Abstract
Previous studies demonstrate that scapulohumeral mechanics improve after subacromial injection. However, it is unclear how injection affects muscle firing. Forty-one subjects with two-tendon rotator cuff tears and 23 volunteer subjects with normal rotator cuffs documented by ultrasonography were examined. Electromyographic activity from 12 muscles was collected during ten functional tasks. Nine symptomatic subjects with rotator cuff tears underwent subacromial injection of anesthetic and underwent repeat electromyographic examination. Subjects with rotator cuff tears demonstrate global electromyographic differences when compared to normal controls. Asymptomatic subjects with rotator cuff tears had significantly increased anterior deltoid firing when compared to symptomatic counterparts during forward shoulder elevation. After subacromial injection, symptomatic subjects demonstrate increased anterior deltoid firing. Previous in vitro and in vivo studies have suggested that pain leads to deltoid inhibition and that subacromial injection leads to improved deltoid firing and, subsequently, improved shoulder function. This study provides direct evidence that subacromial injection improves deltoid firing in symptomatic subjects with rotator cuff tears. These findings reinforce the concept that deltoid inhibition resulting from pain is an important component of the motor disability associated with rotator cuff tears.
Keywords: rotator cuff injuries, intra-articular injection, local anesthetics, electromyography, biomechanics, shoulder joint, muscle, tendon injuries, pain, adult, human
Introduction
It is unclear why some patients with rotator cuff tears feel pain and are functionally weak while other patients are relatively pain-free and able to use the arm effectively. One theory is that symptomatic rotator cuff tears lead to abnormal muscle firing and shoulder function. In subjects with clinically documented subacromial impingement, the infraspinatus, supraspinatus, and middle deltoid demonstrate decreased electromyographic (EMG) activity during certain phases of scaption [10]. In patients with large rotator cuff tears, symptomatic and asymptomatic patients demonstrate different patterns of muscle firing during different tasks [7]. Furthermore, patients with rotator cuff tears demonstrate improvements in scapulohumeral rhythm after subacromial injection [12]. However, no study has examined how anesthetic subacromial injection alters EMG activity in subjects with symptomatic rotator cuff tears.
In addition, previous in vivo and in vitro evidence suggest that there exists a mechanism that utilizes the deltoid to compensate for rotator cuff deficiency [5, 6, 10, 12, 14]. A potential explanation of why symptomatic and asymptomatic subjects differ is that asymptomatic subjects are compensating better with the deltoid because of less pain inhibition. A secondary goal of this study was to evaluate whether electromyographic data can confirm the existence of a compensatory mechanism utilizing the deltoid.
The purpose of this study was to examine EMG firing patterns after anesthetic injection into the subacromial space in subjects with symptomatic rotator cuff tears and to examine differences between symptomatic, asymptomatic, and normal subjects. Three research questions were tested. We wished to document the findings in EMG testing of the rotator cuff musculature in subjects with large rotator cuff tears when compared to healthy controls. In addition, we wished to assess whether asymptomatic subjects with large rotator cuff tears demonstrate any EMG differences when compared to symptomatic subjects with large rotator cuff tears. Finally, we planned to assess how the EMG changes in subjects with large symptomatic rotator cuff tears after analgesic subacromial injection.
Materials and methods
Sixty-four subjects were evaluated including 23 normal control subjects and 41 individuals with two-tendon rotator cuff tears (14 asymptomatic shoulders and 27 symptomatic shoulders). Institutional review board approval was obtained, and informed consent was obtained from all participants. The subjects reported in this study include the original cohort of 18 patients reported in an earlier pilot study [7].
Healthy volunteers were recruited for testing of the normal shoulder group. These subjects had no history of shoulder injury or pain and underwent a screening examination including a complete shoulder examination, plain radiographs of the shoulder (anteroposterior, scapular y view, and axillary), and an ultrasound documenting the absence of rotator cuff pathology. The shoulder ultrasound was performed and interpreted by a single musculoskeletal ultrasonographer with 20 years of experience (R.S.A.) to exclude those individuals with full-thickness rotator cuff tears. A high-frequency linear array transducer was used (Fig. 1).
