Abstract
Cross-lagged panel analysis of interview data collected from survivors of traumatic physical injury (N = 677) was used to examine the temporal relationship between anxiety sensitivity and posttraumatic stress disorder (PTSD) symptom severity. The two constructs were assessed at three time points: within days of physical injury, at 6-month follow-up and at 12-month follow-up. Results indicated that anxiety sensitivity and PTSD symptom severity were reciprocally related such that anxiety sensitivity predicted subsequent PTSD symptom severity and symptom severity predicted later anxiety sensitivity. Findings have both theoretical and clinical implications.
Keywords: Anxiety sensitivity, posttraumatic stress disorder, cross-lagged panel analysis, structural equation modeling, physical injury
Why are some people more susceptible than others to adverse reactions following trauma exposure? This question has stimulated an abundance of potential explanations and one construct, anxiety sensitivity (Reiss & McNally, 1985; Taylor, 1999), has drawn particular interest (e.g., Asmundson & Stapleton, 2008; Lang, Kennedy, & Stein, 2002; Vujanovic, Zvolensky, & Bernstein, 2008). Regarded as a cognitive vulnerability characterized by fear of anxiety and anxiety-related sensations, anxiety sensitivity is generally viewed as a trait-like constellation of interrelated physical, cognitive and social fears stemming from misinterpretation of symptoms of anxiety (Reiss & McNally, 1985). These misapprehensions include fear that externally observable bodily reactions (e.g., shakiness) will elicit social derision, that physical sensations may be harbingers of negative health states (e.g., a heart attack), and that an inability to concentrate is reflective of mental problems (Taylor, 1999).
Anxiety sensitivity may accentuate posttraumatic stress reactions in at least two ways. Individuals with preexisting anxiety sensitivity may respond more extremely to a traumatic stressor, distressed not only by the event but also by their own reactions. In this way, fear of anxiety may promote sensitization to trauma, lowering the threshold for fear reactions to traumatic events and increasing the possibility that exposure to relatively insignificant stressors might subsequently provoke adverse posttraumatic reactions (Rosen & Schulkin, 1998). Secondly, a traumatic event may generate both anxiety sensitivity and posttraumatic distress with anxiety sensitivity ultimately serving to amplify adverse reactions. In this instance, fear of anxiety might be instigated, for example, by the pairing of previously innocuous arousal sensations with aversive reactions in a manner consistent with a classical conditioning account of PTSD onset and maintenance (e.g., Keane, Zimering, & Caddell, 1985). For similar conjecture about the role of anxiety sensitivity in PTSD, see Taylor (2003). In each circumstance, posttraumatic distress—which is characterized by three symptom clusters reflecting (a) reexperiencing of the event (e.g., intrusive thoughts), (b) avoidance of reminders of the event and emotional numbing, and (c) hyperarousal (e.g., exaggerated startle response) (American Psychiatric Association, 2000)—is heightened by anxiety sensitivity.
A small but growing body of research provides indirect evidence that anxiety sensitivity may predispose certain individuals to elevated risk of posttraumatic stress reactions (Asmundson & Stapleton, 2008; Bryant & Panasetis, 2001; Collimore, McCabe, Carleton, & Asmundson, 2008; Fedoroff, Taylor, Asmundson, & Koch, 2000; Feldner, Zvolensky, Schmidt, & Smith, 2008; Lang et al., 2002; Stewart, Conrod, Samoluk, Pihl, & Dongier, 2000; Vujanovic et al., 2008). In a cross-sectional study of 51 trauma survivors, for example, Bryant and Panasetis (2001) reported that individuals who met screening criteria for acute stress disorder had higher anxiety sensitivity relative to their counterparts. Similarly, in a prospective examination of symptoms of PTSD in a non-clinical sample of over 400 young adults, Feldner et al. (2008) observed that anxiety sensitivity was predictive of symptoms over an 18 month period.
The construct of anxiety sensitivity offers the promise of yielding important insights into the development and maintenance of PTSD and may stimulate new therapeutic interventions for the treatment of posttraumatic distress (e.g., Wald & Taylor, 2008). Yet, several issues require further examination. First, much research examining anxiety sensitivity has relied on cross-sectional designs (e.g., Asmundson & Stapleton, 2008; Bryant & Panasetis, 2001; Collimore et al., 2007; Fedoroff et al., 2002). Although such research can yield suggestive findings, prospective studies that incorporate multiple waves of data collection provide a better basis for drawing inferences regarding causality (Finkel, 1995).
Furthermore, of the existing prospective studies in which anxiety sensitivity has been shown to predict subsequent PTSD symptoms (e.g., Feldner et al., 2008; Simpson Jakupcak, & Luterek, 2006), none have adjusted for initial levels of posttraumatic distress. In their examination of nearly 50 trauma-exposed women, for example, Simpson et al. (2006) found that anxiety sensitivity predicted subsequent PTSD symptoms. Yet, without having accounted for preexisting posttraumatic distress, this approach does not allow determination of the extent to which anxiety sensitivity actually contributes to subsequent trauma-related distress. In other words, this analytic strategy leaves open the possibility that preexisting, but unmeasured, posttraumatic distress—rather than anxiety sensitivity—shapes subsequent PTSD symptoms.
Moreover, existing research has not investigated the possibility that PTSD symptoms might themselves directly affect anxiety sensitivity. It is at least conceivable that the repeated experiencing of aversive intrusions and heightened arousal that characterize posttraumatic distress might accentuate subsequent sensitivity to these anxiety reactions (Taylor, 1999; p. 346–347). For example, repeated physiological arousal in response to trauma reminders could lead an individual with PTSD to develop a fear of such arousal-related sensations. Insofar as posttraumatic distress may influence anxiety sensitivity, existing evidence mischaracterizes the true nature of the relationship between the two constructs, and overstates the impact of anxiety sensitivity on posttraumatic distress.
