Abstract
Background
This study explores the role of race, ethnicity, and insurance-status in modifying the effects of air pollution on children’s asthma hospitalizations in Phoenix, Arizona (US) between 2001 and 2003. While controlling for weather, interactions between nitrous dioxide (NO2) and race, ethnicity, and insurance-status are used to predict relative risk for subgroups of children.
Methods
The generalized logit regression model for nominal categorical data within a multinomial likelihood framework was used. This model is specifically suited to small counts and the reporting of 95% confidence intervals for the odds–ratio of hospital admission for one group as compared to another. The odds ratio is known to approximate relative risk for rare events.
Results
Several significant findings were found for race, ethnicity, and insurance-status as modulators for the effect of NO2 on children’s risk for asthma hospitalization: (1) Children without insurance have 1.4 (95% CI: 1.1–1.8) times higher risk of asthma admissions than those with private insurance at exceedances of .02 parts per million (ppm) of NO2 above the seasonal mean; the same finding holds for children without insurance as compared to those with Medicaid; (2) Black children have 2.1 (95% CI: 1.3 –3.3) times higher risk of hospitalization than Hispanic children at seasonal mean NO2 levels, but this disproportionate risk shrinks to 1.7 with exceedances of .02 ppm of NO2 above the seasonal mean. Specific to finding (1) among those children without health insurance, Hispanic children have 2.1 (95% CI: 1.1–3.8) times higher risk of hospitalization than white children. Among all Hispanic children, those without health insurance have 1.9 (95% CI: 1.3–3.0) times greater risk than those with private insurance; the same finding holds for Hispanic children without insurance as compared to Hispanic children with Medicaid. Specific to finding (2), among children with private insurance, the disproportionate risk of black children as compared to Hispanic children is magnified by a factor of 1.3 (95% CI: 1.0–1.8) for exceedances of .02 ppm of NO2 above the seasonal mean.
Conclusions
Although we cannot confirm a cause-effect relationship, this analysis suggests that increasing insurance enrollment for all children, and specifically Hispanic children, may reduce their disproportionate risk from exceedances of air pollution. There are few black children in Phoenix, so further studies are needed to investigate the increasing risk of black children with private insurance as compared to Hispanics at exceedances of NO2.
Keywords: Children’s asthma, air pollution, effect modification, race/ethnicity, health insurance status
1. Introduction
Connections between human health effects, specifically asthma, and air pollution have been well-established (Bernstein et al., 2004; Peel et al., 2005). For example, asthma symptoms (Shannon et al., 2004), missed school days due to asthma (Gilliland et al., 2000), emergency room visits (Slaughter et al., 2005), asthma attacks (Ho et al., 2007), and hospitalizations (Lin et al., 2003) have been significantly associated with air pollutants. This research has raised the question: do certain social groups face greater risks than others from environmental conditions? To address this question, researchers have been looking at socio-economic status as an effect modifier between air pollution and health outcomes, usually all-cause mortality or respiratory-related hospitalizations (Burra et al., 2009; Charafeddine and Boden, 2008; Delfino et al., 2002; Gouveia and Fletcher, 2000; Jerrett et al., 2004). A sub-focus within this literature has been how race and ethnicity interact with socio-economic status to modify the relationship between air pollution and health (Burra et al., 2009; Gwynn and Thurston, 2001; Nauenberg and Basu, 1999). This paper builds upon these studies by exploring the role of environmental conditions in predicting differences in relative risk of asthma hospitalizations for racial/ethnic- and insurance status-based groups of children in Phoenix, Arizona (US) using time series methods suitable for nominal categorical data.
Overall, the effect modification literature has focused more on mortality than on respiratory admissions. However, related to both topics, research has suggested a general trend whereby the effects of daily pollution levels are greater for disadvantaged groups when disadvantage is measured at the individual-level (e.g., the patient is uninsured); results are more mixed when disadvantage is operationalized at the community-level (e.g., the patient lives in a low-income neighborhood) (Laurent et al., 2007; O'Neill et al., 2003). These inconsistencies lead authors of a review article to suggest that a “definitive conclusion” that socioeconomic characteristics do modify the effects of pollution on health has not yet been reached (Laurent et al., 2007: 665). The lack of consensus stems in part from the mix of variables used in the literature. There is variability in terms of the representation of socio-economic status, air pollution, and considerations of race; additionally, there is debate regarding explanations for the findings.
Disadvantaged groups (e.g., poor and minority residents) have been hypothesized to have an increased risk from air pollutants for two reasons: they are differentially sensitive to pollution and/or they are differentially exposed to pollution (Lipfert, 2004; O'Neill et al., 2003). Disadvantaged groups may be more sensitive because of a lack of access to health care and/or lower underlying health status that would intensify the effects of pollution. In addition, increased exposure is likely because poorer quality housing allows outdoor air to permeate indoor spaces and low-income people are more likely to occupy homes in less desirable (e.g., more polluted) neighborhoods due to affordability (Lipfert, 2004; O'Neill et al., 2003). Sensitive groups are more likely to face disproportionate exposure, thus the confounding of health status and exposure make it difficult to attribute the increased risk to sensitivity or exposure.
A second issue in the effect modification literature is how to represent socio-economic status (SES). Individual SES is clearly directly related to health status through individual behaviors and access to health care, but at the community-level, SES may pattern a person’s access to health opportunities, like supermarkets, health clinics, and less stressful living situations (O'Neill et al., 2003). In the case of asthma hospitalizations, individual-level health insurance status is particularly meaningful as an indicator of socio-economic status because it maps directly to access to primary care which influences likelihood of asthma hospitalizations (Brotanek et al., 2005; Canino et al., 2006). It has been used in effect modification studies related to asthma (Chang et al., 2009; Gwynn and Thurston, 2001).
In one of the first studies to look at the effect of insurance status on the association between air pollution and asthma hospitalizations, researchers found that in Los Angeles, people on Medicaid were hospitalized at a significantly higher rate than were those without insurance when PM-10 (particles with a diameter of <10 micrometers) levels increased (Nauenberg and Basu, 1999). This finding related to all ages as daily counts were not high enough to consider age groups separately using their method. More recently, researchers found that associations between repeated hospitalizations and residence near heavily trafficked streets were stronger for children without insurance or Medicaid (combined into one category) than they were for privately insured children (Chang et al., 2009).
In addition to the ‘sensitivity versus exposure’ debate and differences in the operationalization of SES, a third issue in the literature is how to represent pollution levels. A common method is to average pollution monitor data across a city (e.g., Charafeddine and Boden, 2008; Forastiere et al., 2007; Gouveia and Fletcher, 2000; Gwynn and Thurston, 2001; Zanobetti and Schwartz, 2000) and assume that all residents in the city are equally exposed to pollution (Lipfert, 2004). To improve on this assumption, some researchers select only the patients that live near pollution monitors for their study (Martins et al., 2004) or use the monitors to model a spatially explicit pollution surface mapping to seasonal exposure (Delfino et al., 2009). Either method can be difficult to employ in some contexts as urban pollution monitoring networks can be sparse. For example, researchers had only two PM-10 monitors to use in their study of Rome (Forastiere et al., 2007).
Furthermore, there is a lack of consensus surrounding how to summarize daily 24-hour measurements of pollutants. While PM (particulate matter) is more commonly studied in effect modification studies, several studies have also looked at NO2, as we do in this study. Different methods are used to create a daily NO2 value. Burra et al. (2009) relied on two NO2 monitors to calculate a daily NO2 variable. They created an hourly average across both monitors, and then took the maximum averaged hourly reading for each day. Delfino et al. (2003), while not an effect modification study per se, used the one hour maximum to represent NO2 from the one monitor used in their study of Hispanic children and air pollution. A limitation in either approach is that the hourly profile of NO2 varies from day to day with the maximum reading occurring at different times of day. This means that maximum opportunity for exposure occurs at different times of day and given that a child’s daily trajectory is relatively patterned (e.g., inside during school hours), he/she may or may not be outside during the peak exposure period on any given day.
