SYNOPSIS
Objectives
In 2001, the Health Center Growth Initiative was launched to increase access to primary health-care services through the expansion of the health center program. We examined the impact this initiative had on the number and types of patients seen by health centers, as well as the health center characteristics significantly associated with service expansions.
Methods
We conducted secondary and time-trend analyses of the Uniform Data System, an annual dataset submitted to the Bureau of Primary Health Care by all federally qualified health centers. We performed trend and multivariable analyses to examine the impact of the initiative on health center performance.
Results
Health centers that received both new access points and expanded medical capacity funding saw the most rapid growth in patients. These centers experienced a 58% increase in total number of patients and a 60% increase in total number of encounters, compared with 10% and 8%, respectively, for centers receiving no funding at all. Conclusions were unchanged even after controlling for other health center characteristics.
Conclusions
Public funding is critical to sustaining and expanding health center services to the nation's vulnerable populations.
Health centers are community-based, patient-driven organizations located in medically underserved areas (MUAs), which are operated by the Bureau of Primary Health Care (BPHC), part of the Health Resources and Services Administration. They provide family-oriented primary and preventive care—occasionally including oral health, mental health, and substance abuse services—to anyone seeking care, without regard to the individual's insurance or financial status. Health centers serve an estimated 20% of the 48 million people living in MUAs, and function as the nation's primary care safety net for the poor and uninsured in rural and inner-city areas. Almost 40% of patients seen at health centers are uninsured, 35% are covered by Medicaid, and 92% are at ≤200% of the federal poverty level (FPL). In addition, about two-thirds of health center patients are members of minority groups (23% African American and 36% Hispanic/Latino).1
In 2001, former President Bush's Health Center Growth Initiative (HCGI) was launched to increase access to primary health-care services through expansion of the health center program. The primary goal of this initiative was the addition or expansion of 1,200 new health center sites in the nation's most underserved areas in the span of five years, along with the provision of health-care services to an additional six million people. The initiative nearly doubled federal health center funding to implement and sustain the expansion from about $1 billion in 2000 to more than $2 billion. Congress supported the initiative, which was launched in fiscal year 2002 and ended in fiscal year 2007.1
The HCGI focused on two types of growth: the expansion of already existing access points, referred to as expanded medical capacity (EMC), and the addition of new access points (NAPs) in areas where there were previously no health centers. Funds were split between both groups with a distinct set of rules and regulations for each.
NAP grants supported the creation of new service delivery sites for medically underserved populations, and were capped at $650,000 per year. New sites offered comprehensive primary and preventive health-care services in areas where there was limited or no access to care, and allowed for the creation of any type of health center (e.g., community, migrant farm worker, homeless, or public housing). NAP applicants were expected to demonstrate how funds would expand access to health services and increase the number of people served in the targeted community, while also aiming to achieve the primary goals of Healthy People 2010, to increase quality and years of healthy life and eliminate health disparities. In addition, NAP sites were required to be operational within 120 days of a grant award. Applicants had to demonstrate their readiness to provide services for the proposed special population or community, with providers available to serve at the new site within the given time period. These new sites were expected to be functioning at full capacity after two years.
Because the initiative's primary goal was to decrease health disparities among MUAs, new sites were expected to be aware of the specific health-care needs of the targeted community and population. NAP sites were expected to address the most significant barriers to health care in the area, including location of delivery sites and hours of operation, as well as gaps in services and major health-care problems. Oral health, mental health, and substance abuse services were also included in the new sites as part of the guarantee for comprehensive primary and preventive health care.
On the other hand, EMC grants served to expand the capacity of existing health centers to significantly increase the number of people with access to primary health care, particularly in communities where the health center's services were insufficient to cover the needs of the area. The objective of these expansions was to enhance the scope of a health center's reach, improve the health status of people in the area, and decrease health disparities.
EMC delivery sites were set within an established health center's previously approved project, and did not involve the creation of new sites. Examples of EMC development included: expansion of existing primary care medical services, addition of new medical providers where excess facility capacity existed, expansion of hours of operations, or provision of additional medical services through contractual relationships with specialized providers. Grants were capped at $600,000 per year for expansion of existing services, and $150,000 to $250,000 per year for service expansion grants for oral health, mental health, and substance abuse services.
