Abstract
Objectives. Using data on 2868 children born in the Western Australian Pregnancy Cohort (Raine) Study, we examined the association between changes in family socioeconomic status and childhood asthma.
Methods. We determined the likelihood (odds ratio) of a child having asthma at ages 6 and 14 years for 4 family-income trajectories (chronic low, increasing, decreasing, and never low) over the child's lifetime. The trajectories were created from longitudinal latent-class models.
Results. We found a 2-fold increased risk of asthma at age 14 years among children who had lived in a low-income family since birth, especially for girls. Asthma was less likely to occur in children born to single parents; income rose over time in many of these families. Compared with children in chronic low-income families, children in households with increasing incomes had a 60% lower risk of asthma. Single-point measures of low income were not found to be associated with asthma.
Conclusions. Chronic exposure to a low-income environment from birth was associated with the development of persistent asthma. There was also a protective effect against asthma among those children whose families had moved out of poverty.
Asthma disproportionately burdens children living in economically disadvantaged urban communities. Some of this disparity can be attributed to the observation that once asthma is established, lower utilization of prophylactic medications and higher rates of hospitalization are more common among low-income children than among high-income children.1,2 Evidence for the link between socioeconomic status (SES) and the development of asthma is less strong—and is, in fact, contradictory.1,3 Many studies report asthma to be more prevalent among low-SES children, even in countries with universal health care insurance.4–7 However, no association with SES was reported in 1 study,8 and another study documented lower rates of asthma among low-SES children.9 The latter finding is congruent with the lower prevalence of atopic disease in developing countries10 and with the “hygiene” hypothesis, which proposes that exposure to infections and endotoxin is protective against atopic asthma.11 Low-income children have higher infection rates, although endotoxin levels are not always elevated in low-income households.12
Despite this level of uncertainty, it is common for household SES to be treated as a confounding factor and to be used to statistically adjust models testing the association between early life exposures and the development of childhood asthma. As low-income mothers are more likely to smoke and less likely to breastfeed,13,14 SES acts as a proxy measure for these exposures in the absence of available data. However, there is a lack of recognition that contradictory findings on the association of SES with childhood asthma may be a function of the validity of the SES measure. Low-income variables are fraught with measurement error, and there may be considerable fluctuation in household income over the course of a child's life from birth to adolescence.15 Measures of cumulative income, such as the frequency of low-income episodes over time, have shown stronger associations with poor health than have single-point measures.16 Other SES trajectories, such as downward or upward social mobility, have been reported to increase and decrease risk of cardiovascular disease, respectively.17 Fluctuations in family income also affect family functioning and maternal mental health.18
The effects of chronic poverty on child functioning and health have long been recognized.19,20 However, few studies have evaluated childhood asthma in relation to cumulative household income or income trajectories from the time of birth.21 Low-income households and neighborhoods are characterized by high levels of chronic stress,1,22 but no longitudinal studies have investigated the relationship between chronic poverty, chronic stress, and asthma development. To fill this gap in the literature, we studied the relationship between family SES trajectories starting from birth of the child and asthma development in early school age and adolescence. We used maximum-likelihood longitudinal latent-class modeling techniques to identify SES trajectories over time.15,23
METHODS
We conducted a longitudinal evaluation of 2868 children in the Western Australian Pregnancy Cohort (Raine) Study, born from 1989 to 1991 to mothers enrolled at gestational ages of 16 to 20 weeks at antenatal clinics at the main tertiary maternal hospital or nearby practices in Perth, Western Australia.24 Children were followed up at ages 1, 2, 3, 6, 8, 10, and 14 years. We then determined the likelihood of a child having asthma at ages 6 and 14 years according to the child's family-income trajectory over the child's lifetime.
Study measures were obtained from parent surveys administered during the Raine study. Some children were lost to follow-up or were missing data on asthma status, leaving sample totals of 2151 (75% of the Raine study sample) children at age 6 years and 1796 (63% of the study sample) children at age 14 years. Mothers of excluded children were more likely to be single parents, to have less education, and to experience life stress. However, because the Raine study recruited predominantly from a tertiary care hospital that serviced high-risk pregnancies, it overrepresented single parents at first recruitment (14.2%) compared with the general population of Western Australia (10.8%). Subsequent to loss to follow-up at age 14 years, the percentage of children living in single-parent families at age 1 year decreased to 11.6%, closer to the percentage of the general population of Western Australia. In comparison with children who remained in the study, single-parented children at age 1 year who were lost to follow-up at age 14 years did not differ from other children at age 6 years with regard to asthma prevalence or asthma risk factors, such as maternal asthma.
