Abstract
Background
The risk for skin cancer is increased among older males and outdoor workers who have high levels of ultraviolet (UV) exposure.
Purpose
This study was designed to examine the long-term efficacy of UV photography interventions on male outdoor workers, the potential mediators of its impact, and the efficacy of UV photography and skin cancer vs. aging information with this population.
Methods
One hundred forty-eight male outdoor workers were randomly assigned to one of four intervention conditions or a control condition in a two by two plus one factorial design. The men in the intervention conditions received or did not receive a UV photo of their face and watched either a photoaging or skin cancer educational video. Participants completed pre-intervention, immediate post-intervention, and 2-month and 1-year follow-up assessments.
Results
Analysis of covariance and structural equation modeling revealed that participants in the UV photography and cancer information interventions reported higher levels of sun protection cognitions, which were significant partial mediators of increases in sun protection behaviors and decreases in skin color.
Conclusions
This study provides evidence for effective sun protection interventions on male outdoor workers that may help reduce skin cancer risk.
Keywords: Sun protection, Intervention, Skin cancer, UV photos, Outdoor workers, Prevention
Introduction
An estimated 1.3 million new cases of skin cancer are diagnosed annually in the United States, and 90% of them are due to sun exposure [1]. Exposure to ultraviolet (UV) rays has been implicated in the high levels of basal and squamous cell skin cancer, especially among people (primarily men) with jobs that involve intense sun exposure [2–4]. In addition, skin cancer rates are much higher among men than women and excessive UV exposure is a risk factor [1]. Although skin cancer is one of the most common cancers, it is also one of the most preventable. Daily protection from the sun can reduce lifetime UV exposure by more than 50% [5]. Protective behaviors, such as using sunscreen, wearing protective clothing, and avoiding midday sun reduce the risk of skin cancer and skin damage due to UV rays [1, 6, 7]. Long-term sunscreen intervention trials have shown that sunscreen use is associated with a lower risk of basal and squamous cell tumors, precancerous skin lesions, and solar keratoses (a strong determinant of skin cancer risk) [6, 8–10].
Outdoor workers are exposed to approximately six to eight times more UV radiation than indoor workers [11] and are more likely to be diagnosed with skin cancers [2, 12–15]. Previous research has shown that outdoor workers tend to spend many years in outdoor jobs [16]. In addition, many of the outdoor workers in the U.S. have fair skin [17–19], which is associated with an increased risk for skin cancer (e.g., [1, 2]). Nonetheless, they typically do little to protect themselves from the sun during work or leisure [17–19]. This may be partly due to the fact that the majority of outdoor workers are men who engage in lower levels of protection than do women [18, 20, 21]. For these reasons, interventions for this population—male outdoor workers—could provide substantial benefits. However, the majority of UV intervention studies have been directed at people who choose to tan (e.g., at the beach, tanning booths) and are based on the assumption that appearance is the major motivation for UV exposure. This assumption is questionable for people whose jobs require them to be outdoors.
Intervention Research for Outdoor Workers
Although avoidance of UV exposure is ideal, that is not feasible for most outdoor workers; thus, increasing sun protection is the best strategy for this group. A small number of studies have reported interventions designed to increase sun protection among outdoor workers and a few have had some success. For example, Girgis, Sanson-Fisher, and Watson [22] assigned mostly male outdoor electrical workers to a dermatological skin screening and a 30-min educational session on skin cancer and sun protection. They found increased sun protection behaviors (sunscreen and clothing) 1 month post-intervention, but they did not examine longer-term efficacy of the intervention and they did not find significant effects on attitudes. Azizi and colleagues [23] and Borland and colleagues [24] were successful in increasing longer-term sun protection among male outdoor workers via educational interventions, including skin exams, and information videos and brochures addressing the dangers of sun exposure and how to protect oneself. However, cognitions were not assessed. Using a multicomponent intervention at swimming pools, Geller et al. [25] did not find a difference in sun protection behaviors and attitudes between the control and intervention groups, but the young adult aquatic staff working at the intervention pools reported fewer sunburns 6–8 weeks later. Similarly, Buller et al. [26] found a reduction in sunburns among employees of a ski resort receiving a multicomponent intervention. Finally, using a multicomponent intervention, including increasing access to sunscreen and hats and educational messages on sun safety and skin cancer with male and female US postal carriers, Mayer et al. [27] increased sunscreen- and hat-wearing behaviors and decreased skin darkness (measured with a spectrophotometer) 3 months, 1 year, and 2 years later. However, measures of cognitions were not assessed in this study.
This research appears to be promising. However, none of the current studies has examined the long-term effectiveness of different intervention components on cognitions, behavior, and skin color changes. Most of these studies and a number of other programs (many with mixed or null results) aimed at increasing sun protection among high-risk outdoor workers have limitations, including having limited comparison or no control groups, limited examination of cognitions, or not examining long-term effectiveness [17, 28, 29]. In addition, most of the current programs have not focused on high-risk samples of fair-skinned males who have worked outdoors year-round for many years. Some of the more effective interventions with outdoor workers have included multicomponent strategies (e.g., posters, e-mails, educational sessions), but have not examined the efficacy of the different components. Additionally, none of these interventions has identified important and significant mediators of the intervention effects, which is a critical step to understanding the process through which interventions work [29]. Finally, although self-reports of sun protection among outdoor workers appear to be valid [30], it is important to also examine objective measures, such as changes in skin color [27, 31–33].
UV Photography Interventions
Several recent studies have demonstrated the effectiveness of appearance-based interventions that use UV photography to highlight skin damage due to sun exposure [31, 32, 34–36]. The UV camera produces a photo that reveals skin damage unseen by the eye [37]. Chronic UV exposure produces non-uniform pigmentation, which appears as dark blotches and freckles in the photo. These interventions, some of which also include information on the impact of the sun on skin cancer and/or photoaging, enhance knowledge about the link between UV exposure and skin damage and have been shown to increase protection behaviors [31, 32, 35, 36, 38].
Several studies have examined the impact of UV photography among young people and/or those seeking a tan. In two studies of college students, Gibbons et al. [34] found that those who viewed vs. did not view their UV photo reported a decrease in tanning booth use 3–4 weeks later. Using a similar intervention among college students, Mahler and colleagues [39] found that viewing both the UV photo and a video on photoaging was associated with higher intentions to engage in sun protection, higher perceptions of vulnerability to skin damage, and greater sun protection 1 month later. Among beachgoers, Mahler and colleagues [31] found that the UV photo, photoaging information, and a combination of the two had a positive immediate impact on sun protection cognitions and intentions. The positive effects were still evident 2 months later and changes in sun protection behaviors were mediated by protection intentions. Longer-term effects (4–5 months and 1 year post-intervention) on sun protection behaviors and skin color, as measured by spectrophotometry, were also found using both UV photography and photoaging information among young adults [32]; however, this study did not examine the long-term impact on sun-related cognitions. Pagoto and colleagues [35] found that combining the UV photo with information on sun safety and sunscreen use, along with a commitment card and sunscreen samples, had a positive effect on the sun protection habits of Midwestern beachgoers 2 months post-intervention. Weinstock and colleagues [36] also used a multicomponent intervention with a large sample of beachgoers and found positive sun protection effects among the intervention group 24 months post-intervention. However, neither examined sun protection cognitions in addition to intentions and behaviors.
