetime). The most frequently endorsed items were concern with dirt or germs, checking locks or appliances, ordering/arranging compulsions, and rereading or rewriting. Inspection of the scree plot (see Figure 1) generated by DFA indicates an elbow in the curve toward less steep decline after the first 5 factors. Based on the scree plot, the 4–7 factor solutions were compared for optimal interpretability, pattern of loadings, and model fit. While the RMSEA for the 4-factor model (0.052) did not reach the usual threshold for good fit, the overall fit for the other models was quite good (5-factor: 0.042; 6-factor: 0.033; 7-factor: 0.024). OCD phenotypic experts within the OCGS concluded that the 5-factor model, accounting for 52.5% of the variance, was clinically the most compelling (see Table 1) since it comprises the most phenomenologically homogeneous symptom clusters. The symptom factors include: (1) Taboo Thoughts; (2) Symmetry/Ordering; (3) Hoarding; (4) Contamination/Cleaning; (5) Doubt/Checking. For the most part, individual symptoms loaded highly on only one of the factors. Items pertaining to somatic obsessions, somatic checking, symmetry or exactness obsessions with magical thinking, repeating routine activities, rereading/rewriting, counting compulsions, checking that one did not make a mistake, and a fear of stealing did not load on any of the factors. There was also cross-loading of household cleaning between the Contamination/Cleaning and Symmetry/Ordering factors.
Table 1.
Frequency of Individual YBOCS-SC Items and Varimax Rotated Factor Structure Using Dichotomous Factor Analysis (n = 485)
| YBOCS-SC Items | Frequency | Factor Loading | ||||
|---|---|---|---|---|---|---|
| % | Taboo Thoughts | Symmetry/ Ordering | Hoarding | Contam/Cleaning | Doubt/Checking | |
| Forbidden sexual thoughts, images or impulses | 20.5 | 0.832 | 0.047 | 0.024 | 0.092 | −0.058 |
| Obsessions re: homosexuality | 9.9 | 0.813 | 0.123 | 0.005 | 0.053 | −0.064 |
| Obsessions re: incest | 8.2 | 0.782 | 0.055 | 0.042 | 0.144 | −0.056 |
| Obsessions re: aggressive sexual behavior | 6.7 | 0.716 | 0.019 | 0.134 | 0.035 | −0.015 |
| Fear will act on unwanted impulse | 18.7 | 0.655 | 0.079 | 0.064 | −0.131 | 0.269 |
| Fear might harm self | 18.2 | 0.646 | 0.151 | 0.083 | 0.027 | 0.229 |
| Fear might harm others | 30.6 | 0.577 | 0.120 | 0.126 | −0.064 | 0.412 |
| Violent or horrific images | 26.4 | 0.562 | 0.162 | 0.013 | 0.065 | 0.186 |
| Fear of blurting out obscenities | 10.7 | 0.552 | 0.120 | 0.147 | −0.027 | 0.303 |
| Fear doing something embarrassing | 10.5 | 0.518 | 0.118 | 0.092 | 0.033 | 0.169 |
| Concerned with sacrilege | 18.4 | 0.467 | 0.010 | 0.065 | 0.197 | 0.219 |
| Excess concern with morality | 17.0 | 0.452 | 0.055 | 0.060 | 0.255 | 0.216 |
| Ordering/arranging compulsions | 50.1 | 0.024 | 1.000 | 0.141 | 0.053 | −0.025 |
| Symmetry or exactness without magical thinking | 31.9 | 0.025 | 0.590 | 0.044 | 0.059 | −0.145 |
| Hoarding/collecting compulsions | 36.4 | −0.058 | 0.129 | −0.980 | −0.031 | −0.030 |
| Hoarding/saving obsessions | 34.1 | 0.080 | 0.142 | −0.907 | 0.038 | −0.024 |
| Concern with dirt or germs | 43.4 | 0.033 | 0.105 | 0.001 | 0.881 | 0.088 |
| Handwashing rituals | 37.7 | 0.053 | 0.070 | 0.096 | 0.865 | 0.166 |
| Excessive concerns with animals | 13.4 | 0.051 | 0.083 | 0.097 | 0.680 | 0.122 |
| Excessive concerns with environmental contaminants | 13.2 | 0.089 | 0.161 | 0.222 | 0.667 | 0.239 |
| Concerns or disgust with bodily waste or secretions | 21.6 | 0.219 | 0.168 | 0.057 | 0.658 | 0.129 |
| Concerned will get ill because of contaminant | 21.2 | 0.116 | 0.136 | 0.140 | 0.650 | 0.224 |
| Bothered by sticky substances | 14.7 | 0.012 | 0.139 | 0.035 | 0.645 | 0.047 |
| Measures to prevent or remove contact with contaminants | 19.5 | 0.014 | 0.088 | 0.008 | 0.640 | 0.087 |
| Concern with household cleaners | 12.2 | 0.213 | 0.134 | 0.104 | 0.600 | 0.301 |
| No concern with consequence of contamination other than how it might feel | 10.9 | 0.065 | 0.330 | 0.074 | 0.577 | 0.137 |
| Concerned will get others ill by spreading contaminant | 15.5 | 0.138 | 0.174 | 0.011 | 0.555 | 0.429 |
| Showering or grooming rituals | 26.0 | 0.027 | 0.270 | 0.058 | 0.532 | 0.138 |
| Household cleaning | 27.7 | 0.156 | 0.450 | 0.121 | 0.503 | 0.065 |
| Checking that did not harm others | 16.8 | 0.162 | 0.119 | 0.055 | 0.187 | 0.823 |