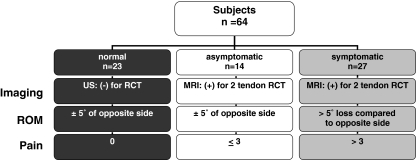
Fig. 1.
Illustration of how subjects were segregated among normal, symptomatic, and asymptomatic groups based on imaging, range of motion, and visual analog scale
Subjects with rotator cuff tears were defined as functionally asymptomatic by history and clinical examination. The 14 functionally asymptomatic subjects were identified as patients who were seen for shoulder pain originally but had resolution of their symptoms after a course of physical therapy and/or subacromial corticosteroid injection. At the time of testing, these subjects had minimal shoulder pain [<3 on the visual analog scale (VAS) which is rated from 0 to 10] and had no activity limitations with active shoulder range of motion within 5° of the opposite side. Magnetic resonance imaging (MRI) of all asymptomatic patients was completed before enrollment in the study to evaluate the size, location, and nature of the tear, as well as associated injuries. Inclusion in the asymptomatic group required the presence of a superoposterior tear involving both the supraspinatus and infraspinatus tendons. Subjects with subscapularis tears were excluded (Fig. 1).
Subjects with symptomatic rotator cuff tears were identified during office visits. Potential symptomatic candidates demonstrated shoulder pain (≥3 on the VAS) and functional limitations with limited active range of motion. In addition, they had documentation of rotator cuff tear involving two tendons by MRI. As with the asymptomatic group, all tears were characterized by the size, location, and nature of the tear, as well as associated injuries. As with the asymptomatic group, inclusion in the study required superoposterior tears involving the supraspinatus and infraspinatus tendons. Criteria for exclusion included a presence of a subscapularis tear or history of previous surgery involving either the dominant or non-dominant shoulder. Nine of the 27 subjects consented to undergo subacromial injection and further testing. The other 19 subjects declined to participate further. For patients who underwent injection, under sterile conditions, 5 cc of 1% lidocaine and 5 cc of 0.5% marcaine were injected into the subacromial space. The injection was performed with a 22.5-gauge needle introduced posterolaterally beneath the undersurface of the acromion (Fig. 1).
After enrollment in the study and a physical examination of the upper extremity, each subject completed the L’Insalata shoulder questionnaire [8], the American Shoulder and Elbow Surgeons (ASES) standardized shoulder assessment form [11], and Simple Shoulder Test [9]. The visual analog score and these validated scores were obtained to help perform our group stratification and were acquired immediately prior to testing.
The mean age was 42 ± 7.7 years for the normal control subjects, 66.2 ± 5.1 years for asymptomatic subjects, and 64.8 ± 11.3 years for all 27 of the symptomatic subjects. Eight males and one female subject with an average age of 62.6 ± 9.7 years underwent subacromial injection. Elevation in the scapular plane was measured with a goniometer. Mean active elevation was 175 ± 3° for normal control subjects, 164 ± 4° for asymptomatic subjects, and 118 ± 20° for symptomatic subjects. The range of motion of the symptomatic subjects was less than those of the asymptomatic or symptomatic subjects (p < 0.01). Screening plain radiographs demonstrated no degenerative changes in the normal control group. Ultrasound examinations of the normal control subjects confirmed the absence of rotator cuff tears in all control subjects. For both the asymptomatic and symptomatic subjects, MRI findings demonstrated comparable superoposterior tear patterns in both groups involving both the supraspinatus and infraspinatus tendons. A single, independent musculoskeletal radiologist (R.S.A.) evaluated all plain film, ultrasound, and MRI studies.
Prior to injection, the average L’Insalata score was 100 for normal control subjects, 84 ± 10 for asymptomatic subjects, and 49 ± 15 for all 27 of the symptomatic subjects. The average ASES score was 100 for normal control subjects, 89 ± 14 for asymptomatic subjects, and 44 ± 17 for symptomatic subjects. The average Simple Shoulder Test score was 12.0 ± 0 for normal control subjects, 11.5 ± 0.5 for asymptomatic subjects, and 5.9 ± 3.0 for symptomatic subjects without injection. In the nine symptomatic subjects that volunteered to undergo injection, when the VAS was administered pre-injection, the average score was 8 while post-injection, the average score was 4. All subjects had improvement of the VAS after subacromial injection.
