Abstract
Background
Studies have shown an association between visual impairment and poor overall function. Studies from Africa and developing countries show high prevalence of visual impairment. More information is needed on the community prevalence and impact of visual impairment among elderly Africans.
Methods
A multi-stage stratified sampling of households was implemented to select persons aged 65 years and over in the south-western and north-central parts of Nigeria. Impairments of distant and near vision were based on subjective self-reports obtained with the use of items derived from the World Health Organization multi-country World Health Survey questionnaire. Impairment was defined as reporting much difficulty to questions on distant and near vision. Disabilities in activities of daily living (ADL) and instrumental activities of daily living (IADL) were evaluated by interview, using standardized scales.
Results
A total of 2054 subjects 957 (46.6%) males and 1097 (53.4) females responded to the questions on vision. 22% (n=453) of the respondents reported distant vision impairment, and 18% (n=377) reported near vision impairment (not mutually exclusive). 15% (n= 312) however reported impairment for both far and near vision. Impairment of distant vision increased progressively with age (P < 0.01). Persons with self reported near vision impairment had elevated risk of functional disability in several IADLs and ADLs than those with out. Distant vision impairment was less associated with role limitations in both ADLs and IADLs.
Conclusion
The prevalence of self reported distant visual impairment was high but that for near visual impairment was less than expected in this elderly African population. Impairment of near vision was found to carry with it a higher burden of functional disability than that of distant vision.
Keywords: visual impairment, activities of daily living, functional disability
Introduction
Visual impairment, that is best-corrected visual acuity less than 6/18 as defined in the International Statistical Classification of Diseases and related Health problems, tenth revision (ICD-10)1 is a global public health problem. The year 2002 global estimates of prevalence of visual impairment and its causes showed that over 161milion people were visually impaired, while 37 million were blind and 124million had low vision2. The prevalence and aetiology of blindness and visual impairment varies according to age, sex, ethnicity, geographical location, occupation, and availability of ophthalmic services to the population3.
Visual impairment is a common finding in surveys of the elderly in both developing and developed countries due to increasing incidence of blinding disorders such as cataract, age related macular degeneration (ARMD), glaucoma, and diabetic retinopathy with increasing age3,4,5, . A World health Organization estimate in 2002 put the prevalence of blindness for those aged 50 years and above in 13 countries from Africa south of the Sahara as 9%, with a further 3 fold increase in prevalence (27%) for those with visual impairment in the same age group2. The result of the prevalence of blindness and low vision survey in Malaysia revealed an age adjusted prevalence of blindness and low vision of 0.29% and 2.44 % respectively but for those aged 60-70 years 0.69% were blind increasing to 4.77% for those aged 70 years or more6. A study to determine the incidence of visual loss in rural southwest Uganda observed that the incidence increased with age from 1.21 per 1000 among people aged 13-34 years to 64.2 per 1000 in those aged 65 years or older 7. A population based study of presbyopia in rural Tanzania observed that 61.7% of the 2040 eligible participants were presbyopic. A higher prevalence of presbyopia was associated with increased age, female gender, higher educational level, and residence in town 8. A study to evaluate the national eye care program after 10 years in the Gambia observed a reduction in the crude prevalence of blindness from 0.70% to 0.42% but a modest but significant increased risk of low vision due to cataract across the country9. The Salisbury Eye Evaluation (SEE) project,10 the Beaver Dam Eye Study,11 and the Melbourne (Australia) Visual Impairment Project 12 all showed increasesd prevalence of vision impairment with age,
Although the standard measure of visual function in eye research has been Snellen visual acuity, other non-Snellen measures of visual function may be more important in determining the functional impact of visual loss in elderly persons. Rubin et al described the correlation between psychophysical measures of visual impairment and self-reported difficulty with everyday visual tasks in a population-based sample of persons aged 65 years and older. Community dwelling adults aged 65 years and older were administered a battery of vision tests including distance acuity, letter contrast sensitivity, disability glare, and stereo acuity. A physical function questionnaire assessed self-reported difficulty with activities of daily living (ADL’s), Instrumental activities of daily living (IADL’s), and mobility activities. A visual function questionnaire assessed self-reported difficulty with a wide variety of everyday visual activities. They observed that poor performance on each of the vision tests except low luminance acuity was independently associated with lower activities of daily vision scale scores.13,14 A recent study examined the association between visual impairment and self reported vision function in a population of 1807 elderly people in the UK aged more than 75 years with the 25-item National Eye Institute Visual Function Questionnaire (NEI-VFQ). It was observed that after adjustment for age, gender, practice and NEI-VFQ sub-scale scores, those complaining of poor vision in general were 4.77 times (95% CI 3.03 to 7.53) more likely to be visually impaired compared to those who did not report difficulty.15
