Summary
Pharyngocutaneous fistula is the most common non-fatal complication following total laryngectomy. To start oral feeding and exclude the presence of a pharyngocutaneous fistula, a subjective test and instrumental assessments using videofluoroscopy, have been described. The aim of this study was to evaluate the effectiveness of oral-pharyngo-oesophageal scintigraphy as an objective and non-invasive tool to establish presence, site and dimensions of the fistula. Observations were performed on 3 male patients, mean age 65 years, who underwent total laryngectomy and mono or bilateral neck dissection after failure of radiotherapy in 2 cases and of conservative laryngeal surgery in the third case, complicated by post-operative pharyngocutaneous fistula. Oral-pharyngo-oesophageal scintigraphy dynamic study with sequential images were obtained during the swallowing phases. In case 1, the test showed a wide pharyngocutaneous fistula the internal orifice of which was at the level of the base of the tongue: on the scintigraphic images, the radiomarked water bolus, from the fistulous orifice, descended along the stoma walls and only a small part reached the oesophagus. In the other two patients, the pharyngocutaneous fistula was small and the internal fistulous orifice was detected in the lower part of T-suture line. In conclusion, scintigraphy offered the possibility to precisely identify presence of pharyngocutaneous fistula and location of its internal orifice and to monitor its spontaneous closure. Therefore, important information could be obtained regarding the suture line status and the possibility of deciding whether to remove the nasogastric tube or to leave it in place. Finally, these data showed that oral-pharyngo-oesophageal scintigraphy could be performed in the early post-operative period to optimize starting safe oral feeding.
Keywords: Total laryngectomy, Complications, Fistula, Scintigraphy
Riassunto
La fistola faringo-cutanea rappresenta la complicanza più frequente dopo laringectomia totale. Lo studio della deglutizione prima della ripresa dell’alimentazione orale si avvale a tutt’oggi di test soggettivi ed accertamenti strumentali mediante videofluoroscopia. Lo scopo di questo studio è stato quello di valutare l’efficacia della scintigrafia oro-faringo-esofagea (OPES, Oral-Pharyngo-Oesophageal Scintigraphy) quale metodica oggettiva e non invasiva per stabilire presenza, sede e dimensione della fistola. Abbiamo osservato 3 pazienti (sesso maschile, età media 65 anni) sottoposti a radioterapia esclusiva in 2 casi e pregressa chirurgia conservativa laringea in un terzo caso e successiva laringectomia totale e svuotamento laterocervicale mono- o bilaterale di salvataggio, con insorgenza post-operatoria di fistola faringo-cutanea. In tali pazienti abbiamo effettuato uno studio scintigrafico dinamico con immagini sequenziali ottenute nelle varie fasi della deglutizione. Nel caso 1 l’esame ha evidenziato un’ampia fistola faringo-cutanea il cui orifizio interno era localizzato a livello della base-lingua: nelle immagini scintigrafiche il bolo radiomarcato fuoriusciva dal tramite fistoloso distribuendosi lungo la regione peristomale raggiungendo l’esofago in minima percentuale. Negli altri 2 pazienti la fistola faringo-cutanea era di piccole dimensioni e l’orifizio interno della fistola è stato rilevato a livello della porzione inferiore della sutura a “T”. In conclusione, la scintigrafia oro-faringo-esofagea ha consentito di identificare la presenza della fistola faringo-cutanea, di localizzarne con precisione il suo orifizio interno e di monitorare la sua chiusura spontanea. Con questa metodica si possono inoltre ottenere informazioni importanti sullo stato della linea di sutura ipofaringo-esofagea al fine di decidere se rimuovere o meno il sondino naso-gastrico. Infine, la precocità di esecuzione della scintigrafia oro-faringo-esofagea nell’immediato post-operatorio potrebbe ottimizzare la ripresa in sicurezza dell’alimentazione orale.
Introduction
Recovery of oral feeding is a crucial key-point in the post-operative management of laryngectomized patients. Pharyngocutaneous fistula (PCF), in particular, is the most common non-fatal complication following total laryngectomy and can occur in the immediate post-operative phase (< 30 days after surgery) or rarely, later 1 2.
It creates a communication between the pharynx and cervical skin around the surgical incision or, less frequently, the stoma of the tracheostomy. Pharyngeal contents, usually saliva, flow through the fistula emerging from the cutaneous orifice 3. To start oral feeding and exclude the presence of a PCF most Authors 4 use a simple subjective test, such as methylene blue dyed water, while others 5 perform a videofluoroscopic evaluation, that has been shown to reveal not only swallowing function (i.e., oral bolus control, presence of pharyngeal residue, aspiration) but also structural changes, such as fistulas.
To our knowledge, no other objective methods offering the possibility to establish presence, site and dimensions of the fistula have been reported so far.
The aim of this study was to evaluate the effectiveness of oral-pharyngo-oesophageal scintigraphy (OPES) as an objective and non-invasive tool to test oral feeding recovery, assess and monitor presence, features and behaviour of PCF following total laryngectomy.
