Abstract
Objective
One in three children globally is stunted in growth. Many of the conditions that promote child stunting are amenable to quality care provided by skilled health workers.
Methods
The study uses household and facility data from the Indonesian Family Life Surveys in 1993 and 1997. The first set of multivariate regression models evaluate whether the number of medical doctors (MDs), nurses, and midwives predict quality of care as measured by adherence to clinical guidelines. The second set explains the relationships between quality and length among children less than 36 months. Using the information generated from these two sets of regressions, we simulate the effect of increasing the number of MDs, nurses, and midwives on child length and stunting.
Results
Increases in the number of MDs and nurses predict increases in the quality of care. Higher quality care is associated with child length in centimeters and stunting. Simulations suggest that large health gains among children under 24 months of age result by placing MDs where none are available.
Conclusions
Improvements in child health could be made by increasing the number of qualified health staff. The returns to investing in improvements in human resources for health are high.
Keywords: Health personnel, Medical staff, Quality of healthcare, Growth, Public policy, Public health
1. Introduction
One in three children globally is stunted in growth [1]. Stunting is associated with negative outcomes in later life, including high rates of morbidity and mortality, reduced cognitive function, and low economic productivity [2–6]. Most of these children live in low-income settings characterized by a high prevalence of communicable diseases and inadequate use of cost-effective interventions [1].
Global initiatives such as the United Nations Millennium Summit emphasize scaling-up basic health interventions in low-income settings to improve health and reduce poverty. However, these initiatives have not yet achieved sustainable gains in coverage or health outcomes in many poor countries. This is primarily because of long-standing weaknesses in health systems [7]. One of the most important health system challenges is ensuring the availability of qualified staffing to deliver primary care. It is estimated that a shortfall of 4 million health workers exists globally, and 70 countries have fewer than 2.5 health workers per 1000 people [8].
In this paper, we use data from Indonesia to evaluate whether medical doctors (MDs), nurses, and midwives predict quality of care, and whether quality is associated with child growth. We address several methodological issues. The first challenge is measuring quality itself. Structural quality, such as supplies or infrastructure, is typically used as a proxy for the quality of medical care. However, structural quality does not capture health worker performance. A growing body of research suggests that inadequate or inappropriate clinical practice is widespread [9] and contributes to poor health outcomes [10–12]. To more accurately capture the quality of healthcare, this study uses case scenarios that measure knowledge about clinical practice guidelines.
A second challenge is selective program placement. Governments typically allocate health resources based on explicit rules and policies. If health resources are targeted to areas of greatest health need, for example, a cross-sectional analysis could conclude that the services are associated with poor health outcomes [13]. To control for program placement, previous studies have modeled the resource allocation criteria [14,15] or used fixed effects that control for both observed and unobserved factors at a given level of observation [16]. This study uses community level fixed effects and a panel of communities, which eliminate from the model and error terms those characteristics that define the allocation of resources.
1.1. The Indonesian health scene
Public health workforce planning and deployment in Indonesia is based on staffing a broad network of public facilities [17]. Staffing ratios are applied by facility type for the main geographic regions: Java Bali (JB) and the more remote Outer Java Bali (OJB) [18]. To achieve the targeted MD per facility ratios, the Ministry of Health (MoH) relied on a system of compulsory service at health centers. Five years of public service was a prerequisite before obtaining a civil service post, a practice license, and medical specialty training. The service requirement was shortened to 3 years for work in remote regions of OJB. This combination of incentives proved successful in increasing the availability of MDs at health centers, even in remote regions. Most physicians, however, moved to urban areas for training or practice after their compulsory service. Thus, sustaining the appropriate levels of qualified staff at health centers has been an ongoing challenge [19].
During the early 1990s, Indonesia faced budget crises. Coping with public resource shortfalls, the Government of Indonesia enacted a zero-growth policy, which froze new hiring in the civil service in 1992. For the health sector, this policy eliminated the key incentive for deployment to remote regions – a shorter period of mandatory service before becoming a civil servant. The final civil service cohorts completed their mandatory service at health centers in 1994 and 1996 in remote and non-remote regions, respectively. Facing demands to staff a large network of primary level facilities, the MoH developed contracting programs that circumvented the hiring restrictions and directly allocated MDs to health centers, using financial incentives to work in remote regions rather than shorter periods of compulsory service [20]. Despite these efforts, less than one-half and one-third of MD targets were filled in health centers for very remote and remote regions, respectively [21]. Previous research has illustrated large declines in quality between 1993 and 1997, which correspond with changes in the number of qualified health staff [19]. We exploit this shock to the health system to explore the relationships among staffing, quality and child length.
2. Materials and methods
2.1. Rationale
Height is a cumulative measure of health reflecting the physiological processes associated with genetics, birth weight and environment [22]. Environmental factors including poor nutrition, infection, perinatal complications, and childhood illnesses could prevent the attainment of full growth potential [2–5].