Several population-based studies have also shown an association between visual impairment and overall function. In Established Populations for the Epidemiological Studies of the Elderly, a population-based study of 5143 elderly persons, severe impairment of visual acuity was associated with a 3-fold increase in the incidence of limitations in mobility and activity of daily living16 The Massachusetts Health Care Panel Study of non-institutionalised elderly persons reported 289 with good vision and 207 with self-perceived visual impairment.17 The poor-vision group was 2.3 times more likely than the group with good vision to need help with grocery shopping and 1.68 times more likely to need help paying bills. In the Salisbury Eye Evaluation project, researchers found visual impairment to be an important predictor of lack of social or religious activities.10 They also found visual loss to be associated with 1.82 times greater odds of significant difficulty on any ADL and to be associated with 2.45 greater odds of significant difficulty on any instrumental ADL. The Blue Mountains Eye Study found that visual impairment affects the independence of elderly persons, especially women.18 A study which examined the impact of presbyopia on the quality of life in rural Tanzania observed that being presbyopic increased the odds of reporting some difficulty with near vision tasks by 2-fold and high difficulty by >8-fold.19 Another study observed functional limitation amongst persons with visual loss from trichiasis (expecially females) in trachoma endemic Tanzania.20
More information is needed on the impact of vision loss in a large elderly African population. This study was therefore carried out with the objective of determining the prevalence of self-reported visual impairment and its impact on functioning in an elderly population in a Nigerian community.
Materials and methods
The Ibadan Survey of Aging (ISA) is a community based survey of the mental and physical health status as well as the functioning and disability of elderly persons (aged 65 years and over) residing in the Yoruba-speaking areas of Nigeria, consisting of eight contiguous states in the south-western and north-central regions (Lagos, Ogun, Osun, Oyo, Ondo, Ekiti, Kogi and Kwara). These states account for about 22% of the Nigerian population (approximately, 25 million people). The survey was conducted between November 2003 and August 2004.
Respondents were selected using a four-stage area probability sampling of households. In the first stage of the sampling, 14 strata were created from an ordered list of all Local Government Areas (LGA’s) in 7 of the states on the basis of 2 strata per state (rural or urban). LGAs in Lagos State were constituted into one self-representing stratum, on the basis of the size and cosmopolitan nature of the state. The LGAs thus formed the Primary Sampling Units (PSUs). An LGA is a geographic unit with a defined administrative and political structure. Two LGAs were selected from each of the 14 strata (except in Kogi State where there was only one rural LGA), with the probability of selection proportional to size. With the 17 self-representing PSUs in Lagos, a total of 44 PSUs was obtained. (One selected PSU in Kwara was subsequently dropped before fieldwork commenced in view of an on-going civil strife in the LGA). In the second stage, four Enumeration Areas (EAs) were systematically selected from each of the 43 PSUs. EAs are geographic units of LGAs and consist of between 50 and 70 housing units. They are a creation of the National Population Commission and are used by the Commission in the conduct of national census.
All selected EAs were visited by research interviewers prior to the interview phase of the survey and an enumeration and listing of all the household units in which persons aged 65 years and older resided was conducted. These lists were entered into a centralized computer data file from which the survey sample of households was drawn randomly from each EA. In the final stage of the selection, which was conducted during the interview phase of the survey, interviewers obtained a full listing of all persons aged 65 years and over residing in the household from an informant. In each households with more than one eligible person (aged 65 years and fluent in the language of the study, Yoruba), the Kish table selection method was used to select one respondent21. When the primary respondent was either unavailable following repeated calls (5 repeated calls were made) or refused to participate, no replacement was made within the household. On the basis of this selection procedure, face-to face interviews were carried out on 2152 respondents, giving a response rate of 74.2%. Non-response was predominantly due to non-availability after repeated visits (14%), interviewers unable to trace the original address (4%), death (3%), and physical incapacitation (2%) and rarely due to refusal (2%). Respondents were informed about the study and provided consent, mostly verbal but sometimes signed, before interviews were conducted.
The survey was approved by the University of Ibadan/University College Hospital, Ibadan Joint Ethical Review Board.
