Abstract
Background
Important questions remain regarding the necessary duration and intensity for methadone treatment to be effective.
Methods
As part of a clinical trial of tuberculosis chemoprophylaxis (Batki et al., 2002), patients with opioid dependence were recruited from an outpatient 21-day methadone detoxification program and were randomly assigned to one of three treatment conditions: 1) continuation in 21-day methadone detoxification; 2) transfer to six-month methadone maintenance with only minimal counseling; or 3) transfer to six-month methadone maintenance with standard twice monthly counseling and as-needed social work and psychiatric services. Both of the six-month maintenance treatments were followed by 1.5 months of detoxification. Urine drug tests and self-report measures were collected at baseline, months 1 through 6, and month 8.5.
Results
Compared to 21-day methadone detoxification, six-month methadone maintenance with either minimal or standard counseling resulted in fewer opiate positive urine tests and days of self-reported heroin and alcohol use. There was no change in cocaine use or other outcome measures. The increased counseling available in the standard counseling condition did not appear to reduce heroin use further than the minimal counseling condition, in contrast to the effect found for more structured counseling in long-term methadone maintenance (McLellan et al., 1993).
Conclusions
Six months of methadone maintenance, even with minimal counseling, reduces heroin and alcohol use more than 21-day methadone detoxification.
Keywords: opioid dependence, methadone maintenance, counseling, contingency management
1. Introduction
Few people with opioid dependence attain long-term remission without medication-assisted treatment (National Institute of Health, 1998; Department of Health and Human Services, 2005). There is a large demand for medication-assisted treatment, particularly methadone, and only a fraction of opioid dependent individuals are receiving treatment. Because of the unmet need and limited treatment resources, it is important to determine the relative effectiveness of methadone treatment of different durations and intensities.
1.1 Methadone Detoxification
Methadone detoxification has been widely used because of its brevity and the resulting ability to serve more patients than long-term methadone maintenance. Although detoxification has been found to be effective in reducing the symptoms of opioid withdrawal, it is not an effective treatment for opioid dependence (Amato et al., 2005b). Because it is widely used but not effective, it is helpful to include methadone detoxification as a routine care control group in studies evaluating methadone maintenance. For example, randomized trials have shown that methadone maintenance results in more opiate free urine test results than methadone detoxification conducted over 60 days (Newman and Whitehill, 1979), 45 days (Vanichseni et al., 1991), or 35 days (Strain et al., 1993).
1.2 Methadone Maintenance with Minimal Counseling
Methadone maintenance is helpful even with minimal counseling. A randomized trial showed reduction in heroin use with just one month of methadone maintenance with occasional counseling, relative to a waiting list control group (Yankovitz et al., 1991). Based on these findings, interim methadone maintenance with minimal counseling was authorized in the U.S.A. for opioid dependent individuals awaiting admission to comprehensive methadone maintenance programs (Federal Register, 1993). Several other countries, such as the Netherlands, allow methadone maintenance without mandatory counseling in office-based settings without time limitations (Solberg et al., 2002).
1.3 Methadone Maintenance with Standard Counseling
In order to improve outcomes, psychosocial interventions such as counseling have been added to methadone maintenance. Randomized trials have shown that methadone maintenance with regular counseling is more effective than no treatment, a waiting list, outpatient drug free treatment, placebo medication, or methadone detoxification, all of which have poor outcomes on urine drug tests as well as other measures (Amato et al., 2005a; Mattick et al., 2003).
Randomized trials have shown that methadone maintenance outcomes are better with regular counseling than with minimal counseling (Amato et al., 2004). In one of these studies (McLellan et al., 1993), standard counseling was provided twice a month, or twice a week if drug tests were positive. In addition, employed patients with drug free urine tests earned up to two take-home doses per week. In contrast, the minimal counseling group received minimal monthly counseling and non-contingent take-home doses for employed patients. Patients were randomly assigned to methadone maintenance with standard versus minimal counseling and followed for six months. Although both treatments reduced drug use, the standard counseling condition reduced heroin and cocaine use more than the minimal counseling condition. In another randomized trial, standard counseling twice a month or more in the first three months of treatment was compared to minimal monthly counseling. The twice monthly counseling reduced opiate positive urine test results relative to minimal counseling (Saxon et al., 1996). Of note, both of these clinical trials comparing standard to minimal counseling were conducted with patients in their first six months of long-term methadone maintenance.
1.4 Short-term Methadone Maintenance
Developed to serve more patients and to limit time on opiate replacement, short-term methadone maintenance consists of several months on a stable dose of methadone followed by a six-to-eight-week taper off methadone. In one randomized study, four months of methadone maintenance followed by a two-month methadone detoxification was compared to long-term methadone maintenance (Sees et al., 2000). Heroin use was similar during the first four months while both groups remained on a stable dose of methadone. Heroin use remained low in the long-term methadone maintenance group, but increased during the taper in months 5 and 6 in the short-term methadone maintenance group.
