Abstract
Conjugated linoleic acid (CLA) exerts a protective effect on experimental inflammatory bowel disease and shows promise as a chemopreventive agent against colorectal cancer (CRC) in mice, although the mechanisms by which it exerts its beneficial effects against malignancies in the gut are not completely understood. Mice lacking PPARγ in immune and epithelial cells and PPARγ-expressing littermates were fed either control or CLA-supplemented (1 g CLA/100 g) diets to determine the role of PPARγ in inflammation-induced CRC. To induce tumor formation and colitis, mice were treated with azoxymethane and then challenged with 2% dextran sodium sulfate, respectively. Dietary CLA ameliorated disease activity, decreased colitis, and prevented adenocarcinoma formation in the PPARγ-expressing floxed mice but not in the tissue-specific PPARγ-null mice. Dietary CLA supplementation significantly decreased the percentages of macrophages in the mesenteric lymph nodes (MLN) regardless of the genotype and increased regulatory T cell numbers in MLN of PPARγ-expressing, but not in the tissue-specific, PPARγ-null mice. Colonic tumor necrosis factor-α mRNA expression was significantly suppressed in CLA-fed, PPARγ-expressing mice. This study suggests CLA ameliorates colitis and prevents tumor formation in part through a PPARγ-dependent mechanism.
Introduction
In the United States, cancers of the colon and rectum were the third most commonly diagnosed cancers among men and women in 2008 (1). An estimated 149,000 people are diagnosed with colorectal cancer (CRC)4 with 50,000 deaths attributable to CRC each year (2,3). The 2 clinical manifestations of inflammatory bowel disease (IBD), ulcerative colitis (UC) and Crohn's disease (CD), drastically increase the risk for developing colon cancer, especially when patients are diagnosed prior to 30 y of age (4). In patients with IBD, after 8–10 y, the risk of developing CRC increases by 0.5–1.0% yearly (5).
Dietary PUFA downmodulate immune and inflammatory responses by controlling eicosanoid synthesis (6) and by activating PPARγ (7), a nuclear hormone receptor expressed by monocytes, macrophages, T cells, dendritic cells, and gastrointestinal epithelial cells in the gut mucosa (8–10). A number of studies have demonstrated upregulation of PPARγ in adipocytes, skeletal muscle, colonic mucosa, and macrophages in response to dietary conjugated linoleic acid (CLA) (11–16), which is a mixture of positional and geometric isomers of octadecadienoic acid with conjugated double bonds. The predominant naturally occurring isomer is cis-9, trans-11 CLA in milk and beef products, whereas commercial CLA preparations contain a racemic mixture of cis-9, trans-11 and trans-10, cis-12 CLA isomers (17). CLA has been investigated as a potential prophylactic intervention for multiple inflammatory diseases, including obesity, hyperinsulinemia, and hypertension (18,19). CLA also modulates pathways involved in apoptosis and the immune response and decreases the risk of developing CRC (15,17,20–22).
Results of a recent clinical study in UC patients demonstrate that rosiglitazone (Avandia), a synthetic agonist of PPARγ and a U.S. FDA-approved drug for treating type II diabetes, is also efficacious in the treatment of mild to moderately active UC (23). However, off target and cardiovascular adverse side effects of Avandia (24,25), including a FDA-issued black box warning, are of concern and will likely limit its adoption by the gastroenterologist community. Nonetheless, CLA remains a promising compound for the dietary chemoprevention of inflammation-induced CRC (26). Dietary supplementation with CLA is thought to suppress chronic inflammation of the gut mucosa and, therefore, could decrease the risk of inflammation-induced CRC. This study was designed to investigate whether dietary CLA supplementation prevents or ameliorates inflammation-induced intestinal tumorigenesis and the role of PPARγ as a molecular target for CLA in CRC chemoprevention.
Materials and Methods
Transfection of SW480 intestinal epithelial cells and RAW 264.7 macrophages.
SW480 intestinal epithelial cells (IEC) were grown in 25-mm2 flasks in Leibovitz L-15 media (Invitrogen) containing 10% fetal bovine serum (FBS) until 60–70% confluence. RAW 264.7 macrophages were grown in 25-mm2 flasks in DMEM (Mediatech) containing 10% FBS. Cells were then treated in replicates of 8 with CLA (1.25, 2.5, and 5 μmol/L; Cayman Chemicals), rosiglitazone (1 μmol/L; Cayman Chemicals) as a positive control, or vehicle (DMSO) and placed in a 37°C incubator with 5% CO2 for 4 and 24 h. Reporter activity assays for PPARγ activity were performed as previously described (27).
Animal procedures.
PPARγ fl/fl; MMTV-Cre+ (tissue-specific PPARγ null) in a C57BL/6 background, which undergo premature termination of translation due to enzymatic activity of the recombinase in epithelial and hematopoietic cells, and PPARγ-expressing floxed littermates (PPARγ floxed), corresponding to a wild-type phenotype, were generated as previously described (15). All mice were housed in animal facilities at the Virginia Polytechnic Institute and State University in a room maintained at 22°C, with a 12-h-light/-dark cycle starting from 0600 h. Mice were genotyped for the PPARγ gene using previously published genotyping protocols (15). Mice were fed purified AIN-93G rodent diets with and without CLA in which all nutritional requirements were met or exceeded. Based on previous findings (15), a 50:50 mixture of the cis-9, trans-11 and trans-10, cis-12 CLA isomers (Loders Croklaan BV) was determined to be ideal for preventing experimental IBD. All the experimental diets contained the same amount of energy (isocaloric) and protein (isonitrogenous) (Table 1). One-month-old mice (n = 10 for each treatment and genotype) were administered the experimental diets supplemented with 10 g/kg of the treatment oil for 42 d prior to the induction of colitis and cancer and throughout the challenge period equivalent to an optimal prophylactic dosage of 45–80 mg/d for each mouse. All experimental procedures were approved by the Institutional Animal Care and Use Committee of the Virginia Polytechnic Institute and State University.
TABLE 1.