There is good reason to believe that the quality of prenatal care affects child growth in low-income settings. In low-income settings, there tends to be a high prevalence of maternal conditions that promote low birth weight, including low energy intake, low pre-pregnancy body mass index, and hypertensive disorders of pregnancy [23,24]. Previous studies in Indonesia have attributed high rates of child stunting to poor prenatal health [25–27]. Persistent untreated illnesses during pregnancy can result in low-birth weight infants that are less likely to catch-up in growth [23,28–30].
Postnatal infections occur more frequently among children with poor prenatal growth [22,31]. Repeated infections can prevent a child from completely restoring weight lost during illnesses and result in a decline in the child’s growth trajectory over the long term [5]. Within the first 2 years in particular, growth rates are higher than in later life and the immune system is developing. Therefore, strengthening clinical case management of common childhood illnesses could also improve growth.
2.2. Behavioral and analytical framework
The production function characterizes health as a form of human capital, where current health status is a function of choices and shocks over the lifetime [32]. An individual’s health capital, such as height, is the result of a set of factors including medical care, personal behaviors, and environment – some of which are observed whereas others are not. The effect that each factor has on health varies by individual biology and socioeconomics, i.e., age, gender, genetic endowments, and education.
Some of the determinants are chosen, such as nutritional intake, medical care, and time spent in seeking care. Others, such as environmental health, are only partially determined by a household’s choices of sanitation, waste disposal, and water source. Yet, some inputs are fully exogenous to the household, such as the portion of the disease environment determined by public health and sanitation infrastructure.
Even though the health production function captures critical information, estimation of its parameters is difficult in practice, given that it would require detailed information about the choice of each input. Such an estimation would require an identifying instrument, such as a price, for each input included in the production function. Furthermore, these choices are simultaneously determined with the outcome, are thus endogenous and likely to be correlated with the error term.
In particular, the quality of care received is a choice variable. Individuals choose whether and where to obtain care based on factors such as the expected efficacy of treatment (quality), price of available providers, the type and severity of illness, and budget constraints. Individuals are not randomly assigned quality, and those that choose a high quality care provider might be more severely ill. Selection bias based on unobserved severity of illness may confound the estimated relationship between quality received and health outcomes.
Consequently, we estimate the reduced-form determinants of health that relate measures of health status to long-term constraints. The reduced-form is obtained by substituting the determinants of the chosen health behaviors into the production function. The reduced-form model does not distinguish the pathways through which quality of care affects health. It captures the combined direct and indirect benefits of quality care rather than solely their influences on behavioral choices.
2.3. Survey design and data sources
The primary data source is the Indonesian Family Life Survey (IFLS) in 1993 and 1997, which collected information from a panel of Indonesian households and communities. The sampling scheme stratified on 13 out of 27 provinces, and 321 enumeration areas were randomly selected from a nationally representative sampling frame. The response rate was 91% of 7730 households in 1993. The 1997 survey re-interviewed 88% of the 1993 households, plus split-off households (total of 7629 households). The 13 provinces comprised 83% of the Indonesian population in 1993. Details of the IFLS are documented elsewhere [33].
This study uses child length as the main dependent variable. Within each household, two children aged 0–14 years were randomly selected. A trained interviewer recorded recumbent length or standing height using Shorr portable measuring boards. Parental height, weight and age were also measured. Weight was taken using the Seca Model 770 scales. In addition to the anthropometric data, household survey modules collected data about basic demographic characteristics, education, and consumption. The short consumption module collected data about household purchases of food, personal and household items, durable goods, and education.
Both rounds of the IFLS used the same protocol for selecting and interviewing health providers. Similar to other low-income settings, no complete list of public and private ambulatory care providers exists from which to draw a sample. Therefore, the sampling frame was generated from information collected in the household survey about knowledge of health providers in the community. The selection among eligible providers was based on a random probability sample with the probability of selection proportionate to the frequency a given location was mentioned by households. Recognizing that the health market is dynamic, the survey is a panel of communities rather than facilities, and the data represent the quality available to the same communities at two points in time. The response rate exceeded 99% in both years; this was probably attributable to the relatively small number of facilities per community, and up to three return visits to complete the interview.
The facility survey measured quality by using clinical case scenarios. These scenarios were administered as interviews with health providers, who responded to a series of questions about history-taking, physical, diagnostics, and treatment or case management for prenatal and child care [34]. The facility survey also detailed information about the most qualified staff working at public facilities, namely MDs, nurses, and midwives. Data about district gross domestic product (GDP) is taken from the Central Statistical Bureau, which was deflated across regions and expressed in 1993 Indonesian rupiah values.
2.4. Analysis plan
The analyses are divided into three parts. The first set of analyses examines the relationships between health staffing and quality of care. The second set analyzes the relationships between quality of care and child health outcomes. Third, the coefficients generated in the first and second sets of regressions are used to simulate the impact of changes in staffing on changes in health outcomes.
In the first set of analyses, we explain variations in quality by the numbers and types of health staff using multivariate linear regression models. The dependent variable is the quality score, which was generated from interviews with health care providers about adherence to clinical protocols. The responses were coded against evidence-based guidelines [35,36], summed up, and expressed as the percent of the total for prenatal and child care. The scores are standardized with a mean of zero and a standard deviation of one.
