Abstract
Objective
To evaluate the association between migraine, episodic vertigo, and Ménière’s disease in families.
Study Design
Clinical report.
Setting
University Neurotology Clinic.
Patients
Index patients identified with Ménière’s disease and migraine and their family members.
Intervention
Structured interview to assess a diagnosis of migraine, episodic vertigo, and Ménière’s disease in 6 families. Genotyping was performed on 3 sets of twins to analyze monozygosity or dizygosity.
Main Outcome Measures
Clinical history of migraine, episodic vertigo, and Ménière’s disease.
Results
Six index patients and 57 family members were interviewed either by a senior neurologist in person over the phone by a trained study coordinator. An additional 6 family members completed questionnaires by mail. All 6 index patients had Ménière’s disease and migraine. Twenty-six (41%) of the 63 relatives met International Classification of Headache Disorders II criteria for migraine headaches. Thirteen (50%) of these 26 experienced migraine with aura. Three others experienced typical aura without headache. Seventeen (27%) of 63 family members experienced recurrent spells of spontaneous episodic vertigo. There was one twin pair in each of 3 families; 2 pairs were monozygotic and one was dizygotic. In each twin pair, one twin had migraine and Ménière’s disease, whereas the other experienced migraine and episodic vertigo without auditory symptoms.
Conclusion
The frequent association of episodic vertigo, migraine, and Ménière’s disease in closely related individuals, including identical twins supports the heritability of a migraine-Ménière’s syndrome, with variable expression of the individual features of hearing loss, episodic vertigo, and migraine headaches.
Keywords: Episodic vertigo, Ménière’s disease, Migraine
Epidemiological and family studies support an association between migraine, episodic vertigo, and Ménière’s disease, but reports on detailed pedigrees are limited (1–9). Several childhood periodic symptoms not temporally associated with headache such as cyclical vomiting, abdominal migraines, and benign paroxysmal vertigo of childhood are recognized as precursors to the development of migraine headaches (10). This indicates that the susceptibility to migraine may manifest as these “migraine equivalents” during different periods of a person’s life. Episodic vertigo, for example, has been shown to occur as commonly as visual auras in migraine patients, often without associated headache (11–13). Aural symptoms and even fluctuating hearing loss has been noted in migraine patients raising the possibility that Ménière’s disease, in some patients, might be directly related to their susceptibility to migraine. If Ménière’s disease could develop as part of a spectrum of migraine-associated symptoms (perhaps as a “complication”), then one would expect to see combinations of migraine, Ménière’s disease, and Ménière’s-like symptoms run within families because there has been growing evidence that migraine has a strong genetic basis.
To show the association between migraine, episodic vertigo, and Ménière’s disease, we report 6 families in which these syndromes were highly associated, indicating that there may be a pathophysiological link between them.
MATERIALS AND METHODS
Index patients were initially identified from our clinical data-base as being diagnosed with Ménière’s disease and migraine. The families described here are a subset of 18 pedigrees in which the probands had met the International Classification of Headache Disorders (ICHD) II criteria for migraine, 1995 American Academy of Otolaryngology–Head and Neck Surgery criteria for definite Ménière’s disease, and had all required clinical and diagnostic evaluations. These original 18 families were reported previously (14). We selected the 6 probands in this study based on their family history of episodic vertigo and because all first-degree relatives and most of the available extended relatives had indicated a willingness to be interviewed. Family members were interviewed using a standardized questionnaire over the phone by a trained study coordinator. If phone interviews could not be arranged, the prospective subject was sent a questionnaire. Diagnosis of migraine and its subtypes were based on ICHD II criteria (10). Vertigo was not considered an aura symptom for the purposes of this study. Episodic vertigo was defined as at least two attacks of spontaneous sensation of rotation lasting longer than 1 minute not exclusively triggered by head movement changes.
Genotyping was performed using 11 polymorphic microsatellite markers on the 3 twin sets from Families 8, 218, and 556 to analyze whether they were monozygotic or dizygotic. Our institutional review board approved the questionnaire and the protocol for obtaining blood samples.
RESULTS
All probands presented with the fluctuating low-frequency hearing loss and episodic vertigo of definite Ménière’s disease according to 1995 American Academy of Otolaryngology–Head and Neck Surgery criteria (15), and all eventually developed fixed unilateral hearing loss. Four of the probands had migraine with aura; 2 had migraine without aura. These patients were evaluated by an experienced neurologist (R.W.B.) and had normal neurological examinations, with the exception of essential tremor in 2 patients.