This current trend of using UV photography and information on UV damage has demonstrated strong promise for appearance-based interventions among populations that are particularly appearance conscious—college students, adolescents, beachgoers, and (young) females (i.e., those who are more likely to tan for appearance reasons [31, 32, 34, 40–42]). It is not clear, however, if this appearance-based intervention is effective with outdoor workers whose exposure is more incidental than intentional. This may especially be the case for older males who are less appearance conscious and thus are less likely to be motivated to engage in health behaviors for appearance reasons [43, 44] and who may also see sunscreen use as feminine [45].
Current Study
The intervention components in the current study draw upon previous interventions on sun protection using the UV photo and/or photoaging and cancer-related videos [31, 32, 34, 39, 46]. The frameworks and constructs examined in these intervention studies are typically drawn from the Health Belief Model [47] and the Prototype Model of Health Behavior [48], both of which describe cognitions thought to mediate the relations between health messages and health behavior. Drawing from the Health Belief Model, previous research has shown that perceptions of risk for skin cancer and damage are associated with higher levels of sun protection [32, 49, 50]. Barriers to sunscreen use (e.g., it is greasy) have also been associated with lower levels of sun protection [51, 52]. The Prototype Model of Health Behavior includes measures of prototypes or social images of people who engage in a health-risk or health-protective behavior. The more positive an individual’s image of a person who engages in a health behavior (e.g., sun protection), the more likely he/she is to engage in the behavior [53, 54]. For example, the more “manly” performing a health behavior is seen to be, the more likely a man is to engage in that behavior [45]. Previous sun protection research using this model has also included perceptions of vulnerability to negative outcomes (e.g., skin cancer) and attitudes (e.g., sunscreen is inconvenient) as core constructs in predicting health behaviors (e.g., sun protection). Gibbons et al. [34] found that the reduction in tanning booth use was mediated by a tanning cognition index composed of tanning attitudes and prototypes of others who engage in tanning behaviors. It is expected that increasing awareness of the link between UV exposure and skin damage will alter images of those who engage in sun protection as well as risk perceptions and attitudes. The present study assessed these images, sun attitudes, and perceptions of vulnerability.
Overview
Participants were randomly assigned either to one of four conditions in a 2 × 2 factorial design  or to a (fifth) control condition (no video, no-UV photo). The goals of the present research were to (a) examine the effectiveness of UV photography and both photoaging and skin cancer information in a sample of high-risk, male outdoor workers over a 1-year period and (b) examine potential mediators of changes in their protective behavior. An additional purpose was to examine which intervention component (i.e., information on skin cancer or photoaging with or without a UV photo) would be more effective with this population. We extended previous research by also examining an objective measure of sun exposure.
or to a (fifth) control condition (no video, no-UV photo). The goals of the present research were to (a) examine the effectiveness of UV photography and both photoaging and skin cancer information in a sample of high-risk, male outdoor workers over a 1-year period and (b) examine potential mediators of changes in their protective behavior. An additional purpose was to examine which intervention component (i.e., information on skin cancer or photoaging with or without a UV photo) would be more effective with this population. We extended previous research by also examining an objective measure of sun exposure.
First, we hypothesized a main effect of the intervention, such that the four conditions of the intervention would have a positive impact on sun protection cognitions and behaviors relative to the control condition. We further hypothesized that the UV photo conditions would be more effective than the no-UV photo conditions. Although the men in the current study are unlikely to be motivated by appearance, it was not known which video would be more effective over time. Finally, we hypothesized that the effects of the intervention on sun protection/skin color would be mediated by the sun protection cognitions outlined in the prototype model. We controlled for factors associated with the likelihood of a skin cancer diagnosis and engagement in sun protection behaviors: sun sensitivity, based on skin color [18, 20, 21, 55]; past history of skin cancer [50, 56]; and years working outdoors [5, 57].
Method
Participants
Sample size projections were based on the results of previous UV photo interventions, which had used intentions to engage in long-term sun protection (long-term behavior measures were unavailable).1 Approximately 200 Iowa Department of Transportation (DOT) road workers were asked to participate in the intervention study and 182 (86%) agreed. Of the 182, 20 participants were used for initial testing of the questionnaires and equipment and did not complete the intervention. Of the remaining 162, 148 met the criteria for inclusion in the study (male, outdoor worker) and completed both the pretest (T1) and post-intervention questionnaires (T2); 97.3% were available to complete the 1-year follow-up (T4). All data collection occurred in June–August.
Design and Procedures
The men answered a pre-intervention questionnaire and had their skin color assessed using skin reflectance spectrophotometry [27, 32] prior to the intervention (T1). The research was conducted at the DOT highway field offices, and the men participated either during work hours or received $75 for participating before or after work. All aspects of the study received institutional review board approval.
Interventions
The overall intervention had two primary elements: (a) a photograph taken of the face with a UV-filter camera and (b) a 12-min educational video on UV risk (focusing on either skin cancer or photoaging). The video discussed the impact of the sun and UV exposure on either photoaging or skin cancer and provided pictures of skin damage (wrinkles and age spots or skin cancer). Each video also provided information about sunscreen use and skin protection (e.g., how much sunscreen to use, an explanation of sun protection factor [SPF], recommendation of an SPF of at least 15). Participants were first randomly assigned by worksite to receive or not receive a UV photo or to be in the control condition. Once the experimenters were at the worksite, they used a random number generator to then assign each worker to see the skin cancer or photoaging video. Thus, participants were assigned to one of five conditions: a control condition or one of the four intervention conditions: no-UV/aging, no-UV/skin cancer, UV/aging, UV/skin cancer.
All participants first had two Polaroid photos taken of their faces: a natural-light black-and-white photo and a UV photo. The filtered UV light is absorbed by the melanin in the skin and the resulting photo highlights the non-uniform epidermal pigmentation that has resulted from chronic exposure to UV rays [37]. Participants in the control and no-UV photo conditions were only shown the natural-light photo and were told the purpose of this photo would be explained at the end of the study. Men in the UV conditions were shown their natural-light photo and their UV photo as comparison. Participants were told that any “dark, freckled, or splotched areas” in the UV photograph that were not evident in the natural-light photograph indicated existing underlying skin damage due to UV exposure that will get worse if they continue to be exposed to the sun without additional protection. Intervention participants then watched their assigned video (cancer or photoaging; for additional details on the manipulations, see Mahler et al. [32, 46, 58]).
Post-Intervention
The men then responded to a second questionnaire (T2) which assessed the retention of the video information and their estimates of long-term skin damage and attitudes toward sun protection. Approximately 2 months (T3) later, participants reported their sun protection behaviors and had their skin color assessed using spectrophotometry [27, 32].2 One year later (T4), participants reported their sun protection cognitions and behaviors. After completion of the questionnaire, skin color was again assessed with the spectrophotometer and all participants were given sunscreen and written information related to sun protection.
Measures
T1 Premanipulation Variables
Demographics (e.g., age, type of job) and previous history of skin cancer (including precancerous spots) were assessed at T1. Skin type was measured using Fitzpatrick’s [59] classification of sun-reactive skin types, which represent the propensity to sunburn and tendency to tan. All analyses controlled for all background variables.