Family-Income Trajectories
We sought to identify trajectories of children with similar childhood experiences of economic disadvantage over time, using maximum-likelihood longitudinal latent-class modeling techniques15,25 rather than predetermined categories. The resultant longitudinal models classified children based on their family's movements in and out of low income over the child's lifetime. This group-based modeling strategy determined the probability of children's low income over time and simultaneously considered timing, duration, and sequencing of family low income. This analytic tool also incorporated the maximum-likelihood missing-data routine, which made maximal use of information on children with 1 or more years of missing data.
Families were first categorized by the dichotomous variable, low income, for each follow-up year. Low income was defined as reported household income of AU $27 000 per year or less (the cutoff value varied according to the income categories specified in each iteration of survey administration) until age 6 years. Because our research interest focused on relative poverty, low income after age 6 years was defined as reported income of $30 000 or less to reflect the increase in disposable income over the 1990s (per the Australian Bureau of Statistics).26 The cutoff values for low income captured the 2 lowest income quintiles of household income in the 1990s and included single-parent and 2-parent households that derived the majority of their income from government assistance.27
Once a family was classified as either low income or not, we used the SAS version 9.2 (SAS Institute Inc, Cary, NC) PROC TRAJ procedure to create income trajectories for the child's family from the time of the child's birth until the child reached age 6 years (first assessment of asthma status) and age 14 years (second assessment of asthma status). We used Bayes's theorem with PROC TRAJ to assign children to the income trajectory group to which they had the highest probability of belonging.15 A. L. K. specified the desired number of trajectories before running each model. Then, starting with 1 trajectory, PROC TRAJ was repeated until models were created for a full range of trajectories (1, 2, 3 … k trajectories).15 Following each iteration, trajectories were graphically represented and descriptive labels were assigned for the pattern of low income over time (e.g., stable, increasing, decreasing) to each trajectory.
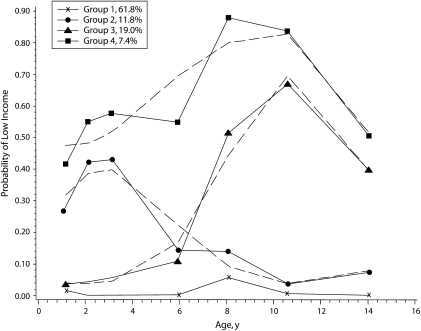
Figure 1 depicts a 4-trajectory model and the estimated probability of a child's membership in each trajectory. Trajectory 4 was labeled as chronic low income (7.4% of children), trajectory 3 was labeled as decreasing income (19%), trajectory 2 was labeled as increasing income (11.8%), and trajectory 1 was labeled as not ever low income (61.8%). Approximately 40% of children in the increasing-income trajectory lived in a low-income household before age 3 years; by age 6 years, this proportion had declined to 15% or less. By contrast, from 40% to 90% of children in the chronic-low-income trajectory had lived in a low-income family since birth.
FIGURE 1.
Probability of a child's membership in 4 low-income trajectories from birth until age 14 years: Western Australia Pregnancy Cohort (Raine) Study, Perth, Australia, 1989–2005.
The Bayesian Information Criterion (BIC) and a sample size–adjusted BIC were used to select the final number of trajectories, with the goal of identifying the fewest number of trajectories that best fit the data.15 The final number of trajectories was established when sequential comparisons of the BIC and adjusted BIC between models with k and k + 1 trajectories yielded no further substantial reductions in the BIC score with the k + 1 model. At age 6 years, the 2-trajectory model fit the data better than the 1-trajectory model; the BIC was reduced by 401 points, and the sample size–adjusted BIC was reduced by 404 points. There was no further improvement with the 3-trajectory model; BIC increased by 2, and the adjusted BIC decreased by 2. At age 14 years, the 4-trajectory model had an improved fit over the 3-trajectory model; BIC was reduced by 49 points, and the sample size–adjusted BIC was reduced by 53 points. The 5-trajectory model was associated with a minimal drop in the BIC and adjusted BIC (7 and 14 points, respectively).
Ultimately, a 2-category income measure (chronic low income vs not) was selected for the analyses at age 6 years, and a 4-category income measure (chronic low, increasing income, decreasing income, not ever low income; Figure 1) was selected for the analyses at age 14 years. These categories were then entered as predictors into the logistic regression model for asthma.
