Abstract
This study identified patterns of alcohol and other drug (AOD) involvement during the decade following adolescent AOD treatment and developmental outcomes in emerging adulthood. AOD and psychosocial variables were assessed at 8 time points from adolescence into adulthood (n = 153; 41.2% women) in an inpatient treatment sample of alcohol and other drug dependent teens. Latent class growth analysis identified six trajectories based on alcohol and substance use frequency which were consistent with developmental transitions and validated by measures of dependency symptoms. While few differences were evident at intake, the educational, occupational and interpersonal attainments were differentially associated with the alcohol/drug trajectories as youth transitioned into adulthood. High rates of high school graduation (71.1%), professional occupations (45.2%), marriage/cohabitation (48.5%), and financial responsibility for children (F[5,27] = 2.75, p=.02) were evident for those with the least alcohol and drug involvement. More severe drug use trajectories were associated with higher rates of dependence, incarceration and more treatment at the final period of assessment. Outcomes of the trajectory of frequent alcohol involvement were distinct from combined alcohol and drug use. These findings highlight the long term diversity of substance use outcomes following adolescent treatment and suggest that identification of these patterns of use following treatment can help clarify the developmental impact of youth alcohol and drug use on outcomes in young adulthood.
Keywords: Adolescence, substance use, trajectories, relapse, longitudinal
1. Introduction
Although it is becoming increasingly clear that heavy alcohol and drug (AOD) involvement during adolescence carries substantial risk (Brown and Ramo, 2006; Spear, 2004), little is known of the adult outcomes of youth treated for alcohol and drug use disorders (A/SUDs). Past investigations have shown that adolescents treated for A/SUDs return to substance use at rates consistent with their adult counterparts (e.g., Brown et al., 1990; Chung and Maisto, 2006; Cornelius et al., 2001; Latimer et al., 2000). While similar in rates of return to use, the impact of AOD use after treatment are different for youth (Brown, 2004; Schulenberg et al., 1996) and may have far reaching developmental consequences (Brown et al., 2008). While advances have been made in characterization of long term substance involvement patterns and its impact on youth in community samples (e.g., Schulenberg and Maggs, 2002), little is known regarding the unfolding patterns of alcohol and drug use and impact on development for youth who received treatment for A/SUDs.
The vast majority of the existing work examining trajectories of AOD involvement in teens after treatment has focused on the early period after treatment (e.g., 1 year: Chung et al., 2004; Chung et al., 2005; 3 years: Chung et al., 2008; 2.5 years: Godley et al., 2004). For example, in a longitudinal study, Chung and colleagues (2008) used latent class growth modeling to characterize patterns of alcohol, marijuana and other drug dependence symptoms across 3 years in adolescents who had experienced a treatment episode (in- or outpatient). They identified six classes for alcohol and marijuana symptoms including Low Improver (or No Symptoms [Marijuana]), High Improver, Stable Low, Moderate Improver, Increasing and Stable High. Four trajectories emerged for other drug symptoms representing No Symptoms, Improving, Increasing, and Stable High. To a large degree, these patterns were concordant across individuals assigned to these classes (only one of four subtypes were discordant). Subtypes differed on the basis of gender, ethnicity, age, conduct disorder and depression, and the patterns identified demonstrated some consistency across the other studies cited above. These studies demonstrate the usefulness of empirically-based AOD trajectories and highlight the need for longer-term follow-ups to understand the course of substance use into early adulthood.
Examination of longer-term substance use patterns among treated teens has used clinical categorization, rather than empirical strategies such as latent class growth analysis (LCGA). For example, work in our lab has characterized the substance involvement, social and behavioral functioning in the years after treatment (Anderson et al., 2007; Brown et al., 2001; Brown et al., 1994; Chung et al., 2003). Based on quantity/frequency of use and associated problems exhibited over multiple follow-up time points after treatment, youth were clinically categorized into five groups: Abstainers (7%), Users (8%), Slow improvers (10%), Worse with time (27%), and Continuous heavy users (48%; Brown et al., 2001). Based on frequency of use and SUD diagnostic criteria at three follow-up time points up to 5.5 years, Winters and colleagues (2007) found that treated youth had consistently better outcomes than wait list controls, while community controls demonstrated lower substance use than the other two group at all three assessed time points. While this initial conceptual approach to treatment outcome was critical, the latent trajectory approach may further our understanding of both post treatment substance involvement patterns and developmentally important functioning as treated adolescents transition into adulthood.
In an early effort to apply latent growth analysis to classify teens' alcohol use in the 8 years following treatment, Abrantes described four trajectories of teen alcohol patterns in 140 who had an inpatient treatment episode (Chung et al., 2003). Based on these 8-year trajectories, teens were labeled as Abstainers (22%), Infrequent users (24%), Worse with time (36%), and Frequent users (18%). Worse alcohol trajectories were associated with more severe alcohol dependence symptoms, severe drug use, and poorer psychosocial functioning in late adolescence. This longitudinal work underscores the importance of extending the trajectory analysis approach beyond the 8 year period as well as incorporating joint consideration of multiple substances (i.e., marijuana, other drugs) which are so often used in conjunction with alcohol among youth in substance abuse treatment (Substance Abuse and Mental Health Services Administration and Office of Applied Studies, 2007).
This investigation has two primary goals: 1) to identify 10 year patterns of AOD use for youth after treatment for A/SUDs in adolescence, and 2) examine the developmental outcomes for youth expected to best represent these patterns of consumption in young adulthood. For full consideration of long-term outcomes, use of alcohol and other drugs were modeled simultaneously using latent class growth analysis (LCGA). Joint approaches, integrating two separate trajectory models, have been used successfully to characterize the comorbidity between alcohol and tobacco use from late adolescence to young adulthood (Jackson et al., 2005) and 1-year alcohol use and AUD symptomatology for youth after treatment (Chung et al., 2005). Further, we examined demographic characteristics (age, sex and ethnicity) and pretreatment substance use, which have commonly been investigated as predictors or associates of substance use trajectory classes in treatment samples (Brown et al., 1989; Chung and Maisto, 2006; Chung et al., 2004; Latimer et al., 2000; Richter et al., 1991).
Given our interest in understanding the developmental impacts of AOD use across time, we examined how youth with differing longitudinal patterns of AOD involvement following treatment managed the developmental transitions of emerging adulthood. Emerging adulthood, the period of development from 18 to 25 years of age, is characterized by transitions to independent living, educational and occupational attainment, and deeper intimacy in interpersonal relationships (Arnett, 2000; Scales et al., 2003). We targeted the domains of independence (financial/residential), industry (education/work), and intimacy (marriage/family) as indicators of developmental attainment in this investigation. As past research has demonstrated that continued treatment (Kelly et al., 2008; Kelly et al., 2000) and living in environments where alcohol or drugs are difficult to acquire (i.e., juvenile hall, jail) influence post-treatment course (Godley et al., 2004), class differences on these variables were compared at each follow up time point.
