Abstract
Francisella tularensis subspecies tularensis is a highly virulent facultative intracellular pathogen of humans and a potential biological weapon. A live vaccine strain, F. tularensis LVS, was developed more than 50 years ago by pragmatic attenuation of a strain of the less virulent holarctica subspecies. LVS was demonstrated to be highly effective in human volunteers who were exposed to intradermal challenge with fully virulent subsp. tularensis, but was less effective against aerosol exposure. LVS faces regulatory hurdles that to date have prevented its licensure for general use. Therefore, a better defined and more effective vaccine is being sought. To this end we have created gene deletion mutants in the virulent subsp. tularensis strain and tested them for their ability to elicit a protective immune response against systemic or aerosol challenge with the highly virulent wild-type subsp. tularensis strain, SCHU S4. Both oral and Intradermal (ID) primary vaccination routes were assessed in BALB/c and C3H/HeN mice as was oral boosting. One SCHU S4 mutant missing the heat shock gene, clpB, was significantly more attenuated than LVS whereas a double deletion mutant missing genes FTT0918 and capB was as attenuated as LVS. In general mice immunized with SCHU S4ΔclpB were significantly better protected against aerosol challenge than mice immunized with LVS. A single ID immunization of BALB/c mice with SCHU S4ΔclpB was at least as effective as any other regimen examined. Mice immunized with SCHU S4Δ0918ΔcapB were generally protected to a similar degree as mice immunized with LVS. A preliminary examination of immune responses to vaccination with LVS, SCHU S4ΔclpB, or SCHU S4Δ0918ΔcapB provided no obvious correlate to their relative efficacies.
1. Introduction
The tularensis and holarctica subspecies of the facultative intracellular bacterial pathogen Francisella tularensis cause tularemia, a severe infectious disease of humans and many other mammals. In particular, human typhoidal tularemia, thought to be caused by inhalation of the more virulent tularensis subspecies had an historical mortality rate of 30% or more when left untreated [1]. This led to the development of of subsp. tularensis as a biological weapon during the first half of the 20th century [2]. There was a concomitant search for effective vaccines against it. In human volunteers, whole killed bacteria and extracts thereof significantly alleviated infection initiated via the skin, but not via the lungs [3-6]. In contrast, a pragmatically-attenuated holarctica strain, F. tularensis LVS, fully protected volunteers against systemic challenge and partially protected them against aerosol challenge. LVS remains the only anti-tularemia vaccine to have been manufactured on a commercial scale in the USA, but currently is only available to at risk laboratory personnel via the Special Immunization Program of the US Department of Defense. In part, this is due to the fact that the basis for its attenuation and its mechanism of action remain poorly understood. In recent years, there has been increased concern about the potential abuse of F. tularensis by terrorists. This has led to renewed efforts to produce licensable vaccines.
The natural distribution of F. tularensis subsp. tularensis is confined to North America, and clinical cases of tularemia caused by its inhalation are extremely rare making it impossible to assess vaccine efficacy via clinical trials. The United States Food and Drug Administration devised the so called Animal Rule for such eventualities (http://www.fda.gov/cber/rules/humeffic.htm). The Animal Rule allows for the exclusive use of animal models to demonstrate vaccine efficacy for rare diseases provided that the mechanism of action of the vaccine in animals predicts its efficacy in humans. With the aforementioned considerations in mind, for the past several years we have been trying to produce novel defined attenuated live vaccines by targeted deletion of virulence genes from the prototypical subsp. tularensis strain, SCHU S4, using a murine model to screen for attenuation and efficacy. Mice have been the mainstay of F. tularensis infections and immunity research for the past 25 years and have been the sole model host used to evaluate efficacy of vaccines against F. tularensis subsp. tularensis during that time.
Previously, we and others have shown that systemic immunization of some mouse strains, e.g. BALB/c mice, with LVS provides excellent long-term protection against systemic, but not aerosol challenge with virulent subsp. tularensis strains of the pathogen [7-9]. This inability to replicate the long-lasting clinical efficacy of transdermally-administered LVS against pulmonary challenge with subsp. tularensis using a well-established small animal model of tularemia could seriously hamper the development of any novel anti-Francisella vaccines against inhalation-initiated infection under the Animal Rule. In particular, none of the other small animal models of tularemia developed during the past 50 years has shown any obvious advantage over mice [10]. Historically, certain non-human primate models of tularemia were reported to better mimic the protection against pulmonary challenge elicited in humans by LVS [4, 11], and might ultimately need to be further developed to satisfy the Animal Rule. However, for ethical and economic reasons, such models are impractical for early stage vaccine discovery.
In the case of LVS, protection against pulmonary tularemia can be slightly improved by using C3H/HeN mice in place of BALB/c mice [8], or by pulmonary or oral vaccination of the latter with LVS [9,12,13]. Additionally, we have shown that a spontaneously-attenuated strain of SCHU S4 or a targeted deletion mutant missing the gene FTT0918, administered intradermally (ID) can provide partial protection to BALB/c mice against aerosol challenge with fully virulent subsp. tularensis [14]. However, these vaccine strains were either as undefined as LVS or retained an unacceptable level of residual virulence to be considered clinically useful. To overcome these problems, we have continued to generate targeted deletion mutants of SCHU S4, and to screen them for attenuation via the ID route. For the current study, two deletion mutant strains, SCHU S4ΔFTT0918ΔcapB and SCHU S4ΔclpB, attenuated to a similar level as LVS by the ID route were generated. Herein, we examine whether they can be shown to elicit better protection than LVS in BALB/c or C3H/HeN mice against aerosol challenge with SCHU S4 using clinically-relevant routes of vaccination, to thereby allow for their further development in accordance with the Animal Rule. The targets were chosen because they were known to be important virulence determinants in F. tularensis. We have previously demonstrated that FTT0918 is a major virulence factor for F. tularensis tularensis, but SCHU S4 Δ0918 was 100-fold less attenuated than LVS when administered to mice via the ID route. [14]. The ClpB chaperone fulfills important cellular functions by solubilization and refolding of aggregated proteins by virtue of its protease function and is a virulence determinant in other facultative intracellular bacteria such as Salmonella enterica serovar Typhimurium [15] and Listeria monocytogenes [16]. Several publications have also identified its important contribution in F. tularensis LVS [17,18] or F. novicida [19-21] intracellular growth and virulence. The capB gene has also been implicated in LVS or F. novicida virulence [17,21]. It shows a 38% amino acid identity with the capsule biosynthetic gene capB of Bacillus anthracis [22]. However, there is no direct evidence that it contributes to capsule formation in F. tularensis.