Measures
Vision was assessed with the use of self-report questions derived from the World Health Organization multi-country World Health Survey questionnaire22. Distant vision was assessed by asking respondents whether, in the past month and with the use of spectacles if they wore any, they had difficulty in seeing and recognizing somebody known to them across the road. For near vision, respondents were asked whether they had difficulty in seeing clearly or reading something held at an arm’s length in the past month with the use of spectacles if they wore any. Possible responses were: no difficulty, some difficulty, and marked difficulty. In this report, persons with marked difficulty are classified as being visually impaired. These self reports were reliably made: analysis of test-retest assessment of 32 respondents conducted approximately one week apart gave a kappa value of 0.80 (s.e. 0.14) for distant vision and 1.0 (s.e. 0.00) for near vision.
Functional limitations were rated in two domains: 1) Activities of daily living (ADL) were assessed with the use of the Katz Index of Independence in Activities of Daily Living: bathing, dressing, toileting, arising and transferring, continence, and feeding. We changed the wording of the transfer item from “bed to chair” to “chair without arms or bed to standing”. 2) Instrumental activities of daily living (IADL) were assessed using a scale of seven items adapted from Nagi Physical Performance Scale and the Health Assessment Questionnaire: walking (around the house), climbing a flight of stairs, reaching above the head to carry something as heavy as 10 pounds, stooping, griping small objects with hands, shopping, and activities such as sweeping the floor with a broom or pruning the grass around the yard. Each of the activities in the two domains was rated: 1) can do without difficulty, 2) can do with some difficulty, 3) can do only with assistance, or 4) unable to do. In this report, a rating of 3 or 4 was used to determine functional limitation on an item. Responses were dichotomized to “yes” or “no”. A sub-group of 37 respondents was assessed twice, about 7 days apart, to determine the test-retest reliability of the disability items. Agreement was generally very good to excellent, ranging from a kappa of 0.65 to 1.0. A full report of the functional status of the sample, showing the distribution and profile of disability, is provided elsewhere23.
Self-reported chronic medical and pain conditions were also assessed in the ISA. Respondents were asked if they had any chronic respiratory conditions (asthma, tuberculosis, other lung disease), digestive conditions (irritable bowel syndrome, ulcer), cardiovascular conditions (high blood pressure, heart disease, heart attack, stroke), cancer, diabetes, or epilepsy. The pain conditions assessed included back or neck pain, chest pains, joint pains, frequent headaches, and a general category of persistent pain in any other body parts. Respondents were asked whether they had experienced each of these conditions in the previous 12 months. Responses were coded “yes” or “no”. In the analysis herein presented, two items were produced from the responses to these questions: any chronic medical condition and any chronic pain condition. Respondents were dichotomized to those with a report of any chronic medical condition in the prior 12 months versus those with no such condition; those with a report of any chronic pain problem in the prior 12 months versus those with no chronic pain.
All the instruments were translated using iterative back-translation method. As part of the translation process, all the instruments used were subjected to cultural adaptation. Thus, for example, in describing 10 Ibs in the functional assessment, a tuber of yam (a local stable) of such weight was used.
Data analysis
In order to take account of the stratified multistage sampling procedure and the associated clustering, weights have been derived and applied to the rates presented in this report. The weights were computed to account for the probability of selection as well as non-response. Non-response bias equation was estimated from demographic (age, sex, marital status) and residence (rural, semi-urban, and urban) variables. The non-response adjustment weight was the multiplicative inverse of the predicted probability of response based on this equation. Also, post-stratification to the target sex and age range were made to adjust for differences between the sample and the total Nigerian population (according to 2000 United Nations projections). The weight so derived was normalized to reset the sum of weights back to the original sample size of 2152.
The analysis took account of the complex sample design and weighting. Thus, we used the jacknife replication method implemented with the STATA statistical package to estimate standard errors for proportions 24. Associations were explored with logistic regression analysis23 and the estimates of standard errors of the Odds Ratio (ORs) obtained were made with the STATA. The logistic regression model explored the risk of specific functional limitations among persons with visual impairment after controlling for the effects of age (in years), sex, and self-reported chronic medical condition so as to reduce the possibility of confounding. All probability tests are two-sided and all estimates are adjusted for design effects. The design effects were based on two sampling error calculation units (SECUs) per stratum, a decision that was dictated by our use of the jacknife replication method.