Asthma Outcome Measures
Current asthma at ages 6 years and 14 years was defined as ever having been diagnosed with asthma by a physician and wheeze or nocturnal cough and receipt of asthma medications (controller and reliever drugs) in the previous 12 months. Previous research has shown that children in the Raine cohort who met this definition of current asthma exhibited significant deficits in lung function and greater sensitivity to the methacholine challenge test for bronchial hyperreactivity.28,29 Risk and protective factors for asthma, derived from parent survey responses, were gender, household income, single-parent status at age 1 year, total number of siblings at birth, maternal history of asthma (recorded during pregnancy), maternal smoking during pregnancy, maternal smoking during the first year, preterm birth (< 37 weeks), low birth weight (< 2500 grams), elective cesarean delivery, maternal age younger than 20 years, maternal education less than high school, pregnancy and family stress indicator (composite score of more than 3 stressful life events from the Tennant and Andrews validated life-events instrument30), duration of exclusive breastfeeding, and pet ownership during the first year of life. The stress indicator was ascertained for the mother during pregnancy, at child age 1 year, and from birth of the child to age 6 or 14 years; the latter was labeled the chronic family stress measure.
Crude odds ratios (ORs) for asthma at ages 6 and 14 years were determined first, followed by ORs adjusted for the aforementioned confounding factors. We calculated ORs with multiple logistic regression analysis, using SAS software. Variables were retained in models at the 95% level of confidence. Separate models were tested for male and female children.
RESULTS
At any given time during the 14-year follow-up period, 8% to 21% of children were living in a low-income household (Table 1). Fourteen percent of children were experiencing chronic low income at age 6 years. This percentage decreased to 7% at age 14 years, when children in decreasing-income and increasing-income households were removed to create separate categories (Table 1 and Figure 1). Twelve percent of children were in increasing-income families at age 14 years. Decreasing-income households accounted for 19% of children at age 14 years. Children who had never lived in low-income households accounted for 86% of children at age 6 years; by age 14 years, this proportion had decreased to 62%.
TABLE 1.
Percentage of Children in Household Income Categories, by Child's Age: Western Australia Pregnancy Cohort (Raine) Study, Perth, Australia, 1989–2005
| Age 1 Year | Age 2 Years | Age 3 Years | Age 6 Years | Age 8 Years | Age 10 Years | Age 14 Years | |
| Low income, % (low-income cutoff) | 8.2 | 10.0 | 10.5 | 8.1 | 21.4 | 19.8 | 12.1 |
| (<$24 000) | (<$27 000) | (<$26 000) | (<$26 000) | (<$30 000) | (<$30 000) | (<$30 000) | |
| No. of trajectories identified | … | … | … | 2 | 3 | 4 | 4 |
| Chronic low income, % | … | … | … | 13.6 | 13.2 | 6.2 | 7.4 |
| Increasing income, % | … | … | … | … | … | 10.1 | 11.8 |
| Decreasing income, % | … | … | … | … | 18.9 | 19 | 19 |
| Not ever low income, % | … | … | … | 86.4 | 67.9 | 64.7 | 61.8 |
Chronic-low-income households were predominantly headed by females and by women who had not completed high school (Table 2). These families experienced the greatest number of stressful life events, as indicated by the life-events instrument. Almost half of the households with increasing income were also headed by females, the majority of whom had not completed high school. Multiple stressful events were also more common in these families. Family stress during pregnancy and the postpartum period was also associated with current asthma at age 6 years; maternal history of asthma and young age were seen more often in chronic-low-income households and with child asthma at age 6 years (data not shown). There were no asthma risk factors in common across income categories and current asthma at age 14 years.
TABLE 2.
Maternal and Family Characteristics of Each Income Trajectory, by Child's Age: Western Australia Pregnancy Cohort (Raine) Study, Perth, Australia, 1989–2005
| Single-Parent Status at Age 1 Year |
Mother Did Not Complete High School |
Family Stress at Age 1 Year |
||||
| Child Aged 6 Years, % | Child Aged 14 Years, % | Child Aged 6 Years, % | Child Aged 14 Years, % | Child Aged 6 Years, % | Child Aged 14 Years, % | |
| Chronic low income | 62.3 | 61.1 | 57.7 | 58.3 | 42.2 | 44.1 |
| Increasing income | … | 44.0 | … | 56.8 | … | 38.0 |
| Decreasing income | … | 9.6 | … | 58.7 | … | 26.3 |
| Not low income | 8.4 | 5.3 | 45.3 | 40.6 | 20.1 | 16.4 |
| Total population | 12.6 | 11.6 | 55.1 | 53.4 | 20.7 | 20.2 |
When defined as a dichotomous variable, low family income at age 1 year was not associated with asthma at age 6 years (unadjusted OR = 0.95; 95% confidence interval [CI] = 0.63, 1.42; adjusted OR [AOR] = 0.91; 95% CI = 0.60, 1.37). Similarly, there were no associations between low income at age 1 year and asthma at age 14 years (OR = 1.10; 95% CI = 0.62, 1.97; AOR = 0.97; 95% CI = 0.54, 1.75). No statistical associations were evident between low household income (defined as a dichotomous variable) at any age and asthma at ages 6 or 14 years.
