Summary
Transposition of the temporalis myofascial flap results in permanent aesthetic stigma in the donor site. Reconstruction of this deformity is desirable. The Authors present personal experience in the use of a porous polyethylene prosthesis to camouflage the temporal defects following transposition of the temporalis myofascial flap. From 2002 to 2005, 12 patients (5 male, 7 female, age range 36-84 years, mean 60), following the transposition of the temporalis myofascial flap, underwent reconstruction of the temporal region defect using porous high-density polyethylene temporal implants. The majority of the neoplasms removed proved to be squamous cell carcinomas of the alveolar crest or of the sinusal antrum. The standard surgical technique was used, namely, hemicoronal access and placement of 12 porous high-density polyethylene prostheses (5 left, 7 right). The size of the implants to be used (small, medium, large) was decided during the surgical operation. Of the 12 patients, 2 underwent post-operative radiotherapy, 6 weeks after the implantation of the prosthesis, without adopting any particular precautions to protect the area directly involved in the prosthesis implant. All patients are alive and free from disease, and implant placement appears to be free from post-operative complications. During the period of radiotherapy no complications. directly or indirectly related to the prosthetic implant, arose. Placement of the high-density polyethylene prosthesis fulfilled its filling effect on the deficit with a cosmetic success rate of 90%, as it was well integrated with no evident discontinuity between the edges of the prosthesis and the surrounding tissue or any alteration in the physiological convexity of the treated region. There were no incidents of pain or dysaesthesia of the skin covering the prosthesis. In conclusion, reconstruction of the temporal defect after temporalis myofascial flap transposition with the use of high-density polyethylene implants is an easy and safe method, with excellent functional and aesthetic results.
Keywords: Maxillectomy, Temporalis myofascial flap, High density polyethylene
Riassunto
La trasposizione del lembo miofasciale temporale esita in reliquati estetici a livello della regione donatrice. Gli Autori presentano la loro esperienza di utilizzo di protesi in polietilene poroso nel camouflage dei difetti temporali dopo allestimento di lembo miofasciale temporale. Tra il 2002 e il 2005, 12 pazienti (5 uomini e 7 donne, età compresa tra 36 ed 84 anni, media: 60) sono stati sottoposti, dopo la trasposizione di lembo miofasciale temporale, alla ricostruzione del difetto temporale con impianto di protesi in high-density polyethylene. La maggior parte delle neoplasie trattate sono risultate carcinomi squamocellulari delle creste alveolari o dell’antro sinusale. Le protesi sono state posizionate mediante accesso emicoronale. La dimensione dell’impianto è stata scelta intraoperatoriamente; in tutti i casi è risultato necessario il rimodellamento della protesi, soprattutto la riduzione e l’accorciamento. Tutti gli impianti sono stati immersi preventivamente in una soluzione antibiotica fino al loro posizionamento in situ e successivamente irrorati dalla stessa soluzione prima della loro stabilizzazione. Dei 12 pazienti 2 sono stati sottoposti a cicli di radioterapia postoperatoria a 6 settimane dal posizionamento dell’impianto senza l’adozione di particolari precauzioni a protezione della regione interessata dalla protesizzazione. Il periodo di follow-up di tali pazienti va da 1 anno a 3 anni; tutti i pazienti sono vivi e liberi da malattia, ed in tutti il posizionamento dell’impianto appare esente da complicanze postoperatorie immediate e tardive. Durante tutto il periodo della radioterapia non si sono verificate complicanze collegate con l’impianto protesico. Le protesi in polietilene ad alta densità a livello del deficit hanno assolto il proprio effetto riempitivo con un successo cosmetico del 90% risultando ben integrate, senza dislivelli tra bordo protesico e tessuti circostanti od alterazione della fisiologica convessità della regione trattata. Non si sono verificati casi di dolore o disestesia della cute sovrastante la protesi. In conclusione l’uso di protesi in polietilene ad alta densità per la ricostruzione dei difetti della regione temporale dopo allestimento di lembi di miofasciale temporale appare essere una metodica efficace e sicura scevra da importanti complicanze postoperatorie immediate e tardive con eccellenti risultati sul piano estetico e funzionale.