Considerations of race have been scant in the effect modifications literature (see Delfino et al., 2009; Gwynn and Thurston, 2001). This is in spite of race being an important focus in the asthma inequalities literature as racial and ethnic disparities are well documented. According to the US Center for Disease Control and Prevention, in the US, African Americans have asthma prevalence rates (9.5 per 10,000) that are 25% higher than whites (7.4 per 10,000) and asthma hospitalization rates that are 240% greater than the rate for whites. Hispanics have asthma prevalence rates that are 6.2 per 10,000 in the population (Akinbami, 2007).
The lack of focus on race in the effect modification studies is in part because many of the effect modification studies are done outside of the US where race is not a standard category on medical forms. The results of race/asthma effect modification studies are mixed. Researchers in New York City used pollution and weather covariates in negative binomial regression models for subgroups (Gwynn and Thurston, 2001). Combining all age groups, they found that risk estimates for minorities were higher than for non-Hispanic whites, but the difference was not statistically significant. They then controlled for insurance status and concluded that the small race difference in pollutant risk estimates was explained by insurance status; those with Medicaid/no insurance (combined into one group) had a higher risk than those with private insurance/Medicare (combined into one group) (Gwynn and Thurston, 2001). Most recently, a study using recurrent event proportional hazards models found no significant differences in risk of repeated asthma hospitalizations between white and Hispanic children associated with exposure to seasonal (not daily) traffic pollution, but significantly lower risk for Asian/black/Native American children as compared to whites (Delfino et al., 2009).
Given our focus on asthma hospitalizations in children, this study builds upon previous work in four ways. First, we consider race and ethnicity by disaggregating black and Hispanic children into separate groups instead of combining them into one minority category. Second, we consider health insurance at the individual-level and disaggregate Medicaid from no insurance, an important consideration since they do not imply the same access to health care. Third, instead of aggregating hourly pollution into one daily value, we divide each day into three time periods, which allows us to record the maximum value within each time period, thus doing a better job of standardizing exposure. Fourth, we utilize a method that is suited to small counts and readily provides 95% confidence intervals for group risk comparisons. This method allows us to disaggregate race and insurance to a greater degree than previous studies (Chang et al., 2009; Gwynn and Thurston, 2001). Small counts have been noted as a limitation, most recently by Chang el al. (2009); they combined public insurance and self-pay (no insurance) into one insurance category when using a proportional hazard modeling strategy. Our method allows us to directly model relative risk, as opposed to modeling risk for each sub-group separately (such as was done by Gwynn and Thurston, 2001).
Specifically, we use an omnibus regression model for nominal categorical data within a multinomial likelihood framework for reporting of relative risk of hospital admission for one group as compared to another (e.g., Hispanic children to white children). However, we are forced to make the assumption that all children are equally exposed to pollution in Phoenix. Given the limited number of monitoring stations, the study would not be possible if we only selected children in neighborhoods near the stations, as was done by Martins et al. (2004). In addition, we model relative risk instead of attributable risk (Gwynn and Thurston, 2001). In other words, our focus is on which social groups are at greater risk, as opposed to which groups comprised the majority of the number of cases related to a given exposure. The following research questions are answered:
Does insurance status modify the effect of daily NO2 levels on relative risk of asthma hospitalization? (To answer this question, we will examine corrected intercepts and slopes in the regression model including environmental variables modulated by insurance status.)
Do race and ethnicity modify the effect of daily NO2 levels on relative risk of asthma hospitalization? (To answer this question, we will examine corrected intercepts and slopes in the regression model including environmental variables modulated by race/ethnicity.)
How do race, ethnicity and insurance status interact to modify the effect of daily NO2 levels on relative risk of asthma hospitalization? (To answer this question, we will examine slopes in the regression model including environmental variables modulated by insurance status within race/ethnicity, and by race/ethnicity within insurance status.)
2. Materials & Methods
2.1 Asthma data
Asthma hospitalization data were obtained from the Arizona Department of Health Services. Patients included are those who spent at least one night in the hospital with asthma as a primary diagnosis (ICD-code 493) between 1 January 2001 and 31 December 2003, had an address in metro Phoenix (Maricopa County), and were aged fourteen or under. For each patient, race/ethnicity and payer was recorded. We used Caucasian-Not Hispanic, Hispanic-Caucasian, and black as our racial/ethnic categories as they represent the three largest racial-ethnic groups in Maricopa County (Bureau of the US Census, 2000). This method of identifying Hispanic patients undercounts their true number, as Hispanic is an ethnic category and can be associated with all racial groups. At the hospital, “Hispanic” is recorded as the racial/ethnic category only if the person is also white so this method does not allow for Black-Hispanic persons. However, 83% of Phoenix’s Hispanic population is of Mexican decent and therefore usually racially white (Bureau of the US Census, 2000). We recoded the thirteen payer categories into three categories (see Johnson et al., 2007) for analysis: uninsured, privately insured, and Medicaid (including State Children’s Health Insurance Program or SCHIP). The federal government created SCHIP in 1997 to cover low-income children who did not qualify for Medicaid. Whereas households on Medicaid do not pay a monthly fee or co-payments for medications and visits to the doctor, SCHIP households have slightly higher incomes and pay a monthly fee based on a sliding income scale; medications and co-pays are still free (State of Arizona, 2005). In Arizona, both are managed care plans that contract with the same providers.
Asthma hospitalization data do not map directly to asthma prevalence rates nor do they include visits to the emergency room or to a primary care provider for asthma. Instead, hospitalization data can be used as a proxy for uncontrolled asthma. In most cases, it is possible to successfully control asthma with medications and regular healthcare; most such patients are never hospitalized (American Academy of Pediatrics, 1999).
2.2 Environmental data
Pollution data (i.e., NO2, PM-10, PM-2.5, Ozone, CO, and SO2) were obtained from the Arizona Department of Environmental Quality for the study period. We began the study with the aim of using six pollution variables, but were restricted to only NO2 and ozone because of data quality issues (i.e., only seasonal monitoring, inconsistent monitoring, or only one monitoring station). For clarity, only the findings for nitrogen dioxide (NO2) are presented here. NO2 is thought to cause respiratory and cardiovascular disease (EPA, 2000) and is an important precursor to ground level ozone. It has been linked to asthma in time-series studies (Migilaretti and Cavallo, 2004; Peel et al., 2005) and has been used as an indicator of traffic-related pollution (Migilaretti and Cavallo, 2004; Scoggins et al., 2004). The US Environmental Protection Agency identifies it as a public health concern as an irritant that exacerbates existing respiratory symptoms and triggers asthma (EPA, 2005).
