Abstract
Brief intervention (BI) research has traditionally examined alcohol and drug use outcomes; however it is unknown whether BIs can also impact on-the-job productivity. This exploratory study examines changes in workplace productivity and related costs for clients receiving a BI for at-risk drinking in the employee assistance program (EAP). Participants were 44 clients attending the EAP for behavioral health concerns, screened for at-risk drinking, assigned to BI+Usual Care (n=25) or UC alone (n=19), and who completed 3-month follow-up. Absenteeism, presenteeism, and productivity costs were derived as outcomes. At follow-up, participants in the BI+UC group had improved productivity when at work (presenteeism) compared to the UC group. The estimated cost savings from improved productivity for the BI+UC group was $1200 per client over the UC group. Groups did not differ by absenteeism (missed days of work). Preliminary evidence suggests the broad impact BIs may have. Implications for future BI research are discussed.
1. Introduction
Employee assistance programs (EAPs) offer short-term counseling and longer-term referrals for a variety of behavioral health concerns such as depression and alcohol problems (Levy Merrick, Volpe-Vartanian, Horgan, & McCann, 2007). EAPs are free and available to about 63% of workplaces with 100+ employees (U.S. Bureau of Labor Statistics, 2006). Services are widespread and can reach individuals of diverse occupations, backgrounds, and income levels. Services are brief, typically four sessions, and include evaluation, brief treatment, and/or outside referral.
Research suggests that EAPs are an underutilized resource for addressing alcohol problems. Between 11 and 35% of the workforce experiences at-risk drinking (Frone, 2006; Mazas et al., 2006; Roche, Pidd, Berry, & Harrison, 2008), which is defined as experiencing non-severe yet substantial alcohol-related problems (Chan, Neighbors, Gilson, Larimer, & Marlatt, 2007; National Institute on Alcohol Abuse and Alcoholism, 2005; Sobell, Sobell, Toneatto, & Leo, 1993; U.S. Preventive Services Task Force, 2004). In the context of the workplace, these individuals may be drinking before or during work, working while intoxicated, or drinking at levels that impact their work productivity. Although EAPs were originally designed to address workplace alcoholism (Roman, 1981; Roman & Blum, 2002), the majority of employees with at-risk drinking are not identified by EAP clinicians or provided services if identified (Chan, Neighbors, & Marlatt, 2004).
Addressing at-risk drinking among employees is important because drinking too much can be associated with worksite problems such as late arrivals, early departures, turnover, co-worker conflict, injuries, absenteeism, and workplace aggression (Mangione et al., 1999; McFarlin & Fals-Stewart, 2002; McFarlin, Fals-Stewart, Major, & Justice, 2001; Osterberg, 2006; Webb et al., 1994), and because at-risk drinking often precedes alcohol abuse and dependence (Institute of Medicine, 1990). Using an EAP to address at-risk drinking may help prevent more serious alcohol consumption and also reduce broader worksite problems.
Alcohol-related consequences are costly to employers and society. Impaired productivity and employment losses are estimated at $93 to $134 billion annually (Burke, 1988; Harwood, 2000; National Institute on Alcohol Abuse and Alcoholism, 2001; Office of National Drug Control Policy, 2001). Direct healthcare costs alone from at-risk drinking are between $26.4 to $35.8 billion per year (Goplerud & Summers, 2005; Harwood, 2000) These estimates do not factor in other costs such as high job turnover rates, coworker conflict, injuries, higher health benefit costs (when the employer subsidizes insurance), and workplace aggression (Mangione et al., 1999; McFarlin & Fals-Stewart, 2002; McFarlin et al., 2001; Webb et al., 1994). Alcohol-related employment problems (e.g., reduced efficiency, premature death, increased unemployment) represent more than 70% of total alcohol costs incurred by workplaces (Harwood, 2000). Targeting preventive services to individuals with at-risk drinking in the worksite may lead to decreases in personal, employer, and societal costs associated with long-term alcohol use disorders and treatment.
Brief interventions (BIs) aim to raise awareness of at-risk drinking and prevent more serious alcohol problems from developing (Substance Abuse and Mental Health Services Administration, 2008). BIs can be delivered in 5–60 minutes in one to five sessions, where clients identified for at-risk behavior are provided normative feedback information, education, skill-building, and practical advice, rather than psychotherapy or other specialized treatment techniques (Babor & Higgins-Biddle, 2000). BIs often utilize a Motivational Interviewing (MI) style (Miller & Rollnick, 2002). MI is a counseling style used to enhance a client’s intrinsic motivation to change by exploring and resolving their ambivalence regarding substance use behavior and desire to change. The style emphasizes a nonconfrontational and nonjudgmental counselor stance, which is contrary to expert or authoritarian styles that serve to confront, educate, and convince clients of the need to change. BIs utilizing MI can stand alone or be used as a prelude if more intensive treatment is warranted.
Substantial evidence supports the effectiveness of BIs in settings such as primary care, trauma centers, and college settings (Bien, Miller, & Tonigan, 1993; Dunn, Deroo, & Rivara, 2001; Fleming et al., 2002; Hettema, Steele, & Miller, 2005; Marlatt et al., 1998). However, only a small number of published studies have examined the efficacy of BIs in worksite settings (Anderson & Larimer, 2002; Osilla, Zellmer, Larimer, Neighbors, & Marlatt, 2008; Webb, Shakeshaft, Sanson-Fisher, & Havard, 2009). Implementing BIs in EAPs or other healthcare settings may be difficult due to barriers at the organizational and clinician level (Watkins, Pincus, Taneilian, & Lloyd, 2003). At the clinician level, insufficient knowledge of the referral process, options for empirically based interventions, discomfort with asking about drinking, time constraints, and lack of screening techniques may all contribute to barriers associated with implementing BIs (Spandorfer, Israel, & Turner, 1999; Adams, Barry, & Fleming, 1996). EAP settings may also face additional barriers specific to the worksite, such as workers’ concerns about confidentiality, time constraints due to work schedules, and stigma associated with obtaining treatment for drinking issues.
