Abstract
Although congenital syphilis is a rare disease in Canada, infected infants may experience severe sequelae, including cerebral palsy, hydrocephalus, sensorineural hearing loss and musculoskeletal deformity. Timely treatment of congenital syphilis during pregnancy may prevent all of the above sequelae. However, the diagnosis of suspected cases and management of congenital syphilis may be confusing, and the potential for severe disability is high when cases are missed. The present review provides assistance to practitioners in the diagnosis of suspected cases and management of children with presumed or confirmed infection.
Keywords: Congenital syphilis
Abstract
Bien que la syphilis congénitale soit une maladie rare au Canada, les nourrissons infectés peuvent présenter des séquelles graves, dont la paralysie cérébrale, l’hydrocéphalie, la surdité neurosensorielle et les difformités musculosquelettiques. Un traitement opportun de la syphilis congénitale pendant la grossesse pourrait prévenir toutes ces séquelles. Cependant, le diagnostic des cas présumés et la prise en charge de la syphilis congénitale peuvent prêter à confusion, et le risque d’incapacités graves est élevé lorsqu’on passe à côté d’un cas. Le présent examen est conçu pour aider les praticiens dans le diagnostic des cas présumés et la prise en charge des enfants souffrant d’une infection présumée ou confirmée.
Congenital syphilis has become a rare disease in Canada. However, infected infants may suffer severe sequelae, including cerebral palsy, hydrocephalus, sensorineural hearing loss and musculoskeletal deformity, all of which may be prevented with timely treatment during pregnancy. Questions about the prevention and management of congenital syphilis persist because the diagnosis of suspected cases and management may be confusing, and the potential for severe disability is high when cases are missed. The present review provides assistance to practitioners in the diagnosis of suspected cases and management of children with presumed or confirmed infection.
Most commonly, transmission occurs transplacentally, and it may occur at any time during gestation; however, the risk of transmission to the fetus depends on the stage of maternal infection. In general, the longer the time that primary infection occurs before pregnancy, the more benign the outcome in the infant with respect to rate and severity of infection. Untreated primary (ie, chancre) or secondary (ie, rash) syphilis in pregnancy results in a 25% risk of stillbirth, a 14% risk of neonatal death, a 41% risk of giving birth to a live but infected infant and only a 20% chance of giving birth to a healthy, uninfected infant. Untreated late syphilis (ie, early and late latent syphilis that occurs more than one to two years after infection) results in a 12% risk of a stillbirth, a 9% risk of neonatal death, a 2% risk of giving birth to an infected infant and a 77% chance of giving birth to an uninfected infant (1). Women whose infection manifests itself during the first year after delivery may also infect their infants.
The present review is based on literature derived from a search of MEDLINE from 1966 to 1999 using the keyword ‘congenital syphilis’. The references of the papers selected were reviewed for articles not found by the search.
EPIDEMIOLOGY OF SYPHILIS
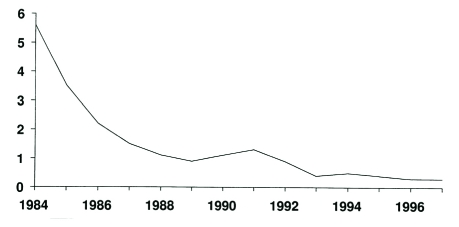
The rate of early symptomatic syphilis among women in Canada peaked at 2.1/100,000 (5.6/100,000 of the total population) in 1984 (Figure 1). While this rate fell subsequently to 0.4/100,000 of the total population by 1995, an equalization of the rates among men and women occurred during this time (2). Between 1992 and 1997, 16 cases of congenital syphilis were reported to Health Canada, the majority of which were from Ontario (3). Although the incidence of congenital syphilis has remained low over the past decade due to the routine screening of pregnant women, it remains an important cause of preventable disability among children. Epidemiological studies in the United States show that gestational syphilis affects predominantly young, unmarried women of low socioeconomic status with multiple sexual partners and inadequate prenatal care, as well as those women who exchange sex for drugs (4).
Figure 1).
