Abstract
Since 1976, experimental and clinical studies have suggested the superiority of vascularized nerve grafts. In this study, a 27-year experience of the senior author is presented regarding vascularized nerve grafts and fascia for complex upper extremity nerve reconstruction. The factors influencing outcomes as well as a comparison with conventional nerve grafts is presented. Since 1981, 21 vascularized nerve grafts, other than vascularized ulnar nerve, were used for reconstruction of nerve injuries in the upper extremity. Indications were prolonged denervation time, failure of the previously used conventional nerve grafts, and excessive scar in the recipient site. Injury was in the hand/wrist area (n = 5), in the forearm (n = 4), in the elbow (n = 2), in the arm (n = 4), or in the plexus (n = 6). Vascularized sural (n = 9), saphenous (n = 8), superficial radial (n = 3), and peroneal (superficial and deep) nerves were used. The mean follow-up was 31.4 months. Vascularized nerve grafts for upper extremity injuries provided good to excellent sensory return in severely scarred upper extremities in patients in whom conventional nerve grafts had failed. They have also provided relief of causalgia after painful neuroma resection and motor function recovery in selective cases even for above the elbow injuries. Small diameter vascularized nerve grafts should be considered for bridging long nerve gaps in regions of excessive scar or for reconstructions where conventional nerve grafts have failed.
Keywords: Vascularized nerve grafts, Upper extremity, Reconstruction, Vascularized fascia
Introduction
The first vascularized nerve graft in the upper extremity was a pedicled nerve graft in 1945 by St. Clair Strange for reconstruction of large nerve defect: the ulnar nerve was transferred in two stages to reconstruct the median nerve [21]. Thirty years later, in 1976, Taylor and Ham reported the first free vascularized nerve graft: 24 cm of the superficial radial nerve based on the radial artery was used to reconstruct a median nerve in a case of Volkmann’s ischemic contracture [22]. In 1981, Terzis and Breindenbach carried out an extensive anatomical study on fresh cadavers using injection techniques in which they defined the blood supply of peripheral nerves that could be used for microvascular transfer and introduced a classification of the blood supply of nerves based on the number of dominant vascular pedicles [2, 24]. Sural nerve was reported initially as a vascularized graft by Gilbert and Fachinelli et al. [6, 7], even though the dominant vascular pedicle was absent in a high percentage of cases [2].
Successful transfer of a conventional nerve graft requires a well-vascularized bed. The clinical indication for a vascularized nerve graft is a scarred recipient bed that will not support a nonvascularized nerve graft. In the upper extremity, vascularized nerve grafts from the distal part of deep peroneal nerve were used for severely scarred digits [14, 15, 19, 20] or sural nerve for gaps less than 7 cm [3, 4]. Townsend and Taylor [29] presented five upper extremity cases where composite saphenous vein-sural nerve graft was used to reconstruct median and/or ulnar nerve defects of 6 to 21 cm in length.
Gu et al. [8] presented the same model of sural nerve graft based on arterialized saphenous vein for the repair of median, ulnar, or radial nerves in 14 patients (21- to 54-year-olds). The indications were nerve defects longer than 10 cm, recipient bed cicatrisation, and coexisting major vessel injury.
Taylor [23] presented long-term results of free vascularized superficial radial nerve transfer in three cases (as a single transfer, as a double barrel transfer, or as a composite flap).
Most of the reports for vascularized nerve grafts in upper extremity injuries involve difficult cases in which the authors explain the reason for use of vascularized nerve grafts and subsequent results. In this study, we present a retrospective review of 21 cases of free vascularized nerve grafts for severe upper extremity nerve injuries. Our much larger experience with vascularized ulnar nerve grafts (151 reconstructions) for brachial plexus reconstruction has been published in a separate report [27].
Material and Method
Since 1981, 21 vascularized nerve grafts were used for reconstruction of nerve injuries in the upper extremity. These were nerve grafts that were transferred as vascularized nerve grafts (n = 15), as vascularized nerve grafts with vascularized fascia (n = 3) or as nonvascularized nerves with vascularized fascia (n = 3). Twelve patients had a right, eight had a left injury, and one had both upper extremities injured. These included 16 males and five females from 7 to 52 years old (mean age 27.7). Most of the patients had work-related injuries (power saw, jet engine, high voltage electric injury), motor vehicle accident (n = 6), or gusted injury (n = 3).Two patients had a fall from high altitude and one fell on glass. Injury was in the hand/wrist area (n = 5), forearm (n = 4), elbow (n = 2), arm (n = 4), or plexus (n = 6). Eight patients suffered a median nerve injury, one ulnar, four both median, and ulnar nerves and six had brachial plexus injury. The indications for reconstruction with vascularized nerve grafts were prolonged denervation time, failure of previously used conventional nerve grafts, and inadequate vascularization of the recipient bed. Denervation time ranged from 3 months to 17 years (mean denervation time 36.4 months).
The mean follow-up was 41.5 months.
Two patients were lost to follow-up and were excluded from the study (Table 1).
