How did the study come about?
The North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD) was created as part of the International Epidemiologic Databases to Evaluate AIDS (IeDEA) initiative. The IeDEA project establishes regional centres for the collection and harmonization of data and the establishment of an international research consortium to address unique and evolving HIV/AIDS research questions requiring the larger sample sizes that can be achieved by combining multiple cohorts. The IeDEA initiative provides a means to implement methodology to effectively pool collected data, thus providing a cost-effective way to generate large data sets to address high-priority research questions in a timely manner. It is frequently difficult to combine data collected under different protocols, and may not be as efficient as collecting predetermined and standardized data elements under a single protocol. By developing a proactive mechanism for the collection of key variables, the IeDEA initiative is designed to enhance the quality, cost-effectiveness and speed of observational cohort studies pertaining to HIV/AIDS.
The NA-ACCORD is a regional collaboration of single-site and multi-site cohorts that includes over 90 000 patients from more than 50 sites throughout the United States and Canada. (Cohorts contributing to NA-ACCORD are listed in the Appendix.) The NA-ACCORD is a collaboration of both academic medical centres and community-based facilities that deliver HIV primary and specialty care, combines classical epidemiological and clinical HIV cohorts, includes both HIV-seropositive and seronegative persons, and is complemented by specimen repositories for conducting translational research.
The NA-ACCORD Steering Committee (SC) provides leadership and general oversight. The SC membership includes the Principal Investigator (PI), Co-PI, Data Management Core Director (DMC), Epidemiology/Biostatistics Core Director (EBC), representatives from each of the participating cohorts, the National Institutes of Health (NIH) Program Officer and Working Group Chairs (see Appendix for membership details). The SC assumes responsibility for the conduct of research performed by the group and is responsible for developing the hypotheses/questions addressed by this combined cohort and ensuring that these studies are carried out efficiently and with the highest scientific standards. It reviews and approves concept sheets proposing secondary hypotheses/research questions and ancillary proposals for research from both internal and external investigators. It oversees the preparation of publications and presentations from the research of the NA-ACCORD. Further, the SC oversees operational methods and procedures and reviews performance-monitoring reports. A subset of the SC, the Executive Committee (EC), acts as the executive arm of the NA-ACCORD. It is composed of the PI, Co-PI, Director of the EBC, Director of the DMC and the Project Manager. It makes day-to-day operational decisions on behalf of the SC, and assigns priorities for activities in the study, consistent with the dictates of the SC.
The work of NA-ACCORD is organized into three major Cores (Administrative, Data management and Epidemiology/Biostatistics) that provide an infrastructure for efficiently merging data from existing cohorts, identification of critical scientific questions and conduct of analyses to address our scientific agenda. The Administrative Core (AC) is located at the Johns Hopkins University in Baltimore, Maryland. The AC staff are responsible for the administrative and operational functions of the NA-ACCORD. The Data Management Core, located at the University of Washington, Seattle, provides expertise and experience in informatics that facilitate the merging of data from multiple heterogeneous sources and the ability to include additional sites over time. The NA-ACCORD EBC is based at Johns Hopkins and includes a network of leaders of interval and clinical HIV cohort studies who have developed innovative HIV/AIDS biostatistical and epidemiological methodologies. The EBC plays a central role in supporting the core NA-ACCORD scientific initiatives and methodological development.
A combination of topic-specific working groups and project-specific writing groups provides forums for communication among study investigators. Working groups with periodic conference calls and meetings aid in coordination of different scientific initiatives and identify areas requiring further investigation. Project writing groups are necessarily smaller groups of individuals with focused goals of conducting and writing up specific projects. Both working and writing groups are fluid and depend upon the current scientific initiatives. Working groups provide expert input to the NA-ACCORD SC on specific areas of form and protocol development and may initiate scientific investigations. The following working groups have already been established: (i) an antiretroviral (ARV) therapy effectiveness working group, which oversees initiatives regarding major study outcomes (such as AIDS, death), therapies and natural/treated history; (ii) a toxicities and comorbidities working group, which oversees initiatives and protocols regarding ARV toxicities and co-morbidities projects and (iii) a specimen repository working group, which advises the SC on use of the specimens from the cohorts participating in NA-ACCORD.
The NA-ACCORD is funded by a collaborative agreement by the National Institute of Allergy and Infectious Diseases (NIAID), part of the NIH.
What does it cover and who is in the sample?
