Abstract
A laboratory study of older adults with osteoarthritis and their spouses was conducted to examine the unique influence of exposure to suffering on caregivers’ risk for impaired psychological and physical health. Spouses’ blood pressure (BP) and heart rate (HR) were monitored during 2 tasks designed to capture their partners’ suffering. First, spouses watched their partners (and a stranger) carry heavy logs across an 8-ft space for 3 min, a task that elicited pain expression. Second, spouses spoke about their partners’ suffering (and also about a typical meal with their partners). Results showed that spouses’ BP and HR increased when watching and talking about their partners’ suffering, and exposure to a partner’s suffering was more physiologically stressful than to a stranger’s suffering. These findings suggest that heightened physiological stress caused by exposure to a loved one’s suffering may be one pathway to caregivers’ increased risk for cardiovascular disease.
Keywords: Cardiovascular reactivity, Caregiving, Interpersonal relationships, Osteoarthritis, Suffering
CARING for a spouse with a disease or disability can have negative consequences for one’s physical and psychological health (Schulz & Beach, 1999; Vitaliano, Zhang, & Scanlan, 2003). However, there is still much debate about the specific pathways through which this occurs. Most research has focused on the physical demands of providing care, staying vigilant to care recipients’ needs, and dealing with problem behaviors (Pinquart & Sörensen, 2003). We suggest that another important pathway is the emotional stress that results from exposure to a loved one’s suffering, partially manifest as increased cardiovascular reactivity.
In close relationships, suffering can be contagious. Numerous studies have shown strong associations between husbands’ and wives’ emotional distress, even after controlling for the effects of sociodemographic factors, functional and health statuses of both members of the dyad, and shared life events (Bookwala & Schulz, 1996; Gaugler et al., 2005; Tower & Kasl, 1995, 1996). People are physiologically reactive to witnessing close others’ pain (Block, 1981; Singer et al., 2004), and there is evidence that partners’ suffering, conceptualized as physical symptoms, psychological distress, and existential or spiritual distress, directly influences caregivers’ depression and prevalence of cardiovascular disease (Schulz et al., 2008, 2009). Emotional distress is likely to mediate the link between partners’ suffering and caregivers’ increased risk for cardiovascular disease. An extensive literature demonstrates that emotional distress increases cardiovascular reactivity (see Bradley & Lang, 2007 and Levenson, 1992 for reviews), and there is evidence to suggest that heightened cardiovascular reactivity over time is associated with an increased risk for cardiovascular disease (Jennings et al., 2004 ; Manuck, Marsland, Kaplan, & Williams, 1995; Treiber et al., 2003).
Although there are a number of studies showing that caregiving, in general, is associated with increased cardiovascular reactivity (Grant et al., 2002; King, Oka, & Young, 1994; Shaw et al., 1997, 1999; Vitaliano, Russo, Bailey, Young, & McCann, 1993; Vitaliano et al., 2002), these studies are descriptive and cross-sectional, and it is unclear what aspects of caregiving are responsible for this increase in reactivity. One exception is a laboratory study by Vitaliano and colleagues suggesting that talking broadly about the emotional aspects of caring for a loved one with Alzheimer’s disease, compared with performing a cognitive task, is associated with higher blood pressure (BP). Although this study shows that a caregiver’s emotional account of the relationship is an important predictor of cardiovascular reactivity, further specificity is needed. We suggest that witnessing a partner’s suffering, in particular, may play an important role in increasing caregivers’ cardiovascular reactivity. Thus, one aim of the present study was to examine the extent to which exposure to a partner’s suffering affects cardiovascular reactivity in an experimental setting. We operationalize exposure to suffering in two ways: We asked spouses to watch their partners perform a pain-eliciting household task and talk about three dimensions of their partners’ suffering—physical symptoms (e.g., pain and fatigue), psychological distress (e.g., anxiety and depression), and existential or spiritual distress (e.g., loss of purpose of life, comfort from religious beliefs). We chose an older adult married sample in which one person was coping with osteoarthritis (OA) because OA is a common chronic condition in later life that often entails pain, disability, and suffering (Centers for Disease Control and Prevention, 2004), and spouses of people with OA are likely to be exposed to their partners’ suffering on a regular basis.