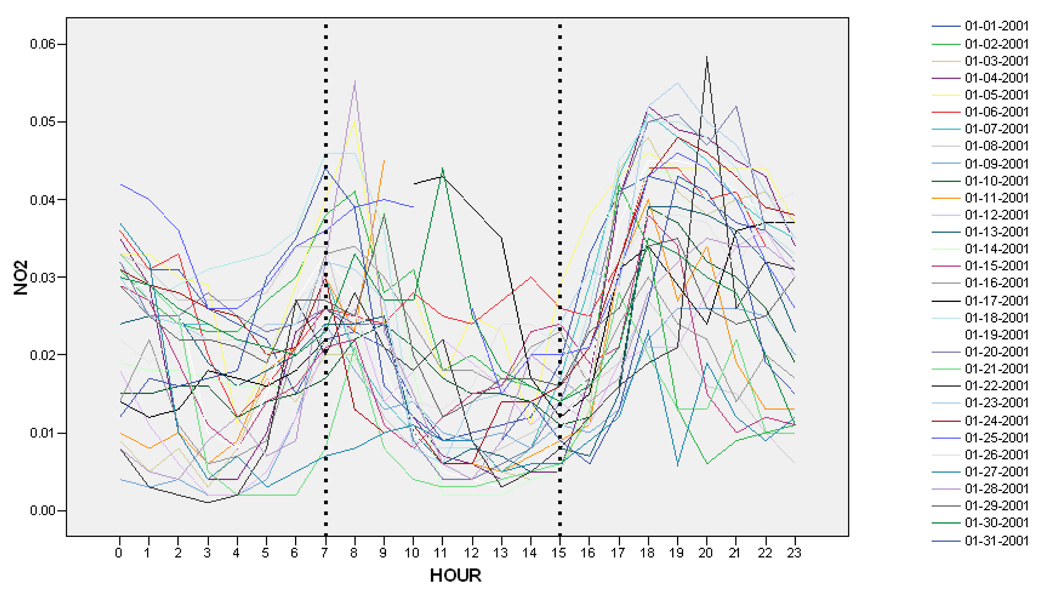
We created three NO2 variables by partitioning the 24-hour day into three equal segments (see Figure 1 for illustration of daily profiles for January 2001) because the shape of the 24-hour profiles of NO2 were not stable from day to day in that the daily peak occurred at different times (see Table 1). If we had created an hourly average across monitors, we would have lost the temporal specificity in the peaks. For this reason, we averaged the maximum reading across the four stations providing NO2 in ppm (parts per million) in Maricopa County within each of the three time-periods (i.e., (1) midnight-7 am, (2) 8 am-3 pm, (3) 4 pm-11 pm); the averaged maximum hourly reading was largest in time period one 305 times, in time period two 91 times and in time period three 571 times. At first, we ran our statistical analysis for all three time periods using variable selection methods, but in the final analysis we selected time period three (i.e., evening levels from 4 pm – 11 pm) as our focus because children are not in school and more likely to be playing outside during this time.
Figure 1.
Hourly levels NO2 from the South Scottsdale monitor for January 2001 divided into three time periods
Table 1.
Number of daily hourly-maximum readings occurring in the three time periods for each of the four NO2 monitors, 2001–2003
| Pollution Monitor |
Time period | Count of daily hourly- maximums occurring in each time period |
Percent | Missing Maximums |
|---|---|---|---|---|
| Midnight - 7 am | 338 | 33.7 | ||
| Central Phoenix |
8 am - 3 pm | 92 | 9.2 | |
| 4 pm - 11 pm | 573 | 57.1 | ||
| 92 | ||||
| Midnight - 7 am | 392 | 39.9 | ||
| Green- wood |
8 am - 3 pm | 185 | 18.8 | |
| 4 pm - 11 pm | 405 | 41.2 | ||
| 113 | ||||
| Midnight - 7 am | 199 | 20.6 | ||
| South Scottsdale |
8 am - 3 pm | 61 | 6.3 | |
| 4 pm - 11 pm | 706 | 73.1 | ||
| 129 | ||||
| Midnight - 7 am | 306 | 30.7 | ||
| West Phoenix |
8 am - 3 pm | 96 | 9.6 | |
| 4 pm - 11 pm | 596 | 59.7 | ||
| 97 | ||||
We then accounted for seasonality in NO2 using a trigonometric filter that removed all cycles with periods of 1–23 months. Our use of residuals assumes that the odds ratio; i.e., the relative risk for subgroups, see equations [1, 2] of the appendix, does not vary seasonally beyond the effects accounted for by the weather variables. It is assumed that the effect of day-of-week cancels out of the odds ratio. In the results, we refer to the positive NO2 residuals as ``exceedances of NO2”, i.e., positive deviations from the time series predicted by the regression model for NO2. Exceedances of NO2 correspond to exposures above the seasonal mean. The 95th percentile of the NO2 residuals is .02 ppm and these high levels occur about 18 days per year. In the ensuing discussions of relative risk, the regression coefficients for the NO2 residuals will be interpreted at NO2 exceedances of .02 ppm.
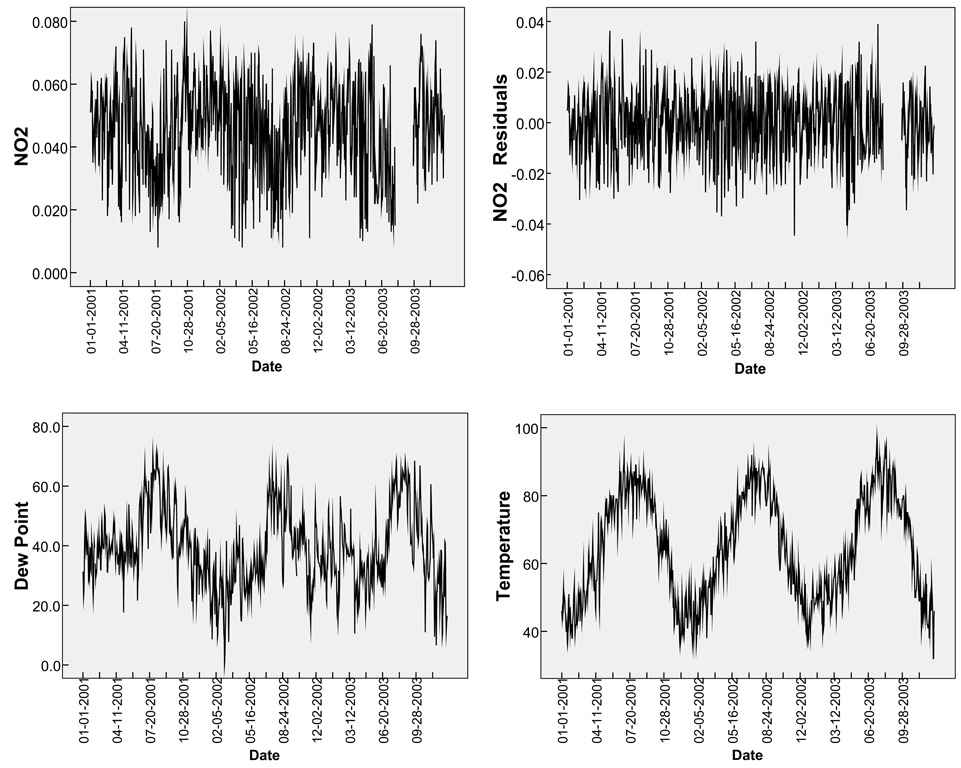
For the weather variables, we obtained daily minimum temperature (see Farhat et al., 2005) and dew point in degrees Fahrenheit from the Arizona State Office of Climatology official observation location at the Phoenix Sky Harbor International Airport. These variables were input directly into the models in raw form. Descriptive statistics of all variables under analysis are included in Table 2; times-series plots of temperature, dew point, NO2, and NO2 residuals are found in Figure 2.
Table 2.
Descriptive statistics for variables in analysis
| Variables | N | Min. | 25th Percentile |
Mean | Median | 75th Percentile |
Max. | Total Admits |
|---|---|---|---|---|---|---|---|---|
| NO2 (evening) [parts per million] | 1040 | 0.008 | 0.036 | 0.046 | 0.047 | 0.057 | 0.079 | N/A |
| Dew Point [Fahrenheit] | 1092 | 0.1 | 30.4 | 39.132 | 38 | 47.15 | 71.3 | N/A |
| Temperature [Fahrenheit] | 1095 | 32 | 51 | 64.507 | 64 | 79 | 96 | N/A |
| Black Admits | 1095 | 0 | 0 | 0.580 | 0 | 1 | 6 | 635 |
| Hispanic Admits | 1095 | 0 | 0 | 1.328 | 1 | 2 | 9 | 1454 |
| White Admits | 1095 | 0 | 1 | 2.034 | 2 | 3 | 11 | 2227 |
| Private Admits | 1095 | 0 | 1 | 2.290 | 2 | 3 | 11 | 2508 |
| No Insurance Admits | 1095 | 0 | 0 | 0.187 | 0 | 0 | 2 | 205 |
| Medicaid Admits | 1095 | 0 | 1 | 1.840 | 1 | 3 | 10 | 2015 |
| Black Medicaid Admits | 1094 | 0 | 0 | 0.287 | 0 | 0 | 3 | 314 |
| Hispanic Medicaid Admits | 1094 | 0 | 0 | 0.748 | 0 | 1 | 5 | 818 |
| White Medicaid Admits | 1094 | 0 | 0 | 0.555 | 0 | 1 | 6 | 607 |
| Black No Insurance Admits | 1094 | 0 | 0 | 0.017 | 0 | 0 | 1 | 19 |
| Hispanic No Insurance Admits | 1094 | 0 | 0 | 0.078 | 0 | 0 | 2 | 85 |
| White No Insurance Admits | 1094 | 0 | 0 | 0.076 | 0 | 0 | 2 | 83 |
| Black Private Admits | 1093 | 0 | 0 | 0.247 | 0 | 0 | 5 | 270 |
| Hispanic Private Admits | 1093 | 0 | 0 | 0.471 | 0 | 1 | 5 | 515 |
| White Private Admits | 1093 | 0 | 0 | 1.317 | 1 | 2 | 9 | 1439 |
Figure 2.