In addition to a lack of literature examining BIs in worksite settings, it is also unknown whether BIs, regardless of setting, impact worksite-specific outcomes. Preliminary evidence suggests that a BI in an EAP can efficaciously reduce heavy drinking, peak blood alcohol content, and drinking consequences compared to clients receiving standard EAP care alone (Osilla et al., 2008), but research has yet to determine whether changes in alcohol-specific outcomes correspond with changes in worksite-specific behaviors such as on-the-job productivity. The impact of BIs on such workplace outcomes may provide new and important insights to the broad application of BIs in other domains.
Worksite outcomes describe behaviors that affect on-the-job productivity and also their associated costs incurred as a result of at-risk drinking. Behaviors include performance while at work (presenteeism) and reduced productivity due to being absent from work (absenteeism; Mattke, Balakrishnan, Bergamo, & Newberry, 2007). Presenteeism measures how efficiently and well an individual performs on-the-job (Mattke et al., 2007). For example, someone with low presenteeism may not do work when expected, work as carefully as they should, concentrate as well on their work, and in general have lower work performance than most coworkers. Absenteeism is measured as the amount of time absent from work because of physical or mental health (Kessler et al., 2004). Someone with high absenteeism would have more hours or days missed from work.
The literature on the impact of drinking on productivity is mixed with studies suggesting no relationship (Burton et al., 2005; Serxner, Gold, & Bultman, 2001), a relationship between at-risk drinking and lower presenteeism but not absenteeism (Pelletier, Boles, & Lynch, 2004), and a relationship with at-risk drinking and increased absenteeism (Goplerud & Summers, 2005; McFarlin & Fals-Stewart, 2002; Roche et al., 2008; Upmark, Moller, & Romelsjo, 1999). As argued by Frone (2006), one of the reasons this relationship is unclear is because most studies fail to specifically measure alcohol impairment in the workplace, making it difficult to discern valid and reliable information. Measuring productivity systematically and with psychometrically sound measures aids in understanding how health conditions, such as at-risk drinking, impact worksite outcomes.
By understanding the impact of at-risk drinking on worksite outcomes, associated costs can be calculated to further reflect how these behaviors translate to financial costs to employers and society. For example, several studies have conducted general cost-benefit analyses of BIs in primary care and emergency department settings. These studies have demonstrated that the societal benefits (e.g., reduced alcohol-related accidents and hospital admissions) far outweigh the implementation costs of BIs (Fleming et al., 2000; Fleming et al., 2002; Gentilello, Ebel, Wickizer, Salkever, & Rivara, 2005; Solberg, Maciosek, & Edwards, 2008). However, no studies to our knowledge have documented costs specifically related to worksite outcomes for an employed population (e.g., cost savings from improved on-the-job productivity). Examining worksite outcomes is important because interventions can have broad impacts on mood, work productivity, job retention, and number of hours worked (e.g., Wang et al., 2007). Thus, improved productivity may significantly impact both health and other work outcomes. The current study (1) explores whether a BI provided by EAP counselors to clients with at-risk drinking can decrease worksite outcomes (presenteeism and absenteeism), and (2) provides preliminary estimates of the productivity-related cost savings for clients in the BI condition compared to EAP usual care (UC). The findings in this study are meant to examine whether worksite productivity may be a promising outcome to examine in future BI studies.
2. Methods
2.1. Screening and recruitment
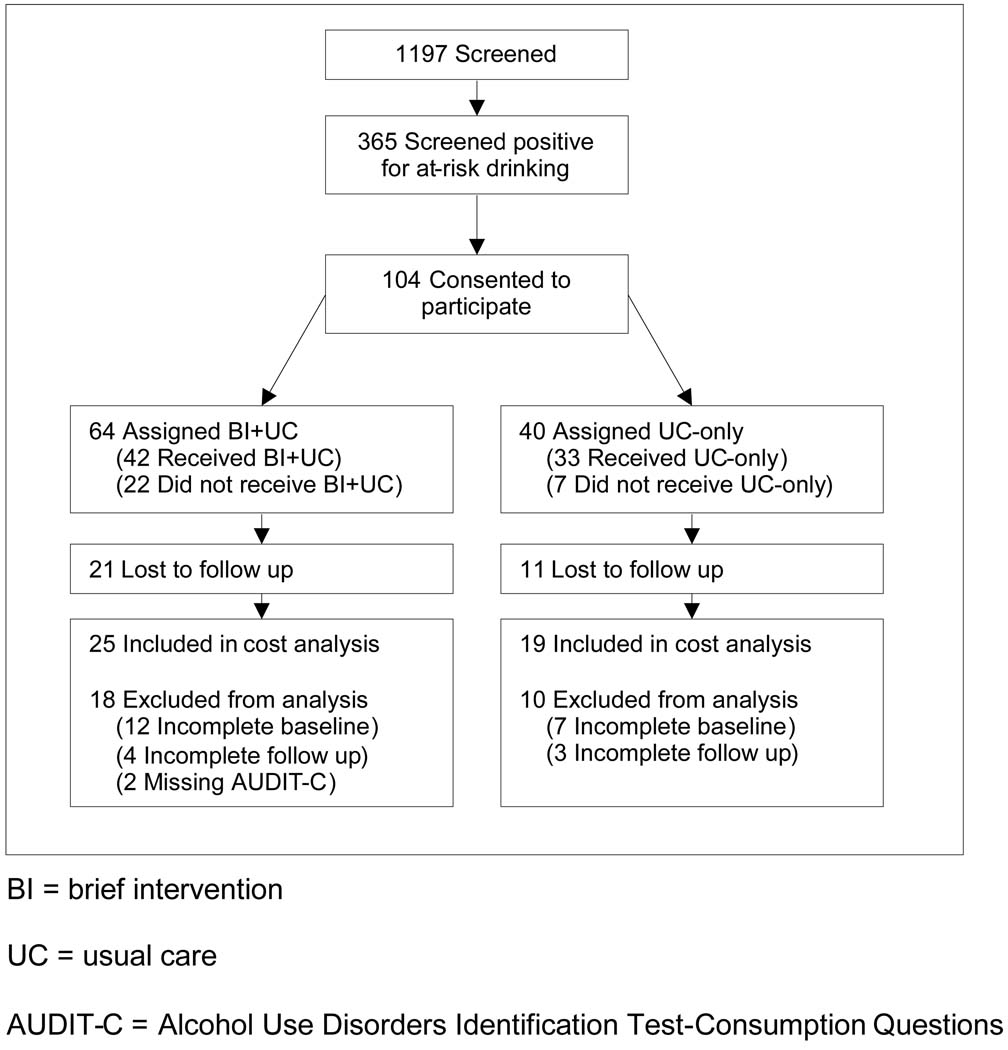
Participants were individuals 18 and older seeking behavioral health services at one of five external EAP offices in three states (see Osilla et al., 2008 for original report). A large EAP corporation that serves over 1,200 employers operated the EAP offices. Before the first EAP appointment, all EAP clients completed a self-report health screen questionnaire, which included questions regarding alcohol consumption from the Alcohol Use Disorders Identification Test-Consumption questions (AUDIT-C; Babor, de la Fuente, Saunders, & Grant, 1992). Clients with AUDIT-C scores greater than or equal to 5 (males) or 3 (female) who were not being seen as a couple or family or because of a work-related mandate were invited to participate in the study (Dawson, Grant, & Stinson, 2005). These cut-off scores represent at-risk drinking criteria defined by the National Institute of Alcohol Abuse and Alcoholism (2005) and the U.S. Department of Health and Human Services (2000). Of the clients screened, about 30% met criteria for at-risk drinking. Figure 1 describes recruitment and attrition of the participants throughout the study. Data were analyzed by group according to an intent-to-treat framework.