A second aim of this study was to examine the extent to which the nature of the relationship influenced a person’s cardiovascular response to another person’s suffering. Research suggests that relationship type and closeness influence emotional and physiological convergence between two individuals. For example, Langford and colleagues (2006) found that mice which were exposed to cage-mates in pain also displayed pain behaviors themselves, and this did not occur for non–cage-mates. These effects were only marginally enhanced in same-sex siblings living together, and a separate experiment confirmed that close genetic relatedness was not required. Human research also demonstrates that valuing another person’s welfare and relationship satisfaction increase empathic reactions to others’ pain (Block, 1981; Singer et al., 2004) and depression (Tower & Kasl, 1995, 1996). Thus, the extent to which people are familiar with and close to one another is likely to influence their psychological and physiological responses to suffering. Therefore, in the current study, we compared cardiovascular reactivity to spouses’ versus opposite-sex strangers’ physical suffering while performing a pain-eliciting task. To gain a deeper understanding of how closeness affects physiological reactions to a partner’s suffering among spouses in particular, we also examined marital satisfaction as a moderator.
Hypotheses
Our central hypothesis is that exposure to suffering in a laboratory setting will uniquely influence caregiving spouses’ cardiovascular functioning. Specifically, we hypothesize that (1) watching a stranger perform a pain-eliciting task will increase caregivers’ systolic and diastolic BP and heart rate (HR) compared with watching a habituation stimulus, but (2) caregivers will have higher BP and HR responses to watching a partner’s than a stranger’s physical suffering. We also hypothesize that (3) talking about the partner’s physical, psychological, and existential or spiritual suffering will increase the caregiver’s BP and HR compared with talking about a mundane interaction such as having lunch with the partner. We will also explore the extent to which marital satisfaction moderates the association between partner suffering and spouses’ BP and HR. We hypothesize that greater marital satisfaction will be associated with greater BP and HR reactivity.
METHODS
Participants
Fifty-three care recipients with OA and their caregiving spouses participated in the study. Care recipients consisted of 27 women and 26 men (mean age = 69.67 years, SD = 8.69; 84.9% Caucasian, 11.3% African American, 3.8% other; 3.8% did not complete high school, 22.6% completed high school only; 49% attended college, 22.6% attended graduate school). Spouses had a mean age of 68.75 (SD = 9.80; 83% Caucasian, 11.3% African American, 5.7% other; 5.7% did not complete high school, 20.8% completed high school only; 41.5% attended college, 32.1% attended graduate school). Participants were recruited from the Gerontology Research Registry at the University of Pittsburgh, which is a database composed of participants from concurrent or past research studies of older adults at the University of Pittsburgh. In order to be eligible to participate in the present study, care recipients had to be more than 45 years old, have experienced pain of at least moderate intensity over the past month, had difficulty with at least one instrumental activity of daily living (IADL), and received assistance from the caregiver with at least one IADL. Participants had to meet a standard criterion (i.e., at least 7 of 10 items answered correctly) for cognitive functioning as measured by the Short Portable Mental Status Questionnaire (Pfeiffer, 1975). Finally, couples were excluded if the caregiver took beta-blockers, because this medication affects HR, one of the primary outcomes of the study. However, caregivers were asked to provide a list and reasons for taking other medications. Medications were evaluated using the Physician’s Desk Reference and classified into a categorical variable for analyses as either having a primary effect or having a 10% frequency of a side effect on BP and HR or not (56.6% of caregivers took medications that had an effect on BP and HR). Eligibility criteria were assessed over the phone before scheduling a laboratory appointment.
Preparation of Stimuli
Habituation video.—
Prior to the study, two standardized videos were made of a healthy older man and a healthy older woman, each walking back and forth across an 8-ft space for 3 min without expressing any pain. These videos were captured with a digital video camera in color with no sound. One of these videos (depicting an opposite-sex target) was shown to caregivers as a control condition.
