Abstract
We present a case of severe metallosis after total elbow arthroplasty in a female patient presenting with manifestations resembling a septic loosening. We discuss the clinical and the operative findings as well as the outcome of this uncommon complication. A review of the literature regarding the pathogenesis, radiographic appearance, and management of metallosis in prosthetic joints is presented.
Keywords: Metallosis, Total elbow arthroplasty, Loosening
Introduction
Metallosis in prosthetic joints with severe wear of the poly inlay is well known by orthopedic surgeons. However, the occurrence of this complication is very uncommon in non-weight-bearing joints such as the elbow or the shoulder. The management of metallosis may be challenging due to the variety of the presenting symptoms and the perioperative findings. We describe a case of severe metallosis in the setting of a total elbow arthroplasty (TEA) presenting with manifestations resembling a septic loosening. We discuss the clinical picture of this uncommon complication, the perioperative findings, and management as well as the outcome. A review of the literature regarding the pathogenesis, radiographic appearance, and management of metallosis in prosthetic joints is presented.
Case Report
In year 2000, a 64-year-old female patient was operated on with unlinked Kudo type 3 with metal-backed ulnar component (Biomet UK Ltd.) TEA for primary osteoarthritis of the left elbow. No perioperative complications were reported and the patient was satisfied with the results 1 year after the operation. At that time, a follow-up X-ray showed acceptable positioning of the prosthesis components with no radiolucencies (Fig. 1).
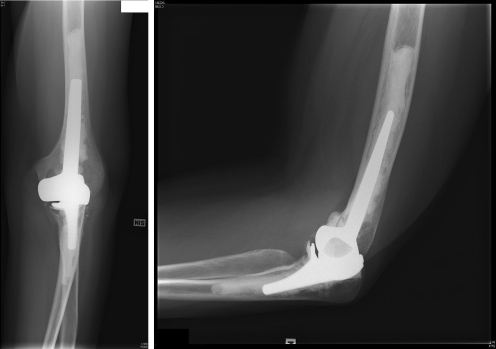
Fig. 1.
Radiographs taken at 1-year follow-up (year 2001) showing a Kudo TEA in an acceptable positioning without radiolucencies.
In January 2006, the patient presented with a history of increasing pain in her operated elbow. The clinical examination revealed mild to moderate swelling, mild warmth, and redness and tenderness of the elbow. The range of motion was 10º to 100º (slightly decreased compared to previous examinations). The X-ray showed mild valgus tilting of the ulnar component, thin radiolucent line around the humeral component, and breakage of the cement mantle (Fig. 2). The laboratory investigations showed leukocyte count = 9,800 cell per cubic millimeter, C-reactive protein = 72 mg/L, and erythrocyte sedimentation rate = 44 mm/h.
Fig. 2.
Radiographs taken when the patient presented with increasing pain in her operated elbow (year 2006). They showed PE wear valgus tilting of the ulnar component radiolucency around the humeral component and fracture of the cement mantle.
Septic loosening was the primary suspicion. However, two-time aspiration of the elbow for culture and sensitivity revealed no bacterial growth.
The patient was scheduled for revision of her TEA.
In April 2006, the patient was operated on in the lateral decubitus position with the use of a tourniquet. The TEA was approached through a posterior triceps split. Once opened, the elbow showed severe metallic debris of the soft tissues and synovium which was filled with black synovial fluid (Fig. 3). After a thorough irrigation of the whole joint, the components of the prosthesis including the surrounding cement were removed. There was an extensive wear of the polyethylene (PE) part of the ulnar component. The removal of the loose components caused a small defect of the humerus. Five deep soft tissue biopsies for bacterial culture and sensitivity testing were taken. A Discovery elbow system (Biomet Orthopedics, Warsaw, IN, USA) was then inserted using a gentamicin-added cement with no pressurization (Fig. 4).
Fig. 3.
Severe metallosis invading the TEA components and the surrounding soft tissues.
Fig. 4.