Figure 1.
Recruitment and attrition of study subjects
Randomization was conducted at the counselor level rather than the participant level due to EAP organizational policy, client access to services, and reluctance to alter workflows. To create a feasible randomization method, counselors were stratified and randomly assigned to either the BI+UC (intervention) or the UC only (comparison) group. Counselor demographics, EAP experience, substance use, and MI experience were collected after obtaining informed consent (Baer et al., 2004). Counselors were stratified by gender and clinical experience and then randomly assigned to one of the intervention groups by coin toss.
The BI was delivered during the second counseling session. All clients received UC for the first session because clients presented with concerns other than drinking required counselor assessment. During the second session, clients in the intervention group received BI, while clients in the comparison group arm received UC. The BI consisted of personalized feedback, which was derived from the client’s baseline assessment and delivered by counselors using a MI style (Miller & Rollnick, 2002). Feedback was modeled after previous research (Anderson & Larimer, 2002; Marlatt et al., 1998) and included a comparison of drinking rates with U.S. norms (Chan et al., 2007), typical and peak blood alcohol content (BAC), alcohol expectations, high risk drinking situations, and negative drinking consequences. A copy of the feedback, tips to maintain moderation, and a personalized BAC card were given to each client. Six female and three male counselors with an average of 19.83 (SD = 9.79) years of counseling experience delivered the BI or UC.
Clients completed a self-report baseline assessment between their first and second session and a follow-up 3 months after baseline. Additional information about the study is described elsewhere (Osilla et al., 2008). Final analyses included participants who completed all assessments (N=44).
2.2. Participants
Participants were 64% female, 84% Caucasian, and an average of 38 years old (SD = 12.87). Participants earned an average annual salary of $33,700 (before taxes, SD = $15,400) and were employed in diverse occupations such as clerical/administrative (e.g., secretary, billing clerk), service (e.g., security officer, food service worker), and professional (e.g., engineer, accountant) jobs. Table 1 summarizes overall and group-level demographics of the sample.
Table 1.
Sample demographics
| Characteristic | Overall (N=44) |
BI+UC (N=25) |
UC-only (N=19) |
|---|---|---|---|
| Gender (% Female) | 63.64 | 68.00 | 57.89 |
| Age, mean yrs (SD) | 38.05 (12.87) | 37.24 (13.64) | 39.10 (12.07) |
| Ethnicity (%) | |||
| Caucasian | 84.09 | 88.00 | 78.95 |
| Latino/Hispanic | 2.27 | 4.00 | 0.00 |
| African American | 2.27 | 4.00 | 0.00 |
| Multi-Racial | 4.55 | 4.00 | 5.26 |
| Other | 6.82 | 0.00 | 15.79 |
| Annul income, mean, US$, (SD) | $33,659.09 | $32,380.00 | $35,342.11 |
| ($15,463.30) | ($13,361.39) | ($18,109.51) | |
| Education (%) | |||
| Graduated from college | 43.90 | 40.91 | 47.37 |
| Attended some college | 39.02 | 45.45 | 31.58 |
| Did not attend college | 17.07 | 13.64 | 21.05 |
| Occupation (%) | |||
| Executive, administrator, or senior | |||
| Manager | 4.55 | 4.00 | 5.26 |
| Professional | 22.73 | 24.00 | 21.05 |
| Technical support | 15.91 | 20.00 | 10.53 |
| Sales | 4.55 | 8.00 | 0.00 |
| Clerical and administrative support | 22.73 | 28.00 | 15.79 |
| Service occupation | 20.45 | 8.00 | 36.84 |
| Precision production and crafts worker | 0.00 | 0.00 | 0.00 |
| Operator or laborer | 9.09 | 8.00 | 10.53 |
2.3. Measures of productivity and costs
Assessments examined work performance at baseline and 3-month follow-up utilizing sections of the World Health Organization’s Health and Productivity Questionnaire (HPQ; Kessler et al., 2004; Kessler et al., 2003). The HPQ measures efficiency and performance at work (presenteeism) and hours missed from work (absenteeism). Self-report of presenteeism and absenteeism from the HPQ has been well validated against supervisor ratings, peer evaluations, and other metrics of job performance (Kessler et al., 2004; Kessler et al., 2003). These variables are calculated as values of efficiency and missed hours. In addition, ratios can be created comparing an individual’s efficiency and missed hours relative to other workers with a similar job type. The HPQ also measures demographics such as the participant’s self-reported job type and average annual income before taxes.
The HPQ can also be used to calculate cost savings associated with changes in employee productivity. These costs translate to the amount of money employers save or lose when an employee is more or less productive at work (e.g., when an employee is absent from work and a replacement is needed). In the context of BI research, information from the HPQ can provide estimates of the costs and cost savings associated with providing BI to employees with at-risk drinking.