Of the 27 potential first-degree relatives, 23 were interviewed by telephone, and three completed questionnaires by mail. Only one surviving first-degree relative could not be contacted by the investigators for clinical information. There were an additional 4 first-degree relatives who were deceased at the time of the study. In addition, 12 second-degree and 22 third-degree relatives completed phone interviews. Three additional third-degree relatives completed questionnaires.
Among the 63 relatives, 13 met the criteria for migraine with aura, 13 for migraine without aura, three for typical aura without headache, and none for basilar migraine or hemiplegic migraine. Seventeen experienced spontaneous episodes of rotational vertigo. The twins in Families 8 and 556 were monozygotic; the twins in Family 218, dizygotic.
Case Material
Family 1
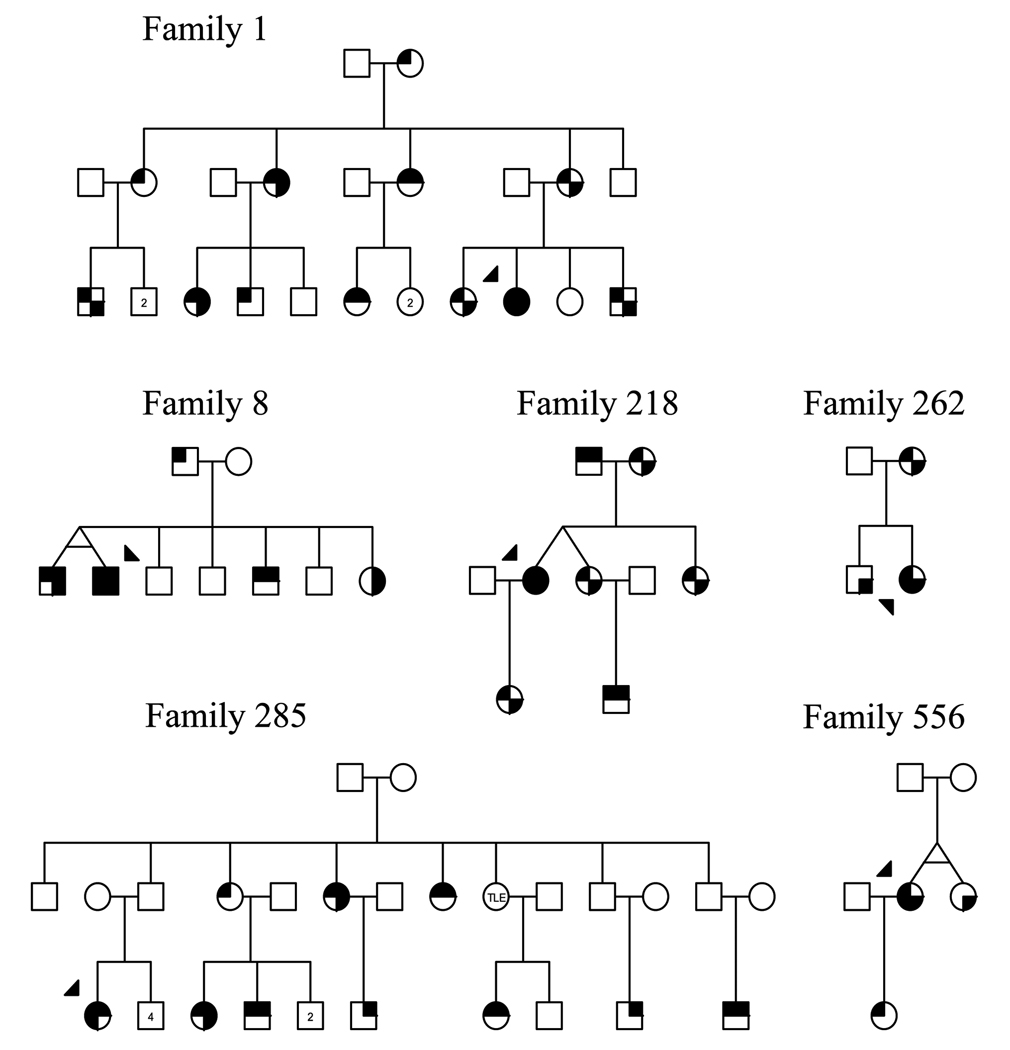
A 51-year-old woman with a history of essential tremor and migraine with aura presented in 1993 with episodic vertigo, left ear fullness, tinnitus, and hearing loss. This eventually led to a fixed left-sided hearing loss. The vertigo spells lasted seconds to hours. In addition, she had essential tremor. All of her symptoms dramatically improved with acetazolamide. Her brother experienced migraine without aura, episodic vertigo, roaring tinnitus, and fullness. His vertigo spells lasted approximately 10 minutes. Either ear could be affected. He had an abnormal electrocochleography study but a normal audiogram. He had a similar history of essential tremor that improved with acetazolamide. Multiple family members including a sister, mother, maternal aunts, and cousins experienced migraine (with or without aura) and episodic vertigo. There were no other family members who had aural symptoms or hearing loss associated with their vertigo spells (Fig. 1). This family was previously reported by Baloh et al. (16) in 1996.
