Abstract
Objective
Survival in women with recurrent or metastatic cervical cancer remains poor. More effective and less toxic regimens are needed. Cisplatin is an effective radiosensitizer, but its single agent activity in recurrent cervical cancer, especially after prior cisplatin exposure, is disappointing, with a response rate of only 13%. Oxaliplatin has preclinical activity in cisplatin-resistant tumors and may have synergic activity when combined with paclitaxel. Our objective is determine the efficacy and toxicity of paclitaxel and oxaliplatin in patients with recurrent or metastatic cervical cancer.
Methods
Patients with histologic confirmation of primary metastatic or recurrent cervical cancer not amenable to surgical management were eligible. Treatment consisted of paclitaxel 175 mg/m2 IV and oxaliplatin 130 mg/m2 IV every 21 days. The primary endpoints were toxicity, recorded every cycle, and response, determined by RECIST criteria were assessed every 9 weeks, with subsequent confirmation as required. Sample size determinations were made using a Simon's two-stage design with a projected overall response proportion of 13% with cisplatin alone. Survival rates were calculated with Kaplan-Meier methods.
Results
Of the 35 patients enrolled, 32 were evaluable. The median age was 56(27-78); 30 had had prior radiation (23 concomitant with cisplatin). Patients completed a mean of 4.2 cycles (1-11). There were 2 complete and 5 partial responses for a total response rate of 7/32 (22%; 95% CI: 9.3%-40.0%). Eight patients had stable disease for an overall clinical benefit rate of 15/32 (47%; 95% CI: 29.1% - 65.3%). The mean time to best response was 13.5 weeks (95% C.I.: 10.6, 16.4). The mean progression-free survival was 21 weeks (95% C.I.: 14.7, 27.2) and mean overall survival was 52.1weeks (95% C.I.: 39.4, 64.8). A total of 135 cycles were administered. There were 28 (20.1%) grade 3/4 hematologic toxicities and 46 (34.1%) grade 3/4 non-hematologic toxicities, which were predominantly sensory neuropathy. There were 13 treatment delays, 4 dose reductions, and no treatment-related deaths.
Conclusions
The combination of paclitaxel and oxaliplatin is an effective regimen in patients with recurrent or persistent cervical cancer including a majority previously exposed to cisplatin. Further study and comparison with other platinum-based regimens is warranted.
Introduction
Cancer of the uterine cervix is the most common cause of gynecologic cancer deaths worldwide. In the United States, there was an estimated 11,270 cases of cervical cancer and 4070 cancer deaths in 2009 [1]. In addition to the mortality associated with this disease, advanced cervical carcinoma is also associated with significant morbidities including renal failure, liver metastases, complex fistulas, and painful bony metastases.
Concomitant chemoradiotherapy has been shown to improve survival in women with locally advanced disease[2]. However, chemotherapy, particularly cisplatin-based regimens, for metastatic disease has not led to major improvements in clinical outcome and is associated with high rate of severe toxicities [3]. Of the cytotoxic drugs which have been evaluated, cisplatin is the most active agent. A randomized trial of cisplatin versus the combination of cisplatin and paclitaxel did demonstrate improved response rates and progression-free survival for the combination, but no impact on survival, which remained in the 8-9 month range even in patients who had largely not been treated with prior cisplatin [4]. Subsequent studies have shown lesser response rates to cisplatin in patients previously exposed to cisplatin as a radiosensitizer, and suggested that topotecan when added to cisplatin enhances the response and survival rates [5]. More recently, a comparison of various cisplatin-based doublets have yielded no differences in outcome, and again suggest that prior cisplatin exposure blunts response rates [6].
Oxaliplatin is a platinum analogue that inhibits DNA synthesis by causing intrastrand cross-links in DNA [7]. However, in preclinical studies, its spectrum of activity and reistance patterns differ from those of cisplatin and carboplatin. Lack of recognition of the hMLH1 and hMSH2 DNA mismatch repair gene of the oxaliplatin diaminocyclohexane platinum adduct is another feature that sets it apart from other platinum [8].
