Abstract
Hypnosis is widely recognized as an empirically supported intervention to improve postsurgical outcomes. However, to date, no research has examined mediators of hypnotic benefit among surgery patients. The present study was designed to test the hypotheses that response expectancies and emotional distress would mediate the effects of an empirically validated presurgical hypnosis intervention on postsurgical side effects (i.e., pain, nausea, and fatigue). In a sample of 200 women undergoing breast conserving surgery (mean age = 48.50 years), structural equation modeling revealed the following: 1) hypnotic effects on postsurgical pain were partially mediated by pain expectancy (p< .0001), but not by distress (p=.12); 2) hypnotic effects on postsurgical nausea were partially mediated by presurgical distress (p=.02), but not by nausea expectancy (p=.10); 3) hypnotic effects on postsurgical fatigue were partially mediated by both fatigue expectancy (p=.0001) and presurgical distress (p=.02). These results improve understanding of the underlying mechanisms responsible for hypnotic phenomena in the surgical setting, and suggest that future hypnotic interventions target patient expectancies and distress to improve postsurgical recovery.
Keywords: hypnosis, surgery, expectancy, distress, mediation
While there are a number of published definitions of hypnosis (e.g., Green, Barabasz, Barrett, & Montgomery, 2004; Kihlstrom, 1985; Kirsch, 1994), hypnosis may be defined as an agreement between a person designated as the hypnotist (e.g., healthcare professional), and a person designated as the client or patient, to participate in a psychotherapeutic technique based on the hypnotist providing suggestions for changes in sensation, perception, cognition, affect, mood, or behavior (Montgomery & Schnur, 2007). For more than a century, the success of hypnosis in improving postsurgical recovery has been documented. Initially, case series designs were used. For example, in the 1800s, James Esdaile reported a 50% decrease in mortality in battlefield surgical patients with whom he used hypnosis (Gravitz, 1988). More recently, randomized controlled trials (Lang et al., 2000; Montgomery et al., 2007) and meta-analyses (Montgomery, David, Winkel, Silverstein, & Bovbjerg, 2002a; Montgomery, DuHamel, & Redd, 2000; Schnur, Kafer, Marcus, & Montgomery, 2008b) have convincingly demonstrated that hypnosis is an effective intervention for controlling side effects of aversive medical procedures, including pain, nausea and fatigue associated with surgery. Meta-analytic data on the effectiveness of hypnosis for surgical patients have shown that 89% of surgical patients in hypnosis groups benefit relative to control group patients (Montgomery et al., 2002a).
However, the empirical literature describing how hypnosis exerts its beneficial effects has not kept pace with clinical outcome data. Although some very early proposed mechanisms (e.g., animal magnetism) (Kirsch, Lynn, & Rhue, 1993) have been discarded, few mechanisms underlying the beneficial effects of hypnosis have been tested in clinical settings, and only a handful in the surgical context (e.g., Montgomery, Weltz, Seltz, & Bovbjerg, 2002b). The dearth of empirical research on mechanisms underlying hypnotic benefit in clinical settings is surprising for at least two reasons. First, there has been a great deal of theoretical debate within the hypnosis community concerning the necessary and sufficient elements of hypnosis (see American Journal of Clinical Hypnosis, Vol. 48, Issue 2–3). This debate has yielded a great number of studies of the mediators (e.g., response expectancies) and moderators (e.g., hypnotic suggestibility) of hypnotic effects. Yet as a general rule, these studies have used healthy volunteer participants rather than clinical populations (e.g., Braffman & Kirsch, 1999; Milling, Reardon, & Carosella, 2006), and results may not generalize to patients facing the threat of surgery. Second, the volume of studies investigating moderators of hypnotic effects (e.g., hypnotic suggestibility) has been far greater than the volume of studies investigating underlying mechanisms (i.e., mediators). That is, the question, “For whom does hypnosis work best?” has received greater scientific attention than the question, “How does hypnosis work?” Learning how hypnosis works is critical to designing and improving hypnotic interventions that specifically target active change mechanisms (Kazdin & Nock, 2003).
Although research on the mediation of hypnotic effects in surgical settings is sparse, two possible mediators have been suggested: response expectancies and emotional distress. Response expectancies (Kirsch, 1985; Kirsch, 1990) are specific expectations for non-volitional outcomes, rather than expectations for behaviors or external events. For example, the expectation that one will become nauseated is a response expectancy, whereas expectations that one will be able to lift one's arm, or that it will rain today are not. Response expectancies reflect automatic (i.e., typically not under voluntary control) processes, and they are hypothesized to directly cause expected outcomes. Work by Kirsch and others has supported the role of response expectancies as a mediator of hypnotic effects outside the surgical setting (e.g., Schoenberger, Kirsch, Gearan, Montgomery, & Pastyrnak, 1997; Wickless & Kirsch, 1989), lending support for this line of inquiry.
The hypothesis that response expectancies lead to postsurgical side effects, including pain, nausea and fatigue, has received some support. For example, in a mixed sample of 183 surgical inpatients, Rubin and colleagues (Rubin, Cleare, & Hotopf, 2004) demonstrated that presurgery expectations of fatigue significantly predicted fatigue following surgery. A study of breast cancer surgical patients indicated that presurgery response expectancies predicted postsurgery pain and fatigue at discharge, however, a significant association between presurgery expectancies for nausea and postsurgery nausea was not found (p < .07) (Montgomery & Bovbjerg, 2004). Expectancies did predict postsurgery nausea in a sample of general, orthopedic, and urologic surgical patients (Sidebotham, Reddy, & Schug, 1997).
To date, only one study has examined response expectancies as a mediator of hypnotic effects in the surgical setting. In that preliminary study of 20 breast cancer surgical patients (Montgomery et al., 2002b), response expectancies were found to mediate the effects of hypnosis on postsurgical pain based on the statistical criteria established by Baron & Kenny (1986). However, due to the small sample size, these results must be viewed with some caution. Additionally, further testing is required to investigate whether expectancies mediate the effects of hypnosis on other common postsurgical side effects (e.g., nausea, fatigue).
