SYNOPSIS
Objectives
West Nile virus (WNV) continues to cause seasonal epidemics of neuroinvasive disease and febrile illness, which have been most dramatic in the central plains states. We studied the epidemiology of WNV disease in North Dakota (ND), a highly epidemic state, six years following its first appearance in the state.
Methods
We analyzed information from cases of WNV disease reported to the ND Department of Health during August 2002 through December 2007.
Results
A total of 1,246 cases of WNV disease were reported in ND; 183 cases experienced neuroinvasive disease, including meningitis, encephalitis, or acute flaccid paralysis. Risk factors associated with developing neuroinvasive disease rather than West Nile fever included older age, male gender, and residence in a rural area. Annual cumulative incidence of neuroinvasive disease in ND ranged from 0.3 per 100,000 population to 14.6 per 100,000 population.
Conclusions
Annual cumulative incidence rates of West Nile neuroinvasive disease suggest that this region offers favorable conditions for its continued enzootic transmission, which highlights the need for improved targeted prevention measures, particularly for rural areas of the state.
West Nile virus (WNV) is naturally maintained within Culex mosquito-avian transmission cycles.1 Culex tarsalis is the primary vector for WNV in North Dakota (ND).2 Upon incidental infection, clinical symptoms in people may appear within three to 14 days and include fever, headache, and fatigue. In severe cases, WNV disease can progress to a neuroinvasive disease resulting in encephalitis or meningitis. Approximately one out of 140 infected people will develop neuroinvasive disease.3
WNV emerged in New York City (NYC) in 19994 and has progressively spread across North America. Introduction of WNV into new regions of the United States has typically been characterized by a relatively low number of human cases during the initial year, followed by amplification to epidemic levels during the subsequent season.5 ND experienced its first cases of WNV disease during 2002 (n=17) followed by a 36-fold increase in cases during 2003 (n=617). Presently, WNV continues to cause seasonal epidemics of neuroinvasive disease and febrile illness, which have been most dramatic in the central plains states, leading one to suspect that this region offers favorable conditions for its continued enzootic transmission.2 In this article, we describe the epidemiology of WNV disease in ND, a highly epidemic state, six years following its first appearance in the state.
METHODS
In ND, human cases of WNV disease are reported directly to the North Dakota Department of Health (NDDoH) through a passive surveillance system. The majority of case reports originate from physicians' offices and laboratories. Cases are classified as either West Nile neuroinvasive disease (i.e., meningitis, encephalitis, or acute flaccid paralysis), West Nile fever, other clinical illness, or unspecified illness. Confirmed and probable cases of WNV disease were defined as described previously.6 We analyzed information from cases of WNV disease (confirmed and probable) reported from August 2002 through December 2007. The NDDoH used a standardized case history form to collect demographic and clinical information about cases that met specific criteria for WNV disease. Variables collected through the surveillance system included race, gender, year of birth, date of onset, hospitalization status, and clinical symptoms. We estimated age by subtracting year of birth from year of disease onset for each case.
We defined a rural area according to the Rural-Urban Commuting Area (RUCA) coding (version 2.0) scheme.7 We calculated annual incidence of neuroinvasive disease as cases per 100,000 population using 2000 U.S. Census data (http://www.census.gov) We then conducted univariate and bivariate analyses using SAS® version 9.1.8 This study was approved by the University of South Dakota Institutional Review Board.
RESULTS
From August 2002 through December 2007, a total of 1,246 cases of WNV disease were reported to NDDoH. The median age at onset for cases was 47 years (range: 2–95 years). Men represented 58% (n=725) of all cases. Seventy-six percent (n=950) of cases were white, 3% (n=30) were American Indian, and race was not reported for 21% (n=266). Sixty-six percent (n=821) of cases resided in a rural area. Dates of illness onset for all cases ranged from June 1 to November 7 during all six years of the study (Table 1).
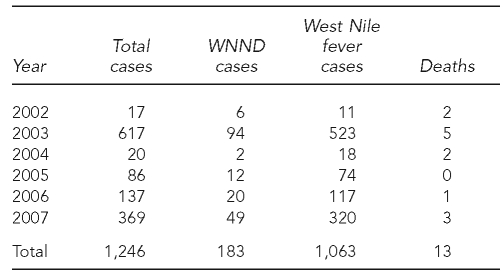
Table 1.