Table 1.
Vascularized nerve grafts (other than vascularized ulnar) for upper extremity injuries reconstruction.
| Patient no. | Type of injury | Gender | L,R | Level | Nerve | DT (months) Y | Age at Sx | F-UP (months) | No. of previous Sx | Intra-Operative (Gap 0, Neuroma 1) | Reconstruction | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vascular fascia | Vascular graft | No strands | Length (cm) | Sensory | Motor | |||||||||||
| 1 | Gunshot | F | L | ARM | MED | 1 | 52 | 0 | 0 | 0 | NO | Sural | 4 | 4 × 10 | NO FU | NO FU |
| 2 | Fall from high | F | R | WRIST | MED | 15Y | 23 | 3 | 2 | 1 | YES | Sural | 2 | 2 × 11 | NO PAIN Sensibility return to near normal levels | Partial resection without downgrading the motor function |
| HAND | ||||||||||||||||
| 3 | Industrial w/ saw | M | L | ELBOW | MED | 96 | 39 | 96 | 2 | 1 | YES | Sural | 4 | 4 × 12 | NO PAIN 2PD < 3.5 | partial resection without downgrading the motor function |
| 4 | Work acc | M | R | WRIST | MED | 42 | 23 | 58 | 3 | 1 | YES | Sural | 3 | 3 × 4 | 2PD < 10 @ 30 months | |
| 5 | Fall in glass door | M | R | ARM | MED | 23 | 7 | 48 | 1 | 0 | NO | Sural | 2 | 2 × 12 3 × 11 | S2PD 4-6 mm | Muscle grade M4 |
| 6 | Jet engine | M | R | WRIST | ULN | 10 | 41 | 23 | 2 | 0 | NO | Sural | 2 | 2 × 15 | S2PD 12-15mm | Partial resection w/o downgrading motor |
| HAND | ||||||||||||||||
| 7 | High voltage electric | M | L + R | FOREARM | MED | 12 | 23 | 42 | 1 | 0 | NO | Saphenous | 2 | 2 × 14 | From MAC and LAC w/ non vasc | Muscle grade 4- Free LD transferred in the 1st stage to create also vasc bed. |
| 8 | Crush garage door | M | L | FOREARM | MED | 44 | 48 | 21 | 4 | 1 | NO | Saphenous | 5 | 5 × 10 | NO PAIN High frequency vibration | Partial resection w/o downgrading motor |
| 9 | Above elbow amputation | M | R | ARM | MED ULN | 12 | 27 | 0 | 1 | 0 | NO | Saphenous | 1 | 40 | NO FU | NO FU |
| 10 | Boat propeller | M | L | ELBOW | ULN | 17 | 23 | 36 | 0 | 0 | NO | Saphenous | 1 | 1 × 30 1 × 30 | 2PD < 10 | @1 year: intrinsic M2 + @ the end of FU: M4 |
| FOREARM | ||||||||||||||||
| 11 | Boat propeller | M | L | ELBOW | MED | 3 | 23 | 36 | 0 | 0 | NO | Superficial and deep (sensory) peroneal | 2 | 2 × 15 3 × 15 8 × 5.5 | 2PD < 10 | @ 1y FDS M3 + FDP M3- @ the end of FU M4 |
| FOREARM | ||||||||||||||||
| 12 | Fall in a bottle | F | R | WRIST | MED | 17Y | 22 | 12 | 3 | 1 | NO | Superficial radial | 2 | 2 × 12 3 × 12 (sural) | No improvement @ 12 months of FU | Partial resection w/o downgrading motor |
| 13 | Gunshot | M | R | ARM | MED | 3 | 24 | 53 | 0 | 0 | YES | Non vasc | 7 | 6 × 13 1 × 13 | 2PD < 10 | @ 40 months Muscle grade M4 |
| 14 | Gunshot | M | R | ARM | ULN | 3 | 24 | 53 | 0 | 0 | YES | Sural Non vasc | 4 | 4 × 8 | 2PD < 10 | @ 52 months Muscle grade M4 |
| 15 | Crush injury | F | L | WRIST | MED | 6 | 51 | 12 | 1 | 1 | YES | Sural | 1 | 1 × 10 | NO PAIN | Neurolysis no motor downgrading |
ULN ulnar nerve, MED median nerve, F female, M male, R right, L left, 2PD two-point discrimination, F-UP follow-up, Y Years
Furthermore, in the six plexopathy patients, the vascularized nerve grafts were used primarily as vascularized conduits for future free muscle transplantation, and the latter will be considered in a separate report (Table 2).
Table 2.