Composition of experimental diets
| Ingredient | Control diet | CLA diet |
|---|---|---|
| g/kg | ||
| Casein | 200 | 200 |
| l-Cystine | 3 | 3 |
| Corn starch | 397.5 | 397.5 |
| Maltodextrin | 132 | 132 |
| Sucrose | 100 | 100 |
| Cellulose | 50 | 50 |
| Mineral mix (AIN-93)1 | 35 | 35 |
| Vitamin mix (AIN-93)2 | 10 | 10 |
| Choline bitartrate | 2.5 | 2.5 |
| Tert-butylhydroquinone3 | 0.014 | 0.014 |
| Soybean oil | 70 | 60 |
| cis9, trans11/trans10, cis12 CLA | 0 | 10 |
Per kg diet: 3 g nicotinic acid, 1.6 g calcium pantotenate, 0.7 g pyridoxine HCl, 0.6 g thiamin HCl, 0.6 g riboflavin, 0.2 g folic acid, 0.02 g D-biotin, 2.5 g vitamin B-12 (0.1% in mannitol), 15 g d,l-α tocopheryl acetate (500 iu/g), 0.8 g vitamin A palmitate (500,000 iu/g), 0.2 g cholecalciferol (500,000 iu/g), 0.075 g vitamin K (phylloquinone), and 974.705 g sucrose.
Per kg diet: 357 g calcium carbonate, 196 g potassium phosphate monobasic, 70.78 g potassium citrate, 74 g sodium chloride, 46.6 g potassium sulfate, 24.3 g magnesium oxide, 6.06 g ferric citrate, 1.65 g zinc carbonate, 0.63 g manganous carbonate, 0.31 g cupric carbonate, 0.01 g potassium iodate, 0.01025 g sodium selenate, 0.00795 g ammonium paramolybdate, 1.45 g sodium meta-silicate, 0.275 g chromium potassium sulfate, 0.0174 g lithium chloride, 0.0815 g boric acid, 0.0635 g sodium fluoride, 0.0318 g nickel carbonate, hydroxide, tetrahydrate, 0.0066 g ammonium vanadate, and 220.716 g sucrose.
Antioxidant.
Induction and evaluation of CRC.
Inflammation-induced CRC was initiated by using an established protocol (28). Specifically, we challenged mice with azoxymethane (10 mg/kg) on wk 6 of the study, followed by a challenge with 2% dextran sodium sulfate (DSS), 36,000–44,000 molecular weight (ICN Biomedicals) in the drinking water for 7 d beginning on wk 7. The 2% DSS dose was lower than the dose we generally use for acute DSS colitis studies (2.5% DSS) but is optimal for more chronic, long-term inflammation and cancer studies. Following the DSS challenge, mice were examined for clinical signs of disease associated with colitis (i.e. perianal soiling, rectal bleeding, diarrhea, and piloerection) by an experienced veterinarian. For the DSS challenge, the disease activity index was calculated using a modification of a previously published compounded clinical score (29). Colonic sections were fixed in 10% buffered neutral formalin, later embedded in paraffin, and then sectioned (6 μm) and stained with hematoxylin and eosin stain for histological examination. Scoring for adenoma and adenocarcinoma formation was conducted as previously described (30,31).
Immune cell isolation from mesenteric lymph nodes.
Mesenteric lymph nodes (MLN) were excised, crushed, and then placed into 3 mL of fluorescence activated cell sorting (FACS) buffer (1× PBS, 5% FBS, and 0.1% sodium azide). Debris was removed from the sample and cells were centrifuged at 290 × g for 5 min. The supernatant was eliminated and the cells were washed with 10 mL of FACS buffer and centrifuged at 290 × g for 10 min. The supernatant was discarded and the cells resuspended at 2 × 103 cells/L.
Immunophenotyping of cells isolated from MLN.
MLN cells were seeded into 96-well plates (Costar) at 2 × 105 cells/well. Nonspecific binding of antibodies was prevented by incubating cells with 20 mg/L FcBlock (BD-Pharmingen) for 20 min. To assess macrophage infiltration, cells were then incubated with anti-mouse anti-F4/80-PE-Cy5 (5 mg/L), anti-CD11b-fluorescein isothiocyanate (FITC) (2 mg/L) (eBioscience), and anti-CCR2-PE (1 mg/L) (R&D Systems) for 20 min in the dark. To determine the regulatory T cells (Treg) infiltration cells were incubated with anti-CD4-FITC and anti-CD25-Pe-Cy5 (BD Pharmingen) for 20 min in the dark. For detection of intracellular Treg marker FoxP3 cells were fixed and permeabilized with Cytofix-Cytoperm solution (BD Pharmingen) after staining for extracellular markers. Cells were then incubated with anti-mouse antibodies to FoxP3 PE (1 mg/L) (eBioscience) diluted in Perm-Wash buffer (BD Pharmingen). Cells were resuspended in 0.2 mL PBS. Data acquisition was computed with a BD LSR II flow cytometer and analysis performed with FACS Diva software (BD Pharmingen).
Colonic and MLN immunohistochemistry.
Frozen serial sections of 10 μm were transferred to poly-l-lysine slides for immunohistochemical staining. Sections were fixed in ice-cold acetone for 5 min and rinsed in 1× PBS. The presence of macrophages was detected with anti-F4/80 conjugated with Alexa Fluor 488 (1:100; eBioscience) and colocalized with anti-Ly6c conjugated with biotin (1:400; Abcam). The presence of CD4 T-cells and Treg was detected with anti-CD4 conjugated with FITC (1:100; eBioscience) and colocalized with anti-FoxP3 conjugated with biotin (1:100; eBioscience). Sections were incubated with primary antibody for 1 h at room temperature, rinsed in 1× PBS, and immunodetection of Ly6c or FoxP3 was performed using streptavidin conjugated with Alexa Fluor 546 (1 mg/L; Invitrogen) incubated for 1 h at room temperature. Following incubation, slides were rinsed in 1× PBS and then ddH20 for 5 min. Fluorescence images were captured with an inverted fluorescent microscope (Nikon Eclipse TE2000-U) and accompanying software (NIS-Elements, Nikon Instruments). Two-color staining was quantified by color segmentation with image analysis software (Image-Pro Plus, Media Cibernetics).
