SYNOPSIS
Objective
We investigated the extent to which smoking status was associated with exposure to occupational (e.g., dust, chemicals, noise, and ergonomic strain) and social (e.g., abuse, sexual harassment, and racial discrimination) workplace hazards in a sample of U.S. multiethnic working-class adults.
Methods
United for Health is a cross-sectional study designed to investigate the combined burden of occupational and social workplace hazards in relation to race/ethnicity, gender, and wage and to evaluate related health effects in a working-class population. Using validated measures, we collected data from 1,282 multiethnic working-class participants using audio computer-assisted interviews. We used multiple imputation methods to impute data for those missing data. Crude and adjusted logistic odds ratios (ORs) were modeled to estimate ORs and 95% confidence intervals (CIs).
Results
The prevalence of smoking was highest among non-Hispanic white workers (38.3%) and lowest for foreign-born workers (13.1%). We found an association between racial discrimination and smoking (OR=1.12, 95% CI 1.01, 1.25). The relationship between smoking and sexual harassment, although not significant, was different for black women compared with men (OR=1.79, 95% CI 0.99, 3.22). We did not find any associations by workplace abuse or by any of the occupational hazards.
Conclusion
These results indicate that racial discrimination might be related to smoking in working-class populations and should be considered in tobacco-control efforts that target this high-risk population.
Even though the harmful effects of cigarette smoking are well documented, 31% of service and 35% of blue-collar workers still smoke cigarettes in the U.S., compared with about 20% of white-collar workers and the general population.1,2 This disparity in smoking status, evident since 1956, persists even after controlling for sociodemographic factors.1,3–5 Yet, limited research has sought to elucidate the influence of exposure to occupational and social workplace hazards on this persistent occupational class disparity in smoking. The predominant approach, as summarized by literature reviews, is to treat workers' smoking as a risk factor unrelated to occupational hazards, but that in combination with occupational hazards leads to poor health.6 Other studies have focused on the role of psychosocial work conditions on smoking behaviors.7
Countering the conventional view separating occupational disparities in smoking from exposure to workplace hazards, a small number of studies have investigated associations between smoking and occupational hazards. For example, in the U.S., one study found higher prevalence of smoking in occupations where workers are exposed to occupational hazards such as irritating dust and fumes,8 while one Japanese and two U.S. studies found a relationship between exposure to noise and cigarette smoking.9–11
A separate body of work has linked smoking with social hazards, such as psychological abuse12 and domestic violence,13 but these studies have typically not addressed work-related social hazards.14 One study of workplace psychological abuse (specifically bullying) reported no differences in smoking prevalence between workers who were bullied and those who were not bullied by their coworkers.15 Another study found a higher prevalence of both smoking and sexual harassment among flight attendants, but the study did not examine the relationship between sexual harassment and smoking.16 In contrast, several studies suggest a positive relationship between racial discrimination and current smoking, with some of these studies employing instruments with questions specifically asking about having experienced racial discrimination on the job.17–22
There are several mechanisms through which hazards can become embodied to manifest in the risk of smoking.23 Hazards can act as stressors and, as such, may exert some of their influence through a stress-mediated mechanism. Smoking is well-known as a source of stress relief,24 especially among the working class.25 Also, we expect a nonstress-mediated pathway between exposure to work-related hazards and smoking. Racial discrimination can affect health via job discrimination leading to lower wages, which in turn leads to increased use of items such as cigarettes as luxury goods. It can also affect job assignment and, hence, exposure to workplace hazards.23
This article examines the extent to which smoking was associated with exposure to occupational (e.g., dust, chemicals, noise, and ergonomic strain) and social (e.g., abuse, sexual harassment, and racial discrimination) workplace hazards in a sample of U.S. multiethnic working-class adults. Our previous analyses of data from this population showed a social patterning whereby the types and severity of both occupational and social workplace hazards were different based on race/ethnicity and nativity. For example, 37% of white participants reported racial discrimination compared with 58% of nonwhite workers, while Latino workers reported a higher burden of exposure to occupational hazards.14,26 Likewise, those born outside the U.S. reported shoulder strain (69%) more frequently compared with U.S. natives.26 Therefore, we stratified our analysis by race/ethnicity and nativity.
METHODS
Study population
The United for Health study was designed to investigate the combined burden of occupational and social workplace hazards in relation to race/ethnicity, gender, and wage and to evaluate related health effects in a working-class population.27 The study was approved by Institutional Review Boards at the Dana-Farber Cancer Institute, Harvard School of Public Health, and University of Massachusetts.