Moreover, oxaliplatin has activity in patients with platinum-pretreated cancers, including ovarian cancer where objective response rates were similar to paclitaxel in this setting (16% vs. 17%). Activity has been observed with oxaliplatin in patients with colon cancer, non-Hodgkin's lymphoma, breast cancer, mesothelioma and non-small cell lung cancer [9-12].
The combination of paclitaxel and oxaliplatin has been studied in a phase I study in platinum-pretreated ovarian cancer[13] and in a phase II study in non-small cell cancer. In the phase I study, the major toxicities were neutropenia and neurologic toxicity. In the phase II study, the same toxicities were observed, with 13 partial responses among 38 patients [14].
Since combination paclitaxel and oxaliplatin have shown high level of activity and tolerability during concurrent administration and promising early clinical efficacy results, the overall objective of this phase II trial was to determine the objective response rates and toxicities of paclitaxel and oxaliplatin in women with metastatic or locally recurrent cervical cancer, Also, this study was performed to begin introducing the hypothesis that sensitivity to oxaliplatin doublets is not greatly affected by prior exposure to cisplatin.
Materials and Methods
Patients
This is an NCI-sponsored multi-institutional open-label phase II trial (NCI 5840, NCT00057863) of paclitaxel 175mg/m2 followed by oxaliplatin 130m/m2 every three weeks in women with recurrent and/or metastatic cervical cancer. Eligible patients were at least 18 years of age, not pregnant, with a pathologically confirmed squamous cell, adenosquamous cell or adenocarcinoma of the uterine cervix, and not eligible for a surgical option. Lesions were metastatic to organs or lymph nodes outside the pelvis or locally recurrent in the pelvis after initial definitive therapy (surgery, radiation or chemoradiation). Measurable disease, defined as at least one lesion ≥20mm in one dimension with conventional techniques or as ≥10mm with spiral CT scan was required. No prior treatment with cytotoxic agents for metastatic or recurrent disease was allowed. Patients who had chemotherapy, radiation therapy or surgery were required to have a four week treatment free window. Eligible patients were required to have a ≥ 2 months life expectancy with an ECOG performance status of ≤2.
Eligible patients had to meet criteria for adequate organ and bone marrow function, including a leukocyte count greater than or equal to 3,000/μL, absolute neutrophil count of greater than 1,500/μL, platelet count of greater than or equal to 100,000/μL, total bilirubin and creatnine within institutional normal limits, AST and ALT that were less than two and half times of the institutional upper limit of normal value.
Patients could not have received any concomitant investigational agents. Potential subjects infected with HIV or known brain metastases were excluded, as were patients with grade 2 or greater neuropathy. Additionally, patients were excluded if they had a known history of allergic reaction attributed to paclitaxel, oxaliplatin, or compounds with similar chemical or biological composition. All patients signed written, informed consent prior to initiating therapy. Institutional review board approval for the protocol and the consent were obtained prior to patient enrollment at each participating institution.
Treatment Plan
Paclitaxel was infused over 3 hours every 21 days, followed by oxaliplatin over 2 hours every 21 days in an outpatient setting. Subjects were clinically evaluated prior to each chemotherapy cycle. Serum chemistry and liver function tests were performed every 3 weeks. Complete blood count was drawn every week. Radiographic assessment with CT scan of the abdomen and pelvis were performed prior to initiation of treatment and every 8 weeks during treatment. Treatment was continued every 3 weeks until disease progression, dose-limiting toxicity, patient withdrawl, or death. Blood transfusions and cytokine (G-CSF) support were given as clinically indicated based on standard NCCN guidelines [15]. Toxicity was graded using standard National Cancer Institute Common Toxicity Criteria, version 2.0. Toxicities were assessed by the treating physicians and tabulated based on case report documentation.