FIG. 1.
Diagram showing pedigrees of families with migraine, episodic vertigo, and Ménière’s disease. Female family members are represented by circles; male family members by squares. Index patients are indicated with an arrowhead. Affected status is indicated by shading in of quadrants according to the following scheme: upper left, migraine; upper right, aura (visual or somatosensory); lower left, hearing loss; lower right, episodic vertigo. Numbers within the circles or squares indicate the number of unaffected individuals in the sibship. TLE indicates temporal lobe epilepsy.
Family 8
A 33-year-old man with migraine with aura presented in 1993 with a 4-year history of severe left-sided headaches accompanied by left eye visual loss, redness, tearing, left-sided hearing loss, aural fullness, and tinnitus. The spells lasted several hours and were only relieved by sleep. He developed a progressive low-frequency hearing loss in the left ear in between the attacks. His identical twin brother had migraine without aura and episodic vertigo attacks associated with left ear fullness but no hearing loss. Both brothers and a third brother had early-onset essential tremor. A sister had episodic vertigo and typical visual auras without headache.
Family 218
A 45-year-old woman with a history of migraine with aura presented in 2003 with a 2-year history of episodic vertigo, fluctuating right-sided hearing loss, and tinnitus. The spells lasted minutes. She underwent a right vestibular nerve section, but several years later, she began experiencing longer periods of fluctuating hearing loss in the left ear. Her fraternal twin sister developed episodic vertigo associated with migraine headaches without aura at age 25 years. She did not have aural symptoms or hearing loss. The patient’s second sister developed episodes of vertigo along with migraine headaches without aura at age 10 years. She experienced low-pitched tinnitus and fullness during the attacks but no hearing loss. The index patient’s daughter developed episodic vertigo at age 15 years and then migraine headaches without aura at age 25 years.
Family 262
A 29-year-old woman with a history of migraine headaches without aura presented in 2003 with an almost 1-year history of fluctuating left-sided hearing loss, tinnitus, and fullness. She developed episodic vertigo 6 weeks before presentation. The vertigo spells typically lasted approximately 8 hours. Audiograms documented a fluctuating low-frequency hearing loss in the left ear, which eventually became a fixed hearing loss. Family history was significant for migraine headaches without aura, episodic vertigo, and panic attacks in her mother. The index patient’s brother developed episodes of vertigo at age 18 years but did not have migraine headaches. Neither the patient’s mother nor brother had aural symptoms or hearing loss.
Family 285
A 42-year-old woman presented in 2000 with a 1-year history of episodic vertigo accompanied by fluctuating right-sided hearing loss, low-pitched tinnitus, and headaches. The spells lasted from 10 minutes to 2 hours. She developed migraine headaches with visual and hemisensory auras with the onset of her vertigo spells. Her headaches typically accompanied the vertigo. An audiogram documented a fixed, right-sided, low-frequency sensor-ineural hearing loss. Family history was significant for several paternal aunts and cousins with migraine, either with or without aura. One of the aunts also experienced episodic vertigo without hearing changes. A paternal cousin also had migraine with aura and episodic vertigo with left-sided tinnitus but without hearing changes.
Family 556
A 61-year-old woman with a history of migraine without aura presented in 2005 with a 15-year history of episodic vertigo, left ear fullness, and hearing loss. The attacks would last 1 to 3 days and culminated in a fixed left-sided hearing loss. Her identical twin sister developed episodic vertigo spells in her 50s, which were not associated with any hearing changes or aural symptoms. She had a history of prostrating headaches that started in her 20s, but these did not meet the ICHD II criteria for migraine.