Detailed descriptions of the study and sampling procedures have been provided in previous articles.14,21,27 Through a partnership with labor unions, we recruited participants at 14 worksites who worked in meat processing, electrical light manufacturing, school bus driving, and retail grocery stores in and around Boston, Massachusetts. Data were collected from March 2003 through August 2004 using a 45-minute bilingual (English and Spanish) questionnaire administered by audio computer-assisted self-interviewing (ACASI). With ACASI, questions are shown on screen as they are read aloud through a headphone, allowing participants to answer questions privately.28 The study had bilingual survey assistants on site to answer questions from participants. Of the 1,776 union members who were eligible for the study, 1,282 (72%) completed the survey. The range of participants per worksite was 31 to 152, with a median of 85 participants across worksites. This analysis (n=1,187) excluded those respondents who were missing data on smoking (n=15) or age (n=43), as well as 37 participants who fell outside the study's age range for eligibility (i.e., 25–65 years).
Measures
To assess gender and race/ethnicity, participants were asked to indicate their gender as women, men, or other and whether they belonged to one of eight racial/ethnic categories (Hispanic, black, African American, white, American Indian/Alaskan Native, Asian, Native Hawaiian or other Pacific Islander, and other). Those who reported that they belonged to the Hispanic or Latino category were classified as Hispanic. The remaining participants who were not black/African American, Latino, or white, comprising approximately 10% of the study population, were classified as “additional race/ethnicity.” Participants were asked to indicate whether they were either foreign-born (i.e., born outside the U.S. and U.S. territories) or native-born (i.e., born in the U.S. or U.S. territories). Age was calculated for each participant based on his/her stated date of birth. Participants chose their educational attainment from among less than 12th grade, high school degree/general educational development, some college/vocational school, four years of college, or graduate degree. We determined their household poverty level, as specified by the U.S. federal poverty guidelines, based on their household income and the number and age of household members supported by this income.29
In keeping with Centers for Disease Control and Prevention (CDC) guidelines, smokers had to meet two criteria: lifetime smoking of at least 100 cigarettes and smoking a cigarette in the last seven days.30 The measures for the social workplace hazards examined in this study and calculation of their summary scores have been previously described.14 In brief, we measured workplace abuse using the generalized workplace abuse instrument, which has eight items adapted to tap into five domains of non-gender-specific abuse.31 The five domains of generalized workplace abuse are verbal aggression, disrespectful behavior, isolation/exclusion, threats/bribes, and physical aggression. We calculated summary scores for workplace abuse by adding up the number of items for which subjects reported at least one experience of workplace abuse and then scoring each item according to frequency of occurrence (score range: 0–16). Sexual harassment was measured using five items that were adapted from two validated instruments designed to tap into three major domains of sexual harassment: sexual coercion, unwanted sexual attention, and gender-based hostility.32 We calculated summary scores for sexual harassment by adding the number of items for which participants reported an experience of sexual harassment (score range: 0–5). The referent period for workplace abuse and sexual harassment was set at past 12 months.
To measure racial discrimination, we used the revised edition of the newly validated Experiences of Discrimination questionnaire.21 We calculated summary values for experience of racial discrimination based on the frequency of experiencing racial discrimination in nine situations (score range: 0–9). The reference period for racial discrimination was set as lifetime, because experiences of racial discrimination can start during childhood, span throughout life, and have a cumulative impact.23
Detailed information about the measures used to assess occupational hazards has also been previously described.26 Briefly, we obtained self-reports of exposure to occupational hazards using a 12-month recall period. We measured noise by asking two questions:33,34 “Have you worked in a noisy area?” with a follow-up question asking about the frequency of exposure per day (<3, 3–6, or >6 hours). Five questions adapted from validated surveys were used to measure exposure to dust and chemicals.35,36 We first asked about exposure, and then we asked follow-up questions about length of exposure, using a four-category scale (never, rarely, sometimes, and often).
We adapted questions from the Washington State Ergonomics Rule to assess exposure to work-related musculoskeletal hazards (i.e., repetitive hand motions and awkward postures during work that strain the shoulder, neck, hand, and back) and length of exposure to these hazards (<1, 1–4, and >4 hours).
