SYNOPSIS
Objective
We determined how Asian and Pacific Islanders (APIs) differ from clients from other ethnic groups in regard to drug use and admissions to drug treatment programs.
Methods
We used national survey and treatment admissions data to characterize drug problems and first-time adult admissions to publicly funded drug treatment programs in the U.S. in 2005.
Results
APIs accounted for 1.9% of illicit drug use in U.S. adults and for 1.3% of adult clients entering drug treatment for the first time. Compared with other ethnic groups, APIs were significantly more likely to be entering treatment for the first time. Stimulants were the primary drug problem for 57.3% of API first-time treatment clients, a significantly greater proportion than other ethnic groups. This figure had increased from 45.3% in 2001, significantly greater than the increase among Caucasian or African American clients. API first-time admissions had used drugs less frequently (13.6 days in the prior 30 days), began drug use at a slightly older age (mean = 20.7 years), and had a shorter period between start of use and first admission (mean = 9.4 years) than other racial/ethnic groups.
Conclusions
Stimulant use was the predominant problem of API clients entering treatment for the first time. APIs were underrepresented in the treatment system relative to their share of the population with drug problems. Diverse groups were aggregated to form the API category. Information on APIs needs to be disaggregated to develop more culturally appropriate and effective treatment.
The literature provides a conflicting picture of drug use among Asian and Pacific Islanders (APIs) in the United States. According to one view, APIs do not have a serious drug use problem. School-age Asians are less likely to use drugs, alcohol, and cigarettes than their peers from other racial/ethnic groups.1,2 Drug use prevalence among Asian Americans for the three most reported drugs—tranquilizers (15.8%), marijuana (12.5%), and painkillers (9.8%)—was less than in Caucasians (29.6%, 36.7%, and 25.8% respectively).3 A comparison between Asian and Caucasian college students found that Asian students were five times more likely to abstain from alcohol and five times less likely to engage in heavy drinking.4
The opposing view holds that the drug problems of the API community have been obscured by the stereotype of the “model minority” and the lack of available data.5,6 This view is supported by evidence that drug use by APIs is increasing. A national survey of drug use and health found that illicit drug use among Asians aged 18 years and older increased by 35.0% between 2000 and 2005, from 2.3% to 3.1%.7,8 Problems with specific drugs have been documented in API ethnic groups, including Mien,9,10 Filipino, Chinese, and Vietnamese,11 as well as API men who have sex with men.12 Adult inhalant abuse was found to be increasing faster among APIs than other ethnic groups.13 Stimulant abuse is a growing problem among API women.14
The number of individuals of API descent who entered publicly funded drug treatment increased by 46% between 1994 and 2001, a much higher increase than was observed for other racial/ethnic groups.15 While there is evidence that API drug users are less likely to get treatment,5,9,16 there is less information about API clients of drug treatment programs and how they differ from clients in other racial/ethnic groups.17,18 APIs are projected to exceed 9% of the U.S. population by 2050,19 and information is needed on the potential demand for treatment from this growing community.
We examined national survey data on illicit drug use to characterize potential demand for treatment from APIs. We used data on admissions to drug treatment programs to characterize individuals entering treatment, comparing APIs with clients of other racial/ethnic backgrounds. We examined whether the admissions of API drug users were more likely to be for first-time treatment. We evaluated data on the population of first-time treatment clients to determine if APIs differed in primary drug problem, frequency of drug use, age at admission, or age at first use. We studied trends of ethnic groups by comparing 2005 findings with data from 2001.
METHODS
Treatment episode dataset
We studied data on admissions to publicly funded drug abuse treatment programs in the Treatment Episode Data Set (TEDS), a 17-item abstract of admissions to U.S. treatment programs collected by the U.S. Substance Abuse and Mental Health Services Administration (SAMHSA).20,21 Data are obtained from all facilities that receive federal public funding through a state agency. TEDS data represent 83% of the TEDS eligible admissions and 67% of the total known treatment admissions in the U.S.15
We examined data from 2001 and 2005 and limited our analysis to adults to be consistent with the literature, which considers adults separately from adolescent drug users.3,13,22 We excluded admissions of people younger than 18 years of age; admissions that were exclusively for alcohol treatment; and any observation that had a missing value for age, gender, primary drug use, frequency of use, or the number of prior treatment attempts.