Based on recent findings, we expected that an abstaining/nonusing trajectory and chronic use trajectory would emerge across the ten years after treatment (Brown et al., 2001; Chung et al., 2005; Clark et al., 2006). In addition, we expected that developmentally-relevant shifts in use patterns might emerge around developmental transition points identified in past studies, such as the move to independent living and graduations from high school and college (Aseltine and Gore, 2005; Kypri et al., 2004; Zucker et al., 2000) and transition to legal consumption of alcohol (age 21). We also expected that males and younger teens at treatment entry might be more likely to experience more severe patterns of alcohol and drug use engagement (Chung and Maisto, 2006; Wiesner et al., 2007). Consistent with young adult development, patterns characterized by lower levels of AOD use across time were expected to demonstrate higher levels of educational and occupational attainment, age appropriate independence from families-of-origin, and greater intimacy and responsibility within their interpersonal relationships.
2. Methods
2.1 Participants
171 youth (40.9% girls), ages 13–18 years of age, were recruited from alcohol and drug use treatment centers in San Diego County between 1988–1994, as a part of a longitudinal study of adolescent alcohol and drug use treatment outcomes (Brown et al., 1994). Recruited youth had a primary diagnosis of alcohol or substance use disorder without concurrent Axis I psychopathology (DSM-III-R; American Psychiatric Association, 1987) exclusive of conduct disorder (94% with CD symptoms at study intake [m # of symptoms=5.9; sd = 2.5 ]; Brown et al., 2001), and had participated in inpatient treatment, incorporating Alcoholic Anonymous 12-step treatment, individual, family and group psychotherapies. Recruited youth met criteria for either alcohol abuse or dependence and 97% met criteria for dependence on at least one other substance (exclusive of nicotine). The clinical sample was representative of the demographic patterns reflected in the school population of greater San Diego County. After 10 years of participation, 5 were lost to follow up due to death, 2 were incarcerated, and 4 were unable to be contacted; 93% of the original teens and 98% of collateral reporters completed the 10 year assessment. One hundred fifty three participants (89.5% of the total sample; 41.2% women) provided detailed substance use data on at least 6 of 8 occasions from study enrollment across a 10-year period after treatment and were included in these analyses. Individuals missing data on more than two occasions did not differ from included cases on the basis of demographics (sex, ethnicity, SES) or substance use patterns at intake. Intake demographics, substance use patterns and substance use diagnoses of participants are presented in Table 1.
Table 1.
Adolescent Alcohol and Drug Treatment Sample: Demographics, Diagnosis and Use Patterns at Study Intake (n=153).
| Sex | |
| Male | 58% |
| Female | 42% |
| Age | |
| Mean | 15.9 (SD = 1.3) |
| Range | 13.0 –18.0 |
| Ethnicity | |
| Caucasian | 74% |
| Hispanic-American | 6% |
| African-American | 5% |
| Other/Mixed | 15% |
| Socioeconomic Status | |
| Hollingshead Index Mean | 29.9 (SD = 12.6) – Middle class |
| Lifetime Substance Use | |
| Alcohol | 100% |
| Marijuana | 99% |
| Amphetamine | 95% |
| Cocaine | 73% |
| Hallucinogens | 69% |
| Inhalants | 44% |
| Barbiturates | 20% |
| Opiate | 17% |
| Lifetime Substance Dependence diagnoses (DSM-IV) | |
| Alcohol | 61% |
| Marijuana | 59% |
| Stimulant | 52% |
| Hallucinogen | 10% |
| Barbiturate | 1% |
| Inhalants | 1% |
| Opiate | 0% |
Note: Diagnosis was determined by CDDR interviews with teen and parent/guardian. Other ethnicity included Asian-American/Pacific Islanders, Native Americans, and those who self-identified as Other or mixed background.
2.2 Procedures
Recruitment and assessment procedures for this longitudinal study have been published elsewhere (Brown et al., 2001; Brown et al., 1994; Brown et al., 1989). Specific to this investigation, youth and their collateral reporter (parent/guardian in adolescence; domestic partners in adulthood) were separately interviewed at study intake (14 – 21 days in treatment) and at 6 months, 1 year, 2 years, 4 years, 6 years, 8 years and 10 years after study enrollment. After study intake, participants were contacted by phone, mail, and e-mail to schedule each follow up. Participants were interviewed in person (approximately 80%) or by phone (greater than 50 miles from research site) to maximize follow up participation. The structured interviews with each subject and resource person pair were conducted by different interviewers trained to criterion to provide independent corroboration of data and confidentiality. We used a structured method of compositing subject and collateral reported information, counting youth reports of use or problems even when not identified in collateral reports, and more heavy use/heavier consequences were included if objective information (e.g., toxicology screens, public information) verified this.
2.3 Measures
2.3.1 Demographic characteristics and developmental outcomes
A 90-minute confidential structured interview (Brown et al., 1994) was completed separately by adolescents and collaterals to gather demographic and background information and information regarding participant experiences with substance use and related variables. A modified version of this interview was conducted at each follow up time point with the participant and separately with a collateral reporter (e.g., parent, spouse as appropriate) to update the information described above, and to collect new information on subsequent alcohol and drug treatment (inpatient and outpatient), current living environments (i.e., incarceration, independent living), changes in dating/marital status and parenthood, and information on current education, financial and employment status. Socioeconomic status at intake was determined using the Hollingshead Index (Hollingshead, 1965) based on parental education, occupation and income. At 10 years, youth SES was estimated using his/her educational level, occupation and income.
2.3.2 Substance Use
The Customary Drinking and Drug Use Record (CDDR; Brown et al., 1998) was used to assess alcohol (i.e., beer, wine, hard liquor) and drug involvement (i.e., marijuana, amphetamines, barbiturates, hallucinogens, cocaine, inhalants, opiates and other drugs) at all assessment points. The Lifetime Version, given at intake, assessed lifetime use of alcohol and eight types of drugs and the Current Version of the CDDR, given at all follow-up assessments, assessed average 30-day use in the last 3 months. For early time periods of assessment, DSM-III-R classifications of dependence were recoded using DSM-IV criteria sets (APA, 1987, 1994). We used substance dependence symptoms, rather than abuse symptoms, as these are considered a more sensitive measure, and are strongly associated with adverse consequences and common risk factors (e.g., Luczak et al., 2004). The CDDR has demonstrated good internal consistency, test-retest, and interrater reliability, as well as convergent and discriminant validity in adolescents and young adults with AUDs and SUDs (Brown et al., 1998; Stewart and Brown, 1995). A random sample of approximately 15 % of subjects completed urine toxicology screens at each follow up assessment to confirm self-report and reports from collaterals. At each time point of assessment, we had no more than two inconsistencies between self-reported use and biological samples. Approximately half were under reporting (i.e., urinalysis identified a substance not reported), and we took the conservative approach of matching data to the biological findings. In the other half of the cases, participants reported use that was not identified on the toxicology screen. The data were maintained as reported because the participants assumed that they had consumed an active substance.