Proposed strategies were required to demonstrate a significant increase in new usage, which was specifically defined to be: (1) a 25% increase in the total number of users or 3,000 new users, whichever was less, for expanding the capacity of an existing program; (2) a 3,000 new user minimum increase for migrant, homeless, or public housing health centers initiating a new health center program; or (3) a 10% increase in the total number of users or 1,000 new users, whichever was less, for expanding a migrant, homeless, or public housing health center program. Similar to NAP sites, EMC sites were also expected to be operational within 120 days of the award, including staff recruitment and availability of services to the community by the deadline.
In 2001, health centers served more than 10 million patients in 3,400 community-based health-care center sites. Five years after launching the HCGI, 1,236 new and expanded access points were added to the health-care system—716 NAPs and 520 EMC—surpassing the goal of 1,200 new sites. From 2001 to 2007, the total number of patients treated increased by 56%, with an additional 5.8 million patients seen at a mean cost of $559 per patient.1
The primary aim of this study was to examine the impact of the HCGI on the total number and types of patients (e.g., according to minority status, uninsurance, private insurance, and poverty status) seen by health centers. While we intuitively expected that additional funding from the initiative would lead to increased numbers of users, it is important to quantify this increase with empirical data. We were also interested in determining which type of grant—NAPs or EMC—led to the greatest increase in overall users as well as increases for specific sociodemographic groups. The second objective was to examine health center characteristics significantly associated with service expansions. In other words, were there additional predictors of health center performance besides the HCGI itself? Results of the study may help policy makers develop future strategies for targeting the health center program's growth to strengthen and expand its role as the primary care safety net for vulnerable populations.
METHODS
Data
The primary dataset for the study came from the Uniform Data System (UDS), an annual dataset submitted to the BPHC by health centers.2 Since its first reporting year in 1996, the UDS has been tracking a variety of information pertinent in reviewing the operation and performance of health centers, including patient demographics, staffing, services provided, utilization rates, clinical indicators, costs, and revenues at the grantee, state, and national levels. The UDS includes two sets of data: (1) the universal report, which is completed by all grantees and provides data on services, staffing, and financing across all programs supported by the BPHC; and (2) the grant reports, which collect data for agencies with multiple BPHC grants and provide a separate report for each migrant, homeless, or public housing program.
Data were extracted from the 2001 to 2006 UDS databases. The year 2001 was chosen as a starting point because it was the year prior to the launch of the HCGI, thus providing baseline information on health centers before the expansion. The year 2006 was the final year of the initiative. For the purpose of this study, health centers in existence since at least 2001 were included. Additionally, we excluded centers with any missing information for the measured variables in any of the six years from analyses. Less than 5% of health centers were dropped due to missing data, and there were insignificant differences in center characteristics between those included and those not included in the analyses.
Measures
Sources of funding.
Health centers were separated into five groups according to funding received from the HCGI. Group A received neither NAP nor EMC funding, and served as the control group capturing the natural growth of health centers. Group B received only NAP funds, Group C only EMC, Group D either EMC or NAP funds, and Group E both NAP and EMC grants. We extracted information on the total number and types of patients seen by the health centers for each of these five groups.
Health center users.
For the purpose of this study, a user was defined as an individual with at least one visit to any of the health center's providers during a given year, while an encounter was defined as a visit between a patient and a provider. We obtained the total number of users during the years of the initiative, in addition to the total number of encounters for each year from 2001 to 2006.
Vulnerable populations.
The UDS also captures information on vulnerable groups served by health centers. We used these data to determine the change in number of patient users for specific demographic groups. Specific vulnerable groups examined included the uninsured, the Medicaid insured, the homeless, racial/ethnic minority groups, and individuals below the FPL. In addition, we examined the privately insured to determine if the initiative also produced an effect on a patient group not considered to be a vulnerable population.
Covariates.
