Abstract
The use of human pluripotent stem cells, including embryonic and induced pluripotent stem cells, in therapeutic applications will require the development of robust, scalable culture technologies for undifferentiated cells. Advances made in large-scale cultures of other mammalian cells will facilitate expansion of undifferentiated human embryonic stem cells (hESCs), but challenges specific to hESCs will also have to be addressed, including development of defined, humanized culture media and substrates, monitoring spontaneous differentiation and heterogeneity in the cultures, and maintaining karyotypic integrity in the cells. This review will describe our current understanding of environmental factors that regulate hESC self-renewal and efforts to provide these cues in various scalable bioreactor culture systems.
Keywords: human embryonic stem cells, culture scaleup, bioreactors
Introduction
The derivation of human pluripotent stem cells, including human embryonic stem cells (hESCs) and human induced pluripotent stem (iPS) cells, has the potential to revolutionize the fields of tissue engineering and regenerative medicine. In the decade since the first successful isolation of hESCs [1], substantial progress has been made in directing differentiation of pluripotent stem cells toward therapeutically-relevant lineages. In order to translate these exciting findings from laboratory scale research to clinical applications, robust culture systems capable of producing clinically-relevant quantities of undifferentiated hESCs and differentiated hESC-derived cells will be needed.
The scalability requirements for human pluripotent stem cell culture will depend on the final incarnation of pluripotent stem cell-derived products. Replacement of ventricular cardiac myocytes killed by a myocardial infarction or treatment of type 1 diabetes mellitus with insulin-secreting islet cells may require approximately 108-109 cells per patient per administration [2], though the number of cells required may vary based on the cell delivery strategy and the survival and functionality of the cells once inside the body. Off-the-shelf products, such as stabilized cells or tissues derived from a banked embryonic stem cell line, would benefit from larger scale culture systems in order to generate a more reproducible product at a lower cost per unit. This review will focus on recent advances in identifying environmental cues that facilitate expansion of undifferentiated pluripotent stem cells and development of methods to apply these cues in a scalable manner.
Self-Renewal Signals for Human Embryonic Stem Cells
Soluble Factors
The initial reported derivations and culture conditions of hESCs utilized mouse embryonic fibroblast (MEF) feeder cells to maintain the blastocyst-derived hESCs in a self-renewing pluripotent state. Numerous other feeder cells, including human fibroblast feeders, fibroblast cell lines, and fibroblasts generated from hESCs, have proven to also support human embryonic stem cell self-renewal. While effective and economical on a laboratory scale, these feeder cocultures and conditioned media systems suffer from lot-to-lot variation in composition and the potential of transmission of xenogenic or infectious agents. Ideally, a scalable culture system would utilize defined, humanized media.
Substantial progress has been made in identifying media components that regulate embryonic stem cell self-renewal and differentiation. Addition of high concentrations of basic fibroblast growth factor (bFGF, FGF2) is sufficient support self-renewal of hESCs in unconditioned medium [3]. bFGF has also been added to medium conditioned by fibroblast feeders and defined media formulations [4-7]. Low stability of bFGF in culture media is one concern regarding the use of this growth factor in scalable embryonic stem cell culture systems. A bFGF engineered to be more stable, or appropriate perfusion of bFGF into the culture system, may reduce the amounts of the protein needed to maintain pluripotency during expansion.
TGFβ superfamily ligands have also been implicated in embryonic stem cell self-renewal and differentiation. Ligands that activate SMAD2/3, including TGFβ1, Activin A, and Nodal, enhance hESC self-renewal while ligands that activate SMAD1/5/8, such as bone morphogenetic proteins (BMPs), induce differentiation [8, 9]. TGFβ signals directly regulate expression of the pluripotency factor Nanog via SMAD binding elements in the Nanog promoter [10, 11]. Thus, addition of TGFβ1, Activin A, or Nodal, or repression of BMPs (e.g. addition of the BMP4 antagonist Noggin), is useful in expanding embryonic cells [4, 12].
Insulin-like growth factors (IGFs) also play a role in maintaining pluripotency. Inhibition of the IGF1 receptor represses hESC self-renewal while addition of an IGF1 analog in conjunction with bFGF and Activin A facilitates expansion of undifferentiated cells [7]. IGF signaling may play a role in feeder-mediated expansion of embryonic stem cells since bFGF stimulates hESC-derived fibroblast feeder cells to secrete IGF, which in turn enhances hESC self-renewal [13].
Wnt ligands also affect embryonic stem cell self-renewal. Addition of Wnt1 to MEF-conditioned media represses spontaneous differentiation [14]. Wnt3a has been reported to induce hESC differentiation [15]. Activation of the canonical Wnt/β-catenin pathway via expression of stabilized β-catenin represses hESC self-renewal [16], while pharmacological activation of the canonical Wnt pathway via a pharmacological inhibitor of glycogen synthase kinase-3 (GSK-3) has been reported to enhance hESC self-renewal.[17]. This apparent discrepancy may be the result of the context or the extent of canonical Wnt signaling. For example, low concentrations of GSK-3 inhibitor induced self-renewal while higher concentrations promoted mesoderm differentiation [16].