DISCUSSION
Familial aggregation and twin studies support a genetic basis for migraine (17–20), and episodic vertigo shows a similar pattern of heritability (21,22). However, could the same disease process cause inner ear damage predisposing to Ménière’s disease? Three observations in our families support the theory that episodic vertigo with hearing loss and episodic vertigo without hearing loss are different manifestations of the same underlying susceptibility.
First, vertigo and fluctuating hearing loss were associated with visual and hemisensory auras in 2 probands (Families 8 and 285). In these cases, a typical Ménière’s syndrome developed within the context of a migraine headache with aura.
Second, the discordance for hearing loss in the identical twins in Families 8 and 556 shows that the same genetic background can lead to different, although very similar, syndromes. In only one of the twins did the syndrome culminate in hearing loss, indicating that environmental and epigenetic factors are important in disease expression.
Third, the index patient in Family 218 developed Ménière’s disease in both ears, whereas the generation above and below her only developed episodic vertigo and migraine. If the transmission of this disorder is genetic, the expression of a partial syndrome seems to be very high, whereas the full Ménière’s phenotype is uncommon.
Episodic vertigo ran in each of the families at a rate much higher than the 1-year population prevalence of vestibular vertigo, which has been estimated to be approximately 4.9% in a recent review by Neuhauser (23). The total prevalence of migraine in these families (48%) for all migraine types in this series was much higher than population estimates of 17.1% for women and 5.6% for men (24). Moreover, the rate of migraine with aura among those with migraine (17 of 32 or 53%) was more than double the rates observed in nonselected migraine patients (12). This implies that processes that predispose to aura may also be important in susceptibility to vertigo.
Migraine may contribute to permanent damage of the ear. Caloric paresis in migraine patients with or without vestibular symptoms occurs at a rate between 15 to 35% (25–27). Vasospasm as a mechanism of migraine-associated sudden sensorineural hearing loss has been proposed based on its association with other features such as visual auras, amaurosis fugax, hemiplegia, and angina (28). A case study showed that migraine can lead to an isolated infarction of the inner ear probably through vasospasm of the small arteries (29). The mechanism of the association of benign paroxysmal vertigo (30,31) and otolithic crises (32) with migraine has also been proposed to be secondary to vasospasm. This proposed vasospastic microvascular ischemic damage to the inner ear could create a susceptibility of developing Ménière’s disease.
A limitation to our study is that subclinical hearing loss was not documented with an audiogram in the family members, although all reported to have normal hearing. It is therefore possible that some of the family members with episodic vertigo may have had primary inner ear disease. The impact is likely to be small, however, given the high prevalence of related symptoms in our participants and relative rarity of vertigo syndromes from primary inner ear etiologies.
There is support for a genetic basis for familial Ménière’s disease, including linkage to Chromosome 12p (33) and an association with certain Class I human leukocyte antigens (34), but our families were too small to determine a similar association. Unlike in these previous reports, hearing loss was the least common symptom in our families, making it less likely that the syndromes are related. Oliveira et al. (35) presented a case series in which 6 of 8 probands with Ménière’s disease had a family history of either Ménière’s disease or episodic vertigo. Many of the patients with Ménière’s disease in his series however had atypical hearing loss, such as early bilateral involvement, high-frequency hearing loss, or even normal hearing. The high prevalence of migraine headaches in his series raises the possibility of whether the episodic vertigo in his patients was part of a spectrum of migraine symptoms, similar to ours.
The search for a single gene conferring susceptibility to the most common forms of migraine headaches has been elusive, and episodic vertigo with or without hearing loss is much less common than migraine headaches. If there is a genetic basis for the association between migraine, episodic vertigo, and Ménière’s syndrome, it is likely to be heterogeneous, polygenic, or to confer susceptibility rather than be deterministic.
Acknowledgments
This study was supported by National Institutes of Health Grant P50 DC 05224 from the National Institute on Deafness and Other Communication Disorders, National Institutes of Health Grant 5 U54 RR019482, and the Clinical Research Training Fellowship from the American Academy of Neurology.
Footnotes
The authors report no conflicts of interest.