To form the trajectories, frequency of use was measured at each time point by quantifying the average alcohol use days per month summed across beer, wine and hard liquor in the past 3 month period (0–90). For example, drinking beer on 15 days, wine on 8 days and hard liquor on 20 days per month on average would result in an estimate of 43 drinking experiences/month. The average 30 day drug use episodes summed across the 8 types of substances used per month in the 3 months prior to assessment (0–240; e.g., marijuana 20 days + cocaine 10 days + LSD 5 days = 35 uses/month). Maximum number of drinks per episode (i.e., the largest amount of alcohol consumed during one use episode) was a composite of the three types of alcoholic beverages (beer, wine, hard liquor) consumed in the episode. Heavy episodic drinking was defined as drinking more than 4[women]/5[men] drinks in an episode in the preceding 3-month period. Marijuana use, other drug use, and polydrug use were examined using marijuana, other drugs (any of the 7 substances), and using multiple drugs in the same use episode at least once in the preceding 3 month period, respectively.
2.4 Analytic Strategy
Latent class growth analysis (LCGA; Muthén, 2001; Nagin, 2005) was used to describe the longitudinal patterns of alcohol and other substance use in this sample. In practice, LCGA creates classes of individual growth trajectory patterns (Muthèn and Muthèn, 2000). In LCGA, and within growth mixture models generally, a latent categorical variable is specified for the model that represents a set of trajectory classes. Each class' expected developmental trajectory takes on a unique and, in many cases, distinct form; each has its own set of parameter estimates for the model that describes the functional form of the expected developmental trajectory. LCGA can model the influence of covariates such as baseline characteristics (e.g., sex, age, ethnicity), while simultaneously determining the class structure (Muthèn and Muthèn, 2000). However, this modifies the expression of the trajectories as a function of these personal characteristics. As our primary goal was to better understand the patterns of post treatment substance use in this sample, a constrained dual trajectory model (Brame et al., 2001) was implemented whereby the combined developmental course of alcohol use frequency and substance use frequency at 7 time points was modeled without initial inclusion of covariates. Baseline characteristics and functioning were subsequently examined after specification of classes. The LCGA included data from assessments at 6 months and 1, 2, 4, 6, 8 and 10 year time points. In this type of analysis, missing data was allowed for any time point (maximum of 2 missing). To reflect the frequency (count) nature of the alcohol and other drug use variables, these measures were modeled as Poisson distributed variables. The model was estimated using MPlus 4.2 (Muthén and Muthén, 2007).
In LCGA models, the number of groups in the latent class variable must be specified. In this study, 3 to 9 class models were compared and through a sequential process of model selection, the LCGA model with the optimum number of latent classes was identified. Given prior work in this sample (Brown et al., 2001; Chung et al., 2003) and others (e.g., Chung et al., 2008) demonstrating heterogeneity in AOD patterns post adolescent treatment, classic regression (1-class) and binary models (2-class: use/non-use) were not evaluated. Following the general standards of Nagin (1999) and Muthén and Muthén (2000), model selection was based on initial quantitative criteria (i.e., Adjusted BIC, Entropy, Bootstrapped Likelihood Ratio Test [BLRT], posterior probabilities) and subsequent consideration of qualitative features (interpretability, discriminant validity) of each model.
As is common with mixture models, local maxima issues were a concern with the likelihood solutions obtained (Hipp and Bauer, 2006). Since it is common for complex mixture models to have multiple maxima, we adopted a conservative approach to guard against the possibility of selecting parameter estimates that are not at the global maximum (For detailed review see Eliason, 1993; Hipp and Bauer, 2006; McLachlan and Peel, 2000). To avoid local maxima, each model was estimated with Mplus's random starts algorithm, using 300 random sets of starting values and 30 final stage optimizations (Muthèn and Muthèn, 1998–2006). After being selected, the 6 class model was rerun with 7000 random starts and 60 final stage solutions to minimize the risk that the reported model was a product of local maxima. Even with the large number of random starts, many local maxima were found among the best fitting solutions. Of the top 10 rank ordered solutions, 6 different maxima were identified and as recommended (Hipp and Bauer, 2006), the local maxima were compared and evaluated for substantive differences between the solutions. The resultant solution with the best likelihood was presented and the parameter estimates were consistent with the parameter estimates for the 5 other top maxima. Under these circumstances, results can be used to draw substantive conclusions from the model (Hipp and Bauer, 2006).
Two strategies were used to determine whether demographic and substance use patterns of youth at treatment entry were related to post treatment trajectory class membership. Multinomial logistic regression (Hosmer and Lemeshow, 2000) was used to test for differences in ethnicity, sex, and alcohol and drug dependence diagnosis among the different classes. First, the logistic models were estimated using data where each subject was assigned to the class with the highest posterior probability. These models were then compared to models estimated using weighted regressions, using the posterior probabilities as regression weights. In this study, the posterior probabilities were high (>.95; Table 2) and in all cases the weighted regressions predicting intake characteristics resulted in outcomes equivalent to analysis based on unitary class assignment of each participant. Consequently, for ease in interpretation, we describe findings based on unitary class assignment below.
Table 2.
Decision Criteria by Class Solution for LCGA Models Youth Followed Ten Years after Treatment
| Classes | Adjusted BIC | Entropy | BLRT (p-value) | Range of maximum probabilities of class membership |
|---|---|---|---|---|
| 3 | 24021 | .998 | <.001 | .972 − .999 |
| 4 | 21790 | .999 | <.001 | .999 + |
| 5 | 20829 | .997 | <.001 | .672 −.999 |
| 6 | 20076 | .998 | <.001 | .957 − .999 |
| 7 | 19505 | .996 | <.001 | .618 − .999 |
| 8 | 19018 | .999 | <.001 | .935 − .999 |
| 9 | 18593 | .994 | <.001 | .778 −.999 |
Note: Range of maximum probabilities of group membership for the 4 class solution had a range of .999 and above suggesting overfit.
ANOVA and Fisher's Exact Test for contingency tables were conducted to validate class distinctions on AOD measures, characterize individuals expected to be within each class and compare psychosocial outcomes at each time point. When an ANOVA or contingency table was found to be significant for a time point, family-wise error corrections were applied to pairwise comparisons in order to determine which groups differed. ANOVAs were followed by Tukey HSD tests and contingency tables were followed by Holm corrected significance tests (Holm, 1979). Given space constraints, the entirety of these results was not presented here. Power analyses (G*Power 3; Faul et al., 2007) indicated that there was adequate power to detect medium to large effect sizes in determining group differences (f = .30; 1-β = .90; p<.05).