Although short-term methadone maintenance did not have effects past the end of treatment, it appeared to protect patients from the harmful effects of heroin use during the time that they were in treatment. This could be helpful for patients who prefer time-limited methadone treatment, and in settings where the number of patients needing methadone maintenance exceeds the number of available treatment slots. Although randomized studies have shown that open-ended methadone maintenance is more effective than methadone detoxification, there are no controlled studies yet comparing short-term methadone maintenance to methadone detoxification.
1.5 Study Aims
This study assessed the benefits of transferring patients to six months of methadone maintenance, with either standard or minimal counseling, compared to keeping them in 21-day outpatient methadone detoxification, the usual care available to them. Although previous randomized trials had compared various methadone dosages to each other and to methadone detoxification controls (e.g. Strain et al., 1993), the present study was the first to compare methadone maintenance with different counseling intensities to each other as well as to a methadone detoxification control group.
This study was primarily designed to test the effects of methadone maintenance on adherence to six months of directly observed tuberculosis (TB) chemoprophylaxis with isoniazid. As described in Batki et al. (2002), heroin dependent patients with latent TB who received methadone maintenance, even with only minimal counseling, were more likely to complete the six-month TB preventive therapy than those who received only 21-day methadone detoxification with monthly visits to a TB clinic. As the earlier report focused on the main findings and did not describe other outcomes, the present report focuses on the effects of the six-month methadone maintenance with different counseling intensities on substance use and psychosocial outcomes.
1.6 Hypotheses
We hypothesized that six months of methadone maintenance, even with only minimal counseling, would result in less substance use, fewer psychiatric symptoms, and fewer family/social problems compared to 21-day methadone detoxification. We further hypothesized that methadone maintenance with standard counseling and a take-home dose contingency would result in more improvement in substance use, psychiatric problems, and family/social problems than methadone maintenance with only minimal counseling.
Differences were expected in outcomes related to drug use, psychiatric, and family/social problems. However, no differences were expected in legal, employment, or medical problems, as these were likely to take longer than six months to change.
2. Methods
2.1 Design
This was a randomized prospective trial with three outpatient treatment arms: 1) a usual care control group consisting of 21-day methadone detoxification, 2) six months of methadone maintenance with minimal counseling followed by a six-week methadone detoxification, or 3) six months of methadone maintenance with standard counseling followed by a six-week methadone detoxification. This study was designed primarily to test the effectiveness of methadone maintenance in increasing completion of six months of TB preventive therapy (as described in Batki et al., 2002). The study also allowed analysis of the effects of six-month methadone maintenance with differing amounts of counseling on substance use and related outcomes.
2.2 Setting
Heroin dependent patients recently discharged from inpatient medical and psychiatric units at San Francisco General Hospital (SFGH) were routinely admitted to the hospital’s outpatient 21-day methadone detoxification program. These patients had limited access to methadone maintenance treatment due to their lack of Medicaid or other insurance, and the shortage of publicly funded methadone maintenance in the county. Buprenorphine treatment was not available in 1995–1997 when this study was conducted. The study created additional six-month methadone maintenance slots at no cost to the research participants, who had a 2 out of 3 chance of being randomly assigned to six-month treatment and a 1 out of 3 chance of remaining in 21-day detoxification.
2.3 Participants
Participants were recruited from a public hospital’s 21-day outpatient methadone detoxification program. Patients in this outpatient detoxification program had not sought out methadone treatment, but instead had been referred from the hospital’s inpatient medical and psychiatric units. To be eligible for this study, patients in the 21-day methadone detoxification program had to meet the following inclusion criteria: 1) latent TB infection as demonstrated by a positive PPD test, a negative chest radiograph, and approval by a TB clinic physician; 2) a DSM-III-R diagnosis of opioid dependence; 3) age between 21 and 59 years; 4) expressed willingness to receive 6 months of isoniazid (INH) preventive therapy and methadone treatment. Patients who were pregnant or had HIV were excluded from this study because they received priority admission to routine long-term methadone maintenance. Patients with active liver disease or aspartate transaminase (AST) greater than three times the upper limit of the normal range were excluded because INH was contraindicated for them.
Patients in the 21-day methadone detoxification program who were eligible for the study underwent complete informed consent procedures, as approved by the University of California San Francisco Institutional Review Board. This included description of study procedures, risks and benefits, payment, and participant rights, all of which followed the international standards for human experimentation. These were presented in writing and in person. Participants signed and received copies of the consent form and a research subject bill of rights. A Federal Certificate of Confidentiality was obtained to further protect participants.
Of the 115 individuals who were eligible and consented to participate in the study, four were excluded during the baseline assessment period. One was found to have past history of INH intolerance, two were judged to have active TB, and one dropped out. The remaining 111 participants were randomly assigned to the treatment conditions.
2.4 Randomization
The schedule for randomization to treatment conditions was generated by a statistician who placed subject assignments in individual sealed envelopes and did not reveal the schedule to project staff. At the conclusion of the final baseline interview, the project staff opened the envelope containing the condition assignment.
2.5 Treatment Conditions
The 111 participants were randomly assigned to one of three outpatient methadone treatment conditions. Depending on this assignment, they either continued in their 21-day methadone detoxification, or were transferred to one of the six-month methadone maintenance conditions.