Reported cases of early symptomatic congenital syphilis in Canada from 1984 to 1997 per 100,000 population. Reproduced from reference 3
As with gonorrhea, chlamydia and chancroid, syphilis is a notifiable disease by all provinces and territories to the federal government. Universal screening in pregnancy remains the standard of care in Canada.
SCREENING FOR SYPHILIS IN PREGNANCY
The serological tests for syphilis are classified as nontreponemal and treponemal tests (5). The nontreponemal tests include the Venereal Disease Research Laboratory (VDRL) or the Rapid Plasma Reagin (RPR) tests, which detect antibody to cardiolipin. Because of the high rate of biological false positives with the VDRL and RPR tests, a positive nontreponemal test is confirmed with a treponemal test, the Fluorescent Treponemal Antibody-Absorption (FTA-ABS) test and/or the Microhemagglutination Assay-Treponema pallidum (MHA-TP) test. The following should be noted:
Gestational syphilis is diagnosed most commonly by routine serological screening of all women during early pregnancy (6).
Women who are considered to be at high risk for acquiring syphilis during pregnancy should undergo repeat testing in the third trimester and at delivery (7).
Women who did not receive prenatal care should have maternal syphilis serology performed before they and their children are discharged; prompt follow-up after discharge should be ensured.
Women may also present with signs and symptoms of primary or secondary syphilis in pregnancy that warrant serological examination at the time of clinical presentation. A description of the clinical stages (including chancre and rash) of syphilis has been reviewed previously (8).
Cord blood testing is not recommended because of the high rate of false positive results (7).
A diagnosis of maternal syphilis during the year after a women gives birth should lead to testing of the infant.
Immigrant parents and children (including foreign adoptees) from regions of the world with a high incidence of syphilis should be screened for syphilis or congenital syphilis in the case of children when first presenting for medical care. Because the incidence of congenital syphilis is extremely low in Canada, the detection rate is likely to be highest in this group.
TREATMENT OF SYPHILIS IN PREGNANCY
The treatment for syphilis in pregnancy is identical to that of adults who are not pregnant, except that penicillin is the only agent that is appropriate for use during pregnancy (9). Tetracyclines are contraindicated in pregnancy because of their effect on fetal bone and tooth development. Erythromycin has inconsistent placental transfer, and treatment failures have been reported (9). For primary, secondary or early latent syphilis, 2.4 million units of benzathine penicillin G (BPG) is given intramuscularly in one dose (10). Some experts recommend a second dose of BPG for pregnant women due to the possibility of treatment failures and transmission to the fetus, especially for secondary syphilis (11,12). For the treatment of late latent syphilis or disease of unknown duration, 2.4 million units of BPG given intramuscularly once weekly for three weeks is recommended (10). Women with a documented penicillin allergy should undergo desensitization and treatment with penicillin (10). Individuals with neurosyphilis should receive 3 to 4 million units of crystalline penicillin G intravenously every 4 h for 10 to 14 days (10). Individuals infected with the human immunodeficiency virus (HIV) should undergo investigation for neurosyphilis before treatment.
Following adequate therapy for primary or secondary syphilis, the required monthly follow-up testing should show at least a fourfold decline in titre three to four months after treatment. If treatment occurs in the latent or late stages or if reinfection occurs, a more gradual decline in titres may be seen, and a low positive titre (1:2, 1:4) may persist in approximately 50% of such individuals for two or more years (ie, a serofast reaction) (5). Women in whom titres fail to decline as predicted require investigation and management for neurosyphilis (lumbar puncture for cell count, protein and VDRL), and further therapy.
RECOMMENDED TESTING FOR OTHER SEXUALLY TRANSMITTED DISEASES
All pregnant women should receive appropriate counselling and recommendations for HIV testing (13). Women who are diagnosed with syphilis during pregnancy should receive HIV testing if this has not been performed previously; hepatitis B surface antigen and hepatitis C antibody testing should also be performed. Chlamydia and gonorrhea cultures are also recommended. Diagnosis and treatment of syphilis in the HIV-infected individual may be problematic because serology may be falsely negative or positive, seroconversion may be delayed and response to treatment may be suboptimal due to abnormalities in cell-mediated immunity (8,11). There may be an increased risk of transplacental HIV transmission to the fetus in syphilis coinfection resulting from placental inflammation (14). HIV infection may also enhance syphilis transmission due to impaired cell-mediated immunity (15). The advice of an expert in the management of HIV should be sought in cases of coinfection with syphilis and HIV.