3. Results
3.1 10 year Patterns of Post Treatment Substance Use & DSM-IV Dependence Symptoms
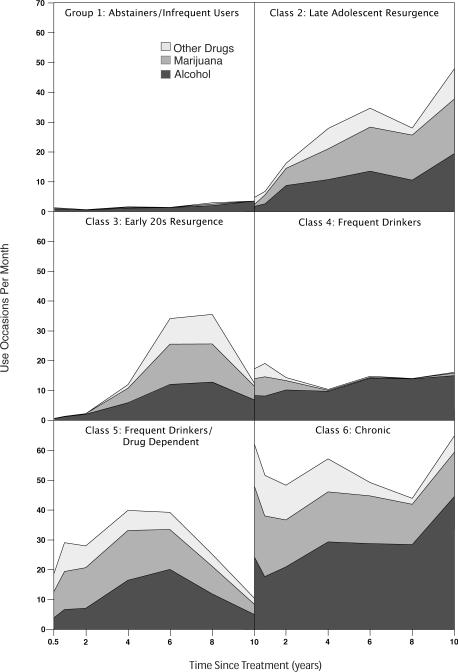
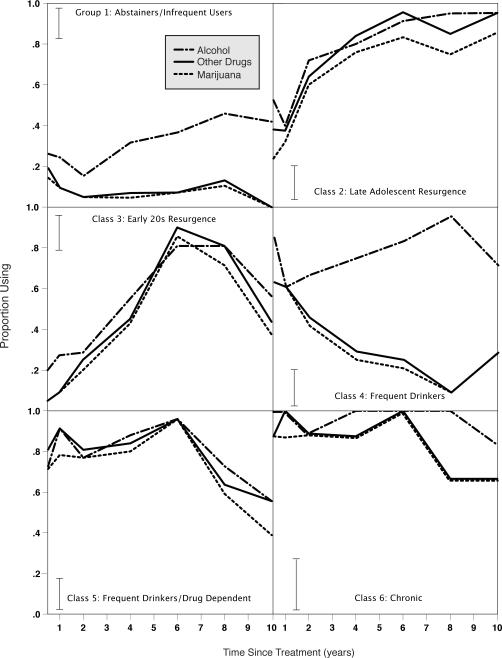
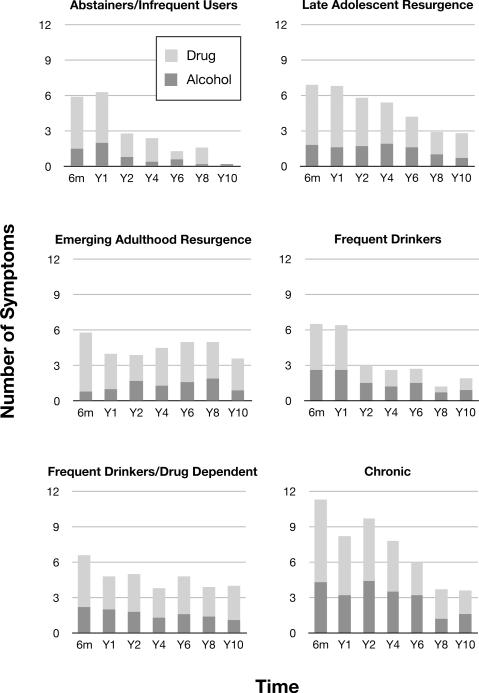
As described above, the series of LCGA models were tested to determine the best fit to the longitudinal data. While the Adjusted BIC dropped with each increase in number of classes and all class models were significant using the BLRT (Table 2), the 6 class solution maximized the interpretability of the longitudinal use patterns within the data. The parameter estimates for this selected model are presented in Table 3. Figures 1 and 2 highlight the topography of alcohol and other drug use within each trajectory class as characterized by individuals with the highest probability of class membership. While the trajectories were modeled on the frequency of alcohol and other drug use, Figure 1 also includes specific information on the frequency of use of marijuana as this substance is considered the most commonly used substance in this age range other than alcohol. Figure 2 shows the percentage of individuals assigned to each class reporting alcohol, marijuana, and other drug use at each time point. Figure 3 provides information on mean A/SUD criteria endorsed at each time period by those assigned to a particular trajectory group.
Table 3.
The 10 Year Latent Class Growth Model Characteristics for Alcohol/Drug Use: 6 Class Solution.
| Latent class | %Sample | Alcohol frequency |
Drug frequency |
||||
|---|---|---|---|---|---|---|---|
| Intercept (SE) | Slope(SE) | Quadratic(SE) | Intercept (SE) | Slope(SE) | Quadratic(SE) | ||
| 1. Abstainers/Infrequent Users | 28.7% | −0.27(.31) | 0.05(.71) | 0.39(.36) | −1.35(.50)* | 0.73(1.4) | −0.32(.64) |
| 2. Late Adolescent Resurgence | 17.6% | 1.35(.17)* | 3.25(.48)* | −1.64(.28)* | 2.96(.24)* | 1.18(.66) | −0.97(.36)* |
| 3. Emerging Adult Resurgence | 14.4% | −0.54(.53) | 4.68(.78)* | −1.77(.30)* | −4.81(1.1)* | 12.58(1.8)* | −4.78(.72)* |
| 4. Frequent Drinkers | 16.3% | 2.09(.20)* | 0.55(.54) | −0.16(.25) | 2.50(.21)* | −4.39(.91)* | 1.57(.59)* |
| 5. Frequent Drinkers/Drug Dependent | 17.0% | 1.22(.15)* | 1.80(.45)* | −0.51(.23)* | 1.35(.17)* | 2.37(.37)* | −0.71(.19)* |
| 6. Chronic | 6.0% | 3.11(.11)* | −0.02(.39) | 0.23(.29) | 3.70(.15)* | −0.90(.56) | 0.38(.34) |
p< .05
Figure 1.
Composite use of alcohol, marijuana and other drugs across a decade after adolescent treatment. Units are in days per month for each type of substance (e.g., days beer + days wine+ days hard liquor, 8 types of drugs), leading to frequencies greater than 30, as more than one type of alcohol or drug could be consumed in a given day.
Figure 2.
Proportion of each class using alcohol, marijuana and other drugs at each follow up time point. Vertical bases represent the mean 95% confidence interval for each class.
Figure 3.
Mean number of DSM-IV alcohol and drug use dependence symptoms endorsed by participants assigned to each trajectory class. For drug dependence symptoms, if participants were polysubstance users, they were credited for a particular symptom only one time, even if they experienced the same symptom for multiple substances.