1) Methadone detoxification (n = 39): In this control intervention, participants remained in the outpatient 21-day methadone detoxification and were not admitted to methadone maintenance. They were eligible for readmission to 21-day detoxification every 7 weeks from the date of the initial detoxification admission. Participants in this treatment condition received their TB preventive medications (INH and pyridoxine) in 30-day supplies at monthly visits to the TB clinic, which was in the same building as the methadone clinic.
2) Six months of methadone maintenance with minimal counseling (Minimal MM) (n = 35): Participants in this group were transferred from the 21-day methadone detoxification program to six-month methadone maintenance. They were guaranteed methadone maintenance for six months (60–90 mg) followed by a six-week taper. Methadone dose was progressively raised, to a maximum of 90 mg per day, until withdrawal symptoms and cravings were eliminated, or until sedation or other side effects occurred, or until participants requested no further increase because of concerns about anticipated withdrawal symptoms during the six-week taper at the end of the six-month treatment. The lower limit of 60 mg per day was selected because doses below this level have been found to be less effective (e.g. Faggiano et al., 2003). The upper limit of 90 mg per day was selected because of concerns that higher doses would make it more difficult to taper off methadone after the six-month period of maintenance.
In this minimal counseling treatment condition, participants received counseling only on an emergency basis or to enforce program rules, approximately once a month for no more than 15 minutes. Urine drug tests and alcohol breathalyzer tests were administered once a week; however, participants and counselors were not given the results, and no take-home methadone doses could be earned based on these results. This level of care approximated the interim methadone maintenance guidelines (Federal Register, 1993). Participants in this treatment condition received their TB preventive therapy in directly observed doses at their daily methadone clinic visits.
3) Six months of methadone maintenance with standard counseling (Standard MM) (n = 37): As in the minimal MM condition, participants were transferred from 21-day methadone detoxification to the six-month methadone maintenance program, and were guaranteed methadone maintenance for six months (60–90 mg) followed by a six-week taper. Likewise, participants in this treatment condition received their TB preventive therapy in directly observed doses at their daily methadone clinic visits. However, in the standard MM condition, participants received counseling twice per month and employed participants could earn two take-home doses in the week after each negative weekly random urine drug test and alcohol breathalyzer test. If the participant and counselor agreed that additional services would be helpful, he/she received additional counseling sessions and/or onsite social work or psychiatric services. In contrast, McLellan et al. (1993) required twice weekly counseling sessions when drug tests were positive, and offered no onsite social work, psychiatric, or medical services.
2.6 Baseline Measures of Participant Characteristics
After study entry, demographic information was obtained and the Structured Clinical Interview for DSM-III-R (SCID) (Spitzer et al., 1989) was administered in order to diagnose the presence or absence of major depressive disorder.
2.7 Outcome Measures Administered at Baseline and Monthly
Participants were asked to complete an interview and provide an observed urine specimen at baseline prior to randomization, as well as at each of the 7 monthly follow-ups. They were paid $12 for each completed interview. Only the once monthly urine samples were used in study analyses, not the additional weekly random urine drug tests and alcohol breathalyzer tests that were collected as part of the standard and minimal methadone maintenance conditions. Urine was analyzed for opiates, methadone, cocaine, amphetamines, barbiturates, benzodiazepines, and phencyclidine. Using the Quantitative Drug Inventory (Gawin and Kleber, 1984), interviewers asked participants to report the frequency and amount of heroin and cocaine use on each day of the past week. The Addiction Severity Index (ASI), fifth edition (McLellan et al., 1992b) was administered to assess addiction problem severity in the past 30 days. The Beck Depression Inventory (BDI) (Beck et al., 1961) was used to assess symptoms of depression experienced in the past week. The Treatment Services Review (TSR) (McLellan et al., 1992a) was used to assess treatment services received in the past week. The TSR asked about services received both within the methadone treatment program (if applicable) and elsewhere.
2.8 Data Analysis
With 111 randomized participants, this study had the power to detect a medium or larger effect size for both dichotomous and continuous measures. Outcomes were compared using parallel models that included treatment condition, assessment month (months 1 through 6, or months 1 through 8.5), and the interaction of condition-by-time. For each outcome measure, its baseline level was included as a covariate. General Estimating Equations were used to adjust for the dependency inherent in repeated measures via Proc Genmod in SAS (v9.13). A contrast statement was used to estimate and test the specific comparisons of interest: a) methadone detoxification versus methadone maintenance with minimal counseling, and b) methadone maintenance with minimal counseling versus methadone maintenance with standard counseling. For binary outcomes a binomial distribution with log link was specified, and for continuous outcomes the normal distribution with identity link was used.
3. Results
3.1 Participant Characteristics
Characteristics of the 111 randomized study participants are shown in Table 1, as well as in Batki et al. (2002, Table 1, p. 286). The majority of patients were male and non-white. Average income was below $2000 per month. Although all were dependent on heroin, only a third stated they wanted to quit heroin completely; most were hoping to use less or use more safely. Over a third met criteria for cocaine dependence or abuse, and over a quarter met criteria for alcohol dependence or abuse.