Dose modifications, as shown in Table 1, were done for dose delays or prolonged or severe toxicity for paclitaxel and/or oxaliplatin. Treatment with both drugs was held for grade 2 neurotoxicity or greater. Treatment was restarted at the same doses for grade 2 neurotoxicity that resolved within 14 days, or it was restarted at a reduced dose level for grade 3 neurotoxicity if it resolved within 14 days. Subjects with grade 4 neurotoxicity were ineligible to continue on this treatment regimen. For hematologic toxicity, treatment with both drugs were held for leukocyte count < 3000/mm3, absolute neutrophil counts < 1500/mm3, or platelet count < 75,000/mm3. Treatment was restarted at full doses when counts recovered. If treatment was held for > 2 weeks, the doses were reduced by one dose level for the next treatment. For subjects who had nadir leukocyte counts < 500/mm3 or platelet counts < 10,000/mm3 associated with fever or bleeding or lasting > 3 days, the dose was reduced for both drugs by one dose level at the next treatment cycle. Treatment was also held for all other toxicities that were grade 2 or greater until they resolved to grade 1 or baseline. Subjects with grade 4 toxicity were removed from the study. If toxicities did not resolve within 3 weeks, the subject was not continued on this treatment regimen.
Table 1. Dose modifications due to delays or toxicities.
| Dose level | Oxaliplatin (mg/m2) | Paclitaxel (mg/m2) |
|---|---|---|
| 0 | 130 | 175 |
| -1 | 100 | 135 |
| -2 | 75 | 100 |
Subjects were reevaluated for responses every 9 weeks. Responses were evaluated using standard RECIST criteria [16] and categorized as a complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD). In the case of SD, follow-up measurements must have met the SD criteria (< 30% decrease or <20% increase in consecutively documented target lesions) at least once after study entry and at a minimum interval of 6-8 weeks after initial response determination.
Statistical Analysis
Sample size determinations were determined using a Simon's two-stage design [17]. We projected an overall objective response proportion (CR+PR) of 13%, below which the response would be unacceptable and an overall objective response proportion of 33%, above which the regimen would be considered worthy of further exploration. The null hypothesis that the overall objective response proportion is less than or equal to 13% was tested against the alternative hypothesis that the response proportion is greater than or equal to 33%. At the end of the second stage, the treatment would be declared effective and worthy of further testing if 7 or more patients responded among the 32 patients entered. These assumptions are based on GOG 179 comparing cisplatin with or without topotecan in a similar group of patients where the response rate for the cisplatin control group was 13% [5]. The sample size computations were performed assuming a 10% level of significance and 90% power. The primary endpoint of the overall objective response rate (CR+PR) was estimated with 95% confidence intervals based on the exact binomial distribution. Secondary endpoints of progression-free survival (PFS) and overall survival (OS) were assessed by Kaplan-Meier survival analysis and 95% confidence intervals were calculated using Greenwood's formula.
Results
The patient characteristics are presented in Table 2. A total of 35 subjects were enrolled in the study from April 2003 until August 2008. The result of the first stage of this study has previously been reported [18]. Of the 35 enrolled subjects, 32 were treated since two subjects did not receive any protocol drug after registration. One additional patient died of cardiac arrest unrelated to treatment after one dose. The median age of treated subjects was 56 (range: 27-78); 30 had had prior radiation, 24 concomitant with cisplatin. Patients completed a median of 4 cycles (range: 1-11). Two patients had a complete response, 5 had a partial response for a total response rate of 7/32 (22%; 95% CI: 9.3%-40.0%). There were also 8 patients with stable disease for an overall clinical benefit rate of 15/32 (47%; 95% CI: 29.1% - 65.3%). The mean time to best response for these 15 patients was 13.5 weeks (95% C.I.: 10.6, 16.4). The mean progression-free survival was 21 weeks (95% C.I.: 14.7, 27.2) and the mean overall survival was 52.1 weeks (95% C.I.: 39.4, 64.8) (See Figure 1 for K-M curve).
Table 2. Patient demographics and baseline disease characteristics (N = 32).
| Median age (years) | 56 (27-78) |
|---|---|
| ECOG performance status | |
| 0 | 10 |
| 1 | 15 |
| 2 | 7 |
| Race | |
| Caucasian | 12 |
| Hispanic | 9 |
| African American | 8 |
| Asian | 3 |
| Histology | |
| Squamous cell carcinoma | 25 |
| Adenocarcinoma | 7 |
| Prior radiation therapy | 24 |
| Prior cisplatin therapy | 31 |
Abbreviation: ECOG = Eastern Cooperative Oncology Group
Figure 1.
