SYNOPSIS
Objective
We examined recent overweight and obesity trends in a multiethnic population of low-income preschool children.
Methods
We defined overweight as sex-specific body mass index (BMI)-for-age ≥85th and <95th percentile and obesity as sex-specific BMI-for-age ≥95th percentile, and calculated them using demographic data and randomly selected height and weight measurements that were recorded while 2- to <5-year-old children were enrolled in the New York State (NYS) Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) during 2002–2007.
Results
Obesity prevalence peaked at 16.7% in 2003, declined from 2003 through 2005, and stabilized at 14.7% through 2007. Among both boys and girls, the downward trend in annual prevalence of obesity was evident only among Hispanic children (22.8% boys and 20.9% girls in 2002 vs. 19.3% boys and 17.5% girls in 2007) and non-Hispanic black children (15.6% boys and 14.2% girls in 2002 vs. 13.6% boys and 12.4% girls in 2007). In contrast, the annual prevalence estimate for overweight showed an increasing trend from 2002 through 2007.
Conclusions
These results showed a slight decline in prevalence of childhood obesity and a continuing rise in prevalence of childhood overweight among children enrolled in the NYS WIC program during 2002–2007. Future research should investigate the extent to which the slight decline in childhood obesity prevalence may be attributable to population-based and high-risk obesity prevention efforts in NYS.
During the last 10 years, much attention has been devoted to monitoring the growing epidemic of childhood obesity in the U.S.1–3 and around the world.4 Obesity among children can lead to poor health-related quality of life, and can also increase the risk of hyperlipidemia, prediabetes, and hypertension.5–7 Furthermore, overweight and obese children are also significantly more likely to become overweight adults,5 thus increasing their lifetime risk of various chronic diseases, including sleep apnea, diabetes, cardiovascular disease, and cerebrovascular disease.
The burden of childhood obesity is higher among some low-income and minority children.8–14 The relationship between socioeconomic status and obesity among children varies by race/ethnicity and age.9,14 Among 2- to 5-year-old Mexican American children, obesity is inversely related to family income, while obesity prevalence rises with income level among black and white children, then declines at income levels above approximately twice the federal poverty level (FPL).14 Explanations for the excess prevalence of obesity in various populations include lack of opportunities for physical activity; higher availability and consumption of affordable, high-calorie, high-fat convenience foods; and lower access to healthy foods, including fruit and vegetables.15,16 While there is widespread acknowledgement that the etiology of childhood obesity includes a complex interaction of many biological and social factors,15,17 there is awareness that strategies that can significantly control the childhood obesity epidemic should emphasize changing children's eating and physical activity environments.13,18,19
The need to change the eating and physical activity environments of low-income and other at-risk children was highlighted by the 2005 Institute of Medicine report,20 which recommended changes to the food packages provided by the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). The WIC program was established in 1972 by the U.S. Department of Agriculture to address hunger and malnutrition among low-income children and pregnant and postpartum women. While food insecurity remains a major concern, the emergence of the childhood obesity epidemic in the ensuing decades has challenged the WIC program to ensure adequate nutrition for low-income, nutritionally at-risk infants, children, and pregnant and postpartum women, while simultaneously promoting healthy eating to minimize the risk of overweight and obesity among participants.
In New York State (NYS), public health officials have worked in partnership with federal, state, and local agencies to make obesity a priority public health issue for all age groups, including preschool-aged children (e.g., children aged 0–5 years).21,22 The state's premier childhood obesity prevention initiative, the Eat Well Play Hard program, promotes healthy eating and physical activity across all nutrition assistance programs, including WIC, the Hunger Prevention and Nutrition Assistance Program, and Child and Adult Care Food Program. In addition to launching population-based strategies to promote healthy eating and physical activity among young children and their families, the NYS Department of Health (DOH) has also enlisted the help of educators and clinicians in statewide efforts to ensure that parents, caregivers, and health-care providers take an active role in the prevention and control of childhood overweight and obesity. The measures taken by the NYS DOH were largely prompted by evidence showing that childhood obesity was steadily increasing among preschool-aged children participating in the NYS WIC program.23 For example, analyses of trends in obesity prevalence from 1989 to 2003 showed an overall obesity prevalence increase from 12% in 1989 to 16% in 2003;23 in comparison, the national prevalence estimate among U.S. children aged 2 to 5 years in 2002 was slightly more than 10%.24
We assessed trends in prevalence of childhood obesity from 2002 to 2007 among preschool-aged children (2 to <5 years of age) enrolled in the NYS WIC program. We also reported on trends in prevalence of overweight during the study period.
