Abstract
Objective
Mind-body complementary and alternative medicine (CAM) modalities (e.g., relaxation or meditation) for symptom management have not been well studied in adolescents with inflammatory bowel disease (IBD). The purposes of this study were to: 1) determine the prevalence of 5 types of mind-body CAM use, and consideration of use for symptom management; 2) assess characteristics associated with regular mind-body CAM use; and 3) examine whether regular and/or considered mind-body CAM use are associated with health-related quality of life (HRQOL).
Methodology
Sixty-seven adolescents with IBD ages 12-19 recruited from a children’s hospital completed a questionnaire on CAM use and the Pediatric Quality of Life Inventory. Logistic regression models were estimated for regular and considered CAM use.
Results
Participants mean (SD) age was 15.5 (2.1) years; 37 (55%) were female; 53 (79%) were white; and 20 (30%) had moderate disease severity. Adolescents used prayer (62%), relaxation (40%), and imagery (21%) once/day to once/week for symptom management. In multivariable analyses, females were more likely to use relaxation (OR=4.38, 95% CI= 1.25-15.29, c statistic=.73). Younger adolescents were more likely to regularly use (OR=.63, 95% CI=.42-.95, c statistic=.72) or consider using (OR=.77, 95% CI=.59-1.00, c statistic=.64) meditation. Adolescents with more severe disease (OR=4.17, 95% CI=1.07-16.29, c statistic=.83) were more willing to consider using relaxation in the future. Adolescents with worse HRQOL were more willing to consider using prayer and meditation for future symptom management (P<.05).
Conclusions
Many adolescents with IBD either currently use or would consider using mind-body CAM for symptom management.
Keywords: complementary and alternative medicine, quality of life, adolescents, inflammatory bowel disease
Introduction
Inflammatory bowel disease (IBD), which comprises ulcerative colitis, Crohn’s disease and indeterminate colitis, is characterized by a chronic and relapsing inflammation of the gastrointestinal (GI) tract. Medical and psychosocial problems experienced by adolescents with IBD have the potential to adversely affect their health-related quality of life (HRQOL). Adolescents with IBD face not only the possibility of delayed growth and puberty and undergoing multiple painful procedures and treatments, but when compared with healthy peers, are also at greater risk of behavioral/emotional difficulties, including depression/anxiety, poorer social functioning, and poorer self-esteem.1-4
Conventional treatment for IBD primarily focuses on alleviating physical GI symptoms often via medications. For many patients, medications are ineffective or have unwanted side effects, prompting them to seek about complementary and alternative medicine (CAM). CAM has been defined as a “group of diverse medical and health care systems, practices, and products that are not presently considered to be part of conventional medicine.”5 The National Center for Complementary and Alternative Medicine groups CAM practices into 5 domains: 1) whole medical systems (e.g., acupuncture), 2) mind-body medicine (e.g., relaxation or hypnosis), 3) biologically-based practices (e.g., vitamins and herbs), 4) manipulative and body-based practices (e.g., massage therapy), and 5) energy medicine (e.g., reiki).5 Interest in mind-body complementary alternative medicine (CAM) modalities for adjunctive symptom management in adults with GI disorders;6-9 however, less is known about the use of such modalities in pediatric GI populations.10-13
Whereas most previous studies of CAM use in GI disorders have focused on the role of biologically-based practices,10, 11, 14 mind-body modalities hold particular promise and are worthy of further investigation for several reasons. First, the complex relationships among the brain, the body, and behavior, particularly among patients with GI conditions, are increasingly being recognized by healthcare providers as important when considering modes of treatment.8, 9 For example, affective disorders co-occur in patients with GI conditions and psychological factors such as stress can exacerbate physical symptoms in GI conditions.8, 9 Second, mind-body modalities are generally inexpensive and available - making them particularly attractive to adolescents.