To examine these issues, we employed a cross-lagged panel analytic framework (Finkel, 1995; Kenny, 1979) within a latent variable context. A major advantage of latent variable modeling over more traditional approaches such as those typically used in research examining the link between anxiety sensitivity and posttraumatic distress is that the former adjusts for differential reliability of measurement (Bollen, 1989). Without this adjustment, it is difficult to determine whether the apparent association between constructs of interest faithfully reflects underlying relations or is biased by differences in the reliability with which constructs are measured. A second benefit of latent variable modeling is that this approach permits assessment of the extent to which the model fits the data (Jöreskog, 1993). Thus, latent variable modeling allows for explicit formulation and comparison of alternative models for the data. Finally, although not unique to latent variable modeling, this technique enables constructs to be represented as both antecedents and consequences, thereby providing models that more closely parallel the complex nature of most clinical phenomena.
The broad aim of the current study was to examine the relationship between anxiety sensitivity and PTSD symptom severity in a sample of individuals who had been hospitalized for treatment of serious physical injuries. Traumatic physical injury exacts an enormous individual and societal toll. Each year approximately 1.5 million persons in the U.S. suffer a physical injury serious enough to require hospitalization (Vyrostek, Annest, & Ryan, 2004). In excess of 20% of hospitalized trauma survivors experience symptoms consistent with PTSD within twelve months of hospitalization (Zatzick et al., 2007). Thus, physical trauma constitutes a particularly important arena in which to evaluate the interconnectedness of anxiety sensitivity and posttraumatic distress following trauma exposure.
Using structural equation modeling of three waves of data obtained from a prospective, longitudinal investigation of the natural course of psychological adjustment following traumatic physical injury, the current study had three objectives: (a) to determine whether anxiety sensitivity prospectively predicts PTSD symptom severity; (b) to assess whether PTSD symptom severity prospectively affects anxiety sensitivity; and (c) to examine whether a reciprocal influence exists such that initial levels of each are associated with subsequent levels of the other.
Method
Participants and Procedures
The sample was recruited between February 2004 and August 2006 from four trauma centers in Los Angeles County: Los Angeles County + University of Southern California Medical Center (LAC+USC), UCLA Medical Center, King-Drew Medical Center, and California Hospital Medical Center. Together, these trauma centers serve a majority of all persons needing specialized trauma care in Los Angeles County. Adult patients were eligible for the study if they met the requirements for the Los Angeles County Trauma registry. The purpose of the registry is to facilitate monitoring of individuals who have suffered potentially life-threatening injuries that required emergent hospitalization and surgical intervention. Trauma patients were ineligible to participate, if they (1) could not communicate in English or Spanish; (2) had been incarcerated at hospital admission; (3) had been homeless prior to hospitalization and expected to be homeless upon discharge; (4) had cognitive impairment that precluded informed consent; or (5) had experienced injuries from family violence or attempted suicide.
Recruitment followed a two stage procedure: stage one identified admitted patients thought to be eligible for the study and stage two used a face-to-face screening interview to verify eligibility. Different methods for identification of potentially eligible individuals were used at the four hospitals due to differences in IRB-approved protocols. At LAC+USC, research staff had direct access to computerized admission records. At the remaining three trauma centers, research staff did not have direct access to medical records, and medical personnel notified research staff of the presence of individuals who appeared to meet study eligibility requirements.
Patients who appeared to be possible candidates (N = 1133) were then approached in their rooms to screen in a face-to-face interview to assess additional eligibility criteria. With one exception, interviewers attempted to screen all patients identified as potentially eligible. Specifically, using order of admission, the research staff approached only every other Hispanic patient at LAC+USC. This random sampling strategy adjusted for the known overrepresentation of Hispanics at this trauma center relative to the overall population served by the Los Angeles County trauma service.
Of persons screened, 10.3% were excluded because they were unable to converse in either English or Spanish, 10.0% because they were homeless and could not give contact information for a follow up interview, 2.4% because injuries were due to an attempted suicide, 1.4% because injuries were caused by family violence, and 0.9% because they had a cognitive impairment that prevented informed consent or understanding the interview. Eighty-nine percent of attempted screenings were completed. To meet the preference of participants, interviews were completed in either English or Spanish.1
Of the 850 patients identified as eligible based on screening, 677 (80%) completed the baseline interview at a median of 9 days following the trauma. Of the 677 who completed an initial interview, 476 (70%) completed 6-month follow-up interviews and 462 (68%) completed 12-month follow-up interviews. The sample averaged 33.31 (SD = 11.72) years of age, and 29.5% of participants were either married (18.5%) or cohabiting (11%). With respect to race/ethnicity, 48.7% identified as Hispanic, 25.3% as non-Hispanic Caucasian, 19.9% as African-American, and 6.1% as another category. Most participants had experienced blunt trauma injuries related to motor vehicle collisions (57.6%), whereas others had survived community violence, i.e., primarily gunshot or knife wounds (36.3%), or other incidents (8.6%).2
The team of screeners and interviewers consisted of individuals who had prior experience in conducting research interviews. Interviewers received 5 full days of training and were required to perform satisfactorily on mock interviews before being approved to begin study interviews. Participants were given $25 for each completed assessment. All participants provided informed consent and study procedures were approved and monitored by the Institutional Review Boards of the RAND Corporation, LAC+USC Medical Center, UCLA Medical Center, King-Drew Medical Center, and California Hospital Medical Center.