METHODS
We obtained data on childhood overweight and obesity in the WIC program from the NYS component of the national Pediatric Nutrition Surveillance System (PedNSS).25 Through PedNSS, in partnership with the Centers for Disease Control and Prevention (CDC), the NYS DOH collects and monitors weight and height data of children from birth to 59 months of age who participate in the WIC program. Each year, the NYS DOH contributes data on approximately 450,000 infants and children who are enrolled in WIC. Due to lack of body mass index (BMI) reference data for children aged 2 years or younger,26,27 we restricted the study population to children aged 24–59 months (referred to as 2 to <5 years of age), as has been done elsewhere.2,28
For each eligible child (i.e., a child whose family's annual household income is ≤185% FPL or whose family is already participating in other public assistance programs), we measured height and weight; data on age, gender, and race/ethnicity were self-reported at WIC clinics during certification (i.e., during initial enrollment into WIC) and recertification visits. The interval between a certification and recertification visit is approximately six months. Height and weight were measured by trained staff according to standard protocol or were taken at physicians' offices within 60 days of initial WIC certification. Height was recorded to the nearest ¼ inch and weight to the nearest ¼ pound. Recorded measures of height and weight were converted to metric equivalents and BMI was computed as weight in kilograms divided by height in meters squared. Race/ethnicity were reported by the child's parent or caregiver. We categorized racial/ethnic groups as Hispanic, non-Hispanic white, non-Hispanic black, and other. We included race/ethnicity in this study because of known variation in obesity across racial/ethnic groups.2 This study was based on an analysis of program surveillance data and, thus, was exempt from review by the NYS DOH Institutional Review Board.
We defined overweight and obesity using the percentile cutoff points derived from the 2000 sex-specific BMI-for-age growth charts from CDC.27,29 Specifically, we computed age- and sex-specific percentiles for BMI based on the reference population for the 2000 CDC growth charts for U.S. children.27 We defined overweight as a sex-specific BMI-for-age ≥85th and <95th percentile and obesity as a sex-specific BMI-for-age ≥95th percentile.29 While the percentile cutoff points used to define excess BMI have not changed from earlier recommendations,27,30 the terminology used in this article is consistent with current recommendations for clinical practice to more accurately reflect the seriousness of associated health risks and provide continuity with adult definitions.29
We analyzed data using SAS® version 9.1.31 Consistent with the methodology used by CDC for the national PedNSS estimates, each year one record per child was randomly selected for inclusion in the analysis.32 Out of 1,187,566 total records available during 2002–2007, 1.6% (n=18,620) were excluded based on CDC criteria for exclusion of biologically implausible values.33 Descriptive statistics were generated to summarize the characteristics of 2- to <5-year-old children who were enrolled in the NYS WIC program each year from 2002 through 2007. Prevalence estimates for overweight and obesity were generated for each calendar year to assess trends during 2002–2007. Due to the racial/ethnic diversity of children whose race/ethnicity was categorized as other, we estimated racial/ethnic-specific trends of prevalence of overweight and obesity only for Hispanic, non-Hispanic black, and non-Hispanic white groups. We did not conduct statistical significance tests because annual WIC data represent a census of all children who participated in WIC.
RESULTS
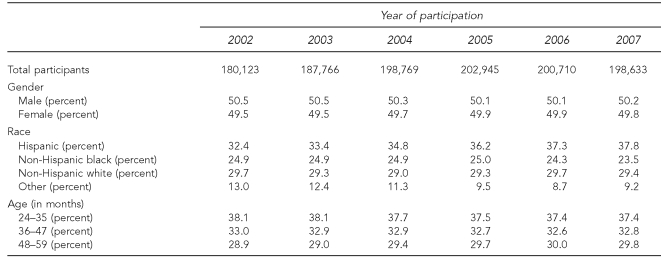
The characteristics of 2- to <5-year-old children who were enrolled in the NYS WIC program for the period 2002–2007 are shown in Table 1. The total number of participating children aged 2 to <5 years ranged from a low of 180,123 in 2002 to a high of 202,945 in 2005. Proportions of male and female children enrolled in WIC each year did not differ significantly from one another, did not differ from year to year, and were generally consistent with the known gender distribution of the general population of 2- to <5-year-olds in NYS.34 Compared with other racial/ethnic categories, the proportion of Hispanic children increased gradually each year, from 32.4% (n=58,360) in 2002 to 37.8% (n=75,282) in 2007. At least two-thirds of all participating children each year were ≤3 years of age.