| Fear will harm others because not careful enough | 26.8 | 0.376 | 0.112 | 0.059 | 0.054 | 0.758 |
| Checking locks or appliances | 56.4 | −0.007 | 0.241 | 0.009 | 0.047 | 0.703 |
| Checking did not harm self | 2.1 | 0.387 | 0.035 | 0.072 | 0.084 | 0.697 |
| Fear will be responsible for something terrible happening | 30.8 | 0.082 | 0.007 | 0.030 | 0.138 | 0.643 |
| Checking that nothing terrible happened | 16.6 | 0.148 | 0.182 | 0.007 | 0.081 | 0.615 |
| Checking that did not make mistake | 38.6 | 0.141 | 0.322 | 0.144 | 0.275 | 0.432 |
| Checking tied to somatic obsessions | 16.8 | 0.391 | 0.099 | 0.274 | 0.177 | 0.256 |
| Excessive concern with body part or aspect of appearance | 15.5 | 0.368 | 0.075 | 0.232 | 0.112 | 0.100 |
| Concern with illness or disease | 28.7 | 0.323 | 0.078 | 0.201 | 0.305 | 0.284 |
| Rereading or rewriting | 44.9 | 0.074 | 0.403 | 0.133 | 0.073 | 0.270 |
| Counting compulsions | 33.5 | 0.127 | 0.373 | 0.084 | 0.135 | 0.256 |
| Symmetry or exactness with magical thinking | 20.8 | 0.059 | 0.355 | 0.055 | 0.072 | 0.278 |
| Need to repeat routine activities | 17.4 | 0.116 | 0.263 | 0.022 | 0.212 | 0.325 |
| Fear will steal things | 4.2 | 0.187 | 0.109 | 0.203 | 0.133 | 0.244 |
| Percentage of variance explained | -- | 22.4 | 11.6 | 6.9 | 6.6 | 4.9 |
Robust loadings (≥ 0.45) are printed in bold underline. Taboo Thoughts: Aggressive, sexual, and religious obsessions; Symmetry/Ordering: Obsessions of symmetry, and ordering/arranging compulsions; Hoarding: Hoarding obsessions and compulsions; Contamination/Cleaning: Contamination obsessions and cleaning compulsions; Doubt/Checking: Overresponsibility for harm obsessions and checking compulsions. YBOCS-SC = Yale-Brown Obsessive Compulsive Scale Symptom Checklist.
Figure 1.
Scree Plot of Dichotomous Factor Analysis of 44 YBOCS-SC Items (n = 485)
3.2. Principal Components Factor Analysis of YBOCS-SC Categories
Table 2 presents frequencies of the 14 lifetime YBOCS-SC categories; contamination obsessions, aggressive obsessions, checking compulsions, and cleaning compulsions were the most frequently endorsed. The principal components factor analysis with varimax rotation resulted in a 5-factor solution (see Table 2), accounting for 64.1% of the total variance: (1) Symmetry/Ordering; (2) Taboo Thoughts; (3) Hoarding; (4) Doubt/Checking; (5) Contamination/Cleaning. All symptom categories, except somatic obsessions, loaded highly on their respective factors.
Table 2.
Frequency of OCD Symptoms by YBOCS-SC Category and Varimax Rotated Factor Structure Using Principal Components Factor Analysis (n = 485)
| Frequency | Factor Loading | |||||
|---|---|---|---|---|---|---|
| YBOCS-SC Categories | ||||||
| % | Symmetry/ Ordering | Taboo Thoughts | Hoarding | Doubt/ Checking | Contam/ Cleaning | |
| Ordering and arranging | 50.0 | 0.839 | −0.048 | 0.094 | −0.074 | 0.033 |
| Obsessions of symmetry | 50.4 | 0.823 | −0.073 | 0.022 | 0.070 | 0.020 |
| Repeating rituals | 51.5 | 0.502 | 0.188 | 0.023 | 0.090 | 0.147 |
| Counting compulsions | 33.5 | 0.476 | 0.143 | 0.072 | 0.148 | 0.088 |
| Sexual obsessions | 25.9 | −0.035 | 0.808 | 0.040 | 0.021 | −0.016 |
| Religious obsessions | 30.8 | 0.094 | 0.737 | −0.061 | 0.043 | 0.146 |
| Aggressive obsessions | 57.9 | 0.114 | 0.588 | −0.003 | 0.438 | −0.069 |
| Hoarding obsessions | 34.1 | 0.087 | 0.043 | 0.923 | 0.049 | 0.030 |
| Hoarding compulsions | 36.4 | 0.097 | −0.041 | 0.921 | −0.004 | −0.011 |
| Overresponsibility for harm | 42.5 | −0.050 | 0.088 | 0.051 | 0.859 | 0.075 |
| Checking compulsions | 72.8 | 0.261 | 0.114 | −0.019 | 0.781 | 0.181 |
| Contamination obsessions | 59.4 | 0.042 | 0.174 | 0.034 | 0.164 | 0.877 |
| Cleaning compulsions | 59.2 | 0.194 | −0.030 | −0.022 | 0.055 | 0.873 |
| Somatic obsessions | 40.0 | 0.168 | 0.380 | 0.064 | 0.286 | 0.258 |
| Percentage of variance explained | -- | 22.5 | 13.7 | 11.1 | 9.2 | 7.6 |
Robust loadings (≥ 0.45) are printed in bold underline. Symmetry/Ordering: Obsessions of symmetry, and repeating, counting and ordering/arranging compulsions; Taboo Thoughts: Aggressive, sexual, and religious obsessions; Hoarding: Hoarding obsessions and compulsions; Doubt/Checking: Overresponsibility for harm obsessions and checking compulsions; Contamination/Cleaning: Contamination obsessions and cleaning compulsions. YBOCS-SC = Yale-Brown Obsessive Compulsive Scale Symptom Checklist.