CLINICAL PRESENTATION
Infants with congenital syphilis may present with typical signs and symptoms or they may be completely asymptomatic at birth. Clinical findings may become obvious in the first few months of life; however, infection may remain undetected in some children until the signs of late congenital syphilis are apparent. The signs and symptoms of early and late congenital syphilis are listed in Tables 1 and 2.
TABLE 1:
Clinical findings related to congenital syphilis in children younger than one year of age
| System | Findings |
|---|---|
| Gestational |
|
| Reticuloendothelial | |
| Mucocutaneous (in 30% to 60%)* | |
| Skeletal (in 70% to 80%)* |
|
| Neurological |
|
| Ocular |
|
| Other organ involvement |
|
Percentages refer to the proportion of symptomatic infants with the given abnormality
Snuffles, skin blisters and crusts contain infectious spirochetes. Children with these lesions should be considered contagious and appropriate contact barrier precautions instituted
TABLE 2:
Clinical findings related to late congenital syphilis in children older than one year of age
| System | Findings |
|---|---|
| Dental (vasculitis due to inflammation of developing tooth buds in late gestation) |
|
| Ear |
|
| Cutaneous |
|
| Skeletal |
|
| Neurological |
|
| Ocular |
|
| Other organ involvement |
|
| Hutchinson’s triad |
|
DIAGNOSTIC TESTING
The surveillance case definition for congenital syphilis is presented in Table 3. A diagnostic algorithm for congenital syphilis is presented in Figure 2. When the diagnosis of congenital syphilis is suspected before or during delivery (based on the maternal history), ideally, an histological examination of the placenta and cord should be performed for typical pathological changes and spirochetes (16). As well, desquamation or ulcerative skin lesions or nasal discharge (‘snuffles’), if present, should be examined for spirochetes by darkfield microscopy or by using fluorescent antibody techniques (5). Snuffles are more likely to occur in infants at one to three months of age. Identification of spirochetes in specimens from lesions or tissue is required for a definitive diagnosis of congenital syphilis (Table 3). In addition to a thorough physical examination, all infants potentially exposed to syphilis in utero should undergo serological testing for syphilis, regardless of maternal treatment. Asymptomatic infants whose mothers receive appropriate treatment should be followed monthly until their nontreponemal antibody disappears. Transplacentally acquired nontreponemal (VDRL or RPR) antibody will be present in most infants, but it disappears in uninfected infants by six months of age. Passively acquired treponemal antibody (FTA-ABS and/or MHA-TP) disappears at 12 to 18 months of age.
TABLE 3:
Surveillance case definition for congenital syphilis
| A confirmed case of congenital syphilis is an infant in whom Treponema pallidum is identified by darkfield microscopy, fluorescent antibody, or other specific stains in specimens from lesions, placenta, umbilical cord or autopsy material. |
A presumptive case of congenital syphilis is when either of the following conditions are present:
|
| A syphilitic stillbirth is defined as a fetal death in which the mother had untreated or inadequately treated syphilis* at delivery of a fetus after a 20-week gestation or of 500 g. |
Inadequate treatment consists of any nonpenicillin therapy or penicillin given less than 30 days before delivery.
See Table 1.
It may be difficult to distinguish between congenital and acquired syphilis in a seropositive child after infancy. Signs may not be obvious and stigmata may not yet have developed. Abnormal values for cerebrospinal fluid Venereal Disease Research Laboratory, cell count, and protein, as well as immunoglobulin M antibodies, may be found in either congenital or acquired syphilis. Findings on long bone x-rays may help because these will indicate congenital syphilis. The decision may ultimately be based on maternal history and clinical judgment; the possibility of sexual abuse also needs to be considered. Reproduced from reference 20
Figure 2).