Twenty-two percent of children living in chronic low-income families had asthma at age 6 years, compared with 18% of children not in this income group. Following adjustment for gender, preterm birth, maternal history of asthma, and dog ownership, the risk of asthma was higher among children in chronic low-income households, although it achieved marginal significance (OR = 1.30; 95% CI = 0.92, 1.83; Table 3). Further adjustment for pregnancy stress and for family stress at age 1 year or persistent family stress from ages 1 to 6 years diminished the low-income association with asthma to nonsignificance. Single-parent status was positively (but not significantly) associated with asthma at age 6 years (OR = 1.26; 95% CI = 0.91, 1.74) and the inclusion of this variable in the model also lessened the effect of chronic low income (data not shown).
TABLE 3.
Likelihood of Having Asthma at Ages 6 Years (n = 2151) and 14 Years (n = 1796), by Income Trajectory: Western Australia Pregnancy Cohort (Raine) Study, Perth, Australia, 1989–2005
| Asthma at Age 6 Years, OR (95% CI) | Asthma at Age 14 Years, OR (95% CI) | |
| Unadjusted model | ||
| Chronic low income | 1.30 (0.94, 1.81) | 1.67 (0.97, 2.86) |
| Increasing income | … | 0.79 (0.40, 1.55) |
| Decreasing income | … | 1.26 (0.87, 1.83) |
| Model adjusted for asthma risk factorsa | ||
| Chronic low income | 1.30 (0.92, 1.83) | 2.30 (1.23, 4.31) |
| Increasing income | … | 0.89 (0.43, 1.87) |
| Decreasing income | … | 1.31 (0.89, 1.93) |
| Single parent family at age 1 y | not in model | 0.49 (0.26, 0.94) |
| Model adjusted for asthma risk factorsa and stress at age 1 y | ||
| Chronic low income | 1.14 (0.74, 1.75) | 2.34 (1.22, 4.48) |
| Increasing income | … | 0.92 (0.44, 1.92) |
| Decreasing income | … | 1.29 (0.86, 1.94) |
| Single parent family at age 1 y | not in model | 0.40 (0.20, 0.80) |
| Pregnancy stress | 1.69 (1.15, 2.48) | 0.99 (0.54, 1.80) |
| Family stress at age 1 y | 1.42 (1.06, 1.90) | 1.25 (0.81, 1.91) |
| Model adjusted for asthma risk factorsa and chronic family stress | ||
| Chronic low income | 1.17 (0.82, 1.65) | 2.21 (1.17, 4.17) |
| Increasing income | … | 0.83 (0.39, 1.74) |
| Decreasing income | … | 1.25 (0.84, 1.85) |
| Single parent family at age 1 y | not in model | 0.45 (0.24, 0.87) |
| Pregnancy stress | 1.48 (1.05, 2.08) | 1.04 (0.59, 1.82) |
| Chronic family stress | 1.82 (1.16, 2.85) | 2.25 (1.28, 3.97) |
Note. OR = odds ratio; CI = confidence interval. Ellipses indicate not applicable. Reference category is never low income.
Asthma risk factors at age 6 years: gender, preterm birth, maternal asthma, and dog ownership in first year. Asthma risk factors at age 14 years: gender, maternal history of asthma, and cat ownership in first year.
The risk of asthma at age 6 years was significantly greater among male children exposed to chronic low income (OR = 1.64; 95% CI = 1.04, 2.57; AOR = 1.62; 95% CI = 1.02, 2.56). Among female children, this association was not seen (OR = 1.11; 95% CI = 0.68, 1.81; AOR = 1.01; 95% CI = 0.60, 1.69).