Studies on CAM use in pediatric IBD have found that 41-51% of children and young adults (ages 4-23 years) with IBD have used CAM in addition to conventional therapies.11, 12, 15 The most commonly used CAM therapies in these samples are similar to those used by adults, and include spiritual interventions (25%), probiotics (22-24%), megavitamins (12-19%), dietary supplements (17-36%), herbal medicines (14%), and fish oil capsules (16%).10-12, 15 Regarding mind-body modalities, in a multi-site sample of 208 children/adolescents with IBD (ages 4-23 years), 10% had used prayer, 5% hypnotherapy, and 2% biofeedback.11 In 335 patients with IBD ages 6-16 years, 4% reported using relaxation and 1% used yoga as an adjunct therapy.12 Parent-reported reasons for CAM use by their child with IBD included: side-effects from traditional medications, ineffectiveness of traditional medications, and hope of a cure.10, 11 Still, few studies have focused specifically on current or intended use of mind-body CAM modalities in adolescents with IBD and none examined CAM use and its associations with HRQOL. In addition, while the data on characteristics associated with CAM use in children and adolescent with IBD is mixed and scant,10, 11 in adults with IBD, poorer HRQOL and being female have been associated with using CAM more frequently.12, 16
This study aimed to: 1) determine the prevalence of 5 types of mind-body CAM use, and consideration of their use, for symptom management in adolescents with IBD; 2) assess demographic and clinical characteristics associated with mind-body CAM use and consideration of use; and 3) examine whether mind-body CAM use and consideration of use is associated with HRQOL. Based on previous studies,12,16 we hypothesized that higher rates of using CAM for symptom management would be associated with poorer HRQOL, female sex, and older age.
Methods
Participants
A convenience sample of 67 adolescents with IBD ages 12 to 19 years were recruited from Cincinnati Children’s Hospital Medical Center and University Hospital in Cincinnati, Ohio at the time of their clinic visit, by telephone, or via flyers. This study was part of a larger project examining health values and health utilities in adolescents with and without a chronic illness.17, 18 Informed consent and assent were obtained from all participants and their parents/guardians. A trained research assistant met with adolescents after clinic appointments or at pre-arranged times between October 2005 and April 2007 to administer the questionnaires. All participants were able to complete questionnaires independently; however, research assistants were available to answer any potential questions. The study was approved by the institutional review boards of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center.
Measures
Demographic/Clinical Variables
We collected data regarding age, sex, race/ethnicity, parental education level, and religious affiliation. A physician (M.S.Y.) performed chart reviews to assess type of IBD (ulcerative colitis, Crohn’s disease, or indeterminate) and disease severity (severe, moderate, mild, inactive) according to the modified clinical score developed by Lloyd-Still and Green for IBD in children.19, 20
Dependent Variables
HRQOL
Patients completed the Pediatric Quality of Life Inventory (PedsQL), 21 a widely-used HRQOL instrument developed and validated for the quality of life concerns of children and adolescents, ages 2-18 years, with or without chronic illness. 21 The PedsQL™ version 4.0 Generic Core Scales are designed to enable comparisons across patients with chronic conditions and healthy populations.21 The adolescent version of the PedsQL takes approximately 4 minutes to complete and consists of 23 core items that assess 4 dimensions: physical functioning, emotional functioning, social functioning, and school functioning. Each subscale is scored from 0 - 100; higher scores indicate better functional status.
Regular Mind-Body CAM Use and Consideration of CAM Use for Symptom Management
We developed and pilot-tested items addressing adolescents’ use of 5 mind-body CAM modalities - prayer, guided imagery, relaxation, meditation, and yoga. Each modality was defined in writing. The questions read: “How often do you use [X modality] for symptom management?” Responses were recorded on a 5-point Likert scale ranging from 1-“I never used this in the last month” to 5-“I used this about one time per day or more in the past month.” We also assessed consideration of CAM use by asking, “Would you consider using [X modality] for symptom management [yes or no]?” Of note, the 2 CAM questions were not mutually exclusive; therefore, a participant reporting that he/she would be willing to consider using a CAM modality in the future could also report that he/she is a “regular user of CAM.”