Chemical analyses of conditioned and unconditioned media suggest that ligands that activate pluripotency pathways are enriched in conditioned media. Activin A, IGF1, and TGF-β1 appear to be secreted by several feeder cell types, including human fetal, human neonatal, and mouse embryonic fibroblasts [18]. Fully-defined humanized culture media that contain some of these ligands have also been developed and commercialized. Long-term self-renewal of hESCs and human iPS cells has been demonstrated in mTeSR, which contains bFGF, TGFβ1, LiCl, GABA, and pipecolic acid [6]. StemPro, another defined feeder-free medium, contains IGF1, bFGF, Activin A, HRG1β, and other components [7].
While growth and differentiation factors that bind cell surface receptors are important regulators of self-renewal, and thus components of embryonic stem cell culture media, lipid molecules also affect the differentiation state of hESCs. Sphingosine-1-phosphate (S1P) suppresses spontaneous differentiation of hESCs cocultured with MEF feeders [19]. Sphingolipid metabolites, including S1P, were shown to enhance hESC self-renewal, and possibly select for undifferentiated hESCs by promoting apoptosis of certain differentiated cell types [20-22]. Albumin is commonly used as a lipid carrier in culture media. Lipid-rich bovine serum albumin (BSA) was shown to stimulate hESC self-renewal while lipid-poor BSA did not [23]. Synthetic lipid carriers may replace albumin in defined culture media [24].
While a variety of soluble factors have been implicated in promoting self-renewal of hESCs, much is still unknown about how to maintain the pluripotent state. Additionally, it is unclear whether manipulating pluripotency through different pathways yields cells that are biologically identical. Advances in understanding the biology of pluripotency may provide opportunities to standardize and optimize medium composition for controlling hESC self-renewal.
Extracellular Matrix
Human embryonic stem cells are typically cultured directly on feeder cells or on Matrigel, a basement membrane matrix extracted from Engelbreth-Holm-Swarm mouse tumors. These substrates are complex, poorly-defined, and typically xenogenic. Additionally, while Matrigel is effective in propagating feeder-free cultures, another concern with this substrate is significant variability in each lot produced. Matrices derived from other human cells, including mesenchymal stem cells, have been used to expand hESCs [24]. A defined extracellular matrix or biomaterial is needed to complement the defined, humanized culture media for human embryonic stem cell expansion.
Several defined matrices have been reported to be suitable substrates for hESC self-renewal. For example, hESCs have been cultured on human fibronectin in medium containing TGFβ1 and bFGF [5] and on collagen I in a defined medium containing heparin, insulin, transferrin, bFGF, and albumin conjugated with oleic acid [25]. Likewise, hESCs have been cultured on human vitronectin, which binds αvβ5 integrins on the undifferentiated hESC surface [26]. A more complex humanized matrix consisting of collagen IV, vitronectin, laminin, and fibronectin was used to culture hESCs in mTeSR [6]. However, a recent comparative study found that these substrates, along with human or fetal bovine serum coatings, are inferior to Matrigel as culture substrates [27]. A combinatorial study assessed hESC self-renewal on different ECMs in the presence or absence of different growth factors [28]. A combination of collagen I, collagen IV, fibronectin, and laminin was able to support long-term self-renewal in MEF-conditioned medium and the defined medium StemPro [7].
Synthetic matrices would likely offer reproducibility and cost advantages over human-sourced or recombinant protein matrices. hESCs have been cultured for a short time on polymer hydrogels functionalized with cell adhesion peptides [29]. Longer-term culture of hESCs encapsulated in hyaluronic acid (HA)-based hydrogels has been reported [30], but monolayer culture on HA substrates did not maintain the cells in an undifferentiated state, suggesting that the HA requires a specific 3D microenvironment to promote self-renewal. hESCs have also been maintained encapsulated in calcium alginate hydrogels for several months without passaging [31].
Intercellular Interactions
Cell-cell interactions also govern embryonic stem cell self-renewal and differentiation. Individualized cells and small clumps do not grow efficiently while large colonies exhibit substantial levels of spontaneous differentiation. Typically, colonies are maintained at an appropriate size for self-renewal by mechanical or chemical means. Mechanical passaging is too labor intensive for large scale cultures while enzymatic dissociation results in heterogeneous colonies and may contribute to chromosomal instability in some cell lines [32]. Recent work has shown that a Rho-associated kinase (ROCK) inhibitor, Y-27632, can promote survival of singularized hESCs in culture [33]. Development of culture processes incorporating a ROCK inhibitor will allow for the seeding of single cells as opposed to heterogeneous aggregates, improving the uniformity of the system.
Several other technologies for regulating embryonic stem cell colony size and shape have also been developed. Matrigel can be micropatterned onto tissue culture substrates which are then passivated with surfactant to prevent cell attachment to unpatterned regions [34]. Colonies on these surfaces remain confined to the Matrigel-printed regions for several days. Alternatively, hESCs colonies can be expanded in 3D microwells in which the substrate between the wells is treated to repel protein adsorption and cell attachment [35, 36]. In microwells, hESCs can be expanded in the undifferentiated state for several weeks if the microwell size is below a threshold corresponding to approximately 1500 cells [35]. The size effects observed during differentiation may be the result of suppression of Smad1 signaling in larger colonies [37].