To focus on current problems facing the treatment system, we characterized clients entering treatment for the first time. TEDS is a dataset of treatment admissions rather than clients. Because it does not provide a client identifier, it is not possible to identify the records that are the repeated treatments of a single client already in the dataset. Each admission record includes the number of prior treatment attempts. We created a dataset of clients by selecting records in which there were no previous treatment attempts. Using TEDS data from 2001 and 2005, we also identified clients who entered treatment for the first time.
Adult patients were assigned to one of five ethnic groups: API, Caucasian, African American, Latino, and other. The API group consisted of people descended from residents of the Far East, the Indian subcontinent, Southeast Asia, or the Pacific Islands. TEDS aggregates APIs as a single category, without specifying the specific Asian ethnicity. We designated as Latino the following TEDS ethnic reporting groups: Puerto Rican, Mexican, Cuban, other specified Hispanic, and Hispanic, not specified. The residual category of “other race” comprised individuals who were Alaska Native, American Indian, another race, or reported two or more races.
TEDS includes 12 categories for primary substance problem. We collapsed these categories into five groups: cocaine, other stimulant, marijuana, opiate, and other. We grouped stimulant, amphetamine, and other nonamphetamine stimulants as “stimulant.” Cocaine and crack were categorized as “cocaine.” We separated cocaine from other stimulants to determine if the frequency of use for these two categories of drugs differed across ethnic groups. We characterized heroin, nonprescription methadone, and other opiates as “opiates.” We included the following in the group “other”: hallucinogens, phencyclidine, inhalants, tranquilizers, barbiturates, over-the-counter medications, and the residual TEDS reporting category of “all other.”
TEDS collects both the age of admission and age at first use as a categorical variable with 12 possible responses. We transformed this categorical response into a continuous variable by assuming values were middle of the range. We estimated the years since start of use as the difference between age at admission and age at first use.
TEDS records the frequency of drug use in the past 30 days as a categorical variable with five possible responses. We transformed this categorical response into a continuous variable by assuming values were at the middle of the range. We transformed categorical responses to continuous variables to provide an intuitive understanding of differences among groups that would not have been possible with a categorical analytic method.
National Survey on Drug Use and Health
We examined data on current illicit drug use from the 2005 National Survey on Drug Use and Health (NSDUH), also collected by SAMHSA.7 This national survey asks people aged 12 years and older about illicit drug use in the prior 30 days. It excludes active-duty military personnel, people with no fixed household address, and institutional residents. We selected data on people aged 18 years and older to be consistent with our analysis of TEDS. We reanalyzed these data to aggregate APIs into a single group to be consistent with the API category used in TEDS.
Statistical analysis
We compared differences in categorical variables among the five racial/ethnic groups using a Chi-square test. If the overall Chi-square test was significant, we compared each pair of ethnic groups for each category, creating a series of 2 × 2 tables. We tested significance using the Scheffe corrected Chi-square statistic (i.e., using the square root of the overall Chi-square as the critical Chi-square value for the 2 × 2 tables).
We examined whether continuous variables differed by racial/ethnic groups using multivariate regression. The continuous variable was the dependent variable in a regression that used indicators for membership in racial/ethnic groups as independent variables. We compared the statistical significance of differences in parameters for ethnic groups with post-hoc hypothesis tests that used the regression variance-covariance matrix.
We used multinomial logistic regression to test whether the change from 2001 to 2005 in the proportion of first-time clients who had a particular drug as their primary problem differed significantly by ethnic group. The change in proportion is the percentage difference between 2001 and 2005. Independent variables were indicators of racial/ethnic group, year, and interaction between year and ethnic group. We reported the statistical significance of the parameters for interaction.