Results
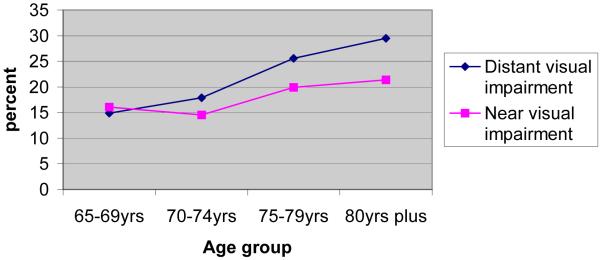
A total of 2054 (95.5%) subjects out of the original sample of 2152 answered the vision related questions. They consisted of 957 (46.6%) males and 1097 (53.4) females. Four hundred and fifty three (22.3%) of the studied population reported having visual impairment for distant vision, 377(18.4%) reported visual impairment for near vision while 312 (15.2) reported visual impairment for both far and near. Although 16.5% of responders reported the use of spectacles it was not possible to determine the proportions reporting visual impairment that might be due to uncorrected refractive errors or underlying ocular pathology. However 391 (75.5%) of respondents who reported visual impairment for far or near wore no corrective lenses, while 60.6% of spectacle wearers reported no vision impairment suggesting they were happy with their corrections. There was no significant difference in the distribution of reported visual impairment for distance between male and female sexes (20.9% of females vs.19.3% of males were visually impaired for distance; P=0.4). Females were however slightly less likely to have reported near vision impairment than males (15.3% vs.18.3%; P=0.06). Table 1 shows the prevalence of self reported visual impairment by age, gender, spectacle use and chronic illness. Table 2 shows the prevalence of self reported visual impairment by ADL and IADL. The relationship between age and prevalence of reported distant visual impairment was that of progressively higher rates with increasing age (P < 0.01). The prevalence of reported impairment of near vision also increased with age up until the 70-74 year age group where there was a marginal drop before it continued to increase. Details are shown in Figure 1
Table1.
prevalence of self reported visual impairment by age, spectacle use and overall health of respondents
| Respondents | N | Distant impairment | Near impairment | Both near &distant | Neither |
|---|---|---|---|---|---|
| Age (years) | % | % | % | % | |
| 65-69 | 676 | 14.9 | 16.1 | 10.1 | 79.0 |
| 70-74 | 469 | 17.2 | 14.4 | 10.7 | 78.3 |
| 75-79 | 285 | 25.6 | 19.8 | 16.6 | 71.1 |
| 80 + | 624 | 29.5 | 21.4 | 19.2 | 68.3 |
| Gender | |||||
| Male | 957 | 19.3 | 18.3 | 12.1 | 74.7 |
| Female | 1097 | 20.9 | 15.3 | 13.1 | 77.3 |
| Use of Spectacle |
334 | 31.5 | 28.7 | 28.6 | 60.6 |
| Self reported poor over all health |
604 | 19.8 | 22.9 | 22.3 | 71.1 |
Table 2.
Self reported visual impairment by ADL/IADL
| ADL/IADL | N | Near impairment | Distant impairment | Both near &distant | Neither |
|---|---|---|---|---|---|
| % | % | % | % | ||
| Difficulty bathing | 46 | 35.9 | 27.8 | 25.9 | 61.8 |
| Dressing | 20 | 46.4 | 46.4 | 45.6 | 53.5 |
| Toileting | 43 | 47.9 | 48.3 | 46.3 | 51.6 |
| Arising and transforming from chair, bed |
23 | 38.8 | 33.3 | 30.7 | 61.1 |
| Continence | 13 | 17.9 | 17.9 | 15.7 | 82.0 |
| Feeding | 7 | 27.6 | 42,5 | 42.6 | 57.4 |
| Walking | 44 | 47.9 | 49.4 | 46.7 | 50.5 |
| Climbing stairs | 110 | 40.5 | 40.7 | 39.2 | 55.1 |
| Reaching out over-head for a load |
83 | 49.9 | 39.0 | 37.1 | 47.1 |
| Stooping | 30 | 40.5 | 44.1 | 42.4 | 55.9 |
| Hand grip (opening door, tap) |
27 | 52.6 | 56.8 | 56.0 | 43.2 |
| General activities in the home |
188 | 37.0 | 39.0 | 38.0 | 57.9 |
Figure 1. Relationship between ageing and prevalence of self reported distant and near visual impairment.