Although it has not been tested directly to date, the possibility that emotional distress is a mediator of beneficial hypnotic effects on postsurgical outcomes is plausible for two reasons: 1) higher levels of emotional distress are predictive of higher levels of postsurgical side effects (e.g., pain, nausea and fatigue), and 2) hypnosis is effective in reducing emotional distress related to medical procedures. In a large number of studies with a variety of patient populations, surgical patients’ presurgery levels of emotional distress significantly predict postsurgery pain (Arntz, van Eck, & Heijmans, 1990; Croog, Baume, & Nalbandian, 1995; Kain, Servarino, Aleander, Pincus, & Mayes, 2000; Katz et al., 2005; Martinez-Urrutia, 1975; Nelson, Zimmerman, & Barnason, 1998; Pick, Pearce, & Legg, 1990; Scott, Clum, & Peoples, 1983; Thomas, Robinson, Champion, McKell, & Pell, 1998). For example, Croog et al. (1995) found that presurgery distress predicted postsurgery pain in dental patients; presurgery state anxiety has been associated with postsurgery pain in cholecystectomy patients (Scott et al., 1983); and Pick et al. (1990) have reported that presurgery distress predicted postsurgery pain intensity in abdominal surgery patients. However, the contribution of emotional distress to postsurgical side effects may not be limited to postsurgical pain. Presurgery distress is also widely believed to be a predisposing factor for postsurgery nausea and vomiting (see Mann, 1998; Watcha & White, 1992). Indeed, anesthesiologists commonly treat heightened distress prior to surgery as a clinical risk factor for postsurgery nausea and vomiting (Mann, 1998). Similarly, emotional distress may contribute to postsurgery levels of fatigue. Supporting this view, Rubin and colleagues (2004) found significant relationships between emotional distress and fatigue in surgery patients at three postsurgery time points. Also, our own study of breast cancer surgical patients has demonstrated that presurgery distress contributes to postsurgery nausea and fatigue after controlling for expectancies in breast cancer surgical patients (Montgomery & Bovbjerg, 2004). Further supporting the potential for mediation of hypnotic effects by emotional distress, both meta-analyses (Schnur et al., 2008b) and randomized clinical trials (Lang et al., 2006; Schnur et al., 2008a) have demonstrated that hypnosis is an effective means for controlling distress related to invasive medical procedures.
Our previous work has demonstrated that hypnosis is an effective treatment for decreasing nausea, fatigue, and pain following breast cancer surgery (Montgomery et al., 2007). However, the mechanisms of these positive effects remains to be illuminated. Pain, nausea, and fatigue are particularly severe problems following breast cancer surgery (Pavlin et al., 1998; Pavlin, Chen, Penaloza, Polissar, & Buckley, 2002; Quinn, Brown, Wallace, & Ashbury, 1994; Shimozuma, Ganz, Petersen, & Hirji, 1999; Watcha & White, 1992), and each has been demonstrated to be responsive to a hypnotic intervention (Montgomery et al., 2007). The purpose of the present study was to investigate the possibility that response expectancies and emotional distress each independently contribute to the mediation of the beneficial effects of presurgery hypnosis on side effects in a sample of breast cancer surgical patients. We hypothesized that the benefits of presurgical hypnosis on postsurgical pain, nausea and fatigue would be significantly mediated by both presurgery response expectancies and emotional distress.
Method
Participants
Participants have been previously described in detail in a previous report demonstrating the clinical effectiveness of presurgical hypnosis for breast cancer surgical patients (Montgomery et al., 2007). In brief, the sample was composed of female patients (N = 200) scheduled for breast conserving surgery (i.e., excisional breast biopsy, lumpectomy). All participants completed IRB-approved written informed consent. Participants were included if they were at least 18 years of age and scheduled to undergo breast conserving surgery; and were excluded if they were currently in treatment for a psychiatric illness or were unable to read and understand English. The mean age of the sample was 48.50 years (SD= 13.05), and the ethnic composition was 63% White, 15% Hispanic, 13% African American, and 9% Other. Thirteen percent had a high school education or less, 24% attended some college, 37% were college graduates, and 26% had some postgraduate education. Fifty-one percent were married. Seventy-four percent underwent an excisional breast biopsy and 26% underwent lumpectomy. None of these variables differed between the hypnosis intervention group and the attention control group (all ps > .40).
Measures
Demographic information was collected from patients using mailed questionnaires (e.g., age, education, marital status). Medical charts were reviewed and abstracted for apposite medical and surgical data (e.g., type of surgery).
Mediators
Response expectancies for postsurgical pain, nausea, and fatigue were assessed using 3 visual analog scale items prior to surgery. Each item was administered twice, once before and once after the study intervention session (Hypnosis or Attention Control). The same 100 mm visual analog scale format was used for each item, however prompts and anchors differed. For example, the VAS item for expected pain stated, “After surgery, how much pain do you think you will feel? Please put a slash through this line (a 100 mm line shown below on actual forms) to indicate how much pain you expect to feel.” This line was anchored by “no pain at all” and “as much pain as there could be.” VAS scores range from 0–100 based on how many millimeters from the left participants made their mark on the line. These visual analog scale items have been used in our previous research with this patient population (Montgomery & Bovbjerg, 2004; Schnur et al., 2007).
Presurgery (post-intervention) emotional distress was assessed using the tension/anxiety subscale of the Short Version of the Profile of Mood States (SV-POMS) (DiLorenzo, Bovbjerg, Montgomery, Jacobsen, & Valdimarsdottir, 1999) as well as visual analog scale items. The SV-POMS tension/anxiety subscale consists of six items. Each item is scored on a 0 (Not at all) to 4 (Extremely) scale and the item scores are summed. Reliability of the tension/anxiety subscale has been documented for breast cancer patients (Cronbach’s alpha = .86) (DiLorenzo et al., 1999).
Visual Analog Scale items were used to measure post-intervention (but presurgery) current levels of emotional upset and relaxation. The VAS items had the same format as the expectancy items described above. For example, the VAS item for emotional upset stated, “Right now, how emotionally upset do you feel? Please put a slash through this line (a 100 mm line shown below on actual forms) to indicate how emotionally upset you feel.” This line was anchored by “not at all upset” and “as upset as I could be.” VAS items are reliable and valid measures (Ahearn, 1997), have been previously used with breast cancer surgical patients (Montgomery & Bovbjerg, 2004; Schnur et al., 2008a), and are practical and effective in the rushed surgical environment where time for completion of measures is extremely limited.
Outcomes
100 mm visual analog scales (VASs) were used to assess patients’ postsurgery subjective pain, nausea, and fatigue (Bijur, Silver, & Gallagher, 2001; Boogaerts, Vanacker, Seidel, Albert, & Bardiau, 2000; Coll, Ameen, & Mead, 2004; McCarthy et al., 2005; Montgomery et al., 2004; Montgomery et al., 2002b; Price et al., 1999; Tanabe et al., 2004; Wolfe, 2004). VASs were administered by BA and MA level research assistants after patients reached standardized hospital criteria for discharge (Chung, Chan, & Ong, 1995).