Statistical Analyses
Frequencies, means, and distributions of study variables were examined. Internal consistency for the PedsQL subscales was assessed by calculating Cronbach’s alpha statistics. There was only one adolescent who reported an outlying severe symptomatology, and only 2 who had an indeterminate/other form of IBD; we excluded those participants’ data from analyses examining differences by severity level or disease type. Skewness and kurtosis of continuous variables were examined to assess normality assumptions. Given the skewed distribution of the ordinal CAM variables, the Regular CAM Use variable was dichotomized as high vs. low usage for all subsequent analyses (high usage = used once a week, a few times a week, or once per day or more; low usage = never used or used once). Bivariate correlations, chi-square analyses, and logistic regression analyses were used to examine relationships among study variables. Variables statistically significant in bivariate analyses at the p<.10 level were entered into multivariable logistic regression models. Multivariable models were run for those outcome variables with more than one significant predictor at the bivariate level, resulting in 2 final multivariable models (for relaxation and consider relaxation). A p-value ≤ 0.05 was used to indicate statistical significance. Analyses were performed using SPSS, version 16.0.1.22
Results
Participants
The mean (SD) age of the 67 participants was 15.5 years (2.1); 37 (55%) were female; 53 (79%) were white; 52 (78%) had Crohn’s Disease; and 26 (39%) were classified as having mild IBD disease severity (Table 1). The mean (SD) time since IBD diagnosis was 3.1 (2.5) years.
Table 1.
Characteristics of Study Population
| Age, years, Mean (SD) | 15.5 (2.1) |
|---|---|
| Sex | |
| Female, N(%) | 37 (55%) |
| Male, N(%) | 30 (45%) |
| Ethnicity | |
| White, N(%) | 53 (79%) |
| Non-White, N(%) | 14 (21%) |
| Highest Level of Parental Education | |
| Graduated High School or GED, N(%) | 5 (8%) |
| Some College, N(%) | 10 (15%) |
| Graduated from College, N(%) | 25 (37%) |
| Graduated with Advanced Degree, N(%) | 18 (27%) |
| Not Sure, N(%) | 9 (13%) |
| Disease Type | |
| Crohn’s Disease, N(%) | 52 (78%) |
| Ulcerative Colitis, N(%) | 13 (19%) |
| Indeterminate/Other, N(%) | 2 (3%) |
| Disease Severity* | |
| Inactive | 20 (30%) |
| Mild | 26 (39%) |
| Moderate | 20 (30%) |
| Severe | 1 (1%) |
| Time Since Diagnosis,† years, Mean (Range) | 3 (1 - 13) |
SD: standard deviation
Assessed according to the method described by Lloyd-Still and Green.17
Adolescent self-report
Regular CAM Use and Consideration of CAM Use
Adolescents with IBD reported using prayer (n = 37 [62%]), relaxation (n = 24 [40%]) and imagery (n=12 [21%]) most commonly for symptom management in the past month (see Figure 1). Prayer (n = 48 [81%]), relaxation (n = 50 [85%]), and imagery (n = 33 [55%]) were also the most common mind-body CAM modalities that adolescents would consider using in the future for symptom management.
Figure 1.
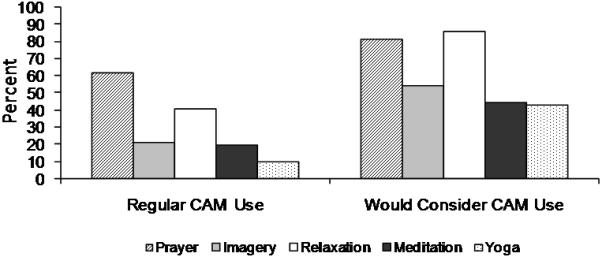
Percent of adolescents who have used or would consider using complementary and alternative medicine modulaties for symptom management. Regular use was defined as used more than once.