The NA-ACCORD is a collaboration of existing North American interval/classical and clinical HIV cohort studies. Figure 1 shows a graphical representation of the location of participating studies, demonstrating the wide geographic representation from the US and Canada. Tables 1 and 2 display characteristics of the cohort studies. Table 1 displays the type of cohort, periods of enrollment and sites of participating studies. Our collaboration includes HIV-infected and HIV-uninfected persons from both academic and community-affiliated facilities and encompasses single-site and multi-site cohorts. Table 2 shows some of the data collection methods from each of the cohorts.
Figure 1.
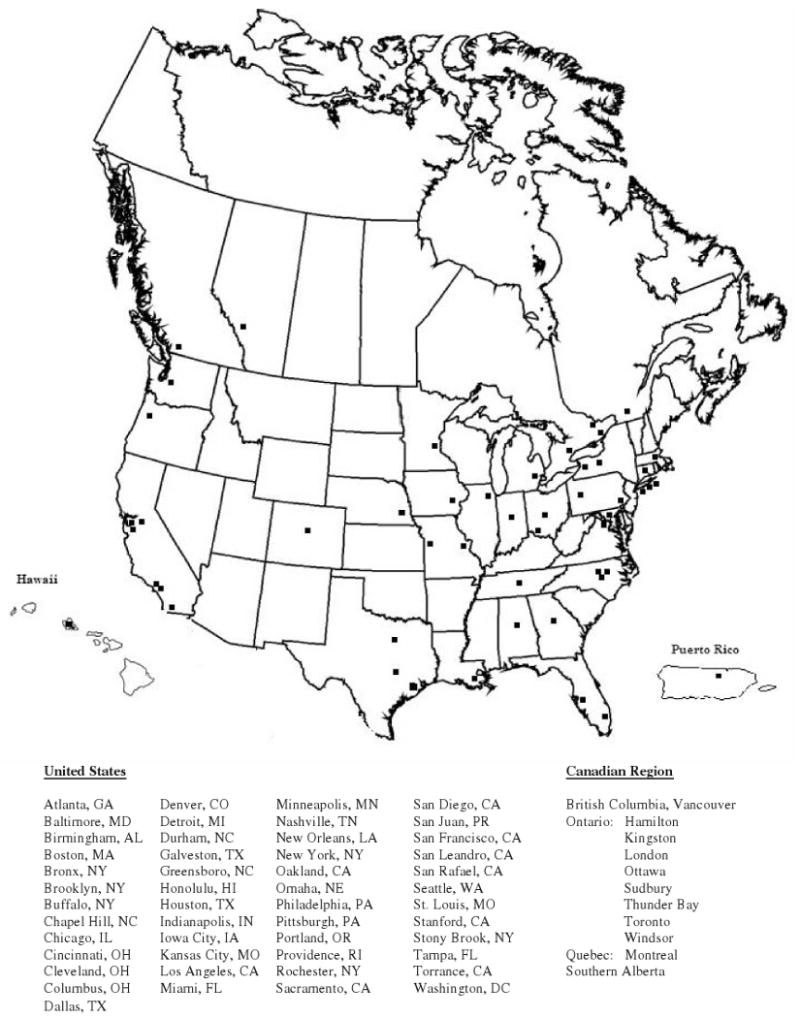
Map of participating sites of the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD)
Table 1.
