Abstract
Aims
The association between depression and substance dependence is poorly understood; examinations of these two disorders over time during key developmental periods can provide insight into how these problems relate to each other. The goal of the present study was to examine longitudinal associations between depression and substance (alcohol and illicit drug) dependence during the period from adolescence through early adulthood.
Participants
Participants in the Minnesota Twin Family Study, a community-based sample of 1252 youth and their families, were used. Youth were first assessed at age 17; they returned to the study at ages 20 and 24.
Measurements
Major depression and drug and alcohol dependence were assessed via structured interviews. Gender was examined as a possible moderator.
Findings
The results indicated that both substance dependence and depression showed stability over time—that is, each disorder was associated with increased risk for the same disorder later. Substance dependence between ages 17 and 20 predicted increased risk of depression between ages 20 and 24. These associations did not differ significantly by gender.
Conclusions
Substance dependence during late adolescence predicts the subsequent occurrence of major depression.
Keywords: major depression, substance dependence, longitudinal, alcohol, drugs
The transition from adolescence to early adulthood is marked by changing demands and multiple adjustments; therefore, it is not surprising that many forms of psychopathology frequently have onsets during this period. Many people with major depressive disorder (MDD) experience their first depressive episodes during this period (Kim-Cohen et al., 2003), and the highest rates of alcohol abuse and dependence are found among 18- to 23-year-olds (Harford et al., 2005). The goal of the present study was to examine how MDD and drug and alcohol dependence (DAD) are associated during the transition from adolescence to early adulthood.
Theoretical considerations have linked MDD to substance use disorders (SUDs), with the concept of “negative affect alcoholism” dating back several decades (Zucker, 1987, 2003). Substances may be used by people with depressive feelings to help them cope (“self-medication”). SUDs may predispose people to MDD, either through physiological effects of the substance or because the consequences of problem use (e.g., family problems) may be depressing. Alternatively, both MDD and SUDs may be different expressions of an underlying risk factor (e.g., difficulty with emotion regulation), a shared comorbid condition (e.g., conduct disorder), or a shared genetic diathesis (Nurnberger et al., 2002); if this is the case, either disorder could appear first.
Overall, evidence has supported the notion that there is an association between these two types of problems (Swendsen and Merikangas, 2000). Previous research has indicated that MDD predicts substance problems (Costello et al., 1999; Dixit and Crum, 2000; Kumpulainen, 2000). Other studies have found that substance problems predict MDD (Bovasso, 2001; Bukstein et al., 1992; Hovens et al., 1994; Rao et al., 2000; Rohde et al., 2001; Stice et al., 2004) and a number of studies have found that MDD predicts substance problems and substance problems predict MDD (Clark et al., 1997; Deykin et al., 1992; Hartka et al., 1991; Hettema et al., 2003). The magnitude of effect—in either or both directions—varies substantially across these studies. Thus, previous research has yielded inconsistent results. This may be related to the fact that some of these previous studies are limited by their retrospective nature, their use of clinic-based samples, and/or their use of samples that vary substantially in age (which may be important if the association between MDD and SUDs varies at different points in development).
There are several potential factors that could account for these discrepant findings. First, there may be a difference in associations between depression and substance involvement when diagnoses versus symptoms (depression) or use (of substances) is considered. When SUDs (abuse and dependence) and depressive diagnoses are considered, the weight of the evidence points to SUDs predicting depressive disorders, both among adolescents (including those followed into their early 20's; Bukstein et al., 1992; Rao et al; Rohde et al., 2001; Stice et al., 2004) and among adults (Bovasso, 2001; Hettema et al., 2003; but see Abraham & Fava, 1999). When heavy use of substances is considered, however, it appears that depression (or depressive symptoms) frequently predicts heavy use among both adolescents (Kumpulainen, 2000) and adults (Dixit & Crum, 2000; Hartka et al., 1991).
Second, these associations may differ by age. There is some indication that depression predicts substance problems and substance problems predict depression among young people (in early to mid-adolescence; Stice et al., 2004). By contrast, from late adolescence to early adulthood, substance problems may predict depression but not the reverse (Rao et al., 2000). In addition, the results of other studies are consistent with the possibility that there may be closer associations between these problems among younger people: (1) adolescent-onset SUDs are more strongly related to depression than adult-onset SUDs (Clark et al., 1998); (2) among males, persistent internalizing problems predict persistent substance use in preadolescence, but not during adolescence (Loeber et al., 1999); and (3) among males, depressive symptoms among 13-year-olds are associated with concurrent alcohol use but not change in alcohol use over time (White, Xie, Thompson, Loeber, & Stouthamer-Loeber, 2001).