RESULTS
Our analysis of data from the 2005 NSDUH found that 1.9% of individuals aged 18 years and older who used illicit drugs in the prior 30 days were APIs.7
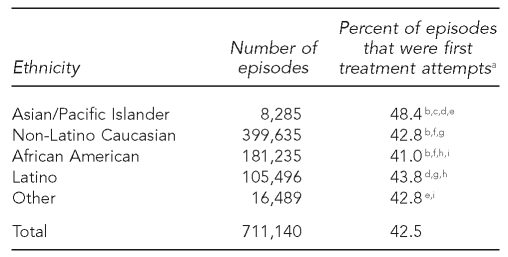
TEDS reported 1.8 million admissions in 2005. We excluded 780,353 admissions that were primarily for treatment of alcohol problems; 112,118 admissions that involved people younger than 18 years of age; and an additional 182,658 observations that had at least one missing field. This left 711,140 adult admissions for drug treatment. Of these, 42.5% were first-time treatment attempts (Table 1). First-time treatment attempts were more common in the admissions of API drug users (48.4%). This percentage was significantly greater than the percentage of admissions that were first-time treatment attempts in the four other groups.
Table 1.
Number of U.S. substance abuse treatment episodes and episodes that were first treatment attempts, by racial/ethnic group, 2005
aFootnotes b through i represent a significant difference between groups (p<0.001).
bAPI vs. Caucasian
cAPI vs. African American
dAPI vs. Latino
eAPI vs. other
fCaucasian vs. African American
gCaucasian vs. Latino
hAfrican American vs. Latino
iAfrican American vs. other
API = Asian/Pacific Islander
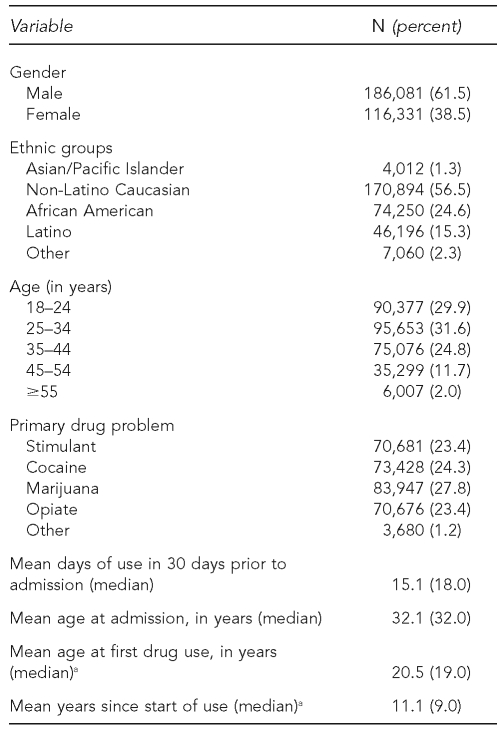
The study cohort comprised 302,412 adult clients who obtained drug treatment for the first time in 2005 (Table 2). The sample was 61.5% male, and individuals of API descent comprised 1.3% of the cohort. A stimulant or cocaine was the primary drug used in 47.7% of first-time clients; marijuana was the primary drug used in another 27.8% of first-time clients. The study cohort had used illicit drugs for a mean of 15.1 days in the 30 days prior to admission. The mean age at treatment admission was 32.1 years. Clients reported that they were a mean of 20.5 years of age when they first used illicit drugs; however, 21.5% of observations did not include this information. Among these observations, there was a mean of 11.1 years between first drug use and first admission to treatment.
Table 2.
Characteristics of U.S. substance abuse clients in their first treatment attempt, by racial/ethnic group, 2005 (n=302,412)
aThe sample had 21.5% of observations with missing values for this variable.
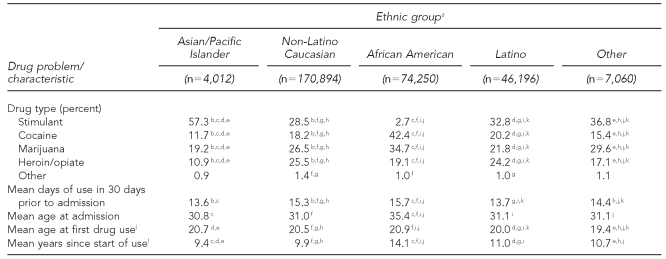
As shown in Table 3, stimulants were the primary drug use problem by ethnic group. Stimulants were the primary drug problem of 57.3% of API first-time treatment clients—a significantly higher proportion than was observed among new treatment entrants who were Caucasian (28.5%), Latino (32.8%), African American (2.7%), or from other ethnic groups (36.8%).
