Abstract
Estrogen deficiency has been regarded as the main causative factor in menopausal symptoms and diseases. Here, we show that although estrogen decreases by 90%, a concurrent but inverse change occurs in iron levels during menopausal transition. For example, levels of serum ferritin are increased by two- to threefold from before menopause to after menopause. This observation has led us to hypothesize that, in addition to estrogen deficiency, increased iron as a result of menopause could be a risk factor affecting the health of postmenopausal women. Further studies on iron and menopause are clinically relevant and may provide novel therapeutic treatments. Antioxid. Redox Signal. 11, 2939–2943.
Introduction
In recent years, interest in the improvement of women's health has received great worldwide attention (30). The commitment of the National Institutes of Health (NIH) and its Office of Research on Women's Health exemplifies the effort taken by the U.S. government and highlights the need for surveillance and screening programs that carefully monitor adverse effects in women. The health of girls and women is affected by developmental, physiological, and psychological age. Women's lives are marked by a continuum from intrauterine life to the elderly years: infancy, childhood and adolescence, menarche, reproductive life, the menopausal transition, postmenopausal years, the elderly and frail elderly. Across the life span of a woman, menopause probably has the greatest impact on health (15). Menopause is a natural aging process during which a woman passes from the reproductive to the nonreproductive years. Despite this natural process, many women still experience menopausal symptoms such as vasomotor episodes or “hot flashes,” as well as pathophysiologic conditions such as loss of bone mineral density and thinning and drying of skin (27).
One of the first observable physiological changes for menopause is the cessation of menstrual periods. Because of the reduction in ovarian functions, estrogen deficiency has been the main focus of menopausal research, interventions, and treatments. Yet, results of a meta-analysis of high-quality randomized controlled trials showed that estrogen-only or a combination with progestin hormone-replacement therapy (HRT) reduced hot flashes in 90% of perimenopausal women, but in just 65% of postmenopausal women (15). Moreover, overall bone turnover is significantly increased in peri- and postmenopausal women but in an imbalanced fashion. Bone resorption increases, at 90%, and bone formation increases at only 45%, resulting in a net loss of bone mineral density (11). The exact mechanism through which bone formation after menopause cannot keep up with bone resorption remains unknown. HRT is partially effective in slowing bone loss in postmenopausal women (33). The benefits and drawbacks of HRT remain controversial, and a substantial number of women have discontinued its use because of concerns about side effects (15). Taking into consideration the partial alleviation and potential risk of HRT, we searched risk factors other than estrogen deficiency in menopausal symptoms and diseases.
Concurrent But Inverse Changes in Iron and Estrogen Levels During Menopause
Menstruation is a unique physiological phenomenon in young women, characterized by the periodic high levels of estrogen and the shedding of the endometrium. Because of this monthly blood loss, iron deficiency is prevalent in premenopausal women (46). During perimenopause, fewer eggs exist for the ovaries to stimulate, and menstrual periods become irregular. This period of fluctuation can last up to 10 years. Cessation of menstruation marks the later stage of perimenopause. Because iron is no longer lost through menstruation, it accumulates in the body.