Participants were classified as exposed to occupational hazards in relation to three sets of exposures: (1) exposed to a noisy area for more than six hours/day, (2) often exposed to dust and chemicals, or (3) exposed more than four hours/day to strained postures in the shoulder, neck, and back, or repetitive hand motions. Based on these criteria, which were based on how the different measures we used classified high exposure, each participant was classified as either exposed or unexposed to each occupational hazard.
Statistical analysis
We first examined the distribution of smoking in the sample, after which we conducted crude and adjusted logistic regression analyses to identify factors that could potentially confound the relationship between smoking and the exposures. Our final model controlled for age, education, race/ethnicity, poverty status, gender, and nativity. Controlling for these potential confounding variables, we built multivariable logistic regression models to investigate the associations between smoking and exposure to workplace hazards. We first conducted these multivariable analyses individually for each hazard and then together in one model, the results of which were similar.
Prior analyses showed a patterning of hazards based on race/ethnicity and nativity; therefore, we stratified our analyses by these variables even though we did not see any statistically significant effect modification.14,26 Prior analyses also indicated a different patterning of sexual harassment based on gender; therefore, we included an interaction term for gender for sexual harassment in the models. All regression analyses controlled for the random effect of worksite and were conducted using GLIMMIX in SAS® software, which is the preferred modeling technique for data where there is potential within-cluster (worksite) correlation and where the number of clusters is small.37,38
Even though no variable had more than 10% missing, a substantial number of study participants (15%) were missing data on at least one key variable in the analyses. To avoid potential internal validity bias due to missing data, we used the Amelia II® program, a bootstrapping-based algorithm that imputes missing data in cross-sectional or longitudinal settings, to create 10 imputed datasets.39 All variables included in the analysis models were part of the imputation model used to predict missing data, and the statistical inference for the imputation took both between- and within-imputation variability into account. We then used the MIANALYZE procedure in SAS to combine the results.
RESULTS
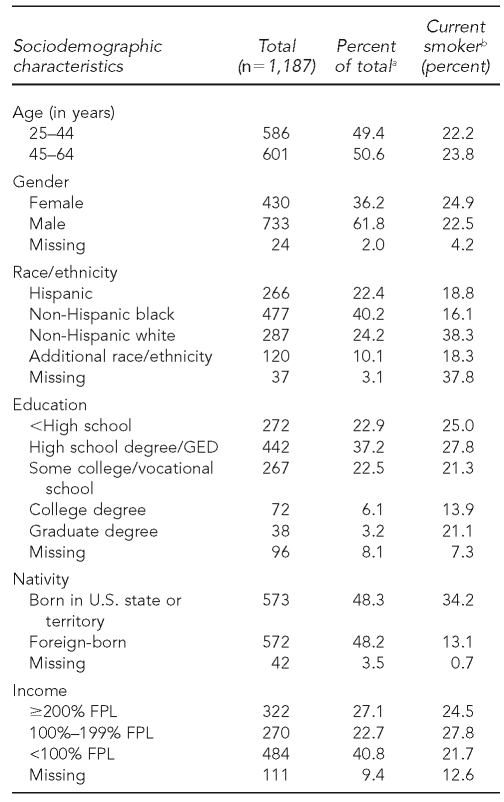
The sociodemographic characteristics of the multiracial/ethnic study participants (40.2% black, 22.4% Hispanic, 24.2% white, 10.1% additional race/ethnicity, and 3.1% unknown race/ethnicity), prior to imputing missing covariates, are shown in Table 1. The overall prevalence of smoking in the sample was 23.0%. The highest prevalence of smoking occurred among non-Hispanic white participants (38.3%) and the lowest prevalence was among foreign-born participants (13.1%).
Table 1.
Sociodemographic characteristics, overall and by smoking prevalence: United for Health Study, Boston, 2003–2004
aColumn percent total
bRow percent total
GED = general educational development
FPL = federal poverty level
Overall, smoking prevalence was higher among people who were exposed vs. those who were unexposed to workplace abuse (25.3% vs. 17.1%, respectively; p=0.003) and chemicals and dust (26.2% vs. 20.5%, respectively; p=0.02). However, smoking prevalence did not differ for those who were exposed vs. those who were unexposed to sexual harassment (21.2% vs. 23.6%, respectively; p=0.41), racial discrimination (25.5% vs. 20.9%, respectively; p=0.13), ergonomic hazards (23.5% vs. 21.8, respectively; p=0.52), and noise (22.8% vs. 23.1%, respectively; p=0.90).