The key explanatory variables are the numbers of MDs, nurses, and midwives. The number of MDs is expressed categorically as 0, 1, and 2 or more. For nurses and midwives, the categories are 0, 1, 2, and 3 or more. None is the omitted category in the regressions. To measure whether nurses and midwives are substitutes for MDs, two interaction terms are generated. The dummy variable for “no MD” is interacted with the natural log of the number of nurses and the number of midwives, and the results are expressed as change in quality with one additional nurse or midwife from the 1993 baseline where no MD is available.
To address program placement, we exploit knowledge about how the Indonesian Government allocates health personnel. Throughout the 1990s, the government allocated health staff based on fixed facility and population criteria by geographic region and inpatient beds [18]. Therefore, the models include community fixed effects, which eliminate from the model and error terms fixed characteristics that define the allocation of resources in addition to other stable regional characteristics [37]. If health workers consistently migrate to urban areas or the national capital, fixed effects also control for this type of migration bias. In addition, the regressions include the availability of inpatient beds, electricity, and microscope, the type of facility, and a dummy variable for the second survey wave to control for changes in Indonesia that affected all communities.
Most communities in this dataset fall within defined areas; therefore, community fixed effects control for changes that took place within administrative regions. The definition of a community, however, purported to define a health-seeking catchment area regardless of administrative boundaries. To take into consideration changes in the definition of communities over time and communities that crossed administrative boundaries, we present an additional model with variables representing factors that could affect health worker sorting. These variables include district GDP, monthly household expenditures, community infrastructure, and maternal age and education for women who experienced a pregnancy between 1990 and 1997.
The second set of analyses examines the relationships between quality and child length. The dependent variable is length, expressed in centimeters and as standard deviation units, or z-scores. z-Scores are derived by subtracting each child’s length from the National Center for Health Statistics (NCHS) median reference standard and dividing by the standard deviation of the reference distribution for a given age and sex (ANTHRO software for calculating pediatric anthropometry, version 1.02, 1999, Centers for Disease Control and WHO). The Indonesian government employs the same software to prepare its anthropometry estimates nationally. Moderate and severe stunting is defined as less than 2 and 3 standard deviations below the reference median. The analyses use cohorts of children less than 36 months of age, given that they are sensitive to the availability of health resources.
The key explanatory variable is the quality score. The facility scores are matched with households using information about their choice of public or private clinical setting in the community. Where more than one public or private provider is available in a given community, we generated a mean score by clinical setting to match with the household. For those households that did not report about clinical setting (17%), weights were generated from community fixed effects regressions using as the dependent variable the choice of public care controlling for household expenditure quartiles, maternal educational levels, 3-month age groups, and a 1997 year dummy variable. From these regressions, we predicted the share of public utilization.
Control variables in the length regressions were based on the socioeconomic determinants of linear growth in developing countries, including household socioeconomic status, parental, and community characteristics [22,38]. They include household wealth as measured by monthly food and non-food expenditures, maternal education, maternal height, maternal weight in kilograms, and paternal height in centimeters. A set of 3-month age–sex dummy variables are included to control for age and sex determinants of length in centimeters and errors in the reference standard for z-scores. A dummy variable for the second survey round is also included to control for factors that affected all communities. Regressions are estimated with fixed effects at community level, which allow us to exploit the community panel to control for any remaining differences in observed and unobserved fixed characteristics of individuals, households, and localities that do not change between 1993 and 1997. All analyses were adjusted for the cluster survey design.
Lastly, we multiply the regression coefficients from the first and second sets of analyses to estimate the impact of increases in health staffing (MDs, nurses, and midwives) on child length and stunting. The simulations aim to predict the relationships between increases in qualified staffing on child length via improvements in the quality of care.
3. Results
Table 1 describes facility characteristics by region and year. Significant declines occurred in the quality of prenatal and child care between 1993 and 1997, and these declines were greater in remote areas (OJB, panel A). In example, prenatal care quality scores declined by 12% in JB and 24% in OJB. Using standardized scores, prenatal care quality declined by 0.34 standard deviation (SD) units for facilities in JB, and 0.65 SD in OJB. Panel B describes human resources. In health centers, increases occurred in the number of MDs in JB, while declines occurred in the number of nurses and midwives. In remote OJB, declines occurred in MDs, while increases occurred in the number of midwives. The last panel indicates that facility structural quality and community infrastructure were stable or improved during the same period.
Table 1.