The size of a stem cell colony also appears to affect the differentiation trajectory of that colony. EBs generated from larger colonies were biased toward neural lineages, evidenced by increased Pax2 expression, while smaller EBs expressed higher levels of Gata6, an endoderm marker [34]. This suggests that regulation of colony size may be an important parameter to control for specific downstream differentiation applications.
Mechanical Forces
Embryonic stem cells are typically cultured in static conditions, but scalable culture systems often employ perfusion or mixing, which can apply mechanical forces to the cells. Relatively little is known about the effects of these mechanical forces on hESC self-renewal or differentiation. Above a threshold strain, cyclic biaxial strain represses hESC spontaneous differentiation, in part by stimulating expression of TGFβ superfamily ligands [38, 39]. Shear stress induced by fluid flow alters the morphology of undifferentiated hESCs, resulting in elongated, spread cells [40]. The physiologic effects of shear on self-renewal and proliferation remain unclear, however. This information will be important for design of bioreactors to expand embryonic stem cells.
Challenges in Scale-Up of Human Embryonic Stem Cell Culture Systems
Due to the large number of cells necessary for many of the intended applications of hESCs, the development of large-scale culture systems for expansion and differentiation of these cells is critical. Many of the challenges in scaling-up cultures of hESCs are commonly faced in other mammalian culture systems. For example, if the cells are cultured in suspension, aggregation can become a problem, resulting in severely limited diffusion of nutrients, growth factors, metabolic byproducts, and dissolved gases within the aggregates. While high levels of agitation can be used to break up aggregates, this also produces shear forces that can cause apoptosis and physical destruction of the cells [41]. Another potential problem in both adherent and suspension cultures is heterogeneity in the culture environment due to gradients in dissolved oxygen and metabolites resulting from insufficient mixing [42]. Heterogeneity in the system can be particularly harmful in hESC cultures, since it may lead to problems such as spontaneous differentiation to undesired cell types or acquisition of abnormal karyotypes. Thus, it is critical to ensure that the culture is adequately mixed while limiting harmful shear forces experienced by the cells.
In addition to the traditional challenges associated with scale-up of mammalian cell cultures, the expansion and differentiation of embryonic stem cells presents unique obstacles in the development of large-scale culture processes. As discussed earlier, maintenance of hESCs in the self-renewing state, which is necessary for expansion, often requires growth factors and extracellular matrices that are quite costly. While the incorporation of perfusion systems to recycle medium or the development of more stable recombinant forms of necessary growth factors may lower cost by reducing the amount of growth factors needed to sustain the culture, it still may not be economically feasible to use many of these components in large-scale culture system. Another concern in expanding hESCs is the genetic stability of these cells through many divisions. Multiple groups have reported the acquisition of chromosomal abnormalities in hESC lines cultured in vitro [43, 44]. Given that karyotypic mutations in vivo can lead to carcinogenesis, the maintenance of karyotypic stability in large-scale cultures will be critical if the cells are to be used for therapeutic purposes.
Monitoring differentiation status of the cells is also a critical factor in scale-up of hESC cultures. Given that no differentiation process will produce a completely homogeneous population of cells, characterization of the differentiation status of the cells in culture throughout the scale-up process is necessary. A recent study involving implantation of mouse embryonic stem cells into mice showed that only 100-500 cells were necessary to form teratomas outside of the implantation site [45]. Thus, various selection processes may need to be utilized in order to ensure that the final cell population is free of undesired cell types and specifically undifferentiated embryonic stem cells. One approach is to develop genetically modified fluorescent reporter lines for a gene specific to the desired cell type which also contain promoter-driven resistance to an antibiotic, allowing for continuous monitoring of the differentiation process via fluorescence microscopy and purification of the desired cell type through antibiotic selection. Various different strategies for genetic modification of hESCs to produce such reporter lines are reviewed by Guidice and Trounson [46]. In developing culture processes with reporter cell lines, it will be critical to consider the stability of the reporter gene insertion as well as the effect of the genetic medication and selection processes on the properties and function of the final cell population.
Finally, large-scale culture systems involving hESCs must be developed in compliance with good manufacturing practice (GMP) standards if the cells are intended for therapeutic use. Though one aspect of developing GMP-quality processes involves the use of sterile equipment and facilities such as cleanrooms, another major GMP concern regarding the safety of hESCs is that many of the cell lines currently in use were derived or cultured in the presence of animal products. For example, even though mouse embryonic fibroblasts (MEFs) that have traditionally been used as feeder cells have been irradiated to render them nonreplicative, N-glycolylneuraminic acid (Neu5Gc), a non-human sialic acid, has been detected in hESCs cultured on MEFs [47]. While it is possible to develop GMP processes that contain animal substances, ideally the culture media, feeder cells, and extracellular matrices that are used in all steps of the process, from derivation to large-scale expansion, should be free from animal components. Thus, in addition to designing large-scale culture processes in compliance with GMP standards, it may be necessary to derive new cell hESC lines under GMP conditions for future use in clinical-grade processes [48].