At age 14 years, current asthma was distributed by income trajectory as follows: 14% of the chronic low-income trajectory, 11% of the decreasing-income trajectory, and 9% of the never low-income trajectory. At 7%, children in the increasing-income group had the lowest prevalence of asthma. Following adjustment for gender, single-parent status, maternal history of asthma, and cat ownership, a statistically significant increased risk of asthma was observed in the chronic low-income group (OR = 2.30; 95% CI = 1.23, 4.31). The increased risk for chronic low income was minimally diminished following further adjustment for family stress at age 1 year or for persistent family stress from ages 1 to 14 years. In all models, single-parent status at age 1 year was associated with a lessened risk of asthma. There were no associations between asthma and the other income trajectories, although the OR for increasing income was consistently less than 1. When we implemented a contrast statement comparing the increasing-income trajectory to the chronic low-income group, the OR adjusted for single-parent status and other confounding factors was statistically significant at a value of 0.37 (95% CI = 0.16, 0.89).
The risk of asthma at age 14 years was 3-fold greater among female children exposed to chronic low income (AOR = 2.95; 95% CI = 1.22, 7.11). No associations were observed with the increasing-income and decreasing-income trajectories. The increased risk for chronic low income was not diminished following further adjustment for family stress at age 1 year or for persistent family stress from ages 1 to 14 years. Among male children, asthma at age 14 years was not significantly associated with any of the income trajectories (for chronic low income, AOR = 1.27; 95% CI = 0.59, 2.73; for increasing income, AOR = 0.87; 95% CI = 0.36, 2.12; for decreasing income, AOR = 1.15; 95% CI = 0.69, 1.91).
DISCUSSION
In a general cohort of 2000 children born in Western Australia in the early 1990s, we observed that children who had lived in a low-income household since birth had a 2-fold increased risk of having asthma at age 14 years. This finding confirms previous associations found between chronic poverty and asthma.20,21 We extended those findings in 2 important ways. First, we reported an association with asthma in adolescence. Second, we implemented measures of family-income trajectories created from statistical models. The trajectory method characterized sequential changes in family economic circumstances over time, such as increasing and decreasing income, and enabled us to parcel out the effects of chronic low income.
There were 4 other findings of note: (1) the association with chronic low income was stronger at age 14 years than at age 6 years, (2) the strength of the association was diminished after accounting for measures of family stress, (3) single-parent status and increasing income were associated with a decreased risk of asthma at age 14 years, and (4) the associations were gender specific. The plausibility and potential biological significance of each of these observations will be explored in detail.
Our definition of asthma had been validated previously.28,29 Further, use of longitudinal data over 14 years allowed us to study the association between children's SES trajectories and 2 asthma phenotypes (asthma at early school age and asthma at adolescence). We found that chronic low income had a stronger association with asthma at age 14 years than at age 6 years. It is well-documented that asthma persists into adolescence in up to one third of children with early-onset wheeze; in addition, persistent asthma has greater heritability and is more likely to be atopic.31 Our findings suggest that chronic low income may have a role to play in the development of persistent asthma.
In our study, family stress was twice as common in low-income households, and was more prevalent when poverty persisted. Pregnancy, early life stress, and chronic family stress were independently associated with asthma at age 6 years. These variables diminished the association between SES and asthma at age 6 years, suggesting that they play a role in the pathway between SES and child asthma. There is a growing body of literature on the association between child exposure to stress in early life and the development of asthma.32–34 Caregiver stress in early life has been associated with increased levels of TNF-α in infants, a proinflammatory cytokine in asthma.33 Scirica et al. reported that infants born into low-income households were more likely to have an atopic profile at birth, suggesting an influence of SES on the developing fetus.35 Their findings were more pronounced among male infants, consistent with our finding that chronic low income was associated with asthma at age 6 years among boys but not girls. Similarly, others have linked parental stress to asthma among boys but not girls at age 6 years.36
By age 14 years, chronic life stress was associated with a 2-fold increase in asthma, whereas pregnancy and early life stress were not. Others have also reported that low-income adolescents were more likely to be exposed to chronic stress over their lifetime and to have asthma.37,38 Family conflict has been known to precipitate elevated cortisol levels in children. Furthermore, heightened production of atopic cytokines, IL-5, and IL-13 has been reported in children with asthma experiencing higher stress levels, as have higher eosinophil counts.7,39 Children with asthma who simultaneously experience acute and chronic stress exhibit a reduction in expression of the glucocorticoid receptor, which can increase the airway inflammatory response to allergens.40 Finally, we found that chronic low income was strongly associated with asthma at age 14 years among girls but not boys. Although females with asthma are more likely to live in low-income environments, these findings are new to the literature.41
Our finding of an inverse association between having a single parent and having asthma at age 14 years suggests that children born to single parents live in a family SES environment that protects against asthma development. The single-parent effect appears to be related to the phenomenon of “moving out of poverty.” Single parents accounted for 44% of households in the increasing-income category. When single-parent status was added to models, it diminished the inverse association between increasing income and asthma. Moreover, when we compared the increasing-income trajectory to the chronic low-income trajectory, the risk of asthma was reduced by more than 60%.