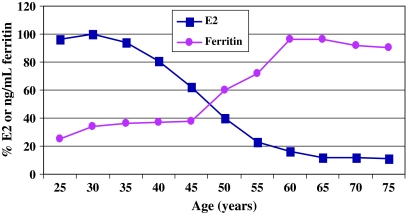
Estrogen and iron are two of the most important growth nutrients in a woman's body development. Estrogen affects the growth, differentiation, and function of tissues such as breasts, skin, and bone (36). Iron is essential for oxygen transport, DNA synthesis, as well as energy production (22). Although estrogen variation over the life span of a woman is considered within normal range, a long duration of exposure to estrogen, including early age at menarche, nulliparity, late first full-time pregnancy, and late menopause, is a well established risk factor for breast cancer (6). Conversely, estrogen deficiency has been considered the major cause of menopausal symptoms and diseases. With the iron data obtained from the Third National Health and Nutrition Examination Survey (NHANES III) (45), Fig. 1 shows that concurrent but inverse changes occur between iron and estrogen levels in healthy women during menopausal transition. Whereas estrogen decreases because of the cessation of ovarian functions, iron increases as a result of decreasing menstrual periods (25, 45). For example, level of serum ferritin is increased by two- to threefold during this period (25). It has been estimated that 1 μg/L serum ferritin corresponds to 120 μg storage iron per kg bodyweight (10). This produces an increase in body iron storage from 4.8 mg/kg bodyweight at the beginning of perimenopause at age 45 years to 12 mg/kg bodyweight after menopause at age 60 years. As shown in Fig. 1, iron deficiency in young women is a relevant health issue that has received great attention from medical professionals. It affects 20% of nonpregnant women aged between 16 and 49 years in industrialized countries and >40% of all women in developing countries (46). Loss of iron in menstrual blood was proposed as a uterine function responsible for the low heart-disease risk of young women (37, 38).
FIG. 1.
Concurrent but inverse changes of ferritin versus estrogen during menopausal transition. Serum levels of 17β-estradiol (E2) were converted to percentage of peak value at 500 pg/ml serum at age 25 years. Levels of ferritin were expressed as nanograms per milliliter serum. E2 data as a function of age were obtained from the website http://www.drlam.com/A3R_brief_in_doc_format/Estrogen Dominance.cfm. Ferritin data were obtained from ref. 45. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article at www.liebertonline.com/ars).
Although increased iron as a result of menopause is considered within normal physiologic range, potential health problems in women, as well as in men or neonates, could be linked to increased iron storage, which is normal but not necessarily healthy (39, 40). For example, a role for iron has been proposed in the pathogenesis of many diseases, such as ischemic heart disease, cancer, diabetes, infections, and neurodegenerative disorders (reviewed in ref. 40). Although healthy levels of iron in human body have not yet been established, it is conceivable that iron imbalance (deficiency or overload) could cause adverse health effects. It has been postulated that iron deficiency in young women plays a role in a high breast cancer recurrence in young patients, and increased iron contributes to a high breast cancer incidence in postmenopausal women (17).
We hypothesize that, in addition to breast cancer and heart disease (17, 38), increased iron could affect other aspects of women's health after menopause. Because the role of iron in menopause has not yet been fully investigated, we used iron studies to show evidence of the role of increased iron in hot flashes, osteoporosis, and skin aging, three common ailments associated with menopause.
Iron and hot flashes
A hot flash indicates the sensation of heat and varies in frequencies among women of different ethnic backgrounds, as well as in durations, recurrence rates, and severities (27). In the Study of Women across the Nation (SWAN), African-American women reported more frequent hot flashes than did white women, who in turn reported more than did Hispanic women (12). Estrogen deficiency plays an important role in this symptom, at least at the beginning of the menopausal transition, as shown by the effectiveness of HRT in 90% of perimenopausal women. Does increased iron contribute to this symptom, particularly in older postmenopausal women in whom HRT is less effective? A literature search found no studies attempting to link iron overload to hot flashes. However, poor temperature regulation leading to cold intolerance has been reported in individuals with iron-deficiency anemia (5). Heat production is impaired by iron deficiency, and heat-loss rate is increased by the demand for tissue oxygenation when decreased blood flow is needed to minimize heat losses to the environment. By examining ferritin data from the NHANES III study (45), we found that serum ferritin levels are parallel with the reported prevalence of hot flashes among African-American, white, and Hispanic women. This observation suggests that, in contrast to iron deficiency leading to cold intolerance, an increase in iron might play a role in postmenopausal hot flashes.
Iron and osteoporosis
Osteoporosis is a common disease characterized by low bone mineral density, resulting in a high incidence of bone fractures, and occurs in ∼50% of women but only in 12% of men older than 50 years (20, 28). By searching for factor(s) other than estrogen deficiency in osteoporosis, we found that both dietary iron deficiency and overload affect bone in animal studies (8, 18, 19, 21, 23, 29). One recent report showed that osteoporosis patients are slightly iron deficient, having lower serum iron and higher transferrin as compared with the control group (7).