Procedures
Breast cancer surgical patients were randomly assigned to a hypnosis intervention group or to an attention control group, as previously described (Montgomery et al., 2007). The hypnosis intervention was a 15 minute session led by a psychologist prior to breast cancer surgery, on the morning of surgery. The scripted hypnosis session included a relaxation-based induction (imagery for muscle relaxation), suggestions for pleasant visual imagery, suggestions to experience relaxation and peace, specific symptom-focused suggestions (e.g., reduced postsurgical pain, nausea, fatigue), a deepening procedure, and instructions for how patients could use hypnosis on their own.
Patients in the Attention Control Group spent identical amounts of time with study personnel as patients in the Hypnosis Group to control for professional attention. The attention control condition was led by the same interventionists who led the hypnosis intervention sessions. However, the interventionists did not lead the Attention Control patients in imagery, relaxation, or even simple discussion. Rather the interventionists allowed patients to direct the flow of the conversation and provided supportive/empathic comments according to standardized procedures (Lang, Speigel, Lutgendorf, & Logan, 1996). The interventionists matched verbal and nonverbal communication patterns, listened attentively, avoided the use of prejudicial or negatively valued language, and used emotionally neutral descriptors in conversation (Lang et al., 1996).
Assessment procedures were as follows. One week before scheduled surgery, patients were mailed the demographic questionnaire to complete at home. This questionnaire was returned to study staff on the morning of surgery. Upon arrival to the hospital on the morning of surgery, patients completed the expectancy measures in order to account for initial expectancy levels. Patients then participated in either a hypnosis intervention session or an attention control session as described above. Immediately following this session (post-intervention), patients completed the assessments of the mediating variables (both expectancy and emotional distress). Following completion of this packet, patients underwent breast surgery. Following surgery, and upon meeting standardized criteria for hospital discharge (Chung et al., 1995) participants completed the outcome measures. All patients were discharged the same day as their breast cancer surgery.
Analytic Approach
Structural equation modeling was used to test simultaneously whether the effect of the hypnosis intervention on postsurgical side effects was mediated by expectancy and/or distress. Models were constructed and tested using maximum likelihood estimation in Mplus version 5.0 (Muthen & Muthen, 2007). Because several related measures of distress were collected immediately following the intervention, a latent distress variable was formed consisting of the POMS Tension/Anxiety subscale, emotional upset VAS, and relaxation VAS (which loaded negatively on distress). A separate confirmatory factor analytic model was analyzed in order to assess the utility of aggregating the three indicators of distress in a single latent variable and to ensure that the measurement component of the model provided a good fit to the data (McDonald & Ho, 2002; Tomarken & Waller, 2003). Fit indices and factor loading estimates indicated that the latent distress variable fit the data quite well (see Results below).
Separate models were constructed for each of the postsurgical side effect outcome variables: pain, nausea and fatigue. In each case, two mediators were tested in the model: expectancy for that outcome (e.g., expected pain predicts experienced pain) and emotional distress prior to surgery. Mediation effects were tested by computing the product of the path coefficients composing the indirect effect (i.e., the path from the intervention to the mediator and from the mediator to the outcome) divided by the bootstrapped standard error of the product. Bootstrapped standard errors were utilized because the underlying distribution of such mediation coefficients is not normally distributed and failure to account for this can reduce statistical power when testing mediation effects (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; Shrout & Bolger, 2002). One thousand bootstrapped samples were utilized to estimate the standard errors of the path coefficients. Multivariate outliers having undue influence on path estimates were identified in each model by examining Cook’s Distance and Mahalanobis Distance measures, and participants with Cook’s D values of > 1.0 and/or Mahalonobis Distance probabilities of p < .001 were removed from models (Cohen, Cohen, West, & Aiken, 2003). Outlier trimming resulted in removal of 5 cases for postsurgical nausea, 4 cases for postsurgical fatigue, and 2 cases for postsurgical pain. Model comparisons with and without outliers supported the importance of removing these cases, as path estimates varied greatly as a function of only a few outlier cases. Residual variances for the mediators were permitted to covary in the structural models, as these measures were gathered at the same time point and modification indices indicated a significant relationship. In addition, each model included a direct path from Group (Hypnosis vs. Attention Control) to the outcome, which provided insight into whether the Group effect was perfectly mediated by expectancy and distress (Baron & Kenny, 1986). Additionally, pre-intervention expectancy (measured immediately before the intervention) was included as a predictor of post-intervention expectancy, thereby controlling for individual differences in expectancy prior to the intervention. Consequently, the effect of the intervention on side effect expectancy represents change in expectancy due to the intervention, or said differently, the path from intervention to expectancy represents the difference between the control group and the hypnosis group, controlling for pre-intervention expectancies. Lastly, in order to test whether surgery type (lumpectomy versus excisional biopsy) moderated the results, multiple-groups models were tested. However, for all three outcomes, Wald chi-squared tests comparing constrained (in which all paths were constrained to be equal across surgery types) versus unconstrained models (in which paths were free to vary across surgery types) indicated no significant differences between surgery types (all ps > .10). Surgery type did not moderate the findings; thus, models combining surgery types are reported below.
In reporting the results, we have adopted the widely used notation described by Baron and Kenny (1986): a refers to the path from the intervention to the mediator, b refers to the path from the mediator to the outcome, c’ refers to the direct path from intervention to outcome after controlling for both mediators (expectancy and distress), and ab refers to the product of the a and b coefficients, which represents the indirect effect of the intervention on the outcome via the mediator.