Cohort characteristics of participating studies of the NA-ACCORD
| Cohort | Cohort type | Enrollment | Sites | Funding* |
|---|---|---|---|---|
| ALIVE | Interval cohort; HIV+ and HIV− | 1988–89;1994–95; 1998; 2000; 2005 | Baltimore, MD | NIH: NIDA |
| ALLRT | Longitudinal study of ACTG enrollees | 2000–ongoing | AACTG sites | NIH: NIAID |
| HIVRN | Clinic-based | 2000–ongoing | 12 sites: NYC (2); Detroit, MI (2); San Diego, CA; Oakland, CA; Portland, OR; Dallas, TX; Kansas City, MO Tampa, FL; Rochester, NY; Philadelphia, PA | AHRQ, HRSA, SAMHSA, NIH |
| HOMER | Clinic-based | 1996–03 | Vancouver, British Columbia | BC Government, CIHR |
| HOPS | Clinic-based | 1993–ongoing | 10 sites: Chicago, IL (2); Denver, CO (2); Tampa, FL; Washington, DC; Stony Brook, NY; Philadelphia, PA; Oakland, CA; San Leandro, CA | CDC |
| JHHCC | Clinic-based | 1993–ongoing | Baltimore, MD (7) | NIH, AHRQ |
| KPNC | Clinic-based | 1981–ongoing | Northern California | State of California, AHRQ, NIH, Internal |
| MACS | Interval cohort; HIV+ and HIV− | 1984, 1987–91, 2001–03 | 4 sites: Baltimore, MD/Washington, DC; Chicago, IL; Pittsburgh, PA; Los Angeles, CA | NIH: NIAID, NCI, NHLBI |
| Montreal | Clinic-based | 1989–ongoing | Montreal, Quebec | UHRESS, FRSQ |
| OHTN | Clinic-based | HOOD: 1995–03; OCS: 2006–ongoing EMR extraction: 2004–ongoing | 8 Ontario sites: Windsor, London, Hamilton, Toronto, Kingston, Ottawa, Sudbury, Thunder Bay | Ontario Ministry of Health and Long Term Care |
| PCRD | Clinic-based | 1995–ongoing | Cleveland, OH | CFAR |
| Polaris | Clinic-based; HIV+ and HIV− | 1998–06 | 8 Ontario sites: Windsor, London, Hamilton, Toronto, Kingston, Ottawa, Sudbury, Thunder Bay | CIHR; Health Canada; OHTN |
| REACH | Population and service based | 1996–ongoing | Tenderloin District of San Francisco, CA | NIH: NIMH, NIDA, Doris Duke, CFAR |
| S. Alberta | Clinic-based | Prospective: 1989–ongoing Retrospective: 1983–89 | Southern Alberta Clinics (4) | Calgary Health Region |
| SCOPE | Clinic-based | 2000–ongoing | San Francisco, CA (2) | NIH, CFAR |
| UAB | Clinic-based | 1995–ongoing | Birmingham, AL | CFAR, CNICS, Mary Fisher CARE Fund |
| UCHCC | Clinic-based | 2000–ongoing | Chapel Hill, NC | NIH; CFAR |
| VACS | Clinic-based | 1999–ongoing | 8 sites: Atlanta, GA; Bronx, NY; Manhattan/Brooklyn, NY; Baltimore, MD; Los Angeles, CA; Pittsburgh, PA; Washington DC, Houston, TX | NIH: NIAAA, VA |
| Vanderbilt | Clinic-based | 1997–ongoing | Nashville, TN | CFAR |
| UW | Clinic-based | 1995–ongoing | Seattle, WA (2) | NIH: NIAID, CFAR, CNICS |
| WIHS | Interval cohort; HIV+ and HIV− | 1994–95; 2001–02 | 6 sites: Bronx/Manhattan, NY; Brooklyn, NY; Los Angeles/S. California/Hawaii; San Francisco, CA; Chicago, IL; Washington, DC. | NIH: NIAID, NCI, NICHD, NIDA |
AHRQ: Agency for Healthcare Research and Quality; CDC: Centers for Disease Control and Prevention; CFAR: Centers for AIDS Research; CIHR: Canadian Institutes of Health Research; CNICS: CFAR Network of Integrated Clinic Systems; FRSQ: Fonds de la recherche en santé du Québec; HAB: HIV/AIDS Bureau; HRSA: Health Resources and Services Administration; NCI: National Cancer Institute; NHLBI: Substance Abuse and Mental Health Services Administration; NIAAA: National Institute on Alcohol Abuse and Alcoholism; NIAID: National Institute of Allergy and Infectious Diseases; NICHD: National Institute of Child Health and Human Development; NIDA: National Institute on Drug Abuse; NIH: National Institutes of Health; NIMH: National Institute of Mental Health; SAMHSA: Substance Abuse and Mental Health Services Administration; UHRESS: Unités hospitalières de recherche, d'enseignement et de soins sur le sida; VA: US Department of Veterans Affairs.
Table 2.