Third, these associations may differ by gender. Several studies have found that MDD and SUDs are more closely related in females than males (Bukstein et al., 1992; Clark et al., 1997; Deykin et al., 1992; Hartka et al., 1991). However, some studies have found close associations among males (Costello et al., 1999; Henry et al., 1993). In addition, several studies have found no gender differences in the associations between MDD and SUDs (Hettema et al., 2003; Marmorstein & Iacono, 2003; Rohde et al., 2001). When longitudinal evidence regarding gender differences is examined, patterns are not clear but it seems possible that SUDs may more commonly precede MDD in males, while MDD may be equally likely to precede or follow SUDs in females (Clark et al., 1997; Hettema et al., 2003).
The aim of the present study was to examine longitudinal associations between MDD and DAD from late adolescence through early adulthood. Although cross-sectional associations between these disorders were examined and considered likely to be present (i.e., at any given time, it was expected that MDD and DAD would be associated), cross-lag associations (MDD predicting DAD over time and vice-versa) were the primary focus. Gender was considered as a potential moderator of these associations. This study filled several gaps in the literature. Using a community-based sample, we focused on diagnoses of DAD and MDD, derived from structured interviews (in contrast to many community-based studies, which rely on questionnaire self-reports of symptoms). We chose to focus on these clinically significant—i.e., diagnosable—disorders, thereby providing a picture of how these DSM disorders (as opposed to depressed moods or substance use patterns) relate over time. Another way in which this study filled a gap in the literature was through its use of participants who were all approximately the same age at each assessment, thus anchoring the effects to particular developmental periods spanning late adolescence and emerging adulthood. We also directly examined potential gender differences (instead of using a sample comprised of only one gender, or analyzing males and females separately, as some studies have done).
Hypotheses were developed based on the literature and theoretical considerations discussed above (both of which point to reasons why DAD may predict MDD as well as why MDD may predict DAD). We hypothesized that that MDD would predict DAD and that DAD would predict MDD across the time period from late adolescence through early adulthood. If developmental differences were found, based on findings to date (Clark et al., 1998; Stice et al., 2004; and Rao et al., 2000), it was expected that these effects would be stronger at younger, compared with older, ages. Because studies have been inconsistent with regard to gender differences we made no prediction about gender effects.
Methods
Participants
Participants were drawn from the community-based sample of the Minnesota Twin Family Study, a longitudinal study of twins and their families. All twins born during specified birth years (males: 1971-1976; females: 1975-1979) in the state of Minnesota were identified and considered for participation; after excluding those twins who were adopted, mentally retarded, or otherwise did not meet inclusion criteria, over 82% of those identified participated in the study. Twins were approximately 17 years old at the time of their enrollment in the study (mean=17.5 [SD=.4] for males; mean=17.5 [SD=.5] for females); 578 males and 674 females were assessed at this time. Participants were subsequently invited to return to the study at ages 20 (mean=20.7 [SD=.5] for males; mean=20.7 [SD=.6] for females) and 24 (mean=24.3 [SD=1.0] for males; mean=25.1 [SD=.7] for females). At age 20, 83% of males and 94% of females returned, while at age 24, 92% of the original sample of males and 94% of the original sample of females returned. Informed consent (of parents and adult participants) and assent (of minor participants at the first assessment) were obtained, and this study was approved by the University of Minnesota Institutional Review Board.
As expected given the demographic make-up of Minnesota at the time the twins were born, the sample was overwhelmingly (approximately 98%) white. Average socioeconomic status levels corresponded to parental occupations such as clerical and sales workers and small business owners. Details regarding this sample and design of the study are provided elsewhere (Iacono et al., 1999; Iacono and McGue 2002).
Measures
Major Depressive Disorder (MDD). MDD was assessed via structured interviews (the Structured Clinical Interview for the DSM-III-R [SCID; Spitzer et al., 1987]). At age 17, lifetime diagnoses (those occurring at any point in the participants’ lives) were used; at ages 20 and 24, MDD that may have occurred during the last 3-4 years (since the last assessment) were assessed. DSM-III-R criteria were used because that was the diagnostic system in use at the time of the first assessment; only definite (meeting all DSM-III-R criteria) diagnoses were used. The organic mood disorder and bereavement rule-outs were applied, so all episodes of MDD occurred in the absence of clear organic causes or the recent death of a close relation.
Drug and Alcohol Dependence (DAD). Alcohol and illicit drug dependence were assessed at each time point via structured interviews (the Substance Abuse Module [Robins et al., 1987], a supplement to the Composite International Diagnostic Interview (CIDI; Robins et al., 1988). If a participant met criteria for a definite (all DSM-III-R criteria) diagnosis of dependence on alcohol or an illicit drug, he or she was considered to have DAD. At age 17, disorders occurring at any point in the participants’ lives were assessed; at ages 20 and 24, disorders that may have occurred since the last assessment (during the last 3-4 years) were assessed.