CAM: complementary and alternative medicine.
Characteristics Associated with Regular CAM Use and Consideration of CAM Use
Males and females reported similar rates of regular use of imagery, prayer, and meditation, and similar rates of consideration of using meditation, imagery, yoga, and prayer (P = NS; Table 2). There were no significant differences in rates of regularly using or considering using prayer, meditation, or yoga by severity of disease (P = NS). There were also no differences in any type of regular CAM use or consideration of CAM use by type of IBD (ulcerative colitis vs. Crohn’s disease; P = NS) or by race (white vs. non-white; P = NS). Age was not significantly associated with regular use of any of the CAM modalities or consideration of CAM modalities with the exception of meditation: younger patients were more likely to use/consider using meditation than were older patients (Table 2).
Table 2.
Bivariate Relationships of Regular CAM Use and Consideration of CAM Use
| Variable | OR (χ2) | 95% CI |
|---|---|---|
| Regular Use | ||
| Imagery | ||
| More severe IBD | 2.13* | .87 - 5.2 |
| Relaxation | ||
| Female | 5.66‡ | 1.71 - 18.71 |
| More severe IBD | 2.24† | 1.07 - 4.67 |
| Meditation | ||
| Age | .63† | .42 - .95 |
| Yoga | ||
| Female | (9.79) ‡ | - |
| Consideration of Use | ||
| Imagery | ||
| More severe IBD | 2.07† | 1.01 - 4.26 |
| Relaxation | ||
| Female | 11.20† | 1.30 - 96.79 |
| More severe IBD | 6.44‡ | 1.69 - 24.48 |
| Meditation | ||
| Age | .77† | .59 - 1.00 |
p < .10
p < .05
p < .01.
CAM: complementary and alternative medicine; OR: odds ratio; CI: confidence interval; IBD: inflammatory bowel disease
In multivariable analyses, females were more likely to regularly use relaxation (OR = 4.38, 95% CI = 1.25 - 15.29, c statistic = .73) as compared with males. Adolescents with more severe disease were more willing to consider using relaxation in the future (OR = 4.17, 95% CI = 1.07 - 16.29, c statistic = .83) as compared with patients with less severe disease.
Associations Between CAM Use and HRQOL
Adolescents who used yoga for symptom management had poorer school functioning, (mean [SD] = 60.8 [9.2]) compared with those who did not use yoga (mean [SD] = 71.3 [19.6], P < 0.05). Regular use of the other 4 CAM modalities was not associated with HRQOL.
The mean [SD] physical functioning score (74.1 [19.9]) was lower for patients willing to consider using prayer than for those not willing to consider using prayer (85.8 [13.7], P < 0.05). The mean [SD] social functioning score (78.7 [16.2]) was lower for patients willing to consider using meditation in the future (90.0 [12.6], P < 0.01).
Discussion
Interest in mind-body modalities for symptom management in GI conditions has been growing both in the public and healthcare arenas.6, 7, 9, 12, 23 Our study found that adolescents with IBD regularly used and would consider using prayer, relaxation and imagery for symptom management more commonly than previously reported in pediatric IBD samples.10, 12 Each of those mind-body CAM modalities is relatively simple to learn and can be easily integrated into daily life (e.g., an adolescent could use deep breathing for relaxation while sitting in class). Mindfulness-based mind-body programs such as stress reduction and biofeedback, which typically involve relaxation training and imagery, have been shown to be effective in reducing pain, improving HRQOL, and improving symptoms in other chronically ill populations.24, 25 In the GI literature, the evidence for effectiveness of mind-body CAM use in alleviating GI symptoms is best for hypnotherapy and cognitive behavioral therapy, primarily in adults with irritable bowel syndrome.6, 26 Rigorous controlled studies are sorely needed to examine the effectiveness of mind-body modalities for alleviating GI symptoms or improving HRQOL in children and adolescents with IBD.