Stranger performing pain-eliciting log task.—
Two standardized videos were also made prior to the study of one older male “stranger” and one older female “stranger” (who both met the same requirements as the care recipients and were not known to caregivers in the study) expressing pain while performing a log-carrying task for 3 min. These videos were in color and included sound. In the log-carrying task, the stranger loaded two 5-lb artificial logs into a leather carrier, carried the logs across an 8-ft space, unloaded each log from the carrier, and repeated the process. This task is similar to those used in previous research on participants with OA and their caregiving spouses to elicit pain expression (Martire et al., 2006; Romano et al., 1991). The strangers were instructed to freely express pain verbally and nonverbally as they experienced it. In addition, they were asked to act as naturally as possible and to pretend they were doing the task at home. Caregivers later watched the video of the opposite-sex stranger in one condition of the experimental session. These videos were used to test the hypothesis that caregivers’ BP and HR are higher when watching a partner compared with a stranger perform a pain-eliciting task.
Because it was not possible to exactly match the stranger and partner conditions in terms of the objective amount of pain expressed, we examined overall differences in pain expression between the stranger and partner videos using independent observers. Ten independent observers rated the pain expression of one of the stranger videos and one of the 10 randomly selected partner videos on a scale from 0 (no pain) to 10 (pain as bad as could be). Raters were not aware of which videos were of strangers and which were of actual participants. According to the observers, more pain was expressed in the stranger videos (M = 4.60, SD = 2.01) than in the partner videos (M = 2.45, SD = 2.50; t(9) = 3.04, p < .05).
Procedure: The Experimental Session
Videotaping the care recipient perform the pain-eliciting log task.—
Each couple came into the laboratory for a 2-hr session. After introductions and consent, the experimenter escorted the caregiver to a waiting room. Meanwhile, the care recipient was videotaped performing the pain-eliciting log-carrying task (see details of the task in the previous section) in a separate area of the laboratory. The video was in color and included sound. The care recipient was instructed to freely express pain verbally and nonverbally as he or she experienced it. It was emphasized that the care recipient express his or her pain as it was felt and not to exaggerate or fake the expression of pain, to act as naturally as possible, and to pretend he or she was performing the task at home. The caregiver was not present during the care recipient’s performance of the task; however, the care recipient was told that the video would be shown to the caregiver during the consent process.
Baseline.—
Next, the caregiver was taken to a sound and electrically shielded chamber that was used to separate the caregiver from the external laboratory environment and reduce electrical noise in the physiological recordings. The caregiver was seated in a comfortable chair, and a video monitor for task presentation was placed on an adjustable platform immediately in front of him or her. The experimenter then explained to the caregiver that he or she would be watching a series of videos and talking about some experiences while his or her BP and HR was monitored. The experimenter explained how the physiological equipment worked and tried to allay any anxiety the caregiver may have felt. The experimenter then attached three silver–silver chloride electrodes to the caregiver (using a modified lead II electrode placement) for measurement of the electrocardiogram (ECG) and placed a standard BP cuff on the upper nondominant arm connected to a General Electric Dinamap Vital Signs Monitor. The experimenter then left the room and took baseline measurements of systolic and diastolic BP and HR for 3 min. BP measurements were taken three times, and HR was monitored continuously during this period. All subsequent conditions also lasted 3 min, with BP measurements taken three times and HR continuously monitored.
Habituation and exposure to partner’s and stranger’s physical suffering.—
After the baseline period, the caregiver privately viewed the habituation stimulus (the video of the opposite-sex adult walking). Next, the caregiver watched the videotape either of his or her partner or of the opposite-sex stranger performing the log-carrying task. The order in which caregivers watched the partner and stranger log tasks was counterbalanced. The habituation condition was used as a comparison to the log task conditions to control for watching the movement of a person.