2. Materials and Methods
2.1 Mice
Female BALB/c and C3H/HeN mice were purchased from Charles Rivers Laboratories (St. Constant, Quebec) and entered experiments at 6-8-weeks of age. Mice were maintained and used in accordance with the recommendations of the Canadian Council on Animal Care Guide to the Care and Use of Experimental Animals.
2.2 Bacterial strains
The ATCC 29684 isolate of LVS was used for comparison with SCHU S4-based vaccines. Spontaneously attenuated SCHU AV and deletion mutant SCHU S4ΔiglC have been described by us previously [14]. The former elicits significant protection against ID or aerosol challenge with F. tularensis subsp tularensis. In contrast, SCHU S4ΔiglC lacks the ability to disseminate from the skin inoculation site and fails to elicit protection [14]. They were included in the current study as positive and negative controls respectively. In-frame deletions of the clpB and capB genes were constructed by allelic exchange using a previously described method for ΔiglC [23] based on integration and excision of a suicide plasmid carrying upstream and downstream sequences of the target gene. The upstream and downstream regions of each of the genes were amplified by PCR. The PCR fragments for each gene contained complementary sequences in the 3′ end of the upstream fragment and the 5′ end of the downstream fragment which were annealed during a second round of PCR. After restriction enzyme digestion and purification, the PCR fragments were cloned into the suicide vector pDMK2, which was later transformed into Escherichia coli S17-1. Conjugation to F. tularensis SCHU S4 was carried out as described previously [23]. Conjugants were selected on media containing 10 μg/ml kanamycin and 50 μg/ml of polymyxin B and confirmed by PCR. To select for a second recombination event, conjugants were plated on medium containing 5% sucrose and the deletion of the genes identified by PCR and the exact location verified by sequencing. The ΔcapB mutation was introduced into the ΔFTT0918 strain to generate a double mutant [14]. The strategy led to the deletion of 1073 out of the 1218 bp of capB and 2463 out of the 2580 bp for clpB.
For the present study, stock cultures of all strains were prepared by growing them as confluent lawns on cystine heart agar supplemented with 1% (w/v) hemoglobin (CHAH). Bacteria were harvested after 48 h incubation at 37°C into freezing medium consisting of modified Mueller Hinton broth containing 10% w/v sucrose. Stocks were aliquotted in volumes of 1 ml and stored at −80°C at a concentration of 1010-1011 CFU / ml.
2.3 Immunization and challenge
We have previously shown that LVS has an oral LD50>108 CFU for BALB/c mice [13], and at this dose it elicits protection against systemic and aerosol challenge with fully virulent F. tularensis subsp. tularensis. The ID LD50 is also >108 CFU, and 105 CFU of LVS administered ID completely protects against systemic challenge, but only prolongs survival by 1-2 days following aerosol challenge, with subsp. tularensis [7,8,12,14]. Prior studies from us also showed that LVS elicits a statistically insignificant improvement in protection in C3H/HeN versus BALB/c mice [12] and that SCHU AV administered ID to BALB/c mice provides an insignificant improvement in protection than LVS against aerosol challenge with subsp. tularensis [14]. Based on the aforementioned findings we chose 105 and 108 CFU as the ID and oral immunizing doses for all of the test vaccine strains and BALB/c and C3H/HeN mice as the model hosts for determining their efficacy. For oral immunization, mice were gavaged once with one or other vaccine strain suspended in 0.2 ml saline. ID inocula were injected into a fold of skin in the mid-belly in a volume of 0.05 ml saline. Aerosol challenges were performed using an InTox Products nose-only exposure chamber as previously described [7,8,12,14]. The protocol results in the delivery of ~20 CFU of SCHU S4 to the lower airways of mice. All animal work was performed in a federally-licensed and Select-Agent-approved small animal containment level 3 facility. In the present study, mice were examined daily for signs of infection and whenever feasible were euthanized by CO2 asphyxiation as soon as they displayed signs of irreversible morbidity. For bacteriology, a 1 cm2 piece of skin surrounding the inoculum site, and livers, spleens, and lungs were removed, minced with scissors, and homogenized using aerosol-proof homogenizers. Organ homogenates were diluted in sterile saline and plated on CHAH. To determine the extent of bacteremia, whole blood collected by cardiac puncture at the time of necropsy was diluted 1:10 in sterile water to lyse host blood cells. The lysate was further diluted in saline and plated as above.
2.4. Statistics
Survival curves were compared using the Mantel-Cox log rank test. Differences in bacterial burdens, serum cytokine levels or serum antibody titres were compared by One-way ANOVA with Tukey's post test, using GraphPad Prizm 5 software. In all cases, differences were considered significant at P<0.05.
3. Results
3.1 Safety of live vaccine strains
During initial screening, all BALB/c mice survived ID challenge with 105 CFU of any of the mutant strains employed in the present study whereas at an ID dose of 107 CFU 1/5 mice immunized with SCHU S4 ΔFTT0918ΔcapB died. Thus, all of the test mutants had an estimated ID LD50 of ≥107 CFU for BALB/c mice versus < 10 CFU for wild-type SCHU S4. SCHU S4ΔiglC was included as a negative control for potential non-specific protective effects of vaccination with live attenuated mutants of SCHU S4. In contrast, SCHU AV was included as a positive control. It is a highly attenuated spontaneous mutant of SCHU S4 that retains its ability to elicit robust protection against systemic challenge and partial protection against aerosol challenge with F. tularensis subsp. tularensis [14]. LVS was included as a reference strain. For the present study, mice received ID inocula of 105 CFU. Previously, we showed that LVS, but not SCHU AV or SCHU S4ΔiglC at this dose, elicited obvious necrosis at the site of injection and visible signs of infection (ruffled fur) in BALB/c mice [14]. SCHU S4 ΔFTT0918ΔcapB was similar to LVS in this regard, whereas SCHU S4ΔclpB was similar to SCHU AV (not shown). LVS at an ID dose of 105 CFU killed a few BALB/c (2/15) mice, whereas all C3H/HeN mice survived this inoculum. The opposite result was observed with SCHU AV which killed 2/15 C3H/HeN mice, but none of the BALB/c mice. Both mouse strains survived ID immunization with SCHU S4ΔclpB and SCHU S4 ΔiglC. Surprisingly, SCHU S4 ΔFTT0918ΔcapB was very virulent for C3H/HeN mice compared to BALB/c mice (105 CFU ID killed 14/15 versus 3/15, respectively). In a follow-up experiment, 7/15 C3H/HeN mice died following ID immunization with 103 CFU SCHU S4 ΔFTT0918ΔcapB (not shown). Previously, we had shown that BALB/c mice survived oral immunization with 108 CFU of LVS and subsequently demonstrated some protection against aerosol challenge with F. tularensis subsp. tularensis [13]. Therefore, we chose this as the test dose for oral immunization with all of the mutants in the current study. By this vaccination route, SCHU AV and SCHU S4 ΔiglC were completely avirulent for both BALB/c and C3H/HeN mice. Likewise, LVS and SCHU S4 ΔclpB were completely attenuated for BALB/c mice, but each killed 5/15 C3H/HeN mice. Finally, SCHU S4ΔFTT0918ΔcapB demonstrated some degree of virulence for both BALB/c and C3H/HeN mice at an oral dose of 108 CFU, killing 3/15 and 6/15 mice, respectively.