Results
Postsurgical Pain
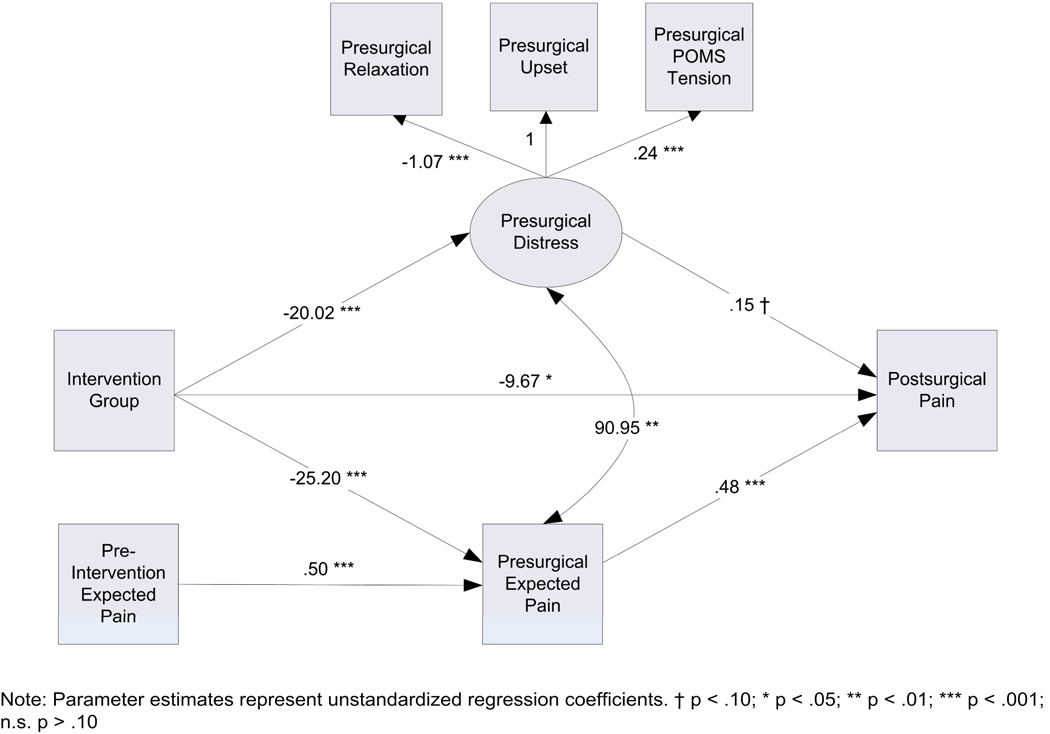
The effect of hypnosis on postsurgical pain was partially mediated by pain expectancy, but not distress (Figure 1). Fit indices indicated that the model approximated the data quite well: χ2(10) = 10.73, p = .38, CFI = 1.00, RMSEA = .02 (90% CI = .00–.08), SRMR = .02. The indirect effect of the intervention on postsurgical pain via pain expectancy was significant: ab = −12.00, S.E. = 3.08, p < .0001. However, presurgical distress did not mediate the intervention–pain relationship: ab = −3.03, S.E. = 1.93, p = 12, despite the fact that the intervention reduced presurgical distress, a = −20.02, S.E. 3.72, p < .0001. The effect of the hypnotic intervention on postsurgical pain was not fully accounted for by the mediators, c’ = −9.67, S.E. = 4.81, p = .04. The model accounted for 33% of the variance in postsurgical pain. Because distress was not found to mediate the intervention-pain relationship (i.e., we failed to find that ab was significantly different from 0), no attempt to compare standardized mediation coefficients was made.
Figure 1.
Structural equation model describing the mediation of hypnosis effects on postsurgical pain.
Postsurgical Nausea
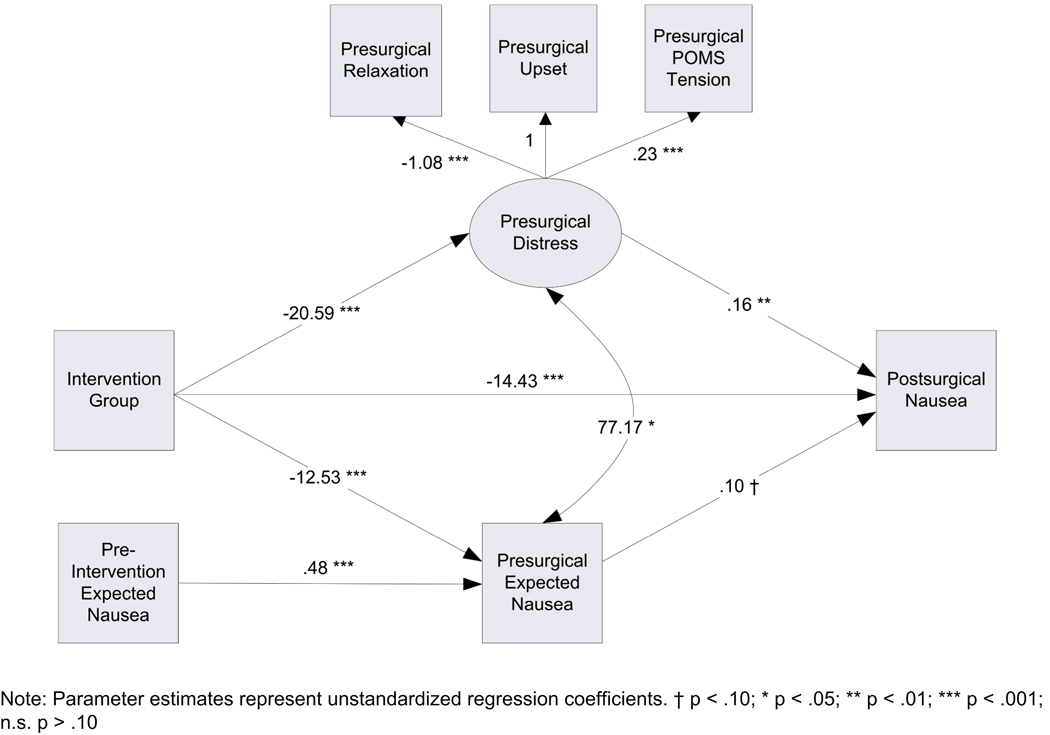
The effect of the hypnotic intervention on postsurgical nausea was partially mediated by presurgical distress and there was also a trend toward mediation by nausea expectancy (Figure 2). The indirect effect of the intervention on postsurgical nausea via presurgical distress was significant, ab = −3.31, S.E. = 1.40, p = .02. Nausea expectancy did not mediate the intervention–nausea effect, ab = −1.21, S.E. = 0.73, p = .10. Nausea expectancy was significantly reduced by the hypnotic intervention, a = −12.53, S.E. = 3.01, p < .0001, but the effect of nausea expectancy on postsurgical nausea was marginal, b = .10, S.E. = .06, p = .09. Thus, the failure of nausea expectancy as a mediator seems to be due to the low association between nausea expectancy and experienced nausea. The effect of the hypnotic intervention on postsurgical nausea remained significant after controlling for expectancy and distress, c’ = −14.43, S.E. = 2.43, p < .0001, suggesting that there may be additional mechanisms of the intervention. The model accounted for 30% of the observed variance in postsurgical nausea and fit the data well: χ2(10) = 13.99, p = .17, CFI = 0.99, RMSEA = .04 (90% CI = .00–.09), SRMR = .04. In order to compare the relative magnitude of the mediation effects, standardized estimates of the ab coefficients, αβ, were computed, which represent coefficients computed on variables that have been standardized to have a mean of zero and standard deviation of one (Cohen et al. 2003). For the presurgical distress mediation path, αβ = −.09, whereas the mediation path for nausea expectancy was αβ =−.03, indicating that distress was approximately three times more potent than expectancy as a mediator.