Introduction
Reconstruction of maxillary defects following removal of malignant tumours from the upper maxilla has evolved significantly over the last 15 years and the techniques most commonly applied today are based on the use of microvascular flaps 1; however, if it is not possible to prepare a microvascular flap, one of the most frequently used reconstructive options is the transposition of the temporalis myofascial flap (TMF) 2. The TMF, quick and easy to prepare, has been used for over a century for covering medium-large congenital, traumatic and oncological defects and its use has been widely documented in the international literature 3–6.
One of the main drawbacks of the transposition of this flap is the permanent residual aesthetic stigma in the temporal region. From the very first applications of the TMF, attempts to achieve craniomaxillofacial reconstruction, such as splitting the temporalis, have been applied aimed at minimizing the negative aesthetic aspects incurred.
The Authors present their experience in using a porous polyethylene prosthesis to camouflage the temporal defects following the transposition of the temporalis muscle.
Materials and methods
Between January 2002 and January 2005, 12 patients (5 male, 7 female, aged between 36-84 years: mean 60), following the transposition of the TMF, underwent reconstruction of the temporal region defect using prefabricated sterile porous high-density polyethylene (HDPE) temporal implants.
The majority of the neoplasms removed proved to be squamous cell carcinomas of the alveolar crest or of the sinusal antrum and the remaining deficits, resulting from maxillectomy, were classified according to the 1997 Spiro index 7.
Reconstruction surgery was carried out at the same time as maxillectomy in all 12 cases.
The standard surgical technique applied was hemicoronal access and placement of the HDPE prostheses (5 left, 7 right) (Figs. 1, 2). The size of the implants to be used (small, medium, large) was decided during the surgical operation.
Fig. 1.
Intra-operative view: temporalis myofascial flap.
Fig. 2.
HDPE prosthesis positioned in temporal defect.
The largest prosthesis was not used in any of the 12 patients as its excessive dimensions made it impossible to disguise its outline and, therefore, it offered poor local-regional cosmetic results.
In our experience, the small size proved suitable for female patients whilst the medium size was more than sufficient for defects in male patients.
Results
The follow-up period for this type of patient varies between a minimum of one to a maximum of three years. To date, all the patients are alive and free from disease, and implant placement appears to be free from post-operative complications, both immediate and later with a 100% success rate.
In all cases, the prosthesis had to be remodelled in order to adapt it to the infra-temporal region, with the most frequent modifications being reduction and shortening of the implant.
All implants were soaked in an antibiotic solution before placement and, once positioned, were sprayed with the same solution before being stabilized and covered by the tailored flap.
Of the 12 patients, 2 underwent post-operative radiotherapy (RT), 6 weeks after implantation of the prosthesis, without adopting any particular precautions to protect the area directly affected by the prosthesis implant. During the period of RT, no complications, directly or indirectly, related to implant of the prosthesis occurred.
The radiological findings of the prosthesis proved to be identical to those of the contralateral temporal musculature. Placement of the HDPE prosthesis has displayed its filling effect on the deficit, with a good cosmetic result, in all our patients, as it was well integrated with no evident discontinuity between the edges of the prosthesis and the surrounding tissue or any alteration in the physiological convexity of the region treated (Figs. 3A, 3B).