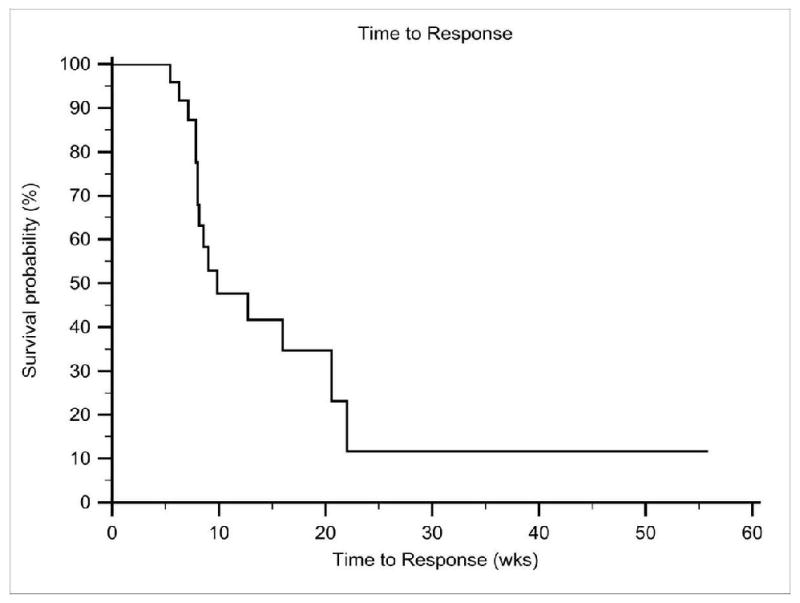
Kaplan-Meier curve of overall survival for subjects treated with paclitaxel plus oxaliplatin
A total of 135 cycles of paclitaxel and oxaliplatin were administered (range 1-11 cycles). There were 28 (20.7%) grade 3/4 hematologic toxicities and 46 (34.1%) grade 3/4 non-hematologic toxicities. Table 3 lists all of the documented toxicities for all protocol-administered cycles. Both hematologic (6/28) and non-hematologic (16/46) events were often due to disease progression. There were 4 patients who developed grade 3 neuropathy and one patient who developed a grade 4 febrile neutropenia on their last completed treatment cycle. There were 13 treatment delays and 4 dose reductions: 2 dose reductions were due to grade 3 neuropathy; 1 was due to prolonged grade 2 neuropathy, and 1 was due to significant nausea and vomiting, requiring hospitalization. There were no treatment-related deaths.
Table 3. All documented toxicities for patients (total of 135 cycles).
| Grade | 3 | 4 |
|---|---|---|
| Hematologic | ||
| Neutropenia | 6 | 2 |
| Febrile neutropenia | 1 | 0 |
| Anemia | 6 | 6 |
| Thrombocytopenia | 4 | 0 |
| Thrombosis | 2 | 0 |
| Coagulopathy | 1 | 0 |
| Non-hematologic | ||
| Gastrointestinal | ||
| Nausea | 1 | 0 |
| Vomitting | 1 | 0 |
| Diarrhea | 1 | 0 |
| Constipation | 1 | 0 |
| Colitis | 1 | 0 |
| Severe vaginal hemorrhage | 1 | 0 |
| Others(bowel perforation fistula and obstruction) | 2 | 1 |
| Neuromuscular | ||
| Neuropathy | 5 | 0 |
| Pain | 5 | 3 |
| Others (weakness, fatigue, somnolence) | 5 | 0 |
| Others | ||
| Electrolytes imbalance | 14 | 0 |
| Dehydration | 1 | 0 |
| Hypersensitivity reaction | 0 | 1 |
| Psychological | 1 | 0 |
| Infection | 1 | 1 |
Discussion
Platinum-based chemotherapy has formed the basis for current treatment of metastatic cancer of the cervix. Trials using paclitaxel plus cisplatin or topotecan plus cisplatin have shown more favorable response rates than cisplatin alone. However, the survival advantage is limited and the toxicities of these regimens have been fairly significant [4, 5]. A four-arm study comparing cisplatin-based doublets has recently been completed, with the study closing early because of improvement in outcome over cisplatin plus paclitaxel was deemed unlikely [6].