Evaluation of the impact of distant vision impairment on self-reported overall health showed that, compared with respondents without impairment, subjects who reported visual impairment for distance had an elevated risk of rating themselves as poor in overall health (Odds Ratio 1.7, 95% confidence interval (CI) 1.10 – 2.62; P < 0.02). This risk trend persisted but was not statistically significant when adjusted for the effects of age (in years), sex, and the presence of self-reported chronic illness (OR=1.5, 95% CI 0.98 – 2.36; P=0.06). The association of near vision impairment with self-reported poor overall health was less striking (unadjusted OR = 1.4, 95% CI 1.01 – 2.05, p = 0.04; adjusted OR = 1.3, 95% CI 0.94 – 1.88, p = 0.10).).
The effects of impairment of distant vision on activities of daily living after adjusting for the effects of age, sex, self reported vision impairment, chronic medical illness, and chronic pain, are shown on Table 3. Persons with impairment of distant vision had marginally elevated although not statistically significant risk of functional disability in toileting, walking, climbing, stooping, gripping, and in the performance of general household activities. Table 4 shows the impact of impairment of near vision on functioning adjusted for self reported distant impairment. There was more than 3-fold elevation of risk for such persons to be disabled in the performance of toileting and dressing (both activities of daily living). Also, persons with near vision impairment were 3 – 4 times more likely to be disabled in all the areas of instrumental activities of daily living examined.
Table 3. Risk of functional disability among persons with self reported distant vision impairment.
| Activity | Odds ratio* | 95% Confidence interval | P-value |
|---|---|---|---|
| Difficulty bathing | 0.5 | 0.11-1.88 | 0.27 NS |
| Dressing | 1.3 | 0.66-2.54 | 0.43 NS |
| Toileting | 1.2 | 0.68-2.23 | 0.47 NS |
| Arising and transferring from chair, bed |
0.5 | 0.19-1.22 | 0.12 NS |
| Continence | 0.4 | 0.16-1.00 | 0.05 |
| Feeding | 2.8 | 0.33-24.14 | 0.33 NS |
| Walking | 1.5 | 0.89-2.45 | 0.12 NS |
| Climbing stairs | 1.1 | 0.59-2.02 | 0.77 NS |
| Reaching out over-head for a load |
0.5 | 0.24-1.41 | 0.23 NS |
| Stooping | 1.4 | 0.69-2.92 | 0.33 NS |
| Hand grip (opening door, tap) |
1.8 | 0.77-4.09 | 0.17 NS |
| General activities in the home |
1.2 | 0.75-1.96 | 0.41 NS |
Adjusted for age (in years), sex, self-reported medical and pain conditions and near vision impairment.
Table 4.
Risk of functional disability among persons with self reported near vision impairment
| Activity | Odds ratio* | 95% Confidence interval | P-value |
|---|---|---|---|
| Difficulty bathing | 4.2 | 0.9-18.86 | 0.06 NS |
| Dressing | 3.3 | 1.77-6.26 | 0.01 |
| Toileting | 3.3 | 1.82-6.10 | 0.01 |
| Arising and transforming from chair, bed |
4.0 | 1.47-11.07 | 0.01 |
| Continence | 1.3 | 0.53-3.32 | 0.53 NS |
| Feeding | 0.8 | 0.36-1.72 | 0.55 NS |
| Walking | 3.3 | 1.78-6.10 | 0.01 |
| Climbing stairs | 3.1 | 1.66-5.94 | 0.01 |
| Reaching out over-head for a load |
7.07 | 2.71-18.45 | 0.01 |
| Stooping | 2.3 | 1.17-4.44 | 0.01 |
| Hand grip (opening door, tap) |
3.03 | 1.33-6.88 | 0.01 |
| General activities in the home |
2.6 | 1.53-4.31 | 0.01 |
Adjusted for age (in years), sex, self-reported distant vision impairment, medical and pain conditions.
Discussion
The study observed a prevalence of self reported visual impairment for distance of 22.3 % and for near of 18.4%. It was not possible to objectively measure the actual visual acuity values of the subjects (by virtue of the study design), self reported assessment of visual function is a useful way of determining visual ability as previously reported by other studies 13,14,15,26,27. The proportion of elderly individuals living with self reported distant visual impairment would appear low when compared to WHO estimates for objective visual impairments of about 27% for the same age group within the study area 2. A survey of older adults in southern India28 reported presence of bilateral visual impairment of 18.7% out of the 5411 subjects studied. A Malaysian population survey observed that the prevalence of low vision for those aged 60-69 years was 12.3 and increasing to 30.6 for those aged 70 years and over6. A study from Tanzania8 which determined the prevalence of presbyopia objectively in a rural African population reported a prevalence rate for presbyopia of 61.7% which was much higher than 18% obtained by self reported near visual impairment by our study but has similarity in showing increasing prevalence with age.