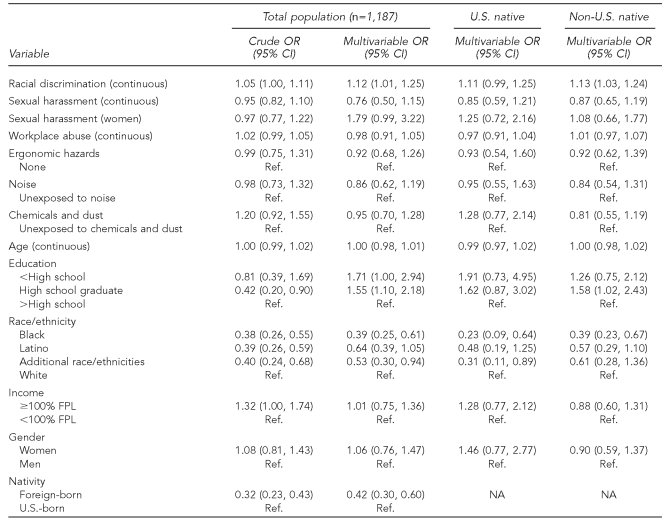
Table 2 summarizes the analytic results, for both crude and adjusted models, from modeling the odds of smoking for the whole population and by nativity. Racial discrimination tended to be associated with smoking in the crude models, and was significantly associated with smoking generally (odds ratio [OR] = 1.12, 95% confidence interval [CI] 1.01, 1.25). We found no evidence of effect modification of this relationship by nativity in stratified analysis. However, the association became nonsignificant for those born in the U.S. (OR=1.11, 95% CI 0.99, 1.25) but remained significant for those born outside the U.S. (OR=1.13, 95% CI 1.03, 1.24). The change in significance was likely due to reduced power in the stratified analysis.
Table 2.
The relationship between social workplace hazards and smoking stratified by nativity: United for Health Study, Boston, 2003–2004
OR = odds ratio
CI = confidence interval
Ref. = referent group
FPL = federal poverty level
NA = not applicable
Exposure to sexual harassment and workplace abuse were not associated with any difference in the odds of being a current smoker in the crude or adjusted models, even when the analyses were stratified by gender. Likewise, exposure to ergonomic hazards, noise, chemicals, and dust were not significantly associated with smoking, although people with exposure to chemicals and dust tended to be at increased risk in crude models (OR=1.20, 95% CI 0.92, 1.55).
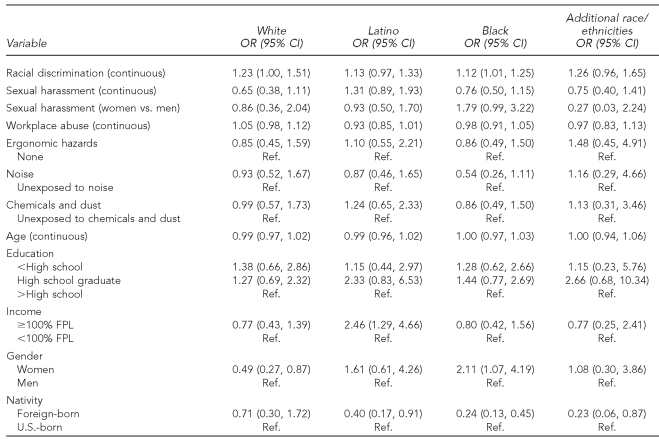
We did not find any evidence of effect modification in the analyses stratified by racial/ethnic category (Table 3); however, the relationship remained significant only for the black participants (OR=1.12, 95% CI 1.01, 1.25). Again, this is possibly due to reduced power in the stratified analysis. The stratified analysis did show that the relationship between smoking and sexual harassment, although not significant, might be different for black women compared with men (OR=1.79, 95% CI 0.99, 3.22).
Table 3.
The relationship between exposure to occupational workplace hazards and smoking stratified by race/ethnicity: United for Health Study, Boston, 2003–2004 (n=1,187)
OR = odds ratio
CI = confidence interval
Ref. = referent group
FPL = federal poverty level
DISCUSSION
We investigated the association between exposure to social and occupational workplace hazards and smoking in a multiethnic U.S. working-class population. Exposure to racial discrimination was associated with increased odds of smoking in our study. This relationship continued to be significant among black respondents, but became nonsignificant for all other racial/ethnic groups in stratified multivariable analyses. It makes sense that the association between racial discrimination and smoking was more pronounced among black participants given the role of racism as a stressor throughout the history of this minority group.40 However, the results could also reflect the reduced power to detect the association in stratified analyses. In contrast, sexual harassment and workplace abuse were not statistically significantly associated with smoking in stratified or combined analyses. Also, there were no significant differences in the association between these exposures and smoking after stratifying the analyses by gender, even though earlier analyses found a patterning of sexual harassment by gender.14 We did not find any relationship between smoking and the occupational hazards we examined.