Summary of data collection methods of participating studies of the NA-ACCORD
| Medical records/EMRa | |||||
|---|---|---|---|---|---|
| Cohort | Patient interviews | Prospective | Retrospective | Other | Specimen repository |
| ALIVE | Yes | No | Yes | Linkage—Medicaid, prison, other | Yes |
| ALLRT | Yes | No | Yes | Yes | |
| HIVRN | No | Yes | Yes | Vital stats | No |
| HOMER | Yes | Yes | Yes | Yes | |
| HOPS | No | Yes | Yes | No | |
| JHHCC | ACASI | Yes | Yes | Admin. data, vital stats, outside records | Yes |
| KPNC | No | Yes | Yes | Admin. data | No |
| MACS | Yes | Yes | Yes | Lab; clinical exam | Yes |
| Montreal | Yes | Yes | Yes | Yes | |
| OHTN | Yes | Yes | Yes | Hospital records, vital stats | Yes |
| PCRD | Yes | Yes | Yes | Yes | |
| Polaris | Yes | Yes | Yes | Yes | |
| REACH | Yes | No | Yes | Yes | |
| S. Alberta | Project specific | Yes | Yes | Yes | |
| SCOPE | Yes | No | Yes | Yes | |
| UAB | Yes | Yes | Yes | Yes | |
| UCHCC | Yes | Yes | Yes | Outside records, admin data, vital stats | Yes |
| VACS | Yes | Yes | Yes | Admin data, provider surveys, pharmacy data | Yes |
| Vanderbilt | No | Yes | Yes | Yes | |
| UW | ACASI | Yes | Yes | Admin data, pharmacy data, vital stats | Yes |
| WIHS | Yes | Yes | Yes | Lab, clinical exam | Yes |
EMR: electronic medical records.
Table 3 provides detailed descriptions of participant characteristics for each of the cohorts which comprise NA-ACCORD. The combined sample size exceeds 90 000 individuals (HIV-infected and HIV-uninfected). Demographically, 29% of the combined sample are women, 45% are non-Hispanic white, 46% are African-American/black and 11% are Hispanic race/ethnicity. HIV-transmission risk groups include 27% intravenous drug users (IDU), 33% men who have sex with men (MSM) and 40% heterosexual or other.
Table 3.
Summary characteristics of participants within the NA-ACCORD studies
| Characteristics | HIV risk category (%) | Race/ethnicity (%) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohort | Inclusion criteria | No Enrolleda (+): HIV+ (-): HIV− | Female (%) | Ageb | MSM | IDU | Hetero | Other/unknown | White | Black | Annual loss to follow-up (%) |
| ALIVE | HIV+ and HIV−, Hx of IDU | (+): 1202 (−): 177 | 26 | 35 | 0 | 100 | 0 | 0 | 10 | 90 | 5 |
| ALLRT | HIV+; ACTG participant | (+): 3331 | 17 | 39 | NA | 10 | NA | 90 | 50 | 28 | 4 |
| HIVRN | HIV+ in care | (+): 12 640 | 30 | 38 | 32 | 35 | 25 | 8 | 30 | 48 | 8 |
| HOMER | HIV+; ARV naïve at enrollment | (+): 2217 | 18 | 39 | NA | 25 | NA | NA | 40 | 2 | 8 |
| HOPS | HIV+ in care | (+): 7800 | 21 | 44 | 61 | 25 | 25 | 5 | 58 | 28 | 10 |
| JHHCC | HIV+ in care | (+): 5800 | 34 | 38 | 22 | 51 | 25 | 2 | 20 | 77 | 6 |
| KPNC | HIV+ Kaiser Permanente health plan members | (+): 17 125 | 11 | 38 | 63 | 7 | 5 | 25 | 62 | 16 | 8 |
| MACS | HIV+ and HIV− men | (+): 3512 (−): 3461 | 0 | 35 | 1 | 9 | 4 | 63 | 24 | 3 | |
| Montreal | HIV+ | (+): 2456 | 20 | 39 | 42 | 12 | 8 | 70 | 11 | 11 | |
| OHTN | HIV+ | (+): 4246 | 11 | 41 | 72 | 9 | 15 | 5 | 78 | 6 | 4 |
| PCRD | HIV+ in care | (+): 1401 | 20 | 37 | 47 | 3 | 33 | 16 | 40 | 51 | 8 |
| Polaris | HIV+ and HIV− | (+): 291 (−): 168 | 7 | 36 | 80 | 6 | 9 | 0 | 82 | 1 | 3 |
| REACH | HIV testing at SRO hotel, homeless shelter or free meal program | (+): 753 | 17 | 47 | 18 | 45 | 0 | 37 | 36 | 48 | 2 |
| S. Alberta | HIV+, resident of Southern Alberta | (+): 2210 | 12 | 35 | 65 | 24 | 31 | 3 | 75 | 6 | 3 |
| SCOPE | HIV+, ARV naïve | (+): 562 | 14 | 44 | 76 | 15 | 9 | 0 | 56 | 24 | 18 |
| UAB | HIV+ in care | (+): 3900 | 21 | 38 | 52 | 12 | 41 | 2 | 54 | 42 | |
| UCHCC | HIV+ in care | (+): 1703 | 32 | 37 | 28 | 16 | 42 | 14 | 32 | 61 | 7 |
| UW | HIV+ in care | (+): 2232 | 15 | 37 | 50 | 25 | 16 | 10 | 65 | 20 | 9 |
| VACS | HIV+ and HIV− veterans in VA system | (+): 3052 (−): 3131 | 2 | 49 | 37 | 43 | 24 | 0 | 21 | 70 | 2 |
| Vanderbilt | HIV+ in care | (+): 3760 | 22 | 36 | 50 | 12 | 29 | 9 | 55 | 35 | 4 |
| WIHS | HIV+ and HIV− | (+): 2825 (−): 959 | 100 | 34 | 0 | 26 | 37 | 37 | 21 | 53 | 2 |
As of 2005.