T2 Manipulation Checks and Sun Protection Attitudes
Two questions assessed the retention of information included in both videos (i.e., minimum recommended SPF level, naming common mistakes people make when using sunscreen). A third question assessed perceptions of skin damage, “How much long-term skin damage do you think you have gotten from the sun?” (1 = none, 7 = a lot). Sun protection attitudes were assessed with the following five statements: “Having a tan… is unhealthy…makes me look healthy …not worth the damage it causes to my skin”; “There is no point in using sunscreen—the damage is already done”; “Sunscreen is more trouble than it’s worth.” Each item was followed by a five-point scale (1 = strongly disagree, 5 = strongly agree; α = 0.65). All items (in all scales) were coded so that a high score represents more favorable sun protection attitudes.
T1 Sun Protection Cognitions
Attitudes (six items) consisted of two items for each of three dimensions: nuisance, e.g., “Using sunscreen before going out on the job would be a nuisance”; appearance, e.g., “Having a tan improves the way I look”; and health, e.g., “I do not think much about getting skin cancer from the sun” (response options ranged from 1 = strongly agree to 5 = strongly disagree; α = 0.71). Perceived risk (four items) consisted of: absolute perceived risk “What do you think the chances are that you will get skin cancer [wrinkles and age spots]?” (1 = no chance, 7 = very likely) and comparative perceived risk “Compared with other men your age, how likely is it that you will get skin cancer [skin damage]?” (1 = much less likely, 7 = much more likely; α = 0.86). Attitudes and perceived risk were standardized and combined into an overall sun protection cognition index at T1 (cf. Gibbons et al. [34]; α = 0.79).
T4 Sun Protection Cognitions
Attitudes (α = 0.73) and perceived risk (α = 0.87) were measured the same as at T1. Prototypes were also assessed at T4 by asking the men to “…think about the type of DOT worker who protects himself from the sun on the job” and “…think about the typical male your age who engages in sun protection” and then rate these images on three adjectives: smart, masculine, self-confident (1 = not at all, 7 = extremely). Factor analysis revealed that the smart items did not combine with the other two items, and so they were not included in the final construct (α = 0.86). Attitudes, perceived risk, and the prototypes were standardized and combined into an overall T4 sun protection cognition index (α = 0.88).
T1 and T4 Sun Protection
There were six sun protection behaviors: “How often do you wear sunscreen (hat/long sleeves) when your job requires you to be outdoors for an extended time,” “In general, when you spend time in the sun, how often do you use sunscreen on your face (body),” and “How often do you wear sunscreen when you are outdoors on your own time.” Skin color was assessed using a Minolta CM-2600d spectrophotometer, which allows for an objective quantification of skin color [60, 61]. This instrument measures skin color on two dimensions that have previously been shown to be sensitive to tanning, L* and b* [27, 31, 62]. L* indexes lightness, with higher values indicating lighter skin color, and b* indexes saturation, with higher values indicating more color (i.e., more tan). At T1 and T4, three consecutive readings of L* and b* were taken from the outer and inner sides of the arm and from the left side of the face. The L* readings did not significantly correlate with the other sun protection items (e.g., T1 ps > 0.3; cf., Mayer et al. [27]) and so were not used in the sun protection construct. The b* readings did correlate with sun protection (e.g., T1 rs = −0.19, −0.17, −0.23, ps < 0.05). The six sun protection items and three b* skin color readings (reverse coded) were standardized and combined into a sun protection index (T1 α = 0.76; T4 α = 0.70).
T3 Sun Protection
At T3, sun protection behavior was assessed with six similar but slightly different behavior items: “During the last 7–8 weeks how often did you…” “wear sunscreen on your face (body) when your job required you to be outdoors?,” “…wear sunscreen on your face (body) when you were outdoors on your own time?,” and “…wear a hat (long sleeves) when your job required you to be outdoors?” Skin color was assessed the same as at T1 and T4. The six sun protection items and three b* skin color readings (reverse coded) were again standardized and combined (α = 0.74).
Results
Statistical Analyses
To examine the impact of the separate intervention components on T2 attitudes, T4 cognitions, and T3 and T4 sun protection, we ran a series of analyses of covariance (ANCOVAs). In order to include the variance associated with the control condition into the mean square error estimate, the four intervention conditions (no-UV/aging, no-UV/cancer, UV/aging, and UV/cancer) and the control group were treated as five groups (e.g., [63, 64]). As mentioned, it was expected that the UV photo conditions would result in the strongest effects. Intervention conditions were combined when they were significantly different from the control group, but not from each other [63]. Cohen’s d, which represents the differences between means divided by the averaged variability, was calculated to represent effect sizes [65]. We then employed structural equation modeling (SEM) to simultaneously examine the long-term effectiveness of the intervention and test the hypothesized mediation of intervention effects through T4 sun protection cognitions on T4 sun protection (using Mplus Version 4.2 with full information maximum likelihood [66]).
Descriptive Statistics
This was a very high-risk group: 81% reported never or only occasionally using sunscreen, 83% reported never or only occasionally wearing long sleeves, 90% reported spending at least 5–6 h in the sun each work day, and 60% reported at least 7–10 h in the sun each day. Ninety-seven percent of the men were White; the age range at T1 was 24 to 64 years (M = 46.5), and the men reported working at DOT an average of 14.3 years and in outdoor jobs an average of 27 years. Older workers and those with a history of skin cancer and lighter skin types reported higher levels of sun protection (ps < 0.05 [44]; see Table 1). As expected, sun protection and cognitions were very stable over time (ps < 0.001). T2 estimates of long-term skin damage were positively associated with T4 cognitions (ps < 0.001), and T2 attitudes were positively correlated with T4 sun protection cognitions and T3 and T4 sun protection (ps < 0.001).
Table 1.
Means, standard deviations, and correlations for indices
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Age | – | ||||||||||
| 2. Years at DOT | 0.28** | – | |||||||||
| 3. History of skin cancer | 0.19* | 0.08 | – | ||||||||
| 4. Skin type | −0.06 | −0.16 | −0.21* | – | |||||||
| 5. T1 cognitions | 0.19* | 0.11 | 0.40*** | −0.10 | – | ||||||
| 6. T1 sun protection | 0.17* | 0.08 | 0.45*** | −0.31*** | 0.48*** | – | |||||
| 7. T2 skin damage | 0.11 | 0.10 | 0.21** | −0.13 | 0.21* | 0.08 | – | ||||
| 8. T2 attitudes | 0.07 | 0.11 | 0.22** | −0.18* | 0.50*** | 0.36*** | 0.21** | – | |||
| 9. T3 sun protection | 0.16* | 0.05 | 0.34*** | −0.28*** | 0.39*** | 0.76*** | 0.09 | 0.37*** | – | ||
| 10. T4 cognitions | −0.04 | 0.06 | 0.37*** | −0.18* | 0.51*** | 0.44*** | 0.34*** | 0.34*** | −0.34*** | – | |
| 11. T4 sun protection | 0.18* | −0.02 | 0.30*** | −0.23** | 0.43*** | 0.78*** | 0.04 | 0.37*** | 0.79*** | 0.53*** | – |
| Mean | 46.1 | 14.2 | 0.05 | 0.00 | 0.00 | 1.00 | 5.14 | 3.53 | 0.99 | −0.01 | 0.99 |
| SD | 9.36 | 8.91 | 0.21 | 0.87 | 0.51 | 0.42 | 1.37 | 0.63 | 0.44 | 0.45 | 0.47 |
| Range | 24–64 | 0.5–38 | 0–1 | 1–6 | −0.9 to 1.5 | −0.04 to 3.6 | 2–7 | 2–5 | 0.03–3.2 | −1 to 1.5 | −0.05 to 3.4 |
N = 148; T2 skin damage = self-reported estimate of long-term skin damage
*p ≤ 0.05, **p < 0.01, ***p < 001
A series of initial general linear model (GLM) analyses of variance (ANOVAs) was performed to examine condition randomization of the control variables: age, years working at the DOT, history of skin cancer, skin type, and T1 sun protection. There was a significant condition effect for years working at DOT, as participants in the no-UV/cancer video condition reported the longest time at the DOT (F(4, 143) = 2.88, p < 0.05). No other significant condition effects were found (all Fs < 0.8, ps > 0.5). All analyses were below the control for all of these variables.