Time-series plots of NO2, NO2 residuals, temperature (minimum), and dew point, 2001–2003.
Note: Positive residuals of NO2 are referred to as exceedances of NO2 in the discussion of the results.
2.3 Statistical methods
We use the generalized logit regression model for nominal data that generalizes logistic regression to responses with more than two categories (Agresti 1990). The probability distribution of race/ethnicity given a hospital admission event is estimated with the generalized logit regression model and then related back to the probability of an event given race/ethnicity by the definition of conditional probability (Fears and Brown, 1986). This is explained in the appendix. The same approach is used when the observational response is the insurance status or the intersection of insurance status and race/ethnicity. The generalized logit models were fitted using Proc Logistic with link=logit available in the SAS® 9.21 software. We forced temperature and dew point terms into the model, while allowing for backward variable selection to pick the best fitting NO2 lag variables (0-, 1-, 2-, 3-day lags) at a 0.2 significance level. Lagged terms take into account the time it may take for persons to mount an immune response to a pollution trigger (Peel et al., 2005; Thompson et al., 2001). In some models, NO2 was not selected as a predictor variable and in others more than one NO2 lag was selected. For significant findings related to our research questions, we report 95% Wald confidence intervals for relative risk. While we ran semi-parametric models (that included temperature and dew point nonparametrically by fitting additive cubic B-splines, including NO2 with lags as linear terms), we only report results from a fully parametric analysis (including temperature, dew point, and NO2 as linear terms) because the findings agreed.
Specifically related to the first two research questions, we corrected the intercepts reported by SAS (see equation [5] in the appendix) for the population of the group in order to investigate differences between race/ethnicity and insurance groups at seasonal mean levels of NO2. We obtained populations for race and ethnicity from the 2000 US Census (Bureau of the US Census, 2000). Populations for insurance groups were obtained using the Health Query database maintained at Arizona State University and the mandatory admissions method of calculating insurance rates (see Johnson et al., 2007 for discussion of method used). These population counts are not needed to interpret the slopes (see discussion in the appendix regarding equation [4]), and were not available for insurance status by race and ethnicity (e.g., Black Medicaid). Group populations are available in Table 3.
Table 3.
Population counts for race, ethnicity, and insurance groups in Maricopa County, 2000
| Group | Population |
|---|---|
| Black Children | 32264 |
| Hispanic Children | 132442 |
| White Children | 395314 |
| Children with Private Insurance | 290489 |
| Children without Insurance | 28838 |
| Children with Medicaid | 359418 |
The method of analysis selected, generalized logit regression for nominal data, uses a multinomial likelihood that accounts for the correlation between the hospital admission event counts by ethnicity/race or by insurance status, while allowing for simultaneous fitting of the model parameters in such a way as to directly obtain the estimates of relative risk of asthma-related hospital admission, for example, of Hispanic to white (Begg and Gray, 1984). Furthermore, the generalized logit model for nominal data is better suited to cities like Phoenix where the daily counts are small. The multinomial model is likelihood equivalent to a Poisson log-linear model (Chen and Kuo, 2001; Palmgren, 1981) including race/ethnicity or insurance status as factors with certain nuisance parameters conditioned out.
3. Results
Results will be presented as answers to the research questions. Only results significant at the .05 level of significance (p<.05) are discussed. When race, ethnicity or insurance-status significantly modify the effect of NO2, we report relative risk (RR) and corresponding 95% Wald confidence intervals for .02 ppm of NO2 exceedance above the seasonal mean. When corrected intercepts are presented, they can be interpreted as the RR at the seasonal mean of NO2 when the matching slope is also significant. If the matching slope is not significant, then the corrected intercept can be interpreted as the RR across all levels of NO2. If the intercept is not significant, but the matching slope is, then the slope can be used to determine RR when levels of NO2 exceed the seasonal mean. Refer to the appendix for additional information about how to interpret the coefficients.
3.1 Does insurance status modify the effect of daily NO2 levels on relative risk of asthma hospitalization?
To answer this question, we interpret the insurance-modulated NO2 corrected intercepts and slopes in the regression models presented in Table 4-A.
Table 4.
Relative risk associated with changes in environmental conditions: Children’s insurance-status (A) and race/ethnicity (B)
| Parameter | b | SE | p | RR3 | LCI | UCI | ||
|---|---|---|---|---|---|---|---|---|
| A | Intercept | Medicaid* | −0.556 | 0.142 | 0.000 | 0.57 | 0.43 | 0.76 |
| Intercept | No Insurance* | −0.506 | 0.352 | 0.151 | ||||
| Intercept | No Insurance+ | 0.050 | 0.355 | 0.887 | ||||
| Temperature | Medicaid* | 0.004 | 0.003 | 0.116 | ||||
| Temperature | No Insurance* | −0.001 | 0.007 | 0.919 | ||||
| Temperature | No Insurance+ | −0.005 | 0.007 | 0.466 | ||||
| Dew Point | Medicaid* | −0.003 | 0.003 | 0.306 | ||||
| Dew Point | No Insurance* | 0.009 | 0.008 | 0.310 | ||||
| Dew Point | No Insurance+ | 0.012 | 0.009 | 0.160 | ||||
| NO2 Lag 1 | Medicaid* | 0.321 | 2.585 | 0.901 | ||||
| NO2 Lag 1 | No Insurance* | 16.490 | 6.724 | 0.014 | 1.39 | 1.07 | 1.81 | |
| NO2 Lag 1 | No Insurance+ | 16.169 | 6.773 | 0.017 | 1.38 | 1.06 | 1.80 | |
| Reference group: Private* | ||||||||
| Reference group: Medicaid+ | ||||||||
| B | Intercept | Black* | 0.813 | 0.219 | 0.000 | 2.25 | 1.47 | 3.46 |
| Intercept | Hispanic* | 0.083 | 0.164 | 0.611 | ||||
| Intercept | Black+ | 0.729 | 0.231 | 0.002 | 2.07 | 1.32 | 3.26 | |
| Temperature | Black* | 0.004 | 0.004 | 0.304 | ||||
| Temperature | Hispanic* | 0.009 | 0.003 | 0.004 | ||||
| Temperature | Black+ | −0.005 | 0.004 | 0.278 | ||||
| Dew Point | Black* | 0.005 | 0.005 | 0.276 | ||||
| Dew Point | Hispanic* | 0.002 | 0.004 | 0.580 | ||||
| Dew Point | Black+ | 0.003 | 0.005 | 0.526 | ||||
| NO2 Lag 0 | Black* | −6.488 | 3.915 | 0.098 | ||||
| NO2 Lag 0 | Hispanic* | 2.539 | 2.965 | 0.392 | ||||
| NO2 Lag 0 | Black+ | −9.026 | 4.130 | 0.029 | 0.83 | 0.71 | 0.98 | |
| Reference group: White* | ||||||||
| Reference group: Hispanic+ | ||||||||
Notes: (1) Intercepts are corrected for population. (2) Models were run separately for each of the two reference groups but are combined for ease of interpretation. (3) RR (relative risk), LCI (lower confidence interval) and UCI (upper confidence interval) are reported for the variables of interest. For the intercepts, LCI and UCI are the upper and lower 95% Wald confidence bounds for RR=exp(b) of specified subgroups at seasonal mean NO2, predicted by the time series regression model. For the slopes, LCI and UCI are the upper and lower 95% Wald confidence bounds for the RR of specified subgroups at .02 ppm of NO2 exceedance.
