SYNOPSIS
Objective
U.S. women experience high rates of unplanned pregnancy and sexually transmitted infections (STIs), yet they seldom combine condoms with highly effective contraceptives for optimal protection. Because oral contraceptives (OCs) have been the predominant form of highly effective contraception in the U.S., it is unknown whether condom use is similarly low with increasingly promoted user-independent methods.
Methods
We used weighted data from the National Survey of Family Growth to assess condom use odds among women relying on OCs vs. user-independent methods (i.e., injectibles, intrauterine devices, and implants). We also estimated the expected reduction in unplanned pregnancies and abortions if half or all of the women currently using a single highly effective method also used condoms.
Results
Across every demographic subgroup based on age, partner status, race/ethnicity, household income, and education, condom use prevalence was lower for women relying on user-independent methods vs. OCs. Multivariable models for adult women also revealed a significant reduction within most demographic subgroups in the odds of condom use among women relying on user-independent methods vs. OCs. Population estimates suggested that if half of all women using highly effective methods alone also used condoms, approximately 40% of unplanned pregnancies and abortions among these women could be prevented, for an annual reduction of 393,000 unplanned pregnancies and nearly 76,000 abortions. If all highly effective method users also used condoms, approximately 80% of unplanned pregnancies and abortions among these women could be prevented, for an annual reduction of 786,000 unplanned pregnancies and nearly 152,000 abortions.
Conclusions
Adding condoms to other methods should be considered seriously as the first line of defense against unplanned pregnancy and STIs. This analysis can serve to target interventions where dual-method promotion is needed most.
National estimates leading back to 1982 indicate that more women in the U.S. have depended on oral contraceptives (OCs) than any other form of reversible birth control.1 While few women taking OCs correctly and consistently can expect to become pregnant during a 12-month period (0.3%), this value is much higher with typical use (8.7%)2 and may contribute to the high unplanned pregnancy rates in the U.S.3 Because differences in pregnancy rates with typical and perfect use are smaller for user-independent methods that do not require women to act daily (e.g., injectibles, intrauterine devices [IUDs], and implants),2,4 these methods have been promoted as one way to prevent unplanned pregnancies.2,5,6
While user-independent methods reduce the risk of unplanned pregnancy, they offer no protection against sexually transmitted infections (STIs), including human immunodeficiency virus/acquired immunodeficiency syndrome. Therefore, women at risk for STIs need to use condoms, but condoms by themselves are less effective for pregnancy prevention than OCs or user-independent methods.2,4 While combining condoms with a second contraceptive method for STI protection may be seen to acknowledge the potential for infidelity and distrust within a relationship,7–9 dual-method use also may be promoted for the dramatic reduction in the risk of unplanned pregnancy that can be achieved by combining a systemic and a barrier method.10,11 Women experiencing difficulty negotiating condom use within the context of relationships they suspect may not be mutually monogamous can be counseled to emphasize the contraceptive benefits of dual-method use while also taking advantage of the benefits of STI protection.
Although there has been a slight increase in the use of condoms for dual protection in the past two decades,12–15 some research suggests that women relying on user-independent methods may be less likely than those using OCs to seek the added protection of condoms.16–19 However, other studies have found no difference in condom use across method type.20–22 Because women using OCs currently account for a large majority of those relying on highly effective reversible birth control methods,23 it will be important to monitor condom use patterns as user-independent methods increasingly are adopted.
We tested the hypothesis that the odds of condom use would be lower among women relying on user-independent methods as compared with OCs. We also estimated how many unplanned pregnancies and abortions could be prevented if half or all of the women relying on highly effective methods alone also used condoms. By using nationally representative data from the National Survey of Family Growth (NSFG), we moved beyond prior studies focusing on specific high-risk populations. In doing so, we controlled for a number of demographic variables and identified groups in which the need to promote condoms for dual protection is greatest.
METHODS
Data source
We used data from cycle six of the NSFG. Since 1973, the NSFG has been a principal source of information on factors affecting pregnancy and birth rates. It includes comprehensive data on sexual activity and contraceptive use and is based on a stratified, multistage probability sample that is nationally representative of households and eligible people in the 50 states and the District of Columbia. For cycle six of this periodic survey, 7,643 women aged 15–44 years were interviewed from March 2002 to February 2003 for a final response rate of 80%.24
Inclusion criteria, and definitions of exposure and outcome
We included women who reported having used a highly effective contraceptive method during the month of their interview or at their last intercourse in the past three months. Highly effective methods included OCs, contraceptive patches, injectibles (i.e., Depo-Provera® or Lunelle®), IUDs (including coils and loops), and Norplant®. No women reported using contraceptive rings.