T2 Manipulation Checks and Attitudes
Knowledge
GLM ANOVAs performed on responses to the manipulation check items revealed a significant condition effect, such that men in the intervention conditions (all of whom watched a video) were more likely than those in the control condition to correctly answer the questions (both ps < 0.001). No significant differences were found between intervention conditions (ps > 0.5).
Skin Damage
To examine the impact of the UV photo on estimates of long-term skin damage, we first compared the two UV photo conditions combined with the no-UV and control conditions combined. The expected photo effect was found: participants who saw their UV photo reported more skin damage from the sun than did those who did not view their UV photo (F(1, 146) = 5.0, p < 0.03, d = 0.41, M = 5.45 vs. 4.93). In addition, men in each UV condition reported significantly higher estimates than did those in the control condition (Fs > 4.9, ps < 0.03, ds > 0.6) and those in the no-UV/cancer condition reported marginally higher estimates than those in the control condition (F(1, 54) = 3.80, d = 0.58, p < 0.06, Ms = 5.33 vs. 4.58). The no-UV/aging condition (M = 4.93) was not significantly different from the control (F(1, 53) = 1.96, p = 0.17).
Attitudes
Planned comparisons using GLM ANCOVAs were first employed to compare each condition to the control condition on T2 attitudes (for the means, see Table 2). All four intervention conditions were significantly different from the control condition (all Fs > 7.55, ps < 0.01, ds > 0.81). Additional ANCOVAs revealed that none of the intervention conditions was significantly different from all the other intervention conditions (Fs < 0.63, ps > 0.4). When the four intervention conditions were combined, as anticipated, intervention participants reported more positive attitudes toward sun protection than did those in the control condition, F(1, 146) = 11.49, p = 0.001, d = 0.86; Ms = 3.6 vs. 3.1, respectively.
Table 2.
Means and standard errors of T2 attitudes and T1, T3, and T4 sun protection
| Variable | No-UV | UV | |||
|---|---|---|---|---|---|
| Aging (n = 30) | Cancer (n = 31) | Aging (n = 31) | Cancer (n = 32) | Control (n = 24) | |
| T2 attitudes | 3.56 (0.09) | 3.65 (0.10) | 3.66 (0.11) | 3.57 (0.09) | 3.01 (0.11) |
| T1 sun protection (pre-intervention) | 1.04 (0.08) | 0.99 (0.09) | 0.93 (0.07) | 0.93 (0.06) | 0.94 (0.09) |
| T3 sun protection (2 months post-intervention) | 0.96 (0.10) | 1.05 (0.09) | 1.12 (0.10) | 0.98 (0.09) | 0.79 (0.10) |
| T4 sun protection (1 year post-intervention) | 0.93 (0.10) | 1.08 (0.09) | 1.13 (0.10) | 1.06 (0.09) | 0.78 (0.11) |
T2 attitudes scale range = 2–5; T1 behavior scale = −0.04 to 3.6; T3 behavior scale = 0.03–3.2; T4 behavior scale = −0.05 to 3.4. Higher numbers indicate more positive sun protection attitudes or sun protection behavior and lighter skin color (darkness reverse coded)
T3 Sun Protection (2-Month Follow-Up)
A series of GLM ANCOVAs was again used to compare each intervention condition to the control condition on T3 sun protection (see Table 2) controlling for T1 sun protection and the additional control variables. When the four intervention conditions were combined, the intervention participants reported more sun protection than did those in the control condition, F(1, 144) = 6.04, p < 0.02, d = 0.68, Ms = 0.78 vs. 1.02, respectively. Participants in the no-UV/aging condition reported marginally higher sun protection than did control participants, F(1, 51) = 3.09, p < 0.09. Participants in the other three intervention conditions reported significantly greater sun protection than those in the control condition (all Fs > 4.15, ps < 0.05, ds ≥ 0.6). Additional ANCOVAs revealed that none of the intervention conditions was significantly different from each other (Fs < 0.82, ps > 0.37).
T4 Sun Protection and Cognitions (1-Year Follow-Up)
T4 Cognitions
Controlling for T1 cognitions, the ANCOVA comparing the control to the no-UV aging condition was not significant (F(1, 52) = 1.82, p < 0.14). When comparing the control condition with the other three (cancer-related) conditions, marginal effects were found such that the men in these conditions tended to report more favorable sun protection cognitions (all Fs > 2.77, ps ≤ 0.10, ds > 0.5). When these three conditions were combined and compared to the no-UV/aging and control conditions combined, the ANCOVA was significant, F(1, 141) = 3.83, p = 0.05, d = 0.36, Ms = 0.05 vs. −0.05, respectively.3
T4 Sun Protection
To more closely examine the effects of the intervention conditions on the major outcome variable, T4 sun protection, a series of GLM ANCOVAs was conducted, controlling for baseline sun protection and background constructs. Upon examination of the mean level of sun protection, it was found that the men in the control condition, followed by those in the no-UV/aging condition, had the lowest level of sun protection (see Table 2). Planned comparisons again compared each condition to the control condition. Sun protection in the no-UV/aging condition was not significantly higher than those in the control condition, F(1, 52) = 2.13, p = 0.15. Participants in the other three conditions with the UV photo and/or cancer video had significantly greater sun protection than did those in the control condition (all Fs > 6.95, ps ≤ 0.01, ds > 0.79). Additional ANCOVAs revealed that the men in the other three conditions had significantly higher levels of sun protection at T4, controlling for T1 levels, than did those in the no-UV/aging condition (ps < 0.02). When the three UV and cancer video interventions were combined and compared to the no-UV/aging and control conditions combined, the ANCOVA was also significant, F(1, 146) = 13.66, p < 0.001, d = 0.72. Thus, photoaging information alone did not produce significant changes in long-term sun protection. These results indicate that the most effective interventions for this high-risk male population were those that included the UV photo and/or information related to skin cancer.