Table 1.
Characteristics of 2- to <5-year-old children enrolled in the New York State WIC program, 2002–2007
WIC = Special Supplemental Nutrition Program for Women, Infants, and Children
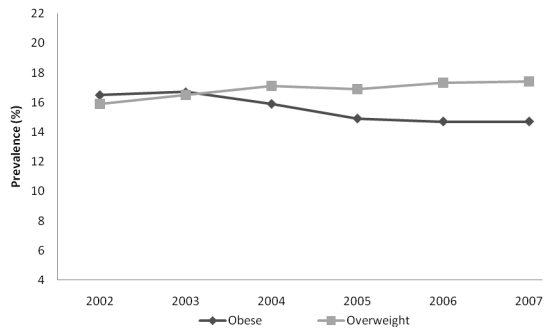
The prevalence proportions for overweight and obesity among all children aged 2 to <5 years in the NYS WIC program showed different trends in the six-year period from 2002 to 2007 (Figure). The annual prevalence for obesity peaked in 2003, underwent a steady decline from 2003 through 2005, and then began to stabilize through 2007, declining 2.0 percentage points between 2002 and 2007 (from 16.7% to 14.7%). In contrast, the annual prevalence estimate for overweight began increasing in 2002, surpassed the prevalence estimate for obesity in 2004, and continued increasing through 2007. The observed trends did not change when prevalence estimates were standardized using the mean racial/ethnic distribution of children aged 2 to <5 years during the study period.
Figure.
Trends in prevalence of obesitya and overweightb among children 2 to <5 years of age participating in the New York State WIC program, 2002–2007
aObesity is defined as a BMI ≥95th percentile of the sex-specific BMI-for-age CDC growth charts.
bOverweight is defined as a BMI ≥85th percentile and <95th percentile of the sex-specific BMI-for-age CDC growth charts.
WIC = Special Supplemental Nutrition Program for Women, Infants, and Children
BMI = body mass index
CDC = Centers for Disease Control and Prevention
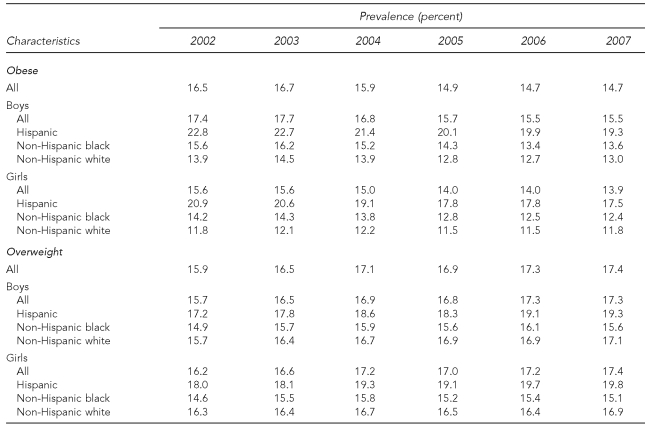
Table 2 shows the annual prevalence proportions for overweight and obesity by gender and race/ethnicity. Regardless of race/ethnicity, the prevalence proportions for obesity (BMI for age ≥95th percentile) were higher among boys than girls for each of the six years. Among both boys and girls, the downward trend in annual prevalence of obesity was evident only among Hispanic children (22.8% boys and 20.9% girls in 2002 vs. 19.3% boys and 17.5% girls in 2007) and non-Hispanic black children (15.6% boys and 14.2% girls in 2002 vs. 13.6% boys and 12.4% girls in 2007). Despite the lack of an apparent downward trend among non-Hispanic white children, the annual prevalence estimates for obesity within each gender group were consistently highest among Hispanic children and lowest among non-Hispanic white children.
Table 2.
Prevalence of obesitya and overweightb among 2- to <5-year-old children enrolled in the New York State WIC program, 2002–2007
aObesity is defined as a BMI ≥95th percentile of the sex-specific BMI-for-age CDC growth charts.
bOverweight is defined as a BMI ≥85th and <95th percentile of the sex-specific BMI-for-age CDC growth charts.
WIC = Special Supplemental Nutrition Program for Women, Infants, and Children
BMI = body mass index
CDC = Centers for Disease Control and Prevention
Unlike obesity, the prevalence of overweight did not differ by gender. However, the prevalence of overweight (BMI-for-age ≥85th and <95th percentile) within each gender group was consistently highest among Hispanic children and lowest among non-Hispanic black children. Annual increases in the prevalence of overweight were more pronounced among Hispanic children, with absolute differences of 2.1% and 1.8% between 2002 and 2007 among boys and girls, respectively.