REFERENCES
- 1.Rassekh C, Harker L. The prevalence of migraine in Ménière’s disease. Laryngoscope. 1992;102:135–138. doi: 10.1288/00005537-199202000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Parker W. Ménière’s disease: etiologic considerations. Arch Otolaryngol Head Neck Surg. 1995;121:377–382. doi: 10.1001/archotol.1995.01890040005001. [DOI] [PubMed] [Google Scholar]
- 3.Hinchcliffe R. Personal and family medical history in Ménière’s disease. J Laryngol Otol. 1967;81:661–668. doi: 10.1017/s0022215100067591. [DOI] [PubMed] [Google Scholar]
- 4.Hinchcliffe R. Headache and Ménière’s disease. Acta Otolaryngol. 1967;63:384–390. doi: 10.3109/00016486709128772. [DOI] [PubMed] [Google Scholar]
- 5.Atkinson M. Migraine and Ménière’s disease. Arch Otolaryngol. 1962;75:46–51. doi: 10.1001/archotol.1962.00740040228008. [DOI] [PubMed] [Google Scholar]
- 6.Radtke A, Lempert T, Gresty MA, Brookes GB, Bronstein AM, Neuhauser H. Migraine and Ménière’s disease: is there a link? Neurology. 2002;59:1700–1704. doi: 10.1212/01.wnl.0000036903.22461.39. [DOI] [PubMed] [Google Scholar]
- 7.Oliveira C, Bazerra RL, Araujo MF, Almeida VF, Messias CI. Ménière’s syndrome and migraine: incidence in one family. Ann Otol Rhinol Laryngol. 1997;106:823–829. doi: 10.1177/000348949710601004. [DOI] [PubMed] [Google Scholar]
- 8.Brown M. Ménière’s syndrome. Arch Neurol Psychiatry. 1941;46:561. [Google Scholar]
- 9.Bernstein J. Occurrence of episodic vertigo and hearing loss in families. Ann Otol Rhinol Laryngol. 1965;74:1011–1021. doi: 10.1177/000348946507400408. [DOI] [PubMed] [Google Scholar]
- 10.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders. Cephalalgia. (2nd edition) 2004;24:1–160. [Google Scholar]
- 11.Kayan A, Hood JD. Neuro-otological manifestations of migraine. Brain. 1984;107:1123–1142. doi: 10.1093/brain/107.4.1123. [DOI] [PubMed] [Google Scholar]
- 12.Stewart W, Linet MS, Celentano DD, Van Natta M, Ziegler D. Age and sex specific incidence rates of migraine with and without visual aura. Am J Epidemiol. 1991;134:1111–1120. doi: 10.1093/oxfordjournals.aje.a116014. [DOI] [PubMed] [Google Scholar]
- 13.Neuhauser H, Leopold M, von Brevern M, Arnold G, Lempert T. The interrelations of migraine, vertigo, and migrainous vertigo. Neurology. 2001;56:436–441. doi: 10.1212/wnl.56.4.436. [DOI] [PubMed] [Google Scholar]
- 14.Cha YH, Brodsky J, Ishiyama J, Sabatti C, Baloh RW. Clinical relevance of migraine in Ménière’s disease. Acta Otolaryngol. 2007 May 8; doi: 10.1080/00016480701242469. Epub. [DOI] [PubMed] [Google Scholar]
- 15.Committee on Hearing and Equilibrium. Guidelines for the diagnosis and evaluation of therapy in Ménière’s disease. Otolaryngol Head Neck Surg. 1995;113:181–185. doi: 10.1016/S0194-5998(95)70102-8. [DOI] [PubMed] [Google Scholar]
- 16.Baloh RW, Foster CA, Yue Q, Nelson SF. Familial migraine with vertigo and essential tremor. Neurology. 1996;46:458–460. doi: 10.1212/wnl.46.2.458. [DOI] [PubMed] [Google Scholar]