3.2 Efficacy of ID vaccination against aerosol challenge
Previously, we showed that BALB/c mice immunized ID with LVS or SCHU AV, but not SCHU S4ΔiglC, survived a subsequent ID challenge with 1000 LD50 of fully-virulent F. tularensis subsp. tularensis [7,8,12,14]. In the present study, this was determined to be the case too for SCHU S4ΔclpB and SCHU S4ΔFTT0918ΔcapB; 100% of mice immunized ID with 103 or 105 CFU of either mutant survived a subsequent ID challenge with 1000 CFU SCHU S4. To determine the degree of protection against inhalation tularemia elicited by ID immunization with 105 CFU, mice were challenged 6 weeks post-vaccination with a low dose (~20 CFU) aerosol of SCHU S4. Note that for this experiment we used C3H/HeN mice that survived ID immunization with 103 CFU of the less attenuated SCHU S4 ΔFTT0918ΔcapB administered 5 weeks earlier to allow for contemporaneous challenge with other test groups. The results are shown in Table 1. All (n=6) naïve BALB/c and C3H/HeN mice died on day 5 of challenge. All vaccine candidates elicited significant protection (P≤0.04), against aerosol challenge in BALB/c mice, compared to naïve mice or mice immunized with the negative control strain SCHU S4ΔiglC. BALB/c mice immunized with SCHU S4ΔclpB showed the best median survival (>28 days) and this was significantly greater than the protection elicited by LVS (P=0.038), but not than that elicited by SCHU AV or SCHU S4 ΔFTT0918ΔcapB. In C3H/HeN mice, LVS, SCHU AV, and SCHU S4ΔclpB but not SCHU S4Δ0918ΔcapB, elicited a statistically significant increase in survival compared to naïve mice or mice immunized with SCHU S4ΔiglC (p≤0.03). As we, and others, have previously shown [8,12, 24], LVS produced a statistically insignificant, improvement in median survival in C3H/HeN versus BALB/c mice challenged by aerosol with SCHU S4. In contrast, all of the SCHU S4-based vaccines elicited a statistically insignificant increase in median survival in BALB/c versus C3H/HeN mice. This result is consistent with our earlier findings with SCHU AV and SCHU S4Δ0918 versus LVS [14].
Table1.
Survival of ID immunized mice following aerosol challenge with SCHU S4.
| Mouse strain | vaccine | Time to death of individual mice (days) |
Median time to death (days) |
|---|---|---|---|
| BALB/c | none | 5,5,5,5,5,5 | 5 |
| BALB/c | LVS | 7,7,8,9,12 | 81 |
| BALB/c | SCHU AV | 6,9,10,10,12 | 101 |
| BALB/c | SCHU S4Δ0918ΔcapB | 5,7,8,>28,>28 | 81 |
| BALB/c | SCHU S4ΔclpB | 8,11,>28,>28,>28 | >281,2 |
| BALB/c | SCHU S4ΔiglC | 5,5,6,6,6 | 6 |
| C3H/HeN | none | 5,5,5,5,5,5 | 5 |
| C3H/HeN | LVS | 9,9,11,12,14 | 111 |
| C3H/HeN | SCHU AV | 6,6,6,7,>28 | 61 |
| C3H/HeN | SCHU S4Δ0918ΔcapB3 | 5,5,5,9,9 | 5 |
| C3H/HeN | SCHU S4ΔclpB | 5,8,10,11,14 | 101 |
| C3H/HeN | SCHU S4ΔiglC | 5,5,5,6,6 | 5 |
Mice were immunized ID with 105 CFU of one or other vaccine and challenged 6 weeks later by aerosol with 20 CFU of SCHU S4.
significantly greater survival (P≤0.03) by Mantel-Cox log rank test) than for naive mice or mice immunized with SCHU ΔiglC.
significantly greater survival than mice immunized with LVS (P = 0.04).
These mice were immunized with 103 CFU.
3.3 Efficacy of oral vaccination against aerosol challenge
Previously, we showed that most BALB/c mice immunized once orally with 108 CFU of LVS were fully protected against low dose aerosol challenge with F. tularensis subsp. tularensis, but this immunity waned substantially after 4 weeks [13]. Others have recently reported similar findings [25]. Therefore, to determine whether any of the other potential vaccine strains in the current study might be superior to LVS in this regard, aerosol challenges were performed 6 weeks post vaccination, when LVS-elicited protection would be expected to have markedly diminished. The results are shown in Table 2. All control mice died on day 5 of challenge, as did all C3H/HeN mice immunized with LVS, SCHU AV, and SCHU S4ΔFTT0918ΔcapB; 2/5 of C3H/HeN mice immunized PO with SCHU S4ΔiglC survived to day 6, but this was not statistically significant. All BALB/c mice immunized with SCHU AV or SCHU S4ΔiglC died on day 5 whereas 2/5 BALB/c mice immunized with either LVS or SCHU S4ΔFTT0918ΔcapB survived to day 7, but this was not statistically significant. In contrast, C3H/HeN and BALB/c mice immunized PO with SCHU S4 ΔclpB survived significantly longer than all other groups of mice (P≤0.025). The different mean survival times between these two mouse strains (12 vs 16 days) was not statistically significant. In the case of LVS and SCHU AV, ID vaccination elicited a statistically significant increase in survival compared to PO vaccination (P≤0.02) in both BALB/c and C3H/HeN mice.
Table 2.