Verbal accounts of a mundane interaction and an episode of physical, psychological, and existential or spiritual suffering.—
Caregivers were asked to give two verbal accounts about the care recipient. A similar procedure has been used by Vitaliano and colleagues (1993). Caregivers were provided with written guidelines around which to organize their accounts. For one of the speeches, caregivers were asked to spend 3 min describing an interaction with the care recipient during a meal together. According to a manipulation check, in which participants rated the extent to which they felt four types of personal distress (disturbed, uneasy, distressed, troubled) on a 7-point scale (1, not at all; 7, extremely) after speaking, participants did not find this to be very distressing (M = 1.77, SD = 1.17). For the other account, caregivers were asked to spend 3 min talking about a specific instance in which the caregiver felt that the care recipient was suffering. Caregivers were asked to elaborate on three dimensions of suffering—physical, psychological, and existential or spiritual aspects. A manipulation check revealed that this was more distressing than talking about the typical meal (M = 4.42, SD = 2.09; t(52) = −9.58, p < .001). The verbal accounts were counterbalanced.
BP and HR
For each condition, a systolic BP mean and a diastolic BP mean were calculated by averaging each of the three automated measurements taken over the 3-min periods. To assess mean HR during each period, R-wave markers in the ECG signal were assessed for artifacts by visual inspection and by an automatic artifact detection algorithm available in a customized software package (Mindware Heart Rate Variability Scoring Module, version 2.16; Mindware Technologies Ltd, Columbus, OH). Following manual corrections of suspected artifacts, the Mindware program estimated the mean HR for each caregiver for each 3-min condition.
Marital Satisfaction
Caregivers were asked to report their level of marital satisfaction using the Marital Adjustment Test (MAT; Locke & Wallace, 1959) at the beginning of the laboratory session in a separate room from their spouse. This measure was completed in addition to a series of other background measures not relevant to the present study hypotheses. The 16-item measure includes one question about the participant’s general level of happiness in the marriage using a scale from 1 (very unhappy) to 7 (perfectly happy), eight questions about agreement or disagreement with the spouse on issues such as handling finances, friends, and philosophy of life on a scale from 1 (always agree) to 6 (always disagree), and seven questions that explore issues such as whether spouses confide in their partner, whether they would marry the same person again, and whether they have similar interests in activities. The scores for the different items are weighted based on their criterion validity in predicting maladjustment and divorce (Locke & Wallace). The range of possible scores is 2–158, with higher scores indicating greater marital satisfaction. The mean marital satisfaction score using the MAT for U.S. samples is 100 (SD = 15; Locke & Wallace). In the present study, caregivers’ average marital satisfaction score was 92.54 (SD = 13.60).
RESULTS
Baseline Differences in Caregivers’ Physiology
First, we entered gender, age, and use of BP medication into multivariate regression models predicting baseline systolic and diastolic BP and HR. We found significant effects of gender on baseline BP such that men had higher systolic and diastolic BP than women (β = .34, t(50) = 2.56, p < .05 and β = .38, t(50) = 2.81, p < .05, respectively). We also found that older caregivers had higher systolic BP at baseline (β = .28, t(50) = 2.12, p < .05). Medications did not have a significant effect on any of the physiological indicators.
Caregivers Are Physiologically Reactive to Suffering
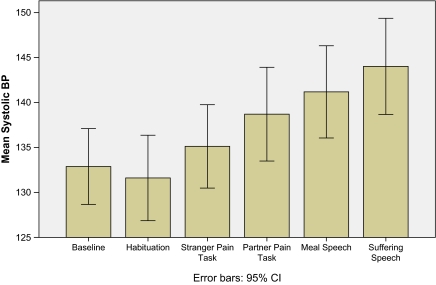
Before testing our hypotheses, we examined whether baseline physiology influenced the extent to which physiology increased from baseline to each experimental condition by calculating difference scores between baseline and each experimental condition and correlating the difference scores with baseline measures. Because these correlations were not significant (r values ranged from −.07 to .11 for systolic BP, −.09 to .00 for diastolic BP, and −.21 to −.15 for HR), we conducted repeated measures analyses of variance to test hypotheses 1 and 2 and t tests to test hypothesis 3 using the unadjusted difference scores. Table 1 shows means and standard deviations for caregivers’ systolic BP, diastolic BP, and mean HR in each condition. The sample size varies for some of the measures and conditions for the following reasons: One caregiver did not watch the habituation video because he or she recognized the target; one care recipient was unable to perform the pain-eliciting task due to high BP; and the remaining variation in sample size was due to issues with movement and instrument connectivity. See Figure 1 for systolic BP means in response to the different experimental conditions (diastolic BP and HR followed a similar pattern).