Median age at enrollment.
In addition to data, most of the participating cohorts have specimen repositories. A working group has been established to provide a forum for oversight and coordination of scientific projects utilizing the network repositories, making recommendations for specimen selection and use to the SC, including quality assurance and logistics. Use of these specimens must meet the approval criteria for use by each of the individual cohorts.
How often have they been followed up?
As investigators, we have a deep appreciation for the nature of differences in how data in NA-ACCORD have been and are being collected. It is vital to understand the similarities and differences between the studies in clinical settings (such as the Johns Hopkins HIV Clinical Cohort and University of Alabama – Birmingham 1917 HIV Cohort) and interval cohort studies (such as Multicenter AIDS Cohort Study, Women's Interagency HIV study, AIDS Link to the Intravenous Experience and AIDS Clinical Trials Group Longitudinal Randomized Trials) that have visits scheduled at pre-specified intervals. The data contributed by clinical databases are determined by ongoing patient care and therefore, the type and timing of data collected is determined by the nature of the health care services provided. Interval cohort studies are designed to have regular set intervals between visits (e.g. every 6 months) in which outcomes are assessed systematically regardless of exposure. We are currently working on several methodological projects to address the integration of these different data sources.1
What has been measured? What is the attrition rate?
The goal of the NA-ACCORD collaboration is to integrate data from established HIV cohorts in Canada and the US that have been collecting data on participants for up to 20 years to address research questions regarding HIV treatment and outcomes. The NA-ACCORD approach to data integration takes advantage of known standards regarding the clinical care of HIV patients, including laboratory, treatment and clinical outcomes data. Validity of NA-ACCORD research rests on knowing the content and meaning of data collected by each cohort, making it possible to integrate data that are comparable across cohorts.
The NA-ACCORD does not maintain a centralized database of all data collected by the participating cohorts. Instead, individual scientific questions are proposed and reviewed using a protocol-driven process that scores the proposal based on scientific merit and the availability of data to address those questions within the NA-ACCORD. For meritorious proposals, inclusion criteria, variables and time-lines are constructed for data collection, and these data are abstracted from each of the participating cohorts and transmitted to the DMC.
The specific aims of the NA-ACCORD also serve as the initial scientific questions to be addressed. These aims are:
To determine optimal management strategies to slow disease progression in persons who are highly ARV-experienced and have multi-drug resistant (MDR) HIV.
To determine the optimal timing of contemporary potent ARV therapies to slow disease progression and characterize optimal therapeutic regimens which achieve rapid virological suppression and reduce comorbidities.
The initial variables being collected will allow us to address the first aim. In addition, these variables are useful for HIV clinical epidemiological research in general and will be central in most studies using NA-ACCORD data. The variables being collected include:
Demographic (age, sex, race/ethnicity, HIV-transmission risk factor)
AIDS-defining clinical diagnoses
Medications (ARV)
Laboratory test results (CD4+ T cell count, plasma HIV-1 RNA concentration)
Vital status (death, lost to follow up, currently active)
Viral resistance (genotypic, phenotypic)
The DMC is responsible for integrating data collected by the individual cohorts. All of the participating NA-ACCORD cohorts are protocol-driven and have ongoing collection of demographic, clinical, laboratory and treatment data into an electronic data system. The NA-ACCORD has the challenge of integrating data from two types of cohorts and assuring that the data are comparable across cohorts in meaning and content. These include clinical cohorts of populations of HIV-infected patients in routine care at academic medical centres and community-based facilities that deliver HIV primary and specialty care, whose data are primarily based upon medical records (electronic/paper) as part of patient care, and interval cohorts of populations of HIV-infected and -uninfected patients prospectively enrolled in cohort studies, whose data are derived independently from medical care, although may be confirmed by clinical records.