The EMG protocol used in this study, both for data collection and signal processing, has been previously documented [7]. In summary, fine-wire electrodes were placed into the supraspinatus, infraspinatus, and subscapularis using a hypodermic needle as a guide. Once the electrodes were placed, the hypodermic needles were removed and the electrodes taped into place. The surface markers were placed 2 cm apart on the corresponding muscle belly at the ideal electrode placement sites. A total of 12 electrodes were placed (Table 1). Once the electrodes were placed and tested for adequate signal processing, the subjects performed a series of 11 maximal voluntary contraction (MVC) normalization tests followed by ten selected functional tasks (Table 2). During the 11 MVC trials, each of which consisted of 3-s isometric contractions in each of the test positions, EMG signals were recorded. For each of the ten selected functional tasks, three consecutive trials were completed and EMG signals were recorded for each of the 12 muscles. After completing the MVC and functional tasks, symptomatic subjects underwent an analgesic injection. Ten minutes after injection, pain was re-characterized with a visual analog scale and the EMG data collection during the functional tasks was repeated.
Table 1.
MVC normalization positions for each muscle
| Muscle | Abbreviation | Test position |
|---|---|---|
| Supraspinatus | Supra | Resisted elevation at 90° elevation in scapular plane, 45° internal rotation and elbow extension |
| Infraspinatus | Infra | Resisted external rotation at 0° elevation in scapular plane and neutral rotation |
| Upper subscapularis | USS | Resisted internal rotation at 90° abduction, neutral rotation, and elbow flexion to 90° |
| Lower subscapularis | LSS | Resisted internal rotation at 90° abduction, neutral rotation, and elbow flexion to 90° |
| Latissimus dorsi | Lat | Resisted extension at 45° elevation in scapular plane and elbow flexion to 90° |
| Pectoralis major | Pec | Resisted horizontal adduction at 90° elevation in scapular plane and elbow flexion to 90° |
| Serratus anterior | Serra | Resisted scapular protraction at 90° shoulder flexion and elbow extended |
| Upper trapezius | UT | Resisted shoulder shrug with subject seated and arm at side |
| Middle trapezius | MT | Resisted shoulder extension at 90° shoulder flexion and elbow flexion to 90° (scapular retraction) |
| Lower trapezius | LT | Resisted shoulder extension at 180° shoulder flexion and elbow extended |
| Anterior deltoid | Ant D | Resisted forward flexion at 0° elevation in scapular plane and elbow flexion to 90° |
| Middle deltoid | Mid D | Resisted abduction at 0° elevation in scapular plane and elbow flexion to 90° |
| Posterior deltoid | Post D | Resisted extension at 0° elevation in scapular plane and elbow flexion to 90 |
Table 2.
Ten functional tasks
| Abbreviation | Function |
|---|---|
| 1#o | Place 1 lb on a shelf overhead without bending your elbow |
| 1#s | Lift 1 lb to the level of your shoulder without bending your elbow |
| 8#o | Lift 8 lb to the level of your shoulder without bending your elbow |
| 8#s | Place 8 lb on a shelf overhead without bending your elbow |
| Mid | Wash the middle of your back or hook a bra |
| Sm | Reach the small of your back to tuck in your shirt with your hand |
| Throw | Throw a softball overhand 10 yd with the affected extremity |
| Walk | Carry 20 lb at your side |
| Toss | Throw a softball underhand 10 yd with the affected extremity |
| Wash | Wash the back of your opposite shoulder |
For the EMG data collected during the MVC normalization tests, the peak amplitude recorded for a given muscle over a 0.5-s interval was calculated and then used as the normalization factor for that muscle for that subject. The EMG signal during the functional tasks for a given muscle was then normalized to the MVC value. This percent of maximal voluntary contraction (%MVC) was used for all data analysis. Normalization is a standard procedure for EMG signal processing when the relative activity of muscle is to be compared between individuals and between groups. Higher normalized values (%MVC) indicate an increase in the relative electrical activation of a given muscle during a task as compared to the amplitude recorded during a MVC. These are not a direct measure of strength of a muscle but rather a measure of increased activation of the muscle. There were 150 possible differences (15 electrode sites multiplied by ten tasks) to compare between each subject group.