Table 1.
Caregivers’ Systolic and Diastolic BP and Mean HR Throughout the Experiment
| Systolic BP |
Diastolic BP |
HR |
|||||||
| n | M | SD | n | M | SD | n | M | SD | |
| Baseline | 53 | 132.27 | 14.77 | 53 | 70.19 | 11.50 | 51 | 67.71 | 9.60 |
| Habituation | 52 | 131.38 | 16.64 | 52 | 69.54 | 11.99 | 51 | 67.19 | 9.85 |
| Partner pain | 52 | 138.46 | 18.23 | 52 | 72.45 | 13.52 | 44 | 69.16 | 10.38 |
| Stranger pain | 53 | 134.54 | 16.19 | 53 | 70.56 | 12.31 | 49 | 68.19 | 10.13 |
| Verbal account of typical meal | 52 | 140.43 | 18.16 | 53 | 76.31 | 13.23 | 52 | 70.22 | 9.97 |
| Verbal account of partner’s suffering | 53 | 143.45 | 18.61 | 53 | 79.07 | 14.63 | 50 | 71.16 | 10.89 |
Notes: BP = blood pressure; HR = heart rate.
Figure 1.
Caregivers’ systolic blood pressure (BP) in response to different experimental conditions.
Watching stranger’s and partner’s physical suffering.—
Our first hypothesis was that caregivers would have increased systolic and diastolic BP and increased HR when watching a stranger perform a pain-eliciting task compared with a habituation stimulus. Our second hypothesis was that caregivers would be more reactive to their partners’ pain than to strangers’ pain. Overall, repeated measures analyses revealed results consistent with our predictions (see Table 2). Effect sizes (partial eta squared) for the significant effects ranged from .12 to .30.
Table 2.
Repeated Measures ANOVA and Contrasts: Comparing Physiological Reactivity Between Habituation, Stranger, and Partner Conditions
| Within-subject effects |
Habituation vs. stranger |
Stranger vs. partner |
|||||||
| df | F | Partial eta squared | df | F | Partial eta squared | df | F | Partial eta squared | |
| Systolic BP | 2 | 20.95** | .30 | 1 | 12.89** | .21 | 1 | 11.34** | .19 |
| Diastolic BP | 2 | 6.45** | .14 | 1 | 1.32 | .03 | 1 | 6.67* | .12 |
| HR | 2 | 8.60** | .18 | 1 | 8.34** | 17 | 1 | 2.71 | .07 |
Notes: Difference scores between baseline physiology and physiology in each experimental condition were used in analyses. ANOVA = analysis of variance; BP = blood pressure; HR = heart rate.
p < .05; **p < .01.
Talking about the partner's physical, psychological, and existential or spiritual suffering.—
Our third hypothesis was that caregivers would have increased systolic and diastolic BP and increased HR when talking about their partners’ suffering compared with talking about a mundane interaction. Results of the t tests were consistent with our predictions (see Table 3). Effect sizes (Cohen’s d) were .50 for systolic BP, .54 for diastolic BP, and .53 for HR.
Table 3.
t Tests: Comparing Physiological Reactivity Between Talking About a Typical Interaction with a Partner and a Partner’s Suffering
| df | t | Cohen's d | |
| Systolic BP | 51 | −2.46* | .50 |
| Diastolic BP | 51 | −2.23* | .54 |
| HR | 48 | −2.48* | .53 |
Notes: Difference scores between baseline physiology and physiology in each experimental condition were used in analyses. BP = blood pressure; HR = heart rate.
p < .05.
Did Marital Satisfaction Influence Reactivity to Partners’ Suffering?
After establishing that marital satisfaction was not related to baseline differences in BP or HR, we tested our hypothesis that marital satisfaction is related to higher cardiovascular reactivity to the partner’s suffering. We did this by simultaneously entering caregivers’ marital satisfaction, age, gender, and medication use into multivariate regression models predicting BP and HR changes from control to experimental conditions using difference scores (e.g., the difference between systolic BP during habituation and while watching the partner in pain and the difference between systolic BP during talking about a typical meal and talking about the partner’s suffering). In contrast to our hypothesis, there were no significant effects of marital satisfaction on changes in reactivity from control to experimental conditions for any of the physiological indicators. (The possible moderating effects of gender were also explored for each of the hypotheses. No significant findings resulted from these exploratory analyses.)