Recent success in the development of induced pluripotent stem cell (iPSC) lines [49, 50] holds promise for the development of patient-specific therapies, and thus it may soon become necessary to develop scalable culture processes for iPS cells. Due to the similarities between hESCs and iPSCs, the culture methods developed for hESC self-renewal and differentiation have simply been adapted for iPS cells. However, these may not be the optimal conditions for iPSC culture processes, so it will be critical to study and the basic mechanisms governing the behavior of these cells, as has been done with hESCs over the past decade, in order to develop robust, scaleable culture systems for iPSCs. Additionally, although scale-up of iPSCs will involve many of the same challenges encountered when using hESCs, such as cost, karyotypic stability, and the use of animal components, an additional challenge will be to ensure that the reprogrammed pluripotent state can be fully suppressed following the differentiation process, especially in cells reprogrammed via constitutive activation of pluripotency regulators.
Scalable Culture Systems for Expansion and Differentiation of Human Embryonic Stem Cells
Microfluidic Culture Systems
Although some potential therapeutic applications of human pluripotent stem cells will require high yields of cells that can only be achieved using large-scale culture systems, microfluidic devices may serve as an efficient tool for optimization of culture conditions for growth and differentiation while also providing the precise control over the cell microenvironment that may be necessary for some tissue engineering applications. Arrays of micro-bioreactors have been developed to study growth and differentiation of hESCs in a perfusion system [40, 51]. The soluble factors and concentration gradients in the microenvironment can be controlled by adjusting operating parameters such as the perfusion rate, resulting in a high-throughput system for evaluating the effects of the microenvironment on various cell processes. While constant perfusion can expose the cells to shear stress and remove important factors secreted by the cells, the development of a micro-bioreactor with a periodic “flow-stop” perfusion system for co-culture of hESCs with human foreskin fibroblast (HFF) feeder cells allows for control of the culture environment without subjecting the cells to continuous shear forces [52].
Rotary Cell Culture Systems
On a larger scale than microfluidic devices, rotary cell culture (RCC) systems provide a well-mixed environment for cell growth without generating harsh shear forces that can damage the cells in culture. Developed by NASA, these reactors contain a rotating 3-D chamber in which cells remain suspended in near free-fall, simulating microgravity conditions. In addition to the reduction in shear stress, these culture systems also provide efficient gas transfer through a permeable silicon membrane [53]. Cells can be seeded in this system with or without the addition of microcarriers, allowing for adherent cells to be grown in this environment.
RCC systems have been used for expansion of human embryoid bodies (hEBs), aggregates of differentiating cells formed from hESCs. Since hEBs must be cultured in suspension, aggregation is a major obstacle in developing large-scale culture systems to promote hEB-based differentiation. In a comparison of two types of RCC reactors, the slow turning lateral vessel (STLV) and the high aspect rotating vessel (HARV), the STLV system enhanced the yield of hEBs compared to the traditional static culture, producing small EBs that did not contain necrotic cores. On the other hand, the HARV system resulted in significant aggregation, leading to cell death and large areas if necrosis within the hEBs [54].
The STLV system has been further enhanced through incorporation of a perfusion system with a dialysis chamber, providing continuous removal of waste products and replenishment of nutrients to maintain a more uniform environment in the bioreactor while reducing costs associated with utilizing large volumes of media [55]. In the development of this system, the main goal was to enhance the differentiation process rather than to improve the growth and expansion of hEBs. Accordingly, the results showed that the hEBs formed in the STLV system with perfusion and dialysis underwent more uniform and efficient differentiation towards a neural lineage than hEBs grown in static cultures. While RCC reactors provide uniform, low-shear environments, they are limited in size and thus may not be capable of producing the quantities of cells needed for some applications of hESCs. Scale-up of stirred culture vessels may be more suitable for these applications.
Stirred Culture Vessels
Stirred vessels such as spinner flasks and stirred-tank bioreactors have been widely employed in scale-up of mammalian cells. Accordingly, many efforts toward developing large-scale culture processes for hESCs have focused on these types of reactors. Spinner flasks have been shown to enhance expansion and uniformity of hEBs while maintaining the capacity for differentiation to hematopoietic progenitor cells as compared to static cultures in 6-well plates [56]. Another study, which compared various stirred culture vessels to the STLV RCC system as well as static cultures, found that the hEB cultures in stirred systems exhibited higher rates of cell growth than in the other systems. Additionally, the stirred vessel that promoted the highest growth rates, the Glass Ball Impeller (GBI) spinner flask, also enhanced differentiation of the hEBs toward cardiomyocytes [57].
In addition to enabling large-scale culture of mammalian cells, stirred bioreactors provide an automated, scalable, controlled environment in which to study the effects of different factors on cell growth or differentiation. For example, a study of the effects of various oxygen levels in cultures of micropatterned hEBs grown in spinner flasks showed that the hypoxic conditions promoted cell growth and enhanced expression of early mesodermal and cardiac markers, providing useful insight into a potential mechanism for enhancing cardiac differentiation [58]. While spinner flasks and other stirred bioreactors are well-suited for processes involving hEBs which grow in suspension, expansion of undifferentiated hESCs typically requires adherence to a surface; addition of microcarriers to stirred culture systems allows for scale-up of these adherent cells.