Our primary exposure variable was the type of highly effective method chosen; our outcome measure was whether or not a condom also had been used. For each woman, we used two series of NSFG variables to define contraceptive use: one that enumerated the four most effective methods used at the last intercourse in the past three months, and another that enumerated the four most effective methods used during the interview month. For the second variable series, we excluded women who had not had intercourse in the past three months. Additionally, because several prior studies have examined the association between sterility and condom use,25–27 and because our objective was to look at condom use patterns among women relying on increasingly promoted user-independent methods vs. OCs, we excluded women who were sterile or dependent upon their partner's sterility. Because very few women meeting our inclusion criteria used contraceptive patches (26 during the interview month and 23 at last intercourse) or Norplant (16 during the interview month and 15 at last intercourse), we placed these respondents in the same categories as women using OCs (for contraceptive patch users) or IUDs (for Norplant users). We considered all methods other than OCs/contraceptive patches to be user-independent.
Covariates
Covariates included age (15–19, 20–24, and ≥25 years), partner status during the past year (married, one partner; single, one partner; and multiple partners), race/ethnicity (Hispanic, non-Hispanic white [NH-white], and non-Hispanic black [NH-black]), household income relative to the federal poverty level (FPL) (0%–199% FPL and ≥200% FPL), and education (no high school diploma vs. ≥high school graduate).
Analysis
We used two series of logistic regression models—one based on the methods used during the interview month and another based on the methods used at the last intercourse in the past three months—to assess condom use odds. After generating weighted sample estimates of the proportion of women using condoms with OCs and with user-independent methods, we calculated crude odds ratios [ORs] to assess unadjusted condom use odds by method type. Next, for adult women aged 20–44 years, we constructed multivariable models to assess adjusted condom use odds; because many women aged 15–19 years had not had the opportunity to finish high school, we excluded them from these adjusted models to allow education to be included as a covariate. With these multivariable models, we first calculated condom use odds, adjusted for demographic variables, among women using OCs and among women relying on user-independent methods. We then constructed further models to assess adjusted condom use odds for women relying on user-independent methods vs. OCs. For these models, we initially entered all our demographic variables along with their two-way interaction with highly effective method type. We then used a backwards elimination procedure to delete interaction terms sequentially, until only those reaching significance at the p<0.05 level remained. Once we had excluded nonsignificant interaction terms, we considered a series of models with all possible combinations of demographic variables as confounders. Among those models generating ORs for condom use within 10.0% of the value obtained with the complete set of confounders, we selected the one with the narrowest confidence interval (CI).28
In addition to assessing condom use odds, we estimated the number of unplanned pregnancies and abortions that could be avoided if half or if all of the women currently using highly effective contraceptive methods alone also used condoms. For this calculation, we used estimated annual pregnancy rates by Kost et al.2 for women using condoms (17.4%), OCs (8.7%), and injectibles (6.7%). These estimates are based on normal use of contraceptive methods (i.e., use effectiveness taking into account forgetting pills, condom breakage, or retuning late for an injection) rather than perfect use. For women using condoms with OCs or injectibles, we then took the product of the probability of pregnancy with each of the individual methods. However, because the estimates by Kost et al. included women using OCs and injectibles with and without condoms, we weighted the contribution of single- and dual-method users to these estimates according to the contraceptive use patterns we derived from the methods used during the interview month. With this weighting, we calculated a 12-month pregnancy rate of 10.0% and 7.4%, respectively, for women using OCs and injectibles alone, and 1.7% and 1.3%, respectively, for women using OCs and injectibles with condoms.
For estimates of annual expected pregnancy rates among women using IUDs/Norplant, we used the mean of the values Trussell4 reports from his review for the two IUDs (Paragard® and Mirena®) and the one implant (Implanon®) currently marketed in the U.S. (0.5%). Taking the joint probability of pregnancy, we calculated a final 12-month rate of 0.1% for women using these methods in conjunction with condoms.
To estimate the number of unplanned pregnancies potentially avoided, we took weighted estimates of the total number of unplanned pregnancies expected with current contraceptive use patterns, and then subtracted estimates of the number of unplanned pregnancies expected if half or all of the women currently using a single highly effective method also used condoms. To determine the prevented fraction of unplanned pregnancies, we used the following formula:
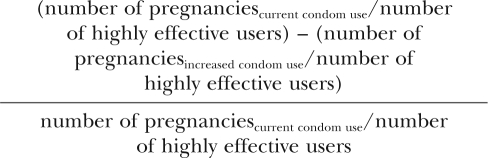 |
To calculate the number of abortions potentially avoided, we used published estimates from 2001 that 1.3 million women obtained an abortion3,29 and that 14.6% of these women had been using a highly effective method.29 Using these values to determine the number of highly effective method users who sought an abortion, we then multiplied the result by our calculated prevented fraction of unplanned pregnancies to obtain our final estimate of abortions prevented.