Materials and Methods
From January to June 2007, 3 male patients, mean age 65 years (range 56-72) were observed, who underwent total laryngectomy and mono or bilateral neck dissection after failure of radiotherapy and conservative surgery in cases 1, 3 and 2, respectively, complicated by post-operative onset of PCF. The patients’ features are outlined in Table I. To establish the presence and size of fistulas, the patients were submitted to OPES. In case 1, the test showed a wide PCF the internal orifice of which was at the level of the base of the tongue: on the scintigraphic images, the radioactive water bolus from the fistulous orifice descended along the stoma walls and only a small part reached the oesophagus (Fig. 1). In the other two patients, the PCF was small and the internal fistulous orifice was detected in the lower part of the T-suture line. On the basis of these observations, it was decided to leave the naso-gastric tube (NGT) in place and conservative treatment was applied. When clinical signs of the fistula were no longer visible, a new OPES evaluation was performed that objectively confirmed the closure of the fistulous tract (Fig. 1).
Table I. Patients’ features.
| Case | Sex | Age (years) | Tumour site | Stage of tumour | Previous therapy | Cause of failure | Surgical procedure |
| 1 | M | 68 | Laryngeal carcinoma | T2N0M0 | Radiotherapy | Persistence | Total laryngectomy + right neck dissection |
| 2 | M | 56 | Laryngeal carcinoma | T3N0M0 | Horizontal supraglottic laryngectomy | Recurrence | Total laryngectomy + bilateral neck dissection |
| 3 | M | 72 | Laryngeal carcinoma | T2N0M0 | Radiotherapy | Persistence | Total laryngectomy + bilateral neck dissection |
Fig. 1. OPES dynamic study: the sequential images were obtained during the swallowing phases (from left to right and from top to bottom).
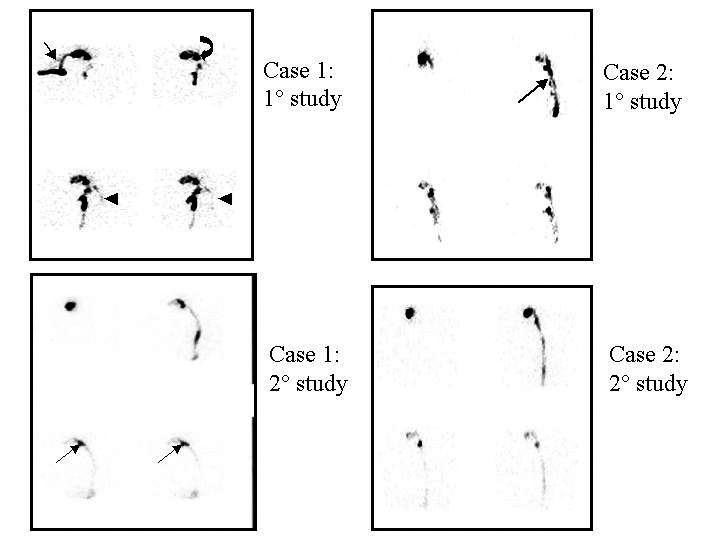
Case 1
Study 1: During bolus administration, using a straw (arrow), deviation of the bolus was observed versus the cutaneous tracheostomy demonstrating the presence of a fistula (“high fistula”) (curved arrow) between the tongue and the tracheostomy. Only a modest quota of the bolus was correctly transported in the oesophagus (head arrows).
Study 2: After 15 days, OPES demonstrated complete closure of the fistula with a regular transport in the oesophagus.
Case 2
Study 1: During transit of the bolus, a slight leakage was observed in front of the anterior wall of the pharynx due to the presence of a fistula (“low fistula”) (arrow).
Study 2: After 7 days, OPES demonstrated closure of the fistula with complete and rapid transport of the bolus in the oesophagus.
Discussion
Following total laryngectomy, most head and neck surgeons tend to withhold oral feeding for 7 to 10 days after surgery, providing adequate nutrition through a naso-gastric feeding tube introduced intra-operatively. This practice is based upon the issue that early start of oral feeding might stress the suture line and result in PCF 6. On the other hand, according to Saydam et al. 2, the start of oral feeding on the first post-operative day should not contribute to fistula formation. Nevertheless, the time after which it is safe to avoid the risk of PCF formation, following total laryngectomy, remains controversial.
In fact, although PCF is a complication that can be managed conservatively without surgical intervention, it still represents a challenge for the head and neck surgeon, prolonging hospitalization, increasing patient morbidity and predisposing also for major neck vessel injury 1 2.
Therefore, it would be worthwhile attempting to find a simple tool, feasible in all laryngectomized patients, to assess oral feeding recovery and to provide objective data on the presence of the fistula and its features.
In clinical practice, before beginning oral feeding, laryngectomized patients make several attempts of feeding, by means of small sips of milk or dyed water (generally with methylene blue) under the physician’s observation; if signs of fistula are observed, the NGT is left in place and conservative treatment is applied 2 7.
Videofluoroscopy is the gold standard radiological technique in swallowing studies. It provides important dynamic criteria to define physiological and anatomical features of swallowing function also after total laryngectomy 5.