Our results are akin to those of Chen et al., who showed that asthma likelihood was lower among children whose families had moved up in income than among children who continued to live in a low-income family.21 Children in low-income households experience higher rates of exposure to endotoxin and infections, which may protect against asthma development.11 These exposures may disappear once household income improves,42 but by then they would have had their effect in shaping the developing immune system during infancy.43 On the other hand, persistence of these exposures may increase risk for asthma. Celedon et al reported that endotoxin exposure in early life protected against the development of atopy, but exposure in later life increased the risk of atopy.44 It is also conceivable that stress levels in these families were lessened as they moved out of poverty; recent literature indicates that persistent stress has the greatest association with asthma.32
Although our findings have biological plausibility, they may be attributed to features of study design and execution. Reverse causation might explain the association between chronic low income and asthma because families caring for children with asthma report fewer hours of employment.45 Reverse causation would not account for the inverse association between single parenthood and asthma, however. Loss to follow-up was also not a likely explanation for this inverse association because single-parented children lost to follow-up did not have higher asthma rates at age 6 years than did children remaining in the study. Our definition of asthma, which specifies treatment with asthma medications, could have resulted in the misclassification of asthma status among children in single-parent families; children in single-parent households are less likely to receive controller asthma medications.46 However, the same would hold true for children in chronic low-income families,2 for which an inverse association was not observed.
In sum, we found an association between chronic exposure to a low-income environment from birth and the development of persistent asthma. In addition, we observed a protective effect against asthma among those children whose families had moved out of poverty. We propose family stress and endotoxin exposure in low-income households as explanations for these findings. Our findings give credence to the notion that SES “gets under the skin” to cause disease, but further study is required to elucidate specific pathways in asthma. However, our research does show that household SES has limited explanatory power as a static exposure measure and may hide valuable evidence for its role in asthma development.
Acknowledgments
The authors wish to acknowledge the Raine Medical Research Foundation, University of Western Australia, and the National Health and Medical Research Council for funding the establishment and continuation of this birth cohort.
Sincere thanks are due to all study families, without whose participation this research could not have been conducted. Many thanks are also extended to the Western Australian Pregnancy Cohort study investigators and research staff. A. L. Kozyrskyj would like to thank Melinda Berinson and all of the other staff at TICHR for their research support of this project.
Human Participant Protection
This study was approved by the institutional ethics committee of the Princess Margaret Hospital for Children.
References
- 1.Gold DR, Wright R. Population disparities in asthma. Annu Rev Public Health 2005;26:89–113 [DOI] [PubMed] [Google Scholar]
- 2.Kozyrskyj AL, Mustard CA, Simons FE. Inhaled corticosteroids in childhood asthma: income differences in use. Pediatr Pulmonol 2003;36(3):241–247 [DOI] [PubMed] [Google Scholar]
- 3.Kozyrskyj AL, O'Neil JD. The social construction of childhood asthma: changing explanations of the relationship between socioeconomic status and asthma. Crit Public Health 1999;9(3):197–210 [Google Scholar]
- 4.Claudio L, Stingone JA, Godbold J. Prevalence of childhood asthma in urban communities: the impact of ethnicity and income. Ann Epidemiol 2006;16(5):332–340 [DOI] [PubMed] [Google Scholar]
- 5.Basagana X, Sunyer J, Kogevinas M, et al. Socioeconomic status and asthma prevalence in young adults: the European Community Respiratory Health Survey. Am J Epidemiol 2004;160(2):178–188 [DOI] [PubMed] [Google Scholar]