We observe that there may have been bias in self reports of visual impairment in view of the lower rates of self reported visual impairment when compared to WHO estimates and the study from Tanzania. Our rates and those of other less developed countries would however appear high when compared to surveys on visual impairment from developed parts of the world. The Salisbury Eye Evaluation survey observed a prevalence of Snellen measured visual impairment 20/40 or worse of 11.4% in whites and 16.4% in blacks10. The Blue Mountains Eye study 18 reported a prevalence of 7.5% for presenting visual acuity less than 20/40. A study on Mexican-Americans28 reported monocular visual impairment of 15.2%. Socio-economic factors and the availability of eye care services may be responsible for the observed differences in prevalence estimates of visual impairment between the developed and developing countries as was suggested in previous reports (the risk for eye problems and the ability of the health system to provide adequately for the visually impaired)2,3. Thus a study which evaluated the Gambia national eye care program (supported by Sight Savers International) after 10 years observed that although the crude prevalence of blindness fell from 0.70% to 0.42%, the risk of blindness was reduced to half its 1986 level in the western region where the national eye care programme was started. There was no evidence of significant change in the risk of blindness in the central and eastern health regions but the gradient of the risk ratios across the three regions from west to east reflected the expected effect of the phased intervention, and suggested a causal relation between the intervention and the changes in risk of blindness6. Of course, cultural and racial differences could not be ruled out as possible differential risk factors. Institutionalized care is not practiced in the studied community and in fact many other African communities with extended family system, and the observed prevalence are not likely to have been affected by the exclusion of institutionalized subjects. In developed countries where institutionalized care is practiced prevalence estimates are likely to be lower because those in institutionalized care are usually excluded.
Self reported near vision impairment more than distant visual impairment was found to be associated with functional disability. This is in consonance with observations from Tanzania which found uncorrected presbyopia to have a significant impact on vision-related quality of life in a rural African setting, with the risk increasing with the degree of presbyopia.19 These disabilities were not attributable to age, sex, or a co-occurring medical or pain condition. Persons with impairment with near vision were particularly more functionally disabled both in activities of daily living as well as instrumental activities of daily living. Frick et al also observed that females with trichiasis with or with out vision loss and men with vision loss were more likely to report difficulties with daily activities of village life in trachoma endemic Tanzania.20 The study by Knudtson et al30 on age related eye disease, quality of life, and functional activity found that persons who had trouble reading small print or recognising people across the street were more likely to have an age related eye disease and many measures of general quality of life and functional activities were related to age related eye diseases but few associations remained significant after adjustment for vision and other co-morbidities. The SEE project, reporting on how visual impairment affects performance of every day life, observed a linear relationship between function and vision measures with both contrast sensitivity and visual acuity loss found to independently contribute to deficits in performance of every day tasks31. Also, Rubin et al32 in evaluating visual impairment and disability in older adults, observed that reduced acuity and contrast sensitivity were significant risk factors for self reported disability.
Our findings suggest that progressive loss of vision with the ageing process is associated with loss of functional independence and therefore has implications for the provision of care for the elderly. Persons who lose their ability to independently perform daily activities will require formal or informal care. In a setting such as ours where formal support services are either non-existent or inadequate, informal caregivers are the traditional sources of support. However, economic pressures and urban migration are putting pressures on these sources and elderly persons in need may no longer be assured of informal support. Governments in developing countries in general, and those in Sub-Sahara Africa will need to be aware of the data such as reported here in planning for the increasing number of elderly persons in their populations.
Limitations
There is need to interpret the results of this study with caution, we admit there must have been much underreporting of visual impairment since it was not possible to objectively take actual measurements of visual acuities as well as determine the causes of visual impairment by virtue of our study design.
In conclusion, our data revealed a high prevalence of self reported visual impairment in an elderly African population and supports previous studies from elsewhere, which showed that visual impairment increases with age and has an adverse effect on the independence and functional ability of the elderly.
Acknowledgment
The project “Ibadan Study of Ageing” was funded by the Wellcome Trust (GR06/94/08/MA).