Figure 2.
Structural equation model for the mediation of hypnosis effects on postsurgical nausea.
Postsurgical Fatigue
The structural equation model for postsurgical fatigue revealed that the effect of the hypnosis intervention was partially mediated by presurgical distress and expected fatigue (Figure 3). The model fit the data reasonably well: χ2(10) = 18.76, p = .04, CFI = 0.98, RMSEA = .07 (90% CI = .01–.12), SRMR = .05. The indirect effect of the intervention on postsurgical fatigue via fatigue expectancy was significant: ab = −8.87, S.E. = 2.68, p = .001. Presurgical distress was also found to mediate the intervention–fatigue relationship: ab = −4.77, S.E. = 2.12, p = .02. The direct effect of the intervention on postsurgical fatigue remained significant after controlling for these mediators, c’ = −9.91, S.E. = 4.72, p = .04. The model accounted for 26% of the variance in postsurgical fatigue. Comparison of the standardized mediation coefficients for the two mediators revealed that fatigue expectancy was approximately twice as potent as presurgical distress: αβ (expectancy) = −.14, αβ (distress) = −.077.
Figure 3.
Structural equation model for the mediation of hypnosis effects on postsurgical fatigue.
Discussion
The purpose of the present study was to investigate two potential psychological mediators of the beneficial effects of a brief hypnosis intervention for breast cancer surgery patients. The pattern of results suggests that hypnosis may operate via different mechanisms depending on the postsurgical side effect in question. Specifically, post-intervention expectancies partially mediated the effect of hypnosis on postsurgical pain and fatigue. Expectancies did not significantly contribute to postsurgery nausea after accounting for distress. Post-intervention distress partially meditated the effect of hypnosis on postsurgical nausea and fatigue. Distress did not contribute to postsurgery pain after accounting for expectancies. In regard to fatigue where both mediators were significant, the effect size for the contribution of expectancies was twice that of distress. Each of the models accounted for roughly 30% of the variance in postsurgical side effects. In each of the three models, presurgery expectancies and distress were significantly related. However, response expectancies and distress differentially mediated hypnosis effects.
When postsurgery pain was examined as the outcome, the results were consistent with: 1) The broad literature suggesting that expectancies predict pain (Montgomery & Bovbjerg, 2004; Montgomery & Kirsch, 1997; Price et al., 1999); 2) Prior experimental studies (using college student samples and investigational pain stimulators) which demonstrated that response expectancies mediated the effects of hypnosis on pain (Milling et al., 2006; Milling, Shores, Coursen, Menario, & Farris, 2007); and, 3) Small sample clinical studies also suggesting that response expectancies mediate the effects of hypnosis in surgical patients (Montgomery et al., 2002b). Together, these data suggest that hypnosis is a successful means to change expectancies for pain, and consequently reduce the experience of postsurgery pain itself in the clinical setting.
Given the extent of the literature linking presurgery distress to postsurgery pain, it is somewhat surprising that differences in distress levels between the hypnosis and control groups did not significantly contribute to the effectiveness of hypnosis intervention. This may be due to differences in study design. That is, the vast majority of studies assessing the contribution of distress to pain in surgery patients do not include the expectancy construct (e.g., Katz et al., 2005), while the present design does. The present results suggest that failure to account for expectancies in predictive models may inflate the amount of variance accounted for by distress. However, a limitation of our approach is that we did not address the multidimensional nature of pain (Melzack & Wall, 1983) from an expectancy perspective. That is, future research may wish to assess sensory and affective pain expectancies, as well as sensory and affective pain, in order to establish a more comprehensive understanding of patients’ postsurgery experiences.
When postsurgery nausea was examined as the outcome, the results revealed that the hypnosis intervention exerted its effects though distress, while the contribution of expectancies to nausea was not significant. The lack of an expectancy effect on nausea is consistent with research showing that expectancies do not contribute to nausea following the first chemotherapy infusion in breast cancer patients (Montgomery & Bovbjerg, 2000). However, that same research revealed that expectancies did contribute to posttreatment nausea after subsequent chemotherapy infusions. Together, these findings suggest that the association between expectancies and nausea may require greater experience in the specific surgical situation in order for expectancies to contribute to nausea outcomes (Montgomery & Bovbjerg, 2000; Rotter, 1982). Future research may wish to test this possibility in patients undergoing multiple surgical procedures. Clinically, these results suggest the importance of controlling and reducing patient distress prior to surgery in order to improve postsurgery nausea. The results further indicated that hypnosis successfully reduced distress prior to surgery, consistent with the general literature on hypnosis and medical procedures (Schnur et al., 2008b).
The pattern of results differed when fatigue was examined as the outcome. Both presurgery expectancies and distress partially mediated the effects of hypnosis on postsurgery fatigue. Comparison of the mediation coefficients for expectancies and distress revealed that both significantly contributed to the experience of postsurgery fatigue. However, expectancy was approximately twice as potent a mediator as presurgical distress. A limitation of our approach is that we did not address the multidimensional nature of fatigue (Piper, 1996). It is possible that the effects of hypnosis on different dimensions of fatigue are mediated differentially. However, a strength of our approach was that our fatigue measure was not confounded with distress. In other words, the mediator and outcome measures were not explicitly sampling overlapping criteria (e.g., distress).
From the clinical perspective, these results reinforce the view that presurgery expectancies and distress should be targeted for intervention prior to breast cancer surgery to improve pain, nausea and fatigue outcomes. Interventions that target only one mechanism or the other may fail to maximize overall clinical benefit for patients, and may leave them suffering unnecessarily. The present results indicating the significant relationship between presurgery response expectancies and distress only reinforce this interpretation. Hypnosis efficiently and effectively modified both expectancies and distress, and the present results indicate concomitant improvements in postsurgical recovery. Other psychological interventions for individuals undergoing medical procedures may also work through the same mechanisms. It would be of interest to investigate whether other interventions (e.g., cognitive-behavioral therapy) also exert their effects in this population through response expectancies and distress.
A limitation of the present study was that we did not include one of the most recognized moderators of hypnotic effects, hypnotic suggestibility (Hilgard, 1965). Hypnotic suggestibility was not included for two reasons: 1) the focus of the present study was on mediators of hypnotic effects in the breast cancer surgical setting, not moderators; 2) The most commonly used and best supported measures of hypnotic suggestibility (Shor & Orne, 1962; Spanos, Radtke, Hodgins, Stam, & Bertrand, 1983; Weitzenhoffer & Hilgard, 1962) take approximately 30–60 minutes to administer. Such a lengthy assessment procedure is not practical in the busy surgical setting, as it takes longer to administer the assessment instrument than the intervention itself (15 minutes). Given the success of the intervention for the vast majority of patients (Montgomery et al., 2007), the clinical importance of assessing hypnotic suggestibility in this setting remains to be demonstrated.