Table 1.
Participant Characteristics
| 21-day detoxification n = 39 | Minimal MM n = 35 | Standard MM n = 37 | p-value | |
|---|---|---|---|---|
| % (n) | % (n) | % (n) | ||
| Gender | ||||
| Male | 74.4% (29) | 54.3% (19) | 54.0% (20) | 0.114 |
| Female | 25.6% (10) | 45.7% (16) | 45.9% (17) | |
| Ethnicity | (n = 37) | |||
| White | 40.5% (15) | 37.1% (13) | 45.9% (17) | 0.896 |
| African American | 27.0% (10) | 34.2% (12) | 29.7% (11) | |
| Latino | 18.9% (7) | 20.0% (7) | 21.6% (8) | |
| Native American | 5.4% (2) | 2.9% (1) | 2.7% (1) | |
| Asian/Pacific Islander | 8.1% (3) | 5.7% (2) | 0.0% (0) | |
| Marital status | ||||
| Married | 12.8% (5) | 20.0% (7) | 13.5% (5) | 0.842 |
| Widowed | 5.1% (2) | 2.9% (1) | 5.4% (2) | |
| Separated | 12.8% (5) | 8.6% (3) | 21.6% (8) | |
| Divorced | 33.3% (13) | 37.1% (13) | 27.0% (10) | |
| Never married | 35.9% (14) | 28.6% (10) | 32.4% (12) | |
| Clinical Variables | ||||
| Opioid dependence | 100% (39) | 100% (35) | 100% (37) | |
| Alcohol dependence | 7.7% (3) | 12.1% (4) | 16.2% (6) | 0.532 |
| Alcohol abuse | 17.9% (7) | 12.1% (4) | 21.6% (8) | 0.568 |
| Cocaine dependence/abuse | 41.0% (16) | 42.4% (15) | 48.6% (18) | 0.780 |
| Current major depression | 43.5% (17) | 21.7% | 34.8% (9) | 0.518 |
| Goal to quit heroin completely | 46.2% (18) | 25.7% (9) | 35.1% (13) | 0.186 |
| Continuous Variables | Mean (S.D.) | |||
| Age (years) | 43 (4.8) | 42.6 (6.2) | 40.2 (4.8) | 0.047 |
| Education (years) | 12.2 (1.6) | 11.9(2.0) | 12.0 (2.3) | 0.79 |
| Income ($ per month) | 1608 (1853) | 1308 (1853) | 1262 (1461) | 0.64 |
| Years of heroin use | 20.4 (8.93) | 16.6 (8.46) | 16.9 (9.41) | 0.121 |
| Beck depression inventory | 16.4 (9.03) | 13.7 (9.81) | 20.2 (11.12) | 0.022 |
Despite random assignment, the treatment groups differed significantly on several characteristics. The standard MM group was slightly younger (mean = 40.2, SD = 4.8) than the minimal MM group (mean = 42.6, SD = 6.2) and the detoxification group (mean = 43.0, SD = 4.8). The detoxification group had higher levels of depressive symptoms (Beck Depression Inventory mean = 20.1, SD = 11.12) than the minimal MM group (mean = 13.7, SD = 9.81) and the standard MM group (mean = 16.4, SD = 9.03).
3.2 Retention in Methadone Maintenance
The median length of stay was 180 days for both the minimal MM group and the standard MM group. The mean was 175.5 days (range 37–221) for the minimal MM group, and 157.5 (range 31–203), for the standard MM group. The difference was not statistically significant (Wilcoxon Log-Rank Chi-square = .4696, p = .4931).
3.3 Completion of Outcome Assessments
Attrition increased at each follow-up period, and was highest in the methadone detoxification group. Urinalysis results for month 8.5 were available for 15 of 39 in methadone detoxification (38.5%), 17 of 35 in minimal MM (48.6%), and 19 of 37 in standard MM (51.4%). We did not impute missing data.
3.4 Effects of Treatment Conditions on Treatment Outcomes
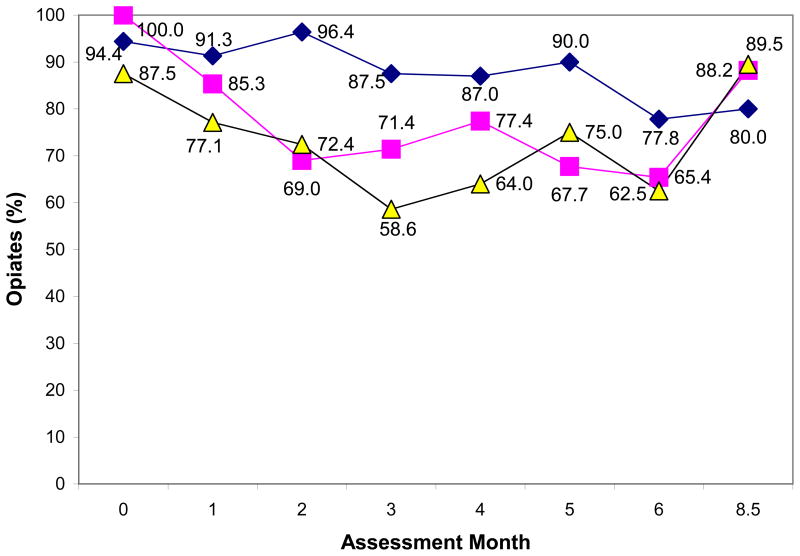
The percentages of urine tests positive for opiates and cocaine, by assessment month and treatment condition, are displayed in Figure 1. The means and standard deviations for self-reported substance use are displayed in Table 2. At the baseline assessment (month 0), when all three treatment groups were in outpatient 21-day methadone detoxification following an inpatient medical or psychiatric hospitalization, the groups’ urinalyses were 87.5–100% opiate positive and their self-reported heroin use averaged 18–19 of the previous 30 days.