Descriptive statistics (means ± SDs) were calculated on the subjective shoulder questionnaires. Descriptive statistics (means ± SDs) of the %MVC were calculated for each muscle during each task. Repeated-measures analyses of variance corrected for multiple comparisons were used to detect differences between the three groups, and post hoc testing was performed to compare normal subjects with both the asymptomatic and symptomatic pre- and post-injection groups. Significance was chosen at an alpha of 0.05.
Results
The EMG findings of normal subjects differed significantly from study subjects with both asymptomatic and symptomatic rotator cuff tears. When comparing asymptomatic to normal subjects, there were 70 of 150 instances (46%) where electromyography differed significantly. When comparing symptomatic to normal subjects, there were 93 of 150 instances (62%) where electromyography differed significantly with a p < 0.05 (Tables 3 and 4).
Table 3.
EMG data for symptomatic cuff tear vs. normal
| Ant D | Mid D | Post D | Pec | Lat | UT | MT | LT | Serra | Supra | Infra | USS | LSS | BB | Br | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1#o | X | X | X | X | |||||||||||
| 1#s | X | X | X | X | X | X | X | X | X | X | |||||
| 8#o | X | X | X | ||||||||||||
| 8#s | X | X | X | X | X | X | X | X | X | X | |||||
| Mid | X | X | X | X | X | X | X | X | X | X | |||||
| Sm | X | X | X | X | X | X | X | X | X | X | X | X | |||
| Throw | X | X | X | X | X | X | X | X | X | X | X | ||||
| Toss | X | X | X | X | X | X | X | X | X | X | X | X | X | ||
| Walk | X | X | X | X | X | X | X | X | X | X | |||||
| Wash | X | X | X | X | X | X | X | X | X | X | X | X |
X indicates significant difference in %MVC between normal and symptomatic rotator cuff tear
Table 4.
EMG data for asymptomatic cuff tear vs. normal
| Ant D | Mid D | Post D | Pec | Lat | UT | MT | LT | Serra | Supra | Infra | USS | LSS | BB | Br | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1#o | X | X | X | X | |||||||||||
| 1#s | X | X | X | X | X | X | X | X | X | X | |||||
| 8#o | X | X | X | X | |||||||||||
| 8#s | X | X | X | X | X | X | X | X | X | X | |||||
| Mid | X | X | X | X | X | X | |||||||||
| Sm | X | X | X | X | X | X | |||||||||
| Throw | X | X | X | X | X | ||||||||||
| Toss | X | X | X | X | X | X | X | X | X | ||||||
| Walk | X | X | X | X | |||||||||||
| Wash | X | X | X | X | X | X | X | X | X | X |
X indicates significant difference in %MVC between normal and asymptomatic rotator cuff tear
The EMG findings in symptomatic and asymptomatic patients were similar in most instances, but differed during active forward elevation. When comparing asymptomatic to symptomatic subjects, there were six instances where there were significant differences (4%; Table 5). Three of these differences occurred in the anterior deltoid during forward elevation tasks. During the 8-lb overhead elevation task, asymptomatic subjects demonstrated significantly higher %MVC in the anterior deltoid than symptomatic subjects (55 ± 12% vs. 39 ± 14%, p < 0.05). During 8- and 1-lb elevation to shoulder height, asymptomatic patients demonstrated significantly greater %MVC in the anterior deltoid compared to the symptomatic patients (8 lb, 48 ± 11% vs. 37 ± 13%, p < 0.05; 1 lb, 34 ± 11% vs. 30 ± 13%, p < 0.05).
Table 5.