Measures
PTSD symptom severity
The civilian version of the Posttraumatic Stress Disorder Checklist (PCL; Weathers et al., 1993) was administered via interview to assess PTSD symptom severity at all three waves. The PCL is a 17 item measure of PTSD symptoms in which participants rate the degree to which they were bothered by each symptom. Responses are provided on a scale ranging from 1 (not at all) to 5 (extremely). At all interviews, symptoms were assessed with respect to the injury as the focal event. At the initial interview, participants were asked to respond with respect to symptoms experienced since the injury. At follow-up interviews, participants answered with respect to the previous two week period. The PCL has been used in diverse samples and possesses solid psychometric properties (Andrykowski, Cordova, Studts & Miller, 1998; Blanchard, Jones-Alexander, Buckley & Forneris, 1996; Denson, Marshall, Schell, & Jaycox, 2007). Descriptive statistics for the PCL at each wave of data collection are displayed in Table 1.
Table 1.
Means and Standard Deviations by Assessment for the PCL and ASI
| Instrument | Assessment |
||
|---|---|---|---|
| Baseline | 6-month | 12-month | |
| PCL | |||
| M | 39.3 | 39.0 | 36.6 |
| SD | 15.2 | 16.8 | 16.1 |
| ASI | |||
| M | 17.8 | 17.1 | 16.3 |
| SD | 12.9 | 13.8 | 14.0 |
Note. For descriptive purposes, scores were derived by summing across PCL and ASI items. Results were generated using Full Information Maximum Likelihood estimation. PCL = Posttraumatic Symptom Checklist (Weathers et al., 1993); ASI = Anxiety Sensitivity Index (Peterson & Reiss, 1992).
Anxiety sensitivity
Anxiety sensitivity was assessed via interview with the Anxiety Sensitivity Index (ASI; Peterson & Reiss, 1992). The ASI is perhaps the most widely used measure of anxiety sensitivity, and numerous studies attest to the reliability and validity of this 16-item measure (Stewart, Taylor & Baker, 1997; Rector, Szacun-Shimizu, & Leybman, 2007). Participants are asked about the experience of fear as it relates to interpretation of their own anxiety-related symptoms (e.g., “Unusual body sensations scare me”). Responses are provided on a 5-pointscale, ranging from 0 (very little) to 4 (very much). At all three interviews, participants were asked to respond without respect to a specific time frame. Descriptive statistics for the ASI at each wave of data collection are displayed in Table 1.
Data Analysis
Our general approach to latent variable modeling involved the implementation of cross-lagged path analysis (e.g., Finkel, 1995; Kenny, 1979), using the Mplus 5.1 software program (Muthén & Muthén, 2008). This modeling technique is widely used to assess causal models in data derived from nonexperimental, longitudinal research designs (Finkel, 1995). Degree of model fit was assessed using the robust chi-square goodness of fit statistic, the comparative fit index (CFI; Bentler, 1990), the Tucker-Lewis Index (TLI; Tucker & Lewis, 1973), the root-mean-square error of approximation (RMSEA; Browne & Cudeck, 1993), and the standardized root mean square residual (SRMR; Bentler, 1995).
To determine model acceptability, Hu and Bentler (1999) have suggested use of 0.95 for the CFI or TLI as well as .06 and 0.08 for the RMSEA and SRMR, respectively. However, these recommendations have stimulated debate about the extent to which any set of criteria holds across all possible applications (Marsh, Hau, & Wen, 2004). Nonetheless, the models tested herein fit comfortably within these guidelines. Because several variables were not normally distributed, a robust chi-squared statistic and standard errors (T2*, Yuan & Bentler, 2000) were used, as implemented in Mplus with the MLR command. When models were nested, we compared them using the scaled difference χ2 test, which adjusts for the scaling correction factor used in MLR estimation (Satora & Bentler, 2001).
To account for sample attrition, we conducted all analyses using expectation maximization (EM) parameter estimates (McLachlan & Krishnan, 1996). This technique for handling missing data avoids sample biases that can occur when one excludes from the analyses those participants who missed one or more follow-up interviews (Little & Rubin, 1987). In addition, this technique provides an unbiased method for increasing inferential power when data are missing at random or completely at random as discussed by Little and Rubin (1987).
To minimize the number of parameters requiring estimation, we created three indicators from the 16 ASI items by aggregating across sets of items reflecting physical, social, and cognitive aspects of anxiety sensitivity. For this purpose, we used the three-first-order factors corresponding to physical, mental, and social concerns as reported by Zinbarg, Mohlman, and Hong (1999). Three PTSD item indicators were also created as observed measures of a single latent PTSD construct by aggregating symptoms within each of the three DSM symptom clusters. That is, separate indices were created for Reexperiencing, Avoidance and Numbing, and Hyperarousal symptom clusters. These six latent variables were used for all three assessments.
Models were developed in a series of steps, following standard guidelines which call for developing an acceptable measurement model prior to incorporating structural parameters (e.g., Bentler, 2000; Mulaik & Millsap, 2000). In an initial step, we fit models for anxiety sensitivity and PTSD symptom severity, using all three waves of data simultaneously. All latent variables were permitted to correlate freely with one another. Correlated errors were also estimated between analogous measured variables across time (Cole, Ciesla, & Steiger, 2007). For example, the unique variance of PTSD Reexperiencing symptoms at initial assessment was permitted to correlate with the unique variance of Reexperiencing symptoms at the 6-month follow-up assessment.