Emory University's Institutional Review Board reviewed this analysis. Because the data were from a public use dataset and had been carefully de-identified, this study was determined not to involve human subjects research requiring informed consent. Analyses were completed with SAS® version 9.2, allowing for a complex weighted sample design.30
RESULTS
Sample description
Of the 7,643 women participating in cycle six of the NSFG, 1,927 used a highly effective method during their interview month; after exclusions for sterility (n=44) and lack of intercourse (n=322), 1,561 women were included in the final analysis. A total of 1,596 women reported using a highly effective method at their last intercourse in the past three months; after exclusions for sterility (n=44), 1,552 women were included in the final analysis. For both measures, our sample represented an estimated 12.4 million women, of whom approximately 80% used OCs, 14% used injectibles, and 6% used IUDs/Norplant (interview month—OCs: 79.7% [95% CI 77.5, 81.8], injectibles: 13.9% [95% CI 12.1, 15.7], and IUDs/Norplant: 6.4% [95% CI 5.0, 7.8]; last intercourse—OCs: 80.0% [95% CI 77.8, 82.3], injectibles: 13.6% [95% CI 11.7, 15.6], and IUDs/Norplant: 6.3% [95% CI 4.8, 7.9]).
Trends in condom use for dual protection
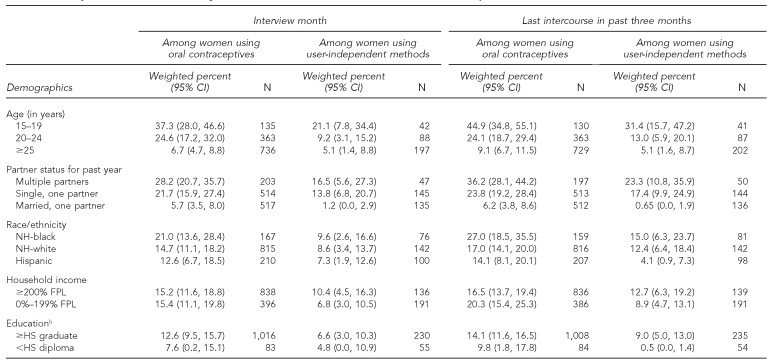
Both as measured by method use during the interview month and by method use at the last intercourse in the past three months, the proportion of women using condoms was highest for OC users (interview month—17.6% [95% CI 15.1, 20.1]; last intercourse—15.2% [95% CI 12.4, 18.1]), intermediate for injectible users (interview month—14.5% [95% CI 9.3, 19.7]; last intercourse—11.3% [95% CI 6.6, 16.1]), and lowest for IUD/implant users (interview month—1.8% [95% CI 0.0, 4.0]; last intercourse—1.9% [95% CI 0.0, 4.0]). Across every subgroup based on age, partner status, race/ethnicity, household income, and education, the proportion of women using condoms was higher among those using OCs vs. user-independent methods (Table 1). Both with OCs and with user-independent methods, condom use generally decreased with age and increased from married women with one partner to women with multiple partners. However, depending on the measure of contraceptive use implemented, only 16.5% to 36.2% of women with multiple partners used condoms. Condom use generally was higher among NH-black women and lower among women without a high school education.
Table 1.
Percentage of women aged 15–44 years using a condom in conjunction with a highly effective contraceptive method, as measured by the method used during the interview month and at last intercourse in the past three monthsa
aWomen were selected for interview in the National Survey of Family Growth based on a nationally representative multistage probability sample of households and eligible people in the 50 states and the District of Columbia. Interviews took place from March 2002 to February 2003.
bExcludes women aged 19 years and younger
CI = confidence interval
NH = non-Hispanic
FPL = federal poverty level
HS = high school
Regression models
Crude association of condom use with method type.
Compared with women using OCs, crude condom use odds were not reduced among women using injectibles (interview month—OR=0.71, 95% CI 0.42, 1.20; last intercourse—OR=0.80, 95% CI 0.51, 1.25). However, the crude odds of condom use were reduced in the group of women using IUDs/Norplant (interview month—OR=0.11, 95% CI 0.03, 0.36; last intercourse—OR=0.09, 95% CI 0.03, 0.30) and in the group of women relying on all user-independent methods combined (interview month—OR=0.51, 95% CI 0.31, 0.83; last intercourse—OR=0.55, 95% CI 0.36, 0.85).