2.3.1. Absenteeism
First, hours missed from work in the past 4 weeks were calculated by subtracting the number of hours participants actually worked in the past 4 weeks from the number of hours their employer expected them to have worked. For example, a typical 40-hour work week would total 160 hours in the past 4 weeks. If a participant worked 100 hours out of an expected 160-hour week, the participant would have missed 60 hours of work in the past 4 weeks. Alternatively, if a participant worked 200 hours out of an expected 160-hour work week, the participant would have worked 40 extra hours in the past 4 weeks (160 minus 200 or −40 hours of work) according to the HPQ scoring system. Second, a ratio representing the percent of work hours missed was calculated by dividing the number of hours missed by the total expected hours of work. For example, if a participant had missed 60 hours of work out of the 160 expected hours, the participant would have missed about 38% of her work hours in the past 4 weeks. However, if a participant worked 40 hours in addition to her 160 expected hours, her ratio of work hours missed would be 125%.
2.3.2. Presenteeism
On-the-job work efficiency/performance in the past 4 weeks was measured on an 11-point scale (0-worst performance to 10-top performance) by asking the participant’s usual performance on the days they worked in the past 4 weeks and the performance of most workers in a job similar to theirs. Consistent with the HPQ scoring instructions (Kessler, Petukhova, McInnes, & Ustun, 2007), these two scores were then multiplied by 10 to yield a presenteeism score between 0 and 100. For example, if a participant scored a 3 on their own performance, their presenteeism score would be 30. A ratio representing the participant’s relative performance compared to most other workers was calculated by dividing the participant’s presenteeism score by the score of most workers. For example, if a participant scored 30 on presenteeism and their rating of most workers was 90, the participant performed at 33% of the level of most workers in a job type similar to hers.
2.3.3. Costs of lost productivity
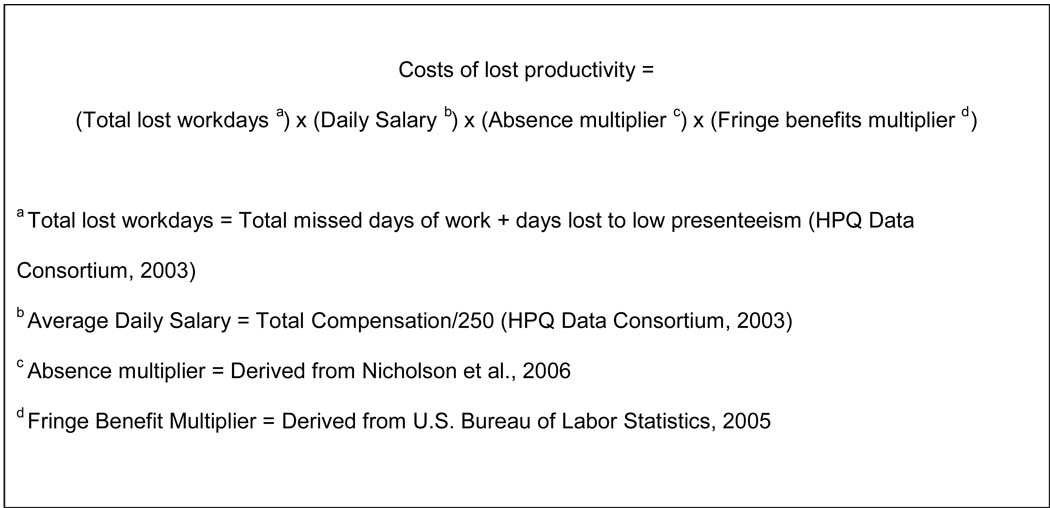
Costs of productivity due to changes in absenteeism and lower presenteeism were monetized by taking the product of total lost workdays, the participant’s average daily salary, a worker absence multiplier, and a fringe benefits multiplier (Loeppke et al., 2007). For interpretation purposes, negative values of cost represent productivity gained (money saved) and positive values of cost represent productivity loss (money lost). Figure 2 summarizes the costs formula and is described briefly below. Total lost workdays was calculated by converting the hours missed from work into total days missed from work, and converting the presenteeism ratio (percent the participant performed at the level of most workers) into the amount of days lost due to low presenteeism (HPQ Data Consortium, 2003). To calculate the latter, the presenteeism ratio was subtracted from 1, then multiplied by the actual days worked in the past 4 weeks (e.g., using the example above, subtracting .33 from 1 and multiplying by the number of days worked (100 hours/8 hours a day = 12.5 days worked), totaling 8.375 days lost due to low presenteeism).
Figure 2.
Cost formula derivation
Worker-absence (Nicholson et al., 2006) and fringe benefit multipliers (U.S. Bureau of Labor Statistics, 2005) were drawn from existing literature to account for how different worker occupations have varying impacts on employers and team production when absent (e.g., absence of a flight attendant or construction worker has a larger impact on employer costs than food service workers). For job categories that did not map onto existing literature, the first and second author independently matched HPQ categories to the existing sources and reached a consensus on discrepancies. For example, the “professional” category in the HPQ was matched to six jobs (Nicholson et al., 2006): Construction engineer; aerospace engineer; mechanical engineer; registered nurse, hospital; registered nurse, hospital operating room; and registered nurse: physician’s office. Taking the average of the worker absence multipliers across the six occupations produced a multiplier of 1.44 for the HPQ “professional” category. Multipliers were interpreted as the percent of the employee’s daily salary incurred by employers when employees are absent (worker-absence multiplier) or when employees receive their fringe benefits (compensation or perks in addition to salary).
2.3.4. Statistical methods
The data were examined for outliers using boxplots and no datapoints were excluded. We used ordinary least squares regression to compare levels of presenteeism and absenteeism in the two groups, controlling for baseline measures of the same variable, to identify significant differences between intervention groups at follow-up. To analyze costs, ordinary least squares regression with bootstrap estimation of standard errors was used to control for baseline differences. Bootstrap estimation was used in order to provide appropriate standard errors with highly skewed costs data. We corrected for clustering of clients within counselors for all outcome measures using Huber-White sandwich estimates and, after correcting, found no substantive differences. Therefore, we present the uncorrected results. Analyses were carried out using Stata 10.0 for Macintosh (StataCorp, 2007).