In the next stage, we examined a series of progressively more stringent hypotheses regarding the equivalence of parameters across assessments. Focusing first on the measurement component of the model, we tested the assumption that analogous factor loadings could be constrained to equality across the three assessments. For example, we tested the hypothesis that the loading of the ASI Physical Symptoms cluster on anxiety sensitivity at baseline was equivalent to the loadings of this symptom cluster on anxiety sensitivity at the 6- and 12-month assessments.
In a second step, we tested cross-lagged models in which latent variables at each assessment were represented as having a path to the other latent variable at the subsequent assessment. Thus, for example, PTSD at the initial assessment was modeled as having a causal influence on anxiety sensitivity as measured at the 6-month assessment. Similarly, anxiety sensitivity at the initial assessment was modeled as affecting PTSD symptom severity as measured at the 6-month assessment. Additionally, we tested both autoregressive and cross-lagged paths from baseline to the 12-month assessment. We retained those effects which gave a statistically significant improvement in the fit of the model.
We then tested constraints representing more strict hypotheses about the structural component of the model. In particular, we examined the tenability of the assumption that analogous regression coefficients were equivalent across time. Thus, for example, we tested the hypothesis that the path from initial PTSD symptom severity to 6-month PTSD symptom severity was equivalent to the path from 6-month PTSD symptom severity to 12-month symptoms.
Results
Descriptive Analyses
For descriptive purposes, overall indexes of PTSD symptom severity and anxiety sensitivity were computed by summing across the 17 PCL items and the 16 ASI items. The EM Maximum Likelihood estimated means and standard deviations for these measures are shown in Table 1 for the three assessments. PCL scores showed little evidence of decline with the passage of time. For the PCL scores, no statistically significant decline from baseline to 6 months was observed (difference = 0.37, 95% CIs 1.94, −1.69; p = 0.58). The decline from baseline to 12 months was statistically significant, but small (difference = 2.1, 95% CIs 0.81, 3.49; p = 0.002). For ASI scores, there was again no significant difference between the mean score at baseline, and the six month follow-up (difference = 0.66; 95% CIs = −0.51, 1.82; p = 0.27; however, the change from baseline to twelve months was statistically significant (difference = 4.0, 95% CIs = 2.8, 5.2; p < 0.001). We calculated coefficient alphas (Cronbach, 1951) for each scale. For the PCL, these coefficients were 0.90 for baseline, 0.93 for 6-month and 0.93 for 12-month follow-up assessments. For the ASI, the corresponding values were 0.90, 0.93, and 0.94, respectively.
A substantial portion of the sample reported clinically significant psychological distress at each assessment. For illustrative purposes, PCL responses were used to identify persons who met screening criteria for PTSD following the procedure recommended by Weathers et al. (1993). Specifically, individual symptoms receiving a score of 3 (moderately) or greater were treated as indicating symptom presence and mapped against the DSM–IV criteria B–D (American Psychiatric Association, 2000). Using this scoring strategy, 25.2% of participants met screening criteria for PTSD at the initial assessment (excluding duration), whereas 21.4% and 20.1% met criteria at the 6- and 12-month follow-up assessments, respectively.
Cross-Lagged Analyses
We followed the procedure described above to estimate a series of nested models which were then compared using the scaled chi-square difference test (Satorra & Bentler, 2001). Fit statistics for these models are shown in Table 2. An initial model, Model 0, consisted of a confirmatory factor analysis with three PTSD latent variables (i.e., one at each assessment) and three anxiety sensitivity latent variables (i.e., one at each assessment). As previously noted, each latent variable was operationalized by three measured indicators. No restrictions were placed on the covariances of the latent variables. Unique variances of analogous indicators across time were correlated. This model fit the data well, χ2 (102) = 137.2, CFI = 0.99, SRMR = 0.023, RMSEA = 0.024.
Table 2.
Fit Indices for Tested Models Involving Anxiety Sensitivity and Overall PTSD Symptom Severity
| Model | χ2 (df) | CFI | TLI | RMSEA | SRMR | Δχ2 (df and p value) |
|---|---|---|---|---|---|---|
| Model 0 | 137.2 (102) | 0.99 | 0.99 | 0.023 | 0.024 | --- |
| Model 1/1a | 162.1 (110) | 0.99 | 0.99 | 0.026 | 0.029 | 24.4 (8, p = .002) |
| Model 2 | 168.1 (112) | 0.99 | 0.99 | 0.027 | 0.031 | 6.2 (2, p = .046) |
| Model 3 | 195.7 (114) | 0.99 | 0.98 | 0.033 | 0.047 | 25.1 (2, p < .001) |
| Model 4 | 167.1 (114) | 0.99 | 0.99 | 0.026 | 0.031 | ---a |
| Model 5 | 169.1 (116) | 0.99 | 0.99 | 0.026 | 0.033 | 1.8 (2, p = .414) |
Note. CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; RMSEA = Root-Mean-Square Error of Approximation; SRMR = Standardized Root-Mean-Square Residual.
Model 4 was compared with Model 2. The test of the difference in fit gave a negativeχ2 statistic, and thus is not reported. Such a result is possible when the models are very close in fit (see Satorra & Bentler, 2001; Satorra & Bentler, 2008).
In Model 1, analogous factor loadings at different points in time were constrained to equality. Despite greater stringency, this model still provided an acceptable fit to the data, χ2 (110) = 162.1, CFI = 0.99, SRMR = 0.029, RMSEA = 0.026. Although the change in model fit was statistically significant by the nested χ2 difference test, the difference in the fit indices was minor, and the model was retained. In the next model, i.e., Model 1a, cross-time covariances were converted to regression estimates in which variables measured at a common time point were regressed onto those measured at previous time points, i.e., a fully cross-lagged model. Thus, for example, 12-month anxiety sensitivity was correlated with 12-month PTSD symptom severity and was modeled as predicted by PTSD symptom severity and anxiety sensitivity at both baseline and 6-month follow-up. Models 1 and 1a are both saturated at the structural level, and are therefore statistically equivalent. Hence, the fit statistics are unchanged.