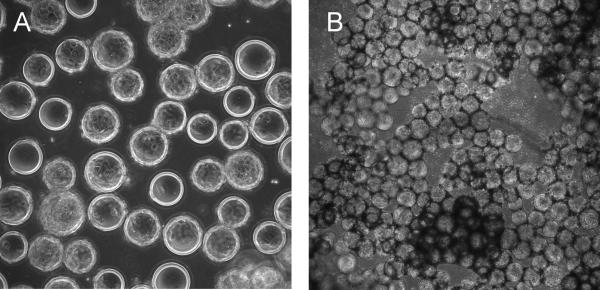
A proof-of-principle study demonstrated that hESCs could be cultured in suspension with MEF-conditioned medium on feeder-free polystyrene microcarriers [59]. Recently, dextran [60] and cellulose-based [61] microcarriers, coated with denatured collagen and Matrigel, respectively, have been shown to promote expansion of hESCs in spinner flasks, generating higher yields of cells than in static 2D cultures. These cells retained the capacity to differentiate into cells from all three germ layers. In addition to MEF-conditioned media, these results were also achieved in two types of defined media, StemPro and mTeSR1 [61]. In addition to the expansion of hESCs, microcarrier-based stirred culture systems have been used in developing processes for directed differentiation of hESCs to definitive endoderm, providing a scalable alternative to hEB-based differentiation methods [62]. Microcarriers have also been incorporated into the process of cryopreservation to improve the recovery of undifferentiated hESCs which were expanded through multiple passages on microcarriers (Figure 2)[63], which is promising given the importance of cryopreservation in the development of large-scale culture systems and the current limitations in the efficiency of available cryopreservation methods.
Figure 2.
Phase contrast images of H9 hESCs cultured in MEF-conditioned media on 300 μm diameter Cytodex 3 microcarriers coated with Matrigel. Images were acquired 1 day (A) and 4 days (B) after seeding. Cells were seeded and cultured as described by [63].
Comparison of Culture Systems
Table 1 summarizes the advantages and disadvantages of each of the culture systems discussed above and includes some basic metrics describing the scalability of the reactors. While microfluidic cell culture devices allow for high-throughput screening of precise aspects of the microenvironment that could prove informative for evaluating various components of stem cell culture processes, these devices themselves are not highly scalable and thus are not likely to be utilized for large-scale cultures. However, mcirofluidic bioreactors may be employed in tissue engineering applications in which detailed microenvironmental control is critical. Though rotary cell culture systems provide efficient gas transfer and low shear environments for hESC growth and differentiation, they are also limited in scalability to a working volume of 5-500mL, and thus may not be suitable for all culture processes involving hESCs. Stirred culture vessels offer the highest degree of scalability, as they can be scaled-up to bioreactor tanks as large as 10,000L, but they also have limitations including high shear stresses on the cells. Ultimately, each clinical application involving will require different bioreactor properties, whether precise control of the microenvironment or efficient scalability for production of large numbers of cells, and thus each bioreactor type will be suitable for different applications of hESCs.
Table 1.
Scalable culture systems for hESC expansion and differentiation
| Bioreactor Type | Working Volume | Max. Reported Yield for hESCs | Advantages | Disadvantages | References |
|---|---|---|---|---|---|
| Microfluidic Systems | 0.1-2mL | 3×104 cells/cm2 | Precise control of microenvironment High-throughput screening of culture conditions | Small scale | 51-52 |
| Rotary Cell Culture Systems | 10-500mL | 36×106 cells/mL | Low-shear environment Efficient gas transfer | Scalability | 54-55 |
| Stirred Culture Systems | 50mL-10,000L | 5×106 cells/mL | Scaleable Well-mixed environment | High-shear environment | 56-63 |
Conclusions
In recent years, there has been tremendous progress in manipulating pluripotency and the differentiation of human pluripotent stem cells. As the field move closer towards therapeutic applications, it will be necessary to address the challenges unique to human pluripotent stem cells in developing large-scale culture systems to realize the potential of these cells. Many of these challenges, including maintenance of pluripotency, acquisition of abnormal karyotypes, inefficiency of differentiation processes, and reliance on animal components, may be overcome as the biological processes governing the behavior of these cells are better understood. The various culture systems discussed in this paper demonstrate the advances that have been made in scaling up the culture of hESCs, laying the foundation for further development of bioreactor systems for human pluripotent stem cell production and differentiation.
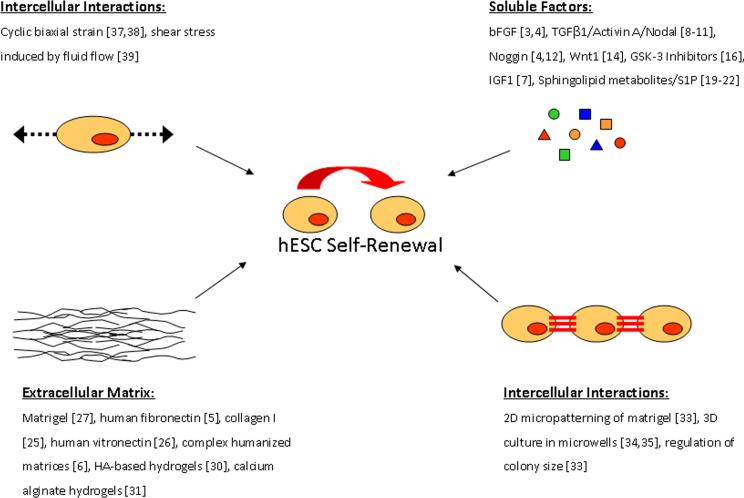
Figure 1.
Environmental factors that regulate hESC self-renewal.