SEM Mediation Model
Measurement Model
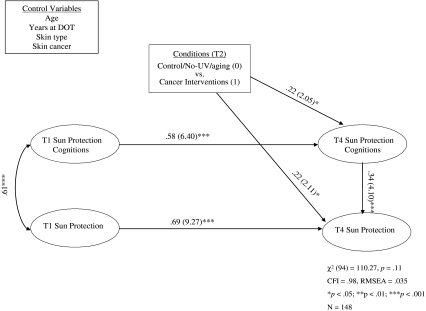
Based on the results of the T4 ANCOVAs, the no-UV/aging and control conditions were combined and compared to the three other interventions in the SEM. The model was designed to examine the intervention effects on the major outcome of interest, sun protection at the 1-year follow-up. The model also examined the impact of the effective intervention components on change in sun protection cognitions and whether these changes mediated the changes in sun protection. The model (see Fig. 1) controlled for all control variables. A confirmatory factor analysis was conducted to determine if the indicators loaded on the constructs as expected. The intervention was coded as dichotomous and specified as a manifest construct (0 = control/no-UV/aging, 1 = cancer video and UV interventions); the other four constructs were specified as latent. Three randomly generated parcels were used as indicators of the latent T1 and T4 sun protection constructs (α = 0.80 and 0.96, respectively), and three randomly generated parcels of the questions were also used as indicators of the latent T1 and T4 sun cognitions constructs in the SEM (T1 α = 0.81 and T4 α = 0.83). The measurement model fit the data well: χ 2(df = 92, N = 148) = 107.44, p = 0.12; comparative fit index (CFI) = 0.986; root mean square error of approximation (RMSEA) = 0.034. All standardized factor loadings were significant and greater than 0.70. To examine potential clustering effects based on worksite, intraclass correlations were calculated for T4 cognitions and sun protection. Both were <0.03, indicating that the proportion of the total variation that could be accounted for by clustering was <3%. The design effects were also <1.2, also suggesting no significant clustering [67].
Fig. 1.
Direct and mediational analyses of intervention effects on sun protection and cognitions 1 year post-intervention, controlling for baseline status and demographic measures
Intervention Efficacy and Mediation Model
The structural model also fit the data well, χ 2(94) = 110.27, p = 0.1; RMSEA = 0.035; CFI = 0.984 (see Fig. 1). In spite of the high stability from T1 to T4 for both cognitions (β = 0.58, z = 6.4, p < 0.001) and sun protection (β = 0.69, z = 9.27, p < 0.001), the direct path from intervention to T4 cognitions was significant (β = 0.23, z = 2.12, p < 0.05), as was the direct effect from the T4 mediator to T4 sun protection (β = 0.34, z = 4.10, p < 0.001). The total effect of the intervention on T4 sun protection was significant, β = 0.29, z = 2.6, p < 0.01. In addition, the indirect effect from intervention to T4 sun protection through cognitions was significant (β = 0.08, z = 2.15, p < 0.05) and the bootstrap 95% confidence interval did not cover zero (−0.12, −0.01), also indicating a significant mediation effect.4 The direct path from intervention to T4 sun protection remained significant in this model (β = 0.22, z = 2.05, p < 0.05), indicating that the intervention had both a direct and a significant mediated effect on sun protection 1 year post-intervention, controlling for sun protection and cognitions 1 year earlier. The model explained 78% of the variance in sun protection 1 year post-intervention; 62% of the variance is explained by T1 sun protection and 16% explained by T4 sun protection cognitions and the intervention.
Discussion
The present study demonstrates the effectiveness of UV photo interventions on a high-risk sample of outdoor workers. Controlling for important covariates, the UV photo and cancer video interventions altered these men’s cognitions about sun protection, and this effect, in turn, partially mediated the significant impact the intervention had on increasing sun protection, including decreasing levels of darkness of skin color. These intervention conditions also had a direct effect on sun protection and cognitions, while controlling for prior sun protection and cognitions. This study replicates the effects of the UV photo interventions on college students and beach patrons [31, 32, 34, 39] and extends these results by showing longer-term (1-year) effectiveness on sun protection and cognitions and by including objective evidence of lower levels of sun exposure.
The men in all four intervention conditions reported more positive sun protection attitudes than did those in the control condition immediately following the intervention. In addition, the men who saw their UV photo reported higher estimates of long-term skin damage (vs. those who did not) and those who saw the cancer video reported marginally higher estimates of damage compared to the control condition [31]. Positive effects on sun protection behaviors and skin color were evident for all intervention conditions 2 months post-intervention, controlling for pre-intervention levels. However, these effects were stronger among the men in the UV photo and cancer video interventions. The direct impact of these three interventions was also very strong on the primary outcome, sun protection, 1 year post-intervention.
Consistent with the Health Belief Model and Prototype Model of Health Behavior, there was also long-term evidence that those who received these cancer-related interventions came to view themselves as more susceptible to photoaging and skin cancer and had a more positive image of men their age who engage in sun protection, as well as more positive attitudes toward sun protection. The findings argue for the importance of changing these cognitions. This evidence of significant partial mediation is similar to the findings of Gibbons et al. [34] who demonstrated that UV photography influenced a similar tanning cognition index in a study of college students.
Intervention Components
Unlike interventions that include many different components, we examined the effectiveness of a single (video only) vs. dual (video plus UV photo) component intervention on sun protection. In decomposing the effects of the intervention, the no-UV photo aging video condition was not as effective in the long-term as the other three conditions. It may be that seeing one’s damage and/or highlighting the link between UV exposure and skin cancer has more impact for this particular population. These results highlight the importance of examining appearance-based vs. skin cancer-based interventions for different populations. Our results indicate that appearance-only interventions may not be as effective for male outdoor workers, especially within an older population, who are less likely to be appearance-motivated [68]. Mahler and colleagues [31] did find significant effects of the no-UV aging condition on cognitions and sun protection 2 months post-intervention; however, this sample consisted of primarily female beachgoers with lower levels of UV exposure.
Previous UV photography interventions have focused primarily on female participants who tend to engage in intentional UV exposure. Although a few other interventions have shown positive effects among high-risk outdoor workers [23, 26, 27], this is the first demonstration of the long-term effectiveness of UV photography and educational information on (high-risk) outdoor workers. In addition, a national survey of adults found that being male and living in the Midwest are associated with some of the lowest levels of sun protection [20]. The finding that the men in our sample also had high rates of UV exposure during leisure time (on average more than 20 h/week), along with the finding that the intervention increased sun protection on their own time, demonstrate the importance of examining UV behaviors among high-risk groups when they are not at work [52].
Limitations
Although the study included more than 24 participants per group and had a very good follow-up rate, future research should extend these findings to larger, more diverse samples. For example, all of the participants were male. It is important to also examine the effectiveness of the intervention on female outdoor workers. In addition, because of the lack of ethnic diversity and the small range of skin types in our sample, we cannot say that the intervention components would result in the same positive outcomes for workers from other racial/ethnic groups and of other skin tones.
Another limitation is that the mediators were measured at the same time as sun protection behaviors and skin color. Although the workers were told there would be a follow-up, they were not scheduled until the week prior, thus it is likely that skin color and sun protection behaviors were a reflection of true change. Additionally, we did not find that any of these factors alone mediated the intervention, thus future studies should continue to examine the cognitive processes underlying the intervention’s impact. Research on men’s health has demonstrated the potential importance of norms (e.g., [45]) and it is possible that perceptions of increased sun protection among coworkers may have had an impact. In addition, the cancer-related information may have increased feelings of worry and fear, perceptions of the severity of UV damage, as well as efficacy in sun protection, which may have motivated the increased sun protection [58, 69, 70]. Finally, we did not find effects with the L* spectrophotometry readings. Although effects have been found for L* among college students [32], Mayer et al. [27] also found b* to be more appropriate for outdoor workers. It is uncertain why these readings appear to tap into different aspects of skin color, but one possibility is that b* is more sensitive to skin color among those with long-term exposure to UV rays [27].