Vascularized nerve grafts (other than vascularized ulnar) for brachial plexus injuries reconstruction.
| No. Of patients | Type of injury | Gender | Extremity | Nerve | Denervation Time (months) | Age at operation | F-UP (months) | Intraoperative findings | Vascularized nerve graft | No of strands | Length (cm) | Type of reconstruction |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | MCA | M | R | C5 To Axill | 19 | 27 | 32 | C5,C6-R C7-T1-A | saphenous | 2 | 2 × 20 | Shoulder abduction |
| 2 | Bicycle hit by a car | F | R | Cervical plexus to free muscle | 12 | 28 | 9 | C5-R C6-T1-A | saphenous | 1 | 1 × 48 | Elbow flexion |
| 3 | MCA | M | R | C5 To free muscle | 63 | 23 | 0 | C5-R C6-T1-A | saphenous | 3 | 2 × 12 1X15 | NO FU |
| 4 | MCA | M | L | C-lat pec To free muscle | 9 | 17 | 40 | C5,C6-R C7,C8-A T1-T | saphenous | 1 | 1 × 23 | Elbow flexion |
| 5 | MCA | M | L | XI To free muscle | 9 | 17 | 40 | C5,C6-R C7,C8-A T1-T | Superficial radial | 1 | 1 × 24 | Finger extension |
| 6 | MVA | M | R | C-lat pec To free muscle | 3 | 11 | 60 | C5-T1-A | Superficial radial | 2 | 1 × 13 1 × 13 | Finger extension |
MCA motor cycle accident, M male, F female, R rupture, A avulsion, T traction
Preoperative Evaluation
Most patients had vascular impairment (vascular injury, multiple previous surgeries, Volkman’s contracture), and an angiogram was imperative especially if multiple procedures were scheduled (free vascularized nerve graft transfer with free vascularized fascia transfer).
Clinical examination included observation of color and trophic changes, sensibility testing including static, and moving two-point discrimination (2PD), von Frey pressure threshold test, high and low frequency vibration, and ninhydrine test for sudomotor function.
In addition, preoperative and postoperative manual muscle testing was performed along with range of motion. The functional assessment was graded according to the British Medical Research Council muscle grading scale that was used and expanded further with intermediate grades of + and − as reported by Terzis and Vekris in 1999 [28].
For brachial plexus reconstruction, see previous descriptions [24–27].
Surgical Technique
Vascularized nerve grafts are folded into segments maintaining their vascular connections. In cases of long gaps, vascularized nerve grafts can be placed in association with nonvascularized nerve grafts to cover the cross-sectional area of the injured nerve. Vascularized fascia (posterior calf or superficial temporal) can be used to improve the blood supply of the underlying bed by enveloping the nerve reconstruction.
Sural nerve Vascularized sural nerve graft in the upper extremity should be used as a free vascularized nerve graft based on the sural artery or along with an arterialized saphenous vein that is transferred in conjunction with the sural nerve.Indications for the use of vascularized posterior calf fascia are:
The level of the injury: At the wrist and forearm, vascularized fascia facilitates gliding of adjacent tendons
To improve the vascularization of the recipient bed. Vascularized fascia can also be used with conventional nerve grafts to improve the blood supply by enveloping the nerve reconstruction. When there is no concomitant head injury, the superficial temporal fascia is an alternative (Fig. 1). The surgical anatomy of the vascularized sural nerve was previously described by Terzis [24] and others [2, 6, 7].
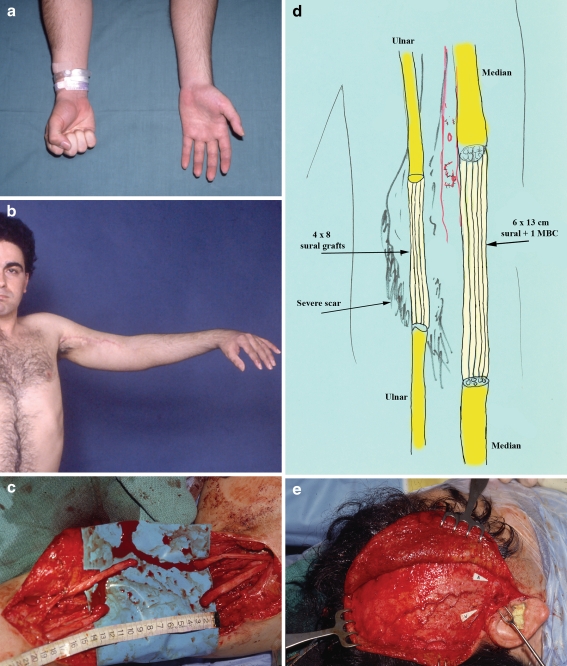
Figure 1.
This is a 24-year-old male who was shot at close range through his left car window. The point of entry was the posteromedial aspect of the upper third of the left arm and the point of exit was the medial aspect of the middle third. He underwent elsewhere emergency vascular repair of the brachial artery with 15 cm saphenous vein graft. There was 12 and 8 cm loss of median and ulnar nerves, respectively. Patient presented to our center 3 months post-injury. Preoperative view of the patient (a, b). On April 1st 1988, 3 months post-injury, the patient underwent: 1. Exploration of the left axilla and upper arm (c). Bilateral sural nerves were harvested, and the ulnar and median nerves were reconstructed with four interposition nerve grafts of 8 cm for the ulnar and six grafts of 13 cm for the median nerve (d). The right superficial temporal fascia flap was harvested based on the superficial temporal vessels (e). Restoration of good vascular bed for the nerve reconstruction took place by wrapping the nerve grafts between the two layers of the free superficial vascularized temporal fascia flap (f). At nearly 6 months, progression of Tinel sign had reached from left axilla to midforearm levels (g) at an impressive rate of 7.8 cm/month, and he was able to pick up a glass and hold it (h). The patient progressed over time and he recovered a powerful grip (i), and he even showed some evidence of intrinsic return (j).