Table 3.
Primary drug problem and other characteristics of U.S. substance abuse treatment clients in their first treatment attempt in 2005, by racial/ethnic group
aFootnotes b through k represent a significant difference between groups (p<0.001).
bAPI vs. Caucasian
cAPI vs. African American
dAPI vs. Latino
eAPI vs. other
fCaucasian vs. African American
gCaucasian vs. Latino
hCaucasian vs. other
iAfrican American vs. Latino
jAfrican American vs. other
kLatino vs. other
lThe sample had 21.5% of observations with missing values for this variable.
API = Asian/Pacific Islander
Cocaine, marijuana, and opiates were the primary drug problem of 11.7%, 19.2%, and 10.9% of API first-time treatment admissions, respectively. All three drugs were significantly less likely to be the primary drug problem of APIs than any other racial/ethnic group. Other drugs were the primary drug problem in 0.9% of API first-time clients. This was not significantly different from any other racial/ethnic group.
TEDS provides information on treatment admissions. We examined data on the age of first drug use, age at treatment admission, years since start of use, and frequency of drug use in the prior 30 days. As shown in Table 3, API first-time seekers were a mean of 20.7 years of age at the time of first drug use, which was significantly older than those in the Latino (20.0 years) and other (19.4 years) groups. API first-time treatment entrants were a mean of 30.8 years of age at the time of treatment admission, which was significantly younger than the African American group (35.4 years). We evaluated the years of drug use at the time of entry into treatment for each racial/ethnic group. First-time treatment seekers who were APIs had a mean of 9.4 years since start of use. This was significantly shorter than the years of use by those identifying as Caucasian (9.9), African American (14.1), Latino (11.0), or other (10.7). An analysis that controlled for primary drug problem reduced but did not eliminate the differences between APIs and the other groups.
We studied the frequency of drug use in the 30 days prior to entry into first-time treatment. API first-time treatment seekers had used drugs for a mean of 13.6 days (Table 3). This duration was significantly less than days of use reported by African American (15.7 days), Latino (13.7 days), and other (14.4 days) treatment entrants.
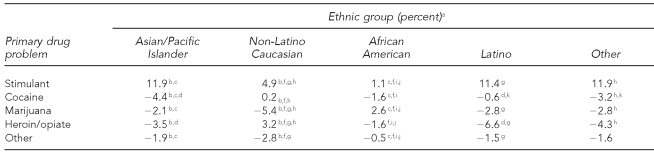
Table 4 describes the change in the primary drug problem of new treatment entrants between 2001 and 2005. Each drug presents the difference in the proportion of new treatment entrants with that problem, by ethnic group. For example, the +11.9% difference in API treatment entrants with stimulants as their primary problem represents the difference between 45.3% of API entrants who had this problem in 2001 and 57.3% who had it in 2005. This difference was significantly higher than the differences in Caucasians (4.9% gain) and African Americans (1.1% gain) who had stimulants as their primary drug problem.
Table 4.
Primary drug problem of new U.S. substance abuse treatment entrants and the difference in the proportion of entrants with this problem in 2001 vs. 2005, by racial/ethnic group
aFootnotes b through k represent a significant difference between two groups (p<0.001).
bAPI vs. Caucasian
cAPI vs. African American
dAPI vs. Latino
eAPI vs. other
fCaucasian vs. African American
gCaucasian vs. Latino
hCaucasian vs. other
iAfrican American vs. Latino
jAfrican American vs. other
kLatino vs. other
API = Asian/Pacific Islander
Among new treatment entrants who were APIs, the difference in percentage with cocaine as their primary problem was 4.4% lower in 2005 than in 2001. This disparity was significantly different from the disparities for Caucasian (0.2% gain), African American (1.6% loss), and Latino (0.6% loss) treatment entrants.