3.3. Familiality of OCD Symptom Dimensions
Table 3 shows the sib-sib correlation for each factor score. While significant sib-sib associations were found for 4 of the 5 factors, Hoarding (rICC = 0.236) was most familial, followed by Taboo Thoughts (rICC = 0.218). Symmetry/Ordering (rICC = 0.098) showed a relatively weak (nonsignificant) association between affected siblings.
Table 3.
Intraclass Correlations of YBOCS-SC Category-Level Factor Scores Between Affected Siblings (n = 145 independent sib pairs)
| Factor | rICC | P |
|---|---|---|
| Symmetry/Ordering | 0.098 | 0.120 |
| Taboo Thoughts | 0.218 | 0.004* |
| Hoarding | 0.236 | 0.002* |
| Doubt/Checking | 0.165 | 0.023* |
| Contamination/Cleaning | 0.169 | 0.020* |
P < 0.05.
Symmerty/Ordering: Obsessions of symmetry, and repeating, counting and ordering/arranging compulsions; Taboo Thoughts: Aggressive, sexual, and religious obsessions; Hoarding: Hoarding obsessions and compulsions; Doubt/Checking: Overresponsibility for harm obsessions and checking compulsions; Contamination/Cleaning: Contamination obsessions and cleaning compulsions. YBOCS-SC = Yale-Brown Obsessive Compulsive Scale Symptom Checklist.
4. Discussion
The aim of the present study was to empirically derive a multidimensional model of OCD symptom structure using individual YBOCS-SC items, extending previous work by this collaborative group using YBOCS-SC a priori categories (Hasler et al., 2007). The new item-based model was then compared to a factor solution based on a traditional principal components analysis of YBOCS-SC categories, adjusted according to a method developed by Pinto et al. (in press). Data were collected from a large (n = 485), well-defined sample of adults with lifetime OCD, from 218 multiply affected OCD families, recruited as part of the OCGS. To our knowledge, this is the first exploratory DFA of individual OCD symptoms, sensitive to the dichotomous, non-normal nature of these data.
The results provide compelling evidence for a multidimensional model of OCD. The item-and category-level analyses yielded nearly identical 5-factor solutions, consisting of Symmetry/Ordering, Taboo Thoughts, Hoarding, Doubt/Checking, and Contamination/Cleaning. These homogeneous symptom clusters correspond to widely accepted and long held themes of OCD. There were few differences between the two solutions. While counting and repeating compulsions loaded on Symmetry/Ordering in the category-level analysis, items pertaining to counting and repeating routine activities did not load on any of the factors in the item-level analysis. The item that deals with symmetry obsessions with magical thinking also did not load on any factor in the item-level analysis, unlike its counterpart without magical thinking (which loaded on Symmetry/Ordering). In the item-level analysis, the household cleaning item loaded on both Contamination/Cleaning and Symmetry/Ordering, likely due to the clinical impression that this item is endorsed both by patients with contamination/harm avoidant concerns and those with “incompleteness.” Meanwhile, in the category-level analysis, the cleaning compulsions category loaded strongly on Contamination/Cleaning.
Our item-level analysis yielded a five-factor solution, as compared to the four factors derived in our previous category-level analysis in the OCGS sample (Hasler et al., 2007). The key difference in the solutions is the separation at the item level of “taboo” (aggressive, sexual, religious) obsessions from “overresponsibility for harm” obsessions, which have traditionally been lumped in the a priori aggressive obsessions category in category-level analyses. Over the years, the placement of aggressive, sexual, and religious obsessions in category-level factorial studies has been quite variable, likely due to the heterogeneity of the a priori aggressive obsessions category, which contains both items targeting fear of aggressive impulses and overresponsibility for harm. Two category-level analyses (Baer, 1994; Hantouche and Lancrenon, 1996) reported a “pure obsessions” factor that is consistent with Taboo Thoughts. However, in both Leckman et al. (1997) and Hasler et al. (2007), aggressive, sexual, and religious obsessions load with somatic obsessions and checking compulsions. Cullen et al. (2007) reported an obsessions factor that consists of aggressive, sexual, religious, and somatic obsessions. Mataix-Cols et al. (1999) reported separate aggressive/checking and sexual/religious dimensions in their 5-factor solution. When symptoms are factor analyzed at the item-level, as in the present study and two others (Summerfeldt et al., 1997; Denys et al., 2004), the fear of aggressive impulse items load with the other “taboo” obsessions (Taboo Thoughts) while the overresponsiblity for harm items load with checking compulsions (Doubt/Checking). Taboo Thoughts and Doubt/Checking are phenomenologically more homogeneous than the corresponding combined aggressive/sexual/religious/somatic/checking factor derived in Hasler et al. (2007) and previously in Leckman et al. (1997).