Statistical Analyses
In order to address our hypothesis about how one disorder precedes the subsequent occurrence of the other from age 17 to age 24, our primary analyses consisted of cross-lag “panel” analyses in Mplus software (Muthen and Muthen, 1998), using logistic regression to model the relationship between MDD and DAD over time. This allowed us to simultaneously model the period from 17-20 and the period from 20-24, allowing for a general examination of these associations and an examination of developmental differences (i.e., whether the prediction during one of these periods was stronger than the prediction during the other period). In such models, each measure is expressed as a function of both measures at the previous time point. For instance, MDD at 20 is predicted by MDD and DAD at 17. In this type of model, any association between age-17 and age-24 disorders is completely mediated by age-20 status; the regression paths “go through” the intermediate assessment age. We also fit two variants of this primary model, in order to examine which fit the data best. First, as a baseline, we fit a model in which all regression paths were estimated: each age-24 disorder was predicted by status on each disorder at the two previous assessments, including age 17, and each age-20 disorder was predicted by status on the two age-17 disorders (as in the cross-lag model). Second, we fit a variant of the standard cross-lag model which included additional paths from age 17 to age 24 for each disorder because preliminary examination of the pattern of data (described below) suggested that this might be warranted. This allowed for direct effects of age-17 status on age-24 status for the same disorder, independent of age-20 status.
To investigate sex differences, for all three models, we derived separate regression coefficients for males and females and then constrained them equal across sexes as a test of sex differences in the magnitude of associations over time. We examined two different information criteria to adjudicate between the two models: Schwartz's Bayesian Information Criterion (BIC; Schwarz, 1978), and Draper's Information Criterion (DIC; Draper, 1995). These employ a penalty of varying strength for the number of parameters being estimated and thus favor model parsimony to different degrees.
Dichotomous dependent variables are treated in Mplus as latent variables, with a continuum of liability underlying the observed variable. A threshold on the underlying continuum divides those with the disorder from those without it. Thresholds were allowed to vary between males and females and across time in order to capture sex differences and variation over time in the prevalence of the two disorders. Because the sample consisted of twins (nonindependent observations), we treated individuals as nested within twin pairs, using Mplus's complex sampling method for estimating standard errors in data with a nested structure (cf. Muthén & Satorra, 1995). Due to the longitudinal nature of the assessment, some individuals were missing data on at least one measure. Mplus uses a full information maximum likelihood approach (via numerical integration in this case) to accommodate missing data for this type of model, rather than by deleting data casewise. When data are missing at random (MAR), this approach is more appropriate than casewise deletion, which is biased (Little & Rubin, 1987). MAR cannot be known unambiguously from the data (Allison, 2002). Yet deleting data casewise (which resulted in losing nearly 300 subjects) yielded very similar results. Because casewise deletion requires a stronger assumption about the mechanism behind missing data than MAR, we felt that the MAR assumption was appropriate.
Results
Table 1 presents the prevalence of DAD and MDD during the three age periods for the sample overall, and for males and females separately.
Table 1.
Prevalence of drug and alcohol dependence (DAD) and major depressive disorder (MDD) at different ages.
| By Age 17 | Age 17-Age 20 | Age 20-Age 24 | |
|---|---|---|---|
| Drug and Alcohol Dependence | 9.0% | 17.8% | 17.5% |
| Males | 11.3% | 27.1% | 26.7% |
| Females | 6.9% | 10.8% | 8.9% |
| Major Depressive Disorder | 6.5% | 5.4% | 9.9% |
| Males | 2.8% | 2.7% | 5.6% |
| Females | 9.7% | 7.5% | 13.7% |
Table 2 presents conditional probabilities of each disorder at the two follow-up assessments as a function of: (1) the same disorder at previous age periods, and (2) the other disorder at previous age periods. Table 3 presents the information in the form of odds ratios, representing the relative odds of an outcome disorder at a given follow-up assessment for those with and without each disorder at the previous assessment. Based on these two tables, several findings are evident. Based on the results in the top half of each table, it is clear that MDD at an earlier age is associated with increased risk for subsequent MDD, especially for females. For example, in Table 2, females without MDD at age 17 have a .057 risk of developing it by age 20, but for those with MDD at 17, the risk jumps threefold to .190. From Table 3, we can see that the corresponding OR for this increased risk is 3.88. This pattern was significant across all ages for females, but not significant for the smaller depressed male sample. Substance dependence at an earlier age also was related to subsequent MDD, but only the OR for female DAD at 20 predicting MDD at 24 was significant (OR=3.23). Turning to the bottom half of each table, it is clear that DAD at an earlier age is associated with increased risk for subsequent DAD. For example, in Table 2, females without DAD at 17 have a .077 risk of developing it by age 20, but for those with DAD at 17, the risk jumps sixfold to .487. The corresponding OR for this increased risk is 11.38 (based on Table 3). This pattern was significant for both males and females at all age periods. MDD only significantly predicted later DAD in one case: for females from 20 to 24 (OR=4.43 from Table 3).