Our findings have important implications for research on smoking in working-class populations and the elimination of disparities in smoking. We found an association between racial discrimination and smoking, which remained significant for black and also non-native workers when the data were stratified. None of the studies described previously, which examined the relationship between racial discrimination and smoking, reported any findings related to nativity.17–22
We did not find any relationship between the occupational hazards we examined and smoking. One Japanese and two U.S. studies reported an association between exposure to noise and smoking.9–11 Two of these studies reported a higher prevalence of smoking with exposure to noise, which we also observed, but these prior studies did not conduct multivariable analyses of this relationship. Therefore, it is unclear whether their results are consistent with ours.9,10 The other study found an association between smoking and noise-induced hearing loss and did not explore a direct multivariable relationship between smoking and noise.11
Limitations
A number of study limitations should be considered when interpreting these results. The study's cross-sectional design limited the ability to make inferences regarding causation. The study relied on self-report of smoking status. We used CDC guidelines, which require smokers to meet two criteria, to classify smokers. Also, the study questionnaire included questions on several different exposures and outcomes; therefore, we do not expect that there was differential misclassification by smoking status. Although we used validated measures of exposures, exposure misclassification is still possible. The study included an industrial hygiene walk-through examination of occupational hazards, results of which corresponded with reports by study participants of exposure to occupational hazards. Other studies, however, have shown that workers may sometimes overreport exposure to ergonomic hazards,41 and may also both underreport and correctly report exposures to other occupational hazards.42,43 Likewise, studies on social hazards suggest that participants are more likely to underreport these hazards.23,44 In this case, misclassification would most likely lead to attenuation of the relationship between exposure to hazards in the workplace and smoking behaviors.
Our use of multiple imputation assumes missing at random, but this assumption cannot be empirically tested.45 Nevertheless, we have enough information on important predictors of missingness and the exposures, which we used to specify the imputation model for multiple imputation. Finally, although the study involved only unionized workers —who represent 12.4% of the U.S. working population46 —the unions provided reliable access to the workers and a safe setting in which they could provide information about the sensitive topics under study without fear of exposure to or retribution from management.47
It is also possible that our definition of exposure diluted any relationship between exposure to occupational hazards and smoking. Our classification separated those with high exposures as exposed and all others as unexposed to occupational hazards. We chose this classification because about 85% of our study participants reported at least one high exposure to an occupational hazard.26 Having a high and limited range of the exposure can, as argued by Rose, limit the ability to find a relationship with the outcome even when one is present.48
Our study indicated a lack of association between sexual harassment and workplace abuse and smoking. We were unable to compare our findings with other reports due to the paucity of studies in the extant literature examining the relationship between these exposures and smoking. Our racial discrimination measure had a time frame of “ever,” whereas the sexual harassment and workplace abuse measures pertained only to the last 12 months. It is possible that the time frame we used for workplace abuse and sexual harassment did not cover the association of these exposures, if any, with smoking, as most people who smoke in the U.S. initiate smoking before age 18.49 A possibly more relevant outcome would have been the likelihood of quitting among those who smoked during the past year, but we did not have data on this outcome.
Strengths
Despite these limitations, our study had several strengths. To our knowledge, our study is the first to examine both social and occupational workplace hazards and their relationship to smoking in a working-class population. We used a multiracial/ethnic working-class population, an understudied working population whose exclusion from research studies is well documented.50,51 Use of this population allowed us to examine potential effect modification by both nativity and race. Also, our use of multiple imputation methods minimized internal validity bias due to missing data because it allowed us to preserve information from those with missing data who otherwise would have been excluded in multivariable analyses.45
CONCLUSION
Although we did not find an association between occupational hazards and smoking, we found a high burden of exposure to occupational hazards in this population. Addressing smoking in this group is particularly relevant because workers are not only exposed to respiratory hazards through cigarette smoking, but also through exposure to occupational hazards. Thus, the risk to the workers' health from smoking is increased, a situation termed “double jeopardy.”52 The workers in our sample were exposed to high levels of both social and occupational workplace hazards.14,26 Further exploration of the relationship between exposure to social and occupational workplace hazards and smoking will require studies with bigger samples of workers with wider distributions of exposure to hazards.