Real-time quantitative RT-PCR.
Total RNA was isolated from colonic specimens using the RNA isolation Minikit (Qiagen) according to the manufacturer's instructions. Real-time RT-PCR was performed as previously described (15). Primer concentrations and annealing temperatures were optimized for the iCycler iQ System (Bio-Rad) for each set of primers using the system's gradient protocol. PCR efficiencies were maintained above 90% and correlation coefficients were maintained above 0.98 for each primer set (Supplemental Table 1) during optimization and also during the real-time PCR of sample DNA. Results are presented as the starting quantity of target cDNA pg/μg of total RNA.
Statistical analysis.
ANOVA was used to determine the significance of the model: main effects of diet, genotype, time, and 2-way and 3-way interactions when time was a factor. ANOVA was performed by using the general linear model procedure of SAS (SAS Institute) as previously described (32). Data were analyzed as 2 × 2 factorial arrangements of treatments. The statistical model was: Yijk = μ + genotypei + dietj + (genotype × diet)ij + error Aijk, in which μ was the general mean, genotypei was the main effect of the ith level of the genotypic effect (expression of PPARγ by immune and epithelial cells), dietj was the main effect of the jth level of the dietary effect (CLA vs. control), (genotype × diet)ij was the interaction effect between genotype and diet, and error A represented the random error. When the model was significant, the analysis was followed by Fisher's least significant difference multiple comparisons method. Data were expressed as the means ± SEM. For analyzing the disease activity index results over time, we used a 3-factor, repeated-measures ANOVA. For this analysis, in addition to the main effects of diet and genotype and the 2-way interaction between diet and genotype (as shown above), the model included the main effect of time, the diet × time, genotype × time interactions, and the 3-factor interaction (diet × genotype × time). Differences were considered significant at P < 0.05.
Results
Modulation of PPARγ activity in RAW macrophages and IEC by CLA stimulation.
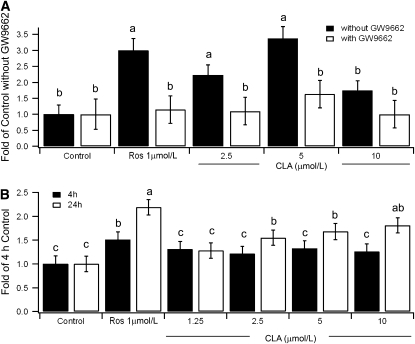
Macrophages were transfected with PPARγ and then stimulated with CLA, with and without the PPARγ inhibitor GW9662. PPARγ reporter activity was significantly greater at 2.5 and 5 μmol/L CLA concentrations compared with control (Fig. 1A). PPARγ activity did not significantly differ from those of a nonstimulated control when in the presence of GW9662. IEC transfected with PPARγ were also stimulated with CLA for both 4 and 24 h, after which PPARγ reporter activity was determined. Though PPARγ activity was not elevated after 4 h, it significantly increased after 24 h at concentrations of 2.5, 5, and 10 μmol/L of CLA (Fig. 1B).
FIGURE 1 .
Effect of CLA on PPARγ reporter activity in Raw 264.7 macrophages (A) and SW480 IEC (B). In A, macrophages were stimulated with 2.5, 5, or 10 μmol/L CLA for 24 h. In B, IEC were stimulated with CLA for 4 or 24 h. Rosiglitazone (Ros) was used in both experiments as a positive control to stimulate PPARγ activity. Values are means + SEM, n = 6. Means without a common letter differ, P < 0.05.
Dietary CLA decreases gross features of IBD and CRC in PPARγ-expressing mice.
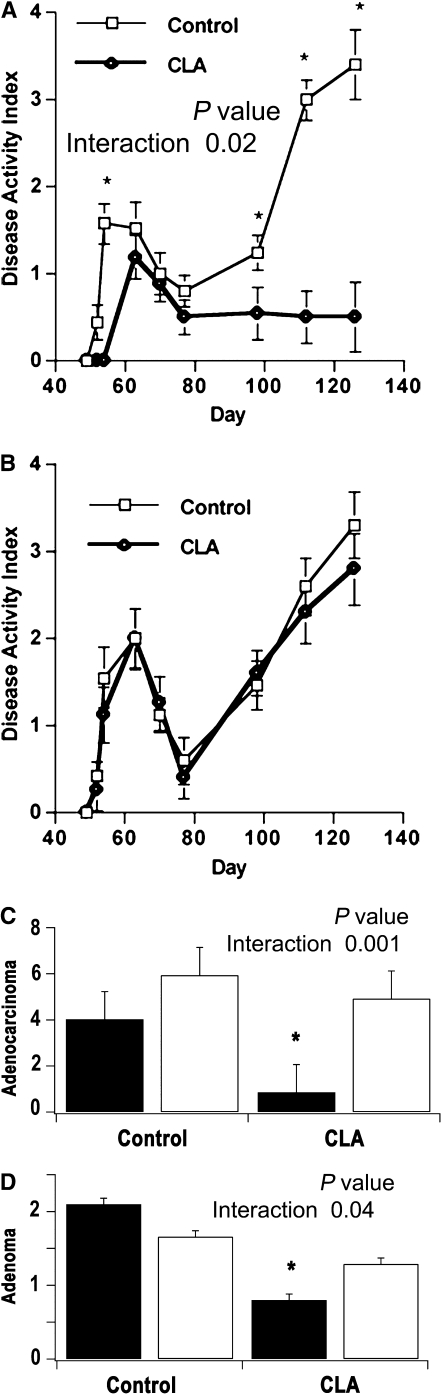
In PPARγ floxed mice, supplementation with CLA prior to the induction of inflammation-induced CRC reduced the severity of colitis compared with the control diet as observed through the disease activity index (Fig. 2A,B). Additionally, PPARγ floxed mice fed CLA had significantly decreased adenoma and adenocarcinoma scores (Fig. 2C,D). Long-term changes in colonic dysplasia and architecture were also prevented by CLA treatment in these mice (Supplemental Fig. 1). The chemopreventive effect of CLA against inflammation-induced CRC was observed only in PPARγ-expressing but not in tissue-specific PPARγ null mice.