Saphenous nerve For brachial plexus injuries, the indications are the same as vascularized ulnar [27] and for more distal injuries when multiple major nerves are injured or the nerve gaps are too long. The length of the nerve graft can range from 31 to 49 cm, even 63 cm in patients with long legs. The surgical anatomy of the saphenous was previously described by Terzis [24, 25].
Superficial radial nerve Simultaneous reconstruction of the radial artery with interposition vein graft is recommended to prevent sacrifice of a major vessel in the injured upper extremity.
Superficial peroneal nerve The distal parts (sensory) of the deep and superficial peroneal nerves on their common vascular pedicle can be transferred simultaneously to reconstruct double-level injury or two injured nerves. The length of the graft ranges from 14 to 30 cm [24]. The surgical anatomy of this nerve as a vascularized graft has been previously described [24].
Results
Vascularized nerve grafts from the lower extremity were used as free vascularized nerve grafts. Sural nerve (n = 9) and saphenous nerve (n = 8) have been used in the majority of cases, along with the sensory component of the deep and superficial peroneal nerves (n = 1). Nerve grafts from the upper extremity as the superficial radial nerve was used as a pedicled vascularized graft. The median nerve was reconstructed in 12 cases, and the ulnar nerve in three and in six cases was part of a plexus reconstruction (Table 2).
For injuries distal to the plexus, five patients had nerve defect and six patients had neuroma in continuity. The length of the nerve grafts was between 4 and 30 cm (mean length 13.5 cm). The appropriate number of nerve folds for median and ulnar nerve reconstruction in mid-forearm was usually four or five grafts. In three cases, conventional nerve grafts were placed along with vascularized nerve grafts to cover the cross-sectional area of the injured nerve.
Sural nerve was used in seven patients, six with median nerve injury, and one with ulnar nerve injury. In one case, the superficial temporal fascia was used with sural nerve grafts to reconstruct a gunshot defect of the median and ulnar nerve in the proximal arm (Fig. 1).
Vascularized saphenous was used in eight cases, four for brachial plexus injuries, and four for upper extremity injuries. For distal injuries, the mean length bridged was 23.5 cm. One patient had both upper extremities involved and another had four failures of previously used conventional nerve grafts. In each case, vascularization was significantly compromised.
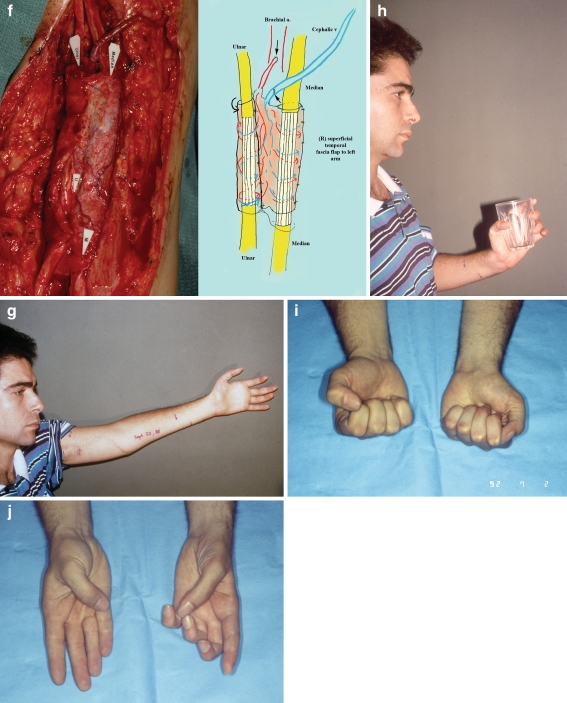
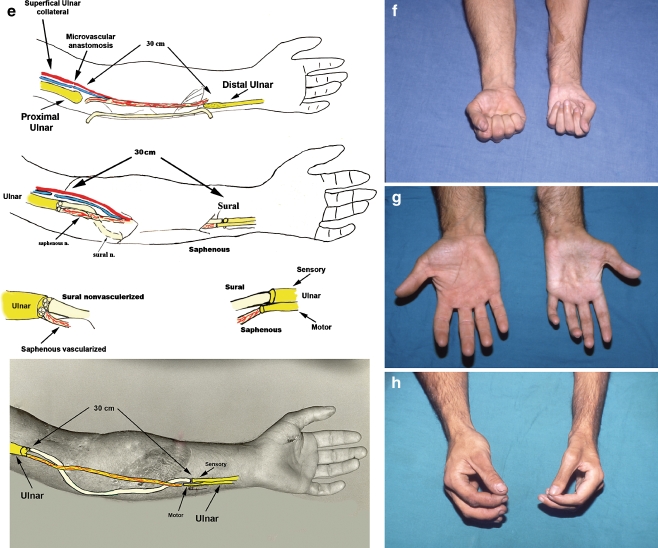
The distal parts (sensory) of the deep and superficial peroneal nerves on their common vascular pedicle were transferred simultaneously to reconstruct the median nerve in a case of double-level injury of both median and ulnar nerve after a boat propeller injury (Fig. 2). The ulnar nerve was reconstructed with a vascularized saphenous nerve. That was the first time (August 1984) that this nerve was used clinically as a free vascularized graft by the senior author (JKT).