Acknowledgments
The authors thank the workers who participated in the study and the unions and employers who collaborated on survey design and data collection. The authors also thank additional team members who engaged in the study: Margaret Quinn, Anne Stoddard, Lisa Bates, Vanessa Costa, Ruth Lederman, Maribel Melendez, Michael Ostler, Grace Sembajwe, Pamela D. Waterman, and Richard Youngstrom.
Footnotes
The United for Health study was funded by grant #R01 OH07366-01 from the National Institute of Occupational Safety and Health to Elizabeth Barbeau. Cassandra Okechukwu was supported by the Centers for Disease Control and Prevention/Association of Schools of Public Health Prevention Research Center Fellowship.
REFERENCES
- 1.Barbeau EM, Krieger N, Soobader MJ. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000 [published erratum appears in Am J Public Health 2004;94:1295] Am J Public Health. 2004;94:269–78. doi: 10.2105/ajph.94.2.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (US) Targeting tobacco use: the nation's leading cause of preventable death, 2008. Atlanta: National Center for Chronic Disease Prevention and Health Promotion, CDC; 2008. [cited 2009 Jun 11]. Also available from: URL: http://www.cdc.gov/nccdphp/publications/aag/pdf/osh.pdf.
- 3.Giovino GA, Pederson LL, Trosclair A. The prevalence of selected cigarette smoking behaviors by occupational class in the United States. Proceedings from: Work, Smoking, and Health: A National Institute for Occupational Safety and Health Scientific Workshop; 2000 Jun 15–16; Washington. [Google Scholar]
- 4.Haenszel W, Shimkin MB, Miller HP. Tobacco smoking patterns in the United States. Public Health Monogr. 1956;45:1–105. [PubMed] [Google Scholar]
- 5.Nelson DE, Emont SL, Brackbill RM, Cameron LL, Peddicord J, Fiore MC. Cigarette smoking prevalence by occupation in the United States. J Occup Med. 1994;36:516–25. A comparison between 1978 to 1980 and 1987 to 1990. [PubMed] [Google Scholar]
- 6.Eakin JM. Work-related determinants of health behavior. In: Goochman DS, editor. Handbook of health behavior research. New York: Plenum Press; 1997. pp. 337–52. [Google Scholar]
- 7.Siegrist J, Rodel A. Work stress and health risk behavior. Scand J Work Environ Health. 2006;32:473–81. doi: 10.5271/sjweh.1052. [DOI] [PubMed] [Google Scholar]
- 8.Sterling T, Weinkam J. The confounding of occupation and smoking and its consequences. Soc Sci Med. 1990;30:457–67. doi: 10.1016/0277-9536(90)90348-v. [DOI] [PubMed] [Google Scholar]
- 9.Cherek DR. Effects of acute exposure to increased levels of background industrial noise on cigarette smoking behavior. Int Arch Occup Environ Health. 1985;56:23–30. doi: 10.1007/BF00380697. [DOI] [PubMed] [Google Scholar]
- 10.Fujino Y, Iso H, Tamakoshi A. A prospective cohort study of perceived noise exposure at work and cerebrovascular diseases among male workers in Japan. J Occup Health. 2007;49:382–8. doi: 10.1539/joh.49.382. [DOI] [PubMed] [Google Scholar]
- 11.Stanbury M, Rafferty AP, Rosenman K. Prevalence of hearing loss and work-related noise-induced hearing loss in Michigan. J Occup Environ Med. 2008;50:72–9. doi: 10.1097/JOM.0b013e31815b568c. [DOI] [PubMed] [Google Scholar]
- 12.Finkelstein DM, Kubzansky LD, Goodman E. Social status, stress, and adolescent smoking. J Adolesc Health. 2006;39:678–85. doi: 10.1016/j.jadohealth.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 13.Jun HJ, Rich-Edwards JW, Boynton-Jarrett R, Wright RJ. Intimate partner violence and cigarette smoking: association between smoking risk and psychological abuse with and without co-occurrence of physical and sexual abuse. Am J Public Health. 2008;98:527–35. doi: 10.2105/AJPH.2003.037663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Krieger N, Waterman PD, Hartman C, Bates LM, Stoddard AM, Quinn MM, et al. Social hazards on the job: workplace abuse, sexual harassment, and racial discrimination —a study of black, Latino, and white low-income women and men workers in the United States. Int J Health Serv. 2006;36:51–85. doi: 10.2190/3EMB-YKRH-EDJ2-0H19. [DOI] [PubMed] [Google Scholar]