Public health facility and socioeconomic characteristics by region, Indonesia, 1993 and 1997.
| Characteristics | Java Bali |
Outer Java Bali |
||
|---|---|---|---|---|
| 1993 | 1997 | 1993 | 1997 | |
| Panel A. Facility quality | ||||
| Prenatal care | ||||
| Quality scores (raw 1–100) | 54.97 | 48.65*** | 49.30 | 37.29*** |
| Standardized scores (SD) | 0.34 | 0.00*** | 0.03 | −0.62*** |
| % of facilities that offer care | 94.9 | 95.3 | 89.1 | 91.9 |
| Child curative care | ||||
| Quality scores (raw 1–100) | 65.96 | 61.24*** | 64.70 | 52.82*** |
| Standardized scores (SD) | 0.17 | −0.06*** | 0.11 | −0.49*** |
| % of facilities that offer care | 98.0 | 98.6 | 97.3 | 97.0 |
| Panel B. Facility staffing | ||||
| Health centers | ||||
| No MD available (%) | 3.35 | 2.96 | 8.22 | 11.77 |
| Number of MDs | 1.39 | 1.54*** | 1.24 | 1.06*** |
| Number of nurses | 4.75 | 4.42** | 5.51 | 5.84 |
| Number of midwives | 3.30 | 2.79*** | 2.72 | 3.21*** |
| Auxiliary health centers | ||||
| Number of nurses | 1.03 | 0.95 | 1.10 | 1.15 |
| Number of midwives | 0.76 | 0.63** | 0.60 | 0.60 |
| Total number of public facilities | 612 | 606 | 380 | 309 |
| Panel C. Facility structural quality and socioeconomics | ||||
| Electricity available (%) | 84.01 | 93.71*** | 66.48 | 87.48*** |
| Microscope available (%) | 50.96 | 50.94 | 38.13 | 50.22*** |
| Community infrastructure index | 36.72 | 41.99*** | 25.92 | 32.94*** |
Notes: Outer Java Bali is the more remote region defined as provinces in Sumatra, Kalimantan, and the Eastern Islands. The community infrastructure index is measured as the proportion of communities with a formal market, public telephone, post office, predominantly piped drinking water, sewage waste disposal system, and garbage disposal system. Frequencies adjusted for sampling design.
p ≤ 0.05.
p ≤ 0.01.
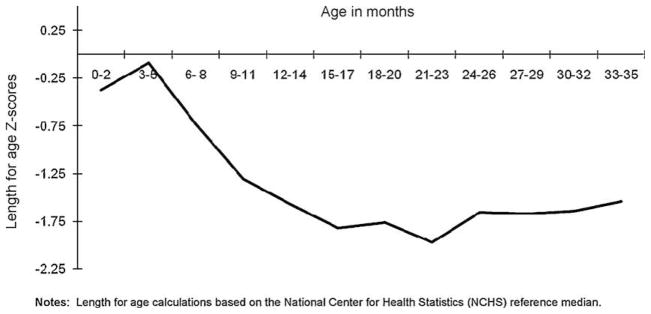
Approximately 35% of children aged <36 months in the sample were stunted in growth (<2 SD below the reference median). At birth to 3 months, length for age in the sample is close to the NCHS reference population; thereafter, growth faltering occurs so that, after 18 months, length for age remains 1.5 standard deviations below the reference median (Fig. 1). This pattern is consistent with other less developed settings [39].
Fig. 1.
Length for age z-scores by 3-month age groups, 0–36 months, 1993 and 1997.
The number and qualifications of health staff are important predictors of the combined prenatal and child care quality scores (Table 2). The inclusion of additional socioeconomic control variables in Model 2 results in slightly more conservative estimates, and the 1997 year dummy is no longer significant. The largest quality gains can be made by increasing the number of MDs. Based on the results from the second model, increasing the number of MDs from none to one and to two more predicts an increase in quality of 0.56 SD and 0.63 SD, respectively. Increasing the number of nurses from none to three or more also has a significant quality impact (0.37 SD). Increasing the number of midwives does not predict variations in quality. The interaction term suggests that midwives are substitutes for MDs. Applying the percentage change to the baseline, one additional midwife in the absence of a MD predicts a 0.18 SD increase in quality.
Table 2.
Fixed effects models explaining the contribution of health staffing to variations in the quality of care, public facilities.
| Explanatory variables | Prenatal and child care quality, standard deviation units |
|
|---|---|---|
| 1 | 2 | |
| Human resources at facility | ||
| Medical doctors (MDs) | ||
| One | 0.593*** [0.204] | 0.561*** [0.203] |
| Two or more | 0.673*** [0.218] | 0.631*** [0.218] |
| Nurses | ||
| One | 0.069 [0.137] | 0.086 [0.136] |
| Two | 0.194 [0.182] | 0.201 [0.182] |
| Three or more | 0.369** [0.185] | 0.368** [0.185] |
| No MD ×Ln number of nurses | −0.009 [0.156] | −0.029 [0.155] |
| Midwives | ||
| One | 0.122 [0.148] | 0.112 [0.148] |
| Two | 0.131 [0.173] | 0.119 [0.172] |
| Three or more | 0.085 [0.174] | 0.082 [0.173] |
| No MD ×Ln number of midwives | 0.393** [0.197] | 0.398** [0.196] |
| 1997 (=1) | −0.399** [0.042] | −0.153 [0.130] |
| Socioeconomic controls | No | Yes |
Notes: Coefficients and standard errors reported, n = 1907. The omitted category is “0” for all three categories of human resources. In addition to the variables shown, all models include facility factors: inpatient beds, electricity, microscope, facility type. Model 2 includes socioeconomic controls (district GDP, household expenditures, maternal age and education).
p ≤ 0.05
p ≤ 0.01.