DISCUSSION
The results of the current study indicate that exposure to a partner’s suffering increases cardiovascular reactivity. Specifically, we found that witnessing another person perform a pain-eliciting household task, compared with watching a habituation stimulus, increases BP and HR, and BP and HR reactivity is higher when the person performing the pain-eliciting task is a spouse compared with a stranger. This was the case even when independent observers rated strangers as expressing more pain than spouses in the videos. We also found that talking about the suffering of the partner compared with talking about a mundane interaction with the partner also increases BP and HR. These data suggest that close family members are at particular risk for the negative health consequences of caregiving and that exposure to suffering is a key factor contributing to these effects.
Caregiving literature has consistently shown increased morbidity associated with strained caregiving but has been relatively silent regarding mechanisms that might account for these effects. Descriptive and case−control studies have identified a number of physiological mechanisms, such as decreased immune functioning, fluctuations in stress hormones, and metabolic changes, that might contribute to health declines (Schulz & Sherwood, 2008). However, these studies are open to methodological criticism because they often use cross-sectional analyses and do not control for possible confounds (e.g., existing health conditions, age, socioeconomic status). Moreover, these studies typically link mechanisms to caregiving stress in general as opposed to specific features of the caregiving experience. Ours is the first study to identify a specific aspect of the caregiving experience—care recipient suffering—and to assess its physiological impact experimentally.
What are some of the implications of our study findings? First, we found that “merely” observing the suffering of partners or talking about the suffering of partners affects caregivers’ well-being. This raises the question of whether other noncaregiving relatives of chronically ill adults experience similar effects of a partner’s suffering. Research by Amirkhanyan and Wolf (2003) suggests that noncaregiving adult children of ill parents experience heightened depressive symptoms compared with caregiving children. This previous research suggests that not only is it important to compare responses to relationship partners and strangers, but future research should also examine different types of relationships (e.g., friends, parents, professional health care workers).
What are the implications of the present study for assessment and interventions for care recipients and caregivers? Interventions that address a partner’s suffering have received little attention in the caregiver intervention literature. Our findings suggest that intervention strategies that directly affect the suffering of the care recipient may be particularly effective in alleviating caregiver distress. Under circumstances where opportunities to control suffering are limited, interventions that help caregivers regulate their emotions may also be useful (e.g., mindfulness therapy; Bishop et al., 2004). Furthermore, a dyadic or couples-oriented approach to implementing intervention strategies is likely to achieve positive effects for both care recipients and caregivers (Berg & Upchurch, 2007; Martire, 2005; Martire & Schulz, 2007).
There are some limitations to this work. Because we used care recipients’ actual behavior as stimuli in the experimental conditions, we were not able to control the amount of suffering that was expressed. Also, the stimuli, although real, were probably less impactful than the types of suffering experienced when caring for a person with high levels of cognitive and physical disability, such as Alzheimer’s disease. We also did not measure respiration during the speech tasks. Differences in respiration along with voice intensity and pace might conceivably contribute to the observed difference between talking about the meal and the suffering of the partner. Also, our sample size was small, which may have decreased our power in detecting the possible effects of marital satisfaction on physiological reactivity to partner suffering.
Taken together, the results of the present study indicate that heightened cardiovascular stress caused by exposure to a loved one’s suffering may be one pathway to caregivers’ increased risk for cardiovascular disease. Although detection of suffering in a loved one can be adaptive and initiate provision of emotional support and assistance, exposure to suffering may also take a physical toll on caregivers. A major strength of this study is that it is one of the first to use experimental methods with ecologically valid stimuli to examine emotional processes in the context of caring for older adults. Finally, our results have important implications for interventions, suggesting that caregivers are likely to benefit from efforts to alleviate care recipients’ suffering.