Related to insurance status, risk estimates for asthma hospital admissions were 0.57 (95% CI: .43–.76) times lower for children with Medicaid as compared to children with private insurance across all levels of NO2. Therefore, relative risk estimates did not depend on NO2 for children with Medicaid as compared with private insurance.
Risk estimates for asthma hospital admissions at .02 ppm of exceedance in NO2 were 1.39 (95% CI: 1.07–1.81) times greater for children without insurance as compared to children with private insurance, and 1.38 (95% CI: 1.06–1.80) times greater for children without insurance as compared to children with Medicaid. Therefore, relative risk estimates did depend on NO2 for these groups.
3.2 Do race and ethnicity modify the effect of daily NO2 levels on relative risk of asthma hospitalization?
To answer this question, we interpret the race and ethnicity-modulated slopes for NO2 and correct the intercepts slopes in the regression models presented in Table 4-B.
Risk estimates for asthma hospital admissions were 2.25 (95% CI: 1.47–3.46) times greater for black children as compared to white children across all levels of NO2. Therefore RR estimates did not depend on NO2 for black children as compared to white children.
Risk estimates for asthma hospital admissions were 2.07 (95% CI: 1.32–3.26) times greater for black children as compared to Hispanic children at seasonal mean levels of NO2. However, risk estimates shrink by a factor of .83 (95% CI: .71–.98) for black children as compared to Hispanic children at a pollution exposure of .02 ppm of NO2 exceedance. Therefore, relative risk estimates did depend on NO2 for black children as compared to Hispanic children.
Relative risk estimates for asthma hospital admissions did not depend on NO2 for white children as compared to Hispanic children.
3.3 How do race, ethnicity and insurance status interact to modify the effect of daily NO2 levels on relative risk of asthma hospitalization?
To answer this question, we interpret the insurance-modulated NO2 slopes for each racial/ethnic group in the regression models presented in Table 5 and the race and ethnicity-modulated NO2 slopes for each insurance group in the regression models presented in Table 6.
Table 5.
Relative risk associated with changes in environmental conditions: Children’s race/ethnicity by Medicaid (A), private insurance (B) and no insurance (C)
| Parameter | b | SE | p | RR3 | LCI | UCI | |||
|---|---|---|---|---|---|---|---|---|---|
| A | Temperature | Black Medicaid* | 0.005 | 0.006 | 0.411 | ||||
| Temperature | Hispanic Medicaid* | 0.012 | 0.005 | 0.013 | |||||
| Temperature | Black Medicaid+ | −0.007 | 0.006 | 0.243 | |||||
| Dew Point | Black Medicaid* | 0.013 | 0.007 | 0.088 | |||||
| Dew Point | Hispanic Medicaid* | 0.001 | 0.006 | 0.881 | |||||
| Dew Point | Black Medicaid+ | 0.012 | 0.007 | 0.094 | |||||
| Reference: White Medicaid* | |||||||||
| Reference: Hispanic Medicaid+ | |||||||||
| B | Temperature | Black Private* | 0.006 | 0.006 | 0.323 | ||||
| Temperature | Hispanic Private* | 0.008 | 0.005 | 0.099 | |||||
| Temperature | Black Private+ | −0.002 | 0.007 | 0.808 | |||||
| Dew Point | Black Private* | −0.005 | 0.007 | 0.533 | |||||
| Dew Point | Hispanic Private* | 0.001 | 0.006 | 0.886 | |||||
| Dew Point | Black Private+ | −0.005 | 0.008 | 0.517 | |||||
| NO2 Lag 1 | Black Private* | −11.909 | 5.950 | 0.045 | 0.79 | 0.62 | 1.00 | ||
| NO2 Lag 1 | Hispanic Private* | −4.323 | 4.707 | 0.359 | |||||
| NO2 Lag 1 | Black Private+ | −7.587 | 6.735 | 0.260 | |||||
| NO2 Lag 2 | Black Private* | 11.852 | 6.346 | 0.062 | 1.27 | 0.99 | 1.63 | ||
| NO2 Lag 2 | Hispanic Private* | −2.919 | 4.685 | 0.533 | |||||
| NO2 Lag 2 | Black Private+ | 14.771 | 7.090 | 0.037 | 1.34 | 1.02 | 1.77 | ||
| Reference: White Private* | |||||||||
| Reference: Hispanic Private+ | |||||||||
| C | Temperature | Black No Insurance* | 0.051 | 0.024 | 0.031 | ||||
| Temperature | Hispanic No Insurance* | 0.032 | 0.015 | 0.038 | |||||
| Temperature | Black No Insurance+ | 0.020 | 0.023 | 0.393 | |||||
| Dew Point | Black No Insurance* | 0.020 | 0.030 | 0.499 | |||||
| Dew Point | Hispanic No Insurance* | 0.025 | 0.020 | 0.200 | |||||
| Dew Point | Black No Insurance+ | −0.005 | 0.030 | 0.876 | |||||
| NO2 Lag 0 | Black No Insurance* | 8.890 | 22.485 | 0.693 | |||||
| NO2 Lag 0 | Hispanic No Insurance* | 36.206 | 15.340 | 0.018 | 2.06 | 1.13 | 3.76 | ||
| NO2 Lag 0 | Black No Insurance+ | −27.316 | 21.840 | 0.211 | |||||
| Reference: White No Insurance* | |||||||||
| Reference: Hispanic No Insurance+ | |||||||||
Notes: (1) Intercepts are not shown because they need to be corrected based on group population, but those numbers are not available, and therefore are not interpretable. (2) Models were run separately for each of the two reference groups but are combined into one table for ease of interpretation. (3) RR (relative risk) and its LCI (lower confidence interval) and UCI (upper confidence interval) are reported for the variables of interest. For the slopes, LCI and UCI are the upper and lower 95% Wald confidence bounds for the RR of specified subgroups at .02 ppm of NO2 exceedance.
Table 6.