The present category-level analysis (adjusted to include a category for overresponsibility for harm obsessions) yielded a solution that matches almost exactly the category-level factors retained by Pinto et al. (in press), using the same statistical methods, in a separate nonfamilial sample of 293 individuals with OCD from the Brown Longitudinal Obsessive Compulsive Study (Pinto et al., 2006). The only differences between the solutions are the order of the factors in each solution and the lack of a robust loading for the somatic obsessions category in the current study. Replicating the results of previous factor analyses is important in demonstrating the generalizability of dimensions across samples (Gorsuch, 1983). This replication suggests that the same underlying structure of OCD symptoms holds in both familial and nonfamilial affected samples, despite differences in study recruitment. In Pinto et al. (in press), the nonfamilial sample was collected at a single site and inclusion criteria included a “primary” diagnosis of DSM-IV OCD (defined as the disorder participants considered their biggest lifetime psychiatric problem) with participants having sought treatment for OCD. In contrast, the current familial sample was collected at six sites. Affected participants all had lifetime DSM-IV OCD but the disorder was not necessarily “primary,” and they may or may not have sought treatment. While early symptom onset was a requirement for probands in the current sample, this was not the case in Pinto et al. (in press). Furthermore, YBOCS-SC data consisted of lifetime symptoms in the present study and current symptoms in Pinto et al. (in press).
Like replication, familiality also affirms the validity (Robins and Guze, 1970) of the distinctive components that make up the complex clinical presentation of OCD and supports their use in genetic studies. Access to a family sample afforded the opportunity to test the familiality of our symptom dimensions in 145 independent affected sib pairs. Significant sib-sib associations for 4 of the 5 factors provided evidence for a considerable familial effect. Hoarding (hoarding obsessions and compulsions) and Taboo Thoughts (aggressive, sexual, and religious obsessions) were the most robustly familial. These findings suggest that our factor solution describes familial components of the disorder but does not allow us to draw any conclusions about whether the source of this familiality is genetic or environmental.
Hoarding has emerged as an independent factor in most previous factorial studies (Mataix- Cols et al., 2005). The familiality of hoarding has been previously demonstrated using data from the OCGS and the Johns Hopkins OCD Family Study, which predated the OCGS. Samuels et al. (2002) reported that the first-degree relatives of hoarding probands had a greater prevalence of hoarding behavior than the relatives of non-hoarding probands, and both Hasler et al. (2007) and Cullen et al. (2007) noted a significant intrafamilial sib-sib correlation for the hoarding factor. When used as a predictor in treatment studies, the hoarding factor also stands out as being associated with poorer response to selective serotonin reuptake inhibitors (SSRIs) (Black et al., 1998; Mataix-Cols et al., 1999; Saxena et al., 2002) and greater likelihood of drop out from cognitive behavior therapy (Mataix-Cols et al., 2002), although a recent study found that hoarding and non-hoarding OCD patients responded equally well to paroxetine (Saxena et al., 2005). Neuroimaging results indicate that the severity of hoarding is negatively correlated with glucose metabolism in the dorsal anterior cingulate cortex (Saxena et al., 2004). In addition, hoarding is the only subphenotype for which genetic linkage results have been reported. Zhang et al. (2002) noted significant allele sharing for the hoarding factor for loci at 4q34, 5q35.2, and 17q25.
The significant sib-sib association for the Taboo Thoughts factor is consistent with the findings of two prior segregation analyses (Alsobrook et al., 1999; Leckman et al., 2003), though those studies used the Leckman et al. (1997) factor which also includes somatic obsessions and checking compulsions. As compared to the rICC for Taboo Thoughts in the present study, Hasler et al. (2007) reported a lower, yet still statistically significant, sib-sib correlation for their more heterogeneous obsessions/checking factor (same as the Leckman et al. (1997) factor). Cullen et al. (2007) reported a sib-sib association of 0.215 for their obsessions factor (which also included somatic obsessions), comparable to the rICC for Taboo Thoughts in the present study, but the correlation was not statistically significant due to limited power (analyses based on only 35 independently affected sib pairs). Further support for this subphenotype comes from studies of treatment response. According to Alonso et al. (2001), high scores on a sexual/religious dimension were associated with poorer long-term outcome with SSRIs and behavior therapy. Similarly, Mataix-Cols et al. (2002) reported that high scores on this dimension were associated with poorer behavior therapy response.