However, hemochromatosis patients, who carry a hemochromatosis Fe (HFE) gene mutation and have an iron-overload condition, are at much higher risks of developing osteoporosis (14, 41). Osteopenia with a T score of 1 SD or less and osteoporosis with a T score of 2.5 SD or less were in 78.9% and 34.5% of iron-overload patients, respectively (14), although vitamin D and parathyroid hormone levels appeared normal in these patients. It is interesting to note that osteoporosis is highly prevalent in middle-aged men with HFE gene mutation (14). These results suggest that early occurrence of iron overload in men carries a risk for osteoporosis. A 20-year delay in iron accumulation because of menstrual periods in women who have the same HFE gene mutation may be protective.
Sickle cell disease, an inherited disorder accompanied by anemia and iron overload because of defective hemoglobin, often leads to osteoporosis and osteopenia (2, 35). Analyses of sickle cell disease patients showed that low bone mineral density was significantly associated with lower body mass index, lower hemoglobin, and higher ferritin levels (35). If these studies are correlative, one case report showed that normalization of serum ferritin by frequent phlebotomies increased bone mineral density of the lumbar spine (3). These studies implicate the role of increased iron in the etiology of postmenopausal osteoporosis (42).
Iron and skin aging
During menopausal transition, the skin becomes thin, dry, and wrinkled, which is due to changes in collagen and elastin content, as well as its ability to retain fluids (9). The human body has a limited capacity to remove excess iron; body iron is normally eliminated through the stool, urine, and exfoliation of epidermal cells. About 20% of the 1-mg iron daily from the diet is excreted through the skin (13). In patients with erythrodermic psoriasis, desquamated skin cells account for up to 38% of total body iron loss (34). When body iron storage increases, the skin is exposed to higher levels of iron, which may cause oxidative damage and skin aging during this process. Moreover, the increased stress may make skin more susceptible to UV damage.
It has been shown that without UV exposure, iron overload alone did not induce skin histologic changes in iron-overloaded transgenic HFE−/− mice. This also was true for mice fed a high-iron diet or for mice injected with iron (1). However, human skin fibroblasts were exposed to UVA; the detrimental effects of iron were observed by a significant increase in matrix metalloproteinase-1 (MMP-1) (31). Preincubation with iron chelators reduced UVA-dependent MMP-1 upregulation, suggesting that iron is involved in UVA-mediated collagen degradation (31). Prolonged UVB exposure also resulted in an accumulation of larger amounts of non-heme iron in sun-exposed skin when compared with nonexposed skin, and treatment with iron chelators significantly decreased UVB-induced skin damage (4). These results indicate that increased iron in the skin enhances oxidative stress when exposed to UV and affects downstream genes, which further promote skin photoaging.
Testing the Hypothesis
As compared with estrogen deficiency, increased iron is an unexplored risk factor in menopausal symptoms and diseases associated with menopause. Appropriate rodent animal models mimicking menopausal conditions of estrogen and iron levels are absent. Previous animal studies used a mouse model with surgical induction of menopause by ovariectomy (32). In ovariectomized mice, serum estradiol baseline levels are significantly decreased, simulating one of the major postmenopausal aspects. From our point of view, another important aspect that has not been taken into account in previous animal studies is the significant increase in iron levels after menopause. Therefore, testing the hypothesis in a research laboratory is difficult because it requires the development of a new model simultaneously simulating iron and estrogen changes. Conversely, epidemiologists could first examine whether iron levels are higher in women who experience more frequent hot flashes or hip fractures than in women without. Because both increased iron and decreased estrogen could affect women's health during and after menopause, a study design to examine two variables and one disease outcome is needed. Information gained may be used by clinicians and basic scientists to see whether the cause–effect relation exists between increased iron and menopausal symptoms and diseases.