Human West Nile virus disease cases by clinical syndrome, North Dakota, 2002–2007a
aNorth Dakota Department of Health. West Nile virus data summaries, 2002–2007 [cited 2009 Jan 5]. Available from: URL: http://www.ndhealth.gov/WNV/Data/Summary.aspx
WNND = West Nile neuroinvasive disease
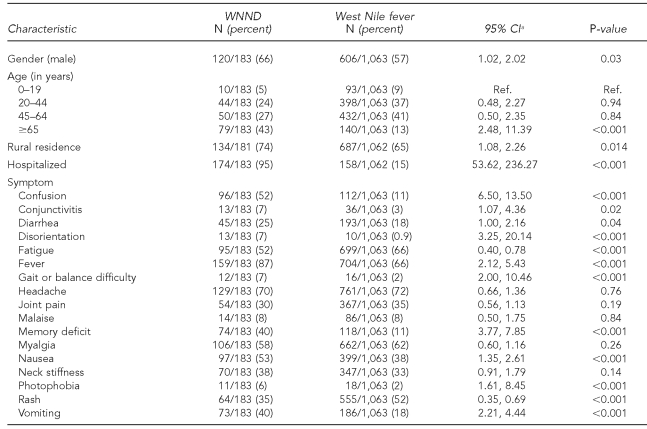
Of the 1,246 cases, 1,063 were classified as West Nile fever and 183 as West Nile neuroinvasive disease (Table 1). The median age of people who were hospitalized for their disease was 58 years (range: 5–95 years). Not surprisingly, a greater proportion of the cases with West Nile neuroinvasive disease were hospitalized (95%) compared with West Nile fever cases (15%, p<0.001). The neuroinvasive disease cases also reported a greater frequency of severe symptoms such as memory deficit (40%) and gait or balance difficulty (7%) than did the West Nile fever cases (11% memory deficit and 2% gait or balance difficulty, both p<0.001). Rash was reported among 35% of neuroinvasive disease cases compared with 52% of West Nile fever cases (p<0.001). Thirteen cases (1%) died of their disease. Among those who died with WNV disease, 77% (10/13) were male and the median age was 81 years (range: 67–95 years). Ninety-two percent (12/13) had encephalitis or meningitis and 92% (12/13) were hospitalized. Significant risk factors for developing West Nile neuroinvasive disease identified on bivariate analysis included older age, male gender, and residing in a rural area (Table 2).
Table 2.
Characteristics of West Nile virus cases reported in North Dakota, 2002–2007
a95% CIs correspond to an odds ratio.
WNND = West Nile neuroinvasive disease
CI = confidence interval
Ref. = reference group
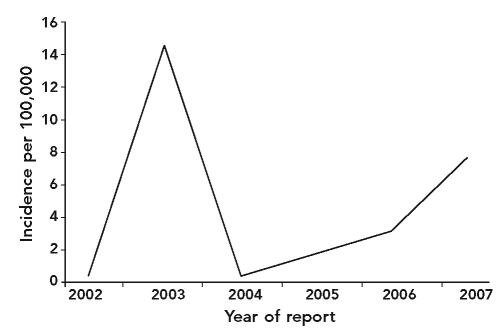
Annual cumulative incidence of neuroinvasive disease in ND ranged from 0.3 per 100,000 population to 14.6 per 100,000 population during the six-year study period (Figure). McLean (118.1 cases/100,000 population), Stutsman (54.8 cases/100,000 population), Morton (47.4 cases/100,000 population), Stark (39.8 cases/100,000 population), Burleigh (24.5 cases/100,000 population), Ward (23.8 cases/100,000 population), and Cass (17.1 cases/100,000 population) counties had a high cumulative incidence of neuroinvasive disease cases during 2002–2007 and consistently had cases of neuroinvasive disease during this time period.
Figure.
Incidence of West Nile neuroinvasive disease in North Dakota, 2002–2007
DISCUSSION
This article summarizes the epidemiologic characteristics of a large population of WNV cases identified through the NDDoH disease surveillance system. Among the case population, 15% experienced neuroinvasive disease. Bivariate analysis revealed that older age and male gender were significant predictors of developing neuroinvasive disease, which have been identified previously.9 Residence in a rural area was also identified as a risk factor for developing neuroinvasive disease rather than West Nile fever. DeGroote et al. reported residence in a rural area as a risk factor for neuroinvasive disease among cases of WNV disease in Iowa, according to surveillance data.10 This finding was in contrast to other studies that reported a predominance of urban/suburban occurrence. Our study finding may be explained in part by the large percentage of people living in rural areas in ND (52%) and the scarcity of aerial spraying of mosquito adulticide in rural areas compared with urban areas.