- 6.Levesque B, Rhainds M, Ernst P, et al. Asthma and allergic rhinitis in Quebec children. Can Respir J 2004;11(5):343–348 [DOI] [PubMed] [Google Scholar]
- 7.Lindbaek M, Wefring KW, Grangard EH, Ovsthus K. Socioeconomical conditions as risk factors for bronchial asthma in children aged 4–5 yrs. Eur Respir J 2003;21(1):105–108 [DOI] [PubMed] [Google Scholar]
- 8.Hancox RJ, Milne BJ, Taylor DR, et al. Relationship between socioeconomic status and asthma: a longitudinal cohort study. Thorax 2004;59(5):376–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shankardass K, McConnell RS, Milam J, et al. The association between contextual socioeconomic factors and prevalent asthma in a cohort of Southern California school children. Soc Sci Med 2007;65(8):1792–1806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stewart AW, Mitchell EA, Pearce N, Strachan DP, Weilandon SK. The relationship of per capita gross national product to the prevalence of symptoms of asthma and other atopic diseases in children (ISAAC). Int J Epidemiol 2001;30(1):173–179 [DOI] [PubMed] [Google Scholar]
- 11.Schaub B, Lauener R, von ME. The many faces of the hygiene hypothesis. J Allergy Clin Immunol 2006;117(5):969–977 [DOI] [PubMed] [Google Scholar]
- 12.Perzanowski MS, Miller RL, Thorne PS, et al. Endotoxin in inner-city homes: associations with wheeze and eczema in early childhood. J Allergy Clin Immunol 2006;117(5):1082–1089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elliott L, Arbes SJ, Harvey ES, et al. Dust weight and asthma prevalence in the National Survey of Lead and Allergens in Housing (NSLAH). Environ Health Perspect 2007;115(2):215–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Almqvist C, Egmar AC, van Hage-Hamsten M, et al. Heredity, pet ownership, and confounding control in a population-based birth cohort. J Allergy Clin Immunol 2003;111(4):800–806 [DOI] [PubMed] [Google Scholar]
- 15.Wagmiller RL, Lennon MC, Kuang L, Alberti PM, Aber JL. The dynamics of economic disadvantage and children's life chances. Am Sociol Rev 2006;71(5):847–866 [Google Scholar]
- 16.Turrell G, Lynch JW, Leite C, Raghunathan T, Kaplan GA. Socioeconomic disadvantage in childhood and across the life course and all-cause mortality and physical function in adulthood: evidence from the Alameda County Study. J Epidemiol Community Health 2007;61(8):723–730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hallqvist J, Lynch J, Bartley M, Lang T, Blane D. Can we disentangle life course processes of accumulation, critical period and social mobility? An analysis of disadvantaged socio-economic positions and myocardial infarction in the Stockholm Heart Epidemiology Program. Soc Sci Med 2004;58(8):1555–1562 [DOI] [PubMed] [Google Scholar]
- 18.Dearing E, Taylor BA, McCartney K. Implications of family income dynamics for women's depressive symptoms during the first 3 years after childbirth. Am J Public Health 2004;94(8):1372–1377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aber JL, Bennett NG, Conley DC, Li J. The effects of poverty on child health and development. Annu Rev Public Health 1997;18:463–483 [DOI] [PubMed] [Google Scholar]
- 20.Seguin L, Nikiema B, Gauvin L, Zunzunegui MV, Xu Q. Duration of poverty and child health in the Quebec Longitudinal Study of Child Development: longitudinal analysis of a birth cohort. Pediatrics 2007;119(5):e1063–e1070 [DOI] [PubMed] [Google Scholar]
- 21.Chen E, Martin AD, Matthews KA. Trajectories of socioeconomic status across children's lifetime predict health. Pediatrics 2007;120(2):e297–e303 [DOI] [PubMed] [Google Scholar]
- 22.Wright RJ. Health effects of socially toxic neighborhoods: the violence and urban asthma paradigm. Clin Chest Med 2006;27(3):413–421 [DOI] [PubMed] [Google Scholar]
- 23.Nagin DS. Analyzing developmental trajectories: a semi-parametric, group-based approach. Psychol Methods 1999;4(2):139–157 [DOI] [PubMed] [Google Scholar]
- 24.Newnham JP, Evans SF, Michael CA, Stanley FJ, Landau LI. Effects of frequent ultrasound during pregnancy: a randomised controlled trial. Lancet 1993;342(8876):887–891 [DOI] [PubMed] [Google Scholar]
- 25.Jones BL, Nagin DS, Roeder KA. SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res 2001;29(3):374–393 [Google Scholar]