Conclusions and Open Questions
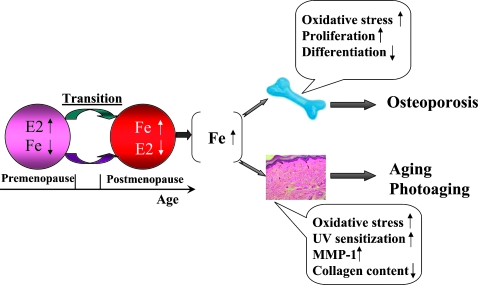
Today, although considerable scientific data are available on the natural biologic and pathologic processes that could affect women's health, substantial gaps in knowledge remain. Efforts have been made to understand the effects of female sex hormones on cellular and organ systems in relation to women's health and disease. As illustrated in Fig. 2, the natural biologic system in young women is high estrogen and low iron. The reverse is true in older women: low estrogen and high iron. Could an increase in iron levels as a result of menopause be a risk factor that affects women's health? Increased iron could lead to oxidative stress and sensitize the skin to UV exposure. Urinary levels of 8-oxo-2'-deoxyguanosine, a marker of oxidative DNA adducts, has been shown to increase with serum ferritin levels in men and women (26). Because iron is a growth nutrient, increased iron could also increase proliferation of osteoblast progenitors without differentiation to mature osteoblasts and thus, slow bone formation.
FIG. 2.
Proposed mechanisms of increased iron as a result of menopause on osteoporosis and skin aging. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article at www.liebertonline.com/ars).
An increase in iron is observed in men during their adolescent years (age 18–30 years) (45), and men do not seem to be immune to the pathologic effects of iron increase (16, 43, 44). The greater incidence of heart disease in men, as well as in postmenopausal women, when compared with the incidence in premenopausal women, has been attributed to higher levels of stored iron in these two groups (38).
Yet important differences exist between men and postmenopausal women in terms of timing and patterns of changes in hormone and iron levels. First, iron increase in men happens in conjunction with the increase of male sex hormones (24, 45), which could provide protection against the harmful effects of the increased iron. Nevertheless, iron increase in women occurs during their midlife (age 42–51 years) at the same time as female sex hormones are decreased. Therefore, the combined effects of increased iron and estrogen deficiency could greatly affect on women's health. Second, it is important to recognize that men and women inherit differently, and thus it is difficult to compare them from the start. Therefore, the observation of increased iron at early age in men accompanied by a lower incidence of osteoporosis should not hinder us from investigating the role of increased iron in menopause. Considering that current menopausal research and treatments focus mainly on ovarian hormones and their receptors, indicting increased iron as a risk factor in menopause-related diseases is more complex, yet more realistic, and worth further investigation.
Abbreviations Used
- HFE
hemochromatosis Fe
- HRT
hormone replacement therapy
- MMP-1
matrix metalloproteinase-1
- NHANES III
Third National Health and Nutrition Examination Survey
Acknowledgments
This work was funded by the National Institutes of Health (NIH CA132684) and in part by NIH grants ES 00260, CA34588, and CA 16087. We thank Daniel Yen from The College of New Jersey for editorial assistance.