The low sib-sib association for Symmetry/Ordering, the only factor with a nonsignificant rICC, contrasts the substantial familiality of this factor in two prior segregation analyses (Alsobrook et al., 1999; Leckman et al., 2003). However, unlike these other studies, the OCGS excluded probands with Tourette Syndrome. Leckman et al. (2003), on the other hand, focused on affected sibling pairs with Tourette Syndrome and included children/adolescents. Therefore the relatively weak association for Symmetry/Ordering in the present study, and in Hasler et al. (2007) (also based on the OCGS sample), is likely due to our exclusion criteria since symmetry/ordering symptoms are a prominent feature of the familiality of Tourette Syndrome (Leckman et al., 2003). The low sib-sib association for Symmetry/Ordering in the present study also contradicts the significant rICC found for this factor in Cullen et al. (2007). Since the authors of that study included two symptoms from the miscellaneous compulsions category – sensory compulsions (touch, tap, rub) and motor compulsions (rituals involving blinking or staring) – in their symmetry factor, the higher sib-sib association for this dimension may have been due to the familiality associated with the added tic-like sensorimotor behaviors.
The present study overcomes many of the limitations of prior factorial studies with its large cohort of extensively characterized OCD patients, novel statistical methods, use of individual YBOCS-SC items, and the collaborative involvement of expert investigators. However, the study also has several limitations of its own. Factor analyses were conducted on a sample of 485 adults recruited as part of a family study of OCD that targeted affected sibling pairs and their first- and second-degree relatives. While the potential limitations of deriving factors from affected relatives were considered, the factor analyses were not corrected for nonindependence because when dealing with correlated data (e.g., family data, longitudinal data, etc.) that are large in number of clusters (or families) and small in cluster sizes, it is generally the case that ignoring the dependence will yield valid estimates of parameters (in this case, factor loadings) but incorrect standard error estimates. Since the standard error estimates were not of particular interest given the aims of this project, the consequences of not correcting for nonindependence in this case are expected to be minimal. The a priori exclusion of open-ended and miscellaneous YBOCS-SC items in the factor analysis may have led to a biased representation of OCD symptoms. The proposed latent symptom groupings are limited to the manifest items available on the YBOCS-SC, though the checklist is the most comprehensive measure of OC symptoms to date and remains the standard in the field. New instruments, like the new edition of the YBOCS (YBOCS-II) and the Dimensional YBOCS (DY-BOCS) (Rosario-Campos et al., 2006), will allow collection of symptom data in a dimensional manner, better facilitating the development of quantitative traits for genetic analyses. Though higher than previous item-level analyses, our subjects-to-items ratio limited power for the DFA. Despite the wide use of principal components analysis (applied here in the category-level analysis), this approach is sensitive to scaling and lacks a probability model. The variable decision rules for retaining factors and scoring the YBOCS-SC categories have led to discrepancies in the number of factors reported across prior studies. In addition, our sample was recruited from a variety of sources, including treatment settings and support groups, and was predominantly female (69.7%) and almost entirely Caucasian (97.1%). Therefore, the results may not generalize to community samples or more diverse groups. Finally, the retrospective assessment approach used, with an emphasis on lifetime OCD symptoms, is vulnerable to memory bias and may be confounded by age at OCD onset. However, the retrospective nature of data collection may not have been a problem considering that our findings replicated a factor structure (Pinto et al., in press), collected from a separate sample, that was based on current symptoms.
As this is the first item-level DFA for OCD symptoms, replication is required in a larger sample utilizing all YBOCS-SC items, including miscellaneous symptoms and open-ended items. Replication of affected sib pair associations for the 5-factor model is also strongly recommended. Further research on the temporal stability of these factors, currently under way, would be another important indicator of the validity of these symptom dimensions. Our sample was restricted to affected adults in the OCGS; upcoming studies should extend these findings to child/adolescent samples as well as individuals with subclinical symptoms.
In summary, based on the consistency between the item- and category-level analyses, as well as the significant familiality demonstrated for 4 of the symptom dimensions, our results represent a logical phenotypic starting point for future genetic studies of OCD. In fact, linkage analyses incorporating these dimensions are forthcoming from collaborators within the OCGS. The use of homogeneous, replicable, and familial subphenotypes will considerably increase the power of such genetic analyses.