Quality predicts significant increases in child length (Table 3, Models 2 and 3). A one standard deviation increase in quality predicts a nearly a half centimeter increase in length among children less than 24 months and 36 months (0.48 and 0.44 cm, respectively). Quality also predicts a 5.7–4.9 percentage point decline in stunting among children less than 18 and 24 months (Models 4 and 5). At the 10% significance level, quality is associated with length for the youngest age group (<18 months) as well as reductions in stunting for children <36 months.
Table 3.
Explaining the contribution of health care quality to child length and stunting, 0–36 months.
| Explanatory variables | Length in centimeters |
Moderate and severe stunting |
||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| <18 months | <24 months | <36 months | <18 months | <24 months | <36 months | |
| Prenatal and child care quality (SD units) | 0.444 [0.256] p = 0.08 |
0.475 [0.231] p = 0.04 |
0.442 [0.189] p = 0.02 |
−0.057 [0.027] p = 0.04 |
−0.049 [0.024] p = 0.04 |
−0.032 [0.019] p = 0.10 |
| Year (1997 = 1) | 0.582 [0.274] p = 0.03 |
0.272 [0.242] p = 0.26 |
0.372 [0.198] p = 0.06 |
0.012 [0.029] p = 0.69 |
0.032 [0.025] p = 0.20 |
0.018 [0.020] p = 0.37 |
| Household, socioeconomic characteristics | Yes | Yes | Yes | Yes | Yes | Yes |
| Maternal and infant characteristics | Yes | Yes | Yes | Yes | Yes | Yes |
| 3-month age/sex dummy variables | Yes | Yes | Yes | Yes | Yes | Yes |
| Constant | −44.601 [33.987] p = 0.19 |
−61.051 [31.013] p = 0.05 |
−102.063 [24.519] p < 0.01 |
12.313 [3.581] p < 0.01 |
13.979 [3.223] p < 0.01 |
15.623 [2.480] p < 0.01 |
| # Observations | 1246 | 1664 | 2563 | 1246 | 1664 | 2563 |
Notes: Coefficients and standard errors reported. Quality score based on the percent of 31 criteria mentioned in the case scenarios measuring the quality of prenatal and child curative care. The index is standardized and expressed as standard deviation units from the mean. All models include household and socioeconomic controls, maternal characteristics, 3-month age/sex dummy variables, community fixed effects, and a dummy variable for 1997. Moderate and severe stunting defined as length for age z-scores less than 2 standard deviations (SD) below the National Center for Health Statistics (NCHS) reference median.
Using the results from the first two sets of regressions, the simulations suggest that the largest gains in length can be made by increasing the number of MDs (Table 4, columns 1–3). Column 2 illustrates the results for length in centimeters among children <24 months. This simulation suggests that increasing the number of MDs from none to one would result in an increase in length of 0.27 cm through increases in the quality of prenatal and child care quality. Among children of the same age group, increasing the number of MDs to two or more is associated with a 0.30-cm increase in length. Improvements in length could also be made by increasing the number of nurses to three or more (0.18 cm), and increasing the number of midwives where no MD is available (0.09 cm).
Table 4.
Simulations predicting the impact of increased health staffing levels on child length and stunting.
| Human resources | Change in length (cm) |
Change in stunting (percentage points) |
||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | |
| <18 months* | <24 months** | <36 months* | <18 months** | <24 months** | <36 months* | |
| Medical doctors (MD)s | ||||||
| One*** | 0.249 | 0.266 | 0.248 | −3.19 | −2.73 | −1.79 |
| Two or more*** | 0.280 | 0.299 | 0.279 | −3.59 | −3.08 | −2.02 |
| Nurses | ||||||
| One | 0.038 | 0.041 | 0.038 | −0.49 | −0.42 | −0.27 |
| Two | 0.089 | 0.095 | 0.089 | −1.14 | −0.98 | −0.64 |
| Three or more** | 0.163 | 0.175 | 0.163 | −2.09 | −1.79 | −1.18 |
| Midwives | ||||||
| One | 0.050 | 0.053 | 0.049 | −0.64 | −0.54 | −0.36 |
| Two | 0.053 | 0.056 | 0.052 | −0.67 | −0.58 | −0.38 |
| Three or more | 0.037 | 0.039 | 0.036 | −0.47 | −0.40 | −0.26 |
| Where no MD is posted | ||||||
| +1 nurse | −0.006 | −0.006 | −0.006 | 0.08 | 0.07 | 0.04 |
| +1 midwife** | 0.081 | 0.087 | 0.081 | −1.04 | −1.04 | −0.59 |
For the outcome of stunting, the largest gains could be made among children <18 months by increasing the number of MDs (column 4). Adding one MD where none are available is associated with a 3.2 percentage point decline in stunting; increasing the number to two or more is associated with a 3.6 percentage point decline. For children less than 24 months, similar declines in stunting could be seen for one additional MD and two or more (2.7 and 3.1 percentage points, respectively). Declines in stunting among children less than 24 months of age could also be made by increasing the number of nurses to three or more (1.8 percentage points), and adding one midwife where no MD is available (1.0 percentage point).