References
- 1.Thylefors B, Negrel AD, Pararajasegaram R, Dadzie KY. Global data on blindness. Bull WHO. 1995;73(1):115–121. [PMC free article] [PubMed] [Google Scholar]
- 2.Resnikoff S, Pascolini D, Etya,le D, Pararajasegaram R, et al. Global data on visual impairment in the year 2002. Bulletin of WHO. 2004;82:844–51. [PMC free article] [PubMed] [Google Scholar]
- 3.Hyman L, Wu S, Connell AMS, Schachat A, Nemesure B, Hennis A, Leske MC. Prevalence and causes of visual impairment in the Barbados eye study. Ophthalmol. 2001;108(10):1751–6. doi: 10.1016/s0161-6420(01)00590-5. [DOI] [PubMed] [Google Scholar]
- 4.Brenner MH, Curbow B, Javitt JC, et al. Vision change and quality of life in the elderly. Response to cataract surgery and treatment of other chronic ocular conditions. Arch Ophthalmol. 1993;111:680–685. doi: 10.1001/archopht.1993.01090050114040. [DOI] [PubMed] [Google Scholar]
- 5.Campbell VA, Crews JE, Moriarty DG, et al. Surveillance for sensory impairment, activity limitation, and health-related quality of life among older adults—United States, 1993-1997. Mor Mortal Wkly Rep CDC Surveill Summ. 1999;48:131–156. [PubMed] [Google Scholar]
- 6.Zainal M, Ismail SM, Ropilah AR, Elias H, Arumugam G, et al. Prevalence of low vision in Malaysian population: results from the National Eye Survey 1996. Br J Ophthalmol. 2002;86(9):951–6. doi: 10.1136/bjo.86.9.951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mbulaiteye SM, Reeves BC, Mulwanyi F, Whitworth JAG, Johnson G. Incidence of visual loss in rural south west Uganda. Br J. Ophthalmol. 2003;87:829–33. doi: 10.1136/bjo.87.7.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Burke AG, Patel I, Munoz B, Kayongoya A, Wilson Mchiwa W, et al. Population-Based Study of Presbyopia in Rural Tanzania. Ophthalmol. 2006;113:726–27. doi: 10.1016/j.ophtha.2006.01.030. [DOI] [PubMed] [Google Scholar]
- 9.Faal H, Minassian DC, Dolin PJ, Mohamed AA, Ajewole J, Johnson GJ. Evaluation of a national eye care programme: re-survey after 10 years. Br J Ophthalmol. 2000;84:948–951. doi: 10.1136/bjo.84.9.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rubin GS, West SK, Munoz B, et al. Salisbury Eye Evaluation Project A comprehensive assessment of visual impairment in a population of older Americans. The SEE Study. Invest Ophthalmol Vis Sci. 1997;38:557–568. [PubMed] [Google Scholar]
- 11.Klein R, Klein BE, Linton KL, De Mets DL. The Beaver Dam Eye Study: visual acuity. Ophthalmology. 1991;98:1310–1315. doi: 10.1016/s0161-6420(91)32137-7. [DOI] [PubMed] [Google Scholar]
- 12.Livingston PM, Lee SE, McCarty CA, Taylor HR. A comparison of participants with non-participants in a population-based epidemiological study: the Melbourne Visual Impairment Project. Ophthalmic Epidemiol. 1997;4:73–81. doi: 10.3109/09286589709057099. [DOI] [PubMed] [Google Scholar]
- 13.Valbuena M, Bandeen-Roche K, Rubin GS, Munoz B, West SK. Self-reported assessment of visual function in a population-based study: the SEE project. Salisbury Eye Evaluation. Invest Ophthalmol Vis Sci. 1999;40(2):280–8. [PubMed] [Google Scholar]
- 14.Rubin GS, Bandeen–Roche K, Huang G, Muñoz B, Schein OD, Fried LP, West SK. The Association of Multiple Visual Impairments with Self-Reported Visual Disability: SEE Project. Investigative Ophthalmology and Visual Science. 2001;42:64–72. [PubMed] [Google Scholar]
- 15.Owen CG, Rudnicka AR, Smeeth L, Evans JR, Wormald RP, Fletcher AE. Is the NEI-VFQ-25 a useful tool in identifying visual impairment in an elderly population? BMC Ophthalmol. 2006 Jun 9;6(1):24. doi: 10.1186/1471-2415-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salive ME, Guralnik J, Glynn RJ, et al. Association of visual impairment with mobility and physical function. J Am Geriatr Soc. 1994;42:287–292. doi: 10.1111/j.1532-5415.1994.tb01753.x. [DOI] [PubMed] [Google Scholar]