Figure 1.
Percent urine tests positive for opiates by assessment month and treatment condition.
( 21-day methadone detoxification,
21-day methadone detoxification,  6-month methadone maintenance with minimal counseling,
6-month methadone maintenance with minimal counseling,  6-month methadone maintenance with standard counseling.) Although the standard errors of some of the proportions may overlap [SEP = p (1-p)/n], the combined difference was statistically significant: Opiate positive urine tests months 1–6: Minimal MM vs. Detox p = .0302. Opiate positive urine tests months 1–8.5: Minimal MM vs. Detox p = .0149.
6-month methadone maintenance with standard counseling.) Although the standard errors of some of the proportions may overlap [SEP = p (1-p)/n], the combined difference was statistically significant: Opiate positive urine tests months 1–6: Minimal MM vs. Detox p = .0302. Opiate positive urine tests months 1–8.5: Minimal MM vs. Detox p = .0149.
Table 2.
Means (Standard Deviations) of Self-Reported Use, by Assessment Month and Treatment Condition.
| Assessment Month | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 8.5 |
|---|---|---|---|---|---|---|---|---|
| Days of Heroin Use | ||||||||
| Detox | 17.7 (10.28) | 17.5 (12.46) | 18.1 (13.48) | 17.4 (12.63) | 18.0 (13.68) | 15.5 (13.43) | 18.4 (12.85) | 12.8 (13.64) |
| Minimal MM | 19.3 (9.50) | 8.0 (6.57) | 5.8 (5.33) | 8.1 (8.55) | 6.3 (7.92) | 6.5 (7.80) | 5.9 (7.69) | 11.3 (12.91) |
| Standard MM | 19.1 (9.84) | 6.1 (8.00) | 4.4 (5.48) | 5.4 (7.03) | 5.9 (7.50) | 4.3 (6.60) | 4.2 (6.67) | 15.2 (13.18) |
| Days of Cocaine Use | ||||||||
| Detox | 5.1 (9.07) | 4.7 (8.60) | 4.0 (8.36) | 4.3 (8.23) | 4.5 (9.03) | 4.6 (8.99) | 4.6 (9.92) | 3.8 (8.59) |
| Minimal MM | 5.5 (8.47) | 5.2 (7.14) | 3.3 (4.34) | 5.7 (9.31) | 4.3 (7.80) | 4.1 (6.12) | 2.2 (3.89) | 3.2 (7.91) |
| Standard MM | 6.2 (9.52) | 4.4 (7.19) | 4.3 (7.00) | 4.4 (7.12) | 5.9 (8.10) | 3.5 (5.93) | 4.0 (6.29) | 4.5 (6.80) |
| Days of Alcohol Use | ||||||||
| Detox | 5.3 (9.40) | 5.1 (9.91) | 5.6 (9.80) | 4.5 (8.89) | 6.4 (11.46) | 5.8 (9.84) | 7.2 (11.15) | 9.1 (12.44) |
| Minimal MM | 5.9 (9.76) | 6.2 (9.39) | 5.9 (8.61) | 6.2 (9.30) | 6.2 (10.12) | 6.9 (10.76) | 6.5 (9.71) | 6.1 (12.01) |
| Standard MM | 7.6 (10.60) | 6.2 (9.49) | 6.5 (8.82) | 7.3 (9.93) | 9.7 (11.71) | 7.9 (10.78) | 8.4 (11.11) | 6.4 (10.35) |
Detox = 21-day methadone detoxification and no maintenance.
Minimal MM = 6-month methadone maintenance with minimal counseling. Standard MM = 6-month methadone maintenance with standard counseling.
Self-reported days of heroin use months 1–6: Minimal MM vs. Detox p = .0003.
Self-reported days of heroin use months 1–8.5: Minimal MM vs. Detox p < .0001.
Self-reported days of alcohol use months 1–6: Minimal MM vs. Detox p = .0192.
Self-reported days of alcohol use months 1–8.5: Minimal MM vs. Detox p = .0065.
No other differences were statistically significant.