Survival of orally immunized mice following aerosol challenge with SCHU S4.
| Mouse strain | vaccine | Time to death of individual mice (days) |
Median time to death (days) |
|---|---|---|---|
| BALB/c | none | 5,5,5,5,5,5 | 5 |
| BALB/c | LVS | 5,5,5,7,7 | 5 |
| BALB/c | SCHU AV | 5,5,5,5 | 5 |
| BALB/c | SCHU S4 Δ0918ΔcapB | 5,5,5,7,7 | 5 |
| BALB/c | SCHU S4ΔclpB | 9,9,16,>28,>28 | 161 |
| BALB/c | SCHU S4ΔiglC | 5,5,5,5,5 | 5 |
| C3H/HeN | none | 5,5,5,5,5,5 | 5 |
| C3H/HeN | LVS | 4,5,5,5,5 | 5 |
| C3H/HeN | SCHU AV | 5,5,5,5,5 | 5 |
| C3H/HeN | SCHU S4Δ0918ΔcapB | 5,5,5,5 | 5 |
| C3H/HeN | SCHU S4 ΔclpB | 5,9,12,13,16 | 121 |
| C3H/HeN | SCHU S4ΔiglC | 5,5,5,6,6 | 5 |
Mice were immunized per os with 108 CFU of one or other vaccine and challenged 6 weeks later by aerosol with 20 CFU of SCHU S4.
significantly greater survival (P≤0.03) than for naive mice or mice of the same strain immunized with any of the other vaccine strains.
3.4 Effect of oral boosting on vaccine efficacy
Eight weeks after ID or PO vaccination, some mice were re-immunized PO with 108 CFU of the homologous mutant strain. In contrast to primary PO immunization, no mice died following oral boosting. Six weeks post-boosting, mice were exposed to an aerosol of SCHU S4 and their survival was monitored (Tables 3 and 4). BALB/c mice ID primed and orally boosted with LVS, SCHU S4Δ0918ΔcapB, or SCHU S4ΔclpB survived significantly longer than naïve mice or mice primed and boosted with SCHU AV or SCHU S4ΔiglC (P≤0.04). This was also the case for C3H/HeN mice immunized and boosted with SCHU S4ΔclpB (P≤0.003). Additionally, BALB/c and C3H/HeN mice primed and boosted with SCHU S4ΔclpB survived significantly longer than mice primed and boosted with LVS (P= 0.03 and 0.003 respectively). Compared to ID priming alone, BALB/c mice primed and boosted with SCHU AV survived SCHU S4 challenge longer (P=0.023) as did C3H/HeN mice primed and boosted with LVS (P<0.002) or SCHU S4ΔclpB (P=0.049). In all other cases there was no significant difference in survival times. Mice orally immunized and boosted with LVS or SCHU S4ΔclpB survived significantly longer than naïve mice or mice immunized with SCHU AV or SCHU S4ΔiglC (P≤0.014). Moreover, C3H/HeN mice orally immunized and boosted with SCHU S4ΔclpB survived significantly longer than mice so immunized with LVS (P=0.003) or SCHU S4Δ091ΔcapB (P= 0.008). In BALB/c mice no significant differences in survival were observed between mice orally primed or orally primed and boosted for any of the test vaccines. In contrast oral priming and boosting of C3H/HeN mice with LVS (P=0.014) or SCHU S4ΔclpB (P=0.047) significantly increased survival compared to oral priming alone.
Table 3.
Survival of ID immunized and orally boosted mice following aerosol challenge with SCHU S4.
| Mouse strain | vaccine | Time to death of individual mice (days) |
Median time to death (days) |
|---|---|---|---|
| BALB/c | none | 5,5,5,5,5,5 | 5 |
| BALB/c | LVS | 6,7,8,8 | 7.51 |
| BALB/c | SCHU AV | 6,6,6,6 | 6 |
| BALB/c | SCHU S4Δ0918ΔcapB | 6,8,8,9 | 81 |
| BALB/c | SCHU S4ΔclpB | 7,9,11,11,>28 | 111,2 |
| BALB/c | SCHU S4ΔiglC | 5,6,6,6 | 6 |
| C3H/HeN | none | 5,5,6,6,6,6, | 6 |
| C3H/HeN | LVS | 5,6,7,7,7,8 | 7 |
| C3H/HeN | SCHU AV | 5,5,6,7 | 5.5 |
| C3H/HeN | SCHU S4Δ0918ΔcapB | 6,6,>28,>28 | 17 |
| C3H/HeN | SCHU S4ΔclpB | 8,13,16,16,19 | 161,2 |
| C3H/HeN | SCHU S4ΔiglC | 5,6,6,6,7 | 6 |
Mice were immunized ID with 105 CFU of one or other vaccine, boosted eight weeks later orally with 108 CFU and challenged 6 weeks after this by aerosol with 20 CFU of SCHU S4.
significantly greater survival (P≤0.04) than for the same strain of naive mice or mice immunized with SCHU AV or SCHU S4ΔiglC.
significantly greater survival (P≤0.03) than for the same strain of mice immunized with LVS.
Table 4.
Survival of orally immunized and orally boosted mice following aerosol challenge.
| Mouse strain | vaccine | Time to death of individual mice (days) |
Median time to death (days) |
|---|---|---|---|
| BALB/c | none | 5,5,5,5,5,5 | 5 |
| BALB/c | LVS | 5,6,7,8,8 | 71 |
| BALB/c | SCHU AV | 5,5,5,5,5 | 5 |
| BALB/c | SCHU S4Δ0918ΔcapB | 5,5,11,13 | 8 |
| BALB/c | SCHU S4ΔclpB | 5,6,11,19,>28 | 111 |
| BALB/c | SCHU S4ΔiglC | 5,5,5,5,5 | 5 |
| C3H/HeN | none | 5,5,5,5,5,5 | 5 |
| C3H/HeN | LVS | 5,6,7,8,8 | 71 |
| C3H/HeN | SCHU AV | 5,5,5,5,5 | 5 |
| C3H/HeN | SCHU S4Δ0918ΔcapB | 5,5,5 | 5 |
| C3H/HeN | SCHU S4ΔclpB | 11,15,>28,>28,>28 | >282 |
| C3H/HeN | SCHU S4ΔiglC | 5,5,5,5,5 | 5 |
Mice were immunized orally with 108 CFU of one or other vaccine, boosted eight weeks later by the same route with 108 CFU and challenged 6 weeks after this by aerosol with 20 CFU of SCHU S4.
significantly greater survival (P≤0.02) than for the same strain of naive mice or mice immunized with SCHU AV or SCHU S4ΔiglC.
significantly greater survival than for the same strain immunized with any other vaccine strain (P≤0.008).