Association of condom use with demographic variables
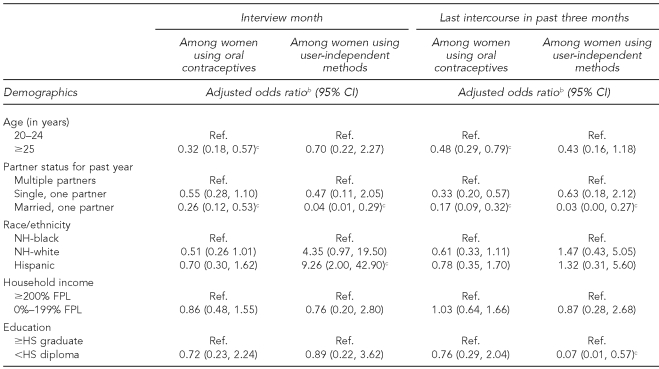
Among adult women, both measures of contraceptive use indicated that condom use odds were lower among older women using OCs, and among married women relying either on OCs or user-independent methods ( Table 2). However, for race/ethnicity and education, the relative odds of condom use among women relying on user-independent methods depended on the measure used for analysis. Condom use odds were higher in Hispanic women when assessed by methods used in the interview month. By contrast, condom use odds were lower in women without a high school education when assessed by method use at the last intercourse in the past three months.
Table 2.
Odds of condom use in conjunction with a highly effective contraceptive method among women aged 20–44 years, adjusted for age, partner status, race/ethnicity, household income, and educationa
aWomen were selected for interview in the National Survey of Family Growth based on a nationally representative multistage probability sample of households and eligible people in the 50 states and the District of Columbia. Interviews took place from March 2002 to February 2003.
bOdds ratios presented by each demographic variable (age, partner status, race/ethnicity, household income, and education) are adjusted for the remaining demographic variables.
cStatistically significant at p<0.05
CI = confidence interval
Ref. = referent group
NH = non-Hispanic
FPL = federal poverty level
HS = high school
Adjusted association of condom use with method type
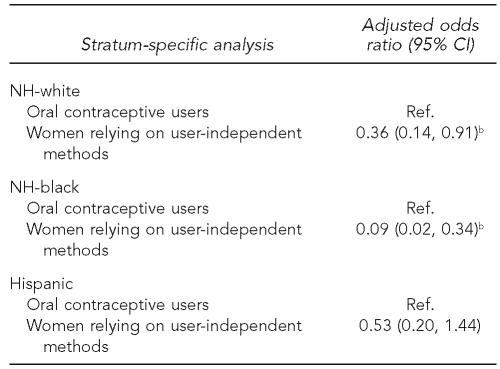
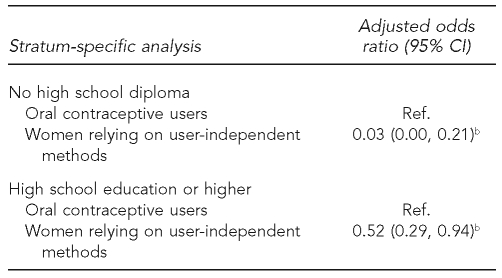
In adjusted models based on method use during the interview month, race/ethnicity modified the association between condom use and highly effective method type (p=0.036). Among NH-white women, condom use odds were reduced among those relying on user-independent methods vs. OCs. Among NH-black women, the odds of condom use with user-independent methods vs. OCs were even lower, but among Hispanic women, method type was not significantly associated with the use of condoms ( Table 3). In adjusted models based on method use at the last intercourse in the past three months, education modified the association between condom use and highly effective method type (p=0.024). Among women with a high school education, condom use odds were reduced among those relying on user-independent methods vs. OCs; among women who did not have a high school education, the odds of condom use with user-independent methods vs. OCs were even lower ( Table 4).
Table 3.
Adjusted odds of condom use among adult women relying on user-independent contraceptive methods as compared with oral contraceptives during the month of interview, stratified by race/ethnicitya
aWomen were selected for interview in the National Survey of Family Growth based on a nationally representative multistage probability sample of households and eligible people in the 50 states and the District of Columbia. Interviews took place from March 2002 to February 2003.
bStatistically significant at p<0.05
CI = confidence interval
NH = non-Hispanic
Ref. = referent group
Table 4.
Adjusted odds of condom use among adult women relying on user-independent contraceptive methods as compared with oral contraceptives at last intercourse in the past three months, stratified by educational statusa
aWomen were selected for interview in the National Survey of Family Growth based on a nationally representative multistage probability sample of households and eligible people in the 50 states and the District of Columbia. Interviews took place from March 2002 to February 2003.
bStatistically significant at p<0.05
CI = confidence interval
Ref. = referent group
Potential reduction in unplanned pregnancies and abortions
Based on current contraceptive use patterns, about 982,000 women using a highly effective method can expect an unplanned pregnancy each year. Of these pregnancies, 862,000 are expected among OC users, 116,000 are expected among injectible users, and 4,000 are expected among women using IUDs/implants. If half of all women using highly effective methods alone also used condoms, an estimated 393,000 (40%) of the unplanned pregnancies among these women could be prevented. With this reduction, the total annual number of unplanned pregnancies in the U.S. would decline 13%, from 3.1 million3 to 2.7 million. A 40% reduction in unplanned pregnancies among these women also would result in an annual reduction of nearly 76,000 abortions. With this reduction, the total annual number of abortions in the U.S. would decline 6%, from 1.3 million29 to 1.2 million.