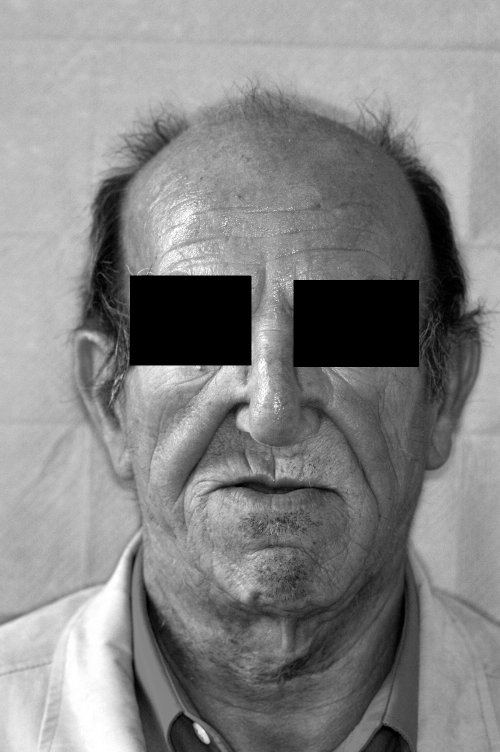
Fig. 3A.
Pre-operative frontal view.
Fig. 3B.
Post-operative frontal view.
There were no cases of pain or dysesthesia of the skin covering the prosthesis; great care and attention were focused on the hemicoronal suture, in order to prevent margin inversion, as well as on post-operative management of the wound.
Discussion
The surgical treatment of tumours located in the middle third of the face presents a reconstruction challenge to the cervicofacial surgeon, in terms of oncological resection and reconstruction of the residual deficit 1 8.
Bone-containing free flaps provide the best solution for maxillary reconstruction needs. Transposition of the temporalis muscle is the method of choice for reconstruction in most cases when preparation of a microsurgical flap is not an option. Unfortunately, however, the loss of volume, in the temporal region, results in profile deformity in this area, characterized by a depression and consequently over-projection of the zygomatic arch and cheek bone which, from an aesthetic point of view, is less than desirable (Fig. 4). The aesthetic deficit, in the temporal region, thus objectively represents a post-operative complication common to every operation of this type.
Fig. 4.
Post-operative frontal view of a patient with temporal defect.
Reconstruction to repair the profile deformity after the preparation of a TMF, should be aimed at overcoming the residual subcutaneous histic deficit by placing an implant to reduce the volume of the defect caused by the transposition of the temporalis, thus restoring facial symmetry 9.
The ideal filling material for this type of defect needs to have specific structural characteristics which favour tissue growth and endoprosthetic vascularization, providing greater adaptability and integration with the skeletal structure with which it comes into contact, and ensuring it maintains its position and three-dimensional compensation effect over time 10.
Over the last 15 years, numerous alloplastic materials have been used to reconstruct the donor site after TMF transposition, amongst which, the most frequently employed has been acrylic bone cement.
Over the last few years, research and industry, in this sector, have made various bio-compatible allogenic implants available, based on different molecular and structural compounds, each of which with its own advantages and disadvantages 11. Bio-materials, on account of their chemo-physical characteristics, have intrinsic properties which are fundamental to the application for which they are used: bio-compatibility with the implant site to reduce the risk of immunologic reaction and rejection, morphologic and volumetric stability of the prosthesis over time, rapid endo-prosthetic vascularization to reduce the risk of infection and, last but not least, easy application and malleability of the material to reduce the risk of it being visible.
With the parallel development of means of osteosynthesis, over the last decade, and titanium stabilizers, possibilities for three-dimensional reconstruction have increased enormously.
Polyethylene has been used since 1947 as a synthetic replacement for deformed or hypoplastic osteocartilaginous parts and the studies of Rubin and Yaremchuk 12 have demonstrated that this material has the ideal characteristics for use in reconstructive surgery for the aesthetic-functional restoration of facial flap donor sites.
Our experience, at present, is limited to a group of 12 patients, in whom we achieved a rapid and satisfactory camouflaging of the temporalis myofascial flap donor site with the use of HDPE prostheses.
The results, at 3-year follow-up, remain stable and symmetry of the temporal region shows no sign of integument depletion or surfacing of the prosthetic material (Figs. 3A, 3B).
In fact, the use of the prosthesis, purely as a filling and camouflaging element and not as a support for soft tissues, minimizes the natural decubitus tendency of the bio-materials.