Figure 2.
This is a 23-year-old male who was involved in a boating accident in which the propeller of a motor boat ran over his left arm. He was taken emergently to a local hospital where he was noted to have severe neurovascular injuries as well as tissue loss of the left forearm. He received elsewhere emergency revascularization of his left extremity with the use of saphenous vein grafts. He had also multiple levels of nerve injuries of the left ulnar and median nerve. Preoperative view of the patient (a, b); 3 months later, he underwent reconstruction of his left median nerve which was transected at four levels (cabove). The sensory part of the superficial and deep peroneal nerves based on their common vascular supply was harvested and used to reconstruct the motor portion of the median nerve (3 × 15 cm, one deep and two superficial peroneal cables). Nonvascularized sural nerve grafts were used to reconstruct the sensory portion of the median nerve (2 cables × 15 cm proximally and 8 cables × 5.5 cm distally; cbelow). Close-up of the proximal coaptation; vascularized nerve grafts on the left, nonvascularized sural nerve grafts on the right (d). Seven months after the injury he underwent reconstruction of the left ulnar nerve utilizing vascularized saphenous nerve graft (1 cable × 30 cm) for the motor portion of the ulnar nerve and sural nerve graft for the sensory component of the ulnar nerve (e). Four years postoperatively, we can see very good results. Powerful finger flexion, thumb opposition, and intrinsic function (f, g, h, i). He can easily pick a can of coke (j) and has never had any morbidity in the donor lower extremity (k).
Tinel’s Sign Progression
The Tinel progression was at a rate of 2.8 to 7.8 cm/month. The regeneration rate was faster than in conventional nerve grafts but often less than in vascularized ulnar nerve grafts [27].
Pain
Preoperatively, five patients had pain due to neuroma in continuity. Pain was evaluated with visual analog pain scale. Resection of the neuroma resulted in pain relief in all patients. Sensibility was restored in 5–7 months in distal forearm lesions (Table 1).
Sensibility
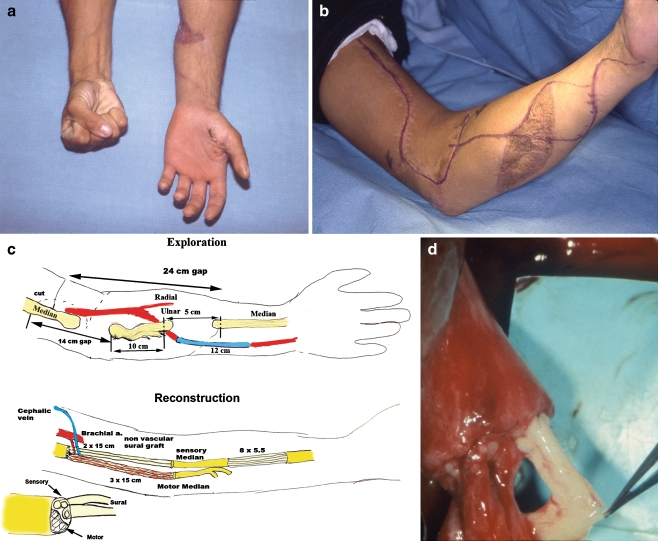
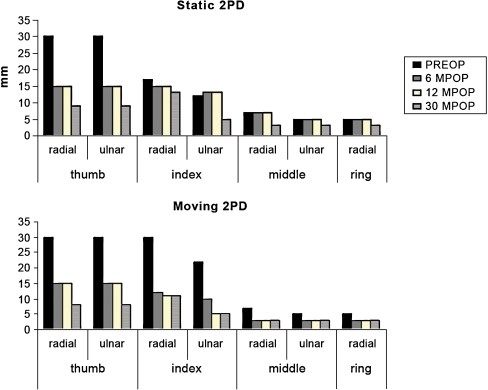
When injury was in the wrist area (n = 5), 2PD (static and moving) improved to near normal levels especially when vascularized fascia was also used (Fig. 3).
Figure 3.
Static and moving two-point discrimination pre- and post-reconstruction with vascularized nerve graft in a median nerve injury.