Table 2.
Proportion of participants with MDD and DAD at the follow-up assessments, as a function of either diagnosis at the preceding assessments.
| MDD at 20 |
MDD at 24 |
|||
|---|---|---|---|---|
| Diagnostic status | Males | Females | Males | Females |
| Immediately preceding assessment | ||||
| MDD | .091 (11) | .190 (58) | .083 (12) | .600 (40) |
| No MDD | .024 (460) | .057 (561) | .052 (407) | .095 (463) |
| DAD | .059 (51) | .132 (38) | .082 (110) | .302 (53) |
| No DAD | .021 (424) | .068 (584) | .042 (312) | .118 (451) |
| Age-17 assessment | ||||
| MDD | – | – | .182 (11) | .370 (54) |
| No MDD | – | – | .052 (445) | .106 (455) |
| DAD at 20 |
DAD at 24 |
|||
|---|---|---|---|---|
| Diagnostic status | Males | Females | Males | Females |
| Immediately preceding assessment | ||||
| DAD | .686 (51) | .487 (39) | .530 (117) | .518 (54) |
| No DAD | .220 (427) | .077 (584) | .132 (319) | .037 (460) |
| MDD | .182 (11) | .170 (59) | .333 (12) | .256 (43) |
| No MDD | .269 (464) | .091 (561) | .233 (421) | .072 (470) |
| Age-17 assessment | ||||
| DAD | – | – | .596 (57) | .394 (33) |
| No DAD | – | – | .222 (436) | .065 (490) |
Note: Numbers represent the proportion of subjects with a diagnosis at the follow-up assessment, with the total number of subjects for that cell in parentheses. Thus, for the cell labeled “Males” under “MDD at 20” in the row “MDD,” the number 11 gives the total number of male subjects with MDD at age 17. Nine percent of them (1) had a diagnosis of MDD again at 20.
Table 3.
Odds ratios (95% confidence intervals) representing continuity in each diagnosis and risk due to the other diagnosis.1
| MDD at 20 | MDD at 24 | |||
|---|---|---|---|---|
| Diagnostic status | Males | Females | Males | Females |
| Immediately preceding assessment | ||||
| MDD relative to No MDD | 3.48 (0.41-29.19) |
3.88 (1.83-8.19) |
5.93 (0.20-13.43) |
8.23 (4.12-16.42) |
| DAD relative to No DAD | 2.12 (0.76-11.17) |
2.08 (0.77-5.63) |
2.03 (0.85-4.90) |
3.23 (1.68-6.21) |
| Age-17 assessment | ||||
| MDD at 17 relative to No MDD | -- | -- | 4.06 (0.83-19.85) |
4.95 (2.64-9.28) |
| DAD at 20 |
DAD at 24 |
|||
|---|---|---|---|---|
| Diagnostic status | Males | Females | Males | Females |
| DAD relative to No DAD | 7.75 (4.11-14.60) |
11.38 (5.66-22.86) |
7.42 (4.56-12.06) |
27.97 (13.61-57.50) |
| MDD relative to No MDD | 0.60 (0.13-2.84) |
2.05 (0.98-4.28) |
1.64 (0.48-5.58) |
4.43 (2.06-9.57) |
| Age-17 assessment | ||||
| DAD at 17 relative to No DAD | -- | -- | 5.17 (2.86-9.36) |
9.35 (4.26-20.51) |
Standard errors were computed from the four relevant cell sizes and are unadjusted for the lack of independence between members of a twin pair.
These associations, however, were not adjusted for any effects of previous occurrences of MDD or DAD, and as noted above, continuity in MDD and DAD across time was substantial. Therefore, we constructed a longitudinal cross-lag model, described next, which makes this adjustment.
Modeling Longitudinal Associations between MDD and DAD
Table 4 gives fit statistics for the different models. The fit statistics (BIC and DIC) favored a sex-general model, so we used that as our final model. We tested for sex differences in the entire model (all regression pathways) at once, and examination of fit statistics comparing sex-varying and sex-invariant models indicated that this sample size was adequate to detect meaningful sex differences in the overall model. In fact, a sample 5 to more than 13 times larger (i.e., more than 5,000 to nearly 15,000) would have been required for the sex-invariant model to have been preferred by DIC and BIC, respectively. However, it remains possible that subtle sex differences in individual pathways could be present. Monte Carlo simulations designed to assess power to detect sex-specific parameters indicated that our power was quite adequate for the vast majority of the 20 regression parameters; specifically, power was greater than .65 for 17 of the 20 parameters. Nevertheless, this was not true in every case and it is therefore possible that there are true sex differences in the magnitude of a few parameters. However, this analysis was aimed at assessing overarching sex differences in links between MDD and DAD during this time period. These power analyses indicate that we can be confident that there are no dramatic sex differences in these associations--if any true sex differences are present, they are small in magnitude.