FIGURE 2 .
Effect of dietary CLA on disease activity index (DAI) in PPARγ floxed (A) and tissue-specific PPARγ null mice (B) at 56, 98, 112, and 126 d, and on the multiplicity of adenocarcinomas (C) and adenomas (D) in PPARγ floxed (black bars) and tissue-specific PPARγ null mice (white bars) on d 126. Values are means + SEM, n = 10. Means at a time with an asterisk differ, P < 0.05.
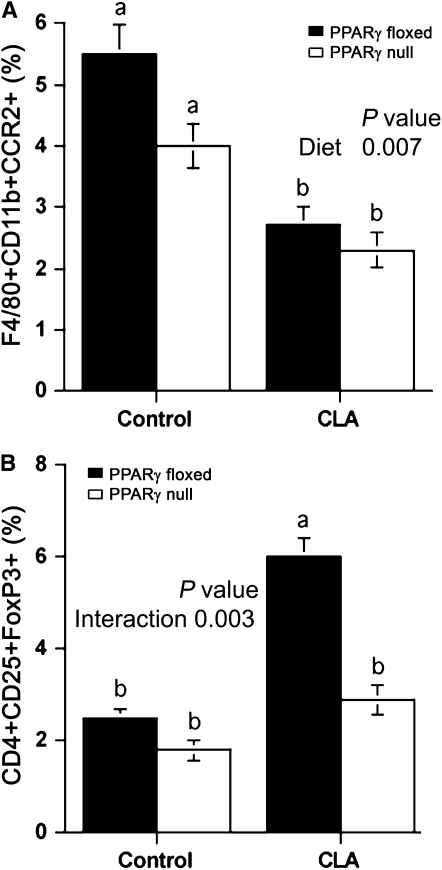
Modulation of the immune cell composition of MLN by CLA.
Dietary CLA supplementation resulted in significantly lower macrophage percentages in MLN regardless of the level of expression of PPARγ (Fig. 3A). The percentage of Treg was greater in PPARγ floxed mice compared with PPARγ null mice fed CLA, indicating the loss of the PPARγ gene abrogated the effect of CLA on Treg levels (Fig. 3B).
FIGURE 3 .
Effect of dietary CLA on the percentages of macrophages (A) and Treg (B) in MLN from PPARγ floxed (black bars) and PPARγ null (white bars) mice. Values are means + SEM, n = 10. Means without a common letter differ, P < 0.05.
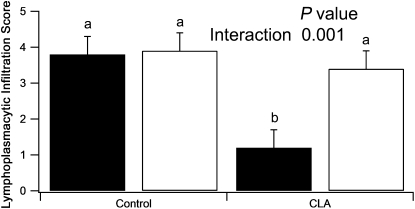
Dietary CLA modulates the immune cell infiltration of the colon.
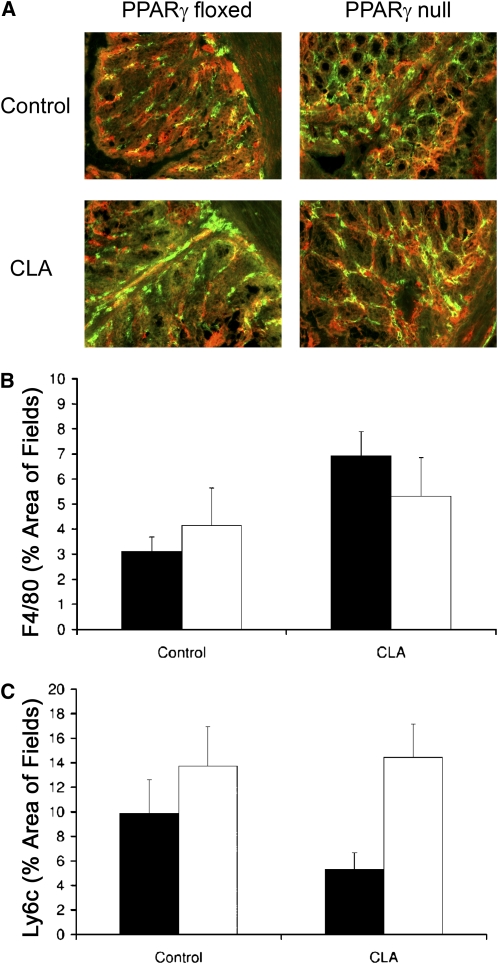
Based on histological examination of cross sections of colonic specimens, CLA lowered the overall immune cell infiltration in a PPARγ-specific manner (Fig. 4). In colons from tissue-specific PPARγ null mice, immune cell infiltration was not suppressed by diet and remained at the same levels as those in colons of PPARγ floxed mice given a control diet (Fig. 4). Macrophage (F4/80) infiltration was localized to the lamina propria and occupied ∼3–7% of tissue area in all colon samples regardless of treatment or genotype. Ly6C, which is a macrophage differentiation marker, was evident throughout the tissues and was localized to areas of macrophage infiltration (Fig. 5A). The total area of Ly6C staining tended to be lower (P = 0.10) in PPARγ floxed mice treated with CLA (Fig. 5B,C). CD4+ T cells were found in the lamina propria usually in small aggregates covering ∼35% of the tissue area. Occasional Treg (FoxP3) were scattered throughout colonic sections but were <1% of the tissue area. Lymphoid follicles contained primarily CD4+ T cells, some of which coexpressed FoxP3 (data not shown). However, at the colonic level, the amount of CD4 and FoxP3-positive cells was not significantly affected by diet or genotype (data not shown).
FIGURE 4 .