3. Results
3.1. Sample characteristics
There were no statistically significant differences between eligible clients who consented versus those who did not consent with the exception that eligible male clients consenting to the study drank more and scored about 1 point higher on the AUDIT-C than male clients who did not consent (F (1, 121) = 6.45, p = .012). Eligible men (n=16) scored an average of 7.78 on the AUDIT-C (SD = 2.08) and women (n=28) scored 4.42 (SD = 1.73). Clients who had missing outcomes data were not significantly different in demographics and at-risk drinking scores compared to clients with these data.
Table 1 compares the demographic characteristics of the intervention and comparison groups. There were no statistically significant differences found at baseline. In addition, participants attended an average of three EAP sessions, which did not differ by group (BI+UC: M = 3.08, SD = 1.35; UC: M = 3.17, SD = 1.34). Table 2 presents raw means and standard deviations for the outcome variables, which were later controlled for in all analyses. Regarding baseline values of missed hours by group, consider the range of missed hours possible (−70 hours to 130 hours). In addition, t-tests showed there were no statistically significant differences in outcome measures at baseline between the two groups. Though the raw data seems to show that the UC-only group demonstrates more improved workplace performance at follow-up, variation and differences at baseline make the raw values difficult to interpret. We therefore controlled for baseline values in all analyses.
Table 2.
Raw means of productivity variables at baseline and follow-up
| BI+UC N=25 |
UC N=19 |
|||
|---|---|---|---|---|
| Baseline | 3 mo FU | Baseline | 3 mo FU | |
| Variable a |
M (SD) |
M (SD) |
M (SD) |
M (SD) |
| ABSENTEEISM | ||||
| Hours Missed b | 8.84 (30.76) |
7.88 (23.03) |
24.95 (50.86) |
16.53 (17.10) |
| Ratio of Work Hours Missed | 0.05 (0.19) |
0.05 (0.14) |
0.15 (0.31) |
0.10 (0.11) |
| PRESENTEEISM | ||||
| Work Performance | 71.20 (18.33) |
84.00 (10.11) |
64.74 (22.20) |
73.16 (13.76) |
| Relative Work Performance | 1.03 (0.31) |
1.18 (0.20) |
0.93 (0.39) |
1.00 (0.21) |
| COSTS | ||||
| Costs of lost productivity | −$153.88 ($2,316.76) |
−$888.52 ($1,556.77) |
$1,316.10 ($3,218.04) |
$776.50 ($1,668.17) |
Each variable was assessed in the past 4 weeks from the assessment
Hours missed ranged from −70 (participant worked 70 hours more than expected in 4 weeks) to 130 (participant worked 130 hours less than expected in 4 weeks)
BI = brief intervention
UC = usual care
3.2. Presenteeism and absenteeism
As shown in Table 3, after controlling for variation in baseline levels of presenteeism, participants in the intervention group had increased presenteeism (better on-the-job efficiency/performance) compared to participants in the comparison group at 3-month follow-up. Participants in the intervention group scored 9.51 points greater than the comparison group (p = 0.010; 95% CI [2.43, 16.58]; d = 0.73). In addition, after controlling for baseline presenteeism ratios (participant’s performance relative to other workers), participants in the intervention group reported higher ratios (better on-the-job performance compared to other workers) than the comparison group. The intervention group scored 0.16 points greater than the comparison group (p = 0.011; 95% CI [0.04, 0.29]; d = 0.72). Both of these measures of presenteeism had large effect sizes for the intervention (using the standard definitions provided by Cohen, 1992). The absenteeism variables failed to achieve statistical significance at the conventional 0.05 level, but were in the predicted direction. Participants in the intervention group had about 6 fewer missed hours of work over the comparison group, and with a small effect size of 0.28.
Table 3.
Adjusted productivity variables at follow-up
| Variable | Difference a | Significance | ||||
|---|---|---|---|---|---|---|
| M | SE | p | 95% CI | d | ||
| ABSENTEEISM (past 4 weeks) | ||||||
| Hours Missed | −5.87 | 6.12 | 0.343 | −18.23 | 6.49 | −0.28 |
| Ratio of Work Hours Missed | −0.04 | 0.04 | 0.346 | −0.11 | 0.04 | −0.28 |
| PRESENTEEISM (past 4 weeks) | ||||||
| Work Performance | 9.51 | 3.50 | 0.010 | 2.43 | 16.58 | 0.73 |
| Relative Work Performance | 0.16 | 0.06 | 0.011 | 0.04 | 0.29 | 0.72 |
| COSTS (past 4 weeks) | ||||||
| Costs of lost productivity | −$1,175.82 | $389.49 | 0.003 | −$2,059.69 | −$491.91 | −0.66 |
Difference between BI+UC and UC groups
BI = brief intervention
UC = usual care
3.3. Costs of lost productivity
Costs of productivity were measured at baseline and follow-up. After controlling for variation in baseline costs, the cost differential per participant in the intervention group at follow-up was estimated to be −$1,175.82 (p = 0.003, CI 95% [−$2,059.69, −$491.91], d = .66) over a participant in the comparison group; a medium effect size for this finding. These were costs saved in the intervention condition from improved productivity over the 4-week time period prior to the follow-up assessment.
4. Discussion
The current study explored whether a BI for at-risk drinking can impact broader outcomes such as presenteeism and absenteeism, and the associated productivity cost savings. Preliminary evidence suggests that worksite productivity increases when EAP clients with at-risk drinking receive a one session BI in addition to UC, compared to those who only receive UC, and that the effect sizes are large. Previous research has shown that BIs can decrease drinking behavior at similar effect sizes (Anderson & Larimer, 2002; Dunn et al., 2001; Hettema et al., 2005), but the effect on workplace productivity as an additional outcome has not been previously explored. Measures of productivity are important because lost productivity is costly to employers and evidence that BIs can decrease costs would document a return on investment for employers and help justify wide dissemination. Further, documenting the impacts of improved productivity would be valuable to employers striving to increase job retention, turnover, and the health of their employees.