Data on other health center characteristics were included in the analyses to obtain the unique effects of the initiative on the total number and types of users. These covariates included the number of primary care physicians in each health center, rural-urban location, net revenue, and primary care physician productivity (defined as the total number of physician encounters divided by the number of full-time equivalent physicians in each center). Data reflecting the size and efficiency of health centers (i.e., number of physicians, net revenue, and productivity) are important because size and efficiency affect the centers' ability to expand and diversify. Larger and more efficient health centers can more easily accommodate the rapid growth resulting from increased funding. Location of the center also holds significance because rural centers often lag behind their urban counterparts due to the unique obstacles faced in rural health care, including distance to providers and poorer health status of the population.
Analyses
We performed analysis of variance to examine the relationship between the type of funding received and the change in total number of patients and encounters, as well as specific patient types. To estimate the unique impact of the initiative, we performed multiple regression analyses controlling for other health center characteristics likely to affect patient services.
RESULTS
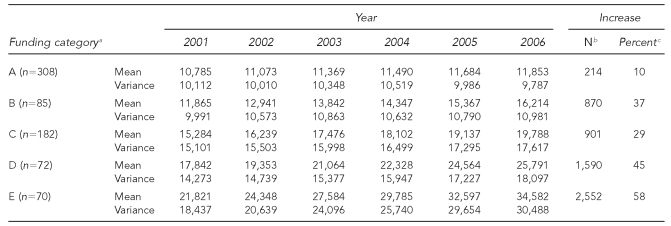
Table 1 shows the effect of the HCGI on the mean total number of patients in health centers. Group E centers (receiving both NAP and EMC awards) had the highest increase in total number of users, while Group A (receiving no awards) had the lowest increase. Group E experienced a mean annual increase of 2,552 patients per center, or about 58% growth from 2001 to 2006. In contrast, Group A centers saw a mean annual increase of 214 users per center, from 10,785 to 11,853, or about a 10% increase during the five-year period. For Groups B (NAP awards only), C (EMC awards only), and D (either NAP or EMC awards), the percentage increases in users fell somewhere in between: 29% for Group C, 37% for Group B, and 45% for Group D.
Table 1.
Mean and standard deviation for annual total health center user increase and percentage increase during the Health Center Growth Initiative, 2001–2006
aA = neither NAP nor EMC funding (i.e., control), B = NAP funding only, C = EMC funding only, D = EMC or NAP funding, and E = EMC and NAP funding.
bMean annual increase in number of health center users
cPercentage increase in users between 2001 and 2006
NAP = new access point
EMC = expanded medical capacity
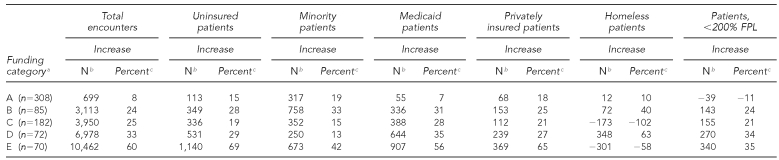
We observed similar trends with other measures of patient characteristics (Table 2). For example, centers receiving no award (i.e., Group A) showed a mean annual increase of 699 encounters per center (about 8%), whereas centers receiving both types of awards (Group E) displayed a mean annual increase of 10,462 encounters per center (about 60%). Centers receiving one type of award (Groups B, C, and D) demonstrated mean annual increases of 24% to 33%, which was in between Groups A and E. With respect to uninsured patients, centers receiving no award had a mean annual increase of 113 patients per center (about 15%), whereas centers receiving both types of awards displayed a mean annual increase of 1,140 patients per center (about 69%). Centers receiving one type of award demonstrated mean annual increases of 19% to 29%. Regarding patients whose family income was <200% FPL, centers receiving no award showed a mean annual decline of 39 patients per center (about –11%), whereas centers receiving both NAP and EMC awards displayed a mean annual increase of 340 patients per center (about 35%). Centers receiving either a NAP or EMC award demonstrated mean annual increases of low-income patients of 2% to 34%.
Table 2.