Cisplatin has been the standard of care in treating women with cervical cancer. GOG 179 compared cisplatin plus topotecan versus cisplatin alone in the treatment of recurrent and persistent cervical cancer. There was an improvement in progression-free survival and overall response rate and overall survival in the cisplatin plus topotecan arm. The overall response rate was 13% for the single-agent cisplatin and 27% when cisplatin was combined with topotecan [5]. The median progression free survival and median survival were 2.9 and 6.5 months for patients treated cisplatin, 4.6 and 9.4 months for patients treated with the combination of cisplatin plus topotecan. In GOG 169, cisplatin was compared to cisplatin plus paclitaxel in the treatment of recurrent or persistent Stage IV sqamous cell carcinoma [4]. The median progression-free-survival in patients treated with cisplatin alone was 2.8 months and 4.8 months for patients treated with cisplatin and paclitaxel. The overall response rate was 19% for cisplatin alone and 36% for the combination regimen. One important aspect in the last two studies by the GOG is that most recruited subjects have been exposed to cisplatin as part of prior concomitant chemoradiotherapy. This practice became widespread after the 1999 NCI alert providing the basis for the routine use of concomitant chemoradiotherapy for all locally-advanced cervical cancer patients [19]. A list of the percent of patients who had prior concomitant chemoradiotherapy and the response rates for GOG 169 and 179 are in Table 4. In GOG 179, less benefit was shown in the group of patients who had previously received concomitant chemoradiotherapy and went on to receive systemic chemotherapy in the study, suggesting a potential chemoresistance to platinum in those previously treated concomitantly with radiation therapy. In our current trial, 75% of the subjects received concomitant chemoradiotherapy with cisplatin for their initial treatment, with the response rate comparable to the recently reported GOG studies using platinum-based regimens (Table 4). This suggests the combination of paclitaxel and oxaliplatin may not be cross-resistant in patients initially treated with concomitant chemoradiotherapy with cisplatin. Since most recent patients with recurrent metastatic cervical cancer have previously received prior concomitant chemoradiotherapy, cross-resistance between these drugs should be subject for further study as it has for ovarian cancer [20]. Because of relatively low response rates to the cisplatin doublets, currently the GOG is examining the role of a non-platinum doublet and whether results are enhanced by bevacizumab.
Table 4. Comparison of response rates for the combination regimen in GOG 169, GOG 179 and current study [21].
| Chemotherapy Regimen | RR | mPFS (months) | mOS (months) | C/RT | RT | |
|---|---|---|---|---|---|---|
| GOG 169 | C/P | 36% | 4.8 | 9.7 | 24% | 91% |
| GOG 179 | C/T | 27% | 4.6 | 9.4 | 63% | |
| Kuo et al | O/P | 22% | 4.6 | 11.7 | 75% | 95% |
C/P: Cisplatin and Paclitaxel
C/T: Cisplatin and Topotecan
O/P: Oxaliplatin and Paclitaxel
RR: Response rate.
mPFS: median progressional free survival.mOS: median overall survival.
C/RT: Percent of patients who received chemotherapy and radiation therapy.
RT: Percent of patients who received radiation therapy.
In our phase II study, paclitaxel and oxaliplatin were well tolerated, but there was cumulative neurotoxicity noted. Attenuation of drug dosage after achieving a response is suggested as a possible strategy to minimize having to abandon the treatment because of sensory neuropathy. Again when compared to cisplatin-based regimens, as shown in GOG 169 and 179, this regimen showed a comparable clinical benefit rate with good tolerability as shown by minimal dose delays, dose reductions, and limited severe toxicity. Future powering of recurrent cervical cancer clinical trials should also take this clinical paradigm of more common use of concomitant chemoradiotherapy with cisplatin into account. At present this is a group of patients with minimal chance of long term survival. Quality of life while on treatment has clear clinical importance for these patients.