Effect of dietary CLA on lymphocytic/macrophage infiltration into colonic lamina propria of PPARγ floxed (black bars) and PPARγ null (white bars) mice. Values are means + SEM, n = 10. Means without a common letter differ, P < 0.05.
FIGURE 5 .
Effect of dietary CLA on Ly6c (red) and F4/80 (green) staining in the colonic lamina propria from PPARγ floxed (black bars) and PPARγ null mice (white bars). (A) Representative photomicrographs illustrating colocalization of F4/80 and Ly6c at an original magnification of 200×. (B,C) The numbers of F4/80- and Ly6c-positive cells, respectively. Values are means + SEM, n = 4.
Modulation of colonic gene expression by CLA and PPARγ deficiency.
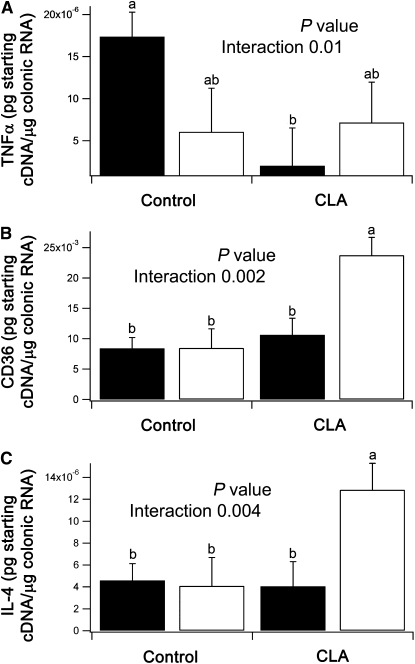
In colons from PPARγ floxed mice, mRNA levels of tumor necrosis factor-α (TNFα) in CLA-treated mice were significantly lower than in control mice (Fig. 6A). However, CLA did not downmodulate TNFα mRNA levels in colons from tissue-specific PPARγ null mice. In addition, CD36 and interleukin (IL)-4 mRNA levels were significantly greater in tissue-specific PPARγ null mice fed the CLA-supplemented diet compared with all other genotypes and treatments (Fig. 6B,C).
FIGURE 6 .
Effect of dietary CLA on colonic expression of TNFα, CD36, and IL-4 in PPARγ floxed (black bars) and PPARγ null (white bars) mice. Values are means + SEM, n = 10. Means without a common letter differ, P < 0.05.
Discussion
CLA has shown promise as a preventative intervention for IBD in pig and mouse models of colitis (11,15,33). Mechanistically, we have shown that CLA ameliorates both DSS and CD4+ T cell-induced colitis by enhancing PPARγ activity and thereby suppressing immune cell infiltration, inflammation, and epithelial erosion in the gut mucosa (15). Because inflammation increases the risk of tumor formation (26) and given that PPARγ is a molecular target for preventing intestinal tumorigenesis and inflammation (34–38), we hypothesized that dietary CLA suppresses intestinal inflammation by activating PPARγ and thereby prevents colonic carcinogenesis. In support of this hypothesis, we found that mice fed CLA-supplemented diets had lower disease activity and suppressed colitis-related adenoma and adenocarcinoma formation, indicating a prevention of colorectal tumor formation by CLA. As in IBD models, the beneficial effect of CLA in disease activity followed a PPARγ-dependent pattern. Interestingly, this model of colitis-related colonic carcinogenesis followed a reproducible biphasic response pattern in which the first peak corresponded to acute inflammation, followed by a period of remission corresponding with a stage of low-grade chronic inflammation. The second peak of disease activity that appeared after 80 d (tissue-specific PPARγ null) or 100 d (PPARγ floxed) coincided with tumor formation.
Macrophages, T cells, and IEC are the major contributors to mucosal inflammation during active IBD, all of which express PPARγ. In colonic epithelial cells, PPARγ is involved in regulating differentiation, inflammation, lipid metabolism, and cellular motility (9,39–41). In macrophages and T cells, PPARγ can antagonize the action of proinflammatory pathways such as nuclear factor-κB signaling and the expression of interferon-γ (42–44). We further hypothesized that dietary CLA modulates immune cell distribution in the mucosal immune system primarily through a PPARγ-dependent manner to reduce colitis, thereby preventing colonic tumorigenesis.
The mucosal immune system is comprised of effector sites, where immune responses take place (colonic mucosa), and inductive sites, where immune responses are initiated (MLN and Peyer's patches). To better understand the suppression of chronic inflammation by dietary CLA, we examined the distribution of immune cell subsets in MLN and colon. CLA suppressed colonic inflammation as was evident by a lower proportion of macrophages and a greater proportion of Treg in MLN compared with control and less lymphoplasmacytic infiltrates in the colonic mucosa. These findings are consistent with our previous results showing that PPARγ-expressing, but not PPARγ null, Treg protect against CD4+ T cell-induced colitis and may, therefore, be involved in an intrinsic mechanism for the prevention of IBD and inflammation-induced CRC (42). In the colonic mucosa, there were fewer (P = 0.10) colonic Ly6C+ macrophages in mice treated with CLA. Interestingly, Ly6C expression decreases as monocytes mature into macrophages and is present at high levels in a subclass of monocytes that have been implicated in the pathogenesis of atherosclerosis (45). Ly6Clow monocyte/macrophages express greater amounts of CX3CR1 compared with their Ly6Chigh counterparts, a chemokine receptor for fratalkine/CX3CL1 (46,47), which drastically reduces the metastatic potential in 2 mouse models of metastatic cancer (48). In contrast, Ly6Chigh monocytes can differentiate into TNFα-producing cells (49). Therefore, a decrease in colonic Ly6C staining and suppression in TNFα mRNA expression indicates a decrease in inflammatory macrophages in the colon.