Following randomization, participants in the methadone detoxification group continued their 21-day taper, and were allowed to repeat detoxification every 7 weeks. Nevertheless, in months 1 through 6, 78%–96% had opiate positive test results, and they reported heroin use an average of 15.5–18.4 days in each follow-up month. Compared to 21-day methadone detoxification, six-month methadone maintenance with minimal counseling resulted in a greater decrease from baseline in opiate positive urine tests (65%–85%, p = .0302) and self-reported heroin use (mean = 5.8–8.1 days per month, p = .0003) during months 1 through 6. These comparisons remained significant when the month 8.5 follow-up assessment was included (p = .0149 for opiate positive urine tests, p < .0001 for days of heroin use).
Six-month methadone maintenance with minimal counseling differed from 21-day detoxification in one other outcome, days of alcohol use. Compared to 21-day detoxification, six-month methadone maintenance with minimal counseling resulted in a greater decrease from baseline in self-reported days of alcohol use during months 1 through 6 (p = .0192), and this difference remained significant when the month 8.5 follow-up assessment was included (p = .0065). There were no significant differences in cocaine positive urine tests or days of cocaine use.
The standard methadone maintenance group did not differ from the minimal methadone maintenance group on any outcome. There were no statistically or clinically significant differences in opiate positive drug tests (59%–77% opiate positive), self-reported heroin use (mean = 4.2–6.1 days per month), self-reported alcohol use, or self-reported cocaine use during months 1 through 6 or when the month 8.5 follow-up assessment was included.
There were no other differences between the treatment groups on any other outcomes, i.e. there were no differences in BDI or in ASI psychiatric or family composite scores. Given that the only changes were in opiate and alcohol use, no one in the standard methadone maintenance condition achieved both employment and a weekly random test result free of all drugs and alcohol, and thus no one earned the available take-home methadone doses.
Analyses were repeated excluding 6 participants in the 21-day methadone detoxification condition who were able to access methadone maintenance in other programs in the county. Results excluding these patients were the same for all variables. Therefore, all findings were presented for the treatment groups as randomized.
4. Discussion
4.1 Interpretation of Findings
Six-month Methadone Maintenance with Minimal Counseling The present study contributed to the evidence that methadone maintenance with minimal counseling reduces opiate positive urine test results and self-reported days of heroin use. An earlier study compared methadone maintenance with minimal counseling to a no-treatment control over one month of follow-up (Yankovitz et al., 1991). The present study compared it to 21-day methadone detoxification, and extended follow-up to 8.5 months.
Six-month methadone maintenance decreased heroin use more than 21-day methadone detoxification. This effect is consistent with previous research demonstrating less heroin use in methadone maintenance compared to methadone detoxification over 35 days (Strain et al., 1993), 45 days (Vanichseni et al., 1991) or 60 days (Newman and Whitehill, 1979). In this study, however, better outcomes were obtained with methadone maintenance even though it was limited to six months and involved only minimal counseling.
In addition to its effects on heroin use, methadone maintenance with minimal counseling appears to facilitate entry into more comprehensive methadone maintenance if available. A randomized study showed that providing 4 months of methadone maintenance with minimal counseling helped more patients access comprehensive methadone maintenance elsewhere than providing referral only (Schwartz et al., 2006, 2007). At four-month follow-up, 75.9% of the minimal methadone group had been able to access comprehensive methadone maintenance, compared to only 20.8% of the referral-only group, and at ten-month follow-up, 64.8% of the minimal methadone group were in comprehensive methadone maintenance, compared to 27.5% of the referral-only group.
4.2 Interpretation of Findings
Six-month Methadone Maintenance with Standard Counseling In the context of six-month methadone maintenance, standard counseling yielded no improvements over minimal counseling. In contrast, studies of the first six months of long-term methadone maintenance showed that standard counseling yielded fewer opiate positive (McLellan et al., 1993; Saxon et al., 1996) and cocaine positive urine results (McLellan et al., 1993) compared to minimal counseling.
The reduction in both opiate and cocaine positive urine results in the McLellan et al. (1993) study could be in part because of the immediate contingencies in their standard counseling condition. Patients with positive urine drug tests lost take-home doses and were required to participate in increased counseling. In contrast, in the present study, positive urine drug tests triggered only offers of increased services, and none of the participants achieved or lost take-home doses.
The differences in the effects found for counseling could also be due in part to differences in study populations. The heroin users in this study had not sought out methadone maintenance on their own. At baseline, over 85% had opiate positive urine tests, in contrast to less than 65% in McLellan et al. (1993). Early positive urine drug tests predict worse six-month treatment outcome in methadone maintenance (e.g. Morral et al., 1999). Indeed, only 36% of participants stated they wanted to stop using heroin; most were hoping to continue using heroin, but to use less and or use more safely (Batki et al., 2002). This population may benefit from motivational interviewing (Miller and Rollnick, 2002;) or contingency management (Elk et al., 1995).
Although short-term methadone maintenance can serve more patients per treatment slot, it is not as effective as long-term methadone maintenance. In a randomized trial comparing four-month methadone maintenance to ongoing methadone maintenance, heroin use was similar during the first four months while both groups were on maintenance, but then increased in the four-month group during their methadone detoxification in months 5 and 6 (Sees et al., 2000).