Relative risk associated with changes in environmental conditions: Children’s insurance status by black (A), Hispanic (B) and white (C)
| Parameter | b | SE | p | RR3 | LCI | UCI | |||
|---|---|---|---|---|---|---|---|---|---|
| A | Temperature | Black Medicaid* | −0.001 | 0.008 | 0.855 | ||||
| Temperature | Black No Insurance* | 0.024 | 0.022 | 0.279 | |||||
| Temperature | Black No Insurance+ | 0.025 | 0.022 | 0.249 | |||||
| Dew Point | Black Medicaid* | 0.010 | 0.009 | 0.286 | |||||
| Dew Point | Black No Insurance* | 0.028 | 0.028 | 0.302 | |||||
| Dew Point | Black No Insurance+ | 0.019 | 0.027 | 0.495 | |||||
| NO2 Lag 2 | Black Medicaid* | −8.469 | 7.204 | 0.240 | |||||
| NO2 Lag 2 | Black No Insurance* | 29.626 | 23.809 | 0.213 | |||||
| NO2 Lag 2 | Black No Insurance+ | 38.095 | 23.683 | 0.108 | |||||
| Reference: Black Private* | |||||||||
| Reference: Black Medicaid+ | |||||||||
| B | Temperature | Hispanic Medicaid* | 0.004 | 0.005 | 0.473 | ||||
| Temperature | Hispanic No Insurance* | 0.004 | 0.011 | 0.738 | |||||
| Temperature | Hispanic No Insurance+ | 0.000 | 0.011 | 0.997 | |||||
| Dew Point | Hispanic Medicaid* | −0.006 | 0.006 | 0.320 | |||||
| Dew Point | Hispanic No Insurance* | 0.021 | 0.014 | 0.150 | |||||
| Dew Point | Hispanic No Insurance+ | 0.027 | 0.014 | 0.055 | |||||
| NO2 Lag 1 | Hispanic Medicaid* | 1.079 | 4.691 | 0.818 | |||||
| NO2 Lag 1 | Hispanic No Insurance* | 33.164 | 11.012 | 0.003 | 1.94 | 1.26 | 2.99 | ||
| NO2 Lag 1 | Hispanic No Insurance+ | 32.085 | 10.775 | 0.003 | 1.90 | 1.25 | 2.90 | ||
| Reference: Hispanic Private* | |||||||||
| Reference: Hispanic Medicaid+ | |||||||||
| C | Temperature | White Medicaid* | −0.002 | 0.004 | 0.622 | ||||
| Temperature | White No Insurance* | −0.014 | 0.011 | 0.191 | |||||
| Temperature | White No Insurance+ | −0.012 | 0.011 | 0.282 | |||||
| Dew Point | White Medicaid* | −0.004 | 0.005 | 0.494 | |||||
| Dew Point | White No Insurance* | −0.008 | 0.013 | 0.512 | |||||
| Dew Point | White No Insurance+ | −0.005 | 0.013 | 0.724 | |||||
| NO2 Lag 0 | White Medicaid* | 3.513 | 4.286 | 0.412 | |||||
| NO2 Lag 0 | White No Insurance* | −16.204 | 10.086 | 0.108 | |||||
| NO2 Lag 0 | White No Insurance+ | −19.716 | 10.460 | 0.059 | |||||
| Reference: White Private* | |||||||||
| Reference: White Medicaid+ | |||||||||
Notes: (1) Intercepts are not shown because they need to be corrected based on group population, but those numbers are not available, and therefore are not interpretable. (2) Models were run separately for each of the two reference groups but are combined into one table for ease of interpretation. (3) RR (relative risk) and its LCI (lower confidence interval) and UCI (upper confidence interval) are reported for the variables of interest. For the slopes, LCI and UCI are the upper and lower 95% Wald confidence bounds for the RR of specified subgroups at .02 ppm of NO2 exceedance.
Among all children with Medicaid, there were no racial or ethnic differences in risk for asthma hospital admissions associated with NO2 (Table 5-A).
Among all children with private insurance, the risk estimate for asthma hospital admissions at the seasonal mean NO2 at lag 1, as predicted by the time series regression model, was 0.79 (95% CI: .62–1.00) times lower for black children when compared to white children (Table 5-B). However, although not significant at lag 2, the sign of the coefficient reverses so that the relative risk becomes 1.27 (95% CI: .99–1.63) times higher for black children as compared to white children (Table 5-B). This change in sign in the regression coefficient of NO2 effectively cancels out the significant finding. The combined RR (calculated by multiplying the RR for lag 1 and lag 2 at the seasonal mean of NO2) is .96 or about one. To investigate this sign switch, we tried combining lag 1 and lag 2 using cumulative NO2 averages over lags 0, 1, and 2, as per Burra et al (2009). When doing so (table not shown), the result for black-private as compared to white-private was not significant (p=.44). This supplementary analysis supports our assertion that the relationship is not significant.
Among all children without insurance, risk estimates associated with .02 ppm of NO2 exceedance were 2.06 (95% CI: 1.13–3.76) times greater for Hispanic children as compared to white children (Table 5-C).
Among all black children, there were no insurance-based differences in risk for asthma hospital admissions associated with NO2 (Table 6-A).
Among Hispanic children, risk estimates associated with .02 ppm of NO2 exceedance were 1.94 (95% CI: 1.26–2.99) times greater for children without insurance as compared to children with Medicaid and 1.90 (95% CI: 1.25–2.90) times greater for children without insurance as compared to children with private insurance (Table 6-B).
Among all white children, there were no insurance-based differences in risk for asthma hospital admissions associated with NO2 (Table 6-C).
4. Discussion
Our findings compliment previous research and shed light on open questions2. Given our focus on access to care through the proxy of insurance status, this paper suggests that having access to care modifies the effect of NO2 on children’s asthma hospitalizations. Associated with NO2 exceedances (Table 4-A), we found that children without insurance had greater risk than insured (i.e., private and Medicaid) children. Unlike Gwynn and Thurston (2001) and Chang et al (2009) who combined those with Medicaid and those without insurance into one category of poor people, our analysis strategy enabled us to disaggregate poor children into two groups that differ in term of access to care: those without insurance and those with Medicaid. This was important because poor children with Medicaid are more likely than poor children without health insurance to receive regular health care including asthma medications, which reduce hospitalizations (Fisher and Mascarenhas, 2007). Given that we find that children without insurance have greater risk than those with Medicaid associated with NO2 exceedances, it seems as if access to care might override some of the deleterious effects of poverty. Research has also shown that using asthma medications can mediate the respiratory effects of pollution (Delfino et al., 2002), so the higher risk faced by uninsured children may relate to the fact that the uninsured are less likely to receive regular asthma care, which is necessary to prevent hospitalizations (American Academy of Pediatrics, 1999).
Considering the effects of race and ethnicity within insurance status, we first found higher risk for Hispanic children without insurance related to NO2 exceedances above the seasonal mean. Not having insurance is closely linked to immigration status in the US (Lessard and Ku, 2003), and it affects Hispanic children the most (Flores and Tomany-Korman, 2008). Specifically, we found that (1) Hispanic children without insurance had higher risk than Hispanic children with insurance (both private and Medicaid) (Table 6-B) and (2) out of all uninsured children, Hispanics had a higher risk than did white children (Table 5-C). Because other studies have focused on blacks versus whites (e.g., Zanobetti and Schwartz, 2000), combined black and Hispanics into one “minority” category (e.g., Gwynn and Thurston, 2001), or combined people with Medicaid and no insurance into one group (e.g., Chang et al., 2009; Gwynn and Thurston, 2001), the increased risk for Hispanics without insurance has been missed. It may not be expected in light of other studies reporting that Hispanics of Mexican decent have lower prevalence rates of asthma than non-Hispanic whites (Akinbami, 2007). However, of all race/ethnicity-insurance groups studied, Hispanics without insurance face a number of access to care challenges, including financial barriers, a lack of health care coverage, coverage limitations, transportation barriers, culture differences, language barriers, and a lack of continuity of care (Berg et al., 2004; Brotanek et al., 2005; Brousseau et al., 2005; Lara et al., 1999). It is likely that these barriers to regular primary care influence risk for uninsured Hispanic children. Second, we found that Medicaid was an equalizer related to risk of hospitalization associated with NO2 exceedances. We found no significant (or even nearly significant) differences between Hispanic, black and white children with Medicaid associated with NO2 exceedances above the seasonal mean (Table 5-A).
Related to race and ethnicity (independent of insurance status), the most notable finding was the higher risk of black children at seasonal mean NO2 as compared with Hispanic children, and then how this disproportionate risk shrinks with increasing NO2 exceedances. This demonstrates that the while black children’s risk of hospitalization remains high, Hispanic children’s risk starts to catch up to black children’s when daily levels of NO2 are high. This sensitivity to higher levels of pollution for Hispanic children may relate to lower rates of access to health care, as discussed above.