Because PPARγ is present in both macrophages and epithelial cells, 2 abundant cell types in the gut mucosa (50), we sought to determine whether CLA could also modulate PPARγ activity in these cell types. We provide in vitro evidence demonstrating that CLA increased PPARγ activity in RAW macrophages and IEC. These findings correspond with previously published data showing elevated mRNA levels of PPARγ, CD36, Keratin 20, and PPARγ coactivator-1α and lower TNFα levels in CLA-fed mice with DSS colitis (15). Therefore, the results of this study are consistent with previous IBD studies in that CLA lowers colonic TNFα mRNA expression through a PPARγ-dependent mechanism. However, this study investigates the modulation of colitis-related carcinogenesis by CLA and PPARγ. Surprisingly, in contrast to the previously published results of the IBD model showing upregulation of CD36 in PPARγ floxed mice (15), the results of the azoxymethane/DSS colonic carcinogenesis model demonstrated that PPARγ null mice fed the CLA had significantly greater levels of IL-4 and CD36 mRNA, which may be explained through compensatory activation PPARα in the colonic mucosa. In this regard, Gocke et al. (51) demonstrated that PPARα directly binds to the IL-4 promoter and the PPARα agonist gemfibrozil ameliorated autoimmune encephalomyelitis in mice in an IL-4–dependent manner. In RAW 264.7 macrophage-derived foam cells, CLA stimulated CD36 expression in part by activating PPARα (52).
In conclusion, these data demonstrate the ability of dietary CLA to suppress colonic tumorigenesis in part through a PPARγ-dependent mechanism. Further time-course studies addressing the ability of CLA to downmodulate the inflammatory process, prevent tumor formation, and suppress progression of colonic carcinogenesis are necessary to more fully characterize the mechanisms and potential application of this supplement in the prevention of human CRC.
Supplementary Material
Acknowledgments
J.B.R. and R.H. designed the study, developed the overall research plan, and maintained study oversight; J.B.R., R.H., S.A.M., N.P.E., and A.J.G. conducted the research; J.B.R., S.A.M., and N.P.E. analyzed the data and performed the statistical analyses; and N.P.E., S.A.M., J.B.R., and E.M.S. wrote the manuscript. All authors read and approved the final manuscript.
Supported in part by award number 5R01AT4308 of the National Center for Complementary and Alternative Medicine at the NIH awarded to J.B.-R., by European Commission grant number 224836, and by funds from the Ramon y Cajal Program and the Nutritional Immunology and Molecular Nutrition Laboratory.
Author disclosures: N. P. Evans, S. A. Misyak, E. M. Schmelz, A. J. Guri, R. Hontecillas, and J. Bassaganya-Riera, no conflicts of interest.
Supplemental Table 1 and Figure 1 are available with the online posting of this paper at jn.nutrition.org.
Abbreviations used: CD, Crohn's disease; CLA, conjugated linoleic acid; CRC, colorectal cancer;DSS, dextran sodium sulfate; FACS, fluorescence activated cell sorting; FBS, fetal bovine serum; FITC, fluorescein isothiocyanate; IBD, inflammatory bowel disease; IEC, intestinal epithelial cell; IL-4, interleukin-4; MLN, mesenteric lymph node; TNFα, tumor necrosis factor-α; Treg, regulatory T cell; UC, ulcerative colitis.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96. [DOI] [PubMed] [Google Scholar]
- 2.Miller BA, Chu KC, Hankey BF, Ries LA. Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control. 2008;19:227–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ries LA, Melbert D, Krapcho M, Stinchcomb DG, Howlader N, Horner MJ, Mariotto A, Miller BA, Feuer EJ, et al. SEER Cancer Statistics Review, 1975–2005. Bethesda (MD): National Cancer Institute; 2008.
- 4.Spunt S, Furman W, La Quaglia M, Bondy M, Goldberg R. Cancer epidemiology in older adolescents and young adults 15 to 29 years of age. In: SEER AYA monograph. Bethesda (MD): National Cancer Institute; 2008. p. 123–33.
- 5.Munkholm P. Review article: the incidence and prevalence of colorectal cancer in inflammatory bowel disease. Aliment Pharmacol Ther. 2003;18 Suppl 2:1–5. [DOI] [PubMed] [Google Scholar]
- 6.Calder PC. Dietary fatty acids and the immune system. Nutr Rev. 1998;56:S70–83. [DOI] [PubMed] [Google Scholar]
- 7.Calder PC. Polyunsaturated fatty acids, inflammatory processes and inflammatory bowel diseases. Mol Nutr Food Res. 2008;52:885–97. [DOI] [PubMed] [Google Scholar]
- 8.Tontonoz P, Nagy L, Alvarez JG, Thomazy VA, Evans RM. PPARgamma promotes monocyte/macrophage differentiation and uptake of oxidized LDL. Cell. 1998;93:241–52. [DOI] [PubMed] [Google Scholar]
- 9.Thompson EA. PPARgamma physiology and pathology in gastrointestinal epithelial cells. Mol Cells. 2007;24:167–76. [PubMed] [Google Scholar]
- 10.Clark RB, Bishop-Bailey D, Estrada-Hernandez T, Hla T, Puddington L, Padula SJ. The nuclear receptor PPAR gamma and immunoregulation: PPAR gamma mediates inhibition of helper T cell responses. J Immunol. 2000;164:1364–71. [DOI] [PubMed] [Google Scholar]
- 11.Hontecillas R, Wannemeulher MJ, Zimmerman DR, Hutto DL, Wilson JH, Ahn DU, Bassaganya-Riera J. Nutritional regulation of porcine bacterial-induced colitis by conjugated linoleic acid. J Nutr. 2002;132:2019–27. [DOI] [PubMed] [Google Scholar]