Differences emerged across all concurrent measures of AOD engagement at each time point: maximum drinks per episode (F-values: 6.5 – 12.4 ps < .00001), percent with heavy episodic drinking (χ2: 21.7 – 45.3, ps < .001), percent using alcohol (χ2: 20.6 – 46.3, ps < .0001), percent using marijuana (χ2: 18.5 – 93.7, ps < .0001), percent using other drugs (χ2: 24.5 – 105.3, ps < .0001) and polydrug use (F-values: 11.2 – 21.9, ps < .00001). Groups differed significantly on meeting criteria for AUD (i.e., 3 or more alcohol dependency symptoms) from 6 months to 4 years after treatment (χ2: 9.3 – 20.1, ps < .05) and SUD diagnosis (i.e., 3 or more drug dependency symptoms) across all time points (χ2: 12.9 – 45.0, ps < .01).
3.1.1 Class 1: Abstainers/Infrequent users
The “Abstaining/Infrequent” pattern of use had the highest probability of group membership (n = 44) and demonstrated the lowest AOD use frequencies (Figure 1). Posthoc comparisons indicated that individuals expected to be in the Abstainers/Infrequent users class had the lowest proportion of alcohol, marijuana and other drug users across time (Figure 2). In the early stages after treatment, participants did endorse some A/SUD symptomatology. By 4 years post treatment, participants assigned to this class did not exceed clinical cut offs for AUD, and by 6 years, no SUDs were identified (Figure 3).
3.1.2 Class 2: Late Adolescent Resurgence
The distinguishing feature of the next two classes (2 & 3) is the timing of the return to heavier substance involvement. Late Adolescent Resurgence (Class 2) demonstrates substance use frequencies rising through adolescence with a subsequent drop in the early adult years (Figure 1). In comparison to Class 3, this use pattern peaks earlier and begins to recover earlier. The frequency of drug use (Figure 1), as well as the proportion of use among individuals expected to be in this class, continue to rise until their peak in late Year 4 and then slowly drop until around 10 years. Similarly, there is a rise in the proportion of youth most likely assigned to this class who exceed clinical cut offs for drug use disorders at 1 year (6 months: 52%, 1 year: 70%, 2 years: 46%). Rates of SUDs among the Late Adolescent Resurgence class exceeded the rates of drug diagnoses for the Class 3 (Emerging Adulthood Resurgence) at 6 months (Fischer's Exact Test, p = .001), 1 year (Fischer's Exact Test, p < .0001), and 2 years (Fischer's Exact Test, p = .002), supporting a different onset and timing of SUD reemergence across time. A similar pattern was not supported for AUDs (see Figure 3).
3.1.3 Class 3: Emerging Adulthood Resurgence
The Emerging Adulthood Resurgence pattern involves initially low frequency AOD use in the first two years post treatment with a sharp rise in frequency, particularly of drug use, from 4 to 10 years after treatment. The quadratic function in this class (Table 3) is manifested in the drop off in frequency at the last time point of assessment (Year 10). This sharp shift around 4 years post treatment (~20 years of age) is seen most clearly for drug involvement (Figures 1 & 2) and a rise in the proportion exceeding clinical cut offs for substance dependency (2 years: 5%, 4 years: 20%, 6 years: 45%).
3.1.4 Class 4: Frequent Drinkers
The pattern of AOD involvement for this trajectory class labeled as Frequent Drinkers was characterized by sustained high frequency drinking across time (Figure 1) with low rates of involvement with any other drug. Relatively low rates of drug use distinguished this Frequent Drinkers trajectory from Classes 5 (Frequent Drinkers/Drug Dependent) and 6 (Chronic). At 2 years post treatment, there is a sharp decline both in frequency of drug use (Figure 1) and percentage of class engaging in other substance use (Figure 2). Youth expected to be in this class drank at high doses (quantity × frequency per month: range = 52.7 – 96.0) but did not have significantly higher rates of alcohol dependence compared to other classes. Interestingly, this pattern of consumption was associated with a spike in quantity × frequency of drinking across the age range associated with the attainment of legal drinking age (Year 6) that remitted by Year 8. No individuals expected to be in this class met criteria for drug dependence at any of the 4 to 10 year assessment time points (Figure 3).
3.1.5 Class 5: Frequent Drinkers/Drug Dependent
The Frequent Drinkers/Drug Dependent trajectory is similar to Class 1 (Abstainers/Infrequent Users) and Class 3 (Emerging Adulthood Resurgence) in that the initial rates of alcohol, and to some extent drug use, initially following treatment (0–6 months) are relatively low. However, this pattern of use shows a sharp upward trajectory in AOD use frequencies across time (Figure 1). These youth are similar to the Worse with Time pattern found in previous work (e.g., Brown et al., 2001; Chung et al., 2004). Substance involvement also rose across time; individuals with a higher probability of class membership increased the frequency of substance use with a greater percentage of group members using AOD at each time point (Figures 1 & 2). These individuals showed a growth in SUDs from 1 year (25%) to 6 years (45%) post treatment.
3.1.6 Class 6: Chronic
The Chronic pattern of AOD involvement had the lowest probability of group membership within this sample, but the highest frequency AOD involvement at almost all time points (Figure 1). Individuals expected to be in the Chronic class had very high rates of SUDs (e.g., 6 months = 86%; 4 years = 50%) post treatment with high level symptom endorsement across time (Figure 3). This trajectory appears similar to severe groups reported in other investigations (Chung et al., 2004; Chung et al., 2005; Clark et al., 2006).
3.2 Demographic and pretreatment substance use as predictors of longitudinal use trajectories
Table 4 compares individuals assigned to each class on intake characteristics, subsequent treatment and incarceration, and developmental outcomes. In general, AOD trajectory classes were demographically similar at intake. Age (Table 4) and ethnicity (χ2 [df = 15] = 19.14, ns) were not significantly related to class membership. However, on the basis of assigning participants to classes with the highest probability of membership, there was a trend for men and women to be distributed differentially across trajectories (p = .06; Table 4) with young men slightly more likely to be represented in the frequent drug use classes (2, 3, 5, and 6). While the average monthly frequency of alcohol consumption (χ2 [df = 5] = 7.7, ns) and rates of heavy episodic drinking (Table 4) were similar at study intake, individuals expected to be within a particular class differed on the average maximum drinks per episode across the past 3 months. Posthoc comparisons suggested that those most likely assigned to the Frequent Drinkers/Drug Dependent class had significantly higher maximum drinks per episode prior to treatment than those most likely to be in the Abstainer/Infrequent User class (Bonferroni corrected p = .004). No specific drug use differences were evident across the trajectory classes except for frequency of marijuana use (Table 4), with Abstainers/Infrequent Users and Frequent Drinkers trajectories having the lowest marijuana frequency at intake while Late Adolescent Resurgence and Emerging Adulthood Resurgence, had the highest pretreatment marijuana use. At intake, other drug use (χ2 [df = 5] = 5.8, ns) and polydrug involvement (F [5, 147] = 0.84, ns) did not significantly differ across trajectory-defined classes. Further, logistic regressions indicated no significant differences across classes in proportions meeting DSM-IV diagnostic criteria for alcohol (χ2 [df = 5] = 8.0, ns) or drug dependence (χ2 [df = 5] = 0.2, ns) prior to study entry.