Acknowledgements
The authors thank Dr. Ying Nie for the images shown in Figure 2. Support was provided by a National Science Foundation Graduate Fellowship to SMA, National Science Foundation grant EFRI-0735903, and National Institute of Biomedical Imaging and Bioengineering grant R01EB007534.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Thomson JA, et al. Embryonic stem cell lines derived from human blastocysts. Science. 1998;282(5391):1145–7. doi: 10.1126/science.282.5391.1145. [DOI] [PubMed] [Google Scholar]
- 2.McDevitt TC, Palecek SP. Innovation in the culture and derivation of pluripotent human stem cells. Curr Opin Biotechnol. 2008;19(5):527–33. doi: 10.1016/j.copbio.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Levenstein ME, et al. Basic fibroblast growth factor support of human embryonic stem cell self-renewal. Stem Cells. 2006;24(3):568–74. doi: 10.1634/stemcells.2005-0247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu RH, et al. Basic FGF and suppression of BMP signaling sustain undifferentiated proliferation of human ES cells. Nat Methods. 2005;2(3):185–90. doi: 10.1038/nmeth744. [DOI] [PubMed] [Google Scholar]
- 5.Amit M, et al. Feeder layer- and serum-free culture of human embryonic stem cells. Biol Reprod. 2004;70(3):837–45. doi: 10.1095/biolreprod.103.021147. [DOI] [PubMed] [Google Scholar]
- 6.Ludwig TE, et al. Derivation of human embryonic stem cells in defined conditions. Nat Biotechnol. 2006;24(2):185–7. doi: 10.1038/nbt1177. [DOI] [PubMed] [Google Scholar]
- 7.Wang L, et al. Self-renewal of human embryonic stem cells requires insulin-like growth factor-1 receptor and ERBB2 receptor signaling. Blood. 2007;110(12):4111–9. doi: 10.1182/blood-2007-03-082586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beattie GM, et al. Activin A maintains pluripotency of human embryonic stem cells in the absence of feeder layers. Stem Cells. 2005;23(4):489–95. doi: 10.1634/stemcells.2004-0279. [DOI] [PubMed] [Google Scholar]
- 9.James D, et al. TGFbeta/activin/nodal signaling is necessary for the maintenance of pluripotency in human embryonic stem cells. Development. 2005;132(6):1273–82. doi: 10.1242/dev.01706. [DOI] [PubMed] [Google Scholar]
- 10.Xu RH, et al. NANOG is a direct target of TGFbeta/activin-mediated SMAD signaling in human ESCs. Cell Stem Cell. 2008;3(2):196–206. doi: 10.1016/j.stem.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vallier L, et al. Activin/Nodal signalling maintains pluripotency by controlling Nanog expression. Development. 2009;136(8):1339–49. doi: 10.1242/dev.033951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang G, et al. Noggin and bFGF cooperate to maintain the pluripotency of human embryonic stem cells in the absence of feeder layers. Biochem Biophys Res Commun. 2005;330(3):934–42. doi: 10.1016/j.bbrc.2005.03.058. [DOI] [PubMed] [Google Scholar]
- 13.Bendall SC, et al. IGF and FGF cooperatively establish the regulatory stem cell niche of pluripotent human cells in vitro. Nature. 2007;448(7157):1015–21. doi: 10.1038/nature06027. [DOI] [PubMed] [Google Scholar]
- 14.Villa-Diaz LG, et al. Analysis of the factors that limit the ability of feeder cells to maintain the undifferentiated state of human embryonic stem cells. Stem Cells Dev. 2009;18(4):641–51. doi: 10.1089/scd.2008.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dravid G, et al. Defining the role of Wnt/beta-catenin signaling in the survival, proliferation, and self-renewal of human embryonic stem cells. Stem Cells. 2005;23(10):1489–501. doi: 10.1634/stemcells.2005-0034. [DOI] [PubMed] [Google Scholar]
- 16.Sumi T, et al. Defining early lineage specification of human embryonic stem cells by the orchestrated balance of canonical Wnt/beta-catenin, Activin/Nodal and BMP signaling. Development. 2008;135(17):2969–79. doi: 10.1242/dev.021121. [DOI] [PubMed] [Google Scholar]
- 17.Sato N, et al. Maintenance of pluripotency in human and mouse embryonic stem cells through activation of Wnt signaling by a pharmacological GSK-3-specific inhibitor. Nat Med. 2004;10(1):55–63. doi: 10.1038/nm979. [DOI] [PubMed] [Google Scholar]
- 18.Prowse AB, et al. Identification of potential pluripotency determinants for human embryonic stem cells following proteomic analysis of human and mouse fibroblast conditioned media. J Proteome Res. 2007;6(9):3796–807. doi: 10.1021/pr0702262. [DOI] [PubMed] [Google Scholar]
- 19.Pebay A, et al. Essential roles of sphingosine-1-phosphate and platelet-derived growth factor in the maintenance of human embryonic stem cells. Stem Cells. 2005;23(10):1541–8. doi: 10.1634/stemcells.2004-0338. [DOI] [PubMed] [Google Scholar]