- 26.Household Income and Income Distribution Canberra: Australian Bureau of Statistics; 2007. Report 6523. [Google Scholar]
- 27.Focus on Families: Income and Housing Canberra: Australian Bureau of Statistics; 1995. Report 4424 [Google Scholar]
- 28.Joseph-Bowen J, de Klerk NH, Firth MJ, Kendall GE, Holt PG, Sly PD. Lung function, bronchial responsiveness, and asthma in a community cohort of 6-year-old children. Am J Respir Crit Care Med 2004;169(7):850–854 [DOI] [PubMed] [Google Scholar]
- 29.Joseph-Bowen J, de Klerk N, Holt PG, Sly PD. Relationship of asthma, atopy, and bronchial responsiveness to serum eosinophil cationic proteins in early childhood. J Allergy Clin Immunol 2004;114(5):1040–1045 [DOI] [PubMed] [Google Scholar]
- 30.Tennant C, Andrews G. A scale to measure the stress of life events. Aust N Z J Psychiatry 1976;10(1):27–32 [DOI] [PubMed] [Google Scholar]
- 31.Martinez FD. What have we learned from the Tucson Children's Respiratory Study? Paediatr Respir Rev 2002;3(3):193–197 [DOI] [PubMed] [Google Scholar]
- 32.Kozyrskyj AL, Mai XM, McGrath P, Hayglass KT, Becker AB, Macneil B. Continued exposure to maternal distress in early life is associated with an increased risk of childhood asthma. Am J Respir Crit Care Med 2008;177(2):142–147 [DOI] [PubMed] [Google Scholar]
- 33.Wright RJ, Finn P, Contreras JP, et al. Chronic caregiver stress and IgE expression, allergen-induced proliferation, and cytokine profiles in a birth cohort predisposed to atopy. J Allergy Clin Immunol 2004;113(6):1051–1057 [DOI] [PubMed] [Google Scholar]
- 34.Klinnert MD, Nelson HS, Price MR, Adinoff AD, Leung DY, Mrazek DA. Onset and persistence of childhood asthma: predictors from infancy. Pediatrics 2001;108(4):E69. [DOI] [PubMed] [Google Scholar]
- 35.Scirica CV, Gold DR, Ryan L, et al. Predictors of cord blood IgE levels in children at risk for asthma and atopy. J Allergy Clin Immunol 2007;119(1):81–88 [DOI] [PubMed] [Google Scholar]
- 36.Milam J, McConnell R, Yao L, Berhane K, Jerrett M, Richardson J. Parental stress and childhood wheeze in a prospective cohort study. J Asthma 2008;45(4):319–323 [DOI] [PubMed] [Google Scholar]
- 37.Chen E, Hanson MD, Paterson LQ, Griffin MJ, Walker HA, Miller GE. Socioeconomic status and inflammatory processes in childhood asthma: the role of psychological stress. J Allergy Clin Immunol 2006;117(5):1014–1020 [DOI] [PubMed] [Google Scholar]
- 38.Chen E, Fisher EB, Bacharier LB, Strunk RC. Socioeconomic status, stress, and immune markers in adolescents with asthma. Psychosom Med 2003;65(6):984–992 [DOI] [PubMed] [Google Scholar]
- 39.Flinn MV, England BG. Social economics of childhood glucocorticoid stress response and health. Am J Phys Anthropol 1997;102(1):33–53 [DOI] [PubMed] [Google Scholar]
- 40.Miller GE, Chen E. Life stress and diminished expression of genes encoding glucocorticoid receptor and beta2-adrenergic receptor in children with asthma. Proc Natl Acad Sci USA 2006;103(14):5496–5501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meng YY, Wilhelm M, Rull RP, English P, Nathan S, Ritz B. Are frequent asthma symptoms among low-income individuals related to heavy traffic near homes, vulnerabilities, or both? Ann Epidemiol 2008;18(5):343–350 [DOI] [PubMed] [Google Scholar]
- 42.Gereda JE, Klinnert MD, Price MR, Leung DY, Liu AH. Metropolitan home living conditions associated with indoor endotoxin levels. J Allergy Clin Immunol 2001;107(5):790–796 [DOI] [PubMed] [Google Scholar]
- 43.Williams LK, Oliver J, Peterson EL, et al. Gene-environment interactions between CD14 C-260T and endotoxin exposure on Foxp3+ and Foxp3- CD4+ lymphocyte numbers and total serum IgE levels in early childhood. Ann Allergy Asthma Immunol 2008;100(2):128–136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Celedon JC, Milton DK, Ramsey CD, et al. Exposure to dust mite allergen and endotoxin in early life and asthma and atopy in childhood. J Allergy Clin Immunol 2007;120(1):144–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smith LA, Hatcher JL, Wertheimer R. The association of childhood asthma with parental employment and welfare receipt. J Am Med Womens Assoc 2002;57:11–15 [PubMed] [Google Scholar]
- 46.Chen AY, Escarce JJ. Family structure and the treatment of childhood asthma. Med Care 2008;46:174–184 [DOI] [PubMed] [Google Scholar]