- 17.Ulrich V, Gervil M, Kyvik KO, Olesen J, Russell MB. Evidence of a genetic factor in migraine with aura: a population-based Danish twin study. Ann Neurol. 1999;45:242–246. doi: 10.1002/1531-8249(199902)45:2<242::aid-ana15>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 18.Gervil M, Ulrich V, Kyvik KO, Olesen J, Russell MB. Migraine without aura: a population-based twin study. Ann Neurol. 1999;46:606–611. doi: 10.1002/1531-8249(199910)46:4<606::aid-ana8>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 19.Russell M, Olesen J. Increased familial risk and evidence of genetic factor in migraine. BMJ. 1995;311:541–544. doi: 10.1136/bmj.311.7004.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Russell M, Iselius L, Olesen J. Migraine without aura and migraine with aura are inherited disorders. Cephalalgia. 1996;16:305–309. doi: 10.1046/j.1468-2982.1996.1605305.x. [DOI] [PubMed] [Google Scholar]
- 21.Oh A, Lee H, Jen JC, Corona S, Jacobson KM, Baloh RW. Familial benign episodic vertigo. Am J Med Genet. 2001;100:287–291. doi: 10.1002/ajmg.1294. [DOI] [PubMed] [Google Scholar]
- 22.Lee H, Jen JC, Wang H, et al. A genome-wide linkage scan of familial benign episodic vertigo: linkage to 22q12 with evidence of heterogeneity. Hum Mol Genet. 2006;15:251–258. doi: 10.1093/hmg/ddi441. [DOI] [PubMed] [Google Scholar]
- 23.Neuhauser HK. Epidemiology of vertigo. Curr Opin Neurol. 2007;20:40–46. doi: 10.1097/WCO.0b013e328013f432. [DOI] [PubMed] [Google Scholar]
- 24.Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology. 2007;68:343–349. doi: 10.1212/01.wnl.0000252808.97649.21. [DOI] [PubMed] [Google Scholar]
- 25.Cutrer F, Baloh RW. Migraine-associated dizziness. Headache. 1992;32:300–304. doi: 10.1111/j.1526-4610.1992.hed3206300.x. [DOI] [PubMed] [Google Scholar]
- 26.Kuritzky A, Toglia UJ, Thomas DO. Vestibular function in migraine. Headache. 1981;21:110–112. doi: 10.1111/j.1526-4610.1981.hed2103110.x. [DOI] [PubMed] [Google Scholar]
- 27.Bir L, Ardic FN, Kara CO, Akalin O, Pinar HS, Celiker A. Migraine patients with or without vertigo: comparison of clinical and electronystagmographic findings. J Otolaryngol. 2003;32:234–238. doi: 10.2310/7070.2003.41718. [DOI] [PubMed] [Google Scholar]
- 28.Viirre E, Baloh RW. Migraine as a cause of sudden hearing loss. Headache. 1996;36:24–28. doi: 10.1046/j.1526-4610.1996.3601024.x. [DOI] [PubMed] [Google Scholar]
- 29.Lee H, Lopez I, Ishiyama A, Baloh RW. Can migraine damage the inner ear? Arch Neurol. 2000;57:1631–1634. doi: 10.1001/archneur.57.11.1631. [DOI] [PubMed] [Google Scholar]
- 30.Ishiyama A, Jacobson KM, Baloh RW. Migraine and benign paroxysmal vertigo. Ann Otol Rhinol Laryngol. 2000;109:377–380. doi: 10.1177/000348940010900407. [DOI] [PubMed] [Google Scholar]
- 31.Uneri A. Migraine and benign paroxysmal positional vertigo: an outcome study of 476 patients. Ear Nose Throat J. 2004;83:814–815. [PubMed] [Google Scholar]
- 32.Ishiyama G, Ishiyama A, Baloh RW. Drop attacks and vertigo secondary to a non- Ménière’s otologic cause. Arch Neurol. 2003;60:71–75. doi: 10.1001/archneur.60.1.71. [DOI] [PubMed] [Google Scholar]
- 33.Klar J, Frykholm C, Friberg U, Dahl N. A Ménière’s disease gene linked to Chromosome 12p12.3. Am J Med Genet. 2006;141B:463–467. doi: 10.1002/ajmg.b.30347. [DOI] [PubMed] [Google Scholar]
- 34.Xenellis J, Morrison AW, McClowsky D, Festenstein H. HLA antigens in the pathogenesis of Ménière’s disease. J Laryngol Otol. 1986;100:21–24. doi: 10.1017/s0022215100098698. [DOI] [PubMed] [Google Scholar]
- 35.Oliveira C, Messias CI, Ferrari I. Occurrence of familial Ménière’s syndrome and migraine in Brasilia. Ann Otol Rhinol Laryngol. 2002;111:229–236. doi: 10.1177/000348940211100307. [DOI] [PubMed] [Google Scholar]