In subsequent models, we added constraints to improve model parsimony (Bentler & Mooijart, 1989). In Model 2, we removed the paths from each latent variable at baseline to the opposite latent variable at 12 month follow-up (i.e., from baseline PTSD symptom severity to 12 month anxiety sensitivity, and from baseline anxiety sensitivity to 12-month PTSD symptom severity). These modifications resulted in worsened overall model fit, Δχ2 (2) = 6.2, p = 0.046. After weighing the modest improvement in model fit to be gained from retaining these paths against the accompanying loss of model parsimony, we chose to remove these paths.3 Next, we removed autoregressive paths from baseline to 12-month follow-up (Model 3) for equivalent latent variables (i.e., the path from PTSD at baseline to PTSD at 12-month follow-up, and from baseline anxiety sensitivity to anxiety sensitivity at 12-month follow-up. The chi-square increase for this constraint was statistically significant (Δχ2 (2) = 25.1, p < 0.001). In addition, the changes in the RMSEA (of 0.006 points) and particularly the SRMR (of 0.016 points) were relatively large. Thus, these paths were retained in subsequent models.
In Model 4, analogous autoregressive paths were constrained to equality as a partial test of stationarity, e.g., the path from PTSD symptom severity at baseline to PTSD symptom severity at 6-month follow-up was constrained to equal the path from PTSD symptom severity at 6-month assessment to PTSD symptom severity at 12-month follow-up. In the nested comparison of Models 2 and 4, the test resulted in a negative chi-square difference; such a negative value can occur when the difference between models is small, and a correction is applied (Satorra & Bentler 2001; Satorra & Bentler, 2008). Thus, these constraints were regarded as tenable and were incorporated.
Finally, for Model 5, we constrained analogous cross-lagged paths to equality as a test of full stationarity. Thus, for example, the path from PTSD symptom severity at baseline to anxiety sensitivity at 6 month follow-up was constrained to equal the path from PTSD symptom severity at 6 months to anxiety sensitivity at 12 months. Imposition of these constraints did not significantly worsen model fit, Δχ2 (2) = 1.8, p = 0.41, and incorporation of these constraints improves power to detect cross-lagged effects (Bentler & Mooijart, 1989). Thus, these restrictions were included. The resulting fully-crossed model proved a good fit to the data: χ2 (116) = 169, p = 0.001, CFI = 0.99, TLI = 0.99, SRMR = .033, RMSEA = 0.026.
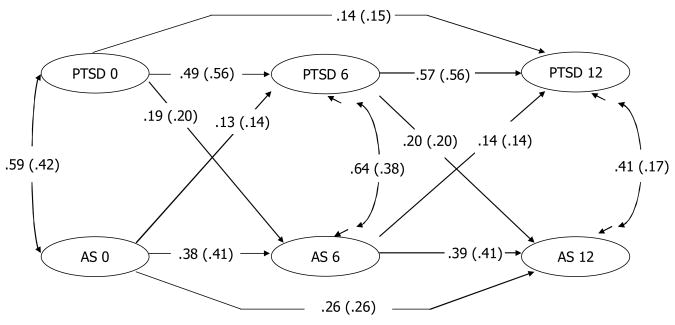
As shown in Figure 1, the paths from initial PTSD symptom severity and anxiety sensitivity to their counterparts at the six-month follow-up assessment was large and statistically significant. Similarly, the paths from 6-month PTSD symptom severity and anxiety sensitivity to their counterparts at the 12-month assessment provided evidence of stability over time. Results also revealed significant cross-lagged relationships involving anxiety sensitivity and PTSD symptom severity. In particular, anxiety sensitivity was positively associated with subsequent PTSD symptom severity such that anxiety sensitivity, as measured at one assessment, predicted PTSD symptom severity as measured at the following assessment. Thus, initial anxiety sensitivity was, for example, a significant predictor PTSD symptom severity at 6-months. Similarly, anxiety sensitivity at 6-month assessment predicted 12-month PTSD symptom severity. That is, individuals with high levels of anxiety sensitivity subsequently developed greater posttraumatic distress than did their less distressed peers, whereas those with lower levels of anxiety sensitivity subsequently experienced less posttraumatic distress relative to their peers. The opposite pattern was also found such that posttraumatic distress predicted subsequent anxiety sensitivity. Thus, PTSD symptom severity at initial assessment was a significant predictor of 6-month anxiety sensitivity. In like fashion, PTSD symptom severity at the 6-month assessment was positively linked with 12-month anxiety sensitivity.
Figure 1.
Structural model of cross-lagged relationship between anxiety sensitivity (AS) and PTSD symptom severity (PTSD), at baseline (0), 6 months (6), and 12 months (12). (The measurement model is not shown). Standardized parameter estimates are shown first, followed by unstandardized estimates in parentheses. Paths are statistically significant at p < 0.001, except paths from AS to subsequent PTSD symptoms, where p = 0.004, and from PTSD at baseline to PTSD at 12 months, where p = 0.003.
In addition, the contemporaneous correlations between the residuals of PTSD symptom severity and anxiety sensitivity (i.e., the partial correlations, controlling for previous assessment levels of both variables) were .64 (p < .001) and .41 (p < .001) for the 6- and 12-month follow-up assessments, respectively.