FUNDING
This work was supported by a Pittsburgh Mind Body Center pilot grant (National Institute of Health, HL076852/076858), the National Institute of Aging (F32 AG031635 to J. K. M.), and a Multidisciplinary Small Grant from the University of Pittsburgh’s Research Council
References
- Amirkhanyan AA, Wolf DA. Caregiver stress and noncaregiver stress: Exploring the pathways of psychiatric morbidity. Gerontologist. 2003;43:817–827. doi: 10.1093/geront/43.6.817. [DOI] [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133:920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal ZV, Abbey S, Speca M, Velting D, et al. Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice. 2004;11:230–241. [Google Scholar]
- Block AR. Investigation of the response of the spouse to chronic pain behavior. Psychosomatic Medicine. 1981;43:415–422. doi: 10.1097/00006842-198110000-00004. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Schulz R. Spousal similarity in subjective well-being: The Cardiovascular Health Study. Psychology and Aging. 1996;11:582–590. doi: 10.1037//0882-7974.11.4.582. [DOI] [PubMed] [Google Scholar]
- Bradley MM, Lang PJ. Emotion and motivation. In: Cacioppo JT, Tassinary LG, Bertson GG, editors. Handbook of psychophysiology. 3rd ed. New York: Cambridge University Press; 2007. pp. 587–589. [Google Scholar]
- Centers for Disease Control and Prevention. Facts about prevalence of arthritis—U.S., 2004. Atlanta, GA: Author; 2004. [Google Scholar]
- Gaugler JE, Hanna N, Linder J, Given CW, Tolbert V, Kataria R, Regine W. Cancer caregiving and subjective stress: A multi-site, multidimensional analysis. Psycho-Oncology. 2005;14:771–785. doi: 10.1002/pon.916. [DOI] [PubMed] [Google Scholar]
- Grant I, Adler KA, Patterson TL, Dimsdale JE, Ziegler MG, Irwin MR. Health consequences of Alzheimer's caregiving transitions: Effects of placement and bereavement. Psychosomatic Medicine. 2002;64:477–486. doi: 10.1097/00006842-200205000-00012. [DOI] [PubMed] [Google Scholar]
- Jennings JR, Kamarck TW, Everson-Rose SA, Kaplan GA, Manuck SB, Salonen JT. Exaggerated blood pressure responses during mental stress are prospectively related to enhanced carotid atherosclerosis in middle-aged Finnish men. Circulation. 2004;110:2198–2203. doi: 10.1161/01.CIR.0000143840.77061.E9. [DOI] [PubMed] [Google Scholar]
- King AC, Oka RK, Young DR. Ambulatory blood pressure and heart rate responses to the stress of work and caregiving in older women. Journal of Gerontology Series A: Biological Sciences and Medical Sciences. 1994;49:M239–M245. doi: 10.1093/geronj/49.6.m239. [DOI] [PubMed] [Google Scholar]
- Langford DJ, Crager SE, Shehzad Z, Smith SB, Sotocinal SG, Levenstadt JS, Chanda M, Levitin DJ, Mogil JS. Social modulation of pain as evidence for empathy in mice. Science. 2006;312:1967–1970. doi: 10.1126/science.1128322. [DOI] [PubMed] [Google Scholar]
- Levenson RW. Autonomic nervous system differences among emotions. Psychological Science. 1992;3:23–27. [Google Scholar]
- Locke H, Wallace K. Short marital-adjustment and prediction tests: Their reliability and validity. Marriage and Family Living. 1959;21:251–255. [Google Scholar]
- Manuck SB, Marsland AL, Kaplan JR, Williams JK. The pathogenicity of behavior and its neuroendocrine mediation: An example from coronary artery disease. Psychosomatic Medicine. 1995;57:275–283. doi: 10.1097/00006842-199505000-00009. [DOI] [PubMed] [Google Scholar]
- Martire LM. The “relative” efficacy of involving family in psychosocial interventions for chronic illness: Are there added benefits to patients and family members? Families, Systems & Health. 2005;23:312–328. [Google Scholar]