To accomplish this, we conducted a detailed audit of data types collected by each cohort, working closely with cohort data management personnel to survey how data are collected, verified and captured in the cohort's electronic data system. This allowed us to examine how reliability, validity and completeness of data collection are monitored for the cohort. The approaches for monitoring data quality among NA-ACCORD cohorts included systematic review of clinician progress notes and other existing medical records, event driven audits and verification of random samples of clinical events.
Centralized data mapping was designed to specify how data are integrated into standard NA-ACCORD codes with known and comparable meanings and content. For example, cohorts differ regarding the level of specificity with which diagnoses are captured. Some cohorts use detailed diagnosis categories (e.g. capturing CMV infection diagnoses separately for each organ system such as ‘CMV esophagitis’). Other cohorts combine diagnoses into a more general category (e.g. ‘CMV infection AIDS-defining unspecified’). The NA-ACCORD standard codes were modified to accommodate these idiosyncrasies to produce an exhaustive and mutually exclusive list of labels for the purposes of mapping cohort data within a data type. As a result of this iterative process, we created data dictionaries for each cohort that specify how data are mapped to a series of NA-ACCORD standard labels and document any data quality issues associated with specific data types.
The resultant database is transmitted to the EBC for statistical analyses designed to address the scientific aims of the study.
What has been found? Key findings and publications
Each of the collaborating cohort studies has been the source for many scientific publications. The MACS, for example, has over 900 scientific publications since 1983 (http://www.statepi.jhsph.edu/macs/macs.html). In addition to studies publishing data individually, several of the cohorts have collaborated over the years2–7 and have collaborated in multinational projects.8–10 However, until the establishment of NA-ACCORD, we are aware of only one collaborative publication that combined data across the US and Canada.11
The focus of NA-ACCORD will be on combining data for specific research questions. We have already begun activities related to our year 1 aim, which is to address scientific questions that focus on the failure of highly active antiretroviral therapy (HAART), with a special focus on MDR virus and its consequences and management. Data collection for this aim is underway.
What are the main strengths and weaknesses?
The NA-ACCORD represents a comprehensive North American regional response to the IeDEA request for application (RFA). The following features of the NA-ACCORD make it ideal to represent the North American region within the overall IeDEA.
We broadly represent HIV care across all of North America with over 60 sites in 25 states and the District of Columbia in the US, and four Canadian provinces.
We are highly-representative of the current demographics of HIV infection in North America.
We principally represent clinical observational cohorts where systems for collection, validation and management of data are well-integrated into clinical HIV care. The interval cohort studies are well-established and include individuals with the full spectrum of exposures and risk for death: from HIV-seronegative individuals with low risk, to individuals with AIDS being treated with HAART.
Our core aims are of great importance for contemporary HIV treatment—the optimal management of HIV-infection in the ARV-experienced individual, and in individuals at earlier stages of disease. These aims perfectly leverage our combined sample size, demographic and clinical heterogeneity and our detailed clinical and therapeutic data. The large sample size will also allow us to assess rare events or questions that require highly specific subpopulations. Additionally, our approach to addressing these issues applies novel and cutting-edge biostatistical and epidemiological methods that take into account the complexity of current HIV treatment and the comorbidities that are of increasing frequency in chronic HIV care.
The study provides a forum that links specimen repositories from individual cohorts with a size and heterogeneity to support any number of basic and translational questions in addition to the concepts that were presented.
The investigators of the NA-ACCORD have significant expertise in clinical, epidemiological and biostatistical substantive areas paired with exemplary experience in the leadership of multi-centre AIDS studies. This team is well-positioned to carry-out the proposed scientific agenda, and identify new Aims for the NA-ACCORD that will arise in the future as HIV care evolves.
Because a critical component for the success of the NA-ACCORD collaboration will be the contribution of data from a wide variety of sources, our initiative will be faced with several challenges:
We are dependent on existing studies of HIV-infection for all aspects of data collection. While every NA-ACCORD project will establish criteria for cohort participation, subject inclusion and minimal data requirements, the ultimate responsibility for validity and accuracy of these data resides with the participating study.
No common protocol exists for defining the timing or components of data collection—thus, it will be important to characterize data availability and completeness prior to embarking on new aims. Since many of the collaborating studies are existing clinical cohorts, initiatives that require either explanatory variables (e.g. human genetic polymorphisms) or outcomes (e.g. measures of physical functioning) that are not part of routine clinical care may be infeasible.