Acknowledgments
This research was supported by NIMH grants R01 MH50214, K23 MH064543, and K23 MH066284. The authors are grateful to Karen Bandeen-Roche, Ph.D. and Paul T. Costa, Jr., Ph.D. for their input on factor analytic methods. The authors also thank the many families participating in the study; the Obsessive Compulsive Foundation; and clinicians and coordinators at each site: Butler Hospital/Brown University (Maria Mancebo, PhD, Richard Marsland, RN, Shirley Yen, PhD); Columbia University (Renee Goodwin, PhD, Joshua Lipsitz, PhD, Jessica Page, PsyD); Johns Hopkins University School of Medicine (Laura Eisen, BS; Karan Lamb, PsyD, Tracey Lichner, PhD, Yung-mei Leong, PhD; Krista Vermillion, BA); Massachusetts General Hospital/Harvard Medical School (Daniel Geller, MD, Anne Chosak, PhD, Michelle Wedig, BS, Evelyn Stewart, MD, Michael Jenike, MD, Beth Gershuny, PhD, Sabine Wilhelm, PhD); NIMH (Lucy Justement, Diane Kazuba, V. Holland LaSalle-Ricci, Theresa B. DeGuzman); University of California-Los Angeles (R. Lindsey Bergman, PhD, Susanna Chang, PhD, Audra Langley, PhD, Amanda Pearlman, BA).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Alonso P, Menchon JM, Pifarre J, Mataix-Cols D, Torres L, Salgado P, Vallejo J. Long-term follow-up and predictors of clinical outcome in obsessive-compulsive patients treated with serotonin reuptake inhibitors and behavioral therapy. Journal of Clinical Psychiatry. 2001;62:535–540. doi: 10.4088/jcp.v62n07a06. [DOI] [PubMed] [Google Scholar]
- Alsobrook JP, Leckman JF, Goodman WK, Rasmussen SA, Pauls DL. Segregation analysis of obsessive-compulsive disorder using symptom-based factor scores. American Journal of Medical Genetics. 1999;88:669–675. doi: 10.1002/(sici)1096-8628(19991215)88:6<669::aid-ajmg17>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Arndt S, Alliger R, Miller D, Flaum M. Symptoms of schizophrenia. Methods, meanings, and mechanisms. Archives of General Psychiatry. 1995;52:341–351. doi: 10.1001/archpsyc.1995.03950170015003. [DOI] [PubMed] [Google Scholar]
- Baer L. Factor analysis of symptom subtypes of obsessive compulsive disorder and their relation to personality and tic disorders. Journal of Clinical Psychiatry. 1994;55 Suppl:18–23. [PubMed] [Google Scholar]
- Black DW, Monahan P, Gable J, Blum N, Clancy G, Baker P. Hoarding and treatment response in 38 nondepressed subjects with obsessive-compulsive disorder. Journal of Clinical Psychiatry. 1998;59:420–425. doi: 10.4088/jcp.v59n0804. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods and Research. 1992;21:230–258. [Google Scholar]
- Calamari JE, Wiegartz PS, Janeck AS. Obsessive-compulsive disorder subgroups: A symptom-based clustering approach. Behaviour Research and Therapy. 1999;37:113–125. doi: 10.1016/s0005-7967(98)00135-1. [DOI] [PubMed] [Google Scholar]
- Calamari JE, Wiegartz PS, Riemann BC, Cohen RJ, Greer A, Jacobi DM, Jahn SC, Carmin C. Obsessive-compulsive disorder subtypes: An attempted replication and extension of a symptom-based taxonomy. Behaviour Research and Therapy. 2004;42:647–670. doi: 10.1016/S0005-7967(03)00173-6. [DOI] [PubMed] [Google Scholar]
- Carey G, Gottesman I. Twin and family studies of anxiety, phobic, and obsessive disorders. In: Klein DF, Rabkin JG, editors. Anxiety: New Research and Changing Concepts. New York: Raven Press; 1981. pp. 117–136. [Google Scholar]
- Cassidy F, Forest K, Murry E, Carroll BJ. A factor analysis of the signs and symptoms of mania. Archives of General Psychiatry. 1998;55:27–32. doi: 10.1001/archpsyc.55.1.27. [DOI] [PubMed] [Google Scholar]
- Christoffersen A. Factor analysis of dichotomous variables. Psychometrika. 1975;40:5–32. [Google Scholar]
- Cullen B, Brown CH, Riddle MA, Grados M, Bienvenu OJ, Hoehn-Saric R, Shugart YY, Liang K, Samuels J, Nestadt G. Factor analysis of the Yale-Brown Obsessive Compulsive Scale in a family study of obsessive-compulsive disorder. Depression and Anxiety. 2007;24:130–138. doi: 10.1002/da.20204. [DOI] [PubMed] [Google Scholar]
- Denys D, de Geus F, van Megen HJ, Westenberg HG. Use of factor analysis to detect potential phenotypes in obsessive-compulsive disorder. Psychiatry Research. 2004;128:273–280. doi: 10.1016/j.psychres.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Fabrigar LR, Wegener DT, MacCallum RC, Strahan EJ. Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods. 1999;4:272–299. [Google Scholar]
- Feinstein SB, Fallon BA, Petkova E, Liebowitz MR. Item-by-item factor analysis of the Yale-Brown Obsessive Compulsive Scale Symptom Checklist. Journal of Neuropsychiatry and Clinical Neurosciences. 2003;15:187–193. doi: 10.1176/jnp.15.2.187. [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischman RL, Hill CL, Heninger GR, Charney DS. The Yale-Brown Obsessive Compulsive Scale: I. Deveopment, use, and reliability. Archives of General Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Gorsuch RL. Factor Analysis. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum; 1983. [Google Scholar]