3.5 Course of infection in vaccinated mice
Based on the preceding results, it is clear that for SCHU S4-based vaccines, neither oral immunization nor oral boosting, nor the use of C3H/HeN mice conferred any survival advantage over a single ID immunization of BALB/c mice. Therefore, since single transdermal administration of LVS by scarification is currently the sole indication for clinical use, all further studies used only ID immunized BALB/c mice. Moreover, since SCHU S4ΔiglC elicited no protection, and SCHU AV was inferior to SCHU S4 ΔFTT0918ΔcapB or SCHU S4ΔclpB, these control groups were not pursued further. Next we confirmed on two additional occasions our initial observation that ID immunization of BALB/c mice with SCHU S4ΔclpB elicited significantly better protection than ID immunization with LVS against aerosol challenge with SCHU S4. In both additional cases, mice immunized with SCHU S4 ΔFTT0918ΔcapB showed a slight, but insignificant increase in median survival versus mice immunized with LVS (not shown). Understanding the basis for the superior performance of SCHU S4ΔclpB versus LVS in this model could provide insights into mechanisms or correlates of protection.
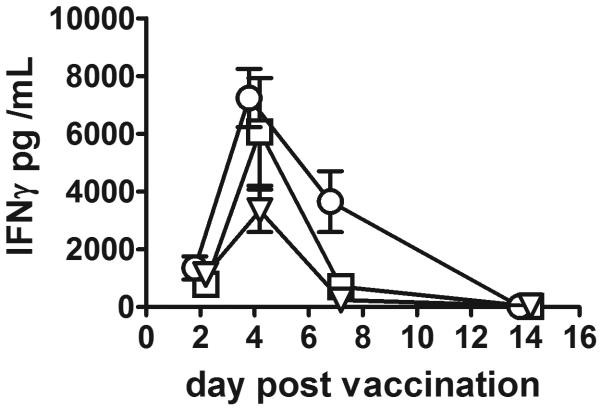
We have previously examined the infection kinetics of LVS in ID immunized mice [7]. Therefore, we were interested to determine the in vivo growth characteristics of SCHU S4 ΔFTT0918ΔcapB and SCHU S4ΔclpB (Figure 1). Overall, in vivo growth kinetics of SCHU S4 ΔFTT0918ΔcapB and SCHU S4ΔclpB were similar to each other and to LVS [7]. Sera from mice immunized ID with 105 CFU of LVS, or SCHU S4 ΔFTT0918ΔcapB, or SCHU S4ΔclpB were collected on days 2,4,7,14 post vaccination and examined for the presence of interferon gamma (IFNγ) as previously described [26]. On day 7 post-vaccination only, circulating levels of IFNγ were significantly greater in mice immunized with SCHU S4 ΔFTT0918ΔcapB versus mice immunized with SCHU S4ΔclpB or LVS (figure 2). Sera were also collected 28 days post vaccination and IgG and IgM ELISA titres against killed SCHU S4 determined as previously described for rabbits [27]. IgG /IgM titres ±SD for mice immunized with SCHU S4 ΔFTT0918ΔcapB (936 ± 274 / 677± 483), SCHU S4ΔclpB (1175 ±283 / 428 ±80), or LVS (1814 ±764 / 411± 142) were compared by one way ANOVA. IgG titres were significantly greater for LVS- versus SCHU S4 ΔFTT0918ΔcapB- immunized mice (P=0.04).
Figure 1.
Course of sublethal infection in mice immunized ID with 105 CFU of SCHU S4 Δ0918ΔcapB (squares) or SCHU S4 ΔclpB (circles). n=4 mice per group.
Figure 2.
Change in serum IFNγ levels following ID immunization with 105 CFU of SCHU S4 ΔFTT0918ΔcapB (squares), SCHU S4 ΔclpB (circles), or LVS (triangles). Mean +/− SEM, n=5/group.
Next we examined the course of infection initiated by inhalation of wild-type SCHU S4 in naive and immunized mice (Table 5). All three vaccines effectively conferred control of the intense bacteremia observed on day 4 of primary infection. By day 2 of infection, mice immunized with SCHU S4ΔclpB harbored significantly fewer bacteria in their lungs than naïve mice or mice immunized with LVS (P<0.05, One way ANOVA with Tukeys post-test). On day 4 of infection, lung burdens were similar in naïve and LVS immunized mice, and burdens in mice immunized with either of the other two attenuated strains were significantly lower than this (P<0.05). LVS-immunized mice harbored >100-fold fewer bacteria in their livers and spleens than naïve mice at day 4 (P<0.05), and mice immunized with either SCHU S4 ΔFTT0918ΔcapB or SCHU S4ΔclpB harbored significantly fewer bacteria than LVS-immunized mice (P<0.05). Naïve mice did not survive beyond day 5. On day 7 of infection, mice immunized with LVS or SCHU S4ΔFTT0918ΔcapB harbored similar numbers of bacteria in the lungs which were significantly higher than the burden in the lungs of mice immunized with SCHU S4ΔclpB. Mice immunized with SCHU S4ΔclpB were better controlling infection in the liver and spleen than mice immunized with SCHU S4ΔFTT0918ΔcapB at this time which, in turn, were performing significantly better than LVS-immunized mice (P<0.05). No LVS immunized and only one SCHU S4 ΔFTT0918ΔcapB immunized mouse survived to day 10 of infection. At this time, mice immunized with SCHU S4ΔclpB harbored similar numbers of bacteria in the lungs, liver and spleen as at day 7. Only between days 10-15 did these mice begin to reduce the bacterial burden in the lungs to the low levels seen in the liver and spleen throughout the course of infection. Similar results were obtained on two separate occasions.
Table 5.
In vivo growth of F. tularensis SCHU S4 following aerosol challenge of vaccinated mice.