Future Directions
Future directions of this research should involve combining the UV photograph and educational information in the workplace setting with other mechanisms used in multicomponent interventions, such as newsletters, supervisor training, workplace policies, provision of protective clothing, and skin examinations [17, 23, 26]. It is also possible that additional exposure to the intervention components would have even stronger impact. Thus far, there have been only a small number of effective behavioral studies in occupational settings [29] and the variations in occupations, measures used, and intervention components make it difficult to directly compare our intervention to those of other settings with other populations. Thus, more studies are needed to determine which components are most effective with which populations.
Analyses from a separate sample of highway road workers who participated in a different survey study (Stock et al., manuscript in preparation) indicated that having coworkers who engage in sun protection or have had skin cancer predicts positive sun protection cognitions and behaviors, suggesting that future research should further explore the effects of coworkers. We have also found that feeling that it is “manly” to wear sunscreen is a strong predictor of sun protection. Thus, including masculine, respected role models [45] may enhance the effects of an intervention on this population. Finally, based on comments made by the participants, we believe it may also be beneficial to make sun protection more convenient and less greasy/messy.
Conclusion
This study adds to the growing literature demonstrating the efficacy of UV photography interventions in reducing harmful UV exposure among an at-risk group. This study is one of the first interventions with outdoor workers to show mediation of long-term effects on sun protection. In addition, baseline measures along with relevant demographic characteristics were assessed and statistically controlled for in all analyses. Due to the increasing rates of skin cancer, particularly among older males and outdoor workers, an effective intervention for increasing sun protection has the potential for significant public health impact. This intervention is inexpensive, brief, and can be easily implemented at worksites. We believe that the important long-term effects of these intervention components have promise for reducing skin cancer risk among high-risk populations.
Acknowledgments
This research was supported by the National Cancer Institute Grant #CA 9051501A2. The authors would like to thank Barbara Mallon of the Iowa Department of Transportation for facilitating this study and the road maintenance workers for participating. We also thank Phil Miller, Shawn Haake, Steve Charman, Morgan Casner, Jamie Blum, and Julie Davis for their assistance in carrying out the project.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
Using Cohen’s power tables with an alpha set at 0.05, the average d at 1.03, and n initially at 24, we found that the estimate of our power would be 0.92 and, with cell sizes of at least 15, the estimated power would be d = 0.75. The average outcome effect size of previous studies that had employed the spectrophotometer to measure skin color (33, 46) was d = 0.69 and a power estimate of greater than 0.66 was estimated for an n of 24 per cell.
A measure of cognitions was also included at T3, but the cognitive measure was not directly comparable to T1 or T4 measures and, therefore, was not included. We did examine if the T3 cognitions mediated the impact of the intervention conditions on T4 sun protection, but these effects were not significant.
When the no-UV/aging and control conditions were combined and compared to the three cancer-related interventions, the ANCOVA was also significant (p < 0.05).
Mediation was not significant when the cognitions (attitudes, perceived risk, and prototype) were separated and examined individually in the model.
An erratum to this article can be found at http://dx.doi.org/10.1007/s12160-010-9179-3
References
- 1.Skin Cancer Foundation. Skin cancer facts. Available at http://www.skincancer.org/skin-cancer-facts/. Accessibility verified October 8, 2009.
- 2.Armstrong BK, Kricker A. The epidemiology of UV induced skin cancer. J Photochem Photobiol B. 2001;63:8–18. doi: 10.1016/S1011-1344(01)00198-1. [DOI] [PubMed] [Google Scholar]
- 3.Strickland PT, Vitasa BC, West SK, Rosenthal FS, Emmett EA, Taylor HR. Qualitative carcinogenesis in man: Solar ultraviolet B dose dependence of skin cancer in Maryland watermen. J Natl Cancer Inst. 1989;81:1910–1913. doi: 10.1093/jnci/81.24.1910. [DOI] [PubMed] [Google Scholar]
- 4.Ramirez CC, Federman DG, Kirsner RS. Skin cancer as an occupational disease: The effect of ultraviolet and other forms of radiation. Int J Dermatol. 2004;44:95–100. doi: 10.1111/j.1365-4632.2005.02301.x. [DOI] [PubMed] [Google Scholar]
- 5.Nole G, Johnson AW. An analysis of cumulative lifetime solar ultraviolet radiation exposure and the benefits of daily sun protection. Dermatol Ther. 2004;17:57–62. doi: 10.1111/j.1396-0296.2004.04S1007.x. [DOI] [PubMed] [Google Scholar]
- 6.Dummer R, Maier T. UV protection and skin cancer. Recent Results Cancer Res. 2002;160:7–12. doi: 10.1007/978-3-642-59410-6_2. [DOI] [PubMed] [Google Scholar]
- 7.Naylor MF, Farmer KC. The case for sunscreens: A review of their use in preventing actinic damage and neoplasia. Arch Dermatol. 1997;133:1146–1154. doi: 10.1001/archderm.133.9.1146. [DOI] [PubMed] [Google Scholar]
- 8.Darlington S, Williams G, Neale R, Frost C, Green A. A randomized controlled trial to assess sunscreen application and beta carotene supplementation in the prevention of solar keratoses. Arch Dermatol. 2003;139:451–455. doi: 10.1001/archderm.139.4.451. [DOI] [PubMed] [Google Scholar]
- 9.Naylor MF, Boyd A, Smith DW, Cameron GS, Hubbard D, Nelder KH. High sun protection factor sunscreens in the suppression of actinic neoplasia. Arch Dermatol. 1995;131:170–175. doi: 10.1001/archderm.131.2.170. [DOI] [PubMed] [Google Scholar]
- 10.Pandeya N, Purdie DM, Green A, Williams G. Repeated occurrence of basal cell carcinoma of the skin and multifailure survival analysis: Follow-up data from the Nambour Skin Cancer Prevention Trial. Am J Epidemiol. 2005;161:748–754. doi: 10.1093/aje/kwi098. [DOI] [PubMed] [Google Scholar]
- 11.Holman CDJ, Gibson IM, Stephenson M, Armstrong BK. Ultraviolet irradiation of human body sites in relation to occupation and outdoor activity: Field studies using personal UVR dosimeters. Clin Exp Dermatol. 1983;8:269–277. doi: 10.1111/j.1365-2230.1983.tb01779.x. [DOI] [PubMed] [Google Scholar]