When the injury was more proximal (n = 10), recovery of sensibility was correlated with patient’s age. In a 7-year-old patient, 2PD returned 4–6 mm at 4 years follow-up. In contrast, a 48-year-old patient perceived only high frequency vibration at 16 months follow-up. Denervation time and length of the nerve graft were relatively constant, since all patients had denervation time more than 1 year and nerve grafts more than 10 cm in length.
When the injury was in the plexus (n = 6), vascularized ulnar nerve grafts were used to give protective sensibility [27].Vascularized saphenous and superficial radial nerves were used to reconstruct motor function only (Table 2).
Motor function
Motor function was restored in six cases, in median (n = 4) and ulnar nerve (n = 2) defects. The level of the injury was at the arm (n = 3) or elbow/proximal forearm (n = 3). The mean age of this group was 20.6 years old. Postoperative, the muscle strength was near normal (muscle grading ≥ 4) even for intrinsic muscles (Fig. 2). Denervation time did not exceed 2 years, and none of the patients had neuroma in continuity. The mean length of the vascularized nerve grafts was 19 cm while for patients that received vascularized fascia and nerve grafts was 12 cm.
A concern with neuroma resection is to preserve existing function and not downgrade the patient. When the neuroma is in the wrist area, the motor branch is separately preserved. When the neuroma is more proximal, the risk of downgrading motor function is higher if identification of the motor component is not possible.
Side Effects
When using vascularized fascia to wrap around the reconstructed nerve(s) in the wrist area, frequently bulky non-esthetic contour is of concern to the patient. Thus, the surgeon has to weigh improving sensibility and alleviating causalgia versus cosmesis.
Discussion
The cases in this report were complex and unique. Because of their diversity, critical statistical analysis was not feasible, but they are useful as they offer 27 years of experience in upper extremity nerve reconstruction. Factors that have influenced outcomes included:
Denervation time (DT)
Patients with denervation time between 3 and 23 months and proximal injuries recovered hand function after both median and ulnar nerve reconstruction.
In other studies [8], denervation time had a profound influence on final results: two patients with denervation time of less than 8 months had full motor function restored; in contrast, patients operated after 18 months had no motor recovery.
In brachial plexus injuries where distances are longer, postoperative muscle strength for patients operated late (DT > 12 months) was significantly decreased compared to the early group [25].
Age
The age of the patient correlated with outcomes in severe brachial plexopathies [27]. In patients younger than 20 years, good and excellent muscle function was restored in 72.7% while for older than 20 years, in 61.5%. In the present study, for motor function reconstruction in young patients (<24 years), motor recovery was almost full (muscle grade ≥ 4).
Neuroma vs. Nerve Gap
Lesions in continuity associated with causalgia as the predominant symptom had multiple previous reconstructions elsewhere (mean 2.8 operations per person) and presented late (mean 9.5 years). In contrast, patients with nerve gaps underwent earlier reconstruction (mean DT 18.1 months), had less pain, and were technically easier to repair. In contrast, others reported better outcomes with lesions in continuity compared to nerve gaps [12].
Length of the Nerve Gap
For nerve gaps less than 7 cm, vascularized sural nerve grafts were found to be superior to conventional grafts especially for repairs in severely scarred beds [3]. Median nerve defects more than 7 cm in length, treated with conventional grafts, yielded poor results [11].
In this study, very good results were achieved even for gaps between 10 and 15 cm (mean length 13.5 cm). Even motor function of intrinsics was recovered after vascularized nerve graft of 30 cm (Fig. 2). Hasegawa et al. [9] supported the use of vascularized sural nerve graft for nerve defects longer than 20 cm. In six upper extremity nerve injuries (five median and one ulnar), the static 2PD test was 10–20 mm.
Koshima et al. 2003 [16] reported 10 mm static 2PD after two and a half years in a 12-cm median nerve gap. This concurs with our results. 2PD in our series was 15 mm by 6 months, 12 and 15 mm by 12 months, and less than 10 mm by 30 months.
Level of Injury
Depending on the level of the injury, median nerve grafting with nonvascularized nerve grafts achieved grade ≥M3 in elbow for 70.5 % of patients, 76.9 % in the wrist [12] and 33.3% (arm) to 52% (elbow) [18]. For ulnar nerve grafts, outcomes were worse [13, 18], and ≥M3 recovery was in 15.4% in the upper arm to 43.6% at elbow even in young population (20–30 years) with short grafts (<4 cm) and DT (1–3.5 months) [18].
In the present study, vascularized nerve grafts or use of vascularized fascia in proximal lesions (Fig. 1) yielded grade 4 or better functional recovery. Early reconstruction of median or ulnar nerve combined with young age facilitated motor recovery.
Vascularized vs. Conventional
Factors contributing to unsatisfactory results with conventional nerve grafts were patient age over 54 years, injuries farther than 56 cm from the finger tip, delays in surgery longer than 24 months, and graft length more than 7 cm [11]. In this series with improved vascularization, excellent results were achieved even for gaps between 10 and 30 cm and even for proximal injuries.