Discussion
This study used covariance structure modeling within a cross-lagged panel analytic framework to examine the interconnectedness of anxiety sensitivity and PTSD symptom severity in a longitudinal study of survivors of serious physical injury. To our knowledge, this research constituted the first examination of the reciprocal relations involving these constructs over multiple assessment points, with previous research focusing exclusively on the possibility that anxiety sensitivity is a causal factor in the development or maintenance of posttraumatic distress. This investigation also differs from others in adjusting for baseline levels of posttraumatic distress and anxiety sensitivity.
Several key findings emerged. First, these results show that anxiety sensitivity predicts future PTSD symptom severity even after adjusting for initial posttraumatic distress. Thus, individuals with high levels of anxiety sensitivity are less likely than their low sensitivity counterparts to experience decreases in posttraumatic distress with the passage of time following trauma exposure. Although other investigations have implicated anxiety sensitivity as a factor shaping the course of adjustment following trauma exposure (e.g., Federoff et al., 2000; Feldner et al., 2008), the current study provides the most rigorous empirical support for this relationship to date. For example, although Federoff et al. (2000) showed that anxiety sensitivity and PTSD symptom severity declined in tandem following treatment for PTSD, this investigation had limited ability to disentangle the causal relations between the two constructs.
Conversely, these results also suggest that PTSD symptoms influence anxiety sensitivity over time. Following trauma exposure, individuals with greater posttraumatic distress, for example, are likely to experience increased anxiety sensitivity. Despite long-standing conjecture that PTSD symptoms might exert an impact on anxiety sensitivity (Taylor, 1999), this study is, to our knowledge, the first to empirically demonstrate that increases in anxiety sensitivity are associated with earlier posttraumatic distress. Inasmuch as previous research has largely neglected this possible explanation of the association between the two constructs, this finding is particularly noteworthy.
Taken together, these findings suggest that the link between anxiety sensitivity and PTSD symptoms is more complex than has been generally appreciated. In particular, the interrelationship appears dynamic and reciprocal in that anxiety sensitivity and PTSD symptoms predict one another over time. This bidirectional pattern of associations indicates that existing research implicating anxiety sensitivity in the maintenance of PTSD symptoms is likely to have overestimated the actual magnitude of the relationship. In other words, a portion of any possible causal association between anxiety sensitivity and PTSD symptom severity identified in prior research (e.g., Asmundson & Stapleton, 2008; Vujanovic et al., 2008) might stem not from the impact of anxiety sensitivity on symptoms but from the influence of symptoms on anxiety sensitivity.
Although observed effect sizes are modest, these results may have important clinical implications. The reciprocal nature of the relationship of anxiety sensitivity and PTSD symptom severity indicates that the two phenomena are likely to act together to confer susceptibility to an insidious cycle in which increased symptoms of PTSD lead to intensified sensitivity to anxiety which, in turn, worsens PTSD symptom severity. These findings imply that clinicians might assess anxiety sensitivity as part of an overall evaluation of vulnerability and resilience factors prior to treatment onset.
Results also suggest that anxiety sensitivity is susceptible to therapies aimed at decreasing fear of anxiety and that these interventions might prove efficacious in treating PTSD. In other words, although anxiety sensitivity is often regarded as a dispositional construct, the apparently malleable nature of anxiety sensitivity offers the possibility that reduction in anxiety sensitivity may lead to lessened PTSD symptom severity. In fact, evidence indicates that interventions to diminish anxiety sensitivity and thereby to decrease PTSD symptoms may prove promising. For example, Wald and Taylor (2007) have provided preliminary evidence that interoceptive exposure—which involves gradual, repeated exposure to feared bodily sensations in supervised therapeutic exercises—can reduce anxiety sensitivity, presumably by helping participants to understand that these sensations are not associated with calamitous consequences (Stewart & Watt, 2008). Similar research also indicates that physical exercise may also serve to reduce anxiety sensitivity (Broman-Fulks & Storey, 2008; Smits et al., 2008). To the extent that either interoceptive exposure or physical exercise reduces anxiety sensitivity, these techniques may be useful as a prelude to therapy for the treatment of PTSD.
In considering these findings, several limitations are worthy of note. First, this study focused solely on the extent to which anxiety sensitivity and PTSD symptom severity serve to maintain one another. Thus, future research is needed to address the possibility that anxiety sensitivity might influence the actual development of symptoms of PTSD. Such research could also help to elucidate whether trauma exposure per se, might be a force in the emergence of anxiety sensitivity.
In addition, our sample was comprised of individuals who had experienced a sudden severe physical injury. To the extent that the relationship between anxiety sensitivity and PTSD symptom severity varies as a function of trauma type, further research is warranted in other samples such as individuals exposed to military combat, natural disaster, or sexual assault. Moreover, approximately three-quarters of our sample were males. Given that gender differences may exist in the mutual interdependence of anxiety sensitivity and PTSD symptom severity (Felder et al., 2008), further research with a larger sample of females is warranted. Similarly, inasmuch as the sample was largely comprised of Hispanics, additional research is required to determine whether findings hold for other ethnic and racial groups.
Furthermore, this research does not allow us to rule out the possibility that an unmeasured variable that correlates with both anxiety sensitivity and PTSD symptom severity might account for the observed pattern of findings. Insofar as neuroticism appears related to both constructs (Cox, Borger, Taylor, Fuentes, & Ross, 1999; Cox, MacPherson, Enns, & McWilliams, 2004), for example, future investigations might examine the possible role of neuroticism in explaining the relationship of anxiety sensitivity and PTSD symptoms. Finally, these results are silent as to the mechanisms linking PTSD symptoms and anxiety sensitivity, and additional study of this topic is needed.