4. Discussion
This paper exploits the external change imposed by the central government’s zero growth policy to capture the relationships among health staffing, quality, and child length among children living in the same communities in 1993 and 1997. We do not aim to estimate the precise effect of the zero growth policy on quality and health outcomes; nor are data available to fully explain the determinants of child growth. To control for the non-random allocation of health resources, we use knowledge about how the government allocates health resources. The community fixed effects control for factors that were the same to communities, such as the sanitation environment, and fixed characteristics that determine the deployment and retention of health resources. Prior research with these data showed that health outcomes are not associated with staff availability or quantity [19]. We focus on the quality of basic services with high utilization levels; prenatal care coverage, for example, was 92% among women reporting about their most recent singleton live birth between 1992 and 1998 [34].
There is little agreement in the literature and across different disciplines about the measurement of quality and its analytical methods. To measure quality, we use case scenarios that measure knowledge and clinical decision-making, and control for patient case mix. We are unaware of studies that validate case scenarios with standardized patients (the gold standard for measuring practice variation) in low-income settings. In more developed settings, it is inconclusive as to whether case scenarios predict behavior [40]. Health care providers knew that they were being studied, which may have provided an incentive to perform well. The scenarios do not comprehensively evaluate all criteria set forth in international standards. However, they were developed by Indonesian physicians who identified aspects of basic care that they considered important in this setting.
National trends in health staffing in Indonesia are described. However, the data used in this study do not include very remote areas. Personnel data were collected from interviews at health facilities; information about working hours or absenteeism is unavailable. Government estimates of the decline in health staffing as a result of the zero growth policy are higher compared with the results reported here. These factors suggest that our results may be conservative. We studied three categories of health workers (MDs, nurses, and midwives); future analyses could examine the contribution of paraprofessionals.
The results about health staffing are limited to public clinics, and it is possible that declines in public quality could have been offset by increases in private quality. To evaluate this empirically, we estimated a series of regressions predicting private quality as a function of public quality. We find that public quality explains a large proportion of the variation in private sector quality, consistent with our knowledge that public health care providers practicing off-hours were the primary source of private ambulatory care. This suggests that the private sector did not fill in the gap created by the decline in public quality.
This study demonstrates positive associations between the numbers and qualifications of health workers and the quality of care. MDs in particular appear to provide important capacity as measured by significantly increased quality; as a result, the simulations suggest that the largest gains in child length could be made by increasing the number of MDs. However, posting MDs to health centers has been difficult to implement in practice. The current incentive packages have been insufficient to attract MDs to fill in the health center staffing gaps, particularly in the most remote regions of Indonesia.
The importance of a MD probably reflects a higher level of professionalism for physician training compared with nurses and midwives. MDs provide care directly as well as supervise and manage activities; the presence of a MD, therefore, could imply a stronger supervisory role. This could explain why midwives, for example, are not significant predictors of prenatal and child care quality, even though they are an important source of prenatal care. We find that increasing the number of midwives in the absence of a MD predicts increases in quality. This is an important finding in this setting because midwives appear to have replaced MDs in rural OJB. Taking a long-term approach, supporting professional development among nurses and midwives are a promising means to improve quality, particularly in remote areas.
5. Conclusions
This paper aims to contribute to a growing body of evidence about health workers and quality of care in low-income settings. Similar to other countries, deployment of health staff in Indonesia is based on quantitative facility targets that are not related to quality improvements or health outcomes. The results suggest that increases in the number of MDs and nurses predict higher quality care, and that higher quality predicts improved child health. Our simulations suggest that the largest health gains for young children could be made by increasing the number of MDs where none are available. The findings here could be relevant for countries that are examining health worker deployment and qualifications to achieve high quality care and better health outcomes. These results suggest that the returns to investing in human resources for health are high.
Acknowledgments
We are grateful to many people who provided comments on this and earlier versions of the paper, including Pandu Harimurti, David Levine, Menno Pradhan, Gunawan Setiadi, Mark Wheeler, in addition to participants of seminars at the University of California, Berkeley, and the World Bank. Sri Hartini and Abdillah Ahsan assisted with government administrative data. The authors are responsible for all errors and omissions. The research was funded by the National Institutes of Health Fogarty International Center and the National Institute of Child Health and Human Development. The opinions expressed herein do not represent the views of the funding organizations. The authors declare that they have no competing interests.
Contributor Information
Sarah L. Barber, Email: barber@haas.berkeley.edu, barbers@wpro.who.int.
Paul J. Gertler, Email: gertler@haas.berkeley.edu.