OPES is based on the rapid sequential recording of 480 images (at a frame rate of 8/sec) after the administration of 10 ml of water containing 37 MBq of 99mTc-Colloid and the patient is placed in orthostatic position in front of a gamma-camera. As we showed in previous studies 8–11 it is a simple, well-tolerated, non-invasive and low-cost technique with a radiation body burden, within very satisfactory limits of radioprotection (0.011 mSv/MBq), that offers the possibility to study all kinds of dysphagia, in clinical practice, and to monitor the results of swallowing rehabilitation. Furthermore, this technique provides abundant quantitative and qualitative objective information, as it reliably calculates the transit times of various swallowing phases, the amount of tracheo-bronchial aspiration, pharyngeal residue of the radioactive bolus and the presence of a short or long gastro-oesophageal reflux. OPES is performed under physiological conditions: for this reason, compared to videofluoroscopy, dynamic scintigraphy appears to be less invasive and for laryngectomized patients, in particular, it is easier to carry out, as the examination is performed by means of a single water bolus, the features and consistency of which are ideal to start feeding attempts following total laryngectomy.
As far as concerns the PCF in our patients, scintigraphy precisely revealed its presence, the internal orifice site location and offered the possibility to monitor its spontaneous closure. Moreover, the amount of radioactive water bolus collected in the fistulous tract provided indirect information regarding its size.
Conclusions
Our preliminary data show that OPES could be routinely performed in all patients following total laryngectomy, also in the early post-operative period to optimize the onset of safe oral feeding. In fact, this examination offers the possibility to obtain important information regarding the suture line status, before deciding whether to remove the nasogastric tube or leave it in place 12. In the case of PCF, scintigraphy could not only reveal its location and size but also monitor its closure in the case of conservative treatment.
References
- 1.Mäkitie AA, Niemensivu R, Hero M, Keski-Säntti H, Bäck L, Kajanti M, et al. Pharyngocutaneous fistula following total laryngectomy: a single institution’s 10-year experience. Eur Arch Otorhinolaryngol 2006;263:1127-30. [DOI] [PubMed] [Google Scholar]
- 2.Saydam L, Kalcioglu T, Kizilay A. Early oral feeding following total laryngectomy. Am J Otolaryngol 2002;23:277-81. [DOI] [PubMed] [Google Scholar]
- 3.Markou KD, Vlachtsis KC, Nikolaou AC, Petridis DG, Kouloulas AI, Daniilidis IC. Incidence and predisposing factors of pharyngocutaneous fistula formation after total laryngectomy. Is there a relationship with tumor recurrence? Eur Arch Otorhinolaryngol 2004;261:61-7. [DOI] [PubMed] [Google Scholar]
- 4.Makitie AA, Irish J, Gullane PJ. Pharyngocutaneous fistula. Curr Opin Otolaryngol Head Neck Surg 2003;11:78-84 [DOI] [PubMed] [Google Scholar]
- 5.Kreuzer SH, Schima W, Schober E, Pokieser P, Kofler G, Lechner G, et al. Complications after laryngeal surgery: videofluoroscopic evaluation of 120 patients. Clinical Radiology 2000;55:775-81. [DOI] [PubMed] [Google Scholar]
- 6.Seven H, Calis AB, Turgut S. A randomized controlled trial of early oral feeding on laryngectomized patients. Laryngoscope 2003;113:1076-9. [DOI] [PubMed] [Google Scholar]
- 7.Galli J, De Corso E, Volante M, Almadori G, Paludetti G. Postlaryngectomy pharyngocutaneous fistula: incidence, predisposing factors, and therapy. Otolaryngology-Head and Neck Surgery 2005;133:689-94. [DOI] [PubMed] [Google Scholar]
- 8.Galli J, Valenza V, D’Alatri L, Reale F, Gajate AS, Di Girolamo S, et al. Postoperative dysphagia versus neurogenic dysphagia: scintigraphic assessment. Ann Otol Rhinol Laryngol 2003;112:20-8. [DOI] [PubMed] [Google Scholar]
- 9.Galli J, Valenza V, Ottaviani F, D’Alatri L, Almadori G, D’Errico GF, et al. Scintigraphic assessment of swallowing after horizontal supraglottic laryngectomy. J Otolaryngol 1999;28:189-96. [PubMed] [Google Scholar]
- 10.Galli J, Volante M, Parrilla C, Rigante M, Valenza V. Oropharyngoesophageal scintigraphy in the diagnostic algorithm of laryngopharyngeal reflux disease: a useful exam? Otolaryngol Head Neck Surg 2005;132:717-21. [DOI] [PubMed] [Google Scholar]
- 11.Galli J, Valenza V, D’Alatri L, Reale F, Almadori G, Paludetti G. Scintigraphic monitoring of swallowing rehabilitation after horizontal supraglottic laryngectomy. Ann Otol Rhinol Laryngol 2000;109:787-90. [DOI] [PubMed] [Google Scholar]
- 12.Hui Y, Ma KM, Wei WI, Ho WK, Yuen PW, Lam LK, et al. Relationship between the size of neopharynx after laryngectomy and long-term swallowing function: an assessment by scintigraphy. Otolaryngol Head Neck Surg 2001;124:225-9. [DOI] [PubMed] [Google Scholar]