EMG data for asymptomatic cuff tear vs. symptomatic cuff tear
| Ant D | Mid D | Post D | Pec | Lat | UT | MT | LT | Serra | Supra | Infra | USS | LSS | BB | Br | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1#o | X | ||||||||||||||
| 1#s | |||||||||||||||
| 8#o | X | ||||||||||||||
| 8#s | X | ||||||||||||||
| Mid | X | ||||||||||||||
| Sm | |||||||||||||||
| Throw | |||||||||||||||
| Toss | |||||||||||||||
| Walk | X | X | |||||||||||||
| Wash |
X indicates significant difference in %MVC between asymptomatic and symptomatic rotator cuff tear
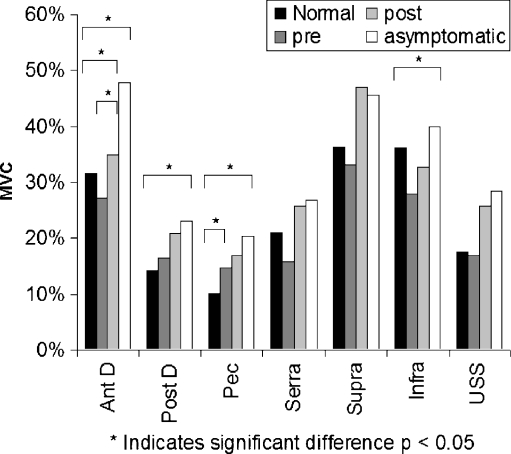
Injection of the subacromial space leads to improved deltoid firing during forward elevation. In pre- vs. post-injection subjects, there were ten instances where electromyography differed significantly (7%; Table 6). Four of these differences occurred in the anterior deltoid, with two of them occurring during forward elevation tasks. The effect of injection demonstrated a significant effect primarily in the anterior deltoid during overhead elevation tasks; however, other data that did not reach significance in this study suggested that injection improved firing globally and approached the firing of the asymptomatic state (Fig. 2).
Fig. 2.
Electromyography of selected muscles during elevation of an 8-lb weight overhead in normal subjects, asymptomatic subjects, symptomatic subjects pre-injection and symptomatic subjects post-injection. Globally, symptomatic patients/post-injection appear to demonstrate global improvement of muscle firing patterns
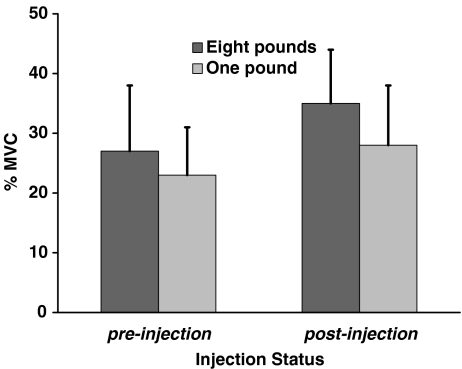
During 8-lb elevation to shoulder height, post-injection subjects demonstrated a significantly greater anterior deltoid %MVC than pre-injection subjects (35 ± 9% vs. 27 ± 11%, p < 0.05). Similarly, in 1-lb elevation to shoulder height, post-injection subjects demonstrated significantly greater %MVC than pre-injection subjects (28 ± 10% vs. 23 ± 8%, p < 0.05; Fig. 3). Range of motion also increased during 1-lb injection to shoulder height from pre- to post-injection (112 ± 31° vs. 117 ± 28°, p = 0.08).
Fig. 3.
In symptomatic subjects, the %MVC of the anterior deltoid improved in both the 8- and 1-lb overhead lift after subacromial injection
Discussion
This study examined electromyographic patterns in normal subjects, subjects with asymptomatic large rotator cuff tears, subjects with symptomatic large rotator cuff tears, and subjects with symptomatic large rotator cuff tears after subacromial anesthetic injection. We found that (1) subjects with large rotator cuff tears have globally different muscle firing activity when compared to healthy controls, (2) EMG activity in the deltoid is significantly different in symptomatic and asymptomatic subjects during forward shoulder elevation, and (3) EMG activity in the deltoid improves after subacromial injection in symptomatic subjects.