4.3 Study Limitations
This study was designed primarily to test the effect of methadone maintenance and directly observed dosing on completion of a six-month course of TB chemoprophylaxis (Batki et al., 2002). As a result, some variables that are relevant to drug treatment outcome were not measured. No data were collected on the duration of and methadone dose during the medical or psychiatric hospitalization preceding outpatient methadone detoxification. There were no measures of counseling session attendance; it is possible that participants in the standard counseling condition did not attend significantly more sessions than those in the minimal counseling condition.
The sample size provided sufficient power to detect medium or larger effect sizes, but not small effect sizes. In addition, the substantial missing drug use data may have reduced power further. Caution must be used in interpreting any lack of difference that may be the result of insufficient power. Also, with the most missing urinalysis data in the methadone detoxification group, and the high likelihood that missing urinalysis results were positive, the difference between methadone detoxification and methadone maintenance outcomes may have been underestimated.
It is possible that the methadone doses at 60–90 mg were too low. Some studies have shown better outcomes with slightly higher doses (e.g. Strain et al., 1999), and many patients may need more than 90 mg to benefit from methadone. However, effective doses have been found to range from 1.5 mg to 191.2 mg and overlap considerably with ineffective dosages (Trafton et al., 2006). In the present study, methadone doses were raised based on clinical need (until withdrawal symptoms and cravings were eliminated, side effects occurred, or participants requested no further increase) up to a maximum of 90 mg because of the six-week taper. Likewise, the other randomized trials of methadone maintenance with minimal counseling also had a target dose of about 80 mg and provided higher or lower doses based on participant needs (Yankovitz et al., 1991; McLellan et al., 1993; Schwartz et al., 2006).
4.4 Conclusions
The findings from this study contribute to the evidence base for short-term methadone maintenance with minimal or standard counseling. Compared to 21-day methadone detoxification, six months of methadone maintenance appears to reduce the frequency of heroin and alcohol use, but not cocaine use. In the first six months of long-term methadone maintenance, standard counseling has been shown to help patients reduce their heroin use more than minimal counseling (McLellan et al., 1993, Saxon et al., 1996). In six-month methadone maintenance, in contrast, heroin use appears to decrease regardless of whether standard or minimal counseling is made available to patients. Incorporating additional interventions used by McLellan et al. (1993), such as requiring more frequent visits after positive drug test results, may increase the impact of standard counseling in six-month methadone maintenance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Amato L, Davoli M, Perucci CA, Ferri M, Faggiano F, Mattick RP. An overview of systematic reviews of the effectiveness of opiate maintenance therapies: Available evidence to inform clinical practice and research. Journal of Substance Abuse Treatment. 2005a;28:321–329. doi: 10.1016/j.jsat.2005.02.007. [DOI] [PubMed] [Google Scholar]
- Amato L, Davoli M, Minozzi S, Ali R, Ferri M. Methadone at tapered doses for the management of opioid withdrawal. Cochrane Database of Systematic Reviews. 2005b;(3) doi: 10.1002/14651858.CD003409.pub3.. Art. No.: CD003409. [DOI] [PubMed] [Google Scholar]
- Amato L, Minozzi S, Davoli M, Vecchi S, Ferri M, Mayet S. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database of Systematic Reviews. 2004;(4) doi: 10.1002/14651858.CD004147.pub2. Art. No.: CD004147. [DOI] [PubMed] [Google Scholar]
- Batki SL, Gruber VA, Bradley JM, Bradley M, Delucchi K. A controlled trial of methadone treatment combined with directly observed isoniazid for tuberculosis prevention in injection drug users. Drug and Alcohol Dependence. 2002;66:283–293. doi: 10.1016/S0376–8716(01)00208-3.. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment. Treatment Improvement Protocol (TIP) Series 43. Rockville, MD, U.S.A: Substance Abuse and Mental Health Services Administration; 2005. Medication-Assisted Treatment for Opioid Addiction in Opioid Treatment Programs. DHHS Publication No. (SMA) 05-4048. [PubMed] [Google Scholar]
- Elk R, Schmitz J, Spiga R, Rhoades H, Andres R, Grabowski J. Behavioral treatment of cocaine-dependent pregnant women and TB-exposed patients. Addictive Behaviors. 1995;20 (4):533–542. doi: 10.1016/0306-4603(94)00076-b. [DOI] [PubMed] [Google Scholar]
- Faggiano F, Vigna-Taglianti F, Versino E, Lemma P. Methadone maintenance at different dosages for opioid dependence. Cochrane Database of Systematic Reviews. 2003;(3) doi: 10.1002/14651858.CD002208. Art. No.: CD002208. [DOI] [PubMed] [Google Scholar]
- Federal Register, Title 21, 1993. Codified at 58 CFR &495, pt 291. U.S.A.