Based on our findings, relaxation programs targeting girls and patients with more severe IBD may attract the greatest amount of interest. Previous studies have found that females and older adolescents use CAM more regularly.27, 28 In our study, it was actually younger adolescents who were more interested in meditating than were older adolescents - a consideration for developing future programs/interventions. Interestingly, while fewer than 20% of adolescents actually reported using meditation or yoga on a regular basis for symptom management, over 40% were willing to consider using those modalities in the future. A recent randomized controlled trial of yoga therapy for 25 adolescents with irritable bowel syndrome found that adolescents doing yoga had less functional disability and less anxiety than the control group.29 Mind-body programs (e.g., relaxation or yoga) aimed at reducing GI symptoms and improving HRQOL should be assessed for feasibility and effectiveness in adolescents with IBD.
Contrary to our study hypotheses, there were virtually no significant relationships between adolescents regularly using CAM and their self-reported HRQOL. The one exception was that those adolescents who used yoga had poorer school functioning. In contrast, Markowitz and colleagues found that CAM use was inversely associated with quality of life in patients with IBD ages 6 to 16 years.12 We speculate that adolescents currently using CAM may have had poorer HRQOL at baseline in hopes that their use of CAM would mitigate some of the effects of IBD on their HRQOL. In potential support of this hypothesis, we found that adolescents with poorer HRQOL were more willing to consider using mind-body CAM modalities (specifically, prayer and meditation) in the future. Poor HRQOL or dissatisfaction with traditional treatment is often cited as a reason for considering CAM use.11, 12 Such information should be used when developing IBD symptom reduction interventions for adolescents.
Future studies of adolescents with IBD should evaluate whether engaging in a brief program of learning a mind-body modality is feasible and effective in improving symptoms and HRQOL. One of the key challenges in conducting mind-body CAM research is that many interventions use multiple modalities (e.g., biofeedback often includes deep breathing, relaxation training, and imagery), making it difficult to distill the critical ingredient or mediating mechanism driving the success of the intervention. Still, given the large number of adolescents with IBD that not only use but would consider using mind-body CAM modalities, the inherent brain-body connection, and the low-cost and mobile nature of these modalities, future research in this area is critical.
Our study had several limitations. First, it was cross-sectional, precluding assessing the temporal nature of relationships among our study variables or drawing causal inferences. In addition, because we only assessed adolescents’ practices and attitudes regarding CAM use, we are not able to draw any conclusions about whether parental CAM use, often a predictor of child CAM use,11 was related to CAM usage in these adolescents. Finally, our sample size was small, represented a single IBD clinic in the midwest, and was mostly from economically advantaged families (as represented by parental education level). Therefore, it may not be generalizable to other areas of the country where the use of such mind-body modalities may be more or less common.
Despite these limitations, important conclusions can be drawn. Mind-body CAM use for symptom management in adolescents with IBD is prevalent, and regardless of whether they have used these modalities before, many adolescents would consider using these modalities in the future. Girls, patients with more severe disease, younger adolescents, and patients with worse HRQOL may be most open to trying CAM. Because these modalities are fairly simple, easy to teach, inexpensive, and can be practiced alone, they should be considered as adjunct approaches to symptom management. A mental health practitioner could routinely teach these modalities via a psychoeducational model of self care. This would be an initial short term investment for clinics that could provide long-term benefits to their patient population. A better understanding of the prevalence and correlates of mind-body CAM use provides the groundwork for conducting randomized controlled trials to determine the the effect of mind-body CAM use on health outcomes in adolescents with IBD.