Algorithm for the treatment and diagnosis of congenital syphilis. *Fluorescent Treponemal Antibody-Absorption or Microhemagglutination Assay-Treponema Pallidum. †Consider to be serofast only if Venereal Disease Research Laboratory/Rapid Plasma Reagin (RPR) is 1:4. CSF Cerebrospinal fluid
A complete diagnostic evaluation, including long bone radiographical examination and lumbar puncture for cell count, protein and VDRL, is warranted in the following situations (11):
if the infant or child has signs or symptoms of congenital syphilis (Table 1);
if there is no documented maternal treatment in pregnancy;
if the mother was treated within four weeks of delivery;
if the maternal treatment was inadequate (with a nonpenicillin regimen or insufficient penicillin dosing) or inadequately documented; or
a fourfold decline in titre following therapy was not documented (possibly due to inadequate treatment).
Long bone radiography is abnormal in approximately 65% of symptomatic, infected babies, while only 6% of asymptomatic infants born to untreated or reinfected mothers have abnormalities (17). It has been argued that the results of long bone radiography in most infected children do not affect decisions regarding therapy (18). However, abnormalities on x-ray may provide the most expeditious evidence of infection, even before serology is available. The usefulness of cerebrospinal fluid (CSF) examination in the diagnosis of congenital syphilis has also been debated. An elevated CSF cell count (greater than 25 cell/mm3), an elevated protein level (greater than 0.15 g/L) and a positive CSF VDRL result have low sensitivity and specificity in the diagnosis of neurosyphilis (18). As well, children with a negative CSF VDRL have gone on to develop later signs of neurosyphilis. While there is controversy in the literature regarding the usefulness of both long bone films and CSF examinations, these tests remain the standard of care (18).
There is no test which, at birth, will identify the asymptomatic baby with normal long bone examination as definitively infected or uninfected. Most infected babies are asymptomatic at birth. Review of maternal serology and follow-up of the infant will, over time, indicate whether infection has occurred. In most cases, the diagnosis is presumptive, and is based on serological and clinical features. All children should have both nontreponemal (VDRL or RPR) and treponemal (FTA-ABS and/or MHA-TP) testing performed. Many laboratories will perform an immunoglobulin (Ig) M assay, most commonly a Western blot, to detect IgM to multiple treponemal proteins (5). Because IgM does not cross the placenta, a positive IgM is consistent with congenital infection. The sensitivity of the IgM Western blot is approximately 83%, with a specificity of 90%. The older FTA-ABS 19S IgM test is less sensitive and specific. Detection of treponemal DNA in tissues or fluids (eg, amniotic fluid, CSF) by polymerase chain reaction has been evaluated but is not routinely available (5).
Ultimately, a presumptive serological diagnosis may also be made when:
an infant’s nontreponemal titre (VDRL or RPR) is fourfold higher than that of the mother when both blood samples are drawn at the time of delivery;
the infant’s nontreponemal titre (VDRL or RPR) persists or increases after birth; or
the infant’s treponemal antibody titre (FTA-ABS and/or MHA-TP) remains positive at 12 to 18 months of age.
TREATMENT
For proven or probable congenital syphilis (Table 3) in the first four weeks of life, treatment consists of aqueous crystalline penicillin G, 50,000 units/kg/dose intravenously every 12 h in the first seven days of life. This is increased to every 8 h after seven days of life, for 10 to 14 days. An alternative treatment is aqueous procaine penicillin G, 50,000 units/kg/day intramuscularly for 10 to14 days. For infants who are at least four weeks of age or older children, treatment is aqueous penicillin G, 50,000 units/kg/dose every 6 h intravenously for 10 to 14 days because of the difficulty in excluding neurosyphilis in this age group (11).