- Haggard EA. Intraclass Correlation and the Analysis of Variance. New York: Dryden Press; 1958. [Google Scholar]
- Hantouche EG, Lancrenon S. Modern typology of symptoms and obsessive-compulsive syndromes: Results of a large French study of 615 patients. Encephale 22 Spec No. 1996;1:9–21. [PubMed] [Google Scholar]
- Hasler G, Pinto A, Greenberg BD, Samuels JF, Fyer AJ, Pauls DL, Knowles JA, McCracken JT, Piacentini J, Riddle MA, Rauch SL, Rasmussen SA, Willour VL, Grados MA, Cullen B, Bienvenu OJ, Shugart YY, Liang K, Hoehn-Saric R, Wang Y, Ronquillo J, Nestadt G, Murphy DL. Familiality of factor analysis-derived YBOCS dimensions in OCD-affected sibling pairs from the OCD Collaborative Genetics Study. Biological Psychiatry. 2007 doi: 10.1016/j.biopsych.2006.05.040. [DOI] [PubMed] [Google Scholar]
- Ivarsson T, Valderhaug R. Symptom patterns in children and adolescents with obsessive-compulsive disorder (OCD) Behaviour Research and Therapy. 2006;44:1105–1116. doi: 10.1016/j.brat.2005.08.008. [DOI] [PubMed] [Google Scholar]
- Jaisoorya TS, Janardhan Reddy YC, Srinath S. Is juvenile obsessive-compulsive disorder a developmental subtype of the disorder? Findings from an Indian study. European Child and Adolescent Psychiatry. 2003;12:290–297. doi: 10.1007/s00787-003-0342-2. [DOI] [PubMed] [Google Scholar]
- Korszun A, Moskvina V, Brewster S, Craddock N, Ferrero F, Gill M, Jones IR, Jones LA, Maier W, Mors O, Owen MJ, Preisig M, Reich T, Rietschel M, Farmer A, McGuffin P. Familiality of symptom dimensions in depression. Archives of General Psychiatry. 2004;61:468–474. doi: 10.1001/archpsyc.61.5.468. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Grice DE, Boardman J, Zhang H, Vitale A, Bondi C, Alsobrook J, Peterson BS, Cohen DJ, Rasmussen SA, Goodman WK, McDougle CJ, Pauls DL. Symptoms of obsessive-compulsive disorder. American Journal of Psychiatry. 1997;154:911–917. doi: 10.1176/ajp.154.7.911. [DOI] [PubMed] [Google Scholar]
- Leckman JF, Pauls DL, Zhang H, Rosario-Campos MC, Katsovich L, Kidd KK, Pakstis AJ, Alsobrook JP, Robertson MM, McMahon WM, Walkup JT, van de Wetering BJM, King RA, Cohen DJ. Obsessive-compulsive symptom dimensions in affected sibling pairs diagnosed with Gilles de la Tourette syndrome. American Journal of Medical Genetics. 2003;116B:60–68. doi: 10.1002/ajmg.b.10001. [DOI] [PubMed] [Google Scholar]
- Liddle PF, Friston KJ, Frith CD, Hirsch SR, Jones T, Frackowiak RS. Patterns of cerebral blood flow in schizophrenia. British Journal of Psychiatry. 1992;160:179–186. doi: 10.1192/bjp.160.2.179. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Fyer AJ, Endicott J, Klein DF. Family Informant Schedule and Criteria. New York: Anxiety Family Study Unit, New York State Psychiatric Institute; 1985. [Google Scholar]
- Mannuzza S, Fyer AJ, Klein DF, Endicott J. Schedule for Affective Disorders and Schizophrenia - Lifetime Version modified for the study of anxiety disorders (SADS-LA): Rationale and conceptual development. Journal of Psychiatric Research. 1986;20:317–325. doi: 10.1016/0022-3956(86)90034-8. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Marks IM, Greist JH, Kobak KA, Baer L. Obsessive-compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: results from a controlled trial. Psychotherapy and Psychosomatics. 2002;71:255–262. doi: 10.1159/000064812. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Rauch SL, Manzo PA, Jenike MA, Baer L. Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. American Journal of Psychiatry. 1999;156:1409–1416. doi: 10.1176/ajp.156.9.1409. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D, Rosario-Campos MC, Leckman JF. A multidimensional model of obsessive-compulsive disorder. American Journal of Psychiatry. 2005;162:228–238. doi: 10.1176/appi.ajp.162.2.228. [DOI] [PubMed] [Google Scholar]
- McKay D, Piacentini J, Greisberg S, Graae F, Jaffer M, Miller J. The structure of childhood obsessions and compulsions: dimensions in an outpatient sample. Behaviour Research and Therapy. 2006;44:137–146. doi: 10.1016/j.brat.2005.02.001. [DOI] [PubMed] [Google Scholar]
- Miguel EC, Leckman JF, Rauch S, Rosario-Campos MC, Hounie AG, Mercadante MT, Chacon P, Pauls DL. Obsessive-compulsive disorder phenotypes: Implications for genetic studies. Molecular Psychiatry. 2005;10:258–275. doi: 10.1038/sj.mp.4001617. [DOI] [PubMed] [Google Scholar]
- Muthén B, Muthén L. Mplus User's Guide. 3rd ed. Los Angeles: Authors; 1998–2004. [Google Scholar]
- Nestadt G, Samuels J, Riddle M, Bienvenu OJ, Liang KY, LaBuda M, Walkup J, Grados M, Hoehn-Saric R. A family study of obsessive-compulsive disorder. Archives of General Psychiatry. 2000;57:358–363. doi: 10.1001/archpsyc.57.4.358. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric Theory. 3rd ed. Toronto: McGraw-Hill; 1994. [Google Scholar]