Acknowledgments
Funding: National Institute for Child Health and Human Development #K23HD052639 (Cotton, PI); National Institute for Child Health and Human Development #K23HD044556 (Yi, PI); National Center for Complementary and Alternative Medicine #K24AT001676 (Tsevat, PI)
References
- 1.De Boer M, Grootenhuis M, Derkx B, Last B. Health-related quality of life and psychosocial functioning of adolescents with inflammatory bowel disease. Inflamm Bowel Dis. 2005 Apr;11(4):400–406. doi: 10.1097/01.mib.0000164024.10848.0a. [DOI] [PubMed] [Google Scholar]
- 2.Mackner LM, Sisson DP, Crandall WV. Review: psychosocial issues in pediatric inflammatory bowel disease. J Pediatr Psychol. 2004 Jun;29(4):243–257. doi: 10.1093/jpepsy/jsh027. [DOI] [PubMed] [Google Scholar]
- 3.Petrak F, Hardt J, Clement T, Borner N, Egle UT, Hoffmann SO. Impaired health-related quality of life in inflammatory bowel diseases: psychosocial impact and coping styles in a national German sample. Scand J Gastroenterol. 2001 Apr;36(4):375–382. doi: 10.1080/003655201300051171. [DOI] [PubMed] [Google Scholar]
- 4.van der Zaag-Loonen HJ, Grootenhuis MA, Last BF, Derkx HH. Coping strategies and quality of life of adolescents with inflammatory bowel disease. Qual Life Res. 2004 Jun;13(5):1011–1019. doi: 10.1023/B:QURE.0000025598.89003.0c. [DOI] [PubMed] [Google Scholar]
- 5.NCCAM [Accessed October 3, 2008]; What is CAM? n.d.; http://nccam.nih.gov/health/whatiscam/#1.
- 6.Gerson CD, Gerson MJ. A collaborative health care model for the treatment of irritable bowel syndrome. Clin Gastroenterol Hepatol. 2003 Nov;1(6):446–452. doi: 10.1016/s1542-3565(03)00218-0. [DOI] [PubMed] [Google Scholar]
- 7.Kearney DJ, Brown-Chang J. Complementary and alternative medicine for IBS in adults: mind-body interventions. Nat Clin Pract Gastroenterol Hepatol. 2008 Nov;5(11):624–636. doi: 10.1038/ncpgasthep1257. [DOI] [PubMed] [Google Scholar]
- 8.Naliboff BD, Frese MP, Rapgay L. Mind/Body psychological treatments for irritable bowel syndrome. Evid Based Complement Alternat Med. 2008 Mar;5(1):41–50. doi: 10.1093/ecam/nem046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anton PA. Stress and mind-body impact on the course of inflammatory bowel disease. Seminars in Gastrointestinal Disease. 1999;10(1):14–19. [PubMed] [Google Scholar]
- 10.Day AS, Whitten KE, Bohane TD. Use of complementary and alternative medicines by children and adolescents with inflammatory bowel disease. J Paediatr Child Health. 2004 Dec;40(12):681–684. doi: 10.1111/j.1440-1754.2004.00510.x. [DOI] [PubMed] [Google Scholar]
- 11.Heuschkel R, Afzal N, Wuerth A, et al. Complementary medicine use in children and young adults with inflammatory bowel disease. Am J Gastroenterol. 2002 Feb;97(2):382–388. doi: 10.1111/j.1572-0241.2002.05474.x. [DOI] [PubMed] [Google Scholar]
- 12.Markowitz JE, Mamula P, delRosario JF, et al. Patterns of complementary and alternative medicine use in a population of pediatric patients with inflammatory bowel disease. Inflamm Bowel Dis. 2004 Sep;10(5):599–605. doi: 10.1097/00054725-200409000-00015. [DOI] [PubMed] [Google Scholar]
- 13.Otley AR, Verhoef MJ, Best A. Prevalence and determinants of use of complementary and alternative medicine in a Canadian pediatric inflammatory bowel disease population. Gastroenterol. 2001;120:A213. al. e. [Google Scholar]
- 14.Hilsden RJ, Scott CM, Verhoef MJ. Complementary medicine use by patients with inflammatory bowel disease. Am J Gastroenterol. 1998 May;93(5):697–701. doi: 10.1111/j.1572-0241.1998.208_a.x. [DOI] [PubMed] [Google Scholar]