Consistent with the literature, the increase in productivity comes primarily from increases in presenteeism and not decreases in absenteeism (Goetzel et al., 2004; Hemp, 2004). One hypothesis would be that absenteeism may be a byproduct of more severe drinking consequences not detectable among at-risk drinkers. For example, research suggests that absenteeism increases as alcohol consumption increases (Roche et al., 2008; Upmark et al., 1999). Thus, individuals with clinical diagnoses of alcohol abuse and dependence may be more likely to experience absenteeism. Because this study specifically recruited individuals with at-risk drinking, changes in absenteeism may not have been detectable. Also, our sample size was small, which may affect why differences were not detectable.
The increase in productivity may translate directly into cost savings for employers and EAPs interested in implementing BIs. BIs are inexpensive to deliver (Zarkin, Bray, Davis, Babor, & Higgins-Biddle, 2003) and the benefits far outweigh the costs (Fleming et al., 2000; Fleming et al., 2002; Gentilello et al., 2005; Solberg et al., 2008). Thus, the implementation costs may be negligible compared to the amount saved. In this study, the estimated cost savings from productivity at 3-month follow-up was about $1,200 for each client that attended the one-session intervention. Participants from both groups received the same amount of services and did not differ in the total number of EAP sessions they attended, allowing us to attribute the savings to the intervention because of randomization (Kessler & Stang, 2006).
We conducted an exploratory study to examine whether workplace productivity may be a promising outcome for future BI research. As such, this study has several limitations. First, our small sample size does affect our ability to generalize these findings. While outliers were not noted, samples with fewer participants can be easily influenced by atypical participants than samples with more participants. The generalizability of the results to other EAPs and non-EAP worksite settings is also unknown. Second, randomization occurred at the counselor level, which may impact interpretation of the generalizability of these results. Although the use of an appropriate correction did not substantively alter our results, individually randomized studies at the participant level have greater power to detect effects (Murray, 1998). Third, this study recruited participants from various occupations and while we controlled for baseline variations of absenteeism and presenteeism, these variables may vary by occupation because of policies and workplace norms (e.g., obligation to stay home if ill when working in a medical setting; Lerner & Lee, 2006). Fourth, the long-term sustainability of performance outcomes and cost savings is unknown. The HPQ only assesses the costs of the past 4 weeks at the 3-month follow-up and we do not have data on opportunity costs (e.g., decision to attend the EAP during work hours) and longer-term costs. Thus, it is difficult to know whether costs were saved continuously since baseline. Also, the extent to which those cost savings might be carried forward or invalidated by later events is unknown. Finally, we tested more than one outcome variable, and therefore our type I error rate is potentially inflated. While we considered adjusting for multiple tests, we felt the Bonferroni or Benjamini-Hochberg correction would not be well suited for this exploratory study given the small sample size and the potential to further reduce power. Thus, these findings should be interpreted as preliminary and further research with larger and more diverse samples is encouraged.
Future BI research may consider examining the effects of presenteeism and absenteeism with larger samples (including general work and non-EAP samples) and longer follow-up to assess the longer-term cost savings associated with BIs. These studies may also estimate societal costs associated with improved productivity (e.g., reduced car accidents and rates of alcohol use disorders) and how these costs further offset BI implementation costs (e.g., to evaluate cost-effectiveness). For example, previous cost-benefit analyses examining a BI in primary care and trauma settings (e.g., Fleming et al., 2000; Gentilello et al., 2005) may be applied to BIs with an employed population.
This study demonstrates preliminary evidence of how alcohol-related BIs can significantly impact worksite outcomes. The EAP is an underutilized resource that has great potential for providing screening and BIs for the large proportions of employees that experience at-risk drinking. Utilizing EAPs meets both employer goals to improve productivity and public health goals of curbing alcohol use disorders. BIs are currently among the most highly recommended preventive services in primary care because of significant personal and societal benefits (Solberg et al., 2008) and are equally important as routine care for the worksite. Widely implementing BIs in standard EAP care may have the potential for decreasing the prevalence of alcohol use disorders in the worksite and improving broader outcomes such as worksite productivity.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Adams WL, Barry KL, Fleming MF. Screening for problem drinkers in older primary care patients. Journal of the American Medical Association. 1996;276:1964–1967. [PubMed] [Google Scholar]
- Anderson BK, Larimer ME. Problem drinking and the workplace: An individualized approach to prevention. Psychology of Addictive Behaviors. 2002;16:243–251. [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant MA. AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care. Geneva, Switzerland: World Health Organization; 1992. [Google Scholar]
- Babor TF, Higgins-Biddle JC. Alcohol screening and brief intervention: dissemination strategies for medical practice and public health. Addiction. 2000;95:677–686. doi: 10.1046/j.1360-0443.2000.9556773.x. [DOI] [PubMed] [Google Scholar]
- Baer JS, Rosengren DB, Dunn CW, Wells EA, Ogle RL, Hartzler B. An evaluation of workshop training in motivational interviewing for addiction and mental health clinicians. Drug and Alcohol Dependence. 2004;73:99–106. doi: 10.1016/j.drugalcdep.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Bien TH, Miller WR, Tonigan JS. Brief interventions for alcohol problems. Addiction. 1993;88:315–336. doi: 10.1111/j.1360-0443.1993.tb00820.x. [DOI] [PubMed] [Google Scholar]
- Burke TR. The economic impact of alcohol abuse and alcoholism. Public Health Reports. 1988;103:564–568. [PMC free article] [PubMed] [Google Scholar]
- Burton WN, Chen CY, Conti DJ, Schultz AB, Pransky G, Edington DW. The association of health risks with on-the-job productivity. Journal of Occupational and Environmental Medicine. 2005;47:769–777. doi: 10.1097/01.jom.0000169088.03301.e4. [DOI] [PubMed] [Google Scholar]
- Chan KK, Neighbors C, Gilson M, Larimer ME, Marlatt GA. Epidemiological trends in drinking by age and gender: providing normative feedback to adults. Addictive Behaviors. 2007;32:967–976. doi: 10.1016/j.addbeh.2006.07.003. [DOI] [PubMed] [Google Scholar]
- Chan KK, Neighbors C, Marlatt GA. The effect of referral source for employee assistance programs: Implications for brief interventions for addictive behavior problems. Addictive Behaviors. 2004;29:1883–1887. doi: 10.1016/j.addbeh.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Cohen J. A Power Primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS. The AUDIT-C: screening for alcohol use disorders and risk drinking in the presence of other psychiatric disorders. Comprehensive Psychiatry. 2005;46:405–416. doi: 10.1016/j.comppsych.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: a systematic review. Addiction. 2001;96:1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Benefit-cost analysis of brief physician advice with problem drinkers in primary care settings. Medical Care. 2000;38:7–18. doi: 10.1097/00005650-200001000-00003. [DOI] [PubMed] [Google Scholar]
- Fleming MF, Mundt MP, French MT, Manwell LB, Stauffacher EA, Barry KL. Brief physician advice for problem drinkers: long-term efficacy and benefit-cost analysis. Alcoholism: Clinical and Experimental Research. 2002;26:36–43. [PubMed] [Google Scholar]
- Frone MR. Prevalence and distribution of alcohol use and impairment in the workplace: a US national survey. Journal of Studies on Alcohol. 2006;67:147–156. doi: 10.15288/jsa.2006.67.147. [DOI] [PubMed] [Google Scholar]
- Gentilello LM, Ebel BE, Wickizer TM, Salkever DS, Rivara FP. Alcohol interventions for trauma patients treated in emergency departments and hospitals: a cost benefit analysis. Annals of Surgery. 2005;241:541–550. doi: 10.1097/01.sla.0000157133.80396.1c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting US employers. Journal of Occupational and Environmental Medicine. 2004;46:398–412. doi: 10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- Goplerud E, Summers C. Methods Used by Ensuring Solutions to Calculate Company-Specific Business Costs of Problem Drinking. 2005 Retrieved January 6, 2009 from http://www.alcoholcostcalculator.org/business/about/?page=1.