If all of the women using highly effective methods also used condoms, an estimated 786,000 (80%) of the unplanned pregnancies among these women could be prevented. With this reduction, the estimated total annual number of unplanned pregnancies in the U.S. would decline 25%, from 3.1 million3 to 2.3 million. An 80% reduction in unplanned pregnancies among these women also would result in an annual reduction of nearly 152,000 abortions. With this reduction, the total annual number of abortions in the U.S. would decline 12%, from 1.3 million29 to 1.1 million.
DISCUSSION
This analysis adds support to prior studies suggesting that women using highly effective birth control methods other than OCs may be less likely to seek the added protection of condoms.16–19 Thus, in conjunction with prior research, our analysis suggests that advocating the use of contraceptive methods that have low typical-use failure rates requires simultaneous emphasis on the importance and benefits of combining these methods with condoms. By using a nationally representative sample and controlling for demographic variables, we move beyond prior analyses in identifying populations for which this message might be particularly important. Indeed, depending on the measure implemented to assess contraceptive use patterns, our analysis suggests that among NH-black women and women without a high school diploma, condom use may be especially low for those relying on user-independent methods as compared with OCs.
Our findings also illustrate that numerous women are placing themselves at risk for STIs and unplanned pregnancies that could be avoided. Although condom use odds by partner status were highest for women with multiple partners, the proportion of these women at risk for STIs who used a condom in conjunction with their highly effective method was quite low (16.5% to 36.2%). In addition, based on current contraceptive use patterns, we estimated that each year, approximately 982,000 U.S. women using a highly effective method can expect an unplanned pregnancy. Nearly 190,000 of these women may choose to have an abortion. If anywhere from half to all of the women using highly effective methods alone also used condoms, unplanned pregnancies and abortions among these women potentially could be reduced by about 40% to 80%.
The large reduction in unplanned pregnancies and abortions also provides a rationale that may be much easier for women to use than STI avoidance when negotiating condom use. Women having difficulty negotiating condom use within relationships that may not be mutually monogamous should therefore be counseled to emphasize the contraceptive benefits of dual-method use, while also taking advantage of the benefits of STI protection. Additionally, women in mutually monogamous relationships who are switching to OCs or injectibles should be counseled that they can maximize protection against unplanned pregnancy by continuing their use of condoms.
Despite the benefits of combining condoms with a second method, this is not the optimal solution for all women. Very few women (0.5%) can expect to become pregnant during a 12-month period using IUDs or implants. This percentage is even lower than for the combined use of condoms with OCs or injectibles (1.3% to 1.7%). Thus, for women in a mutually monogamous relationship, the use of an IUD or implant alone may be preferable. On the other hand, women who perceive substantial barriers to actively planning their pregnancies may wish to use condoms alone. Women who perceive such barriers often choose less-effective methods, and may report that a pregnancy resulting from contraceptive failure was in fact intended, or at least welcomed.31 Nonetheless, in other cases, the use of less effective methods is not a means to avoid active planning. For instance, compared with mainstream Protestant women, Catholic women are more likely to use coital avoidance methods,32 but they also have comparatively high abortion rates.33 Given the numerous documented advantages of planned pregnancies, we must improve our understanding of the processes women use to make family planning decisions and when the selection of a less effective method might be most appropriate.
While using condoms for dual protection may not be optimal for all women, promoting this practice among women for whom it is appropriate has the potential to result in substantial cost savings. Adding condoms to a more highly effective method does require additional spending for a second method. However, in contrast with implants and IUDs, which often are not provided because of high upfront costs, male condoms, OCs, and injectibles are comparatively inexpensive and are provided by virtually all publicly funded family planning clinics.34,35 Thus, combining condoms with OCs and injectibles has the potential to prevent many unplanned pregnancies while imposing small additional costs. Given estimates that every dollar invested in helping women avoid unwanted pregnancies saves $4.02 in Medicaid expenditures that otherwise would have been needed for pregnancy-related care,34 a simple intervention such as this could result in enormous cost savings.