The difference in percentage of API new treatment entrants with marijuana as their primary problem was 2.1% lower in 2005 than in 2001, which was significantly different from Caucasians (5.4% loss) and African Americans (2.6% gain). The difference in percentage of API new treatment entrants who had other drugs as their primary problem was 1.9% lower in 2005 than in 2001. The difference was significantly different from Caucasian (2.8% loss) and African American (0.5% loss) treatment entrants.
DISCUSSION
Individuals of API descent comprise more than 4.0% of the U.S. population.23 We found that in 2005, APIs accounted for 1.9% of the adult population that used drugs. We evaluated data from publicly funded drug treatment programs and found that APIs comprised only 1.3% of the adults who entered drug treatment for the first time in 2005.
There are several possible reasons to explain why treatment entrants were less likely to be of API descent. We found that illicit drug use is less prevalent in the API community, but this finding provides only part of the explanation. API drug users may be less likely to enter treatment programs, particularly public treatment programs, because they are more likely to have private insurance.
These survey data do not show the social context of API substance use behavior. There is evidence that APIs prefer to deal with crises within the family before seeking outside help, and that a sense of shame about drug use leads to a delay in seeking treatment.17,24,25 The stigma of drug use may lead to underreporting of prevalence of illicit drug use among APIs in national surveys. APIs also face institutional barriers to treatment.5,16,26
We found evidence that severity of illness in those seeking treatment for the first time may be lower in APIs. API clients began drug use at an older age, entered treatment at a younger age, had a shorter drug use history, and used drugs less frequently than clients from many other racial/ethnic groups. Contrary to earlier observations, this evidence suggests that API drug users may be more likely to enter treatment, given the severity of problems.
If APIs are more likely to enter treatment, this may be related to the high proportion of APIs with stimulants as their primary drug problem. Addiction to stimulants occurs faster, and the time from addiction to treatment is shorter compared with other drugs.27 We observed that new treatment entrants who had stimulants as their primary drug problem had a shorter drug use history at the time they entered treatment. Our analyses showed that API treatment entrants had a shorter drug use history, even after controlling for primary drug problem.
The data in TEDS do not represent all treatment services delivered in the U.S. In general, SAMHSA collects admission data from state-certified and licensed drug treatment agencies in the U.S. Due to licensing regulations, which differ from state to state, certain types of facilities are not consistently included in TEDS. Facilities that may not be counted in TEDS include (1) private facilities, (2) independent practitioners, (3) hospital-based drug treatment programs not certified by the state, (4) correctional facilities, and (5) federally funded treatment programs.15
The types of treatment excluded from the TEDS data are more likely to be covered by employer-funded medical insurance. The percentage of adult APIs without insurance coverage differs by studies.28,29 However, APIs living below the federal poverty level have a much higher uninsurance rate than their non-Hispanic white and African American counterparts.29 APIs were not more likely than other ethnic groups to have insurance coverage.29 It is thus unlikely that low rates of treatment seen in TEDS data are offset by high rates of substance abuse treatment funded by private insurance.
We found that API patients were more likely than patients from other racial/ethnic groups to be entering treatment for the first time. There are several possible explanations for this finding. It may be that drug use is only now emerging as a problem in the API community. It may be that APIs have good treatment outcomes and that they are less likely to repeat their treatments. It may be that there is effective community outreach to substance-abusing APIs that leads them to seek treatment. The stigma associated with treatment may be less evident among younger APIs. Finally, it may be that API treatment entrants did not have a positive experience in their first treatment attempt and, therefore, fewer returned for subsequent treatment.