The management of an asymptomatic, exposed infant is controversial. Some experts give a full course of penicillin to infants who are asymptomatic (with normal CSF and radiographic examination) and have an inadequate maternal treatment history, including no maternal treatment; insufficient penicillin treatment (eg, single dose of benzathine penicillin G for late latent syphilis); failed penicillin therapy (inadequate response to treatment); adequate therapy that is given less than one month before delivery; or treatment with a nonpenicillin regimen. The alterative to immediate treatment is close follow-up with initiation of therapy when the signs or symptoms of congenital syphilis develop, or when nontreponemal titres increase or fail to decline. Single dose benzathine penicillin G is recommended by some experts for this scenario, especially when follow-up cannot be assured (11). However, failures have occurred using this treatment regimen (19). Therefore, if adequate follow-up of an exposed, asymptomatic infant cannot be guaranteed, consideration should be given to a full course of therapy for the child before discharge from the hospital. Infants born to mothers who are HIV coinfected and in whom follow-up cannot be assured, should be treated for 10 to 14 days, regardless of maternal treatment history and symptomatology because the response to maternal treatment is unpredictable. Children born to mothers who develop the signs or symptoms of secondary or early latent syphilis within one year after delivery should be tested and treated if serology is reactive.
Some infants will experience a reaction following the initiation of therapy. This consists of fever, chills, tachypnea, tachycardia, hypotension and accentuation of cutaneous lesions. This reaction may also occur in women treated in pregnancy, precipitating labour or possibly fetal death. The etiology of this reaction is most likely related to the inflammatory response to dead or dying spirochetes (13).
SEROLOGICAL AND CLINICAL FOLLOW-UP
In children with congenital syphilis, serial nontreponemal (VDRL or RPR) serology should be repeated at one, two, four, six and 12 months. The nontreponemal titre should become nonreactive by 12 months of age when children are treated appropriately. Children with persistently positive titres, even at a low level, should be considered for a second course of treatment. Infants with neurosyphilis (positive CSF VDRL, or abnormal cell count or protein) who were treated should have a repeat CSF examination at six month intervals until results are normal. A positive CSF VDRL six months after treatment requires for a second course of treatment. Uninfected infants should also have serial nontreponemal titres taken, which should become nonreactive by six months of age (13). Passively acquired maternal treponemal antibody (FTA-ABS and/or MHA-TP) is not likely to persist beyond 15 to 18 months.
Infants with congenital syphilis may require multi-disciplinary follow-up. While the prognosis is considered to be very good for infants treated during the first two months of life, there are no published data with yearly long term follow-up. Cases that are missed in early infancy may present as described in Table 3, with sensorineural hearing loss being the most common manifestation.
SUMMARY POINTS
All pregnant women should be tested for syphilis in pregnancy. Women at high risk for acquiring syphilis in pregnancy should be retested at the beginning of the third trimester (28 weeks) and at delivery. HIV testing should be recommended to all pregnant women. HIV testing is particularly important in women with positive syphilis serology, as is testing for hepatitis B surface antigen, hepatitis C antibody, chlamydia and gonorrhea.
Penicillin is the only antibiotic proven to be effective in the management of gestational syphilis. Children born to mothers treated with a nonpenicillin regimen should be considered to have been treated inadequately.
Syphilis and HIV coinfection is not uncommon. Seroconversion may be delayed and clinical presentation atypical in HIV-infected women. Treatment failures for gestational syphilis are more common in this group; treatment of infants should be given consideration regardless of serology and symptomatology.
Diagnosis and management of congenital syphilis should be based on maternal history, clinical findings and nontreponemal (VDRL or RPR) and treponemal testing (FTA-ABS and/or MHA-TP). Tests to identify definitively infected infants at birth, such as IgM and DNA detection (polymerase chain reaction), are considered investigational. The persistence of treponemal antibody after 15 to 18 months of age may confirm congenital infection in the asymptomatic child.
All children with clinical or serological evidence of congenital syphilis should be treated with penicillin G for 10 to 14 days. Close clinical and serological follow-up of all children potentially exposed to syphilis in utero is required.