Health center patient characteristics: mean frequency and percentage increases among users during the Health Center Growth Initiative, 2001–2006
aA = neither NAP nor EMC funding (i.e., control), B = NAP funding only, C = EMC funding only, D = EMC or NAP funding, and E = EMC and NAP funding.
bMean annual increase in number of health center users
cPercentage increase in users between 2001 and 2006
FPL = federal poverty level
NAP = new access point
EMC = expanded medical capacity
We observed a similar pattern among insured patients. Centers receiving no award showed a mean annual increase of 55 Medicaid patients per center (about 7%), whereas centers receiving both awards displayed a mean annual increase of 907 Medicaid patients per center (about 56%). Centers receiving only one award demonstrated mean annual increases of Medicaid patients of 28% to 35%. Similarly, centers receiving no award showed a mean annual increase of 68 privately insured patients per center (about 18%), whereas centers receiving both awards displayed a mean annual increase of 369 patients per center (about 65%). Centers receiving only one award demonstrated mean annual increases of privately insured patients of 21% to 27%.
The patterns were somewhat different for two other patient measures: minority patients and homeless patients. For minority patients, centers receiving both types of awards (Group E) displayed the greatest gain, a mean annual increase of 673 minority patients per center (about 42%), followed by centers receiving NAP awards only (Group B) with a mean annual increase of 758 patients per center (about 33%). However, we observed no significant differences among the other three groups (A, C, and D), as their minority patients increased annually by 13% to 19%. For homeless patients, centers receiving both types of awards showed declines, whereas other groups showed both declines and gains. Detailed annual patient information for all these measures is available from the corresponding author upon request.
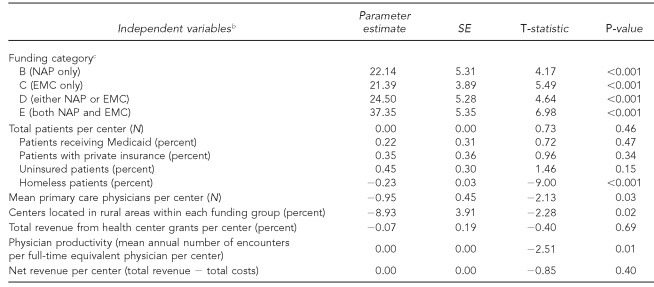
We performed multiple regression analyses to examine the impact of the initiative, as well as other health center characteristics, on health centers' performance in expanding care. Table 3 shows the impact of these factors on the percent increase in total number of patients. Compared with centers that received no award (Group A), centers that received either NAP or EMC awards (Groups B, C, D, and E) were likely to see significantly more patients (p<0.001); this was particularly evident for centers that received both types of awards (Group E). A few other health center characteristics were significantly associated with patients seen. Rural location was a barrier to seeing more patients, as was serving a greater proportion of homeless patients. Having more physician providers was also associated with serving fewer patients.
Table 3.
Multiple regression analysis: health center characteristics associated with an increase in number of health center patients during the Health Center Growth Initiative, 2001–2006a
aModel R2 = 0.53
bIndependent variables are from 2006.
cReference = group A (no award)
SE = standard error
NAP = new access point
EMC = expanded medical capacity
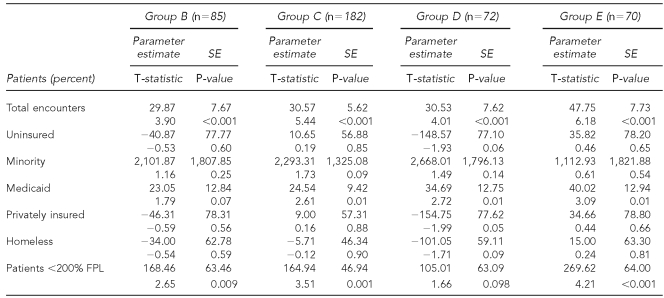
Regression results of the impact of the initiative on other patient characteristics are summarized in Table 4. Controlling for other health center characteristics, funding status had a positive and significant impact on total patient encounters (p<0.001 for all funding groups), Medicaid patients (p=0.01 for Groups C, D, and E), and patients whose family income was <200% FPL (p=0.009 for Group B, p≤0.001 for Groups C and E). However, there were no significant impacts on minority, uninsured, privately insured, and homeless patients (p>0.05). Results of other health center covariates are available upon request.
Table 4.
Multiple regression analysis: associations between funding categories and health center patient characteristics during the Health Center Growth Initiative, 2001–2006a
aCovariates included total users, total physician providers, percent rural users, percent revenue from government health center program, physician productivity, and net revenue. Group A (no award, n=308) was the reference group, Group B = NAP funding only, Group C = EMC funding only, Group D = EMC or NAP funding, and Group E = EMC and NAP funding.