Conclusion
In sum, this longitudinal study provides empirical evidence that anxiety sensitivity may affect, and be affected by, the severity of PTSD symptoms following traumatic physical injury. The reciprocal nature of the relationship of anxiety sensitivity and PTSD symptom severity shows how PTSD-related distress might be maintained in the aftermath of trauma. These results also suggest that anxiety sensitivity might be an important target for interventions aimed ultimately at reducing PTSD symptom severity.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (R01MH56122) and the National Institute on Alcohol Abuse and Alcoholism (R01AA014246). The views expressed are ours and do not necessarily reflect those of the NIAAA, the NIMH or RAND. We express appreciation to Drs. Howard Belzberg, Henry Cryer, Gudata Hinika, Peter Meade, and Vivek Shetty for facilitating data collection. We also thank the RAND Survey Research Group and Harris Interactive for their assistance with data collection. We gratefully acknowledge the generosity of the trauma survivors who participated in this study.
Footnotes
At baseline, 120 persons completed the interview in Spanish. A separate series of analyses were conducted after omitting this group. An essentially identical pattern of findings emerged for participants who completed the interview in English as compared to the combined sample of English- and Spanish-speaking participants. The latter analyses indicated that results do not appear to vary as a function of language of participation.
Categories are not mutually exclusive.
The full series of models was also run with these parameters included, and the pattern of findings was unchanged.
Contributor Information
Grant N. Marshall, RAND Corporation; Santa Monica, CA
Jeremy N. V. Miles, RAND Corporation; Santa Monica, CA
Sherry H. Stewart, Dalhousie University, Halifax, Canada; and RAND Corporation; Santa Monica, CA
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, D. C: Author; 2000. [Google Scholar]
- Andrykowski MA, Cordova MJ, Studts JL, Miller TW. Posttraumatic stress disorder after treatment for breast cancer: Prevalence of diagnosis and use of the PTSD Checklist-Civilian Version (PCL-C) as a screening instrument. Journal of Consulting and Clinical Psychology. 1998;66:586–590. doi: 10.1037//0022-006x.66.3.586. [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, Stapleton JA. Associations between dimensions of anxiety sensitivity and PTSD symptom clusters in active-duty police officers. Cognitive Behaviour Therapy. 2008;37:66–75. doi: 10.1080/16506070801969005. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Rites, wrongs, and gold in model testing. Structural Equation Modeling. 2000;7:82–91. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM. EQS Structural Equations Program Manual. Encino, CA: Multivariate Software; 1995. [Google Scholar]
- Bentler PM, Mooijart A. Choice of structural model via parsimony: A rational based on precision. Psychological Bulletin. 1989;106:315–317. doi: 10.1037/0033-2909.106.2.315. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Broman-Fulks JJ, Storey KM. Evaluation of a brief aerobic exercise intervention for high anxiety sensitivity. Anxiety, Stress and Coping. 2008;21:117–128. doi: 10.1080/10615800701762675. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Bryant RA, Panasetis P. Panic symptoms during trauma and acute stress disorder. Behaviour Research and Therapy. 2001;39:961–966. doi: 10.1016/s0005-7967(00)00086-3. [DOI] [PubMed] [Google Scholar]
- Cole DA, Ciesla JA, Steiger JH. The insidious effects of failing to include-design driven correlated residuals in latent variable covariance structure analysis. Psychological Methods. 2007;12:381–398. doi: 10.1037/1082-989X.12.4.381. [DOI] [PubMed] [Google Scholar]
- Collimore KC, McCabe RE, Carleton RN, Asmundson GJ. Media exposure and dimensions of anxiety sensitivity: Differential associations with PTSD symptom clusters. Anxiety Disorders. 2008;22:1021–1028. doi: 10.1016/j.janxdis.2007.11.002. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Borger SC, Taylor S, Fuentes K, Ross LM. Anxiety sensitivity and the five-factor model of personality. Behaviour Research and Therapy. 1999;37:633–641. doi: 10.1016/s0005-7967(98)00174-0. [DOI] [PubMed] [Google Scholar]
- Cox BJ, MacPherson PS, Enns MW, McWilliams LA. Neuroticism and self-criticism associated with posttraumatic stress disorder in a nationally representative sample. Behaviour Research and Therapy. 2004;42:105–114. doi: 10.1016/s0005-7967(03)00105-0. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- Denson TF, Marshall GN, Schell TL, Jaycox LH. Predictors of posttraumatic distress one year after exposure to community violence: The importance of acute symptom severity. Journal of Consulting and Clinical Psychology. 2007;75:683–692. doi: 10.1037/0022-006X.75.5.683. [DOI] [PubMed] [Google Scholar]
- Fedoroff IC, Taylor S, Asmundson GJG, Koch WJ. Cognitive factors in traumatic stress reactions: Predicting PTSD symptoms from anxiety sensitivity and beliefs about harmful events. Behavioral and Cognitive Psychotherapy. 2000;28:5–15. [Google Scholar]
- Feldner MT, Zvolensky MJ, Schmidt NB, Smith RC. A prospective test of anxiety sensitivity as a moderator of the relation between gender and posttraumatic symptom maintenance among high anxiety sensitive young adults. Depression and Anxiety. 2008;25:190–199. doi: 10.1002/da.20281. [DOI] [PubMed] [Google Scholar]