Table 4.
Fit statistics for logistic regression models.
| Model | Log Likelihood | Number of parameters | DIC | BIC |
|---|---|---|---|---|
| All paths estimated | −2037.0 | 33 | 4246.6 | 4306.9 |
| All paths, no sex differences | −2047.9 | 21 | 4205.6 | 4244.0 |
| Age 17-age 24 continuity | −2038.7 | 29 | 4229.1 | 4282.1 |
| Age 17-age 24 continuity, no sex differences | −2049.2 | 19 | 4197.8 | 4232.6 |
| Standard cross-lag | −2051.2 | 25 | 4233.2 | 4278.8 |
| Standard cross-lag, no sex differences | −2061.7 | 17 | 4212.3 | 4243.5 |
Note: Number of parameters is the number of freely estimated parameters in the model; BIC is Schwartz's Bayesian Information Criterion; DIC is Draper's Information Criterion. For all information criteria, smaller values indicate better fit. Bold type indicates the best-fitting model by each fit statistic. The “all paths estimated” model includes all regression paths (each age-24 disorder predicted by status on each disorder at the two previous assessments, and each age-20 disorder predicted by status on the two age-17 disorders) and allows for different models for males and females. The “all paths estimated, no sex differences” model is the same except it does not allow for sex differences in the paths. The “age 17-age 24 continuity” model is like the standard cross-lag model (in which any association between age-17 and age-24 disorders is completely mediated by age-20 status) except it also includes direct paths from MDD at 17 to MDD at 24 and from DAD at 17 to DAD at 24; it allows for different models for males and females. The “age 17-age 24 continuity, no sex differences model” is the same except it does not allow for sex differences in the paths. The “standard cross-lag” model assumes that any association between age-17 and age-24 disorders is completely mediated by age-20 status (the regression paths “go through” the intermediate assessment age); it allows for different models for males and females. The “standard cross-lag, no sex differences” model is the same except it does not allow for sex differences in the paths.
This final model included all cross-lag and continuity paths along with direct paths from age-17 status to status on the same disorder at age 24, with paths constrained equal for males and females. This indicates that a direct effect of diagnostic status at age 17 on status for the same disorder at age 24 was warranted for each disorder, and that sex differences in the magnitude of regression paths were not significant.
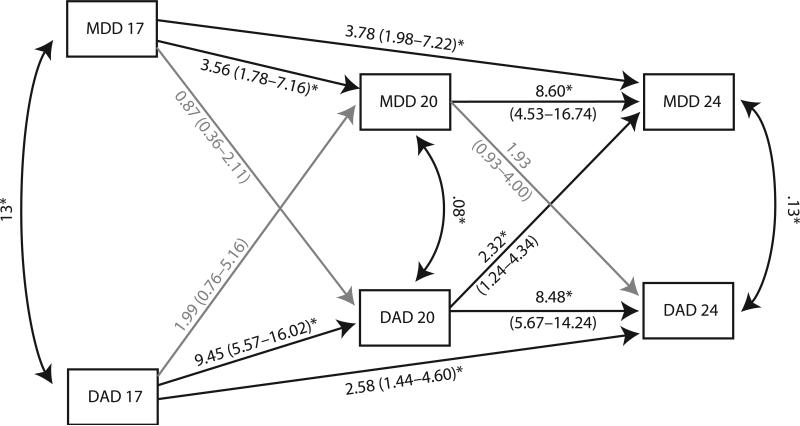
Results of the best-fitting model are presented graphically in Figure 1. Regression paths are represented by directional, single-headed arrows. Non-significant paths are shaded light gray. These are accompanied by odds ratios, with 95% confidence intervals in parentheses, which give the odds of the outcome disorder (the disorder being predicted) for those with the disorder predicting it (MDD or DAD at the previous time point) relative to those without the predictor disorder. These odds ratios are adjusted for all other components in the model, as well as for the presence of twins (correlated observations) in the sample. Although not part of the model, concurrent correlations between MDD and DAD are given (in the form of Phi correlations).
Figure 1. Longitudinal associations between major depressive disorder and substance dependence.
Values printed along straight, directional arrows represent odds ratios, with 95% confidence intervals in parentheses. Values next to the curved arrows connecting MDD and DAD at each age are Pearson correlations between the disorders. MDD=major depressive disorder; DAD=drug and alcohol dependence.
Echoing the results presented in Tables 2 and 3, all stability associations were significant. This indicates that, independent of presence of the other disorder, the presence of each problem at an earlier time point was associated with increased odds of the same problem at a later time point. Continuity in DAD was somewhat greater than continuity in MDD, which is consistent with the observed data presented in Tables 2 and 3, though it should be noted that the confidence intervals overlap and therefore this difference is not large. On the other hand, the direct effect of age-17 status on age-24 status was somewhat greater for MDD than for DAD (though again, the confidence intervals overlap), which is consistent with MDD being more episodic than DAD.