SE = standard error
FPL = federal poverty level
NAP = new access point
EMC = expanded medical capacity
DISCUSSION
Health centers are the nation's primary care safety net for the poor and uninsured in rural and inner-city areas. The HCGI was launched in 2001 to strengthen and expand health centers, with the goal of creating at least 1,200 new or expanded access points in the hopes of increasing the total number of health center patients by six million people. The results of this study confirm that the HCGI has indeed produced an increase of this magnitude.
The study also sheds light on which type of funding led to the greatest increase in overall users, as well as increases for specific sociodemographic groups. In particular, centers that received both NAP and EMC funding (Group E) saw rapid growth, with a 58% increase in total number of patients and a 60% increase in total number of encounters. Conversely, centers that receiving no funding saw growth rates of only 10% for number of patients and 8% for encounters. Multiple regression analyses showed similar patterns of growth for Medicaid and low-income patients. Centers that received either NAP or EMC funding, but not both, displayed an intermediate level of growth. These findings indicate that health centers that received both NAP and EMC funding ostensibly received more money during the duration of the initiative and, thus, were given greater opportunities to expand. In addition to creating new delivery sites, these centers were also provided with additional resources to enlarge their initial projects. Compared with health centers that received only one fund or none at all, the rapid growth of these NAP- and EMC-funded centers was reasonable and expected.
Vulnerable populations most affected by the initiative included Medicaid beneficiaries and those whose family income was <200% FPL (who comprised more than 90% of patients seen in health centers in 2007).1 When health centers received both types of funding, these two groups saw a 56% and 35% increase in the number of patients, respectively. Centers receiving only one type of fund also saw rapid growth, which was significantly higher than growth among centers without funding. These results demonstrate the influence of the expansion initiative on these vulnerable patient groups.
Health centers located in rural areas had more difficulties expanding services, with rural location being associated with negative patient growth. Previous research has indicated that planned expansions in rural centers are hindered by understaffing and difficulties in recruiting health-care personnel to these areas.3 Thus, personnel shortages could have impeded the growth of rural health centers. Possible solutions for attracting more medical providers include increasing salaries, expanding loan forgiveness programs, improving the quality of rural housing and schools, and providing assistance with spousal job searches.
Health centers serving more homeless patients also experienced difficulties in expanding their services. These difficulties may be because this patient population is disproportionately burdened with multiple health and psychosocial needs; meeting these complex needs is challenging and requires the provision of comprehensive mental health, substance abuse, and ancillary services.4 It may also be difficult to recruit health-care providers with appropriate specialty training relevant to the unique needs of this population. In addition, recruiting and retaining new patients may be complicated by the transient nature of homeless individuals' lives.5
We did not conduct analyses regarding the impact of neighborhood demographic characteristics on health centers' growth. However, it is certainly plausible that centers in persistent poverty places are at a disadvantage in increasing the number of patients. While we have no direct evidence of this possibility from our data, results of our multiple regression analyses indicate that centers serving higher proportions of homeless patients and those located in rural areas had negative patient growth. To the extent that homelessness and rural location indicate lack of community resources and serve as proxy measures of community poverty, these findings suggest, but do not confirm, that low-income communities are at a disadvantage when attempting to increase the number of health center users. Additional research is needed to explicitly examine characteristics of the communities in which health centers are located, and to identify specific sociodemographic factors that enable or hinder health center growth.
In the last decade, a growing body of literature has documented a positive association linking primary care—which health centers are noted for providing—to better health status and lower morbidity.6–15 Previous studies have also shown that health centers provide access to primary care, ensure continuity of care, and deliver comprehensive services as well as, if not better than, other health-care settings.16–19 Our study indicates that increasing health center funding can play a considerable role in reducing disparities and improving access to care for vulnerable populations, such as low-income and Medicaid-insured individuals. These groups tend to suffer from the poorest health outcomes and have the greatest health needs; thus, increasing their utilization of health centers has the potential to improve their health status.