Key outcome variables will need to be defined with as much standardization as is feasible across different studies. Complex laboratory tests, such as T-cell subsets, HIV viral load and HIV resistance are routinely used in the clinical management of HIV-infected individuals but may be measured using a variety of techniques and assays. Definitions for clinical outcomes (such as AIDS) need to accommodate heterogeneity in source and level of report, from patient-report to pathology-confirmed diagnoses.
How can I collaborate? Where can I find out more?
To address our scientific agenda, the pooling and harmonizing of high-quality and timely data from established cohorts to create a sufficiently large and up-to-date data set is required. This endeavour will create an understandable tension between the aspirations of investigators involved with individual cohorts and those of the collaborations as a whole. Issues naturally will arise concerning ownership of data, report writing, publication and attribution. Therefore the following principles will guide our scientific agenda.
Ownership of individual cohort data remains with the contributing cohort.
An individual cohort can choose to participate or not in any scientific aim or sub-aim.
All cohorts will have input and one vote in the SC irrespective of contributing data to a specific scientific aim or question.
By agreeing to participate in a scientific project, participants commit themselves to supplying data elements specified by the DMC and EBC in a timely manner.
Data transmitted to the DMC by an individual participating cohort will be used only to address that specific scientific question. The data will not be used for unrelated questions without the express permission of that cohort.
After a scientific question has been addressed (e.g. analysis, generation of final reports and manuscripts), the data for that question will be archived and the SC and individual cohorts would have to approve any additional uses of the original data.
Process for outside collaborators
We encourage collaborators who are not members of NA-ACCORD or partner institutions to be involved in data and/or laboratory analyses. These collaborators will be required to acknowledge the NA-ACCORD. Collaborating scientists will be encouraged to pose relevant scientific questions beyond the data analysis as contracted by the NA-ACCORD; however, these requests for approval for data analysis, presentation or publication must follow the principles outlined in the policies above. Outside investigators should name an NA-ACCORD contact person whose responsibility is to ensure that the lead investigator has had the opportunity to share his/her ideas with the working groups. Proposals will follow the same review process and publication policies as those proposed by internal investigators: development of a concept sheet that is reviewed by the SC.
Process for adding new collaborating cohorts
We welcome the addition of collaborating cohorts to the NA-ACCORD. Three cohorts, in fact, have been added since the original application was approved. Addition of a cohort requires approval of the existing SC. As per the specifications of the IeDEA RFA, only established clinical or interval cohorts will be added. The funding does not support development of new cohorts or the ongoing support of cohorts. Cohorts may comprise HIV-seropositive with or without HIV-seronegative individuals. Addition of cohorts must be approved by the SC after review of the application. Once approved, the cohort will be represented on the SC and have one vote.
An application for new cohorts has been developed and is available on our web-site (http://statepiaps.jhsph.edu/naaccord/).
Acknowledgments
NA-ACCORD is funded by the National Institute of Allergy and Infectious Diseases, National Institutes of Health (U01-AI-069918).
Appendix
NA-ACCORD participating cohorts and steering committee members
AIDS Link to the IntraVenous Experience (ALIVE; Gregory Kirk)
AIDS Clinical Trials Group Longitudinal Linked Randomized Trials (ALLRT; Ronald Bosch)
HIV Research Network (HIVRN; Kelly Gebo)
HAART Observational Medical Evaluation and Research (HOMER; Robert Hogg)
HIV Outpatient Study (HOPS; John T. Brooks)
Johns Hopkins HIV Clinical Cohort (JHHCC; Richard Moore)
Kaiser Permanente Northern California (KPNC; Michael Horberg)
Multicenter AIDS Cohort Study (MACS; Lisa Jacobson)
Montreal Chest Institute Immunodeficiency Service Cohort (Marina Klein)
Ontario HIV Treatment Network Cohort Study (OHTN; Sean Rourke)
John T. Carey Special Immunology Unit Patient Care and Research Database, Case Western Reserve University (PCRD; Benigno Rodriguez)
Polaris HIV Seroconversion Study (Liviana Calzavara)
Research in Access to Care for the Homeless Cohort (REACH; David Bangsberg)
Southern Alberta Clinic Cohort (John Gill)
Study of the Consequences of the Protease Inhibitor Era (SCOPE; Jeffrey Martin)
University of Alabama at Birmingham 1917 Clinic Cohort (Michael Saag)
University of North Carolina at Chapel Hill HIV Clinical Cohort (UCHCC; Joseph Eron)
University of Washington HIV Cohort (Mari Kitahata)
Veterans Aging Cohort Study (VACS; Amy Justice)
Vanderbilt-Meharry CFAR Cohort (Timothy Sterling)
Women's Interagency HIV Study (WIHS; Stephen Gange)
Executive Committee: Richard Moore (PI and Chair), Michael Saag (co-PI), Stephen Gange, Mari Kitahata, Rosemary McKaig.