- 15.Kivimaki M, Elovainio M, Vahtera J. Workplace bullying and sickness absence in hospital staff. Occup Environ Med. 2000;57:656–60. doi: 10.1136/oem.57.10.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunnarsdottir HK, Sveinsdottir H, Bernburg JG, Fridriksdottir H, Tomasson K. Lifestyle, harassment at work and self-assessed health of female flight attendants, nurses and teachers. Work. 2006;27:165–72. [PubMed] [Google Scholar]
- 17.Bennett GG, Wolin KY, Robinson EL, Fowler S, Edwards CL. Perceived racial/ethnic harassment and tobacco use among African American young adults. Am J Public Health. 2005;95:238–40. doi: 10.2105/AJPH.2004.037812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borrell LN, Jacobs DR, Jr, Williams DR, Pletcher MJ, Houston TK, Kiefe CI. Self-reported racial discrimination and substance use in the Coronary Artery Risk Development in Adults Study. Am J Epidemiol. 2007;166:1068–79. doi: 10.1093/aje/kwm180. [DOI] [PubMed] [Google Scholar]
- 19.Guthrie BJ, Young AM, Williams DR, Boyd CJ, Kintner EK. African American girls' smoking habits and day-to-day experiences with racial discrimination. Nurs Res. 2002;51:183–90. doi: 10.1097/00006199-200205000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Harris R, Tobias M, Jeffreys M, Waldegrave K, Karlsen S, Nazroo J. Racism and health: the relationship between experience of racial discrimination and health in New Zealand. Soc Sci Med. 2006;63:1428–41. doi: 10.1016/j.socscimed.2006.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61:1576–96. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Landrine H, Klonoff EA. Racial discrimination and cigarette smoking among blacks: findings from two studies. Ethn Dis. 2000;10:195–202. [PubMed] [Google Scholar]
- 23.Krieger N. Embodying inequality: a review of concepts, measures, and methods for studying health consequences of discrimination. Int J Health Serv. 1999;29:295–352. doi: 10.2190/M11W-VWXE-KQM9-G97Q. [DOI] [PubMed] [Google Scholar]
- 24.Department of Health and Human Services (US) 1998 Surgeon General's report —tobacco use among U.S. racial/ethnic minority groups. Atlanta: Centers for Disease Control and Prevention (US); 1998. [Google Scholar]
- 25.Lundberg U. Stress responses in low-status jobs and their relationship to health risks: musculoskeletal disorders. Ann N Y Acad Sci. 1999;896:162–72. doi: 10.1111/j.1749-6632.1999.tb08113.x. [DOI] [PubMed] [Google Scholar]
- 26.Quinn MM, Sembajwe G, Stoddard AM, Kriebel D, Krieger N, Sorensen G, et al. Social disparities in the burden of occupational exposures: results of a cross-sectional study. Am J Ind Med. 2007;50:861–75. doi: 10.1002/ajim.20529. [DOI] [PubMed] [Google Scholar]
- 27.Barbeau EM, Hartman C, Quinn MM, Stoddard AM, Krieger N. Methods for recruiting white, black, and Hispanic working-class women and men to a study of physical and social hazards at work: the United for Health study. Int J Health Serv. 2007;37:127–44. doi: 10.2190/B0N2-5850-6467-0230. [DOI] [PubMed] [Google Scholar]
- 28.Office of Applied Studies, Substance Abuse and Mental Health Services Administration (US) Development of computer-assisted interviewing procedures for the National Household Survey on Drug Abuse. Washington: SAMHSA; 2001. [Google Scholar]
- 29.Census Bureau (US) Poverty thresholds for 2003 by size of family and number of related children under 18 years. [cited 2009 Oct]. Available from: URL: http://www.census.gov/hhes/www/poverty/threshld/thresh03.html.