References
- 1.Adams BD. Lazova R. Andrews NC. Milstone LM. Iron in skin of mice with three etiologies of systemic iron overload. J Invest Dermatol. 2005;125:1200–1205. doi: 10.1111/j.0022-202X.2005.23949.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adewoye AH. Chen TC. Ma Q. McMahon L. Mathieu J. Malabanan A. Steinberg MH. Holick MF. Sickle cell bone disease: response to vitamin D and calcium. Am J Hematol. 2008;83:271–274. doi: 10.1002/ajh.21085. [DOI] [PubMed] [Google Scholar]
- 3.Angelopoulos NG. Goula AK. Papanikolaou G. Tolis G. Osteoporosis in HFE2 juvenile hemochromatosis: a case report and review of the literature. Osteoporos Int. 2006;17:150–155. doi: 10.1007/s00198-005-1920-6. [DOI] [PubMed] [Google Scholar]
- 4.Bissett DL. Chatterjee R. Hannon DP. Chronic ultraviolet radiation-induced increase in skin iron and the photoprotective effect of topically applied iron chelators. Photochem Photobiol. 1991;54:215–223. doi: 10.1111/j.1751-1097.1991.tb02009.x. [DOI] [PubMed] [Google Scholar]
- 5.Brigham D. Beard J. Iron and thermoregulation: a review. Crit Rev Food Sci Nutr. 1996;36:747–763. doi: 10.1080/10408399609527748. [DOI] [PubMed] [Google Scholar]
- 6.Clemons M. Goss P. Estrogen and the risk of breast cancer. N Engl J Med. 2001;344:276–285. doi: 10.1056/NEJM200101253440407. [DOI] [PubMed] [Google Scholar]
- 7.D'Amelio P. Cristofaro MA. Tamone C. Morra E. Di Bella S. Isaia G. Grimaldi A. Gennero L. Gariboldi A. Ponzetto A. Pescarmona GP. Isaia GC. Role of iron metabolism and oxidative damage in postmenopausal bone loss. Bone. 2008;43:1010–1015. doi: 10.1016/j.bone.2008.08.107. [DOI] [PubMed] [Google Scholar]
- 8.de Vernejoul MC. Pointillart A. Golenzer CC. Morieux C. Bielakoff J. Modrowski D. Miravet L. Effects of iron overload on bone remodeling in pigs. Am J Pathol. 1984;116:377–384. [PMC free article] [PubMed] [Google Scholar]
- 9.Fenske NA. Lober CW. Structural and functional changes of normal aging skin. J Am Acad Dermatol. 1986;15:571–585. doi: 10.1016/s0190-9622(86)70208-9. [DOI] [PubMed] [Google Scholar]
- 10.Finch CA. Bellotti V. Stray S. Lipschitz DA. Cook JD. Pippard MJ. Huebers HA. Plasma ferritin determination as a diagnostic tool. West J Med. 1986;145:657–663. [PMC free article] [PubMed] [Google Scholar]
- 11.Garnero P. Sornay-Rendu E. Chapuy MC. Delmas PD. Increased bone turnover in late postmenopausal women is a major determinant of osteoporosis. J Bone Miner Res. 1996;11:337–349. doi: 10.1002/jbmr.5650110307. [DOI] [PubMed] [Google Scholar]
- 12.Gold EB. Sternfeld B. Kelsey JL. Brown C. Mouton C. Reame N. Salamone L. Stellato R. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40–55 years of age. Am J Epidemiol. 2000;152:463–473. doi: 10.1093/aje/152.5.463. [DOI] [PubMed] [Google Scholar]
- 13.Gruen AB. Zhou J. Morton KA. Milstone LM. Photodegraded nifedipine stimulates uptake and retention of iron in human epidermal keratinocytes. J Invest Dermatol. 2001;116:774–777. doi: 10.1046/j.1523-1747.2001.01318.x. [DOI] [PubMed] [Google Scholar]
- 14.Guggenbuhl P. Deugnier Y. Boisdet JF. Rolland Y. Perdriger A. Pawlotsky Y. Chales G. Bone mineral density in men with genetic hemochromatosis and HFE gene mutation. Osteoporos Int. 2005;16:1809–1814. doi: 10.1007/s00198-005-1934-0. [DOI] [PubMed] [Google Scholar]
- 15.Hickey M. Davis SR. Sturdee DW. Treatment of menopausal symptoms: what shall we do now? Lancet. 2005;366:409–421. doi: 10.1016/S0140-6736(05)66519-1. [DOI] [PubMed] [Google Scholar]