Given the potential benefits of dual-method use with condoms, more research is needed to better understand how we can most effectively promote the use of condoms with a second, more highly effective contraceptive method. Promoting dual-method use will require that we overcome unique barriers, including: the desire to not worry about contraception at each act of intercourse that may motivate women to switch to another method; inconsistent condom use or abandonment of condoms with the adoption of a second, more highly effective contraceptive method;36 the need to simultaneously address two unrelated decision processes for women with committed and casual partners;36–38 and the negative association of condoms as a method for preventing STIs that acknowledges the potential for infidelity and distrust within a relationship.7–9 One suggestion for promoting dual-method use has been to implement targeted interventions that assess individual perceptions of unplanned pregnancy and STI risks within the contexts in which women are making contraceptive decisions.36,39 However, while this type of intervention has promoted faster self-reported initiation of dual-method use, it has yet to have an effect on unplanned pregnancy rates or the acquisition of STIs.40 Interventions focusing on men also need to be explored, given that having a male partner with a positive attitude about condoms is one of the strongest predictors of dual-method use.21,41
Limitations
While our study illustrates the importance of advocating dual-method use with condoms and identifies groups in which the need for monitoring and intervention is greatest, our analysis had several limitations. Foremost, both of our outcome measures had certain weaknesses. One advantage of using the methods that women relied upon at their last intercourse is that the probability that a woman would have been classified as a condom user would have been proportional to the consistency of her condom use. Nonetheless, this measure reflects a single act of intercourse and indicates nothing about the diversity of contraceptive use patterns that women may have with different partners. In particular, women with multiple partners may be more likely to use condoms in secondary or casual relationships, but condom use in this context would have been missed for women who last had intercourse with their primary, committed partner. On the other hand, while enumerating the methods used during the interview month provides a more comprehensive measure of contraceptive choice, our analysis based on this measure provides no indication of the consistency of condom use. Moreover, because the information necessary to exclude women who had not had intercourse in the past month had been removed from the public use dataset, we had to rely on a recoded variable to exclude women who had not been sexually active for a full three months. Consequently, we misclassified a certain number of women as single-method users simply because they had not had the opportunity to use a condom in the past month.
In addition to the weaknesses of our outcome measures, the small number of women who relied on user-independent methods limited the conclusions we could draw from our analysis. The limited number of data points in some strata undoubtedly led to significant interaction terms and differences between our outcome measures that we might not have seen with a larger sample size. Moreover, even though there may be important differences in condom use patterns among women using IUDs/Norplant and injectibles, the small number of women using these methods forced us to combine them into a single category. In particular, although we classified injectibles as a user-independent method, this form of contraception differs from IUDs and implantable contraceptives in that women must still return to their health-care provider every three months for their injections. Consequently, women using injectibles must make a greater effort to ensure the effectiveness of their method, but they also have more frequent opportunities for counseling.21
A final limitation of our analysis was that we were unable to include women aged 15–19 years in our adjusted models. Given the prevalence of STIs among teenagers42 and their high rate of unplanned pregnancy,3 monitoring condom use in this group is important. However, given the declines in teenage pregnancy rates and increases in their condom use that were not paralleled in adult women during the decade leading up to the last NSFG,12,13,43,44 detailed analyses focusing on this age group alone13,14,43 likely are of greater value than a combined analysis.
CONCLUSIONS
This analysis suggests that many women are placing themselves at risk for STIs and unplanned pregnancies that could be avoided by using condoms in addition to their more highly effective contraceptive method. Although further research will be needed as the number of women relying on user-independent methods increases, our analysis points to populations in which the use of condoms for dual protection should be monitored carefully. In particular, women having difficulty negotiating condom use within relationships that may not be mutually monogamous should be counseled to emphasize the contraceptive benefits of using condoms for dual protection. Additionally, women in mutually monogamous relationships who are switching to OCs or injectibles should be counseled that they can maximize protection against unplanned pregnancy by continuing their use of condoms. In the meantime, although dual-method use may not be appropriate for all women, promoting condoms in addition to a highly effective method should be seriously considered as the first line of defense against unplanned pregnancy and STIs.