References
- 1.de Onis M, Frongillo EA, Blössner M. Is malnutrition declining? An analysis of changes in levels of child malnutrition since 1980. Bulletin of the World Health Organization. 2000;78:1222–33. [PMC free article] [PubMed] [Google Scholar]
- 2.Berkman DS, Lescano AG, Gilman RH, Lopez SL, Black MM. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow-up study. Lancet. 2002;359(9306):564–71. doi: 10.1016/S0140-6736(02)07744-9. [DOI] [PubMed] [Google Scholar]
- 3.Martorell R. The nature of child malnutrition and its long-term implications. Food and Nutrition Bulletin. 1999;20(3):288–92. [Google Scholar]
- 4.Mendez MA, Adair LS. Severity and timing of stunting in the first two years of life affect performance on cognitive tests in late childhood. Journal of Nutrition. 1999;129:1555–62. doi: 10.1093/jn/129.8.1555. [DOI] [PubMed] [Google Scholar]
- 5.Pelletier DL. The relationship between child anthropometry and mortality in developing countries: implications for policy, program, and future research. Journal of Nutrition. 1994;124(10 Suppl):2047S–81S. doi: 10.1093/jn/124.suppl_10.2047S. [DOI] [PubMed] [Google Scholar]
- 6.Spurr GB, Barac-Nieto M, Maksud MG. Productivity and maximal oxygen consumption in sugarcane cutters. American Journal of Clinical Nutrition. 1997;30(3):316–21. doi: 10.1093/ajcn/30.3.316. [DOI] [PubMed] [Google Scholar]
- 7.Bryce J, el Arifeen S, Pariyo G, Lanata C, Gwatkin D, Habicht JP. Multi-Country Evaluation of IMCI Study Group: reducing child mortality: can public health deliver? Lancet. 2003;362(9378):159–64. doi: 10.1016/s0140-6736(03)13870-6. [DOI] [PubMed] [Google Scholar]
- 8.Joint Learning Initiative. Human Resources for Health Overcoming the Crisis. Boston: Harvard College; 2004. [Google Scholar]
- 9.Das J, Gertler PJ. Variations in practice quality in five low-income countries: a conceptual overview. Health Affairs (Milwood) 2007;26(3):w296–309. doi: 10.1377/hlthaff.26.3.w296. [DOI] [PubMed] [Google Scholar]
- 10.Molyneux E, Ahmad S, Robertson A. Improved triage and emergency care for children reduces inpatient mortality in a resource-constrained setting. Bulletin of the World Health Organization. 2006;84(4):314–9. doi: 10.2471/blt.04.019505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barros F, Victora C, Barros A, Santos I, Albernaz E, Matijasevich A, Domingues M, Sclowitz I, Hallal P, Silveira M. The challenge of reducing neonatal mortality in middle-income countries: findings from three Brazilian birth cohorts in 1982, 1993, and 2004. Lancet. 2005;365:847–54. doi: 10.1016/S0140-6736(05)71042-4. [DOI] [PubMed] [Google Scholar]
- 12.Ashworth A, Chopra M, McCoy D, Sanders D, Jackson D, Karaolis N, Sogaula N, Schofield C. WHO guidelines for management of severe malnutrition in rural South African hospitals: effect on case fatality and the influence of operational factors. Lancet. 2004;363:1110–5. doi: 10.1016/S0140-6736(04)15894-7. [DOI] [PubMed] [Google Scholar]
- 13.Rosenzweig M, Wolpin M. Evaluating the effects of optimally distributed public programs: child health and family planning interventions. American Economic Review. 1986;76(3):470–82. [Google Scholar]
- 14.Angeles G, Guilkey DK, Mroz TA. Purposive program placement and the estimation of family planning programs effects in Tanzania. Journal of the American Statistical Association. 1998;9(443):884–99. [Google Scholar]
- 15.Molyneaux J, Gertler PJ. The impact of targeted family planning programs in Indonesia. Population and Development Review. 2001;26(Suppl 1):61–85. [Google Scholar]
- 16.Pitt MM, Rosenzweig MR, Gibbons D. The determinants and consequences of the placement of government programs in Indonesia. World Bank Economic Review. 1993;7(3):319–48. [Google Scholar]
- 17.World Bank. Indonesia’s Health Work force: Issues and Options No. 12835-IND. Washington, DC: 1994. [Google Scholar]
- 18.Ministry of Health, Republic of Indonesia. Health Center Manual. Jakarta: 19971998 19911992 19891990. [Google Scholar]
- 19.Barber SL, Gertler PJ, Harimurti P. The contribution of human resources to the quality of care in Indonesia. Health Affairs (Millwood) 2007;26(2):w367–79. doi: 10.1377/hlthaff.26.3.w367. [DOI] [PubMed] [Google Scholar]
- 20.Chomitz K, Sediati G, Azrul A, Ismail N, Widarti . Developing Incentives for Doctors to Serve in Remote and Rural Areas. World Bank Policy Research Paper; Washington DC: 1998. What do doctors want? [Google Scholar]