- Harwood H. Updating Estimates of the Economic Costs of Alcohol Abuse in the United States: Estimates, Update Methods, and Data. Report prepared by The Lewin Group for the National Institute on Alcohol Abuse and Alcoholism. Rockville, MD: National Institutes of Health; 2000. [Google Scholar]
- Hemp P. Presenteeism: at work--but out of it. Harvard Business Review. 2004;82:49–58. 155. [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- HPQ Data Consortium. Health-at-Work Reporting System: Explanation of Concepts and Calculations. 2003 Retrieved June 12, 2008 from http://www.hpq.org/abtcalc.htm.
- Institute of Medicine. Broadening the Base of Treatment for Alcohol Problems: Report of a Study by a Committee of the Institute of Medicine, Division of Mental Health and Behavioral Medicine. Washington, DC: National Academy Press; 1990. [Google Scholar]
- Kessler R, Petukhova M, McInnes K, Ustun TB. HPQ Short Form (Absenteeism and Presenteeism Questions and Scoring Rules) 2007 Retrieved February 29, 2008 from http://www.hcp.med.harvard.edu/hpq/ftpdir/absenteeism%20presenteeism%20scoring%20memo%20050107.pdf.
- Kessler RC, Ames M, Hymel PA, Loeppke R, McKenas DK, Richling DE, et al. Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. Journal of Occupational and Environmental Medicine. 2004;46:S23–S37. doi: 10.1097/01.jom.0000126683.75201.c5. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Barber C, Beck A, Berglund P, Cleary PD, McKenas D, et al. The World Health Organization Health and Work Performance Questionnaire (HPQ) Journal of Occupational and Environmental Medicine. 2003;45:156–174. doi: 10.1097/01.jom.0000052967.43131.51. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Stang PE. Intersecting issues in the evaluation of heatlh and work productivity. In: Kessler RC, Stang PE, editors. Health & work productivity: making the business case for quality health care. Chicago: University of Chicago Press; 2006. pp. 1–28. [Google Scholar]
- Lerner DJ, Lee J. Measuring health-related work productivity with self-reports. In: Kessler RC, Stang PE, editors. Health & work productivity: making the business case for quality health care. Chicago: University of Chicago Press; 2006. pp. 66–87. [Google Scholar]
- Levy Merrick ES, Volpe-Vartanian J, Horgan CM, McCann B. Revisiting employee assistance programs and substance use problems in the workplace: key issues and a research agenda. Psychiatric Services. 2007;58:1262–1264. doi: 10.1176/appi.ps.58.10.1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeppke R, Taitel M, Richling D, Parry T, Kessler RC, Hymel P, et al. Health and productivity as a business strategy. Journal of Occupational and Environmental Medicine. 2007;49:712–721. doi: 10.1097/JOM.0b013e318133a4be. [DOI] [PubMed] [Google Scholar]
- Mangione TW, Howland J, Amick B, Cote J, Lee M, Bell N, et al. Employee drinking practices and work performance. Journal of Studies on Alcohol. 1999;60:261–270. doi: 10.15288/jsa.1999.60.261. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Kivlahan DR, Dimeff LA, Larimer ME, Quigley LA, et al. Screening and brief intervention for high-risk college student drinkers: Results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology. 1998;66:604–615. doi: 10.1037//0022-006x.66.4.604. [DOI] [PubMed] [Google Scholar]
- Mattke S, Balakrishnan A, Bergamo G, Newberry SJ. A review of methods to measure health-related productivity loss. American Journal of Managed Care. 2007;13:211–217. [PubMed] [Google Scholar]
- Mazas CA, Cofta-Woerpel L, Daza P, Fouladi RT, Vidrine JI, Cinciripini PM. At-risk drinking in employed men and women. Annals of Behavioral Medicine. 2006;31:279–287. doi: 10.1207/s15324796abm3103_10. [DOI] [PubMed] [Google Scholar]
- McFarlin SK, Fals-Stewart W. Workplace absenteeism and alcohol use: a sequential analysis. Psychology of Addictive Behaviors. 2002;16:17–21. doi: 10.1037//0893-164x.16.1.17. [DOI] [PubMed] [Google Scholar]
- McFarlin SK, Fals-Stewart W, Major DA, Justice EM. Alcohol use and workplace aggression: an examination of perpetration and victimization. Journal of Substance Abuse. 2001;13:303–321. doi: 10.1016/s0899-3289(01)00080-3. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. New York, NY: Guilford Press; 2002. [Google Scholar]
- Murray DM. Design and Analysis of Group-Randomized Trials. Oxford: Oxford University Press; 1998. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Economic perspectives in alcoholism research. Alcohol Alert. 2001;51:1–4. [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism. Helping Patients Who Drink Too Much: A Clinician's Guide. Rockville, MD: National Institute on Alcohol Abuse and Alcoholism; 2005. [Google Scholar]
- Nicholson S, Pauly MV, Polsky D, Sharda C, Szrek H, Berger ML. Measuring the effects of work loss on productivity with team production. Health Economics. 2006;15:111–123. doi: 10.1002/hec.1052. [DOI] [PubMed] [Google Scholar]