Admittedly, improving access to care through expansions to the health center program has its limitations. Despite the creation of new centers and the expansion of existing centers, there have been no significant increases in on-site specialty services and diagnostic testing.20 Though primary care certainly contributes to improved health outcomes, the availability of secondary and tertiary care is also essential. Unfortunately, many off-site providers do not accept uninsured or Medicaid patients as readily as health centers, thus restricting these populations' access to specialty care. Furthermore, research has shown that increasing insurance coverage is a more efficient tool in improving access to care than expanding health-care services.21
Limitations
This study was subject to several limitations. First, due to the secondary nature of the data, we did not have information to account for the influence of external or additional internal factors that may have affected health center patient increases. These factors include health center management characteristics, practice characteristics, community characteristics, the culture of the center, and the influence of the board. Attention to these factors would provide better insight into the effects of the initiative on the total number of patients and encounters.
Second, the study design implies that increased numbers of health center users indicate increased access to care. Because we used UDS data, we did not have information on non-center users; therefore, it was not possible to confirm whether the health center expansions actually increased access for people who previously had no access to care or whether they simply provided alternative sources of care for people who already had access to care in other settings (e.g., physicians' offices and hospital outpatient departments). Results from this study show that there was growth in both uninsured and insured patients in health centers between 2001 and 2006. This growth could be interpreted to imply that both situations occurred, with uninsured individuals gaining new access to previously unavailable care and insured individuals experiencing more barriers to care in other health-care settings, thus increasingly turning to safety-net health centers. Future studies should employ population-based data to investigate time trends in health center access and usage, and to determine whether or not increased numbers of health center patients were offset by decreased numbers of patients in other health-care settings.
Third, the HCGI concluded just two years ago; therefore, it is difficult to assess its ultimate impact on the health center program. It is as yet unknown whether health centers will be able to maintain the rate of patient increase seen during the initiative without support from EMC or NAP grants. Further monitoring is necessary to examine the sustainability of the unprecedented growth seen in this recent time period. The ability to maintain the number of patients and encounters would be an important indicator of the success or failure of the HCGI.
Finally, this study did not address the quality of the care received in health centers. The rapid expansion experienced by these sites could have led to lower quality of care as they adjusted to an increased patient load. While providing greater access to health care for vulnerable populations is an important factor in improving the health of the nation, the quality of care provided is just as significant. Lower quality of care would do little to bridge disparities and improve the health status of the medically indigent.
CONCLUSIONS
The positive association found between health center funding and total number of patients confirms that the HCGI was successful in strengthening the nation's primary care safety net. Future funding to support the improvement and expansion of this program will continue to play a significant role in reducing health-care disparities and improving the health of vulnerable populations that utilize health centers.
Acknowledgments
The authors thank Angeli Bueno, who contributed to the writing of this article, and Yunji Huang, who conducted the data analysis.
The authors acknowledge the financial support for this study by the Bureau of Primary Health Care, Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS). The views expressed in this article are those of the authors and do not necessarily reflect the official policies of HHS or HRSA, nor does mention of the department or agency imply endorsement by the U.S. government.
REFERENCES
- 1.Department of Health and Human Services, Health Resources and Services Administration, Bureau of Primary Health Care (US) Health centers: America's primary care safety net, reflections on success, 2002–2007. Rockville (MD): HHS; 2008. Jun, [Google Scholar]