Evidence suggests that drug-dependent APIs admitted to treatment had a more negative attitude toward treatment and were less likely to report a need or have received prior treatment than non-API drug-dependent users.17,18 Treatment mandated by the legal system, family coercion, or a lack of culturally appropriate treatment models may also explain why APIs who seek treatment are less likely to return for treatment, but evidence of this assertion is scarce.5,6,17,24 Substance-dependent APIs are less likely to show the need for treatment and less likely to seek treatment than Caucasians.17 The strong stigma associated with drug use in the API community and the lack of culturally appropriate treatment models may contribute to delays in obtaining treatment.,6,10,11
API racial status is a category that comprises races/ethnicities that are culturally and socially diverse, that have different drug problems, and that have different thresholds for seeking treatment. A number of studies provide details of these different drug use patterns and behaviors.
Use of illicit drugs is more prevalent among Pacific Islanders than among Asians. The 2005 NSDUH found that 8.7% of Native Hawaiian and other Pacific Islanders had used illicit drugs in the prior 30 days compared with 3.1% among Asians.7
Methamphetamines are an important drug problem among Filipinos.25 Filipinos who use this drug, which they call “shabu,” use multiple drugs and also inject heroin. Chinese and Vietnamese in the San Francisco area prefer to smoke crack; few inject drugs.11 API men who have sex with men reported mainly using ecstasy, marijuana, ketamine, and methamphetamine.12 Southeast Asian immigrants have a long history of opium use, and it has been a challenging task for treatment facilities to reach out to them.9
Limitations
This study had several limitations. It was limited by the small size of the API sample and the aggregation of APIs into a single category in the TEDS data. This consolidation prevents the understanding of possible differences in drug use behaviors among the different API cultural and ethnic groups. Surveys such as TEDS need to be modified to identify the specific Asian ethnicity of clients. This will identify which drugs are problems for specific ethnic groups, and the languages and cultures of clients who need treatment. It will also help providers comply with stimulant abuse treatment guidelines, which recommend that treatment reflect cultural sensitivity.30
We found that in 2005, the proportion of new treatment entrants with stimulants as their primary drug problem was higher among APIs than any other racial/ethnic group, and that growth in this group was greater among APIs than in any other group. This finding is consistent with literature suggesting that stimulants are the preferred drug of choice among APIs.14,22,25 The multiyear data comparison showed the admission rate for stimulants is higher and growing faster than other groups. There are possible explanations for this pattern. Stimulants may be familiar to APIs because they are commonly used in Asia.31–33 Stimulants are also affordable and easy to access in the local community.34 APIs, like people of other racial/ethnic groups, seek the physiological effects of stimulants or the social environment associated with using stimulants.12,25,35,36 It may mean that APIs using stimulants are finding themselves in need of treatment sooner compared with users of other drugs.27
CONCLUSION
Further investigation is needed to understand the problems of API drug users, the factors that influence their decision to seek treatment, and the elements of more successful treatment in this population. More investigation is needed of the API social environment to understand why stimulants are the predominant drug abused in this community. Effectiveness studies are needed to identify how stimulant abuse can be better addressed in mainstream treatment programs. Answers to these questions are becoming more important to the U.S. treatment system. Drug use is growing in this community and people of API origin are a rapidly growing part of the U.S. population.
Footnotes
This study was supported by the National Institute on Drug Abuse grant # P50 DA09253. The authors thank Carmen Masson, PhD, and Van Ta, PhD, MPH, who gave helpful reviews of an earlier version of this article; and Kevin Delucchi, PhD, for his advice on the statistical tests.