- 17.Branch LG, Horowitz A, Carr C. The implications for everyday life of incident self-reported visual decline among people over age 65 living in the community. Gerontologist. 1989;29:359–365. doi: 10.1093/geront/29.3.359. [DOI] [PubMed] [Google Scholar]
- 18.Chia E, Wang JJ, Rochtchina E, Smith W, Cumming RR, Mitchell P. Impact of bilateral visual impairment on health-related quality of life: the Blue Mountains Eye study. Invest Ophthalmol and Vis Sci. 2004;45:71–76. doi: 10.1167/iovs.03-0661. [DOI] [PubMed] [Google Scholar]
- 19.Patel I, Munoz B, Burke AG, Kayongoya A, Mchiwa W, Schwarzwalder AW, West SK. Impact of Presbyopia on Quality of Life in a Rural African Setting. Ophthalmol. 2006;113(5):728–734. doi: 10.1016/j.ophtha.2006.01.028. [DOI] [PubMed] [Google Scholar]
- 20.Frick KD, Melia BM, Buhrmann RR, West SK. Trichiasis and disability in a trachoma endemic area of Tanzania. Arch Ophthalmol. 2001;119:1839–1844. doi: 10.1001/archopht.119.12.1839. [DOI] [PubMed] [Google Scholar]
- 21.Kish L. Survey Sampling. John Wiley & Sons; New York: 1995. [Google Scholar]
- 22.Ustun TB, Chatterji S, Mechbal A, Murray CJL, WHS Collaborating Groups . The World Health Surveys. In: Murray CJL, Evans DB, editors. Health Systems Performance Assessment: Debates, Methods and Empiricism. World Health Organization; Geneva: 2003. [Google Scholar]
- 23.Gureje O, Ogunniyi A, Kola L, Afolabi E. Functional disability in elderly Nigerians: results from the Ibadan Study of Aging. J Am Geriatr Soc. 2006 doi: 10.1111/j.1532-5415.2006.00944.x. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.StataCorp . Stata Statistical Software, version 7.0 for Windows. Stata, College Station; Texas: 2001. [Google Scholar]
- 25.Hosmer DW, Lemeshow S. Applied Logistic Regression. Second Edition John Wiley & Sons; New York: 2000. [Google Scholar]
- 26.West S, Munoz B, Rubin GS, Schein OD, Bandeen-Roche K, Zeger S, German S, Fried LP, The SEE project Function and visual impairment in a population-based study of older adults. Invest Ophthalmol Vis Sci. 1997;38(1):72–82. Salisbury Eye Evaluation. [PubMed] [Google Scholar]
- 27.Massof RW, Rubin GS. Visual function assessment questionnaires. Surv Ophthalmol. 2001;45(6):531–48. doi: 10.1016/s0039-6257(01)00194-1. [DOI] [PubMed] [Google Scholar]
- 28.Nirmalan PK, Thulasiraj RD, Meneksha V, Rahmanthullah R, Ramakrishnan R, Padmavathi A, et al. A population based eye survey of older adults in Tirunelveli district of south India; blindness, cataract surgery and visual outcomes. Br J of Ophthalmol. 2002;86:505–12. doi: 10.1136/bjo.86.5.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Broman AT, Munoz B, Rodriguez J, Sanchez R, Quigley HA, Klein R, et al. The Impact of Visual Impairment and Eye Disease on Vision-Related Quality of Life in a Mexican-American Population: Proyecto VER. Invest Ophthalmol and Vis Sci. 2002;43:3393–3398. [PubMed] [Google Scholar]
- 30.Knudtson MD, Klein BE, Klein R, Cruickshanks KJ, Lee KE. Age related eye disease, quality of life and functional activity. Arch Ophtalmol. 2005;123(6):807–14. doi: 10.1001/archopht.123.6.807. [DOI] [PubMed] [Google Scholar]
- 31.West SK, Rubin GS, Broman AT, Muñoz B, Bandeen-Roche K, Turano K, The SEE Project How Does Visual Impairment Affect Performance on Tasks of Everyday Life? Arch Ophthalmol. 2002;120:774–780. doi: 10.1001/archopht.120.6.774. [DOI] [PubMed] [Google Scholar]
- 32.Rubin GS, Roche KB, Prasada-Rao P, Fried LP. Visual impairment and disability in older adults. Optom Vis Sci. 1994;71(12):750–60. doi: 10.1097/00006324-199412000-00005. [DOI] [PubMed] [Google Scholar]