Table 4.
Intake and 10 Year Characteristics of Alcohol/Drug Use Trajectories by Posterior Probability Class Assignment (N =153).
| Class 1 Abstainer | Class 2 Late Adol | Class 3 Emg Adult | Class 4 Freq Drink | Class 5 FD/DD | Class 6 Chronic | Diff | |
|---|---|---|---|---|---|---|---|
| Intake | |||||||
| Age | 16.0 (1.5) | 15.8 (1.2) | 15.7 (1.3) | 16.4 (1.1) | 15.5(1.0) | 15.9(1.5) | F(5,147)=1.5 |
| Sex (F) | 56.8% | 33.3% | 31.8% | 52.0% | 26.9% | 22.2% | χ2(df=5)= 10.7 |
| Caucasian | 54.5% | 55.6% | 50.0% | 56.0% | 53.9% | 44.4% | χ2(df=5)= 0.5 |
| SES | 29.6(12.1) | 29.4(9.8) | 26.9(13.4) | 27.6(11.7) | 32.6(12.1) | 38.8(20.6) | F(5,146)=1.6 |
| AlcMax | 7.5(7.1) | 11.7(9.6) | 10.7(9.3) | 13.4(11.5) | 16.9(12.6) | 14.0(14.3) | F(5,146) = 3.1* |
| HEDrk | 57.1% | 74.1% | 77.3% | 76.0% | 80.0% | 66.7% | χ2(df=5)= 5.8 |
| MJ Freq | 12.8(12.5) | 19.8(10.7) | 19.3(12.0) | 10.8(11.6) | 17.5(12.5) | 17.2(12.7) | F(5,147)=2.5* |
| Control Variables | |||||||
| Incarcerated | 31.8% | 63.0% | 77.3% | 48.0% | 65.4% | 88.9% | χ2(df=5)= 20.5*** |
| Treatment (Inpt/Outpt) | 5% (3% /3%) | 26% (19% /15%) | 17% (12% 16%) | 12% (8% /12%) | 0% | 44% (20%/ 43%) | Fisher's Exact Test** |
| 10 Year Status | |||||||
| HS Grad | 71.1% | 65.2% | 44.4% | 82.6% | 64.0% | 28.6% | χ2(df=5) = 11.2* |
| SES | 43.1(14.8) | 53.1(12.6) | 50.8(11.8) | 42.0 (13.6) | 51.7(17.8) | 55.9(13.3) | F(5,H2) = 2.8* |
| Occupation | χ2(df=5)= 24.8* | ||||||
| Unemploy | 6.5% | 4.8% | 12.5% | 15.8% | 21.8% | 42.9% | |
| Unskilled | 41.9% | 81.0% | 68.8% | 31.6% | 47.8% | 42.9% | |
| Professional | 45.2% | 9.5% | 12.5% | 47.4% | 26.1% | 14.3% | |
| Managerial | 6.5% | 4.8% | 6.3% | 5.3% | 4.4% | 0% | |
| Married | 48.5% | 13.0% | 16.7%% | 52.2% | 36.0% | 0% | χ2(df=5)= 17.5** |
| Parent | 55.3% | 39.1% | 38.9% | 60.9% | 36.0% | 28.6% | χ2(df=5)= 6.0 |
Note: Class assignment is based on highest posterior probability of class membership. Alc Max: Maximum drinks/episode; HEDrk: heavy episodic drinkers (percent reporting 4+/5+drinks [females/males] per episode); MJ Freq: average days using marijuana per month; HS Grad: high school graduation; SES: socioeconomic status; Unemployed: Unemployed; Treatment: AOD treatment;
p<.05
p<.01
p<.001
3.3 Subsequent Treatment and Incarceration
To determine the potential role of post treatment controlled environments and/or treatment on these outcome patterns, both inpatient and outpatient treatment episodes and incarceration measured at each assessment time point were examined in relation to trajectory class. Prior to the 10 year assessment, probability of trajectory class membership was not associated with differences in treatment episodes at any time point. At the final assessment, trajectories differed significantly (Table 4), with individuals expected to be in the Chronic and Late Adolescent Resurgence groups reporting the greatest level of treatment exposure.
Incarceration at any time after initial adolescent treatment was significantly different on the basis of class assignment, with the most severe groups demonstrating the greatest percentage of incarceration (Table 4). When examining patterns of incarceration, there was a trend for individuals assigned to the Chronic group to have the highest number of sentences and longest sentences. For example, those with the Chronic class assignment had approximately three and a half jail terms compared to a range of 2.0 to 2.6 for other groups. Patterns were similar for those who were incarcerated in the Abstaining/Infrequent Users and Frequent Drinkers categories (2.0 times in jail), with 5 of 8 individuals expected to be Abstainers/Infrequent Users and 7 of 9 Frequent Drinkers incarcerated for less than 1 week. In comparison, all individuals in the Chronic class who had served time in jail spent more than a month incarcerated. When examining mean days served across each time point of assessment, assignment to the Chronic group was associated with the longest time incarcerated, with a mean of 77.9 days served (sd = 196.3). Pairwise comparisons demonstrated that length of stay was significantly higher than any other class assignment (Tukey WSD, p <.01), with mean differences ranging from 56.6 to 74.3 days. There were no significant differences among the remaining categories.
3.4 Alcohol and Substance Use Trajectories and Developmental Milestones of Emerging Adulthood
3.4.1 Industry: Education/Work
The impact of probability of class membership on educational attainment and occupational status was examined at 10 years post treatment as well as the timing of transitions in these areas. At 10 years, individuals expected to be within each class differed on rates of graduation from high school, with Abstainer/Infrequent Users and Frequent Drinkers having the greatest high school completion rate (Table 4). However, across trajectory classes, youth did not differ on the mean age of high school graduation for those with a diploma (F[5, 8]) = 1.28, ns). Of note, few members of this sample were college graduates by 10 years (n = 13; m age = 25.9, sd = 1.7), and no one expected to be a member of the Chronic class attained this level of education. As a result of low college attendance rates, differences based on rates of college completion or age of completion did not emerge.
Occupational status varied significantly in relation to trajectory classes (Table 4). Participants' report of their current occupation at 10 year assessment was divided into four categories: unemployed, unskilled/semi-skilled workers (e.g. machine operator, clerical), professionals (e.g., small business owner, administrator), and managerial/executives (e.g., business manager, higher executive). The majority of participants expected to be within the Chronic class reported being unemployed or engaging in unskilled/semi-skilled work, while Late Adolescent and Emerging Adulthood Resurgent groups were most likely to be in unskilled or semi-skilled positions. Individuals assigned to the Abstainer/Infrequent Users and Frequent Drinkers classes were most often in professional positions.