- 20.Inniss K, Moore H. Mediation of apoptosis and proliferation of human embryonic stem cells by sphingosine-1-phosphate. Stem Cells Dev. 2006;15(6):789–96. doi: 10.1089/scd.2006.15.789. [DOI] [PubMed] [Google Scholar]
- 21.Wong RC, et al. Anti-apoptotic effect of sphingosine-1-phosphate and platelet-derived growth factor in human embryonic stem cells. Stem Cells Dev. 2007;16(6):989–1001. doi: 10.1089/scd.2007.0057. [DOI] [PubMed] [Google Scholar]
- 22.Salli U, et al. Propagation of undifferentiated human embryonic stem cells with nano-liposomal ceramide. Stem Cells Dev. 2008 doi: 10.1089/scd.2007.0271. [DOI] [PubMed] [Google Scholar]
- 23.Garcia-Gonzalo FR, Belmonte JC. Albumin-associated lipids regulate human embryonic stem cell self-renewal. PLoS ONE. 2008;3(1):e1384. doi: 10.1371/journal.pone.0001384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Peiffer I, et al. Use of xenofree matrices and molecularly-defined media to control human embryonic stem cell pluripotency: effect of low physiological TGF-beta concentrations. Stem Cells Dev. 2008;17(3):519–33. doi: 10.1089/scd.2007.0279. [DOI] [PubMed] [Google Scholar]
- 25.Furue MK, et al. Heparin promotes the growth of human embryonic stem cells in a defined serum-free medium. Proc Natl Acad Sci U S A. 2008;105(36):13409–14. doi: 10.1073/pnas.0806136105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Braam SR, et al. Recombinant vitronectin is a functionally defined substrate that supports human embryonic stem cell self-renewal via alphavbeta5 integrin. Stem Cells. 2008;26(9):2257–65. doi: 10.1634/stemcells.2008-0291. [DOI] [PubMed] [Google Scholar]
- 27.Hakala H, et al. Comparison of Biomaterials and Extracellular Matrices as a Culture Platform for Multiple, Independently Derived Human Embryonic Stem Cell Lines. Tissue Eng Part A. 2009 doi: 10.1089/ten.tea.2008.0316. [DOI] [PubMed] [Google Scholar]
- 28.Brafman DA, et al. Defining Long-Term Maintenance Conditions of Human Embryonic Stem Cells With Arrayed Cellular Microenvironment Technology. Stem Cells Dev. 2009 doi: 10.1089/scd.2008.0410. [DOI] [PubMed] [Google Scholar]
- 29.Li YJ, et al. Hydrogels as artificial matrices for human embryonic stem cell self-renewal. J Biomed Mater Res A. 2006;79(1):1–5. doi: 10.1002/jbm.a.30732. [DOI] [PubMed] [Google Scholar]
- 30.Gerecht S, et al. Hyaluronic acid hydrogel for controlled self-renewal and differentiation of human embryonic stem cells. Proc Natl Acad Sci U S A. 2007;104(27):11298–303. doi: 10.1073/pnas.0703723104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siti-Ismail N, et al. The benefit of human embryonic stem cell encapsulation for prolonged feeder-free maintenance. Biomaterials. 2008;29(29):3946–52. doi: 10.1016/j.biomaterials.2008.04.027. [DOI] [PubMed] [Google Scholar]
- 32.Mitalipova MM, et al. Preserving the genetic integrity of human embryonic stem cells. Nat Biotechnol. 2005;23(1):19–20. doi: 10.1038/nbt0105-19. [DOI] [PubMed] [Google Scholar]
- 33.Watanabe K, et al. A ROCK inhibitor permits survival of dissociated human embryonic stem cells. Nat Biotechnol. 2007;25(6):681–6. doi: 10.1038/nbt1310. [DOI] [PubMed] [Google Scholar]
- 34.Bauwens CL, et al. Control of human embryonic stem cell colony and aggregate size heterogeneity influences differentiation trajectories. Stem Cells. 2008;26(9):2300–10. doi: 10.1634/stemcells.2008-0183. [DOI] [PubMed] [Google Scholar]
- 35.Mohr JC, de Pablo JJ, Palecek SP. 3-D microwell culture of human embryonic stem cells. Biomaterials. 2006;27(36):6032–42. doi: 10.1016/j.biomaterials.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 36.Moeller HC, et al. A microwell array system for stem cell culture. Biomaterials. 2008;29(6):752–63. doi: 10.1016/j.biomaterials.2007.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peerani R, et al. Niche-mediated control of human embryonic stem cell self-renewal and differentiation. Embo J. 2007;26(22):4744–55. doi: 10.1038/sj.emboj.7601896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Saha S, et al. TGFbeta/Activin/Nodal pathway in inhibition of human embryonic stem cell differentiation by mechanical strain. Biophys J. 2008;94(10):4123–33. doi: 10.1529/biophysj.107.119891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saha S, et al. Inhibition of human embryonic stem cell differentiation by mechanical strain. J Cell Physiol. 2006;206(1):126–37. doi: 10.1002/jcp.20441. [DOI] [PubMed] [Google Scholar]
- 40.Cimetta E, et al. Micro-bioreactor arrays for controlling cellular environments: design principles for human embryonic stem cell applications. Methods. 2009;47(2):81–9. doi: 10.1016/j.ymeth.2008.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chisti Y. Hydrodynamic damage to animal cells. Crit Rev Biotechnol. 2001;21(2):67–110. doi: 10.1080/20013891081692. [DOI] [PubMed] [Google Scholar]