Turning to the cross-lag effects, after adjusting for earlier occurrences of each disorder, DAD between 17 and 20 was associated with significantly increased risk for MDD between 20 and 24. Although DAD prior to age 17 was associated with an approximately doubled risk for MDD between 17 and 20, this effect was not statistically significant. MDD at earlier ages did not significantly predict later DAD (though there was a somewhat elevated risk for later DAD among people who had MDD between 17 and 20).
Discussion
Inspection of tables 2 and 3 and Figure 1 point to 3 key findings. First, DAD between 17 and 20 significantly predicted increased risk for MDD between 20 and 24, even once continuity effects in these disorders are adjusted for. In addition, DAD by age 17 was associated with approximately twofold increased risk for MDD between 17 and 20, though this effect was not statistically significant. Second, both DAD and MDD exhibit significant continuity from early adolescence through early adulthood, and the occurrence of either disorder during adolescence predicts it again in early adulthood, even net the effect of its (possible) occurrence in late adolescence. Third, these associations did not differ significantly by gender.
There are several reasons that DAD could predict depression during the period from late adolescence to early adulthood. First, the physiological effects of heavy substance use might render people susceptible to depression. If this is the case, it is not clear why this association was significant for one developmental period but not at earlier ages; perhaps, because many youth move out of their parents’ home between 17 and 20 and are therefore under less supervision than they had been prior to age 17, their substance problems may involve even heavier use than earlier substance problems and this could cause physiological changes that place them at especially increased risk for depression. Second, the negative consequences of substance dependence could precipitate a depressive episode. There are numerous potential consequences that could do so, ranging from failing out of college to difficulty keeping a job to increased family conflict to trouble with the law. A thorough examination of these potential mediating factors would be a useful goal of future research. Interestingly, the results of this study imply that stressors arising due to substance problems between 17 and 20 are more likely to result in depression than those stressors that occur earlier; this could be due to the nature or severity of the stressors, or to the life challenges that occur during this period (transitioning to post-high school education or a job, living on one's own for the first time). Third, late adolescents who use substances heavily may fail to develop adaptive ways of coping with negative emotions and life stress; when they encounter the additional stress associated with adulthood, they may not be able to cope adaptively and this may precipitate a depressive episode. Further research examining the reasons behind these associations—and specifically attempting to clarify whether they are present consistently over development or whether they are stronger during some developmental periods than others—would be useful.
The results of this study also speak to the stability of these disorders over time. For both DAD and MDD, having the disorder during an earlier time period predicted its occurrence during a later time period. This was true both for contiguous (pre-17 to 17-20 and 17-20 to 20-24) and non-contiguous (pre-17 to 20-24) time periods, indicating that having one of these disorders predicts having it again later, even if it does not recur or continue immediately. There was some indication that these continuity effects may have been stronger for DAD, perhaps due to the episodic nature of MDD; however, the overlap in the stability confidence intervals across these two disorders indicates that any differences that may be present are slight.
DAD and MDD were modestly but significantly associated with each other at 17, 20 and 24. This confirms the findings of previous studies indicating that there are cross-sectional associations between these two disorders.
The finding that path coefficients could be constrained equal across gender indicates that despite differences in prevalence of these disorders (and possibly small differences in the stability of disorders, as illustrated in Tables 2 and 3), the overall associations between these disorders across time are not significantly different for males and females. It should be noted, however, that when simple odds ratios were examined, MDD between 17 and 20 predicted DAD from 20-24 among females only (odds ratio=4.4; Table 3) and DAD between 17 and 20 predicted MDD from 20-24 among females only (odds ratio=3.2; Table 3). These factors suggest the possibility of subtle sex differences that the overall model failed to capture. Future research examining individuals’ trajectories of symptoms over time will be informative in further explaining these associations for both males and females.
In addition to these primary findings, there was a somewhat elevated risk for DAD at 24 among people with MDD at 20; the odds ratio representing this increase in risk was significant for females. However, this association was non-significant following adjustment for prior disorders. Despite this, the overall increase in risk raises the possibility that at relatively later developmental stages, and/or among females, there may be a significant MDD-to-DAD pathway. Future research examining this possibility, perhaps with more closely spaced assessments and/or over a longer time period, would be useful.