| Vaccine group | Tissue | Log10 SD bacterial burden on day post-aerosol-challenge: | ||||
|---|---|---|---|---|---|---|
| 2 | 4 | 7 | 10 | 14 | ||
| Naive | lungs | 6.09± 0.11 | 7.71± 0.20 | |||
| LVS | 6.0± 0.17 | 7.52± 0.07 | 8.31± 0.20 | |||
| Δ0918γΔcapB | 5.65± 0.141,2 | 6.37± 0.211,2 | 8.24 ± 0.08 | 8.60 (1/1) | ||
| ΔclpB | 4.79 ± 0.931,2 | 5.94 ± 0.461,2 | 6.27± 0.962,3 | 6.91 ± 0.96 | 3.97± 1.83 | |
| Naive | liver | 4.04± 0.88 | 7.99 ± 0.25 | |||
| LVS | 3.07 ± 0.58 | 5.77 ± 0.131 | 7.94± 0.73 | |||
| Δ0918ΔcapB | 2.68 (3/4) | 4.25± 0.451,2 | 6.23 ± 0.412 | 7.66 (1/1) | ||
| ΔclpB | 1.87 (2/4)1 | 4.26 ± 0.411,2 | 4.14± 0.642,3 | 5.33± 0.70 | 3.70 (3/4) | |
| Naive | spleen | 3.85± 1.0 | 8.26 ± 0.98 | |||
| LVS | 2.13± 0.761 | 5.75 ± 0.171 | 7.54 ± 0.92 | |||
| Δ0918ΔcapB | 2.36 (3/4) | 4.10 ± 0.181,2 | 5.50 ± 0.372 | 6.23 (1/1) | ||
| ΔclpB | 2.43 ± 0.461 | 3.76 ± 0.381,2 | 3.63 ± 0.582,3 | 4.52± 0.82 | 3.41 ± 1.43 | |
| Naive | Blood /mL | 2.82± 0.94 | 7.19 ± 0.03 | |||
| LVS | 3.47 (1/4)1 | 3.22 ± 0.871 | 4.22 (2/4) | |||
| Δ0918ΔcapB | <2.01 | 3.0 (1/4)1 | 3.91± 0.78 | 3.56 (1/1) | ||
| ΔclpB | 2.85 (1/4)1 | 2.0 (1/4)1 | 2.0 (1/4) | 4.38 (2/4) | <2.0 (0/4) | |
Mice (n=4 / group were immunized ID with 105 CFU of one or other attenuated strain of F. tularensis, then challenged 6 weeks later with an aerosol of SCHU S4.
burden significantly lower than in naïve mice
burden significantly lower than in LVS-immunized mice
burden significantly lower than in SCHU S4Δ0918ΔcapB immunized mice
4. Discussion
The current study examined the ability of novel defined live vaccine candidates to protect mice from ID or aerosol challenge with the highly virulent F. tularensis subsp. tularensis strain, SCHU S4, relative to the protection induced by LVS. LVS has been extensively tested in humans and experimental animals, predominantly mice, for efficacy against infections caused by subsp tularensis initiated via transdermal or pulmonary portals of entry [3-13]. Extensive immunological studies have also been conducted on human and murine hosts immunized with LVS, but to date, no common correlate of protection has been demonstrated. For humans, further vaccination and challenge studies might be required to break this impasse, but such studies will face considerable regulatory hurdles compared to animal studies. Most human studies have employed single dose vaccination by scarification as the method of LVS administration, and this remains the sole clinically indicated use. By this route LVS elicits complete protection against infections initiated via the skin, and partial protection against exposure to an aerosol of the pathogen. The former situation can be recapitulated in mice, the latter less so. In humans, LVS administered by inhalation or by ingestion also protects against systemically- or inhalation-initiated infection [reviewed in 13, 32]. In mice, these routes of LVS administration appear to afford greater protection than transdermal routes against airborne challenge with subsp. tularensis [13]. Currently, several live anti-viral or anti-bacterial vaccines are administered by inhalation or ingestion [28-31]. Moreover, both routes potentially offer a more tolerable means of vaccination than hypodermic injection. Additionally, for LVS at least, the oral route seems to be at least as safe as the ID route. In contrast, LVS is more virulent for humans and experimental animals when administered directly to the lungs [5, 33, 34]. This appears to be the case too with SCHU S4-based vaccines; in our hands the IN LD50 for LVS and SCHU S4 Δ0918ΔcapB is ~ 103 CFU, and for SCHU S4ΔclpB ~106 CFU). Another potential problem with oral or pulmonary administration of live attenuated strains of F. tularensis is that it exposes the vaccine to a variety of normal flora from which it might acquire homologs of the virulence genes that were deleted in order to attenuate it. Therefore, transdermal injection still appears to be the most rational route for administering live vaccines against F. tularensis, especially when coupled with the extensive clinical data for LVS given via this versus other routes.
LVS administered ID or orally to mice has been shown to elicit partial protection against aerosol challenge measured as enhanced survival for a day or so [7,8,12,14]. Therefore, it might be possible to predict efficacy of novel vaccines against inhalation tularemia in humans by comparing their efficacy relative to LVS in mice. As proof-of-concept for this possibility, in the current study we have generated defined experimental live vaccine strains by deleting specific virulence genes from fully virulent F. tularensis subsp. tularensis strain SCHU S4 and compared them against LVS for their ability to elicit protection against pulmonary challenge following ID or oral vaccination using two mouse strains for which such efficacy has been previously demonstrated by one or other route. In particular, two deletion mutants, SCHU S4 Δ0918ΔcapB and SCHU S4ΔclpB, showed levels of attenuation similar to LVS (>1-million-fold versus wild-type SCHU S4 by the ID route) and were as effective as LVS at combating ID challenge with >1000 LD50 of the fully virulent pathogen. Against an aerosol challenge, SCHU S4 ΔclpB significantly outperformed LVS when given ID or orally to BALB/c mice. In C3H/HeN mice both vaccines performed at a similar level when given ID, but SCHU S4ΔclpB was significantly better than LVS when given orally. Indeed, it was the only strain to elicit any measurable protection when given orally. ID primed and orally boosted mice of both strains were significantly better protected by SCHU S4ΔclpB versus LVS. Oral boosting of orally primed mice also resulted in better protection for mice immunized with SCHU S4ΔclpB versus LVS, but this only reached statistical significance in C3H/HeN mice. SCHU S4 Δ0918ΔcapB elicited similar protection as LVS in BALB/c mice regardless of vaccination regimen, but the results were more mixed in C3H/HeN mice. Furthermore, C3H/HeN mice did reveal SCHU S4 Δ0918ΔcapB to be less attenuated than SCHU S4ΔclpB, a phenomenon which was masked in BALB/c mice. No vaccination regimen offered any obvious advantage over single dose ID immunization of BALB/c mice, and results with this model reflected the majority finding of all of the others that were examined. Therefore, this model was adopted for all further studies. In this model, the superiority of SCHU S4 ΔclpB versus LVS correlated with an enhanced ability of mice immunized with it to control a subsequent aerosol challenge with SCHU S4. Surprisingly, by day 10 of infection, the lungs of mice immunized with SCHU S4ΔclpB still contained 1 million francisellae, a number that was reduced 1000-fold by day 14. Thus, even mice that were fully protected had difficulty killing F. tularensis in the lungs. A similar situation has been reported for inhaled Mycobacterium tuberculosis [35] and Listeria monocytogenes [36] in systemically immunized mice possibly suggesting a common defect in the ability to express anti-bacterial immunity in the lungs versus other organs.