- 16.Hu FB. The iron-heart hypothesis: search for the ironclad evidence. JAMA. 2007;297:639–641. doi: 10.1001/jama.297.6.639. [DOI] [PubMed] [Google Scholar]
- 17.Huang X. Does iron have a role in breast cancer? Lancet Oncol. 2008;9:803–807. doi: 10.1016/S1470-2045(08)70200-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Isomura H. Fujie K. Shibata K. Inoue N. Iizuka T. Takebe G. Takahashi K. Nishihira J. Izumi H. Sakamoto W. Bone metabolism and oxidative stress in postmenopausal rats with iron overload. Toxicology. 2004;197:93–100. doi: 10.1016/j.tox.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 19.Katsumata S. Tsuboi R. Uehara M. Suzuki K. Dietary iron deficiency decreases serum osteocalcin concentration and bone mineral density in rats. Biosci Biotechnol Biochem. 2006;70:2547–2550. doi: 10.1271/bbb.60221. [DOI] [PubMed] [Google Scholar]
- 20.Lane JM. Serota AC. Raphael B. Osteoporosis: differences and similarities in male and female patients. Orthop Clin North Am. 2006;37:601–609. doi: 10.1016/j.ocl.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Liu G. Men P. Kenner GH. Miller SC. Age-associated iron accumulation in bone: implications for postmenopausal osteoporosis and a new target for prevention and treatment by chelation. Biometals. 2006;19:245–251. doi: 10.1007/s10534-005-6666-2. [DOI] [PubMed] [Google Scholar]
- 22.MacKenzie EL. Iwasaki K. Tsuji Y. Intracellular iron transport and storage: from molecular mechanisms to health implications. Antioxid Redox Signal. 2008;10:997–1030. doi: 10.1089/ars.2007.1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Medeiros DM. Plattner A. Jennings D. Stoecker B. Bone morphology, strength and density are compromised in iron-deficient rats and exacerbated by calcium restriction. J Nutr. 2002;132:3135–3141. doi: 10.1093/jn/131.10.3135. [DOI] [PubMed] [Google Scholar]
- 24.Milman N. Serum ferritin in Danes: studies of iron status from infancy to old age, during blood donation and pregnancy. Int J Hematol. 1996;63:103–135. doi: 10.1016/0925-5710(95)00426-2. [DOI] [PubMed] [Google Scholar]
- 25.Milman N. Kirchhoff M. Iron stores in 1359, 30- to 60-year-old Danish women: evaluation by serum ferritin and hemoglobin. Ann Hematol. 1992;64:22–27. doi: 10.1007/BF01811467. [DOI] [PubMed] [Google Scholar]
- 26.Nakano M. Kawanishi Y. Kamohara S. Uchida Y. Shiota M. Inatomi Y. Komori T. Miyazawa K. Gondo K. Yamasawa I. Oxidative DNA damage (8-hydroxydeoxyguanosine) and body iron status: a study on 2507 healthy people. Free Radic Biol Med. 2003;35:826–832. doi: 10.1016/s0891-5849(03)00432-5. [DOI] [PubMed] [Google Scholar]
- 27.Nelson HD. Menopause. Lancet. 2008;371:760–770. doi: 10.1016/S0140-6736(08)60346-3. [DOI] [PubMed] [Google Scholar]
- 28.O'Connor MI. Sex differences in osteoarthritis of the hip and knee. J Am Acad Orthop Surg. 2007;15(suppl 1):S22–S25. [PubMed] [Google Scholar]
- 29.Parelman M. Stoecker B. Baker A. Medeiros D. Iron restriction negatively affects bone in female rats and mineralization of hFOB osteoblast cells. Exp Biol Med (Maywood) 2006;231:378–386. doi: 10.1177/153537020623100403. [DOI] [PubMed] [Google Scholar]
- 30.Pinn VW. A new mosaic for women's health. J Dent Educ. 2004;68:7–14. [PubMed] [Google Scholar]