Considering the effect of insurance within racial and ethnic groups, the shrinking gap between black and Hispanic children is not found among those with private insurance. Instead, among children with private insurance, the disproportionate risk of black children as compared to Hispanic children is magnified for exceedances of .02 ppm of NO2 above the seasonal mean (Table 5-B). The ethnic composition of Phoenix – with low percentages of blacks and higher percentages of Hispanics – may play a role in this relationship. In a nationally representative study, Haas et al (2004) found that the ethnic make-up of one’s county influenced perceptions of access to care. When blacks lived in counties with lower percentages of blacks, they reported more barriers to accessing health care in terms of difficulties and financial barriers than when they lived in counties with higher percentages of blacks. A related, but weaker, relationship was found for Hispanics. When living in a county with higher percentages of Hispanics, they reported significantly fewer difficulties in obtaining care, but similar financial barriers (Haas et al., 2004). Related to our study, blacks with private insurance in Phoenix may perceive additional barriers to accessing health care than their Hispanic counterparts that result in increased risk to NO2. This relationship was not found for those with Medicaid, where race/ethnicity was not a factor in predicting risk. Because only 6% of Phoenix children are African American (see Table 3), future work should explore relationships in cities with larger African American populations.
5. Conclusion
In sum, this paper contributes to discussions of insurance status, race, and ethnicity as effect modifiers for the effects of air pollution on risk of children’s hospitalizations for asthma. Our study demonstrates a statistical method suitable for small counts that allows for the disaggregation of social groups. Specifically, we considered Hispanic and black children as unique groups as opposed to combining them into a ‘minority’ group and we separated the uninsured from those with Medicaid as opposed to combining them into a ‘poor group.’ Considering these groups separately is important because these social groups face distinct challenges to asthma management which might contribute to their risk of hospitalization due to environmental air pollution. Although we cannot confirm a cause-effect relationship, this analysis suggests the heightened risk for those without insurance and secondarily Hispanic children without insurance, to traffic-related air pollution. We recommend policies to increase insurance rates of children in order to reduce their risk. Further studies are needed to explain the increased risk to NO2 exceedances for blacks with private insurance as compared to Hispanics.
Acknowledgements
We recognize Wade Bannister at Arizona State University for his assistance with the insurance counts used in this paper and for his patience and prompt attention to all of our questions and concerns. Dr. Robert Balling at Arizona State University also assisted with an earlier iteration of this paper. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of NSF, NIH or NCRR.
Funding Sources: Supported by National Science Foundation’s ADVANCE grant for women in science at University of Texas at El Paso (Grant No. 0245071) and partially by NIH SCORE 2S06 GM008012 and RCMI-NCRR 5G12 RR008124.
6. Appendix
Let Yt denote the indicator of a hospital admission, and Rt the race/ethnicity of a randomly selected member of the population on day t. The race/ethnicity categories assigned to Rt are white (W), black (B), and Hispanic (H). The discussion that follows equally holds when Rt is instead the insurance status (Medicaid, Private, No Insurance), or insurance status by race/ethnicity (e.g., Medicaid-White).
A model is proposed for the relative risk θR(t) of hospital admission for race/ethnicity R (Hispanic or black) as compared to white (W):
| (1) |
| (2) |
for R ∈ {W, B, H}, where xt = (x1t, … , xpt) are covariates, such as pollution or weather variables with seasonal effects removed. The parameters of the reference group are set to zero: αW = 0 and βWj = 0; j = 1, … , p. The model (2) for the relative risk is motivated by the logistic regression model. The heuristic argument is that if we let
then the corresponding odds-ratio
approximates the desired relative risk (1), assuming that the likelihood of hospitalization for asthma is rare. The slope coefficients (β’s) in the regression model (2) for the relative risk are zero when race/ethnicity does not modulate the effects of the weather or pollution covariates. The intercepts (α’s) are zero when, after controlling for the effects of pollution and weather, race/ethnicity is not a risk factor for hospital admission at the seasonal mean value of pollution and weather.
The available patient data consists of race/ethnicity and insurance status for the cases only, that is hospital admissions that have Yt = 1. Such observational data allow us to fit a generalized logit regression model for nominal data (Agresti 1990):
which implies
| (3) |
where α′R = α′R – a′W, and β′Rj = b′Rj – b′Wj; j = 1, … p. The parameters of the reference group are zero: α′W = 0 and β′Wj = 0; j = 1, … , p. We derive, as in Fears and Brown (1996), the relationship between the slope and intercept parameters of equations (2) and (3), namely that
| (4) |
| (5) |
where NR and NW are the population counts for race/ethnicity R (Hispanic or black) and white. The derivation begins by considering (1) the desired relative risk
and applying the rule P(A|B, C) = P(A, B|C)/P(B|C), then P(A, B|C) = P(B|A, C)P(A|C). Letting the events A, B, C denote A : Yt = 1, B : Rt = R, C : xt, the desired odds ratio is
Upon substituting the regression models for θR(t) and θ′R(t) given by equations (2) and (3):
for all values of the covariates x1t, … , xpt. This implies the desired result, namely (4) and (5).
The implication of equation (4) is that tests of significance for the covariates in (2) are equivalent to tests of significance for the covariates in (3). However, a test of significance for the intercept term in (2) is not equivalent to a test of significance for the intercept term in (3); see the offset in equation (5). So, a test of the hypotheses
is equivalent to a test of the hypotheses
These hypotheses may be tested using the Wald test statistic :
that has an asymptotic chi-square distribution with one-degree of freedom under the null hypothesis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. in the USA and other countries. ® indicates USA registration.
In reviewing the findings for weather variables, Hispanic children had increased risk of hospitalization as compared to white children with temperature increases (Table 4B). Within the joint insurance-race and ethnicity models, a pattern emerged whereby black and Hispanic children without insurance had significantly higher risk of asthma admission than white children without insurance when temperature increased (Table 5-C). This finding may relate to living environments of poor, minority residents in Phoenix that do not isolate children from climatic changes, such as residence in homes without cooling systems. Further, asthma inhalers become less effective when used at temperatures above 77° F (Hoye et al 2005) and highs are above 77° F eight months of the year. In addition, for those on Medicaid, Hispanic children had significantly higher risk of asthma admission than white children when temperature increased (Table 5-A)
Ethics: Data were received from Arizona Department of Health Services without any identifying or personal information.