In conclusion, in our experience, HDPE has proved, thanks to its bio-compatibility, morphologic and volumetric stability over time, rapid vascularization and easy application, to be the most suitable material for the reconstruction and enhancement of bone contours in cranio-facial profile correction in patients who have undergone TMF transposition.
The use of HDPE prostheses in the reconstruction of defects in the temporal region following transposition of a TMF would appear to be a safe and efficacious method, without serious immediate and long-term post-operative complications 13–15; in patients undergoing RT, the medium/short-term results would appear to be the same as those in patients who did not receive this type of treatment, thus confirming the wide range of application for the HDPE prosthesis.
References
- 1.Rogers SN, Lowe D, McNally D. Health-related quality of life after maxillectomy: a comparison between prosthetic obturation and free flap. J Oral Maxillofac Surg 2003;61:174-81. [DOI] [PubMed] [Google Scholar]
- 2.Bradley P, Brockbank J. The temporalis muscle flap in oral reconstruction. J Maxillofac Surg 1981;9:139-45. [DOI] [PubMed] [Google Scholar]
- 3.Shagets FW, Panje WR, Shore JW. Use of temporalis muscle flaps in complicated defects of the head and face. Arch Otolaryngol Head Neck Surg 1986;112:60-5. [DOI] [PubMed] [Google Scholar]
- 4.Koranda FC, McMahon MF, Jernstrom VR. The temporalis muscle flap for intraoral reconstruction. Arch Otolaryngol Head Neck Surg 1987;113:740-3. [DOI] [PubMed] [Google Scholar]
- 5.Habel G, Hensher R. The versatility of temporalis muscle flap in reconstructive surgery. Br J Oral Maxillofac Surg 1986;24:96-101. [DOI] [PubMed] [Google Scholar]
- 6.Colmenero C, Martorell V, Colmenero B. Temporalis myofascial flap for maxillofacial reconstruction. J Oral Maxillofac Surg 1991;49:1067-73. [DOI] [PubMed] [Google Scholar]
- 7.Spiro RH, Strong EW, Shah JP. Maxillectomy and its classification. Head Neck 1997;19:309-14. [DOI] [PubMed] [Google Scholar]
- 8.Brown JS, Rogers SN, McNally DN. A modified classification for the maxillectomy defect. Head Neck 2000;22:17-26. [DOI] [PubMed] [Google Scholar]
- 9.Lacey M, Antonyshyn O. Use of porous high-density polyethylene implants in temporal contour reconstruction. J Craniofac Surg 1993;4:74-8. [DOI] [PubMed] [Google Scholar]
- 10.Costantino PD, Friedman CD, Lane A. Synthetic biomaterials in facial plastic and reconstructive surgery. Fac Plast Surg 1993;9:1-15. [DOI] [PubMed] [Google Scholar]
- 11.Smith JE, Ducic Y, Adelson R. The utility of the temporalis muscle flap for oropharyngeal, base of the tongue and nasopharyngeal reconstruction. Otolaryngol Head Neck Surg 2005;132:373-80. [DOI] [PubMed] [Google Scholar]
- 12.Rubin PJ, Yaremchuk MJ. Complications and toxicities of implantable biomaterials used in facial reconstructive and aesthetic surgery: a comprehensive review of the literature. Plast Reconstr Surg 1997;100:1336-53. [DOI] [PubMed] [Google Scholar]
- 13.Sauer BW. Implants. Technical aspects of porex surgical polyethylene implants. In: Janecka IP, Tiedemann K, editors. Skull base surgery: anatomy, biology and technology. Philadelphia, PA: Lippincott-Raven; 1997. p. 353-67. [Google Scholar]
- 14.Menderes A, Baytekin C, Topcu A. Craniofacial reconstruction with high-density porous polyethylene implants. J Craniofac Surg 2004;15:719-24. [DOI] [PubMed] [Google Scholar]
- 15.Rapidis AD, Day TA. The use of temporal polyethylene implant after temporalis myofascial flap transposition: clinical and radiographic results from its use in 21 patients. J Oral Maxillofac Surg 2006;64:12-22. [DOI] [PubMed] [Google Scholar]