REFERENCES
- 1.JG Au, SI Donaldson. Social influences as explanations for substance use differences among Asian-American and European-American adolescents. J Psychoactive Drugs. 2000;32:15–23. doi: 10.1080/02791072.2000.10400208. [DOI] [PubMed] [Google Scholar]
- 2.E Maddahian, MD Newcomb, PM Bentler. Single and multiple patterns of adolescent substance use: longitudinal comparisons of four ethnic groups. J Drug Educ. 1985;15:311–26. doi: 10.2190/2UEC-5ADY-GJMB-4J6G. [DOI] [PubMed] [Google Scholar]
- 3.DG McLaughlin, JS Raymond, SR Murakami, D Goebert. Drug use among Asian Americans in Hawaii. J Psychoactive Drugs. 1987;19:85–94. doi: 10.1080/02791072.1987.10472383. [DOI] [PubMed] [Google Scholar]
- 4.T O'Hare. Differences in Asian and white drinking: consumption level, drinking contexts, and expectancies. Addict Behav. 1995; 20:261–6. doi: 10.1016/0306-4603(94)00061-1. [DOI] [PubMed] [Google Scholar]
- 5.DY Ja, B Aoki. Substance abuse treatment: cultural barriers in the Asian-American community. J Psychoactive Drugs. 1993;25:61–71. doi: 10.1080/02791072.1993.10472592. [DOI] [PubMed] [Google Scholar]
- 6.MM Mercado. The invisible family: counseling Asian American substance abusers and their families. Family J. 2000;8:267–72. [Google Scholar]
- 7.Office of Applied Studies. Results from the 2005 National Survey on Drug Use and Health: national findings. Rockville (MD): Department of Health and Human Services, Substance Abuse and Mental Health Services Administration (US); 2005. [Google Scholar]
- 8.Office of Applied Studies. 2000 National Survey on Drug Use and Health: detailed tables. Rockville (MD): Department of Health and Human Services, Substance Abuse and Mental Health Services Administration (US); 2000. [Google Scholar]
- 9.J Martin, JE Zweben. Addressing treatment needs of Southeast Asian Mien opium users in California. J Psychoactive Drugs. 1993; 25:73–6. doi: 10.1080/02791072.1993.10472593. [DOI] [PubMed] [Google Scholar]
- 10.J Westermeyer, T Lyfoung, M Westermeyer, J Neider. Opium addiction among Indochinese refugees in the United States: characteristics of addicts and their opium use. Am J Drug Alcohol Abuse. 1991;17:267–77. doi: 10.3109/00952999109027551. [DOI] [PubMed] [Google Scholar]
- 11.T Nemoto, B Aoki, K Huang, A Morris, H Nguyen, W Wong. Drug use behaviors among Asian drug users in San Francisco. Addict Behav. 1999;24:823–38. doi: 10.1016/s0306-4603(99)00020-9. [DOI] [PubMed] [Google Scholar]
- 12.KH Choi, D Operario, SE Gregorich, W McFarland, D MacKellar, L Valleroy. Substance use, substance choice, and unprotected anal intercourse among young Asian American and Pacific Islander men who have sex with men. AIDS Educ Prev. 2005;17:418–29. doi: 10.1521/aeap.2005.17.5.418. [DOI] [PubMed] [Google Scholar]
- 13.LT Wu, CL Ringwalt. Inhalant use and disorders among adults in the United States. Drug Alcohol Depend. 2006;85:1–11. doi: 10.1016/j.drugalcdep.2006.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Office of Applied Studies. The DASIS report: Asians and Pacific Islanders in substance abuse treatment admissions, 1999. Rockville (MD): Department of Health and Human Services, Substance Abuse and Mental Health Services Administration (US); 2002. [Google Scholar]
- 15.Office of Applied Studies. Treatment Episode Data Set (TEDS) 1994–2004: national admissions to substance abuse treatment services. Rockville (MD): Department of Health and Human Services, Substance Abuse and Mental Health Services Administration (US); 2006. [Google Scholar]
- 16.P Perez-Arce, KD Carr, JL Sorensen. Cultural issues in an outpatient program for stimulant abusers. J Psychoactive Drugs. 1993;25:35–44. doi: 10.1080/02791072.1993.10472589. [DOI] [PubMed] [Google Scholar]