There were clearly numerous differences in muscle firing during various tasks between asymptomatic and symptomatic subjects with rotator cuff tears and normal controls. The number of differences was much smaller when comparing asymptomatic and symptomatic subjects; however, these differences occurred mainly in the anterior deltoid during forward elevation tasks. These data suggest that pain inhibition of the deltoid is a primary actor in shoulder dysfunction in the setting of rotator cuff tear. Previous in vitro and in vivo studies have suggested this possibility, but to our knowledge, this is the first study to provide direct evidence that diminished deltoid firing has a direct relationship to shoulder dysfunction.
In vitro biomechanical studies suggest that there exists a mechanism utilizing the deltoid to compensate for rotator cuff tears to preserve shoulder function. Thompson et al. [14] demonstrated that arm abduction could be performed by increasing force applied through the middle deltoid when no force is applied through the supraspinatus. Studies by Kedgley et al. [6] suggested that as the rotator cuff tears, the plane of elevation moves posteriorly, necessitating recruitment of the deltoid and other muscles than the rotator cuff for arm abduction. Hansen et al. [5] demonstrated that increasing force applied through the deltoid can compensate for increasingly larger rotator cuff tears.
If this mechanism utilizing the deltoid is able to compensate for a rotator cuff tear, why are some patients able to compensate while others have difficulty? Previous in vivo work from Scibek et al. suggests that subacromial injection in patients with rotator cuff tears improves scapulohumeral rhythm, and work from Reddy et al. suggests that in patients with impingement, there is decreased middle deltoid firing [10, 12, 14]. These studies imply that pain leads to inhibition of the deltoid.
The results from this study provide direct evidence that anterior deltoid firing is statistically greater in asymptomatic than symptomatic subjects. Most strikingly, subacromial injection in symptomatic subjects leads to significant increases in anterior deltoid firing during the same elevation tasks. This study helps unify previous studies: Subacromial injection in patients with symptomatic rotator cuff tears results in improved deltoid firing as in patients with subacromial impingement. That subsequent improvement in deltoid firing is likely why scapulohumeral rhythm improves with subacromial injection.
These findings may be applied to clinical observations. Patients who undergo subacromial decompression with debridement of partial rotator cuff tears generally demonstrate at least short-term improvements in clinical outcomes [1, 3, 13]. In addition, patients who undergo rotator cuff repair generally maintain clinical improvements in validated outcome measures despite structural repair failure [2, 4]. In these cases, bursectomy and subacromial decompression may provide substantial pain relief, thereby improving deltoid compensation and, subsequently, patient outcomes. However, it is unclear whether rotator cuff surgery restores normal mechanics or facilitates compensatory mechanics. Ultimately, the greatest utility of these findings are to apply them to our understanding of the symptomatology of rotator cuff tears.
There are several potential limitations to this study. Electromyographic data are affected by equipment type and quality, reproducibility of actions among patients examined, and signal artifact. Patient movements such as lifting overhead or throwing vary widely among individuals. We felt that attempting to standardize these movements would be artificial and subsequently accepted this variability. By accepting this variability, there are caveats: For example, the elevation to shoulder height task may be more representative of forward shoulder elevation than the overhead elevation task, as only normal and asymptomatic subjects could fully elevate overhead. In addition, type II error is highly probable in studies using electromyography because of the wide variation in data acquired. In order to minimize type II error in electromyographic studies, large cohorts are required; however, economic considerations make these large cohorts impractical. Our findings should be considered with the caveat that there is a considerable degree of variability in quantitative EMG studies and only the most statistically robust results are likely to be reproducible by future researchers. We demonstrated that our rotator cuff groups were different by patient-rated outcomes, but we did not demonstrate structural equivalence of our rotator cuff tear groups. Tear location, tear size, fatty atrophy, and associated pathology may introduce variation in data. In addition to these patient variables, electrical signals from the heart can contaminate electromyography, especially in left-sided leads near the cardiac apex. An additional limitation is that our injections were not guided by ultrasound. Subacromial injection does not entirely alleviate subacromial symptoms, and symptom relief can vary between patients as noted by the VAS score decreasing from 8 to 4. Another weakness of the study design was the lack of an a priori power analysis. We performed an a posteriori power analysis of the upper subscapularis, lower subscapularis, and supraspinatus. We found that in our cohort, we had adequate power with a beta of 98% to demonstrate that there was no difference in the supraspinatus during the 8-lb overhead elevation. However, other findings which were found not be significant do not have adequate statistical power to comment on whether they fire differently or similarly during specific activities.