- Finkel S. Causal analysis with panel data. London: Sage; 1995. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jöreskog KG. Testing structural equation models. In: Bollen KA, Long JS, editors. Testing structural equation models. Thousand Oaks, CA: Sage; 1993. pp. 294–316. [Google Scholar]
- Kenny DA. Correlation and causality. New York: Wiley; 1979. [Google Scholar]
- Lang AJ, Kennedy CM, Stein MB. Anxiety sensitivity and PTSD among female victims of intimate partner violence. Depression and Anxiety. 2002;16:77–83. doi: 10.1002/da.10062. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Marsh HW, Hau KT, Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers of overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling. 2004;11:320–341. [Google Scholar]
- McLachlan GJ, Krishnan T. The EM algorithm and extensions. New York: Wiley-Interscience; 1996. [Google Scholar]
- Mulaik SA, Millsap RE. Doing the four-step right. Structural Equation Modeling. 2000;7:36–73. [Google Scholar]
- Muthén B, Muthén L. Mplus 4.2. Los Angeles: Muthén and Muthén; 2008. [Google Scholar]
- Peterson RA, Reiss S. Anxiety Sensitivity Index Manual. Palos Heights, IL: International Diagnostic Systems; 1992. [Google Scholar]
- Rector NA, Szacun-Shimizu K, Leybman M. Anxiety sensitivity within the anxiety disorders: Disorder-specific sensitivities and depression comorbidity. Behaviour Research and Therapy. 2007;45:1967–1975. doi: 10.1016/j.brat.2006.09.017. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. San Diego: Academic Press; 1985. pp. 107–121. [Google Scholar]
- Rosen JB, Schulkin J. From normal fear to pathological anxiety. Psychological Review. 1998;105:325–350. doi: 10.1037/0033-295x.105.2.325. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler P. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/s11336-009-9135-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satorra A, Bentler P. Ensuring positiveness of the scaled difference chi-square test statistic. 2008 doi: 10.1007/s11336-009-9135-y. UCLA Statistics Preprints 548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Mitchell MA, Richey JA. Anxiety sensitivity as an incremental predictor of later anxiety symptoms and syndromes. Comprehensive Psychiatry. 2008;49:407–412. doi: 10.1016/j.comppsych.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Simms LJ, Watson D, Doebbeling BN. Confirmatory factor analyses of posttraumatic stress symptoms in deployed and nondeployed veterans of the Gulf War. Journal of Abnormal Psychology. 2002;111:637–647. doi: 10.1037//0021-843x.111.4.637. [DOI] [PubMed] [Google Scholar]
- Simpson T, Jakupcak M, Luterek JA. Fear and avoidance of internal experiences among patients with substance use disorders and PTSD: The centrality of anxiety sensitivity. Journal of Traumatic Stress. 2006;19:481–491. doi: 10.1002/jts.20128. [DOI] [PubMed] [Google Scholar]
- Smits JA, Berry AC, Rosenfield D, Powers MB, Behar E, Otto MW. Reducing anxiety sensitivity with exercise. Depression & Anxiety. 2008;25:689–699. doi: 10.1002/da.20411. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Conrod PJ, Samoluk SB, Pihl RO, Dongier M. Posttraumatic stress disorder symptoms and situation-specific drinking in women substance abusers. Alcoholism Treatment Quarterly. 2000;18:31–47. [Google Scholar]
- Stewart SH, Taylor S, Baker JM. Gender differences in dimensions of anxiety sensitivity. Journal of Anxiety Disorders. 1997;11:179–200. doi: 10.1016/s0887-6185(97)00005-4. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Watt MC. Introduction to the special issue on interoceptive exposure in the treatment of anxiety and related disorders: Novel applications and mechanisms of action. Journal of Cognitive Psychotherapy. 2008;22:291–302. [Google Scholar]
- Taylor S. Anxiety sensitivity and its implications for understanding and treating PTSD. Journal of Cognitive Psychotherapy. 2003;17:179–186. [Google Scholar]
- Taylor S. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Vujanovic AA, Zvolensky MJ, Bernstein A. Incremental associations between facets of anxiety sensitivity and posttraumatic stress and panic symptoms among trauma-exposed adults. Cognitive Behaviour Therapy. 2008;37:76–89. doi: 10.1080/16506070801969039. [DOI] [PubMed] [Google Scholar]
- Vyrostek SB, Annest JL, Ryan GW. Surveillance for fatal and nonfatal injuries—United States, 2001. Morbidity and Mortality Weekly Report. 2004;53:1–57. [PubMed] [Google Scholar]
- Wald J, Taylor S. Efficacy of interoceptive exposure therapy combined with trauma-related exposure therapy for posttraumatic stress disorder: A pilot study. Journal of Anxiety Disorders. 2007;21:1050–1060. doi: 10.1016/j.janxdis.2006.10.010. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska J, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Ninth annual meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Accessed July 1, 2009]. http://www.pdhealth.mil/library/downloads/PCL_sychometrics.doc. [Google Scholar]
- Yuan KH, Bentler PM. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. In: Sobel ME, Becker MP, editors. Sociological Methodology. Vol. 30. 2000. pp. 165–200. [Google Scholar]
- Zatzick DF, Rivara FP, Nathens AB, Jurkovich GJ, Wang J, Fan M, et al. A nationwide US study of post-traumatic stress after hospitalization for physical injury. Psychological Medicine. 2007;37:1469–1480. doi: 10.1017/S0033291707000943. [DOI] [PubMed] [Google Scholar]
- Zinbarg R, Mohlman J, Hong N. Dimensions of anxiety sensitivity. In: Taylor S, editor. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Hillsdale, NJ: Erlbaum; 1999. pp. 83–114. [Google Scholar]