- Pauls DL, Alsobrook JP, Goodman W, Rasmussen S, Leckman JF. A family study of obsessive-compulsive disorder. American Journal of Psychiatry. 1995;152:76–84. doi: 10.1176/ajp.152.1.76. [DOI] [PubMed] [Google Scholar]
- Pinto A, Eisen JL, Mancebo MC, Greenberg BD, Stout RL, Rasmussen SA. Taboo thoughts and doubt/checking: A refinement of the factor structure for obsessive compulsive disorder symptoms. Psychiatry Research. doi: 10.1016/j.psychres.2006.09.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto A, Mancebo MC, Eisen JL, Pagano ME, Rasmussen SA. The Brown Longitudinal Obsessive Compulsive Study: Clinical features and symptoms of the sample at intake. Journal of Clinical Psychiatry. 2006;67:703–711. doi: 10.4088/jcp.v67n0503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen SA, Eisen JL. Clinical and epidemiologic findings of significance to neuropharmacologic trials in OCD. Psychopharmacology Bulletin. 1988;24:466–470. [PubMed] [Google Scholar]
- Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: Its application to schizophrenia. American Journal of Psychiatry. 1970;126:983–987. doi: 10.1176/ajp.126.7.983. [DOI] [PubMed] [Google Scholar]
- Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D, Katsovich L, Scahill L, King RA, Woody SR, Tolin D, Hollander E, Kano Y, Leckman JF. The Dimensional Yale-Brown Obsessive-Compulsive Scale (DY-BOCS): an instrument for assessing obsessive-compulsive symptom dimensions. Molecular Psychiatry. 2006;11:495–504. doi: 10.1038/sj.mp.4001798. [DOI] [PubMed] [Google Scholar]
- Rovine MJ. Estimating nonshared environment using sibling discrepancy scores. In: Hetherington EM, Reiss D, Plomin R, editors. Separate Social Worlds of Siblings: The Impact of Nonshared Environment on Development. Hillsdale, NJ: Erlbaum; 1994. pp. 33–61. [Google Scholar]
- Samuels J, Bienvenu OJ, 3rd, Riddle MA, Cullen BA, Grados MA, Liang KY, Hoehn-Saric R, Nestadt G. Hoarding in obsessive compulsive disorder: results from a case-control study. Behaviour Research and Therapy. 2002;40:517–528. doi: 10.1016/s0005-7967(01)00026-2. [DOI] [PubMed] [Google Scholar]
- Samuels JF, Riddle MA, Greenberg BD, Fyer AJ, McCracken JT, Rauch SL, Murphy DL, Grados MA, Pinto A, Knowles JA, Piacentini J, Cannistraro PA, Cullen B, Bienvenu OJ, 3rd, Rasmussen SA, Pauls DL, Willour VL, Shugart YY, Liang K, Hoehn-Saric R, Nestadt G. The OCD Collaborative Genetics Study: Methods and sample description. American Journal of Medical Genetics. 2006;141B:201–207. doi: 10.1002/ajmg.b.30224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxena S, Brody AL, Maidment KM, Smith EC, Zohrabi N, Katz E, Baker SK, Baxter LR. Cerebral glucose metabolism in obsessive-compulsive hoarding. American Journal of Psychiatry. 2004;161:1038–1048. doi: 10.1176/appi.ajp.161.6.1038. [DOI] [PubMed] [Google Scholar]
- Saxena S, Maidment KM, Brody AL, Baxter LR. Paroxetine treatment of compulsive hoarding; Annual Meeting of the American College of Neuropsychopharmacology; Waikaloa, HI: 2005. [Google Scholar]
- Saxena S, Maidment KM, Vapnik T, Golden G, Rishwain T, Rosen RM, Tarlow G, Bystritsky A. Obsessive-compulsive horading: symptom severity and response to multimodal treatment. Journal of Clinical Psychiatry. 2002;63:21–27. [PubMed] [Google Scholar]
- Steiger JH, Lind J. Statistically based tests for the number of common factors, the Annual meeting of the Psychometric Society; Iowa City: 1980. [Google Scholar]
- Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B, Faraone SV. Long-term outcome of pediatric obsessive-compulsive disorder: A meta-analysis and qualitative review of the literature. Acta Psychiatrica Scandinavica. 2004;110:4–13. doi: 10.1111/j.1600-0447.2004.00302.x. [DOI] [PubMed] [Google Scholar]
- Stewart SE, Rosario MC, Brown TA, Carter AS, Leckman JF, Sukhodolsky D, Katsovitch L, King R, Geller D, Pauls DL. Principal components analysis of obsessive-compulsive disorder symptoms in children and adolescents. Biological Psychiatry. 2007;61:285–291. doi: 10.1016/j.biopsych.2006.08.040. [DOI] [PubMed] [Google Scholar]
- Summerfeldt LJ, Richter MA, Antony MM, Huta VM, Swinson RP. Symptom structure in OCD: Factor analytic evidence for subgroups; 1997 Annual Meeting New Research Program and Abstracts; Washington, DC: American Psychiatric Association; 1997. [Google Scholar]
- Summerfeldt LJ, Richter MA, Antony MM, Swinson RP. Symptom structure in obsessive-compulsive disorder: A confirmatory factor-analytic study. Behaviour Research and Therapy. 1999;37:297–311. doi: 10.1016/s0005-7967(98)00134-x. [DOI] [PubMed] [Google Scholar]
- Zhang H, Leckman JF, Pauls DL, Tsai CP, Kidd KK, Campos MR. Genomewide scan of hoarding in sib pairs in which both sibs have Gilles de la Tourette syndrome. American Journal of Human Genetics. 2002;70:896–904. doi: 10.1086/339520. [DOI] [PMC free article] [PubMed] [Google Scholar]