- Gawin FH, Kleber HD. Cocaine abuse treatment: open pilot trial with desipramine and lithium carbonate. Archives of General Psychiatry. 1984;41:903–909. doi: 10.1001/archpsyc.1984.01790200085011. [DOI] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kinber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. The Cochrane database of Systematic Reviews, 2003. 2003;(2) doi: 10.1002/14651858.CD002209.. Art. No.: CD002209. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Alterman AI, Cacciola J, Metzger D, O’Brien CP. A new measure of substance abuse treatment: initial studies of the Treatment Services Review. Journal of Nervous and Mental Disease. 1992a;168:26–38. doi: 10.1016/S0740–5472(03)00106-5. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Arndt IO, Metzger DS, Woody GE, O’Brien CP. The effects of psychosocial services in substance abuse treatment. Journal of the American Medical Association. 1993;269:1953–1959. [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati H, Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992b;9(3):199–213. doi: 10.1016/0740-5472(92)90062-S.. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2. New York: Guilford Press; 2002. [Google Scholar]
- Morral AR, Belding MA, Iguchi MY. Identifying methadone maintenance clients at risk for poor treatment response: pretreatment and early progress indicators. Drug and Alcohol Dependence. 1999;55:25–33. doi: 10.1016/S0376–8716(98)00176-8. [DOI] [PubMed] [Google Scholar]
- Newman G, Whitehill WB. Double-blind comparison of methadone and placebo maintenance treatments of narcotic addicts in Hong Kong. Lancet. 1979;2 (8141):485–488. doi: 10.1016/s0140-6736(79)91550-2. [DOI] [PubMed] [Google Scholar]
- National Institute of Health (NIH) Consensus Development Panel. Effective medical treatment of opiate addiction. Journal of the American Medical Association. 1998;280:1936–1943. [PubMed] [Google Scholar]
- Saxon AJ, Wells EA, Fleming C, Jackson TR, Calsyn DA. Pre-treatment characteristics, program philosophy and level of ancillary services as predictors of methadone maintenance treatment outcome. Addiction. 1996;91:1197–1209. doi: 10.1046/j.1360-0443.1996.918119711.x. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Highfield D, Jaffe JH, Brady JV, Butler CB, Rouse CO, Callaman JM, O’Grady KE, Battjes RJ. A randomized controlled trial of interim methadone maintenance. Archives of General Psychiatry. 2006;63:102–109. doi: 10.1001/archpsyc.63.1.102. [DOI] [PubMed] [Google Scholar]
- Schwartz RP, Jaffe JH, Highfield DA, Callaman JM, O’Grady KE. A randomized controlled trial of interim methadone maintenance: 10-month follow-up. Drug and Alcohol Dependence. 2007;86:30–36. doi: 10.1016/j.drugalcdep.2006.04.017.. [DOI] [PubMed] [Google Scholar]
- Sees KL, Delucchi KL, Masson C, Rosen A, Clark HW, Robillard H, Banys P, Hall SM. Methadone maintenance vs 180-day psychosocially enriched detoxification for treatment of opioid dependence: A randomized controlled trial. Journal of the American Medical Association. 2000;283 (10):1303–1310. doi: 10.1001/jama.283.10.1303. [DOI] [PubMed] [Google Scholar]
- Solberg U, Burkhart G, Nilson M. An overview of opiate substitution treatment in the European Union and Norway. International Journal of Drug Policy. 2002;13:477–484. [Google Scholar]
- Spitzer RI, Williams JBW, First MB. Structured Clinical Interview for DSM-III-R Patient Version. Biometrics Research Department; New York: 1989. [Google Scholar]
- Strain EC, Stitzer ML, Liebson IA, Bigelow GE. Dose-response effects of methadone in the treatment of opioid dependence. Annals of Internal Medicine. 1993;119:23–27. doi: 10.7326/0003-4819-119-1-199307010-00004. [DOI] [PubMed] [Google Scholar]
- Strain EC, Bigelow GE, Liebson IA, Stitzer ML. Moderate- vs. high-dose methadone in the treatment of opioid dependence: A randomized trial. Journal of the American Medical Association. 1999;281:1000–1005. doi: 10.1001/jama.281.11.1000. [DOI] [PubMed] [Google Scholar]
- Trafton JA, Minkel J, Humphreys K. Determining effective methadone doses for individual opioid-dependent patients. Public Library of Science Medicine. 2006;3:e80. doi: 10.1371/journal.pmed.0030080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanichseni S, Wongsuwan B, Choopanya K, Wongpanich K. A controlled trial of methadone maintenance in a population of intravenous drug users in Bangkok: Implications for prevention of HIV. International Journal of the Addictions. 1991;26:1313–1320. doi: 10.3109/10826089109062163. [DOI] [PubMed] [Google Scholar]
- Yancovitz SR, Des Jarlais DC, Peskoe Peyser N, Drew E, Friedmann P, Trigg HL, Robinson JW. A randomized trial of an interim methadone maintenance clinic. American Journal of Public Health. 1991;81:1185–1191. doi: 10.2105/ajph.81.9.1185. [DOI] [PMC free article] [PubMed] [Google Scholar]