- 2.Department of Health and Human Services, Health Resources and Services Administration, Bureau of Primary Health Care (US) 2008 uniform data system reporting manual. Rockville (MD): HHS; 2008. [Google Scholar]
- 3.Rosenblatt RA, Andrilla CH, Curtin T, Hart LG. Shortages of medical personnel at community health centers—implications for planned expansion. JAMA. 2006;295:1042–9. doi: 10.1001/jama.295.9.1042. [DOI] [PubMed] [Google Scholar]
- 4.Zlotnick C, Zerger S. Survey findings on characteristics and health status of clients treated by the federally funded (US) Health Care for the Homeless programs. Health Soc Care Community. 2009;17:18–26. doi: 10.1111/j.1365-2524.2008.00793.x. [DOI] [PubMed] [Google Scholar]
- 5.Luck J, Andersen R, Wenzel S, Arangua L, Wood D, Gelberg L. Providers of primary care to homeless women in Los Angeles County. J Ambul Care Manage. 2002;25:53–67. doi: 10.1097/00004479-200204000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Shi L. Primary care, specialty care, and life chances. Int J Health Serv. 1994;24:431–58. doi: 10.2190/BDUU-J0JD-BVEX-N90B. [DOI] [PubMed] [Google Scholar]
- 7.Shi L, Starfield B, Kennedy B, Kawachi I. Income inequality, primary care, and health indicators. J Fam Pract. 1999;48:275–84. [PubMed] [Google Scholar]
- 8.Shi L, Starfield B. The effect of primary care physician supply and income inequality on mortality among blacks and whites in US metropolitan areas. Am J Public Health. 2001;91:1246–50. doi: 10.2105/ajph.91.8.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970–1998. Health Serv Res. 2003;38:831–65. doi: 10.1111/1475-6773.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi L, Macinko J, Starfield B, Wulu J, Regan R, Politzer R. The relationship between primary care, income inequality, and mortality in US states, 1980–1995. J Am Board Fam Pract. 2003;16:412–22. doi: 10.3122/jabfm.16.5.412. [DOI] [PubMed] [Google Scholar]
- 11.Shi L, Macinko J, Starfield B, Xu J, Politzer R. Primary care, income inequality, and stroke mortality in the United States: a longitudinal analysis, 1985–1995. Stroke. 2003;34:1958–64. doi: 10.1161/01.STR.0000082380.80444.A9. [DOI] [PubMed] [Google Scholar]
- 12.Shi L, Macinko J, Starfield B, Politzer R, Xu J. Primary care, race, and mortality in US states. Soc Sci Med. 2005;61:65–75. doi: 10.1016/j.socscimed.2004.11.056. [DOI] [PubMed] [Google Scholar]
- 13.Shi L, Macinko J, Starfield B, Politzer R, Xu J. Primary care, social inequalities, and all-cause, heart disease, and cancer mortality in US counties: a comparison between urban and non-urban areas. Public Health. 2005;119:699–710. doi: 10.1016/j.puhe.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Starfield B, Shi L, Grover A, Macinko J. The effects of specialist supply on populations' health: assessing the evidence. Health Aff (Millwood) 2005 doi: 10.1377/hlthaff.w5.97. Suppl Web exclusives:W5-97-107. [DOI] [PubMed] [Google Scholar]
- 15.Starfield B, Shi L, Macinko J. Contributions of primary care to health systems and health. Milbank Q. 2005;83:457–502. doi: 10.1111/j.1468-0009.2005.00409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Politzer RM, Yoon J, Shi L, Hughes RG, Regan J, Gaston MH. Inequality in America: the contribution of health centers in reducing and eliminating disparities in access to care. Med Care Res Rev. 2001;58:234–48. doi: 10.1177/107755870105800205. [DOI] [PubMed] [Google Scholar]
- 17.Shi L, Regan J, Politzer RM, Luo J. Community health centers and racial/ethnic disparities in healthy life. Int J Health Serv. 2001;31: 567–82. doi: 10.2190/QHGC-YVML-7GMK-77C1. [DOI] [PubMed] [Google Scholar]
- 18.Shi L, Starfield B, Xu J, Politzer R, Regan J. Primary care quality: community health center and health maintenance organization. South Med J. 2003;96:787–95. doi: 10.1097/01.SMJ.0000066811.53167.2E. [DOI] [PubMed] [Google Scholar]
- 19.Shi L, Stevens GD. The role of community health centers in delivering primary care to the underserved: experiences of the uninsured and Medicaid insured. J Ambul Care Manage. 2007;30:159–70. doi: 10.1097/01.JAC.0000264606.50123.6d. [DOI] [PubMed] [Google Scholar]
- 20.Cook NL, Hicks LS, O'Malley J, Keegan T, Guadagnoli E, Landon BE. Access to specialty care and medical services in community health centers. Health Aff (Millwood) 2007;26:1459–68. doi: 10.1377/hlthaff.26.5.1459. [DOI] [PubMed] [Google Scholar]
- 21.Cunningham P, Hadley J. Expanding care versus expanding coverage: how to improve access to care. Health Aff (Millwood) 2004;23:234–44. doi: 10.1377/hlthaff.23.4.234. [DOI] [PubMed] [Google Scholar]