Radiographs of the revision surgery using the Discovery elbow system. Asymptomatic cement leak from a bony defect in the humerus.
The taken biopsies revealed no bacterial growth. Postoperatively, the patient improved successively, and, 18 months after the operation, the patient had no pain in her elbow; the range of motion was from 0º to 120º and the X-ray showed satisfactory positioning of the TEA components.
Our patient was informed that data concerning her case would be submitted for publication.
Discussion
Metallosis is defined as infiltration of metallic wear debris in periprosthetic soft and bony tissues [5]. It usually happens as a result of metal–metal contact in patients with metal-on-metal arthroplasty or in patients with PE wear or fracture with subsequent abrasion of the underlying metal surfaces [2]. Typically, metallosis occurs after some years of the arthroplasty operation [11]. In our patient, metallosis gave complaints 6 years after the primary TEA operation and radiographs showed signs of PE wear.
As discussed by Bullough [3], when the metallic wear particles are released, they give rise to at least three types of effect. First, these particles can be fragmented into smaller-sized components with overall larger surface area leading to increased toxicity at the particle–host tissue interface. Second, particles with suitable size can be directly phagocytosed (mainly by histiocytes) leading to local inflammatory reaction with giant cell infiltration. This may activate an osteoclast-mediated bone resorption and osteolysis. Metallosis was found be associated with periprosthetic osteolysis in 77.4% of cases [5]. Third, some of the phagocytosed (and maybe free) particles migrate to local lymph nodes, spleen, liver, and lungs. While the effect of this phenomenon on remote organs is still controversial, local necrosis and fibrosis can be encountered [4].
Metallosis has been reported in the setting of hip and knee arthroplasties [5,6,13,14,16]. However, the prevalence of metallosis in non-weight-bearing joints is very uncommon [9,12].
The clinical presentation of periprosthetic metallosis is variable and may represent a diagnostic challenge. In many cases, the patient shows loosening manifestations with pain and instability of the affected joint [5]. Others show extra-articular swellings due to granuloma formation [1,16]. Similar to our patient, metallosis can even mimic septic loosening of the prosthesis [10].
Radiographically, metallosis can be seen as a radio-dense line, described as “the bubble sign” by Su et al. [15] and as metal-line sign by Weissman et al. [17]. Moreover, it can resemble heterotopic ossification [11]. A more consistent but less specific radiographic finding in patients with histologically proven metallosis is osteolysis around the prosthetic components [5,7,8]. In our patient, manifestations of PE wear with subsequent titling of the ulnar component, radiolucent zone around the humeral component, and cement mantle fracture were noted.
When considering revision surgery for patients with metallosis, prompt action is necessary to prevent rapid and severe loss of bone stock by the accompanying osteolysis [5]. Complete removal of the metallic debris may not be possible in all cases, and it is seldom necessary [5]. In such cases, priority should be given to appropriate management of osteolysis. In our patient, revision surgery using the Discovery elbow system was associated with pain relief, increasing stability and range of motion and improved function one and half year postoperatively.
In summary, this case report discusses a very uncommon complication of PE wear with subsequent metallosis in non-weight-bearing joint. The presentation was that of septic loosening and the radiographs showed nonspecific changes. Revision surgery resulted in a very good outcome.