DISCUSSION
The results of this study suggest that the prevalence of obesity (referred to as overweight in earlier studies) among low-income preschool-aged children in NYS may have peaked during 2002–2003, with a subsequent downward trend beginning in 2004 and continuing through 2007, particularly among Hispanic and non-Hispanic black children. In contrast, previous evidence demonstrated increasing trends in childhood obesity in 2- to <5-year-old children enrolled in the NYS WIC program between 1989 and 200323 and in the national PedNSS.10,28 Interestingly, the recent decreasing trend in prevalence of obesity occurred during a period when the proportion of Hispanic children participating in the NYS WIC program was continually increasing. As evidenced by the gender- and race/ethnicity-specific prevalence estimates in this study, Hispanic children had higher prevalence estimates for overweight and obesity compared with non-Hispanic black and white children, with the disparities remaining throughout the study period.2,12,35–37
To our knowledge, this is the first study to suggest a flattening or decreasing trend in obesity prevalence in a sample of low-income preschool-aged children—a known high-risk population for childhood overweight and obesity in the U.S. Evidence suggesting that the widely documented increase in childhood obesity in recent years could now be abating has also come from recent analyses of data representing the general population of 2- to 5-year-old boys and girls in the U.S. Comparisons of National Health and Nutrition Examination Survey (NHANES) estimates of prevalence of high BMI for age from 1999 to 2006 suggest that the prevalence of obesity among the general population of 2- to 5-year-old boys and girls in the U.S. may have also peaked.2 The results of the present study suggest that low-income preschool-aged children participating in the NYS WIC program have not only experienced a peak, but are also experiencing a downward trend in the prevalence of obesity.
Strengths and limitations
Our study design had several strengths that should be highlighted. First, we derived annual estimates for overweight and obesity prevalence primarily from measured weight and height data collected by trained WIC staff from the entire population of 2- to <5-year-olds participating in WIC each year. Therefore, each annual prevalence estimate represents the actual distribution of overweight or obesity in the entire population of children enrolled in the NYS WIC program. Furthermore, the six-year study period (2002–2007) provided an adequate number of data points to conduct a trends analysis and, thus, increased the likelihood that the observed downward trend is likely to be real and not due to chance.
Our study was also subject to several limitations. First, the data do not represent the same cohort of children from year to year. With the exception of the racial/ethnic composition, however, the demographic characteristics of the study population remained largely the same during the study period. Second, we did not have information on national origin; thus, we were unable to assess the extent to which the observed trends in this study varied among Hispanic subgroups in NYS (e.g., Puerto Rican vs. Mexican American children). Finally, our data include weight and height measures taken at physicians' offices within 60 days of initial WIC certification. The accuracy and precision of weight and height measures obtained during clinical visits may not be comparable with those obtained using standard protocol by trained WIC staff. However, any error that may have resulted from the inclusion of weight and height measures taken at the participating child's primary care provider would be expected to result in random error rather than in systematic error, leading either to the overestimation or underestimation of obesity prevalence.
In all, it is very unlikely that the aforementioned limitations could have led to the observed trends in obesity prevalence in this study. Furthermore, the methods used in this study were consistent with those of previous studies that documented the increasing trend in childhood obesity. The results of this study should, therefore, reflect true trends in prevalence of obesity among children who were enrolled in the NYS WIC program from 2002 to 2007.
CONCLUSIONS
Despite evidence of a downward trend in prevalence of obesity, this study also presents results that are still a cause for concern. First, obesity prevalence estimates among low-income children enrolled in WIC in NYS are still higher than the national estimates from NHANES2 (12.6%) and approximate those from the national PedNSS38 (14.9%). Predictably, increasing prevalence of overweight will likely be a natural consequence of successful efforts to decrease obesity prevalence over time, as children who were obese or would have become obese are instead assigned to the overweight category as a result of efforts to prevent obesity. Such changes, however, need to be distinguished from a situation in which normal-weight children gain excess weight and move to the overweight category.