- Martire LM, Keefe FJ, Schulz R, Ready R, Beach SR, Rudy TE, Starz TW. Older spouses’ perceptions of partners’ chronic arthritis pain: Implications for spousal responses, support provision, and caregiving experiences. Psychology and Aging. 2006;21:222–230. doi: 10.1037/0882-7974.21.2.222. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R. Involving family in psychosocial interventions for chronic illness. Current Directions in Psychological Science. 2007;16:90–94. [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sörensen S. Associations of stressors and uplifts of caregiving with caregiver burden and depressive mood: A meta-analysis. Journal of Gerontology: Psychological Sciences. 2003;58:112–128. doi: 10.1093/geronb/58.2.p112. [DOI] [PubMed] [Google Scholar]
- Romano JM, Turner JA, Friedman LS, Bulcroft RA, Jensen MP, Hops H. Observational assessment of chronic pain patient-spouse behavioral interaction. Behavior Therapy. 1991;22:549–568. [Google Scholar]
- Schulz R, Beach SR. Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. Journal of the American Medical Association. 1999;282:2215–2260. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- Schulz R, Beach SR, Hebert RS, Martire LM, Monin JK, Tompkins CA, Albert SM. Spousal suffering and partner's depression and cardiovascular disease: The Cardiovascular Health Study. American Journal of Geriatric Psychiatry. 2009;17:1354–1372. doi: 10.1097/JGP.0b013e318198775b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, McGinnis KA, Zhang S, Martire LM, Hebert RS, Beach SR, Zdaniuk B, Czaja SJ, Belle SH. Dementia patient suffering and caregiver depression. Alzheimer Disease & Associated Disorders. 2008;22:170–176. doi: 10.1097/WAD.0b013e31816653cc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. American Journal of Nursing. 2008;108(9):23–27. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw WS, Patterson TL, Semple SJ, Ho S, Irwin MR, Hauger RL, Grant I. Longitudinal analysis of multiple indicators of health decline among spousal caregivers. Annals of Behavioral Medicine. 1997;19:101–109. doi: 10.1007/BF02883326. [DOI] [PubMed] [Google Scholar]
- Shaw WS, Patterson TL, Ziegler MG, Dimsdale J, Semple SJ, Grant I. Accelerated risk of hypertensive blood pressure recordings among Alzheimer caregivers. Journal of Psychosomatic Research. 1999;46:215–227. doi: 10.1016/s0022-3999(98)00084-1. [DOI] [PubMed] [Google Scholar]
- Singer T, Seymour B, O’Doherty J, Kaube H, Dolan RJ, Frith CD. Empathy for pain involves the affective but not sensory components of pain. Science. 2004;303:1157–1161. doi: 10.1126/science.1093535. [DOI] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses and the moderating effect of marital closeness. Psychology and Aging. 1995;10:625–638. doi: 10.1037//0882-7974.10.4.625. [DOI] [PubMed] [Google Scholar]
- Tower RB, Kasl SV. Depressive symptoms across older spouses: Longitudinal influences. Psychology and Aging. 1996;11:683–697. doi: 10.1037//0882-7974.11.4.683. [DOI] [PubMed] [Google Scholar]
- Treiber FA, Kamarck T, Schniederman N, Sheffield D, Kapuku G, Taylor T. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosomatic Medicine. 2003;65:46–62. doi: 10.1097/00006842-200301000-00007. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Russo J, Bailey SL, Young HM, McCann BS. Psychosocial factors associated with cardiovascular reactivity in older adults. Psychosomatic Medicine. 1993;55:164–177. doi: 10.1097/00006842-199303000-00005. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Scanlan JM, Zhang J, Savage MV, Hirsch I, Siegler IC. A path model of chronic stress, the metabolic syndrome, and coronary heart disease. Psychosomatic Medicine. 2002;64:418–435. doi: 10.1097/00006842-200205000-00006. [DOI] [PubMed] [Google Scholar]
- Vitaliano PP, Zhang J, Scanlan JM. Is caregiving hazardous to one's physical health? A meta-analysis. Psychological Bulletin. 2003;129:946–972. doi: 10.1037/0033-2909.129.6.946. [DOI] [PubMed] [Google Scholar]