Administrative Core: Richard Moore, Aimee Freeman, Carol Lent.
Epidemiology/Biostatistics Core: Stephen Gange (Core Director), Ronald Bosch, Stephen Cole, Sarah Holte, Lisa Jacobson, Bryan Lau, Barry Merriman, Gayle Springer.
Data Management Core: Mari Kitahata (Core Director), William Lober, Stephen Van Rompaey, Brenda Simon, Eric Webster, Seth Wolpin.
Working Groups
Specimen Repository Working Group [David Haas (Vanderbilt University), Chair];
ARV Effectiveness Working Group [Steven Deeks (University of California-San Francisco), Chair];
Toxicities and Comorbidities Working Group (John Gill, Chair).
National Institutes of Health Program Officer: Rosemary McKaig
Footnotes
Conflict of interest: None declared.
References
- 1.Lau B, Gange SJ, Moore RD. The Clinical Cohort Study: Epidemiologic Issues. Provisionally accepted for publication, AIDS Research and Human Retrovirology [Google Scholar]
- 2.Rodriguez B, Sethi AK, Cheruvu VK, et al. Predictive value of plasma HIV RNA level on rate of CD4 T-cell decline in untreated HIV infection. JAMA. 2006;296:1498–506. doi: 10.1001/jama.296.12.1498. [DOI] [PubMed] [Google Scholar]
- 3.Anastos K, Gange SJ, Lau B, et al. Association of race and gender with HIV-1 RNA levels and immunologic progression. J Acquir Immune Defic Syndr. 2000;24:218–26. doi: 10.1097/00126334-200007010-00004. [DOI] [PubMed] [Google Scholar]
- 4.Chu H, Gange SJ, Yamashita TE, et al. Individual variation in CD4 cell count trajectory among human immunodeficiency virus-infected men and women on long-term highly active antiretroviral therapy: an application using a Bayesian random change-point model. Am J Epidemiol. 2005;162:787–97. doi: 10.1093/aje/kwi268. [DOI] [PubMed] [Google Scholar]
- 5.Schneider MF, Gange SJ, Williams CM, et al. Patterns of the hazard of death after AIDS through the evolution of antiretroviral therapy: 1984–2004. AIDS. 2005;19:2009–18. doi: 10.1097/01.aids.0000189864.90053.22. [DOI] [PubMed] [Google Scholar]
- 6.Morris J, Mehta S, Jacobson LP, Gange SJ. Injection drug use and patterns of highly active antiretroviral therapy use: an analysis of ALIVE, WIHS, and MACS cohorts. Submitted for publication. doi: 10.1186/1742-6405-4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dean M, Carrington M, Winkler C, et al. Genetic restriction of HIV-1 infection and progression to AIDS by a deletion allele of the CKR5 structural gene. Hemophilia Growth and Development Study, Multicenter AIDS Cohort Study, Multicenter Hemophilia Cohort Study, San Francisco City Cohort, ALIVE Study. Science. 1996;273:1856–62. doi: 10.1126/science.273.5283.1856. [DOI] [PubMed] [Google Scholar]
- 8.Ledergerber B, Lundgren JD, Walker AS, et al. Predictors of trend in CD4-positive T-cell count and mortality among HIV-1-infected individuals with virological failure to all three antiretroviral-drug classes. Lancet. 2004;364:51–62. doi: 10.1016/S0140-6736(04)16589-6. [DOI] [PubMed] [Google Scholar]
- 9.Braitstein P, Brinkhof MW, Dabis F, et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet. 2006;367:817–24. doi: 10.1016/S0140-6736(06)68337-2. [DOI] [PubMed] [Google Scholar]
- 10.May MT, Sterne JA, Costagliola D, et al. HIV treatment response and prognosis in Europe and North America in the first decade of highly active antiretroviral therapy: a collaborative analysis. Lancet. 2006;368:451–8. doi: 10.1016/S0140-6736(06)69152-6. Erratum in:1996;274:1069. [DOI] [PubMed] [Google Scholar]
- 11.Braithwaite RS, Shechter S, Roberts MS, et al. Explaining variability in the relationship between antiretroviral adherence and HIV mutation accumulation. J Antimicrob Chemother. 2006;58:1036–43. doi: 10.1093/jac/dkl386. [DOI] [PubMed] [Google Scholar]