- 21.Ministry of Health, Republic of Indonesia. Indonesian Health Profile. Jakarta: 2001. [Google Scholar]
- 22.Martorell R, Habicht JP. Growth in early childhood in developing countries. In: Falkner F, Tanner JM, editors. Human growth: a comprehensive treatise, volume 3. Methodology and ecological, genetic and nutritional effects on growth. 2. New York: Plenum Press; 1986. [Google Scholar]
- 23.Kramer MS. Intrauterine growth and gestational duration determinants. Pediatrics. 1987;80(4):502–11. [PubMed] [Google Scholar]
- 24.Neufeld LM, Haas JD, Grajeda R, Martorell R. Changes in maternal weight from the first to second trimester of pregnancy are associated with fetal growth and infant length at birth. American Journal of Clinical Nutrition. 2004;79(4):646–52. doi: 10.1093/ajcn/79.4.646. [DOI] [PubMed] [Google Scholar]
- 25.De Pee S, Bloem MW, Sari M, Kiess L, Yip R, Kosen S. The high prevalence of low hemoglobin concentration among Indonesian infants aged 3–5 months is related to maternal anemia. Journal of Nutrition. 2002;132:2215–21. doi: 10.1093/jn/132.8.2215. [DOI] [PubMed] [Google Scholar]
- 26.Schmidt MK, Muslimantun S, West CE, Schultink W, Gross R, Hautvast JG. Nutritional status and linear growth of Indonesian infants in West Java are determined more by prenatal environment than postnatal factors. Journal of Nutrition. 2002;132:2202–7. doi: 10.1093/jn/132.8.2202. [DOI] [PubMed] [Google Scholar]
- 27.Sekiyama M, Ohtsuka RJ. Significant effects of birth-related biological factors on pre-adolescent nutritional status among rural Sundanese in West Java, Indonesia. Journal of Biosocial Science. 2005;37:413–26. doi: 10.1017/s0021932004006819. [DOI] [PubMed] [Google Scholar]
- 28.Villar J, Belizan JM. The timing factor in the pathophysiology of the intrauterine growth retardation syndrome. Obstetrics Gynecological Survey. 1982;32(8):499–506. doi: 10.1097/00006254-198208000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Barros FC, Huttly S, Victora C, Kirkwood B, Vaughan J. Comparison of the causes and consequences of prematurity and intrauterine growth retardation: a longitudinal study in southern Brazil. Pediatrics. 1992;90(2 Pt 1):238–44. [PubMed] [Google Scholar]
- 30.Bergström S. Infection-related morbidities in the mother, fetus, and neonate. Journal of Nutrition. 2003;133:1656S–60S. doi: 10.1093/jn/133.5.1656S. [DOI] [PubMed] [Google Scholar]
- 31.Stephensen C. Burden of infection on growth failure. Journal of Nutrition. 1999;129(Suppl):534S–8S. doi: 10.1093/jn/129.2.534S. [DOI] [PubMed] [Google Scholar]
- 32.Grossman M. On the concept of health capital and demand for health. Journal of Political Economy. 1972;80:223–55. [Google Scholar]
- 33.Frankenberg E, Thomas D. The Indonesia Family Life Survey: Study Design and Results from Waves 1 and 2. DRU-2238/1-NIA/NICHD. RAND; Santa Monica CA: 2000. [Google Scholar]
- 34.Barber SL, Gertler PJ, Harimurti P. Differences in access to high-quality outpatient care in Indonesia. Health Affairs (Millwood) 2007;26(3):w352–66. doi: 10.1377/hlthaff.26.3.w352. [DOI] [PubMed] [Google Scholar]
- 35.World Health Organization. Recommended interventions for improving maternal and newborn health. WHO/MPS/07.05. Geneva: 2007. [Google Scholar]
- 36.World Health Organization. Technical Basis for adapting clinical guidelines, feeding recommendations, and local terms. Geneva: 2002. Integrated Management of Childhood Illness: IMCI Adaption Guide Version 5, Section C. [Google Scholar]
- 37.Deaton A. The analysis of household surveys: microeconometric analysis for development policy. Baltimore, MD: Johns Hopkins University Press for the World Bank; 1997. [Google Scholar]
- 38.Frongillo EA, de Onis M, Hanson K. Socioeconomic and demographic factors are associated with worldwide patterns of stunting and wasting. Journal of Nutrition. 1997;127:2302–9. doi: 10.1093/jn/127.12.2302. [DOI] [PubMed] [Google Scholar]
- 39.Shrimpton R, Victora CG, de Onis M, Lima RC, Blossner M, Clugston G. Worldwide timing of growth faltering: implications for nutritional interventions. Pediatrics. 2001;107(5):E75. doi: 10.1542/peds.107.5.e75. [DOI] [PubMed] [Google Scholar]
- 40.Jones TV, Gerrity MS, Earp J. Written case simulations: do they predict physicians’ behavior? Journal of Clinical Epidemiology. 1990;43:805–15. doi: 10.1016/0895-4356(90)90241-g. [DOI] [PubMed] [Google Scholar]