While the design of this study did not allow for any causal inferences to be made, several childhood obesity prevention and control strategies that the NYS DOH has employed during the past dozen years may be associated with the observed downward trend in childhood obesity prevalence. Chief among these strategies is the statewide Eat Well Play Hard initiative, which simultaneously promotes developmentally appropriate physical activity, consumption of low-fat milk and other dairy products, and consumption of fruit and vegetables among all NYS children.22 It is also likely that other societal changes recognizing and addressing obesity as a growing health problem may have begun to affect obesity rates during this time period. These strategies and others that focus on the promotion of breastfeeding, early recognition of childhood overweight and obesity using sex-specific BMI-for-age percentiles, and use of consistent nutrition and lifestyle messages21 will need to be maintained for this trend to continue. Within the health-care sector, physicians and other health-care professionals should continue to monitor children's BMI for age; review children's dietary and physical activity behaviors; and advocate for policies that support home, school, and neighborhood environments that are conducive to healthy eating and physical activity.29,39,40
Continued monitoring and analysis, both at the state and national level, are necessary to determine if a true downward trend in childhood obesity is indeed occurring nationwide. Specifically, future studies should examine childhood obesity trends among 2- to <5-year-old children who are enrolled in other state WIC programs, as well as in the national PedNSS. A related area of focus for future research should be the identification of shifts in the distribution of BMI by age, gender, and race/ethnicity; evidence from such studies has the potential to shed light on which subgroups of children are being adequately exposed to ongoing childhood obesity prevention efforts. Finally, efficient targeting of public health resources will require the continued conduct of rigorous evaluation studies to identify effective strategies for addressing unhealthy eating and sedentary behaviors, both of which are leading risk factors for childhood obesity and overweight.29
Footnotes
The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the New York State Department of Health.
REFERENCES
- 1.Freedman DS, Khan LK, Serdula MK, Ogden CL, Dietz WH. Racial and ethnic differences in secular trends for childhood BMI, weight, and height. Obesity (Silver Spring) 2006;14:301–8. doi: 10.1038/oby.2006.39. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–5. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132:2087–102. doi: 10.1053/j.gastro.2007.03.052. [DOI] [PubMed] [Google Scholar]
- 4.Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes (Lond) 2008;32:1431–7. doi: 10.1038/ijo.2008.102. [DOI] [PubMed] [Google Scholar]
- 5.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101(3 Pt 2):518–25. [PubMed] [Google Scholar]
- 6.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–9. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 7.Williams J, Wake M, Hesketh K, Maher E, Waters E. Health-related quality of life of overweight and obese children. JAMA. 2005;293:70–6. doi: 10.1001/jama.293.1.70. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006;84:707–16. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- 10.Sherry B, Mei Z, Scanlon KS, Mokdad AH, Grummer-Strawn LM. Trends in state-specific prevalence of overweight and underweight in 2- through 4-year-old children from low-income families from 1989 through 2000. Arch Pediatr Adolesc Med. 2004;158:1116–24. doi: 10.1001/archpedi.158.12.1116. [DOI] [PubMed] [Google Scholar]
- 11.Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;103:e85. doi: 10.1542/peds.103.6.e85. [DOI] [PubMed] [Google Scholar]
- 12.Kimbro RT, Brooks-Gunn J, McLanahan S. Racial and ethnic differentials in overweight and obesity among 3-year-old children. Am J Public Health. 2007;97:298–305. doi: 10.2105/AJPH.2005.080812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Child. 2006;16:187–207. doi: 10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- 14.Freedman DS, Ogden CL, Flegal KM, Khan LK, Serdula MK, Dietz WH. Childhood overweight and family income. MedGenMed. 2007;9:26. [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson PM, Butcher KE. Childhood obesity: trends and potential causes. Future Child. 2006;16:19–45. doi: 10.1353/foc.2006.0001. [DOI] [PubMed] [Google Scholar]
- 16.Hill JO, Peters JC. Environmental contributions to the obesity epidemic. Science. 1998;280:1371–4. doi: 10.1126/science.280.5368.1371. [DOI] [PubMed] [Google Scholar]
- 17.Drewnowski A. Obesity and the food environment: dietary energy density and diet costs. Am J Prev Med. 2004;27(3) Suppl:154–62. doi: 10.1016/j.amepre.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 18.Bluford DA, Sherry B, Scanlon KS. Interventions to prevent or treat obesity in preschool children: a review of evaluated programs. Obesity (Silver Spring) 2007;15:1356–72. doi: 10.1038/oby.2007.163. [DOI] [PubMed] [Google Scholar]
- 19.Story M, Kaphingst KM, French S. The role of child care settings in obesity prevention. Future Child. 2006;16:143–68. doi: 10.1353/foc.2006.0010. [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine. WIC food packages: time for a change. Washington: National Academies Press; 2005. [Google Scholar]
- 21.New York State Department of Health. New York State strategic plan for overweight and obesity prevention. Revised 2008. [cited 2008 Aug 8]. Available from: URL: http://www.health.state.ny.us/prevention/obesity/strategic_plan.