- 12.Puntoni R, Ceppi M, Ugolini D, et al. Increased incidence of cutaneous malignant melanoma among longshoremen in Genoa, Italy: The role of sunlight and occupational exposure. Occup Environ Med. 2005;62:270–271. doi: 10.1136/oem.2004.018374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gies P, Wright J. Measured solar ultraviolet radiation exposures of outdoor workers in Queensland in the building and construction industry. Photochem Photobiol. 2003;78:342–348. doi: 10.1562/0031-8655(2003)078<0342:MSUREO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 14.Radespiel-Tröger M, Meyer M, Pfahlberg A, Lausen B, Uter W, Gefeller O. Outdoor work and skin cancer incidence: A registry-based study in Bavaria. Int Arch Occup Environ Health. 2008;82:357–363. doi: 10.1007/s00420-008-0342-0. [DOI] [PubMed] [Google Scholar]
- 15.Severi G, English DR. Descriptive epidemiology of skin cancer. In: Hill D, Elwood JM, English DR, editors. Prevention of Skin Cancer. Dordrecht: Kluwer Academic; 2004. pp. 73–87. [Google Scholar]
- 16.Vishvakarman D, Wong JC. Description of the use of a risk estimation model to assess the increased risk of non-melanoma skin cancer among outdoor workers in Central Queensland, Australia. Photodermatol Photoimmunol Photomed. 2003;19:81–88. doi: 10.1034/j.1600-0781.2003.00012.x. [DOI] [PubMed] [Google Scholar]
- 17.Glanz K, Buller DB, Saraiya M. Reducing ultraviolet radiation exposure among outdoor workers: State of the evidence and recommendations. Environ Health. 2007;6:22. doi: 10.1186/1476-069X-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lewis E, Mayer JA, Slymen D. Postal workers’ occupational and leisure-time sun safety behaviors (United States) Cancer Causes Control. 2006;17:181–186. doi: 10.1007/s10552-005-0482-4. [DOI] [PubMed] [Google Scholar]
- 19.Pichon LC, Mayer JA, Slymen DJ, Elder JP, Lewis EC, Galindo GR. Ethnoracial differences among outdoor workers in key sun-safety behaviors. Am J Prev Med. 2005;28:374–378. doi: 10.1016/j.amepre.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Coups EJ, Manne SL, Heckman CJ. Multiple skin cancer risk behaviors in the U.S. population. Am J Prev Med. 2008;34:87–93. doi: 10.1016/j.amepre.2007.09.032. [DOI] [PubMed] [Google Scholar]
- 21.Weinstock MA, Rossi JS, Redding CA, Maddock JE, Cottrill SD. Sun protection behaviors and stages of change for the primary prevention of skin cancers among beachgoers in southeastern New England. Ann Behav Med. 2000;22:286–293. doi: 10.1007/BF02895664. [DOI] [PubMed] [Google Scholar]
- 22.Girgis A, Sanson-Fisher RW, Watson A. A workplace intervention for increasing outdoor workers’ use of solar protection. Am J Public Health. 1994;84:77–81. doi: 10.2105/AJPH.84.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Azizi E, Flint P, Sadetzki S, et al. A graded work site intervention program to improve sun protection and skin cancer awareness in outdoors workers in Israel. Cancer Causes Control. 2000;11:513–521. doi: 10.1023/A:1008970224998. [DOI] [PubMed] [Google Scholar]
- 24.Borland RM, Hocking B, Godkin GA, Gibbs AF, Hill DJ. The impact of a skin cancer control education package for outdoor workers. Med J Aust. 1991;154:686–688. doi: 10.5694/j.1326-5377.1991.tb121261.x. [DOI] [PubMed] [Google Scholar]
- 25.Geller AC, Glanz K, Shigaki D, Isnec MR, Sun T, Maddock J. Impact of a skin cancer prevention on outdoor aquatics staff: The Pool Cool program in Hawaii and Massachusetts. Prev Med. 2001;33:155–161. doi: 10.1006/pmed.2001.0870. [DOI] [PubMed] [Google Scholar]
- 26.Buller DB, Andersen PA, Walkosz BJ, et al. Randomized trial testing a worksite sun protection program in an outdoor recreation industry. Health Educ Behav. 2005;32:514–535. doi: 10.1177/1090198105276211. [DOI] [PubMed] [Google Scholar]
- 27.Mayer JA, Slymen DJ, Clapp EJ, et al. Promoting sun safety among US Postal Service letter carriers: Impact of a 2-year intervention. Am J Public Health. 2007;97:559–565. doi: 10.2105/AJPH.2005.083907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Glanz K, Mayer JA. Reducing ultraviolet radiation exposure to prevent skin cancer: Methodology and measurement. Am J Prev Med. 2005;2:131–142. doi: 10.1016/j.amepre.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 29.Saraiya M, Glanz K, Briss PA, et al. Interventions to prevent skin cancer by reducing exposure to ultraviolet radiation: A systematic review. Am J Prev Med. 2004;27:422–466. doi: 10.1016/j.amepre.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 30.Oh SS, Mayer JA, Lewis EC, et al. Validating outdoor workers’ self-report of sun protection. Prev Med. 2004;39:798–803. doi: 10.1016/j.ypmed.2004.03.011. [DOI] [PubMed] [Google Scholar]
- 31.Mahler HIM, Kulik JA, Gerrard M, Gibbons FX. Effects of two appearance-based interventions on the sun protection behaviors of southern California beach patrons. Basic Appl Soc Psychol. 2006;28(2):63–272. [Google Scholar]
- 32.Mahler HIM, Kulik JA, Gerrard M, Gibbons FX. Long-term effects of appearance-based interventions on sun protection behaviors. Health Psychol. 2007;26:350–360. doi: 10.1037/0278-6133.26.3.350. [DOI] [PubMed] [Google Scholar]
- 33.Buller DB, Buller MK, Beach B, Ertl G. Sunny days, healthy ways: Evaluation of a skin cancer prevention curriculum for elementary school-aged children. J Am Acad Dermatol. 1996;35:911–922. doi: 10.1016/S0190-9622(96)90115-2. [DOI] [PubMed] [Google Scholar]
- 34.Gibbons FX, Gerrard M, Lane DJ, Mahler HIM, Kulik JA. Using UV photography to reduce use of tanning booths: A test of cognitive mediation. Health Psychol. 2005;24:358–363. doi: 10.1037/0278-6133.24.4.358. [DOI] [PubMed] [Google Scholar]
- 35.Pagoto S, McChargue DE, Fuqua WR. Effects of a multicomponent intervention on motivation and sun protection behaviors among Midwestern beachgoers. Health Psychol. 2003;22:429–433. doi: 10.1037/0278-6133.22.4.429. [DOI] [PubMed] [Google Scholar]
- 36.Weinstock MA, Rossi JS, Redding CA, Maddock JE. Randomized controlled community trial of the efficacy of a multicomponent stage-matched intervention to increase sun protection among beachgoers. Prev Med. 2002;35:584–592. doi: 10.1006/pmed.2002.1114. [DOI] [PubMed] [Google Scholar]
- 37.Fulton JE. Utilizing the ultraviolet (UV Detect) camera to enhance the appearance of photodamage and other skin conditions. Dermatol Surg. 1997;23:163–169. doi: 10.1016/S1076-0512(97)00097-6. [DOI] [PubMed] [Google Scholar]
- 38.Weinstock MA, Rossi JS. The Rhode Island Sun Smart project: A scientific approach to skin cancer prevention. Clin Dermatol. 1998;16:411–413. doi: 10.1016/S0738-081X(98)00013-3. [DOI] [PubMed] [Google Scholar]
- 39.Mahler HIM, Kulik JA, Harrell MA, Correa A, Gibbons FX, Gerrard M. A randomized trial examining the effects of UV photo, photoaging information, and use of sunless tanning lotion on sun protection behaviors of young adults. Arch Dermatol. 2005;141:373–380. doi: 10.1001/archderm.141.3.373. [DOI] [PubMed] [Google Scholar]