A preliminary examination of the immune responses elicited by each vaccine provided no obvious reason for the superior ability of SCHU S4ΔclpB to elicit protective pulmonary immunity against inhaled F. tularensis. More detailed analyses are underway. Finally, to belay regulatory concerns about possible reversion to a wild-type virulent phenotype, it will probably be necessary to delete additional unlinked virulence genes from SCHU S4ΔclpB. However, further attenuation of this mutant could lead to an unacceptable loss of immunogenicity. Indeed, such issues have plagued live vaccine development against other intracellular bacteria [37-39]. Nevertheless, live vaccines against S. Typhi containing multiple gene deletions have been developed for human use [40-41].
Acknowledgements
We thank Michel Cleroux, Xigeng Zhao, and Kevan McRae for technical assistance. We thank Dr. Lawrence A. Wolfraim and Dr. Mark Bolanowski, DynPort Vaccine Company, for their encouragement and support for, and critical review of this work. This project has been funded in whole or in part with Federal funds from the National Institute of Allergy and Infectious Diseases, National Institutes of Health, Department of Health and Human Services, under Contract HHSN266200500041C and Grant No. A160689.
The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sjostedt A. Tularemia: History, epidemiology, pathogen physiology and clinical manifestations. Ann New York Acad Sci. 2007;1105:1–29. doi: 10.1196/annals.1409.009. [DOI] [PubMed] [Google Scholar]
- 2.Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, et al. Tularemia as a biological weapon: medical and public health management. JAMA. 2001;285:2763–73. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- 3.Saslaw S, Eigelsbach HT, Wilson HE, Prior JA, Carhart S. Tularemia vaccine study. I. Intracutaneous challenge. Arch Int Med. 1961;107:689–701. doi: 10.1001/archinte.1961.03620050055006. [DOI] [PubMed] [Google Scholar]
- 4.Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S. Tularemia vaccine study II. Respiratory challenge. Arch Int Med. 1961;107:702–14. doi: 10.1001/archinte.1961.03620050068007. [DOI] [PubMed] [Google Scholar]
- 5.Hornick RB, Eigelsbach HT. Aerogenic immunization of man with live tularemia vaccine. Bact Revs. 1966;30:532–38. doi: 10.1128/br.30.3.532-538.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCrumb FR. Aerosol infection of man with Pasteurella tularensis. Bact Revs. 1961;25:262. doi: 10.1128/br.25.3.262-267.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen W, Shen H, Webb A, KuoLee R, Conlan JW. Tularemia in BALB/c and C57BL/6 mice vaccinated with Francisella tularensis LVS and challenged intradermally, or by aerosol with virulent isolates of the pathogen; protection varies depending on pathogen virulence, route of exposure, and host genetic background. Vaccine. 2003;21:3690–700. doi: 10.1016/s0264-410x(03)00386-4. [DOI] [PubMed] [Google Scholar]
- 8.Shen H, Chen W, Conlan JW. Susceptibility of various mouse strains to systemically- or aerosol- initiated tularemia by virulent type A Francisella tularensis before and after immunization with the attenuated live vaccine strain of the pathogen. Vaccine. 2004;22:2116–21. doi: 10.1016/j.vaccine.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Wu TH, Hutt JA, Garrison KA, Berliba LS, Zhou Y, Lyons CR. Intransal vaccination induces protective immunity against intranasal infection with virulent Francisella tularensis biovar A. Infect Immun. 2005;73:2644–54. doi: 10.1128/IAI.73.5.2644-2654.2005. 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lyons CR, Wu TH. Animal models of Francisella tularensis infection. Ann New York Acad Sci. 2007;1105:238–65. doi: 10.1196/annals.1409.003. [DOI] [PubMed] [Google Scholar]
- 11.Eigelsbach HT, Tulis J, Overholt EL, Griffith WR. Aerogenic immunization of the monkey and guinea pig with live tularemia vaccine. Proc. Soc Exptl Biol Med. 1961;108:732–4. doi: 10.3181/00379727-108-27049. [DOI] [PubMed] [Google Scholar]
- 12.Conlan JW, Shen H, KuoLee R, Zhao X, Chen W. Aerosol-, but not intradermal- immunization with the live vaccine strain of Francisella tularensis protects mice against subsequent aerosol challenge with a highly virulent type A strain of the pathogen by an αβ T cell- and interferon gamma- dependent mechanism. Vaccine. 2005;23:2477–85. doi: 10.1016/j.vaccine.2004.10.034. [DOI] [PubMed] [Google Scholar]
- 13.KuoLee R, Harris G, Conlan JW, Chen W. Oral immunization of mice with the live vaccine strain (LVS) of Francisella tularensis protects mice against respiratory challenge with virulent type A F. tularensis. Vaccine. 2007;25:3781–91. doi: 10.1016/j.vaccine.2007.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Twine SM, Bystrom M, Chen W, Forsman M, Golovliov IR, Johansson A, et al. A mutant of Francisella tularensis strain SCHU S4 lacking the ability to express a 58 kDa protein is attenuated for virulence and an effective live vaccine. Infect Immun. 2005;73:8345–52. doi: 10.1128/IAI.73.12.8345-8352.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Turner AK, Lovell MA, Hulme SD, Zhang-Barber L, Barrow P. Identification of Salmonella typhimurium genes required for colonization of the chicken alimentary tract and for virulence in newly hatched chicks. Infect Immun. 1998;66:2099–2106. doi: 10.1128/iai.66.5.2099-2106.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chastanet A, Derre I, Nair S, Msadek T. clpB a novel member of the Listeria monocytogenes ctsR regulon is involved in virulence but not in general stress tolerance. J Bact. 2004;186:1165–74. doi: 10.1128/JB.186.4.1165-1174.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Su J, Yang J, Zhao D, Kawula TH, Banas JA, Zhang JR. Genome-wide identification of Francisella tularensis virulence determinants. Infect Immun. 2007;75:3089–101. doi: 10.1128/IAI.01865-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meibom KL, Dubial I, Dupuis M, Barel M, Lenco J, Stulik J, et al. The heat-shock protein clpB of Francisella tularensis is involved in stress tolerance and is required for multiplication in target organs of infected mice. Mol Microbiol. 2008;67:1384–1401. doi: 10.1111/j.1365-2958.2008.06139.x. [DOI] [PubMed] [Google Scholar]