Limitations
One limitation of this study was that case reporting through ND is a passive surveillance system, dependent on the reporting of cases by health-care providers and laboratories to NDDoH. As a result, reporting to NDDoH is likely incomplete (leading to an underestimation of the true disease incidence) and may be variable by jurisdiction, and even over time within a jurisdiction. Reporting differences between West Nile neuroinvasive disease and West Nile fever also exist. Neuroinvasive disease case reporting is relatively complete compared with West Nile fever case reporting, largely because serious cases are more likely to be reported than mild cases. Presently, the majority of human WNV testing in ND is performed at the state public health laboratory; however, commercial testing kits are becoming more widely available for use in ND and other areas in the U.S.
CONCLUSION
The number of reported cases of WNV disease in ND has varied considerably from 2002 through 2007. However, annual cumulative incidence rates of neuroinvasive disease in ND remain substantially higher than those for other states,11,12 suggesting that epidemic transmission of WNV will continue during subsequent years. This highlights the need for improved targeted prevention measures, particularly for rural areas of the state.
REFERENCES
- 1.Komar N. West Nile virus: epidemiology and ecology in North America. Adv Virus Res. 2003;61:185–234. doi: 10.1016/s0065-3527(03)61005-5. [DOI] [PubMed] [Google Scholar]
- 2.Bell JA, Brewer CM, Mickelson NJ, Garman GW, Vaughan JA. West Nile virus epizootiology, central Red River Valley, North Dakota and Minnesota, 2002–2005. Emerg Infect Dis. 2006;12:1245–7. doi: 10.3201/eid1208.060129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mostashari F, Bunning ML, Kitsutani PT, Singer DA, Nash D, Cooper MJ, et al. Epidemic West Nile encephalitis, New York, 1999: results of a household-based seroepidemiological survey. Lancet. 2001;358:261–4. doi: 10.1016/S0140-6736(01)05480-0. [DOI] [PubMed] [Google Scholar]
- 4.Nash D, Mostashari F, Fine A, Miller J, O'Leary D, Murray K, et al. The outbreak of West Nile virus infection in the New York City area in 1999. N Engl J Med. 2001;344:1807–14. doi: 10.1056/NEJM200106143442401. [DOI] [PubMed] [Google Scholar]
- 5.Reisen W, Lothrop H, Chiles R, Madon M, Cossen C, Woods L, et al. West Nile virus in California. Emerg Infect Dis. 2004;10:1369–78. doi: 10.3201/eid1008.040077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Council of State and Territorial Epidemiologists. Position statement: revision of the national surveillance case definition of diseases caused by neurotropic domestic arboviruses, including the addition to the NNDSS of non-neuroinvasive illnesses caused by these viruses. [cited 2008 Jun 24]. Available from: URL: http://www.cste.org/ps/2004pdf/04-ID-01-final.pdf.
- 7.Rural Health Research Center, University of Washington. Rural-urban commuting area codes (RUCAs) [cited 2008 Dec 31]. Available from: URL: http://depts.washington.edu/uwruca.
- 8.SAS Institute, Inc. Cary (NC): SAS Institute, Inc.; 2006. SAS®: Version 9.1 for Windows. [Google Scholar]
- 9.Jean CM, Honarmand S, Louie JK, Glaser CA. Risk factors for West Nile virus neuroinvasive disease, California, 2005. Emerg Infect Dis. 2007;13:1918–20. doi: 10.3201/eid1312.061265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.DeGroote JP, Sugumaran R, Brend SM, Tucker BJ, Bartholomay LC. Landscape, demographic, entomological, and climatic associations with human disease incidence of West Nile virus in the state of Iowa, USA. Int J Health Geogr. 2008;7:19. doi: 10.1186/1476-072X-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lindsey NP, Kuhn S, Campbell GL, Hayes EB. West Nile virus neuroinvasive disease incidence in the United States, 2002–2006. Vector Borne Zoonotic Dis. 2008;8:35–9. doi: 10.1089/vbz.2007.0137. [DOI] [PubMed] [Google Scholar]
- 12.West Nile virus activity—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(26):720–3. [PubMed] [Google Scholar]