Particular strengths of this study included its community-based sample (thereby avoiding the biases associated with treatment-seeking samples); its focus on diagnoses of DAD and MDD, derived from structured interviews; its use of participants who were all the same age at each assessment (allowing for interpretation of developmental effects linked to narrowly defined age intervals covering the transition form adolescence to early adulthood); and its direct analysis of potential gender effects. Of course, this study has limitations. The sample is predominantly Caucasian; although based on census data they were representative of the population of families with at least one child in the state of Minnesota at the time the adolescent participants were born (Holdcraft & Iacono, 2005), it is not known how well these findings would generalize to other groups. We used DSM-III-R diagnostic criteria; although cases of substance-induced depressive disorder were eliminated, it is not clear whether or how using the DSM-IV criteria would have affected our results. In particular, the DSM-IV requirement that clinically significant impairment or distress be present may affect the prevalence and/or implications of the diagnoses. In addition, substance problems, once they emerge, are likely to wax and wane over time, whereas major depression is conceptualized as an episodic disorder, with relatively discrete onsets and offsets. In part because of this, it is difficult to fully understand the processes involved in the relationships found; future research using more closely-spaced assessments, and perhaps tracking both depressive symptoms as well as episodes and substance use as well as dependence diagnoses, would be useful. It is also important to note that the model described in this study is not a causal model; instead, it describes associations between variables over time. For example, we cannot infer that DAD between ages 17 and 20 causes MDD between 20 and 24.
More research into the mechanisms behind this association between DAD and later MDD is necessary. The results of the present study indicate that there may be age/development-specific longitudinal associations between these types of problems, thus highlighting the importance of considering development in examinations of this topic. Investigation into different possible explanations of these findings would provide information regarding the best ways to prevent MDD among young people with DAD and would also help clarify whether or not there are subtle gender and/or developmental differences in these associations.
Acknowledgements
This research was supported by grants AA09367 from the National Institute on Alcohol Abuse and Alcoholism, DA05147 and DA016892 from the National Institute on Drug Abuse, and a research grant from the Alcoholic Beverage Medical Research Foundation.
References
- Abraham HD, Fava M. Order of onset of substance abuse and depression in a sample of depressed outpatients. Compr Psychiatry. 1999;40:44–50. doi: 10.1016/s0010-440x(99)90076-7. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing data. Sage Publications; Thousand Oaks, CA: 2002. [Google Scholar]
- Bovasso GB. Cannabis abuse as a risk factor for depressive symptoms. Am J Psychiatry. 2001;158:2033–2037. doi: 10.1176/appi.ajp.158.12.2033. [DOI] [PubMed] [Google Scholar]
- Bukstein OG, Glancy LJ, Kaminer Y. Patterns of affective comorbidity in a clinical population of dually diagnosed adolescent substance abusers. J Am Acad Child Adolesc Psychiatry. 1992;31:1041–1045. doi: 10.1097/00004583-199211000-00007. [DOI] [PubMed] [Google Scholar]
- Clark DB, Kirisci L, Tarter RE. Adolescent versus adult onset and the development of substance use disorders in males. Drug Alcohol Depend. 1998;49:115–121. doi: 10.1016/s0376-8716(97)00154-3. [DOI] [PubMed] [Google Scholar]
- Clark DB, Pollock N, Bukstein OG, Mezzich AC, Bromberger JT, Donovan JE. Gender and comorbid psychopathology in adolescents with alcohol dependence. J Am Acad Child Adolesc Psychiatry. 1997;36:1195–1203. doi: 10.1097/00004583-199709000-00011. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Federman E, Angold A. Development of psychiatric comorbidity with substance abuse in adolescents: Effects of timing and sex. J Clinical Child Psychol. 1999;28:298–311. doi: 10.1207/S15374424jccp280302. [DOI] [PubMed] [Google Scholar]
- Deykin EY, Buka SL, Zeena TH. Depressive illness among chemically dependent adolescents. Am J Psychiatry. 1992;149:1341–1347. doi: 10.1176/ajp.149.10.1341. [DOI] [PubMed] [Google Scholar]
- Dixit AR, Crum RM. Prospective study of depression and the risk of heavy alcohol use in women. Am J Psychiatry. 2000;157:751–758. doi: 10.1176/appi.ajp.157.5.751. [DOI] [PubMed] [Google Scholar]
- Draper D. Assessment and propagation of model uncertainty. Journal of the Royal Statistical Society: Series B (Methodology) 1995;57:45–97. [Google Scholar]
- Harford TC, Grant BF, Yi H, Chen CM. Patterns of DSM-IV alcohol abuse and dependence criteria among adolescents and adults: Results from the 2001 National Household Survey on Drug Abuse. Alcoholism: Clinical Experimental Res. 2005;29:810–828. doi: 10.1097/01.alc.0000164381.67723.76. [DOI] [PubMed] [Google Scholar]