These limitations are useful in comparing our results to those of Kelly et al. [7]. This initial pilot study found electromyographic differences in symptomatic vs. asymptomatic patients with rotator cuff tears, most notably with increased subscapularis activity during heavy lifting and internal rotation tasks. The results of this study confirmed that there are global differences in electromyographic firing patterns during shoulder tasks when comparing normal patients, symptomatic patients, and asymptomatic patients. The current study confirmed that there are trends toward increased subscapularis activity in asymptomatic patients during forward elevation; however, the previous findings of increased subscapularis activity in asymptomatic patients during internal rotation tasks were not reproduced.
It is important to note that it is unclear how increased muscle firing translates clinically. There are no studies to our knowledge documenting the relationship with muscle firing or range of motion. Our study provides some indirect evidence: when comparing symptomatic and asymptomatic patients, asymptomatic patients demonstrated greater firing of the anterior deltoid with 8-lb weighted forward elevation and correspondingly had a greater range of unweighted active forward elevation (164 ± 4° for asymptomatic subjects and 118 ± 20° for symptomatic subjects, p < 0.01). However, this correlation requires further study. We observed limited improvement of range of motion with subacromial injection; however, it is important to note that after injection, the muscles about the shoulder are likely quite deconditioned and modest clinical improvements would be expected. There was also an incomplete response to subacromial injection, and although there is a gross association with improvement in range of motion, there is no hard statistical association in our study.
The differences in these two studies may be a result of structural heterogeneity of rotator cuff tears and associated pathology between the two cohorts. In addition, a number of significant findings in the pilot study were seen as trends in the larger study, giving some probabilistic support of these earlier findings.
The logical extension of this study is to obtain electromyographic data from patients who have undergone rotator cuff repair and have either healed or have a persistent defect. One would predict that patients with healed rotator cuff tendons should demonstrate EMG patterns similar to normal patients, and despite being asymptomatic, patients with incompletely healed rotator cuff tendons should demonstrate EMG patterns similar to asymptomatic patients with rotator cuff tears.
In conclusion, subacromial injection increases anterior deltoid firing during forward elevation tasks in symptomatic subjects with large rotator cuff tears. These increases approach, but do not equal the increased anterior deltoid firing in asymptomatic subjects with large rotator cuff tears. In the context of the global EMG patterns observed in symptomatic and asymptomatic rotator cuff tears, subacromial injection decreases anterior deltoid inhibition and subsequently improves compensatory mechanics during forward shoulder elevation.
Acknowledgments
The authors gratefully acknowledge the assistance of Mark W. Lenhoff and Brian S. Pansy for data analysis; Ronald S. Adler MD for musculoskeletal imaging and interpretation; David W. Altchek MD, Russell F. Warren MD, Edward V. Craig MD, and Thomas L. Wickiewicz MD for their suggestions for study improvement and patient contributions; Daniel E. Weiland MD and Samuel P. Robinson MD for early project development and patient recruitment; and previous sports fellows Eric L. Chehab MD, Aimee S. Klapach MD, William M. Isbell MD, Daniel P. Tomlinson MD, and Nikhil N. Verma MD for their involvement in patient recruitment.
Footnotes
Each author certifies that he or she has no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participating in the study was obtained.
This study was performed at Leon Root, M.D. Motion Analysis Laboratory, Hospital for Special Surgery, 510 East 73rd Street, New York, NY 10021, USA.