- 30.Cigarette smoking among adults—United States, 1992 and changes in the definition of current cigarette smoking. MMWR Morb Mortal Wkly Rep. 1994;43(19):342–6. [PubMed] [Google Scholar]
- 31.Richman JA, Rospenda KM, Nawyn SJ, Flaherty JA, Fendrich M, Drum ML, et al. Sexual harassment and generalized workplace abuse among university employees: prevalence and mental health correlates. Am J Public Health. 1999;89:358–63. doi: 10.2105/ajph.89.3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fitzgerald LF, Drasgow F, Hulin CL, Gelfand MJ, Magley VJ. Antecedents and consequences of sexual harassment in organizations: a test of an integrated model. J Appl Psychol. 1997;82:578–89. doi: 10.1037/0021-9010.82.4.578. [DOI] [PubMed] [Google Scholar]
- 33.American National Standard Institute. Draft American National Standard: evaluating the effectiveness of hearing conservation programs. New York: Acoustical Society of America; 1991. [Google Scholar]
- 34.World Health Organization. Occupational and community noise. Geneva: WHO; 2001. [Google Scholar]
- 35.European Community Respiratory Health Survey. ECRHS I. London: Department of Public Health Medicine UMDS St. Thomas Campus; 1993. [Google Scholar]
- 36.Ferris BG. Epidemiology Standardization Project (American Thoracic Society) Am Rev Respir Dis. 1978;118(6 Pt 2):1–120. [PubMed] [Google Scholar]
- 37.Bellamy SL, Gibberd R, Hancock L, Howley P, Kennedy B, Klar N, et al. Analysis of dichotomous outcome data for community intervention studies. Stat Methods Med Res. 2000;9:135–59. doi: 10.1177/096228020000900205. [DOI] [PubMed] [Google Scholar]
- 38.SAS Institute, Inc. SAS®: Version 9.2 for Windows. Cary (NC): SAS Institute, Inc; 2008. [Google Scholar]
- 39.King G, Honaker J, Joseph A, Scheve K. Analyzing incomplete political science data: an alternative algorithm for multiple imputation. Am Poli Sci Rev. 2001;95:49–69. [Google Scholar]
- 40.Krieger N. Discrimination and health. In: Berkman LF, Kawachi I, editors. Social epidemiology. New York: Oxford University Press; 2000. pp. p. 36–75. [Google Scholar]
- 41.Spielholz P, Silverstein B, Morgan M, Checkoway H, Kaufman J. Comparison of self-report, video observation and direct measurement methods for upper extremity musculoskeletal disorder physical risk factors. Ergonomics. 2001;44:588–613. doi: 10.1080/00140130118050. [DOI] [PubMed] [Google Scholar]
- 42.Brower PS, Attfield MD. Reliability of reported occupational history information for US coal miners, 1969–1977. Am J Epidemiol. 1998;148:920–6. doi: 10.1093/oxfordjournals.aje.a009718. [DOI] [PubMed] [Google Scholar]
- 43.Ikin JF, Fritschi L, Sim MR. Reproducibility of survey results from a study of occupation-related respiratory health in the aluminum industry. Appl Occup Environ Hyg. 2002;17:774–82. doi: 10.1080/10473220290096023. [DOI] [PubMed] [Google Scholar]
- 44.Hodson G, Esses VM. Distancing oneself from negative attributes and the personal/group discrimination discrepancy. J Experiment Soc Psychol. 2002;38:500–7. [Google Scholar]
- 45.Allison P. Missing data. Thousand Oaks (CA): Sage Publications; 2002. [Google Scholar]
- 46.Department of Labor, Bureau of Labor Statistics (US) Union members summary. 2008. [cited 2009 Jun 11]. Available from: URL: http://www.bls.gov/news.release/union2.nr0.htm.
- 47.Yates MD. Why unions matter. New York: Monthly Review Press; 1998. [Google Scholar]
- 48.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14:32–8. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- 49.Youth tobacco surveillance—United States, 2000 [published erratum appears in MMWR Surveill Summ 2001;50(46):1036] MMWR Surveill Summ. 2001;50(4):1–84. [PubMed] [Google Scholar]
- 50.Frumkin H, Walker ED, Friedman-Jimenez G. Minority workers and communities. Occup Med. 1999;14:495–517. [PubMed] [Google Scholar]
- 51.Murray LR. Sick and tired of being sick and tired: scientific evidence, methods, and research implications for racial and ethnic disparities in occupational health. Am J Public Health. 2003;93:221–6. doi: 10.2105/ajph.93.2.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sorensen G, Stoddard A, Hammond SK, Hebert JR, Avrunin JS, Ockene JK. Double jeopardy: workplace hazards and behavioral risks for craftspersons and laborers. Am J Health Promot. 1996;10:355–63. doi: 10.4278/0890-1171-10.5.355. [DOI] [PubMed] [Google Scholar]