REFERENCES
- 1.Ingraham NR. The value of penicillin alone in the prevention and treatment of congenital syphilis. Acta Dermato Veneriologica. 1951;31:60–88. [PubMed] [Google Scholar]
- 2.Romanowski B. Syphilis: Epidemiology and control. Can J Hum Sexuality. 1997;6:171–7. [Google Scholar]
- 3.Health Canada Sexually transmitted diseases in Canada: 1996 surveillance report (with preliminary 1997 data) Can Commun Dis Rep. 1999;25:S1. [Google Scholar]
- 4.Rawstron SA, Jenkins S, Blanchard S, Li PW, Bromberg K. Maternal and congenital syphilis in Brooklyn NY. Epidemiology, transmission and diagnosis. Am J Dis Child. 1993;147:727–31. doi: 10.1001/archpedi.1993.02160310029012. [DOI] [PubMed] [Google Scholar]
- 5.Larsen SA, Steiner BM, Rudolph AH. Laboratory diagnosis and interpretation of tests for syphilis. Clin Microbiol Rev. 1995;8:1–21. doi: 10.1128/cmr.8.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Clinical Practice-Obstetrics Committee Healthy beginnings: guidelines for care during pregnancy and childbirth. Journal of Society of Obstetricians and Gynaecologists of Canada. 1998;71:28–9. [Google Scholar]
- 7.Guidelines for the prevention and control of congenital syphilis. Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 1988;37(Suppl 1):1–13. [PubMed] [Google Scholar]
- 8.Singh AE, Romanowski B. Syphilis: Review with emphasis on clinical, epidemiologic, and some biologic features. Clin Microbiol Rev. 1999;12:187–209. doi: 10.1128/cmr.12.2.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rolfs RT. Treatment of syphilis, 1993. Clin Infect Dis. 1995;20(Suppl 1):S23–38. doi: 10.1093/clinids/20.supplement_1.s23. [DOI] [PubMed] [Google Scholar]
- 10.Health Canada . Canadian STD Guidelines. Ottawa: Health Canada; 1998. pp. 150–9. [Google Scholar]
- 11.1998 Guidelines for the treatment of sexually transmitted diseases. Centers for Disease Control and Prevention. MMWR Morb Mortal Wkly Rep. 1998;47(RR–1):1–111. [PubMed] [Google Scholar]
- 12.Alexander JM, Sheffield JS, Sanchez PJ, Mayfield J, Wendel GD., Jr Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol. 1999;93:5–8. doi: 10.1016/s0029-7844(98)00338-x. [DOI] [PubMed] [Google Scholar]
- 13.US Public Health Service recommendations for human immunodeficiency virus counseling and voluntary testing for pregnant women. MMWR Morb Mortal Wkly Rep. 1995;44(RR–7):1–15. [PubMed] [Google Scholar]
- 14.Sanchez PJ. Congenital syphilis. Adv Pediatr Infect Dis. 1992;7:161–80. [PubMed] [Google Scholar]
- 15.Lee MJ, Hallmark RJ, Frenkel LM, Del Priore G. Maternal syphilis and vertical perinatal transmission of human immunodeficiency virus type-1 infection. Int J Gynecol Obstet. 1998;63:247–52. doi: 10.1016/s0020-7292(98)00165-9. [DOI] [PubMed] [Google Scholar]
- 16.Russell P, Altshuler G. Placental abnormalities of congenital syphilis. A neglected aid to diagnosis. Am J Dis Child. 1974;128:160–3. doi: 10.1001/archpedi.1974.02110270034007. [DOI] [PubMed] [Google Scholar]
- 17.Moyer VA, Schneider V, Yetman R, Garcia-Prats J, Parks D, Cooper T. Contribution of long-bone radiographs to the management of congenital syphilis in the newborn infant. Arch Pediatr Adolesc Med. 1998;152:353–7. doi: 10.1001/archpedi.152.4.353. [DOI] [PubMed] [Google Scholar]
- 18.Risser WL, Hwang LY. Problems in the current case definitions of congenital syphilis. J Pediatr. 1996;129:499–505. doi: 10.1016/s0022-3476(96)70113-0. [DOI] [PubMed] [Google Scholar]
- 19.Beck-Sague D, Alexander ER. Failure of benzathine penicillin G treatment in early congenital syphilis. Pediatr Infect Dis J. 1987;6:1061–4. [PubMed] [Google Scholar]
- 20.Wharton M, Chorba TL, Vogt RL, Morse DL, Buehler JW. Case definitions for public health surveillance. MMWR Morb Mortal Wkly Rep. 1990;39(RR–13):1–43. [PubMed] [Google Scholar]