References
- 1.Akimoto M, Hara H, Suzuki H. Metallosis of the skin mimicking malignant skin tumour. Br J Dermatol. 2003;149(3):653. doi: 10.1046/j.1365-2133.2003.05387.x. [DOI] [PubMed] [Google Scholar]
- 2.Berry DJ, Barnes CL, Scott RD, Cabanela ME, Poss R. Catastrophic failure of the polyethylene liner of uncemented acetabular components. J Bone Joint Surg Br. 1994;76(4):575–578. [PubMed] [Google Scholar]
- 3.Bullough PG. Metallosis. J Bone Joint Surg Br. 1994;76(5):687–688. [PubMed] [Google Scholar]
- 4.Case CP, Langkamer VG, James C, Palmer MR, Kemp AJ, Heap PF, Solomon L. Widespread dissemination of metal debris from implants. J Bone Joint Surg Br. 1994;76(5):701–712. [PubMed] [Google Scholar]
- 5.Chang JD, Lee SS, Hur M, Seo EM, Chung YK, Lee CJ. Revision total hip arthroplasty in hip joints with metallosis: a single-center experience with 31 cases. J Arthroplasty. 2005;20(5):568–573. doi: 10.1016/j.arth.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 6.Chew FS, Ramsdell MG, Keel SB. Metallosis after total knee replacement. AJR Am J Roentgenol. 1998;170(6):1556. doi: 10.2214/ajr.170.6.9609173. [DOI] [PubMed] [Google Scholar]
- 7.Heffernan EJ, Alkubaidan FO, Nielsen TO, Munk PL. The imaging appearances of metallosis. Skeletal Radiol. 2008;37(1):59–62. doi: 10.1007/s00256-007-0362-y. [DOI] [PubMed] [Google Scholar]
- 8.Hernigou P, Poignard A, Nogier A, Manicom O. Osteolysis in revision total knee arthroplasty: a comparative study of osteolysis with and without metallosis. Rev Chir Orthop Repar Appar Mot. 2005;91(1):51–57. doi: 10.1016/s0035-1040(05)84275-8. [DOI] [PubMed] [Google Scholar]
- 9.Hopkins AR, Hansen UN, Amis AA, Knight L, Taylor M, Levy O, Copeland SA. Wear in the prosthetic shoulder: association with design parameters. J Biomech Eng. 2007;129(2):223–230. doi: 10.1115/1.2486060. [DOI] [PubMed] [Google Scholar]
- 10.Huo MH, Romness DW, Huo SM. Metallosis mimicking infection in a cemented total knee replacement. Orthopedics. 1997;20(5):466–470. doi: 10.3928/0147-7447-19970501-17. [DOI] [PubMed] [Google Scholar]
- 11.Khan RJ, Wimhurst J, Foroughi S, Toms A. The natural history of metallosis from catastrophic failure of a polyethylene liner in a total hip. J Arthroplasty 2008; in press. [DOI] [PubMed]
- 12.Kudo H, Iwano K, Nishino J. Cementless or hybrid total elbow arthroplasty with titanium-alloy implants. A study of interim clinical results and specific complications. J Arthroplasty. 1994;9(3):269–278. doi: 10.1016/0883-5403(94)90081-7. [DOI] [PubMed] [Google Scholar]
- 13.Matsushita I, Morita Y, Gejo R, Kimura T. Severe bone defects and reduced mineralization caused by massive metallosis after total knee arthroplasty: histopathologic and bone morphometric findings. Mod Rheumatol. 2007;17(6):507–510. doi: 10.1007/s10165-007-0618-3. [DOI] [PubMed] [Google Scholar]
- 14.McGovern TF, Moskal JT. Radiographic evaluation of periprosthetic metallosis after total knee arthroplasty. J South Orthop Assoc. 2002;11(1):18–24. [PubMed] [Google Scholar]
- 15.Su EP, Callander PW, Salvati EA. The bubble sign: a new radiographic sign in total hip arthroplasty. J Arthroplasty. 2003;18(1):110–112. doi: 10.1054/arth.2003.50007. [DOI] [PubMed] [Google Scholar]
- 16.Tan GM, Lynne G, Sarbjit S. Osteolysis and wear debris after total knee arthroplasty presenting with extra-articular metallosis in the calf. J Arthroplasty. 2008;23(5):775–780. doi: 10.1016/j.arth.2007.05.031. [DOI] [PubMed] [Google Scholar]
- 17.Weissman BN, Scott RD, Brick GW, Corson JM. Radiographic detection of metal-induced synovitis as a complication of arthroplasty of the knee. J Bone Joint Surg Am. 1991;73(7):1002–1007. [PubMed] [Google Scholar]