- 22.Jesaitis A, Race P. Eat Well Play Hard—New York State's initiative to prevent childhood obesity. Pediatr Nutr. 2000;23:11–3. [Google Scholar]
- 23.Edmunds LS, Woelfel ML, Dennison BA, Stratton H, Pruzek RM, Abusabha R. Overweight trends among children enrolled in the New York State Special Supplemental Nutrition Program for Women, Infants, and Children. J Am Diet Assoc. 2006;106:113–7. doi: 10.1016/j.jada.2005.09.052. [DOI] [PubMed] [Google Scholar]
- 24.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 25.Centers for Disease Control and Prevention (US) Pediatric and Pregnancy Nutrition Surveillance System. [cited 2008 Aug 5]. Available from: URL: http://www.cdc.gov/pednss.
- 26.Mei Z, Grummer-Strawn LM, Pietrobelli A, Goulding A, Goran MI, Dietz WH. Validity of body mass index compared with other body-composition screening indexes for the assessment of body fatness in children and adolescents. Am J Clin Nutr. 2002;75:978–85. doi: 10.1093/ajcn/75.6.978. [DOI] [PubMed] [Google Scholar]
- 27.Kuczmarski RJ, Ogden CL, Guo SS, Gummer-Strawn LM, Flegal KM, Mei Z, et al. 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002;(246) [PubMed] [Google Scholar]
- 28.Polhamus B, Dalenius K, Borland E, Smith B, Grummer-Strawn L. Pediatric nutrition surveillance report 2006. Atlanta: CDC (US); 2007. [PubMed] [Google Scholar]
- 29.Barlow SE, the Expert Committee Expert Committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120:S164–92. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 30.Barlow SE, Dietz WH. Obesity evaluation and treatment: Expert Committee recommendations. Pediatrics. 1998;102:E29. doi: 10.1542/peds.102.3.e29. [DOI] [PubMed] [Google Scholar]
- 31.SAS Institute, Inc. SAS®: Version 9.1.3. Cary (NC): SAS Institute, Inc.; 2004. [Google Scholar]
- 32.CDC (US) How to read a data table. [cited 2008 Aug 5]. Available from: URL: http://www.cdc.gov/pednss/how_to/read_a_data_table/index.htm.
- 33.CDC (US) An SAS program for the CDC growth charts. [cited 2008 Aug 5]. Available from: URL: http://www.cdc.gov/nccdphp/dnpa/growthcharts/resources/sas.htm.
- 34.New York State Department of Health. Vital statistics of New York State 2006: table 1: estimated population by age, sex and region, New York State—2006. [cited 2008 Jul 28]. Available from: URL: http://www.health.state.ny.us/nysdoh/vital_statistics/2006/table01.htm.
- 35.Ogden CL, Flegal KM, Carroll MD, Johnson CL. Prevalence and trends in overweight among US children and adolescents, 1999–2000. JAMA. 2002;288:1728–32. doi: 10.1001/jama.288.14.1728. [DOI] [PubMed] [Google Scholar]
- 36.Thorpe LE, List DG, Marx T, May L, Helgerson SD, Frieden TR. Childhood obesity in New York City elementary school students. Am J Public Health. 2004;94:1496–1500. doi: 10.2105/ajph.94.9.1496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nelson JA, Carpenter K, Chiasson MA. Diet, activity, and overweight among preschool-age children enrolled in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) Prev Chronic Dis. 2006;3:A49. [PMC free article] [PubMed] [Google Scholar]
- 38.CDC (US) Pediatric data tables: table 12: 2007 Pediatric Nutrition Surveillance Summary: summary of trends in growth and anemia indicators. [cited 2008 Aug 27]. Available from: URL: http://www.cdc.gov/pednss/pednss_tables/tables_numeric.htm.
- 39.Stettler N. The global epidemic of childhood obesity: is there a role for the paediatrician? Obes Rev. 2004;5:91–2. doi: 10.1111/j.1467-789X.2004.00138.x. [DOI] [PubMed] [Google Scholar]
- 40.Krebs NF, Jacobson MS, American Academy of Pediatrics Committee on Nutrition. Prevention of pediatric overweight and obesity. Pediatrics. 2003;112:424–30. doi: 10.1542/peds.112.2.424. [DOI] [PubMed] [Google Scholar]