A second limitation of the study is that we did not include assessments of all potential mediators (i.e., distress) prior to the intervention. Although classic approaches to mediation (Baron & Kenny, 1986) do not require such pre-assessments, their addition would have likely have strengthened present arguments regarding mediation. A third limitation of the study is that the mediational effects demonstrated here may or may not generalize to all hypnosis interventions (e.g., lengthier hypnosis interventions), and therefore these effects should be replicated. However, as expectancies are often considered a common factor across psychotherapy techniques in general (Frank & Frank, 1991; Kirsch, 1999), it is likely that expectancies would play some role, regardless of intervention length.
On average, our models accounted for approximately 30% of the variance in the side effect outcomes. Of course, this leaves 70% of the variance in postsugery pain, nausea and fatigue unexplained. A host of medical and surgical factors may account for a large portion of this variance, but one can speculate that other psychological factors may contribute as well. For example, meta-analyses indicate that therapeutic relationship factors (e.g., therapeutic alliance, empathy) have been found to account for 10% of the variance in psychotherapy outcomes (Bohart, Elliott, Greenberg, & Watson, 2002; Horvath & Bedi, 2002; Martin, Garske, & Davis, 2000). Future research may wish to investigate the contribution of these factors to postsurgery outcomes.
Although there have been studies of mediators of hypnotic effects in experimental settings with healthy participants (e.g., Schoenberger et al., 1997; Wickless et al., 1989), few studies have identified mediators in clinical settings. The present results fill that gap. Our study is the first to identify the mediational roles of response expectancies and emotional distress in a sample of breast cancer surgical patients receiving a hypnosis intervention. Despite common misconceptions of hypnosis as frightening or mysterious, our results indicate that hypnosis works to a significant extent through two very basic categories of psychological mechanisms - cognitions and emotions. The present results improve our understanding of the underlying mechanisms responsible for hypnotic phenomena in the surgical setting, are consistent with a sociocognitive view of hypnosis (Kirsch, 1991), and indicate that future hypnotic interventions should specifically target patient expectancies and distress to reduce postsurgical pain, nausea and fatigue. This can be accomplished clinically through wording of hypnotic intervention suggestions to alter expectancies for specific postsurgical side effects (reduced pain, reduced nausea and reduced fatigue), as well as for reduced distress and increased relaxation.
Acknowledgments
This research was supported by grants from the National Cancer Institute (CA129094-01; CA131473) and the American Cancer Society (CRTG 04-213-01-CPPB). The funding agencies had no role in the design, data collection, or data analysis of the study, or in the writing of this manuscript.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- Ahearn EP. The use of visual analog scales in mood disorders: a critical review. Journal of Psychiatric Research. 1997;31:569–579. doi: 10.1016/s0022-3956(97)00029-0. [DOI] [PubMed] [Google Scholar]
- Arntz A, van Eck M, Heijmans M. Predictions of dental pain: the fear of any expected evil is worse than the evil itself. Behavior Research and Therapy. 1990;28:29–41. doi: 10.1016/0005-7967(90)90052-k. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bijur PE, Silver W, Gallagher EJ. Reliability of the visual analog scale for measurement of acute pain. Academic of Emergency Medicine. 2001;8:1153–1157. doi: 10.1111/j.1553-2712.2001.tb01132.x. [DOI] [PubMed] [Google Scholar]
- Bohart AC, Elliott R, Greenberg LS, Watson JC. Empathy. In: Norcross JC, editor. Psychotherapy relationships that work: Therapist contributions and responsiveness to patients. New York, NY: Oxford University Press; 2002. pp. 89–108. [Google Scholar]
- Boogaerts JG, Vanacker E, Seidel L, Albert A, Bardiau FM. Assessment of postoperative nausea using a visual analogue scale. Acta Anaesthesiologica Scandinavica. 2000;44:470–474. doi: 10.1034/j.1399-6576.2000.440420.x. [DOI] [PubMed] [Google Scholar]
- Braffman W, Kirsch I. Imaginative suggestibility and hypnotizability: an empirical analysis. Journal of Personality and Social Psychology. 1999;77:578–587. doi: 10.1037//0022-3514.77.3.578. [DOI] [PubMed] [Google Scholar]
- Chung F, Chan VWS, Ong D. A post-anesthetic discharge scoring system for home readiness after ambulatory surgery. Journal of Clinical Anesthesia. 1995;7:500–506. doi: 10.1016/0952-8180(95)00130-a. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd ed. New Jersey: Lawrence Erlbaum; 2003. [Google Scholar]
- Coll AM, Ameen JR, Mead D. Postoperative pain assessment tools in day surgery: literature review. Journal of Advanced Nursing. 2004;46:124–133. doi: 10.1111/j.1365-2648.2003.02972.x. [DOI] [PubMed] [Google Scholar]
- Croog SH, Baume RM, Nalbandian J. Pre-surgery psychological charectoristics, pain response, and activities impairment in female patients with repeated periodontal surgery. Journal of Psychosomatic Research. 1995;39:39–51. doi: 10.1016/0022-3999(94)00089-n. [DOI] [PubMed] [Google Scholar]
- DiLorenzo TA, Bovbjerg DH, Montgomery GH, Jacobsen PB, Valdimarsdottir H. The application of a shortened version of the profile of mood states in a sample of breast cancer chemotherapy patients. British Journal of Health Psychology. 1999;4:315–325. [Google Scholar]
- Frank JD, Frank JB. Persuasion and healing: A comparative study of psychotherapy. 3rd ed. Baltimore: Johns Hopkins University Press; 1991. [Google Scholar]
- Gravitz MA. Early uses of hypnosis as surgical anesthesia. American Journal of Clinical Hypnosis. 1988;30:201–208. doi: 10.1080/00029157.1988.10402733. [DOI] [PubMed] [Google Scholar]