- 42.Marks DM. Equipment design considerations for large scale cell culture. Cytotechnology. 2003;42(1):21–33. doi: 10.1023/A:1026103405618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Draper JS, et al. Recurrent gain of chromosomes 17q and 12 in cultured human embryonic stem cells. Nat Biotechnol. 2004;22(1):53–4. doi: 10.1038/nbt922. [DOI] [PubMed] [Google Scholar]
- 44.Maitra A, et al. Genomic alterations in cultured human embryonic stem cells. Nat Genet. 2005;37(10):1099–103. doi: 10.1038/ng1631. [DOI] [PubMed] [Google Scholar]
- 45.Cao F, et al. Spatial and temporal kinetics of teratoma formation from murine embryonic stem cell transplantation. Stem Cells Dev. 2007;16(6):883–91. doi: 10.1089/scd.2007.0160. [DOI] [PubMed] [Google Scholar]
- 46.Giudice A, Trounson A. Genetic modification of human embryonic stem cells for derivation of target cells. Cell Stem Cell. 2008;2(5):422–33. doi: 10.1016/j.stem.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 47.Martin MJ, et al. Human embryonic stem cells express an immunogenic nonhuman sialic acid. Nat Med. 2005;11(2):228–32. doi: 10.1038/nm1181. [DOI] [PubMed] [Google Scholar]
- 48.Unger C, et al. Good manufacturing practice and clinical-grade human embryonic stem cell lines. Hum Mol Genet. 2008;17(R1):R48–53. doi: 10.1093/hmg/ddn079. [DOI] [PubMed] [Google Scholar]
- 49.Takahashi K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131(5):861–72. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 50.Yu J, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318(5858):1917–20. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- 51.Figallo E, et al. Micro-bioreactor array for controlling cellular microenvironments. Lab Chip. 2007;7(6):710–9. doi: 10.1039/b700063d. [DOI] [PubMed] [Google Scholar]
- 52.Korin N, et al. Periodic “flow-stop” perfusion microchannel bioreactors for mammalian and human embryonic stem cell long-term culture. Biomed Microdevices. 2009;11(1):87–94. doi: 10.1007/s10544-008-9212-5. [DOI] [PubMed] [Google Scholar]
- 53.Morrison DR. Suspension cell culture in microgravity and development of a space bioreactor. Space Bioreactor Science Workshop.; Johnson Space Center. 1987.pp. 1–18. [Google Scholar]
- 54.Gerecht-Nir S, Cohen S, Itskovitz-Eldor J. Bioreactor cultivation enhances the efficiency of human embryoid body (hEB) formation and differentiation. Biotechnol Bioeng. 2004;86(5):493–502. doi: 10.1002/bit.20045. [DOI] [PubMed] [Google Scholar]
- 55.Come J, et al. Improvement of culture conditions of human embryoid bodies using a controlled perfused and dialyzed bioreactor system. Tissue Eng Part C Methods. 2008;14(4):289–98. doi: 10.1089/ten.tec.2008.0029. [DOI] [PubMed] [Google Scholar]
- 56.Cameron CM, Hu WS, Kaufman DS. Improved development of human embryonic stem cell-derived embryoid bodies by stirred vessel cultivation. Biotechnol Bioeng. 2006;94(5):938–48. doi: 10.1002/bit.20919. [DOI] [PubMed] [Google Scholar]
- 57.Yirme G, et al. Establishing a dynamic process for the formation, propagation, and differentiation of human embryoid bodies. Stem Cells Dev. 2008;17(6):1227–41. doi: 10.1089/scd.2007.0272. [DOI] [PubMed] [Google Scholar]
- 58.Niebruegge S, et al. Generation of human embryonic stem cell-derived mesoderm and cardiac cells using size-specified aggregates in an oxygen-controlled bioreactor. Biotechnol Bioeng. 2009;102(2):493–507. doi: 10.1002/bit.22065. [DOI] [PubMed] [Google Scholar]
- 59.Phillips BW, et al. Attachment and growth of human embryonic stem cells on microcarriers. J Biotechnol. 2008;138(12):24–32. doi: 10.1016/j.jbiotec.2008.07.1997. [DOI] [PubMed] [Google Scholar]
- 60.Fernandes AM, et al. Successful scale-up of human embryonic stem cell production in a stirred microcarrier culture system. Braz J Med Biol Res. 2009;42(6):515–22. doi: 10.1590/s0100-879x2009000600007. [DOI] [PubMed] [Google Scholar]
- 61.Oh SK, et al. Long-term microcarrier suspension cultures of human embryonic stem cells. Stem Cell Res. 2009 doi: 10.1016/j.scr.2009.02.005. [DOI] [PubMed] [Google Scholar]
- 62.Lock LT, Tzanakakis ES. Expansion and Differentiation of Human Embryonic Stem Cells to Endoderm Progeny in a Microcarrier Stirred-Suspension Culture. Tissue Eng Part A. 2009 doi: 10.1089/ten.tea.2008.0455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Nie Y, et al. Scalable culture and cryopreservation of human embryonic stem cells on microcarriers. Biotechnol Prog. 2009;25(1):20–31. doi: 10.1002/btpr.110. [DOI] [PMC free article] [PubMed] [Google Scholar]