We realize some of the limitations of the study, including its small sample size, yielding relatively wide 95% confidence intervals of response. However, its prospective nature in a consortium including ethnically and racially-diverse catchment area, and a large percentage of cases that have received prior radiation and cisplatin speak for the potential for wide applicability of these results. Therefore, this regimen should be considered for testing as an arm within a future randomized cooperative group Phase III trial.
Acknowledgments
This work was presented at the SGO annual meeting in San Antonio, TX February, 2009
Research support: This study is supported by an NCI grant, N01-CM62204
Footnotes
Conflict of interest statement
The authors declare that there are no relationships that may present conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dennis Yi-Shin Kuo, Montefiore Medical Center/Albert Einstein College of Medicine.
Stephanie V. Blank, NYU Langone Medical Center.
Paul J. Christo, New York Presbyterian Hospital/Weill Cornell Medical College.
Mimi Kim, Albert Einstein College of Medicine.
Thomas A. Caputo, Weill Cornell Medical College.
Bhavana Pothuri, NYU Medical Center.
Dawn Hershman, New York Presbyterian Hospital/Columbia University.
Noah Goldman, Beth Israel Medical Center New York.
Percy S. Ivy, NCI/CTEP.
Carolyn D. Runowicz, University of Connecticut Health Center.
Franco Muggia, NYU Langone Medical Center.
Gary L. Goldberg, Montefiore Medical Center/Albert Einstein College of Medicine.
Mark H. Einstein, Montefiore Medical Center/Albert Einstein College of Medicine.
References
- 1.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics, 2009. CA Cancer J Clin. 2009;59:225–73. doi: 10.3322/caac.20006. [DOI] [PubMed] [Google Scholar]
- 2.Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, Clarke-Pearson DL, Insalaco S. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999;340:1144–53. doi: 10.1056/NEJM199904153401502. [DOI] [PubMed] [Google Scholar]
- 3.Omura GA. Chemotherapy for stage IVB or recurrent cancer of the uterine cervix. J Natl Cancer Inst Monogr. 1996:123–6. [PubMed] [Google Scholar]
- 4.Moore DH, Blessing JA, McQuellon RP, Thaler HT, Cella D, Benda J, Miller DS, Olt G, King S, Boggess JF, Rocereto TF. Phase III study of cisplatin with or without paclitaxel in stage IVB, recurrent, or persistent squamous cell carcinoma of the cervix: a gynecologic oncology group study. J Clin Oncol. 2004;22:3113–9. doi: 10.1200/JCO.2004.04.170. [DOI] [PubMed] [Google Scholar]
- 5.Long HJ, 3rd, Bundy BN, Grendys EC, Jr, Benda JA, McMeekin DS, Sorosky J, Miller DS, Eaton LA, Fiorica JV. Randomized phase III trial of cisplatin with or without topotecan in carcinoma of the uterine cervix: a Gynecologic Oncology Group Study. J Clin Oncol. 2005;23:4626–33. doi: 10.1200/JCO.2005.10.021. [DOI] [PubMed] [Google Scholar]
- 6.Monk BJ, Sill MW, McMeekin DS, Cohn DE, Ramondetta LM, Boardman CH, Benda J, Cella D. Phase III Trial of Four Cisplatin-Containing Doublet Combinations in Stage IVB, Recurrent, or Persistent Cervical Carcinoma: A Gynecologic Oncology Group Study. J Clin Oncol. 2009 Aug 31; doi: 10.1200/JCO.2009.21.8909. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Culy CR, Clemett D, Wiseman LR. Oxaliplatin. A review of its pharmacological properties and clinical efficacy in metastatic colorectal cancer and its potential in other malignancies. Drugs. 2000;60:895–924. doi: 10.2165/00003495-200060040-00005. [DOI] [PubMed] [Google Scholar]