- 31.Polte T. Tyrrell RM. Involvement of lipid peroxidation and organic peroxides in UVA-induced matrix metalloproteinase-1 expression. Free Radic Biol Med. 2004;36:1566–1574. doi: 10.1016/j.freeradbiomed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 32.Raafat AM. Hofseth LJ. Li S. Bennett JM. Haslam SZ. A mouse model to study the effects of hormone replacement therapy on normal mammary gland during menopause: enhanced proliferative response to estrogen in late postmenopausal mice. Endocrinology. 1999;140:2570–2580. doi: 10.1210/endo.140.6.6634. [DOI] [PubMed] [Google Scholar]
- 33.Ravn P. Bidstrup M. Wasnich RD. Davis JW. McClung MR. Balske A. Coupland C. Sahota O. Kaur A. Daley M. Cizza G. Alendronate and estrogen-progestin in the long-term prevention of bone loss: four-year results from the early postmenopausal intervention cohort study: a randomized, controlled trial. Ann Intern Med. 1999;131:935–942. doi: 10.7326/0003-4819-131-12-199912210-00005. [DOI] [PubMed] [Google Scholar]
- 34.Reizenstein P. Skog E. Stigell P. Radio-iron content of epithelium and cell turnover in psoriasis: iron excretion in man, II. Acta Derm Venereol. 1968;48:70–74. [PubMed] [Google Scholar]
- 35.Sarrai M. Duroseau H. D'Augustine J. Moktan S. Bellevue R. Bone mass density in adults with sickle cell disease. Br J Haematol. 2007;136:666–672. doi: 10.1111/j.1365-2141.2006.06487.x. [DOI] [PubMed] [Google Scholar]
- 36.Simm PJ. Bajpai A. Russo VC. Werther GA. Estrogens and growth. Pediatr Endocrinol Rev. 2008;6:32–41. [PubMed] [Google Scholar]
- 37.Sullivan JL. Are menstruating women protected from heart disease because of, or in spite of, estrogen? relevance to the iron hypothesis. Am Heart J. 2003;145:190–194. doi: 10.1067/mhj.2003.142. [DOI] [PubMed] [Google Scholar]
- 38.Sullivan JL. Iron and the sex difference in heart disease risk. Lancet. 1981;1:1293–1294. doi: 10.1016/s0140-6736(81)92463-6. [DOI] [PubMed] [Google Scholar]
- 39.Sullivan JL. Iron, plasma antioxidants, and the ‘oxygen radical disease of prematurity’. Am J Dis Child. 1988;142:1341–1344. doi: 10.1001/archpedi.1988.02150120095048. [DOI] [PubMed] [Google Scholar]
- 40.Sullivan JL. Is stored iron safe? J Lab Clin Med. 2004;144:280–284. doi: 10.1016/j.lab.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 41.Valenti L. Varenna M. Fracanzani AL. Rossi V. Fargion S. Sinigaglia L. Association between iron overload and osteoporosis in patients with hereditary hemochromatosis. Osteoporos Int. 2009;20:549–555. doi: 10.1007/s00198-008-0701-4. [DOI] [PubMed] [Google Scholar]
- 42.Weinberg ED. Role of iron in osteoporosis. Pediatr Endocrinol Rev. 2008;6(suppl 1):81–85. [PubMed] [Google Scholar]
- 43.Zacharski LR. Chow BK. Howes PS. Shamayeva G. Baron JA. Dalman RL. Malenka DJ. Ozaki CK. Lavori PW. Decreased cancer risk after iron reduction in patients with peripheral arterial disease: results from a randomized trial. J Natl Cancer Inst. 2008;100:996–1002. doi: 10.1093/jnci/djn209. [DOI] [PubMed] [Google Scholar]
- 44.Zacharski LR. Chow BK. Howes PS. Shamayeva G. Baron JA. Dalman RL. Malenka DJ. Ozaki CK. Lavori PW. Reduction of iron stores and cardiovascular outcomes in patients with peripheral arterial disease: a randomized controlled trial. JAMA. 2007;297:603–610. doi: 10.1001/jama.297.6.603. [DOI] [PubMed] [Google Scholar]
- 45.Zacharski LR. Ornstein DL. Woloshin S. Schwartz LM. Association of age, sex, and race with body iron stores in adults: analysis of NHANES III data. Am Heart J. 2000;140:98–104. doi: 10.1067/mhj.2000.106646. [DOI] [PubMed] [Google Scholar]
- 46.Zimmermann MB. Hurrell RF. Nutritional iron deficiency. Lancet. 2007;370:511–520. doi: 10.1016/S0140-6736(07)61235-5. [DOI] [PubMed] [Google Scholar]