- Office of National Drug Control Policy. The economic costs of drug abuse in the United States, 1992–1998. Washington, DC: Executive Office of the President; 2001. [Google Scholar]
- Osilla KC, Zellmer SP, Larimer ME, Neighbors C, Marlatt GA. A brief intervention for at-risk drinking in an employee assistance program. Journal of Studies on Alcohol and Drugs. 2008;69:14–20. doi: 10.15288/jsad.2008.69.14. [DOI] [PubMed] [Google Scholar]
- Osterberg E. Sickness absence as an alcohol-related problem. Addiction. 2006;101:1378–1379. doi: 10.1111/j.1360-0443.2006.01643.x. [DOI] [PubMed] [Google Scholar]
- Pelletier B, Boles M, Lynch W. Change in health risks and work productivity over time. Journal of Occupational and Environmental Medicine. 2004;46:746–754. doi: 10.1097/01.jom.0000131920.74668.e1. [DOI] [PubMed] [Google Scholar]
- Roche AM, Pidd K, Berry JG, Harrison JE. Workers' drinking patterns: the impact on absenteeism in the Australian work-place. Addiction. 2008;103:738–748. doi: 10.1111/j.1360-0443.2008.02154.x. [DOI] [PubMed] [Google Scholar]
- Roman PM. From employee alcoholism to employee assistance. Deemphases on prevention and alcohol problems in work-based programs. Journal of Studies on Alcohol. 1981;42:244–272. doi: 10.15288/jsa.1981.42.244. [DOI] [PubMed] [Google Scholar]
- Roman PM, Blum TC. The workplace and alcohol problem prevention. Alcohol Res Health. 2002;26:49–57. [PMC free article] [PubMed] [Google Scholar]
- Serxner SA, Gold DB, Bultman KK. The impact of behavioral health risks on worker absenteeism. Journal of Occupational and Environmental Medicine. 2001;43:347–354. doi: 10.1097/00043764-200104000-00010. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Toneatto T, Leo GI. What triggers the resolution of alcohol problems without treatment? Alcoholism: Clinical and Experimental Research. 1993;17:217–224. doi: 10.1111/j.1530-0277.1993.tb00752.x. [DOI] [PubMed] [Google Scholar]
- Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse: ranking its health impact and cost effectiveness. American Journal of Preventive Medicine. 2008;34:143–152. doi: 10.1016/j.amepre.2007.09.035. e143. [DOI] [PubMed] [Google Scholar]
- Spandorfer JM, Israel Y, Turner BJ. Primary care physicians' views on screening and management of alcohol abuse: Inconsistencies with national guidelines. The Journal of Family Practice. 1999;48:899–902. [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 10. College Station, TX: StataCorp LP; 2007. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Screening, Brief Intervention, and Referral to Treatment (SBIRT): Core Components: Brief Intervention. 2008 Retrieved January 12, 2009 from http://sbirt.samhsa.gov/core_comp/brief_int.htm.
- U.S. Bureau of Labor Statistics. Employer Costs for Employee Compensation [statistics] 2005 Retrieved January 7, 2009 from http://data.bls.gov/PDQ/outside.jsp?survey=cm.
- U.S. Bureau of Labor Statistics. National Compensation Survey: Employee Benefits in Private Industry in the United States, March 2006, Summary. Washington, DC: US Department of Labor, Bureau of Labor Statistics; 2006. [Google Scholar]
- U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration 1998 National Household Survey on Drug Abuse. Rockville, MD: SAMHSA; 2000. [Google Scholar]
- U.S. Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Annals of Internal Medicine. 2004;140:554–556. doi: 10.7326/0003-4819-140-7-200404060-00016. [DOI] [PubMed] [Google Scholar]
- Upmark M, Moller J, Romelsjo A. Longitudinal, population-based study of self reported alcohol habits, high levels of sickness absence, and disability pensions. Journal of Epidemiology and Community Health. 1999;53:223–229. doi: 10.1136/jech.53.4.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Simon GE, Avorn J, Azocar F, Ludman EJ, McCulloch J, et al. Telephone Screening, Outreach, and Care Management for Depressed Workers and Impact on Clinical and Work Productivity Outcomes: A Randomized Controlled Trial. JAMA. 2007;298:1401–1411. doi: 10.1001/jama.298.12.1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins KE, Pincus HA, Taneilian TL, Lloyd J. Using the chronic care model to improve treatment of alcohol use disorders in primary care settings. Journal of Studies on Alcohol. 2003;64:209–218. doi: 10.15288/jsa.2003.64.209. [DOI] [PubMed] [Google Scholar]
- Webb G, Shakeshaft A, Sanson-Fisher R, Havard A. A systematic review of work-place interventions for alcohol-related problems. Addiction. 2009;104:365–377. doi: 10.1111/j.1360-0443.2008.02472.x. [DOI] [PubMed] [Google Scholar]
- Webb GR, Redman S, Hennrikus DJ, Kelman GR, Gibberd R, Sanson-Fisher R. The relationships between high-risk and problem drinking and the occurrence of work injuries and related absences. Journal of Studies on Alcohol. 1994;55:434–446. doi: 10.15288/jsa.1994.55.434. [DOI] [PubMed] [Google Scholar]
- Zarkin GA, Bray JW, Davis KL, Babor TF, Higgins-Biddle JC. The costs of screening and brief intervention for risky alcohol use. Journal of Studies on Alcohol. 2003;64:849–857. doi: 10.15288/jsa.2003.64.849. [DOI] [PubMed] [Google Scholar]