3.4.2 Independence: Financial/Residential
More than half of the sample was financially independent from their families of origin 10 years after treatment (56.4%) when the average age was 25.9 years. At that time, socioeconomic status, as measured by the Hollingshead Socioeconomic Status scores differed across trajectory groups (Table 4). As expected, individuals expected to be Abstainers/Infrequent Users obtained one of the best (lowest) mean SES index scores which were significantly lower than the mean of the other groups with histories of varying use patterns over 10 years (t[112] = −2.46, p= .02). Participants assigned to the Frequent Drinking class demonstrated consistent levels of SES to the Abstaining/Infrequent Users class (Table 4).
Independent living, defined as not living with parental figures or relatives (excluding spouse/children) was examined at all assessment time points. Youth assigned to the trajectory classes did not differ on their independent living environments across time but showed a developmental shift of greater independent living over time across all classes over time. On average, youth transitioned to independent living at age 19.6 (sd = 1.7), but individuals expected to be in different trajectory classes did not differ on the timing of this transition (F[5, 117]= 1.06, ns).
3.4.3 Intimacy: Marriage and Family
While about half of those expected to be Abstainers/Infrequent Users and Frequent Drinkers married at some point between treatment and 10 years post treatment, only small percentages of those associated with Late Adolescent Resurgence, Emerging Adulthood Resurgence, and Frequent Drinkers/Drug Dependent groups married (Table 4). None of those with highest probability of Chronic class membership had been married. When comparing classes on the percentage single versus cohabitating or being married, participants expected to be Frequent Drinkers were most likely to marry or live with a partner (69.6%) whereas those with highest probability for being in the Chronic class were least likely (14.3%; χ2 [df = 5] = 23.7, p < .0001) to be in such a stable partnership. On average, youth who married (n = 31) did so around age 26.4 (sd = 1.2) and the timing did not significantly differ by trajectory class probability (F[4, 26]= 1.11, ns).
While young adults in our sample did not significantly differ on the overall number of biological children as a function of trajectory class probability (F [5, 128] = 0.83, ns), about half of those assigned to the Abstainer/Infrequent User and Frequent Drinker groups had children in the decade after treatment compared to 28–39% those with drug involved patterns (Table 4). Young adults with the highest Abstainers/Infrequent User probability were significantly more likely to maintain full financial responsibility for their children compared to those with more frequent alcohol and drug use trajectories (F[5, 127]=2.75, p = .02). Age of childbirth (women: F[5,26]=1.29, ns; men: F[5,22]=1.87, ns) did not differ on the basis of assigned class membership.
4. Discussion
We identified six longitudinal patterns of alcohol and other drug use over the decade following adolescent alcohol and drug treatment: Abstainers/Infrequent Users, Late Adolescent Resurgence, Emerging Adulthood Resurgence, Frequent Drinkers, Frequent Drinkers/Drug Dependent, and Chronic. These trajectories reflect both the diversity of youth outcomes and dynamics of AOD involvement as adolescents transition into adulthood. Consistent with recent findings for youth in the first few years post treatment (Chung et al., 2003; Chung et al., 2005), the vast majority of this sample, approximately two thirds, dramatically improved after treatment. This early successful Abstaining/Infrequent pattern of use has been found in prior investigations of post treatment outcomes (Brown et al., 2001; Chung et al., 2004). As youth transition out of adolescence, two trajectory classes emerged with distinct differences in the timing of post treatment accelerations in substance involvement (Late Adolescent Resurgence & Emerging Adulthood Resurgence). Similarly, Clark and colleagues (2006) found six trajectory classes when modeling retrospective reports of SUD symptoms across early adolescence to mid-adulthood in SUD adults, including the presence of classes distinguished by developmental shifts in mid-adolescence, late adolescence and in emerging adulthood. These time periods correspond to important developmental transitions reflected in prior conceptualizations of development and empirical research (Aseltine and Gore, 2005; Brown et al., 2008; Chassin et al., 2004; Kypri et al., 2004). Additional measures of AOD involvement and DSM-IV diagnostic symptoms support the characterization of distinct patterns of AOD engagement and problems for teens following treatment.
Beyond the identification of these patterns, we were interested in how long term patterns of alcohol and other substance use after treatment related to attainment of the developmental milestones common to emerging adulthood (Arnett, 2000). As expected, trajectory classes characterized by lowest rates and levels of use were most likely to have more optimal psychosocial outcomes as young adults. Interestingly, the Frequent Drinkers trajectory class shared the characteristics of better occupational attainment, stable and intimate relationships, and fiscal responsibility for children with the Abstaining/Infrequent Use trajectory class. This finding highlights that some individuals who enter SUD treatment during adolescence may resolve their drug involvement but come to drink alcohol relatively frequently as they transition into young adulthood while remaining sub-threshold for alcohol dependence into their mid twenties. By contrast, frequent use of alcohol in conjunction with other substance use during late adolescence and emerging adulthood were associated with poorer occupational and family functioning as well as important diagnostic and functioning problems. Our choice to include the Chronic class, despite the small number of individuals exhibiting this use trajectory pattern (6%), seemed to capture a unique pattern of persistent AOD use which was qualitatively worse than others who had also received treatment and was associated with the most severe developmental consequences during young adulthood. Despite the lower prevalence rates, similar patterns have been demonstrated in other samples (e.g., Chung et al., 2008).
Given the influence of treatment and incarceration on adolescent substance involvement (Anderson et al., 2007; Brown and Ramo, 2006; Chung and Maisto, 2006; Godley et al., 2004), we examined these factors that might impact the emergence or transitions in these trajectories. Youth assigned to classes did not differ on their exposure to alcohol and drug treatment across the first 8 years of assessment following treatment despite substantial proportions of the sample meeting criteria for A/SUD over the course of study. However, trajectory-related differences in treatment exposure emerged at the final time point. The overall low rates of treatment for youth with continued heavy AOD use and dependence in emerging adulthood raises questions about opportunities for assessment, intervention and the continuity of care for individuals with a history of A/SUD treatment during adolescence. Further, the difference in treatment status at the final assessment point may reflect more the current treatment system (access, opportunities, triggers for treatment) than need and argues for routine screening, as well as new venues and strategies for identification and intervention in the early twenties.
In comparison to other work explicitly modeling controlled environments and substance use after treatment (Godley et al., 2004), we found that incarceration did vary between groups with the most severe longitudinal use patterns associated with the highest proportions being incarcerated, and largest number and longest duration of jail or prison terms. For example, individuals with a Chronic pattern spent the longest period of time incarcerated and tended to have more frequent and longer individual stays. This suggests that living within a restricted environment was not the primary force in lower rates of use for the other groups and that such severe and protracted use is associated with more serious and costly offenses over time. Piquero et al. (2001) identified the importance of incorporating incarceration as a time-varying covariate in longitudinal substance use research. While sample size limited doing so in the present study, these findings underscore the potential value of considering incarceration as well as treatment in modeling the mechanisms of change and consequences of substance involvement in adolescence and early adulthood.