REFERENCES
- 1.Mosher WD, Martinez GM, Chandra A, Abma JC, Wilson SJ. Use of contraception and use of family planning services in the United States: 1982–2002. Adv Data. 2004;350:1–36. [PubMed] [Google Scholar]
- 2.Kost K, Singh S, Vaughan B, Trussell J, Bankole A. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception. 2008;77:10–21. doi: 10.1016/j.contraception.2007.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 4.Trussell J. Contraceptive efficacy. In: Trussell J, Nelson AL, Cates W Jr, Stewart F, Kowal D, editors. Contraceptive technology. 19th ed. New York: Ardent Media; 2007. pp. 747–826. [Google Scholar]
- 5.Nelson AL. Reversible female contraception: current options and new developments. Expert Rev Med Devices. 2007;4:241–52. doi: 10.1586/17434440.4.2.241. [DOI] [PubMed] [Google Scholar]
- 6.Speidel JJ, Harper CC, Shields WC. The potential of long-acting reversible contraception to decrease unintended pregnancy. Contraception. 2008;78:197–200. doi: 10.1016/j.contraception.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Woodsong C, Koo HP. Two good reasons: women's and men's perspectives on dual contraceptive use. Soc Sci Med. 1999;49:567–80. doi: 10.1016/s0277-9536(99)00060-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berer M. Dual protection: more needed than practiced or understood. Reprod Health Matters. 2006;14:162–70. doi: 10.1016/S0968-8080(06)28262-4. [DOI] [PubMed] [Google Scholar]
- 9.Cates W, Jr, Steiner MJ. Dual protection against unintended pregnancy and sexually transmitted infections: what is the best contraceptive approach? Sex Transm Dis. 2002;29:168–74. doi: 10.1097/00007435-200203000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Trussell J, Hatcher RA, Cates W, Jr, Stewart FH, Kost K. A guide to interpreting contraceptive efficacy studies. Obstet Gynecol. 1990;76(3 Pt 2):558–67. [PubMed] [Google Scholar]
- 11.Trussell J, Kost K. Contraceptive failure in the United States: a critical review of the literature. Stud Fam Plann. 1987;18:237–83. [PubMed] [Google Scholar]
- 12.Anderson JE, Santelli J, Mugalla C. Changes in HIV-related preventive behavior in the US population: data from national surveys, 1987–2002. J Acquir Immune Defic Syndr. 2003;34:195–202. doi: 10.1097/00126334-200310010-00010. [DOI] [PubMed] [Google Scholar]
- 13.Abma JC, Martinez GM, Mosher WD, Dawson BS. Teenagers in the United States: sexual activity, contraceptive use, and childbearing, 2002. Vital Health Stat 23. 2004;(24) [PubMed] [Google Scholar]
- 14.Santelli JS, Morrow B, Anderson JE, Lindberg LD. Contraceptive use and pregnancy risk among U.S. high school students, 1991–2003. Perspect Sex Reprod Health. 2006;38:106–11. doi: 10.1363/psrh.38.106.06. [DOI] [PubMed] [Google Scholar]
- 15.Bankole A, Darroch JE, Singh S. Determinants of trends in condom use in the United States, 1988–1995. Fam Plann Perspect. 1999;31:264–71. [PubMed] [Google Scholar]
- 16.Darney PD, Callegari LS, Swift A, Atkinson ES, Robert AM. Condom practices of urban teens using Norplant contraceptive implants, oral contraceptives, and condoms for contraception. Am J Obstet Gynecol. 1999;180:929–37. doi: 10.1016/s0002-9378(99)70664-2. [DOI] [PubMed] [Google Scholar]
- 17.Santelli JS, Davis M, Celentano DD, Crump AD, Burwell LG. Combined use of condoms with other contraceptive methods among inner-city Baltimore women. Fam Plann Perspect. 1995;27:74–8. [PubMed] [Google Scholar]
- 18.Sayegh MA, Fortenberry JD, Shew M, Orr DP. The developmental association of relationship quality, hormonal contraceptive choice and condom non-use among adolescent women. J Adolesc Health. 2006;39:388–95. doi: 10.1016/j.jadohealth.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 19.Berenson AB, Wiemann CM. Use of levonorgestrel implants versus oral contraceptives in adolescence: a case-control study. Am J Obstet Gynecol. 1995;172(4 Pt 1):1128–37. doi: 10.1016/0002-9378(95)91471-4. [DOI] [PubMed] [Google Scholar]
- 20.Polaneczky M, Slap G, Forke C, Rappaport A, Sondheimer S. The use of levonorgestrel implants (Norplant) for contraception in adolescent mothers. N Engl J Med. 1994;331:1201–6. doi: 10.1056/NEJM199411033311806. [DOI] [PubMed] [Google Scholar]
- 21.Sangi-Haghpeykar H, Posner SF, Poindexter AN., III Consistency of condom use among low-income hormonal contraceptive users. Perspect Sex Reprod Health. 2005;37:184–91. doi: 10.1363/psrh.37.184.05. [DOI] [PubMed] [Google Scholar]
- 22.Roye CF. Condom use by Hispanic and African-American adolescent girls who use hormonal contraception. J Adolesc Health. 1998;23:205–11. doi: 10.1016/s1054-139x(97)00264-4. [DOI] [PubMed] [Google Scholar]
- 23.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat 23. 2005;(25) [PubMed] [Google Scholar]