- 19.Gray CG, Cowley SC, Cheung KK, Nano FE. The identification of five genetic loci of Francisella novicida associated with intracellular growth. FEMS Microbiol Lett. 2002;215:53–6. doi: 10.1111/j.1574-6968.2002.tb11369.x. [DOI] [PubMed] [Google Scholar]
- 20.Tempel R, Lai XH, Crosa L, Kozlowicz B, Heffron F. Attenuated Francisella novicida transposon mutants protect mice against wild-type challenge. Infect Immun. 2006;74:5095–105. doi: 10.1128/IAI.00598-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Weiss DS, Brotke A, Henry T, Margolis JJ, Chan K, Monack DM. In vivo negative selection screen identifies genes required for Francisella virulence. Proc Nat Acad Sci. 2007;104:6037–42. doi: 10.1073/pnas.0609675104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Larsson P, Oyston PCF, Chain P, Chu MC, Duffield M, Fuxelius H-H, et al. The complete genome sequence of Francisella tularensis, the causative agent of tularemia. Nat Genet. 2005;37:153–9. doi: 10.1038/ng1499. [DOI] [PubMed] [Google Scholar]
- 23.Golovliov I, Sjostedt A, Mokrievich A, V. Pavlov V. A method for allelic replacement in Francisella tularensis. FEMS Microbiol Lett. 2002;222:273–80. doi: 10.1016/S0378-1097(03)00313-6. [DOI] [PubMed] [Google Scholar]
- 24.Huntley JF, Conley PG, Rasko DA, Hagman KE, Apicella MA, Norgaard MV. Native outer membrane proteins protect mice against pulmonary challenge with virulent type A Francisella tularensis. Infect Immun. 2008;76:3664–71. doi: 10.1128/IAI.00374-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ray HJ, Cong Y, Murthy AK, Selby DM, Klose KE, Barker JR, et al. Oral live vaccine-strain-induced protective immunity against pulmonary Francisella tularensis challenge is mediated by CD4+ T cells and antibodies, including immunoglobulin A. Clin Vaccine Immunol. 2009;16:444–52. doi: 10.1128/CVI.00405-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Conlan JW, Zhao X, Harris G, Shen H, Bolanowski M, Rietz C, et al. Molecular immunology of experimental primary tularemia in mice infected by respiratory or intradermal routes with type A Francisella tularensis. Mol Immunol. 2008;45:2962–69. doi: 10.1016/j.molimm.2008.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pasetti MF, Cuberos L, Horn TL, Shearer JD, Matthews SJ, House RV, et al. An improved Francsiella tularensis live vaccine strain (LVS) is well tolerated and highly immunogenic when administered to rabbits in escalating doses using various immunization routes. Vaccine. 2008;26:1173–85. doi: 10.1016/j.vaccine.2008.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wong-Chew RM, Islas-Romero R, Garcia-Garcia ML, Beeler JA, Audet S, Santos-Preciado JI, et al. Immunogenicity of aerosol measles vaccine given as the primary measles immunization to nine-month-old Mexican children. Vaccine. 2006;24:683–90. doi: 10.1016/j.vaccine.2005.08.045. [DOI] [PubMed] [Google Scholar]
- 29.Block SL, Reisinger KS, Hultquist M, Walker RE. Comparative immunogenicities of frozen and refrigerated forulations of live attenuated influenza vaccine in healthy subjects. Antimicrob Agents Chemother. 2007;51:4001–8. doi: 10.1128/AAC.00517-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prikazsky V, Leroux-Roels G, Van Damme P, Safary A, Colau B, Duchene M. Comparative pre-clinical and clinical experience with oral polio vaccine produced on MRC-5 cells or on primary monkey kidney cells. Vaccine. 2005;23:4219–27. doi: 10.1016/j.vaccine.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Kirkpatrick BD, Tenney KM, Larsson CJ, O'Neill JP, Ventrone C, Bentley M, Upton M, Hindle Z, et al. The novel oral typhoid vaccine M01ZH09 is well tolerated and highly immunogenic in 2 vaccine presentations. J. Infect Dis. 2005;192:360–6. doi: 10.1086/431605. [DOI] [PubMed] [Google Scholar]
- 32.Hornick RB, Dawkins AT, Eiglesbach HT, Tulis JJ. Oral tularemia vaccine in man. Antimicrob Agents Chemother. 1966;6:11–14. doi: 10.1128/AAC.6.1.11. [DOI] [PubMed] [Google Scholar]
- 33.Fortier AH, Slayter MV, Ziemba R, Meltzer MS, Nacy CA. Live vaccine strain of Francisella tularensis: Infection and immunity in mice. Infect Immun. 1991;59:2922–8. doi: 10.1128/iai.59.9.2922-2928.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Conlan JW, KuoLee R, Shen H, Webb A. Different host defences are required to protect mice from primary systemic vs pulmonary infection with the facultative intracellular bacterial pathogen, Francisella tularensis LVS. Microb Pathog. 2002;32:34. doi: 10.1006/mpat.2001.0489. [DOI] [PubMed] [Google Scholar]
- 35.Medina E, North RJ. Genetically susceptible mice remain proportionally more susceptible to tuberculosis after vaccination. Immunology. 1999;96:16–21. doi: 10.1046/j.1365-2567.1999.00663.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Truitt GL, Mackaness GB. Cell-mediated resistance to aerogenic infection of the lung. Am Rev Rep Dis. 1971;104:829–843. doi: 10.1164/arrd.1971.104.6.829. [DOI] [PubMed] [Google Scholar]
- 37.Garmory HS, Brown KA, Titball RW. Salmonella vaccines for use in humans: present and future perspectives. FEMS Microbiol Revs. 2002;26:393–53. doi: 10.1111/j.1574-6976.2002.tb00619.x. [DOI] [PubMed] [Google Scholar]
- 38.Stocker BAD. Aromatic-dependent Salmonella as anti-bacterial vaccines and as presenters of heterologous antigens or of DNA encoding them. Vaccine. 2000;83:45–50. doi: 10.1016/s0168-1656(00)00297-2. [DOI] [PubMed] [Google Scholar]
- 39.Levine MM, Kotloff KL, Barry EM, Pasetti MF, Sztein MB. Clinical trials of Shigella vaccines: two steps forward and one step back on a long, hard road. Nat Rev Microbiol. 2007;5:540–553. doi: 10.1038/nrmicro1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tacket CO, Sztein MB, Losonsky GA, Wasserman SS, Nataro JP, Edelman R, et al. Safety of live oral Salmonella typhi vaccine strains with deletions in htrA and aroC aroD and immune response in humans. Infect Immun. 1997;65:452–56. doi: 10.1128/iai.65.2.452-456.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hindle Z, Chatfield SN, Phillimore J, Bentley JM, Johnson J, Cosgrove CA, et al. Characterization of Salmonella enterica derivatives harboring defined aroC and Salmonella pathogenicity island 2 type III secretion system (ssaV) mutations by immunization of healthy volunteers. Infect Immun. 2002;70:3457–67. doi: 10.1128/IAI.70.7.3457-3467.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]