- 40.Hillhouse JJ, Turrisi R, Kastner M. Modeling tanning along behavioral tendencies using appearance motivation, self-monitoring and the theory of planned behavior. Health Educ Res. 2000;15:405–414. doi: 10.1093/her/15.4.405. [DOI] [PubMed] [Google Scholar]
- 41.Hillhouse J, Turrisi R, Stapleton J, Robinson J. A randomized controlled trial of an appearance-focused intervention to prevent skin cancer. Cancer. 2008;113:3257–3266. doi: 10.1002/cncr.23922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pratt K, Borland R. Predictors of sun protection among adolescents at the beach. Aust Psychol. 1994;29:135–139. doi: 10.1080/00050069408257337. [DOI] [Google Scholar]
- 43.Levy AS, Heaton AW. Weight control practices of U.S. adults trying to lose weight. Ann Intern Med. 1993;119:661–666. doi: 10.7326/0003-4819-119-7_part_2-199310011-00007. [DOI] [PubMed] [Google Scholar]
- 44.Halliwell E, Dittmar H. A qualitative investigation of women’s and men’s body image concerns and their attitudes toward aging. Sex Roles. 2003;49:675–684. doi: 10.1023/B:SERS.0000003137.71080.97. [DOI] [Google Scholar]
- 45.Courtenay WH. Constructions of masculinity and their influence on men’s well-being: A theory of gender and health. Soc Sci Med. 2000;50:1385–1401. doi: 10.1016/S0277-9536(99)00390-1. [DOI] [PubMed] [Google Scholar]
- 46.Mahler HIM, Fitzpatrick B, Parker P, Lapin A. The relative effects of a health-based versus an appearance-based intervention designed to increase sunscreen use. Am J Health Promot. 1997;11:426–429. doi: 10.4278/0890-1171-11.6.426. [DOI] [PubMed] [Google Scholar]
- 47.Janz NK, Becker MH. The Health Belief Model: A decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 48.Gibbons FX, Gerrard M, Lane DJ. A social reaction model of adolescent health risk. In: Suls JM, Wallston KA, editors. Social Psychological Foundations of Health and Illness. Malden: Blackwell; 2003. pp. 107–136. [Google Scholar]
- 49.Azzarello LM, Dessureault S, Jacobsen PB. Sun-protective behavior among individuals with a family history of melanoma. Cancer Epidemiol Biomarkers Prev. 2006;15:142–145. doi: 10.1158/1055-9965.EPI-05-0478. [DOI] [PubMed] [Google Scholar]
- 50.Hall IH, May DS, Lew RA, Koh HK, Nadel M. Sun protection behaviors of the U.S. white population. Prev Med. 1997;26:401–407. doi: 10.1006/pmed.1997.0168. [DOI] [PubMed] [Google Scholar]
- 51.Carmel S, Shani E, Rosenberg L. The role of age and an expanded Health Belief Model in predicting skin cancer protective behavior. Health Educ Res. 1994;9:443–447. doi: 10.1093/her/9.4.433. [DOI] [PubMed] [Google Scholar]
- 52.Woolley T, Buettner PG, Lowe J. Sun-related behaviors of outdoor working men with a history of non-melanoma skin cancer. J Occup Environ Med. 2002;44:847–854. doi: 10.1097/00043764-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 53.Gerrard M, Gibbons FX, Reis-Bergan M, Trudeau L, Vande Lune L, Buunk BP. Inhibitory effects of drinker and non-drinker prototypes on adolescent alcohol consumption. Health Psychol. 2002;21:601–609. doi: 10.1037/0278-6133.21.6.601. [DOI] [PubMed] [Google Scholar]
- 54.Gerrard M, Gibbons FX, Stock ML, Vande Lune LS, Cleveland MJ. Images of smokers and willingness to smoke among African American pre-adolescents: An application of the prototype/willingness model of adolescent health risk behavior to smoking initiation. J Pediatr Psychol. 2005;30:305–318. doi: 10.1093/jpepsy/jsi026. [DOI] [PubMed] [Google Scholar]
- 55.Dennis LK, VanBeek MJ, Beane Freeman LE, Smith BJ, Dawson DV, Coughlin JA. Sunburns and risk of cutaneous melanoma: Does age matter? A comprehensive meta-analysis. Ann Epidemiol. 2008;18:614–627. doi: 10.1016/j.annepidem.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hourani LL, LaFleur B. Predictors of gender differences in sunscreen use and screening outcome among skin cancer screening participants. J Behav Med. 1995;18:461–477. doi: 10.1007/BF01904774. [DOI] [PubMed] [Google Scholar]
- 57.Salas R, Mayer JA, Hoerster KD. Sun-protective behaviors of California farmworkers. J Occup Environ Med. 2005;47:1244–1249. doi: 10.1097/01.jom.0000177080.58808.3b. [DOI] [PubMed] [Google Scholar]
- 58.Mahler HIM, Kulik JA, Gibbons FX, Gerrard M, Harrell J. Effects of appearance-based interventions on sun protection intentions and self-reported behaviors. Health Psychol. 2003;22:199–209. doi: 10.1037/0278-6133.22.2.199. [DOI] [PubMed] [Google Scholar]
- 59.Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869–871. doi: 10.1001/archderm.124.6.869. [DOI] [PubMed] [Google Scholar]
- 60.Afromowitz MA, Van Liew GS, Heimbach DM. Clinical evaluation of burn injuries using an optical reflectance technique. IEEE Trans Biomed Eng. 1987;BME-34:126–127. doi: 10.1109/TBME.1987.326036. [DOI] [PubMed] [Google Scholar]
- 61.Bjerring P, Andersen PH. Skin reflectance spectrophotometry. Photodermatol. 1987;4:167–171. [PubMed] [Google Scholar]
- 62.Levine N, Sheftel SN, Eytan T, et al. Induction of skin tanning by subcutaneous administration of a potent synthetic melanotropin. JAMA. 1991;266:2730–2736. doi: 10.1001/jama.266.19.2730. [DOI] [PubMed] [Google Scholar]
- 63.Himmelfarb S. What do you do when the control group doesn’t fit into the factorial design? Psychol Bull. 1975;82:363–368. doi: 10.1037/0033-2909.82.3.363. [DOI] [Google Scholar]
- 64.Gendolla GHE. College freshmens’ orientation to experts’ personal characteristics after failure and the customary description of others in terms of dispositions. J Appl Soc Psychol. 1999;29:1761–1776. doi: 10.1111/j.1559-1816.1999.tb02049.x. [DOI] [Google Scholar]
- 65.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale: Erlbaum; 1988. [Google Scholar]
- 66.Muthén LK, Muthén BO. Mplus User’s Guide. 4. Los Angeles: Muthén & Muthén; 2007. [Google Scholar]
- 67.Rowe AK, Lama M, Onikpo F, Deming MS. Design effects and intraclass correlation coefficients from a health facility cluster survey in Benin. Int J Qual Health Care. 2002;14:521–523. doi: 10.1093/intqhc/14.6.521. [DOI] [PubMed] [Google Scholar]
- 68.Cafri G, Thompson JK, Roehrig M, et al. Appearance motives to tan and not tan: Evidence for validity and reliability of a new scale. Ann Behav Med. 2008;35:209–220. doi: 10.1007/s12160-008-9022-2. [DOI] [PubMed] [Google Scholar]
- 69.McCaul KD, Mullens AB. Affect, thought, and self-protective health behavior: The case of worry and cancer screening. In: Suls JM, Wallston KA, editors. Social Psychological Foundations of Health and Illness. Malden: Blackwell; 2003. pp. 137–168. [Google Scholar]
- 70.Schmiege SJ, Bryan A, Klein WMP. Distinctions between worry and perceived risk in the context of the theory of planned behavior. J Appl Soc Psychol. 2009;39:95–119. doi: 10.1111/j.1559-1816.2008.00431.x. [DOI] [Google Scholar]