- 24.Groves RM, Benson G, Mosher WD, Rosenbaum J, Granda P, Axinn W, et al. Plan and operation of Cycle 6 of the National Survey of Family Growth. Vital Health Stat 1. 2005;(42) [PubMed] [Google Scholar]
- 25.Sangi-Haghpeykar H, Horth F, Poindexter AN., III Condom use among sterilized and nonsterilized Hispanic women. Sex Transm Dis. 2001;28:546–51. doi: 10.1097/00007435-200109000-00013. [DOI] [PubMed] [Google Scholar]
- 26.HIV-risk behaviors of sterilized and nonsterilized women in drug-treatment programs—Philadelphia, 1989–1991. MMWR Morb Mortal Wkly Rep. 1992;41(9):149–52. [PubMed] [Google Scholar]
- 27.Surgical sterilization among women and use of condoms—Baltimore, 1989–1990. MMWR Morb Mortal Wkly Rep. 1992;41(31):568–9. 75. [PubMed] [Google Scholar]
- 28.Kleinbaum DG, Klein M. Logistic regression: a self-learning text. 2nd ed. New York: Springer; 2005. [Google Scholar]
- 29.Jones RK, Darroch JE, Henshaw SK. Contraceptive use among U.S. women having abortions in 2000–2001. Perspect Sex Reprod Health. 2002;34:294–303. [PubMed] [Google Scholar]
- 30.SAS Institute, Inc. SAS®: Version 9.2. Cary (NC): SAS Institute, Inc; 2009. [Google Scholar]
- 31.Lifflander A, Gaydos LM, Hogue CJ. Circumstances of pregnancy: low income women in Georgia describe the difference between planned and unplanned pregnancies. Matern Child Health J. 2007;11:81–9. doi: 10.1007/s10995-006-0138-3. [DOI] [PubMed] [Google Scholar]
- 32.Kramer MR, Hogue CJ, Gaydos LM. Noncontracepting behavior in women at risk for unintended pregnancy: what's religion got to do with it? Ann Epidemiol. 2007;17:327–34. doi: 10.1016/j.annepidem.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 33.Jones RK, Darroch JE, Henshaw SK. Patterns in the socioeconomic characteristics of women obtaining abortions in 2000–2001. Perspect Sex Reprod Health. 2002;34:226–35. [PubMed] [Google Scholar]
- 34.Gold RB, Sonfield A, Richards CL, Frost JJ. Next steps for America's family planning program: leveraging the potential of Medicaid and Title X in an evolving health care system. New York: Guttmacher Institute; 2009. [cited 2009 Oct 7]. Also available from: URL: http://www.guttmacher.org/pubs/NextSteps.pdf. [Google Scholar]
- 35.Lindberg LD, Frost JJ, Sten C, Dailard C. The provision and funding of contraceptive services at publicly funded family planning agencies: 1995–2003. Perspect Sex Reprod Health. 2006;38:37–45. doi: 10.1363/psrh.38.037.06. [DOI] [PubMed] [Google Scholar]
- 36.Ott MA, Adler NE, Millstein SG, Tschann JM, Ellen JM. The trade-off between hormonal contraceptives and condoms among adolescents. Perspect Sex Reprod Health. 2002;34:6–14. [PubMed] [Google Scholar]
- 37.Plichta SB, Weisman CS, Nathanson CA, Ensminger ME, Robinson JC. Partner-specific condom use among adolescent women clients of a family planning clinic. J Adolesc Health. 1992;13:506–11. doi: 10.1016/1054-139x(92)90015-4. [DOI] [PubMed] [Google Scholar]
- 38.Lansky A, Thomas JC, Earp JA. Partner-specific sexual behaviors among persons with both main and other partners. Fam Plann Perspect. 1998;30:93–6. [PubMed] [Google Scholar]
- 39.Mantell JE, Hoffman S, Exner TM, Stein ZA, Atkins K. Family planning providers' perspectives on dual protection. Perspect Sex Reprod Health. 2003;35:71–8. doi: 10.1363/3507103. [DOI] [PubMed] [Google Scholar]
- 40.Peipert JF, Redding CA, Blume JD, Allsworth JE, Matteson KA, Lozowski F, et al. Tailored intervention to increase dual-contraceptive method use: a randomized trial to reduce unintended pregnancies and sexually transmitted infections. Am J Obstet Gynecol. 2008;198:630.e1–8. doi: 10.1016/j.ajog.2008.01.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weisman CS, Plichta S, Nathanson CA, Ensminger M, Robinson JC. Consistency of condom use for disease prevention among adolescent users of oral contraceptives. Fam Plann Perspect. 1991;23:71–4. [PubMed] [Google Scholar]
- 42.Datta SD, Sternberg M, Johnson RE, Berman S, Papp JR, McQuillan G, et al. Gonorrhea and chlamydia in the United States among persons 14 to 39 years of age, 1999 to 2002. Ann Intern Med. 2007;147:89–96. doi: 10.7326/0003-4819-147-2-200707170-00007. [DOI] [PubMed] [Google Scholar]
- 43.Santelli JS, Lindberg LD, Finer LB, Singh S. Explaining recent declines in adolescent pregnancy in the United States: the contribution of abstinence and improved contraceptive use. Am J Public Health. 2007;97:150–6. doi: 10.2105/AJPH.2006.089169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ventura SJ, Abma JC, Mosher WD, Henshaw SK. Estimated pregnancy rates by outcome for the United States, 1990–2004. Natl Vital Stat Rep. 2008 Apr 14;56:1–25. 28. [PubMed] [Google Scholar]