- 12.McNeel RL, Smith EO, Mersmann HJ. Isomers of conjugated linoleic acid modulate human preadipocyte differentiation. In Vitro Cell Dev Biol Anim. 2003;39:375–82. [DOI] [PubMed] [Google Scholar]
- 13.Meadus WJ, MacInnis R, Dugan ME. Prolonged dietary treatment with conjugated linoleic acid stimulates porcine muscle peroxisome proliferator activated receptor gamma and glutamine-fructose aminotransferase gene expression in vivo. J Mol Endocrinol. 2002;28:79–86. [DOI] [PubMed] [Google Scholar]
- 14.Kohno H, Suzuki R, Yasui Y, Hosokawa M, Miyashita K, Tanaka T. Pomegranate seed oil rich in conjugated linolenic acid suppresses chemically induced colon carcinogenesis in rats. Cancer Sci. 2004;95:481–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bassaganya-Riera J, Reynolds K, Martino-Catt S, Cui Y, Hennighausen L, Gonzalez F, Rohrer J, Benninghoff AU, Hontecillas R. Activation of PPAR gamma and delta by conjugated linoleic acid mediates protection from experimental inflammatory bowel disease. Gastroenterology. 2004;127:777–91. [DOI] [PubMed] [Google Scholar]
- 16.Yu Y, Correll PH, Vanden Heuvel JP. Conjugated linoleic acid decreases production of pro-inflammatory products in macrophages: evidence for a PPAR gamma-dependent mechanism. Biochim Biophys Acta. 2002;1581:89–99. [DOI] [PubMed] [Google Scholar]
- 17.Bassaganya-Riera J, Hontecillas R, Beitz DC. Colonic anti-inflammatory mechanisms of conjugated linoleic acid. Clin Nutr. 2002;21:451–9. [DOI] [PubMed] [Google Scholar]
- 18.Park Y, Storkson JM, Albright KJ, Liu W, Pariza MW. Evidence that the trans-10,cis-12 isomer of conjugated linoleic acid induces body composition changes in mice. Lipids. 1999;34:235–41. [DOI] [PubMed] [Google Scholar]
- 19.Nagao K, Inoue N, Wang YM, Yanagita T. Conjugated linoleic acid enhances plasma adiponectin level and alleviates hyperinsulinemia and hypertension in Zucker diabetic fatty (fa/fa) rats. Biochem Biophys Res Commun. 2003;310:562–6. [DOI] [PubMed] [Google Scholar]
- 20.Bassaganya-Riera J, Hontecillas R. CLA and n-3 PUFA differentially modulate clinical activity and colonic PPAR-responsive gene expression in a pig model of experimental IBD. Clin Nutr. 2006;25:454–65. [DOI] [PubMed] [Google Scholar]
- 21.Serini S, Piccioni E, Merendino N, Calviello G. Dietary polyunsaturated fatty acids as inducers of apoptosis: implications for cancer. Apoptosis. 2009;14:135–52. [DOI] [PubMed] [Google Scholar]
- 22.O'Shea M, Bassaganya-Riera J, Mohede IC. Immunomodulatory properties of conjugated linoleic acid. Am J Clin Nutr. 2004;79:S1199–206. [DOI] [PubMed] [Google Scholar]
- 23.Lewis JD, Lichtenstein GR, Deren JJ, Sands BE, Hanauer SB, Katz JA, Lashner B, Present DH, Chuai S, et al. Rosiglitazone for active ulcerative colitis: a randomized placebo-controlled trial. Gastroenterology. 2008;134:688–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Marcy TR, Britton ML, Blevins SM. Second-generation thiazolidinediones and hepatotoxicity. Ann Pharmacother. 2004;38:1419–23. [DOI] [PubMed] [Google Scholar]
- 25.Nesto RW, Bell D, Bonow RO, Fonseca V, Grundy SM, Horton ES, Le Winter M, Porte D, Semenkovich CF, et al. Thiazolidinedione use, fluid retention, and congestive heart failure: a consensus statement from the American Heart Association and American Diabetes Association. October 7, 2003. Circulation. 2003;108:2941–8. [DOI] [PubMed] [Google Scholar]
- 26.Carter AB, Misyak SA, Hontecillas R, Bassaganya-Riera J. Dietary modulation of inflammation-induced colorectal cancer through PPARgamma. PPAR Res. 2009;2009:498352. [DOI] [PMC free article] [PubMed]
- 27.Guri AJ, Hontecillas R, Si H, Liu D, Bassaganya-Riera J. Dietary abscisic acid ameliorates glucose tolerance and obesity-related inflammation in db/db mice fed high-fat diets. Clin Nutr. 2007;26:107–16. [DOI] [PubMed] [Google Scholar]
- 28.Kohno H, Suzuki R, Sugie S, Tanaka T. Suppression of colitis-related mouse colon carcinogenesis by a COX-2 inhibitor and PPAR ligands. BMC Cancer. 2005;5:46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saubermann LJ, Beck P, De Jong YP, Pitman RS, Ryan MS, Kim HS, Exley M, Snapper S, Balk SP, et al. Activation of natural killer T cells by alpha-galactosylceramide in the presence of CD1d provides protection against colitis in mice. Gastroenterology. 2000;119:119–28. [DOI] [PubMed] [Google Scholar]
- 30.Riddell RH, Goldman H, Ransohoff DF, Appelman HD, Fenoglio CM, Haggitt RC, Ahren C, Correa P, Hamilton SR, et al. Dysplasia in inflammatory bowel disease: standardized classification with provisional clinical applications. Hum Pathol. 1983;14:931–68. [DOI] [PubMed] [Google Scholar]
- 31.Pascal RR. Dysplasia and early carcinoma in inflammatory bowel disease and colorectal adenomas. Hum Pathol. 1994;25:1160–71. [DOI] [PubMed] [Google Scholar]
- 32.Bassaganya-Riera J, Guri AJ, Noble AM, Reynolds KA, King J, Wood CM, Ashby M, Rai D, Hontecillas R. Arachidonic acid-and docosahexaenoic acid-enriched formulas modulate antigen-specific T cell responses to influenza virus in neonatal piglets. Am J Clin Nutr. 2007;85:824–36. [DOI] [PubMed] [Google Scholar]