There are few clinical controlled comparative studies, since it is difficult to design such a study. Doi et al. 1992 [5] used 27 vascularized and 22 conventional sural nerve grafts to multiple upper extremity recipients. Results were superior for vascularized compared with nonvascularized in terms of the rate of axonal regeneration, rate of EMG return, and final sensory and motor outcome.
Mackinnon et al. [17] used one superficial vascularized radial nerve graft and one conventional sural nerve graft to reconstruct a median nerve defect in two stages. Sensory function was superior on the side of the vascularized nerve graft.
Boorman and Sykes [1] published a case report in which two lengths of 5 cm of the lateral antebrachial cutaneous nerve was used, one vascularized and one nonvascularized, to reconstruct both digital nerves of the thumb. At 9 months, the vascularized graft side was found to have better sensory recovery.
In the five cases reported [29], the denervation time was 5 months to 2 years, and results showed improved vascularization of the extremity, higher rates of Tinel advancement, and early EMG response. Comparing vascularized vs. nonvascularized nerve grafts in cases that both ulnar and median nerves were reconstructed (one with vascularized and the other with nonvascularized graft), the results favored the vascularized nerve grafts.
In devastating brachial plexus injuries, vascularized ulna nerve grafts for median nerve neurotization yielded protective sensation in the hand in 91.6% of the patients [27] and produced better outcomes compared to conventional nerve grafts (51 % protective sensation) [28].
Tinel’s Sign Advancement
Doi et al. [3] initially based the superiority of vascularization in the faster rate of Tinel sign advancement, but this does not necessarily translate in improved results.
In our study, the Tinel sign progressed at a rate of 2.8 to 7.8 cm/month. Taylor reported similar results [29]. This was a slower rate that was encountered with vascularized ulnar nerve grafts (mean rate of advancement 6.67 ± 2.3 cm/month) [25, 27].
Nerve Graft Selection
Sural nerve grafts can be used when there is also a need for vascularized fascia and saphenous nerves when a long nerve gap exists. Vascularized ulnar nerve graft has been reported for reconstruction of large defects of the upper extremity [10], but in our center, this procedure is reserved for severe avulsion plexopathies [27].
Conclusion
Vascularized nerve grafts for complex upper extremity injuries have provided good to excellent sensory return in severely scarred beds in patients in whom conventional nerve grafts had failed. They have also provided relief of causalgia after painful neuroma resection and rewarding degree of motor recovery in selective cases even for above the elbow injuries. Vascularized nerve grafts can also be used successfully to bridge long nerve gaps (10–30 cm) and also for patients who present late for treatment. As long as preoperative needle electromyography indicates that the denervated targets are still present (fibrillations).
References
- 1.Boorman JG, Sykes PJ. Vascularised versus conventional nerve grafting: a case report. J Hand Surg [Br] 1987;2:218–220. doi: 10.1016/0266-7681_87_90016-7. [DOI] [PubMed] [Google Scholar]
- 2.Breidenbach WC, Terzis JK. The anatomy of free vascularized nerve grafts. Clin Plast Surg. 1984;1:65–71. [PubMed] [Google Scholar]
- 3.Doi K, Kuwata N, Kawakami F, et al. The free vascularized sural nerve graft. Microsurgery. 1984;5:175–184. doi: 10.1002/micr.1920050403. [DOI] [PubMed] [Google Scholar]
- 4.Doi K, Kuwata N, Sakai K, et al. A reliable technique of free vascularized sural nerve grafting and preliminary results of clinical applications. J Hand Surg [Am] 1987;12:677–684. doi: 10.1016/s0363-5023(87)80047-3. [DOI] [PubMed] [Google Scholar]
- 5.Doi K, Tamaru K, Sakai K, et al. A comparison of vascularized and conventional sural nerve grafts. J Hand Surg [Am] 1992;4:670–676. doi: 10.1016/0363-5023(92)90315-G. [DOI] [PubMed] [Google Scholar]
- 6.Fachinelli A, Masquelet AC, Restrepo J, et al. The vascularized sural nerve. Int J Microsurg. 1981;3:57. [Google Scholar]
- 7.Gilbert A. Vascularized sural nerve graft. In: Terzis JK, editor. Microreconstruction of nerve injuries. Philadelphia: W.B.Saunders; 1987. pp. 101–16. [Google Scholar]