- Hartka E, Johnstone B, Leino EV, Motoyoshi M, Temple MT, Fillmore KM. A meta-analysis of depressive symptomatology and alcohol consumption over time. Br J Addiction. 1991;86:1283–1298. doi: 10.1111/j.1360-0443.1991.tb01704.x. [DOI] [PubMed] [Google Scholar]
- Henry B, Feehan M, McGee R, et al. The importance of conduct problems and depressive symptoms in predicting adolescent substance use. J Abnorm Child Psychol. 1993;21:469–480. doi: 10.1007/BF00916314. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, Kendler KS. The effects of anxiety, substance use and conduct disorders on risk of major depressive disorder. Psychol Med. 2003;33:1423–1432. doi: 10.1017/s0033291703008365. [DOI] [PubMed] [Google Scholar]
- Holdcraft LC, Iacono WG. Cross-generational effects on gender differences in psychoactive drug abuse and dependence. Drug Alc Depend. 2004;74:147–158. doi: 10.1016/j.drugalcdep.2003.11.016. [DOI] [PubMed] [Google Scholar]
- Hovens JGFM, Cantwell DP, Kiriakos R. Psychiatric comorbidity in hospitalized adolescent substance abusers. J Am Acad Child Adoles Psychiatry. 1994;33:476–483. doi: 10.1097/00004583-199405000-00005. [DOI] [PubMed] [Google Scholar]
- Iacono WG, Carlson SR, Taylor J, Elkins IJ, McGue M. Behavioral disinhibition and the development of substance-use disorders: Findings from the Minnesota Twin Family Study. Dev Psychopath. 1999;11:869–900. doi: 10.1017/s0954579499002369. [DOI] [PubMed] [Google Scholar]
- Iacono WG, McGue M. Minnesota Twin Family Study. Twin Res. 2002;5:482–487. doi: 10.1375/136905202320906327. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington H, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder. Arch Gen Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Kumpulainen K. Psychiatric symptoms and deviance in early adolescence predict heavy alcohol use 3 years later. Addiction. 2000;95:1847–1857. doi: 10.1046/j.1360-0443.2000.9512184713.x. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. Wiley & sons; Hoboken, NJ: 1987. [Google Scholar]
- Loeber R, Stouthamer-Loeber M, White HR. Developmental aspects of delinquency and internalizing problems and their association with persistent juvenile substance use between ages 7 and 18. J Clin Child Psychol. 1999;28:322–332. doi: 10.1207/S15374424jccp280304. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG. Major depression and conduct disorder in a twin sample: Gender, functioning, and risk for future psychopathology. J Am Acad Child Adoles Psychiatry. 2003;42:225–233. doi: 10.1097/00004583-200302000-00017. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user's guide. 3rd ed. Muthén & Muthén; Los Angeles: 19882005. [Google Scholar]
- Muthén BO, Satorra A. Complex sample data in structural equation modeling. Sociological Methodology. 1995;25:267–316. [Google Scholar]
- Nurnberger JI, Foroud T, Flury L, Meyer ET, Wiegand R. Is there a genetic relationship between alcoholism and depression? Alcohol Res Health. 2002;26:233–240. [PMC free article] [PubMed] [Google Scholar]
- Rao U, Daley SE, Hammen C. Relationship between depression and substance use disorders in adolescent women during the transition to adulthood. J Am Acad Child Adoles Psychiatry. 2000;39:215–222. doi: 10.1097/00004583-200002000-00022. [DOI] [PubMed] [Google Scholar]
- Robins LN, Baber T, Cottler LB. Composite International Diagnostic Interview: Expanded Substance Abuse Module. 1987.
- Robins LN, Wing J, Wittchen H-U, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA, Sartorius N, Towle LH. The Composite International Diagnostic Interview. Arch Gen Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Kahler CW, Seeley JR, Brown RA. Natural course of alcohol use disorders from adolescence to young adulthood. J Am Acad Child Adoles Psychiatry. 2001;40:83–90. doi: 10.1097/00004583-200101000-00020. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Annals of Statistics. 1978;6:461–464. [Google Scholar]
- Spitzer RL, Williams JBW, Gibbons M, First MB. Structured Clinical Interview for DSM-III-R (SCID) Biometrics Research Division, New York State Psychiatric Institute; New York: 1987. [Google Scholar]
- Stice E, Burton EM, Shaw H. Prospective relations between bulimic pathology, depression, and substance abuse: Unpacking comorbidity in adolescent girls. J Consult Clin Psychol. 2004;72:62–71. doi: 10.1037/0022-006X.72.1.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20:173–189. doi: 10.1016/s0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- White HR, Xie M, Thompson W, Loeber R, Stouthamer-Loeber M. Psychopathology as a predictor of adolescent drug use trajectories. Psychol Addict Beh. 2001;15:210–218. [PubMed] [Google Scholar]
- Zucker RA. The four alcoholisms: A developmental account of the etiological process. In: Dienstbier RA, Rivers PC, editors. Nebraska Symposium on Motivation 1986: Alcohol and Addictive Behavior. 1987. pp. 27–83. [PubMed] [Google Scholar]
- Zucker RA. Causal structure of alcohol use and problems in early life: Multilevel etiology and implications for prevention. In: Biglan A, Wang MC, Walberg HJ, editors. Preventing Youth Problems. pp. 33–62. [Google Scholar]