References
- 1.Altchek DW, Warren RF, Wickiewicz TL, Skyhar MJ, Ortiz G, Schwartz E. Arthroscopic acromioplasty: Technique and results. J. Bone Jt. Surg. Am. 1990;72:1198–1207. [PubMed] [Google Scholar]
- 2.Anderson K, Boothby M, Aschenbrener D, Holsbeeck M. Outcome and structural integrity after arthroscopic rotator cuff repair using 2 rows of fixation: Minimum 2 year follow-up. Am. J. Sports Med. 2006;34:1899–1905. doi: 10.1177/0363546506290187. [DOI] [PubMed] [Google Scholar]
- 3.Cordasco FA, Backer M, Craig EV, Klein D, Warren RF. The partial-thickness rotator cuff tear: is acromioplasty without repair sufficient? Am. J. Sports Med. 2002;30(2):257–60. doi: 10.1177/03635465020300021801. [DOI] [PubMed] [Google Scholar]
- 4.Galatz LM, Ball CM, Teefey SA, Middleton WD, Yamaguchi K. The outcome and integrity of completely arthroscopically repaired large and massive rotator cuff tears. J. Bone Jt. Surg. 2004;86A:219–224. doi: 10.2106/00004623-200402000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Hansen ML, Otis JC, Johnson JS, Cordasco FA, Craig EV, Warren RF. Biomechanics of massive rotator cuff tears: Implications for treatment. J. Bone Jt. Surg. Am. 2008;90:316–25. doi: 10.2106/JBJS.F.00880. [DOI] [PubMed] [Google Scholar]
- 6.Kedgley AE, Mackenzie GA, Ferreira LM, Johnson JA, Faber KJ. In vitro kinematics of the shoulder following rotator cuff injury. Clin. Biomech. 2007;22:1068–73. doi: 10.1016/j.clinbiomech.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 7.Kelly BT, Williams RJ, Cordasco FA, Backus SI, Otis JC, Weiland DE, et al. Differential patterns of muscle activation in patients with symptomatic and asymptomatic rotator cuff tears. J. Shoulder Elbow Surg. 2005;14:165–171. doi: 10.1016/j.jse.2004.06.010. [DOI] [PubMed] [Google Scholar]
- 8.L’Insalata JC, Warren RF, Cohen SB, Altchek DW, Peterson MG. A self-administered questionnaire for assessment of symptoms and function of the shoulder. J. Bone Jt. Surg. 1997;79A:738–48. [PubMed] [Google Scholar]
- 9.Lippett S, Harryman DT, Matsen FA. A practical tool for evaluating function: The simple shoulder test. In: Matsen FA, Fu FH, Hawkins R, editors. The Shoulder: A Balance of Mobility and Stability. Chicago: Park Ridge; 1993. pp. 501–18. [Google Scholar]
- 10.Reddy AS, Mohr KJ, Pink MM, Jobe FW. Electromyographic analysis of the deltoid and rotator cuff muscles in persons with subacromial impingement. J. Shoulder Elbow Surg. 2000;9:519–23. doi: 10.1067/mse.2000.109410. [DOI] [PubMed] [Google Scholar]
- 11.Richards RR, An KN, Bigliani L, Friedman RJ, Gartsman GM, Gristina AG, et al. A standardized method for the assessment of shoulder function. J. Shoulder Elbow Surg. 1994;3:347–52. doi: 10.1016/S1058-2746(09)80019-0. [DOI] [PubMed] [Google Scholar]
- 12.Scibek JS, Mell AG, Downie BK, Carpenter JE, Hughes RE. Shoulder kinematics in patients with full thickness rotator cuff tears after a subacromial injection. J. Shoulder Elbow Surg. 2008;17:172–81. doi: 10.1016/j.jse.2007.05.010. [DOI] [PubMed] [Google Scholar]
- 13.Snyder SJ, Pachelli AF, Del Pizzo W, Friedman MJ, Ferkel RD, Pattee G. Partial thickness rotator cuff tears: Results of arthroscopic treatment. Arthroscopy. 1991;7:1–7. doi: 10.1016/0749-8063(91)90070-e. [DOI] [PubMed] [Google Scholar]
- 14.Thompson WO, Debski RE, Boardman ND, 3rd, Taskiran E, Warner JJ, Fu FH, et al. A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am. J. Sports Med. 1996;24:286–92. doi: 10.1177/036354659602400307. [DOI] [PubMed] [Google Scholar]