- 8.Cvitkovic E. Ongoing and unsaid on oxaliplatin: the hope. Br J Cancer. 1998;77 4:8–11. doi: 10.1038/bjc.1998.429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thuss-Patience PC, von Minckwitz G, Kretzschmar A, Loibl S, Schaller G, Dorken B, Reichardt P. Oxaliplatin and 5-fluorouracil for heavily pretreated metastatic breast cancer: a preliminary phase II study. Anticancer Drugs. 2003;14:549–53. doi: 10.1097/00001813-200308000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Cortinovis D, Bidoli P, Zilembo N, Fusi A, Bajetta E. Oxaliplatin doublets in non-small cell lung cancer: a literature review. Lung Cancer. 2008;60:325–31. doi: 10.1016/j.lungcan.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 11.Tomek S, Manegold C. Chemotherapy for malignant pleural mesothelioma: past results and recent developments. Lung Cancer. 2004;45 1:S103–19. doi: 10.1016/j.lungcan.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 12.Machover D, Delmas-Marsalet B, Misra SC, Gumus Y, Goldschmidt E, Schilf A, Frenoy N, Emile JF, Debuire B, Guettier C, Farrokhi P, Boulefdaoui B, Norol F, Parquet N, Ulusakarya A, Jasmin C. Dexamethasone, high-dose cytarabine, and oxaliplatin (DHAOx) as salvage treatment for patients with initially refractory or relapsed non-Hodgkin's lymphoma. Ann Oncol. 2001;12:1439–43. doi: 10.1023/a:1012501305214. [DOI] [PubMed] [Google Scholar]
- 13.Faivre S, Kalla S, Cvitkovic E, Bourdon O, Hauteville D, Dourte LM, Bensmaine MA, Itzhaki M, Marty M, Extra JM. Oxaliplatin and paclitaxel combination in patients with platinum-pretreated ovarian carcinoma: an investigator-originated compassionate-use experience. Ann Oncol. 1999;10:1125–8. doi: 10.1023/a:1008334215414. [DOI] [PubMed] [Google Scholar]
- 14.Winegarden JD, Mauer AM, Otterson GA, Rudin CM, Villalona-Calero MA, Lanzotti VJ, Szeto L, Kasza K, Hoffman PC, Vokes EE. A phase II study of oxaliplatin and paclitaxel in patients with advanced non-small-cell lung cancer. Ann Oncol. 2004;15:915–20. doi: 10.1093/annonc/mdh215. [DOI] [PubMed] [Google Scholar]
- 15.NCCN Clinical Practice Guidelines. [7/6/09]; http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- 16.Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG. New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst. 2000;92(3):205–16. doi: 10.1093/jnci/92.3.205. [DOI] [PubMed] [Google Scholar]
- 17.Simon R. Optimal two-stage designs for phase II clinical trials. Control Clin Trials. 1989;10:1–10. doi: 10.1016/0197-2456(89)90015-9. [DOI] [PubMed] [Google Scholar]
- 18.Kuo DYS, Kobrinsky B, Christos P, Blank S, Caputo T, Runowicz CD, Pothuri B, Ivy PS, Muggia F, Wadler S. Oxaliplatin plus paclitaxel in first-line for recurrent and metastatic cervical cancer. J Clin Oncol, ASCO Annual Meeting Proceedings Part I. 2007;25(No 18S June 20 Supplement):5549. [Google Scholar]
- 19.NCI Alert for the use of concomitant chemoradiotherapy. [7/6/09]; In; http://www.cancer.gov/newscenter/cervicalcancer.
- 20.Stordal B, Pavlakis N, Davey R. A systematic review of platinum and taxane resistance from bench to clinic: an inverse relationship. Cancer Treat Rev. 2007;33(8):688–703. doi: 10.1016/j.ctrv.2007.07.013. [DOI] [PubMed] [Google Scholar]
- 21.Long HJ., 3rd Discussion of Abstract # 27: Paclitaxel Plus Oxaliplatin for Recurrent or Metastatic Cervical Cancer: A New York Cancer Consortium Study. Gynecol Oncol. 2009;112(2):S15. doi: 10.1016/j.ygyno.2009.10.082. [DOI] [PMC free article] [PubMed] [Google Scholar]