- 17.JT Sakai, PM Ho, JH Shore, NK Risk, RK Price. Asians in the United States: substance dependence and use of substance-dependence treatment. J Subst Abuse Treat. 2005;29:75–84. doi: 10.1016/j.jsat.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 18.N Niv, EC Wong, YI Hser. Asian Americans in community-based substance abuse treatment: service needs, utilization, and outcomes. J Subst Abuse Treat. 2007;33:313–9. doi: 10.1016/j.jsat.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 19.Census Bureau (US). Washington: Department of Commerce (US); 2000. The Asian population: 2000. [Google Scholar]
- 20.Substance Abuse and Mental Health Services Administration (US). Treatment Episode Data Set (TEDS), 2001, vol. 2004. Rockville (MD): Department of Health and Human Services (US); 2004. [Google Scholar]
- 21.Substance Abuse and Mental Health Services Administration (US). Treatment Episode Data Set (TEDS), 2005, vol. 2007. Rockville (MD): Department of Health and Human Services (US); 2007. [Google Scholar]
- 22.D Operario, T Nemoto. Sexual risk behavior and substance use among a sample of Asian Pacific Islander transgendered women. AIDS Educ Prev. 2005;17:430–43. doi: 10.1521/aeap.2005.17.5.430. [DOI] [PubMed] [Google Scholar]
- 23.Census Bureau (US). Washington: Population Division, Census Bureau; 2006. Table 3: annual estimates of the population by sex, race, and Hispanic or Latin origin for the United States: April 1, 2000, to July 1, 2005 (NC-EST2005-03), vol. 2006. [Google Scholar]
- 24.SM Kwok. Research note: exploring the experiences of Chinese in drug treatment programs in Vancouver. Br J Social Work. 2000;30:663–72. [Google Scholar]
- 25.T Nemoto, D Operario, T Soma. Risk behaviors of Filipino methamphetamine users in San Francisco: implications for prevention and treatment of drug use and HIV. Public Health Rep. 2002;117(suppl 1):30–8. [PMC free article] [PubMed] [Google Scholar]
- 26.CE D'Avanzo. Southeast Asians: Asian-Pacific Americans at risk for substance misuse. Subst Use Misuse. 1997;32:829–48. doi: 10.3109/10826089709055861. [DOI] [PubMed] [Google Scholar]
- 27.F Gonzalez Castro, EH Barrington, MA Walton, RA Rawson. Cocaine and methamphetamine: differential addiction rates. Psychol Addict Behav. 2000;14:390–6. [PubMed] [Google Scholar]
- 28.N Ponce, RJ Nordyke, S Hirota. Uninsured working immigrants: a view from a California county. J Immigr Health. 2005;7:45–53. doi: 10.1007/s10903-005-1390-0. [DOI] [PubMed] [Google Scholar]
- 29.M Ro. Moving forward: addressing the health of Asian American and Pacific Islander women. Am J Public Health. 2002;92:516–9. doi: 10.2105/ajph.92.4.516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.RA Rawson. Treatment for stimulant use disorders: Treatment Improvement Protocol (TIP) series 33. Rockville (MD): Department of Health and Human Services, Substance Abuse and Mental Health Services Administration (US); 1999. [PubMed] [Google Scholar]
- 31.K Ahmad. Asia grapples with spreading amphetamine abuse. Lancet. 2003;361:1878–9. doi: 10.1016/S0140-6736(03)13548-9. [DOI] [PubMed] [Google Scholar]
- 32. Bangkok KTG. Need for speed. Time 2001 Feb 26.
- 33.SG Sherman, C Sutcliffe, B Srirojn, CA Latkin, A Aramratanna, DD Celentano. Evaluation of a peer network intervention trial among young methamphetamine users in Chiang Mai, Thailand. Soc Sci Med. 2009;68:69–79. doi: 10.1016/j.socscimed.2008.09.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.RW Derlet, B Heischober. Methamphetamine. Stimulant of the 1990s? West J Med. 1990;153:625–8. [PMC free article] [PubMed] [Google Scholar]
- 35.AM Barr, WJ Panenka, GW MacEwan, AE Thornton, DJ Lang, WG Honer, et al. The need for speed: an update on methamphetamine addiction. J Psychiatry Neurosci. 2006;31:301–13. [PMC free article] [PubMed] [Google Scholar]
- 36.R Garofalo, BS Mustanski, DJ McKirnan, A Herrick, GR Donenberg. Methamphetamine and young men who have sex with men: understanding patterns and correlates of use and the association with HIV-related sexual risk. Arch Pediatr Adolesc Med. 2007;161:591–6. doi: 10.1001/archpedi.161.6.591. [DOI] [PMC free article] [PubMed] [Google Scholar]