- 33.Hontecillas R, Bassaganya-Riera J, Wilson J, Hutto DL, Wannemuehler MJ. CD4+ T-cell responses and distribution at the colonic mucosa during Brachyspira hyodysenteriae-induced colitis in pigs. Immunology. 2005;115:127–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dai Y, Qiao L, Chan KW, Yang M, Ye J, Ma J, Zou B, Gu Q, Wang J, et al. Peroxisome proliferator-activated receptor-gamma contributes to the inhibitory effects of Embelin on colon carcinogenesis. Cancer Res. 2009;69:4776–83. [DOI] [PubMed] [Google Scholar]
- 35.Takano S, Kubota T, Nishibori H, Hasegawa H, Ishii Y, Nitori N, Ochiai H, Okabayashi K, Kitagawa Y, et al. Pioglitazone, a ligand for peroxisome proliferator-activated receptor-gamma acts as an inhibitor of colon cancer liver metastasis. Anticancer Res. 2008;28:3593–9. [PubMed] [Google Scholar]
- 36.Ogino S, Shima K, Baba Y, Nosho K, Irahara N, Kure S, Chen L, Toyoda S, Kirkner GJ, et al. Colorectal cancer expression of peroxisome proliferator-activated receptor gamma (PPARG, PPARgamma) is associated with good prognosis. Gastroenterology. 2009;136:1242–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pancione M, Forte N, Sabatino L, Tomaselli E, Parente D, Febbraro A, Colantuoni V. Reduced beta-catenin and peroxisome proliferator-activated receptor-gamma expression levels are associated with colorectal cancer metastatic progression: correlation with tumor-associated macrophages, cyclooxygenase 2, and patient outcome. Hum Pathol. 2009;40:714–25. [DOI] [PubMed] [Google Scholar]
- 38.Fujisawa T, Sugiyama M, Tomimoto A, Wada K, Endo H, Takahashi H, Yoneda K, Yoneda M, Inamori M, et al. Inhibition of peroxisome proliferator-activated receptor gamma promotes tumorigenesis through activation of the beta-catenin/T cell factor (TCF) pathway in the mouse intestine. J Pharmacol Sci. 2008;108:535–44. [DOI] [PubMed] [Google Scholar]
- 39.Su W, Bush CR, Necela BM, Calcagno SR, Murray NR, Fields AP, Thompson EA. Differential expression, distribution, and function of PPAR-gamma in the proximal and distal colon. Physiol Genomics. 2007;30:342–53. [DOI] [PubMed] [Google Scholar]
- 40.Lefebvre M, Paulweber B, Fajas L, Woods J, McCrary C, Colombel JF, Najib J, Fruchart JC, Datz C, et al. Peroxisome proliferator-activated receptor gamma is induced during differentiation of colon epithelium cells. J Endocrinol. 1999;162:331–40. [DOI] [PubMed] [Google Scholar]
- 41.Chen L, Necela BM, Su W, Yanagisawa M, Anastasiadis PZ, Fields AP, Thompson EA. Peroxisome proliferator-activated receptor gamma promotes epithelial to mesenchymal transformation by Rho GTPase-dependent activation of ERK1/2. J Biol Chem. 2006;281:24575–87. [DOI] [PubMed] [Google Scholar]
- 42.Hontecillas R, Bassaganya-Riera J. Peroxisome proliferator-activated receptor gamma is required for regulatory CD4+ T cell-mediated protection against colitis. J Immunol. 2007;178:2940–9. [DOI] [PubMed] [Google Scholar]
- 43.Chung SW, Kang BY, Kim SH, Pak YK, Cho D, Trinchieri G, Kim TS. Oxidized low density lipoprotein inhibits interleukin-12 production in lipopolysaccharide-activated mouse macrophages via direct interactions between peroxisome proliferator-activated receptor-gamma and nuclear factor-kappa B. J Biol Chem. 2000;275:32681–7. [DOI] [PubMed] [Google Scholar]
- 44.Wang L, Zhu J, Shan S, Qin Y, Kong Y, Liu J, Wang Y, Xie Y. Repression of interferon-gamma expression in T cells by Prospero-related homeobox protein. Cell Res. 2008;18:911–20. [DOI] [PubMed] [Google Scholar]
- 45.Swirski FK, Libby P, Aikawa E, Alcaide P, Luscinskas FW, Weissleder R, Pittet MJ. Ly-6Chi monocytes dominate hypercholesterolemia-associated monocytosis and give rise to macrophages in atheromata. J Clin Invest. 2007;117:195–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5:953–64. [DOI] [PubMed] [Google Scholar]
- 47.Bassaganya-Riera J, Misyak S, Guri AJ, Hontecillas R. PPAR gamma is highly expressed in F4/80 (hi) adipose tissue macrophages and dampens adipose-tissue inflammation. Cell Immunol. 2009;258:138–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vitale S, Cambien B, Karimdjee BF, Barthel R, Staccini P, Luci C, Breittmayer V, Anjuere F, Schmid-Alliana A, et al. Tissue-specific differential antitumour effect of molecular forms of fractalkine in a mouse model of metastatic colon cancer. Gut. 2007;56:365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Geissmann F, Auffray C, Palframan R, Wirrig C, Ciocca A, Campisi L, Narni-Mancinelli E, Lauvau G. Blood monocytes: distinct subsets, how they relate to dendritic cells, and their possible roles in the regulation of T-cell responses. Immunol Cell Biol. 2008;86:398–408. [DOI] [PubMed] [Google Scholar]
- 50.Szeles L, Torocsik D, Nagy L. PPARgamma in immunity and inflammation: cell types and diseases. Biochim Biophys Acta. 1771;2007:1014–30. [DOI] [PubMed] [Google Scholar]
- 51.Gocke AR, Hussain RZ, Yang Y, Peng H, Weiner J, Ben LH, Drew PD, Stuve O, Lovett-Racke AE, et al. Transcriptional modulation of the immune response by peroxisome proliferator-activated receptor-{alpha} agonists in autoimmune disease. J Immunol. 2009;182:4479–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ringseis R, Wen G, Saal D, Eder K. Conjugated linoleic acid isomers reduce cholesterol accumulation in acetylated LDL-induced mouse RAW264.7 macrophage-derived foam cells. Lipids. 2008;43:913–23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.