- 15.Wong AP, Clark AL, Garnett EA, et al. Use of complementary medicine in pediatric patients with Inflammatory Bowel Disease: Results from a multicenter study. J Pediatr Gastroenterol Nutr. 2008;48:55–60. doi: 10.1097/MPG.0b013e318169330f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bensoussan M, Jovenin N, Garcia B, et al. Complementary and alternative medicine use by patients with inflammatory bowel disease: results from a postal survey. Gastroenterol Clin Biol. 2006 Jan;30(1):14–23. doi: 10.1016/s0399-8320(06)73072-x. [DOI] [PubMed] [Google Scholar]
- 17.Cotton S, Kudel I, Roberts YH, et al. Spiritual well-being and mental health outcomes in adolescents with or without inflammatory bowel disease. J Adolesc Health. 2009;44(5):485–492. doi: 10.1016/j.jadohealth.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yi MSBM, Sherman SN, et al. Health values in adolescents with or without inflammatory bowel disease. J Pediatr. 2009;4(154):527–534. doi: 10.1016/j.jpeds.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bunn SK, Bisset WM, Main MJ, Golden BE. Fecal calprotectin as a measure of disease activity in childhood inflammatory bowel disease. J Pediatr Gastroenterol Nutr. 2001 Feb;32(2):171–177. doi: 10.1097/00005176-200102000-00015. [DOI] [PubMed] [Google Scholar]
- 20.Lloyd-Still JD, Green OC. A clinical scoring system for chronic inflammatory bowel disease in children. Dig Dis Sci. 1979 Aug;24(8):620–624. doi: 10.1007/BF01333706. [DOI] [PubMed] [Google Scholar]
- 21.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001 Aug;39(8):800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 22.SPSS . SPSS Base 15.0.1 User’s Guide. Prentice Hall; Chicago, IL: 2006. [Google Scholar]
- 23.Mayer EA, Raeen H, Bolus R, Naliboff B, Kuo W-C, Mayer M. Psychoeducational intervention in IBS improves symptoms and health-related quality of life: A controlled study (abstr) Gastroenterology. 2003;124(A398) [Google Scholar]
- 24.Kieviet-Stijnen A, Visser A, Garssen B, Hudig W. Mindfulness-based stress reduction training for oncology patients: patients’ appraisal and changes in well-being. Patient Educ Couns. 2008 Sep;72(3):436–442. doi: 10.1016/j.pec.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 25.Loening-Baucke V. Biofeedback treatment for chronic constipation and encopresis in childhood: long-term outcome. Pediatrics. 1995 Jul;96(1 Pt 1):105–110. [PubMed] [Google Scholar]
- 26.Webb AN, Kukuruzovic RH, Catto-Smith AG, Sawyer SM. Hypnotherapy for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2007;(4) doi: 10.1002/14651858.CD005110.pub2. CD005110. [DOI] [PubMed] [Google Scholar]
- 27.Ottolini MC, Hamburger EK, Loprieato JO, et al. Complementary and alternative medicine use among children in the Washington, DC area. Ambul Pediatr. 2001 Mar-Apr;1(2):122–125. doi: 10.1367/1539-4409(2001)001<0122:caamua>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 28.Reznik M, Ozuah PO, Franco K, Cohen R, Motlow F. Use of complementary therapy by adolescents with asthma. Arch Pediatr Adolesc Med. 2002 Oct;156(10):1042–1044. doi: 10.1001/archpedi.156.10.1042. [DOI] [PubMed] [Google Scholar]
- 29.Kuttner L, Chambers CT, Hardial J, Israel DM, Jacobson K, Evans K. A randomized trial of yoga for adolescents with irritable bowel syndrome. Pain Res Manag. 2006 Winter;11(4):217–223. doi: 10.1155/2006/731628. [DOI] [PMC free article] [PubMed] [Google Scholar]