- 8.Gu YD, Wu MM, Zheng YL, et al. Arterialized venous free sural nerve grafting. Ann Plast Surg. 1985;4:332–339. doi: 10.1097/00000637-198510000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Hasegawa T, Nakamura S, Manabe T, et al. Vascularized nerve grafts for the treatment of large nerve gap after severe trauma to an upper extremity. Arch Orthop Trauma Surg. 2004;124:209–213. doi: 10.1007/s00402-003-0617-6. [DOI] [PubMed] [Google Scholar]
- 10.Hattori Y, Doi K, Ikeda K. Vascularized ulnar nerve graft for reconstruction of a large defect of the median or radial nerves after severe trauma of the upper extremity. J Hand Surg [Am] 2005;30:986–989. doi: 10.1016/j.jhsa.2005.03.017. [DOI] [PubMed] [Google Scholar]
- 11.Kallio PK, Vastamaki M. An analysis of the results of late reconstruction of 132 median nerves. J Hand Surg [Br] 1993;18:97–105. doi: 10.1016/0266-7681(93)90205-t. [DOI] [PubMed] [Google Scholar]
- 12.Kim DH, Kam AC, Chandika P, et al. Surgical management and outcomes in patients with median nerve lesions. J Neurosurg. 2001;95:584–594. doi: 10.3171/jns.2001.95.4.0584. [DOI] [PubMed] [Google Scholar]
- 13.Kim DH, Han K, Tiel RL, et al. Surgical outcomes of 654 ulnar nerve lesions. J Neurosurg. 2003;98:993–1004. doi: 10.3171/jns.2003.98.5.0993. [DOI] [PubMed] [Google Scholar]
- 14.Koshima I, Murashita T, Soeda S. Free vascularized deep peroneal neurocutaneous flap for repair of digital nerve defect involving severe finger damage. J Hand Surg [Am] 1991;16:227–229. doi: 10.1016/s0363-5023(10)80101-7. [DOI] [PubMed] [Google Scholar]
- 15.Koshima I, Okumoto K, Umeda N, et al. Free vascularized deep peroneal nerve grafts. J Reconstr Microsurg. 1996;12:131–141. doi: 10.1055/s-2007-1006466. [DOI] [PubMed] [Google Scholar]
- 16.Koshima I, Nanba Y, Tsutsui T, et al. Vascularized femoral nerve graft with anterolateral thigh true perforator flap for massive defects after cancer ablation in the upper arm. J Reconstr Microsurg. 2003;19:299–302. doi: 10.1055/s-2003-42498. [DOI] [PubMed] [Google Scholar]
- 17.Mackinnon SE, Kelly L, Hunter DA. Comparison of regeneration across a vascularized versus conventional nerve graft: case report. Microsurgery. 1988;4:226–234. doi: 10.1002/micr.1920090403. [DOI] [PubMed] [Google Scholar]
- 18.Roganovic Z, Pavlicevic G. Difference in recovery potential of peripheral nerves after graft repairs. Neurosurgery. 2006;59:621–633. doi: 10.1227/01.NEU.0000228869.48866.BD. [DOI] [PubMed] [Google Scholar]
- 19.Rose EH, Kowalski TA. Restoration of sensibility to anesthetic scarred digits with free vascularized nerve grafts from the dorsum of the foot. J Hand Surg [Am] 1985;4:514–521. doi: 10.1016/s0363-5023(85)80075-7. [DOI] [PubMed] [Google Scholar]
- 20.Rose EH, Kowalski TA, Norris MS. The reversed venous arterialized nerve graft in digital nerve reconstruction across scarred beds. Plast Reconstr Surg. 1989;4:593–604. doi: 10.1097/00006534-198904000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Strange FGSC. An operation for nerve pedicle grafting. Preliminary communications. Br J Surg. 1947;34:423. doi: 10.1002/bjs.18003413617. [DOI] [PubMed] [Google Scholar]
- 22.Taylor GI, Ham FJ. The free vascularized nerve graft. Plast Reconstr Surg. 1976;57:413–426. doi: 10.1097/00006534-197604000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Taylor GI. Free vascularized nerve transfer in the upper extremity. Hand Clin. 1999;4:673–695. [PubMed] [Google Scholar]
- 24.Terzis JK, Breidenbach WC. The anatomy of free vascularized nerve grafts. In: Terzis JK, editor. Microreconstruction of nerve injuries. Philadelphia: W.B.Saunders; 1987. pp. 101–16. [Google Scholar]
- 25.Terzis JK, Kostopoulos VK. Vascularized nerve grafts: a review. Atlas Hand Clin. 2005;10:101–102. doi: 10.1016/j.ahc.2004.08.004. [DOI] [Google Scholar]
- 26.Terzis JK, Kostopoulos VK. The surgical treatment of Brachial Plexus Injuries in Adults. Plast Reconstr Surg. 2007;119:73–92. doi: 10.1097/01.prs.0000254859.51903.97. [DOI] [PubMed] [Google Scholar]
- 27.Terzis JK, Kostopoulos VK. Vascularized ulnar nerve graft. 151 reconstructions for posttraumatic brachial plexus palsy. Plast. Reconstr. Surg. 2009;123:1276–91. [DOI] [PubMed]
- 28.Terzis JK, Vekris MD, Soucacos PN. Outcomes of brachial plexus reconstruction in 204 patients with devastating paralysis. Plast Reconstr Surg. 1999;5:1221–1240. doi: 10.1097/00006534-199910000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Townsend PL, Taylor GI. Vascularised nerve grafts using composite arterialised neuro-venous systems. Br J Plast Surg. 1984;1:1–17. doi: 10.1016/0007-1226(84)90034-1. [DOI] [PubMed] [Google Scholar]