References
- Akinbami L. Asthma Prevalence, Health Care Use and Mortality: United States, 2003–05. Vol. 2008. Hyattsville, MD: Department of Health and Human Services, Center for Disease Control and Prevention, National Center for Health Statistics; 2007. [Google Scholar]
- American Academy of Pediatrics. Pediatric Asthma Promoting Best Practices: Guide For Managing Asthma in Children. Rochester, NY: University of Rochester Academic Service Consortium; 1999. [Google Scholar]
- Begg C, Gray R. Calculation of polychotomous logistic regression parameters using individualized regressions. Biometrika. 1984;71:11–18. [Google Scholar]
- Berg J, et al. Latino Children with Asthma: Rates and Risks for Medical Care Utilization. Journal of Asthma. 2004;41:147–157. doi: 10.1081/jas-120026072. [DOI] [PubMed] [Google Scholar]
- Bernstein JA, et al. Health effects of air pollution. Journal of Allergy and Clinical Immunology. 2004;114:1116–1123. doi: 10.1016/j.jaci.2004.08.030. [DOI] [PubMed] [Google Scholar]
- Brotanek JA, et al. Inadequate access to care among children with asthma from Spanish-speaking families. Journal of Health Care for the Poor and Underserved. 2005;16:63–73. doi: 10.1353/hpu.2005.0005. [DOI] [PubMed] [Google Scholar]
- Brousseau DC, et al. Disparities for Latino children in the timely receipt of medical care. Ambulatory Pediatrics. 2005;5:319–325. doi: 10.1367/A04-203R1.1. [DOI] [PubMed] [Google Scholar]
- Bureau of the US Census. Summary File 3. 2000 [Google Scholar]
- Burra TA, et al. Social disadvantage, air pollution, and asthma physician visits in Toronto, Canada. Environmental Research. 2009 doi: 10.1016/j.envres.2009.03.004. doi:10.1016/j.envres.2009.03.004. [DOI] [PubMed] [Google Scholar]
- Canino G, et al. Asthma disparities in the prevalence, morbidity, and treatment of Latino children. Social Science & Medicine. 2006;63:2926–2937. doi: 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- Chang J, et al. Repeated respiratory hospital encounters among children with asthma and residential proximity to traffic. Occupational and environmental medicine. 2009;66:90–98. doi: 10.1136/oem.2008.039412. [DOI] [PubMed] [Google Scholar]
- Charafeddine R, Boden LI. Does income inequality modify the association between air pollution and health? Environmental Research. 2008;106:81–88. doi: 10.1016/j.envres.2007.09.005. [DOI] [PubMed] [Google Scholar]
- Chen Z, Kuo L. A note on estimation of the multinomial logit model with random effects. The American Statistician. 2001;55:89–95. [Google Scholar]
- Delfino RJ, et al. Repeated hospital encounters for asthma in children and exposure to traffic-related air pollution near the home. Annals of Allergy Asthma & Immunology. 2009;102:138–144. doi: 10.1016/S1081-1206(10)60244-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino RJ, et al. Asthma symptoms in Hispanic children and daily ambient exposures to toxic and criteria air pollutants. Environmental Health Perspectives. 2003;111:647–656. doi: 10.1289/ehp.5992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delfino RJ, et al. Association of Asthma Symptoms with Peak Particulate Air Pollution and Effect Modification by Anti-inflammatory Medication Use. Environmental Health Perspectives. 2002;110:A607–A617. doi: 10.1289/ehp.021100607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EPA. NOx - How Nitrogen Oxides Affect The Way We Live & Breathe. Vol. 2005. Environmental Protection Agency; 2000. [Google Scholar]
- EPA. More Details on Nitrogen Dioxide- Based on Data Through 2002. Vol. 2005. Environmental Protection Agency; 2005. [Google Scholar]
- Farhat SCL, et al. Effect of air pollution on pediatric respiratory emergency room visits and hospital admissions. Brazilian Journal of Medical and Biological Research. 2005;38:227–235. doi: 10.1590/s0100-879x2005000200011. [DOI] [PubMed] [Google Scholar]
- Fears T, Brown C. Logistic regression methods for retrospective case-control studies using complex sampling procedures. Biometrics. 1986;42:955–960. [PubMed] [Google Scholar]
- Fisher MA, Mascarenhas AK. Does Medicaid improve utilization of medical and dental services and health outcomes for Medicaid-eligible children in the United States? Community Dentistry and Oral Epidemiology. 2007;35:263–271. doi: 10.1111/j.1600-0528.2007.00341.x. [DOI] [PubMed] [Google Scholar]
- Flores G, Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121:E286–E298. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- Forastiere F, et al. Socioeconomic status, particulate air pollution, and daily mortality: Differential exposure or differential susceptibility. American Journal of Industrial Medicine. 2007;50:208–216. doi: 10.1002/ajim.20368. [DOI] [PubMed] [Google Scholar]
- Gilliland FD, et al. Effects of Ambient Air Pollution in School Absenteeism Due to Respiratory Illness. Epidemiology. 2000;12:43–54. doi: 10.1097/00001648-200101000-00009. [DOI] [PubMed] [Google Scholar]
- Gouveia N, Fletcher T. Time series analysis of air pollution and mortality: effects by cause, age and socioeconomic status. Journal of Epidemiology and Community Health. 2000;54:750–755. doi: 10.1136/jech.54.10.750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gwynn RC, Thurston GD. The burden of air pollution: Impacts among racial minorities. Environmental Health Perspectives. 2001;109:501–506. doi: 10.1289/ehp.01109s4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas J, et al. Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual’s county of residence. Medical Care. 2004;42:707–714. doi: 10.1097/01.mlr.0000129906.95881.83. [DOI] [PubMed] [Google Scholar]
- Ho W-C, et al. Air pollution, weather, and associated risk factors related to asthma prevalence and attack rate. Environmental Research. 2007;104:402–409. doi: 10.1016/j.envres.2007.01.007. [DOI] [PubMed] [Google Scholar]
- Jerrett M, et al. Do socioeconomic characteristics modify the short term association between air pollution and mortality? Evidence from a zonal time series in Hamilton, Canada. journal of Epidemiological Community Health. 2004;58:31–40. doi: 10.1136/jech.58.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson WG, et al. Tempe, AZ: Arizona State University, Center for Health Information & Research, School of Computing and Informatics; 2007. Health Insurance in Arizona: Residents of Maricopa County. [Google Scholar]
- Lara M, et al. Physician perceptions of barriers to care for inner-city Latino children with asthma. Journal of Health Care for the Poor & Underserved. 1999;10:27–44. doi: 10.1353/hpu.2010.0785. [DOI] [PubMed] [Google Scholar]
- Laurent O, et al. Effect of socioeconomic status on the relationship between atmospheric pollution and mortality. Journal of Epidemiological Community Health. 2007;61:665–675. doi: 10.1136/jech.2006.053611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessard G, Ku L. Gaps In Coverage for Children in Immigrant Families. Future of Children. 2003;13:105–115. [PubMed] [Google Scholar]
- Lin M, et al. Effect of short-term exposure to gaseous pollution on asthma hospitalisation in children: a bi-directional case-crossover analysis. Journal of Epidemiology and Community Health. 2003;57:50–55. doi: 10.1136/jech.57.1.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipfert FW. Air pollution and poverty: Does the sword cut both ways? Journal of Epidemiological Community Health. 2004;58:2–3. doi: 10.1136/jech.58.1.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins MCH, et al. Influence of socioeconomic conditions on air pollution adverse health effects in elderly people: an analysis of six regions in Sao Paulo, Brazil. Journal of Epidemiological Community Health. 2004;58:41–46. doi: 10.1136/jech.58.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Migilaretti G, Cavallo F. Urban air pollution and asthma in children. Pediatric Pulmonology. 2004;38:198–203. doi: 10.1002/ppul.20057. [DOI] [PubMed] [Google Scholar]
- Nauenberg E, Basu K. Effect of insurance coverage on the relationship between asthma hospitalizations and exposure to air pollution. Public Health Reports. 1999:114. [PMC free article] [PubMed] [Google Scholar]
- O'Neill MS, et al. Health, wealth, and air pollution: Advancing theory and methods. Environmental Health Perspectives. 2003;111:1861–1870. doi: 10.1289/ehp.6334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmgren J. The Fisher information matrix for log linear models arguing conditionally on observed explanatory variables. Biometrika. 1981;68:563–566. [Google Scholar]
- Peel JL, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005;16:164–174. doi: 10.1097/01.ede.0000152905.42113.db. [DOI] [PubMed] [Google Scholar]
- Scoggins A, et al. Spatial analysis of annual air pollution exposure and mortality. Science of the Total Environment. 2004;321:71–85. doi: 10.1016/j.scitotenv.2003.09.020. [DOI] [PubMed] [Google Scholar]
- Shannon MW, et al. Ambient air pollution: Health hazards to children. Pediatrics. 2004;114:1699–1707. doi: 10.1542/peds.2004-2166. [DOI] [PubMed] [Google Scholar]
- Slaughter JC, et al. Association between particulate matter and emergency room visits, hospital admissions and mortality in Spokane, Washington. Journal of Exposure Analysis and Environmental Epidemiology. 2005;15:153–159. doi: 10.1038/sj.jea.7500382. [DOI] [PubMed] [Google Scholar]
- State of Arizona. Kids Care. 2005;Vol. 2006 [Google Scholar]
- Thompson AJ, et al. Acute Asthma Exacerbations and Air Pollutants in Children Living in Belfast, Northern Ireland. Archives of Environmental Health. 2001;56:234–241. doi: 10.1080/00039890109604447. [DOI] [PubMed] [Google Scholar]
- Zanobetti A, Schwartz J. Race, gender and social status as modifers of the effects of PM10 on mortality. Journal of Occupational and Environmental Medicine. 2000;42:469–474. doi: 10.1097/00043764-200005000-00002. [DOI] [PubMed] [Google Scholar]