- Green JP, Barabasz AF, Barrett D, Montgomery GH. Forging Ahead: The 2003 APA Division 30 Definition of Hypnosis. International Journal of Clinical and Experimental Hypnosis. 2004;53:259–264. doi: 10.1080/00207140590961321. [DOI] [PubMed] [Google Scholar]
- Hilgard ER. Hypnotic Susceptibility. New York: Brace and Wared; 1965. [Google Scholar]
- Horvath AO, Bedi RP. The alliance. In: Norcross JC, editor. Psychotherapy relationships that work: Therapist contributions and responsiveness to patients. New York, NY: Oxford University Press, Inc; 2002. pp. 37–69. [Google Scholar]
- Kain ZN, Servarino F, Aleander GM, Pincus S, Mayes LC. Preoperative anxiety and postoperative pain in women undergoing hysterectomy. A repeated-measures design. Journal of Psychosomatic Research. 2000;49:417–422. doi: 10.1016/s0022-3999(00)00189-6. [DOI] [PubMed] [Google Scholar]
- Katz J, Pleshuck E, Andrus C, Hogan L, Jung B, Kulick D, et al. Risk factors for acute pain and its persistence following breast cancer surgery. Pain. 2005;119:16–25. doi: 10.1016/j.pain.2005.09.008. [DOI] [PubMed] [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: methodological issues and research recommendations. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kihlstrom JF. Hypnosis. Annual Review of Physiology. 1985:385–418. doi: 10.1146/annurev.ps.36.020185.002125. [DOI] [PubMed] [Google Scholar]
- Kirsch I. How expectancies shape experience. 1st ed. Washington, DC: American Psychological Association; 1999. [Google Scholar]
- Kirsch I. Response expectancy as a determinant of experience and behavior. American Psychologist. 1985;40:1189–1202. [Google Scholar]
- Kirsch I. Changing expectations: A key to effective psychotherapy. Pacific Grove, CA: Brooks/Cole; 1990. [Google Scholar]
- Kirsch I. Defining hypnosis for the public. Contemporary Hypnosis. 1994;11:142–143. [Google Scholar]
- Kirsch I. The social learning theory of hypnosis. In: Lynn SJ, Rhue JW, editors. Theories of hypnosis: Current models and perspectives. New York: The Guilford Press; 1991. pp. 439–465. [Google Scholar]
- Kirsch I, Lynn SJ, Rhue JW. Introduction to Clinical Hypnosis. In: Rhue JW, Lynn SJ, Kirsch I, editors. Handbook of Clinical Hypnosis. Washington, DC: American Psychological Association; 1993. pp. 3–22. [Google Scholar]
- Lang EV, Benotsch EG, Fick LJ, Lutgendorf S, Berbaum ML, Berbaum KS, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures: a randomised trial. Lancet. 2000;355:1486–1490. doi: 10.1016/S0140-6736(00)02162-0. [DOI] [PubMed] [Google Scholar]
- Lang EV, Berbaum KS, Faintuch S, Hatsiopoulou O, Halsey N, Li X, et al. Adjunctive self-hypnotic relaxation for outpatient medical procedures: A prospective randomized trial with women undergoing large core breast biopsy. Pain. 2006;126:155–164. doi: 10.1016/j.pain.2006.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang EV, Speigel D, Lutgendorf S, Logan H. Empathic attention and self-hypnotic relaxation for interventional radiological procedures. Iowa City, IA: The University of Iowa; 1996. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann A. A continuing postoperative complication: nausea and vomiting--who is affected, why, and what are the contributing factors? A review. CRNA: The Clinical Forum of Nurse Anesthetists. 1998;9:19–29. [PubMed] [Google Scholar]
- Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: a meta-analytic review. Journal of Consulting and Clinical Psychology. 2000;68:438–450. [PubMed] [Google Scholar]
- Martinez-Urrutia A. Anxiety and pain in surgical patients. Journal of Consulting and Clinical Psychology. 1975;43:437–442. doi: 10.1037/h0076898. [DOI] [PubMed] [Google Scholar]
- McCarthy M, Jr., Chang CH, Pickard AS, Giobbie-Hurder A, Price DD, Jonasson O, et al. Visual analog scales for assessing surgical pain. Journal of the American College of Surgeons. 2005;201:245–252. doi: 10.1016/j.jamcollsurg.2005.03.034. [DOI] [PubMed] [Google Scholar]
- McDonald RP, Ho MH. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7:64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- Melzack R, Wall PD. The challenge of pain. New York: Basic Books; 1983. [Google Scholar]
- Milling LS, Reardon JM, Carosella GM. Mediation and moderation of psychological pain treatments: response expectancies and hypnotic suggestibility. Journal of Consulting and Clinical Psychology. 2006;74:253–262. doi: 10.1037/0022-006X.74.2.253. [DOI] [PubMed] [Google Scholar]
- Milling LS, Shores JS, Coursen EL, Menario DJ, Farris CD. Response expectancies, treatment credibility, and hypnotic suggestibility: mediator and moderator effects in hypnotic and cognitive-behavioral pain interventions. Annals of Behavioral Medicine. 2007;33:167–178. doi: 10.1007/BF02879898. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Bovbjerg DH. Pre-infusion expectations predict post-treatment nausea during repeated adjuvant chemotherapy infusions for breast cancer. British Journal of Health Psychology. 2000;5:105–119. [Google Scholar]
- Montgomery GH, Bovbjerg DH. Pre-surgery distress and specific response expectancies predict post-surgery outcomes in surgery patients confronting breast cancer. Health Psychology. 2004;23:381–387. doi: 10.1037/0278-6133.23.4.381. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Bovbjerg DH, Schnur JB, David D, Goldfarb A, Weltz CR, et al. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. Journal of the National Cancer Institute. 2007;99:1304–1312. doi: 10.1093/jnci/djm106. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, David D, Winkel G, Silverstein JH, Bovbjerg DH. The effectiveness of adjunctive hypnosis with surgical patients: A meta-analysis. Anesthesia and Analgesia. 2002a;94:1639–1645. doi: 10.1097/00000539-200206000-00052. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, DuHamel KN, Redd WH. A meta-analysis of hypnotically induced analgesia: how effective is hypnosis? International Journal of Clinical and Experimental Hypnosis. 2000;48:138–153. doi: 10.1080/00207140008410045. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Kirsch I. Classical conditioning and the placebo effect. Pain. 1997;72:107–113. doi: 10.1016/s0304-3959(97)00016-x. [DOI] [PubMed] [Google Scholar]
- Montgomery GH, Schnur J. Panel discussion on definition of hypnosis; Presentation at the Society of Clinical and Experimental Hypnosis Annual Meeting; Anaheim, CA. 2007. Oct, [Google Scholar]
- Montgomery GH, Weltz CR, Seltz G, Bovbjerg DH. Brief pre-surgery hypnosis reduces distress and pain in excisional breast biopsy patients. International Journal of Clinical and Experimental Hypnosis. 2002b;50:17–32. doi: 10.1080/00207140208410088. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user's guide. Fifth ed. Los Angeles, CA: Muthen & Muthen; 2007. [Google Scholar]
- Nelson FV, Zimmerman L, Barnason S. The relationship and influence of anxiety on postoperative pain in the coronary artery bypass graft patient. Journal of Pain and Symptom Management. 1998;15:102–109. [PubMed] [Google Scholar]
- Pavlin DJ, Chen C, Penaloza DA, Polissar NL, Buckley FP. Pain as a factor complicating recovery and discharge after ambulatory surgery. Anesthesia and Analgesia. 2002;95:627–634. doi: 10.1097/00000539-200209000-00025. [DOI] [PubMed] [Google Scholar]
- Pavlin DJ, Rapp SE, Polissar NL, Malmgren JA, Koerschgen M, Keyes H. Factors affecting discharge time in adult outpatients. Anesthesia and Analgesia. 1998;87:816–826. doi: 10.1097/00000539-199810000-00014. [DOI] [PubMed] [Google Scholar]
- Pick B, Pearce S, Legg C. Cognitive responses and the control of post-operative pain. British Journal of Clinical Psychology. 1990;29:400–415. doi: 10.1111/j.2044-8260.1990.tb00904.x. [DOI] [PubMed] [Google Scholar]
- Piper BF. Measuring fatigue. In: Stromborg M, Olson S, editors. Instruments for clinical research in health care. 2 ed. Philadelphia: W.B. Saunders; 1996. [Google Scholar]
- Price DD, Milling LS, Kirsch I, Duff A, Montgomery GH, Nicholls SS. An analysis of factors that contribute to the magnitude of placebo analgesia in an experimental paradigm. Pain. 1999;83:147–156. doi: 10.1016/s0304-3959(99)00081-0. [DOI] [PubMed] [Google Scholar]
- Quinn A, Brown J, Wallace P, Ashbury A. Studies in postoperative sequelae. Nausea and vomiting - still a problem. Anaesthesia. 1994;49:62–65. doi: 10.1111/j.1365-2044.1994.tb03316.x. [DOI] [PubMed] [Google Scholar]
- Rotter JB. The development and application of social learning theory. New York: Praeger; 1982. [Google Scholar]
- Rubin GJ, Cleare A, Hotopf M. Psychological factors in postoperative fatigue. Psychosomatic Medicine. 2004;66:959–964. doi: 10.1097/01.psy.0000143636.09159.f1. [DOI] [PubMed] [Google Scholar]
- Schnur JB, Bovbjerg DH, David D, Tatrow K, Goldfarb AB, Silverstein JH, et al. Hypnosis decreases presurgical distress in excisional breast biopsy patients. Anesthesia and Analgesia. 2008a;106:440–444. doi: 10.1213/ane.0b013e31815edb13. table. [DOI] [PubMed] [Google Scholar]
- Schnur JB, Hallquist MN, Bovbjerg DH, Silverstein JH, Stoiceska A, Montgomery GH. Predictors of expectancies for post-surgical pain and fatigue in breast cancer surgical patients. Personality and Individual Differences. 2007;42:419–429. doi: 10.1016/j.paid.2006.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnur JB, Kafer I, Marcus C, Montgomery GH. Hypnosis to manage distress related to medical procedures: A meta-analysis. Contemporary Hypnosis. 2008b;25:114–128. doi: 10.1002/ch.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoenberger NE, Kirsch I, Gearan P, Montgomery GH, Pastyrnak SL. Hypnotic enhancement of a cognitive behavioral treatment for public speaking anxiety. Behavior Therapy. 1997;28:127–140. [Google Scholar]
- Scott LE, Clum GA, Peoples JB. Preoperative predictors of postoperative pain. Pain. 1983;15:283–293. doi: 10.1016/0304-3959(83)90063-5. [DOI] [PubMed] [Google Scholar]
- Shimozuma K, Ganz PA, Petersen L, Hirji K. Quality of life in the first year after breast cancer surgery: rehabilitation needs and patterns of recovery. Breast Cancer Research and Treatment. 1999;56:45–57. doi: 10.1023/a:1006214830854. [DOI] [PubMed] [Google Scholar]
- Shor RE, Orne EC. The Harvard Group Scale of Hypnotic Susceptibility, Form A. Palo Alto, CA: Consulting Psychologists Press; 1962. [Google Scholar]
- Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- Sidebotham DA, Reddy M, Schug SA. Influence of postoperative pain therapy on nausea and vomiting. Schmerz. 1997;11:241–246. doi: 10.1007/s004820050092. [DOI] [PubMed] [Google Scholar]
- Spanos NP, Radtke HL, Hodgins DC, Stam HJ, Bertrand LD. The Carleton University responsiveness to suggestion scale: normative data and psychometric properties. Psychological Reports. 1983;53:523–535. doi: 10.2466/pr0.1983.53.2.523. [DOI] [PubMed] [Google Scholar]
- Tanabe P, Steinmann R, Anderson J, Johnson D, Metcalf S, Ring-Hurn E. Factors affecting pain scores during female urethral catheterization. Academic Emergency Medicine. 2004;11:699–702. [PubMed] [Google Scholar]
- Thomas T, Robinson C, Champion D, McKell M, Pell M. Prediction and assessment of the severity of post-operative pain and of satisfaction with management. Pain. 1998;75:177–185. doi: 10.1016/s0304-3959(97)00218-2. [DOI] [PubMed] [Google Scholar]
- Tomarken AJ, Waller NG. Potential problems with "well fitting" models. Journal of Abnormal Psychology. 2003;112:578–598. doi: 10.1037/0021-843X.112.4.578. [DOI] [PubMed] [Google Scholar]
- Watcha MF, White PF. Postoperative nausea and vomiting: its etiology, treatment, and prevention. Anesthesiology. 1992;77:162–184. doi: 10.1097/00000542-199207000-00023. [DOI] [PubMed] [Google Scholar]
- Weitzenhoffer AM, Hilgard ER. Stanford Hypnotic Susceptibility Scale - Form C. Palo Alto, CA: Consulting Psychologists Press, Inc; 1962. [Google Scholar]
- Wickless C, Kirsch I. Effects of verbal and experiential expectancy manipulations on hypnotic susceptibility. Journal of Personality and Social Psychology. 1989;57:762–768. [Google Scholar]
- Wolfe F. Fatigue assessments in rheumatoid arthritis: comparative performance of visual analog scales and longer fatigue questionnaires in 7760 patients. The Journal of Rheumatology. 2004;31:1896–1902. [PubMed] [Google Scholar]