This investigation had a number of strengths including the length of follow up, high follow up rates, use of an integrated modeling strategy to develop the descriptive classes considering both alcohol and other drugs and a priori hypotheses. To our knowledge, this is the first investigation that used LCGA to examine patterns across the ten years following adolescent inpatient substance use treatment. Our ability to examine both alcohol and substance use characteristics across 8 measurement time points during a period of rapid developmental change is a hallmark of this project; it allowed for examination of shifts in substance use at relevant adolescent/young adult transitions. The use of a dual trajectory LCGA approach provides a view of how both alcohol and other drug use fluctuate and reciprocally influence each other across the transition into adulthood and has been described as the most appropriate way to model “developmental comorbidity” (Jackson et al., 2005, p. 622).
Clinicians working with SUD individuals and their families can use this developmental trajectory approach to inform treatment planning. For example, for some teens, alcohol and other drug use tends to change together across time (e.g., Late Adolescent Resurgence and Frequent Drinkers/Drug Dependent groups), while others clearly have a consistent heavier pattern of alcohol use compared to marijuana or other drug use after treatment (Abstainers/Infrequent users and Frequent Drinkers). Further, our work has identified a number of important developmental periods when youth treated for alcohol and drug problems may be particularly in need of or receptive to treatment. As clients in recovery reach developmental periods when risk for a resurgence of use is greatest (late adolescence and emerging adulthood), these time points should be seen as “critical” opportunities for screening, assessment, relapse prevention and supporting normal development through non-substance using behaviors (e.g., job training, eliciting help from non-using social supports; Brown et al., 2008). Given the high rate of problems in core developmental arenas and cost of problems associated with heavy alcohol and drug involvement during this period, universal screening is called for. Future research should address the mechanisms by which these periods of developmental transition influence clinical course of AOD use and effectiveness of developmentally tailored interventions.
There are limitations on the conclusions drawn from this investigation. First, youth recruited into this study were primarily mid- and late adolescents (ages 15–17 years). The commonality that distinguished trajectories was in AOD frequency, not age of treatment. While trajectories were similar on age and distribution of youth across these categories, we cannot be specific as to age-related transitions. In addition, a number of different statistical strategies exist for examining longitudinal data of this type. Each strategy has its strengths and weaknesses (Bauer, 2007). In the case of LCGA, it is important to remember that it is inherently a descriptive technique. The investigator chooses the best fitting model on the basis of both theory and statistical criteria; these decisions could be made differently on the basis of alternative theories. For example, we chose a model with fairly high posterior probabilities (Table 2). This could suggest that the model has been closely fit to the data and consequently, prediction error will need to be examined when this classification system is applied to new populations of youth (Burnham and Anderson, 2002; Hastie et al., 2001). As our goal was to best describe the dominant longitudinal patterns of use (including simultaneous use of different substances) over time, this approach seems most appropriate for initial examination of long term course. Further studies should consider the impact of covariates on the description of AOD patterns across development. Comparisons of these findings to other investigations using other operationalizations of use and alternative modeling strategies will be useful in the future to provide convergence of evidence for typical patterns of post treatment clinical course and developmental periods of risk. While intake substance use (severity of alcohol use episodes and frequency of marijuana use) varied between classes, the diagnoses at intake did not. It remains to be seen whether this reflects inadequacies in the current diagnostic system for youth (Chung and Martin, 2005) or fact that severity of use rather than consequences (i.e., symptoms) are more associated with long term patterns of persistence or remission. Lastly, the sample was relatively small for conducting this type of longitudinal analyses, requiring further validation in other samples of alcohol or substance use disordered youth. Power analyses suggested our sample size was adequate to detect medium to large effect sizes; more subtle distinctions between groups might emerge in larger samples.
The goal of this investigation was to identify long term, developmentally relevant patterns in AOD use for treated youth. These patterns were associated with differential success in meeting the developmental milestones associated with the transition to adulthood. Clarification of the dispersion of outcomes following youth treatment can lead to better assessment of the effectiveness of treatments (e.g., Schulenberg and Maggs, 2002; Witkiewitz and Marlatt, 2004) and facilitate the development of new treatments or targeted timing of special interventions (Brown et al., 2008). Outcomes from addiction treatment necessarily reflect dynamic processes (Brown, 2004; Brown and Ramo, 2006) and should be examined from a framework that can account for the interaction between the person and environment over time.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
5. References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 3rd ed Author; Washington, DC: 1987. [Google Scholar]
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Anderson KG, Ramo DE, Schulte MT, Cummins K, Brown SA. Substance use treatment outcomes for youth: Integrating personal and environmental predictors. Drug Alcohol Depend. 2007;88:42–48. doi: 10.1016/j.drugalcdep.2006.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett JJ. Emerging Adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480. [PubMed] [Google Scholar]
- Aseltine RH, Jr., Gore S. Work, postsecondary education, and psychosocial functioning following the transition from high school. J Adolesc Res. 2005;20:615–639. [Google Scholar]
- Bauer DJ. Observations on the use of growth mixture models in behavioral research. Multivariate Behav Res. 2007;42:757–786. [Google Scholar]
- Brame B, Nagin DS, Tremblay RE. Developmental trajectories of physical aggression from school entry to late adolescence. J Child Psychol Psychiatry. 2001;42:503–512. [PubMed] [Google Scholar]
- Brown SA. Measuring youth outcomes from alcohol and drug treatment. Addictions. 2004;99:38–46. doi: 10.1111/j.1360-0443.2004.00853.x. [DOI] [PubMed] [Google Scholar]
- Brown SA, D'Amico EJ, McCarthy DM, Tapert SF. Four-year outcomes from adolescent alcohol and drug treatment. J Stud Alcohol. 2001;96 doi: 10.15288/jsa.2001.62.381. [DOI] [PubMed] [Google Scholar]
- Brown SA, McGue MK, Maggs J, Schulenberg JE, Hingson R, Swartzwelder HS, Martin CS, Chung T, Tapert SF, Sher KJ, Winters K, Lowman C, Murphy SA. A developmental perspective on alcohol and youth ages 16–20. Pediatrics. 2008;121:S290–S310. doi: 10.1542/peds.2007-2243D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Mott MA, Myers MG. Adolescent alcohol and drug treatment outcome. In: Watson RR, editor. Drug and alcohol abuse prevention. Humana Press; Clifton, NJ: 1990. pp. 373–403. [Google Scholar]
- Brown SA, Myers MG, Lippke LF, Stewart DG, Tapert SF, Vik PW. Psychometric Evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. J Stud Alcohol. 1998;59:427–439. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Mott MA, Vik PW. Correlates of success following treatment for adolescent substance abuse. Appl Prev Psychol. 1994;3 [Google Scholar]
- Brown SA, Ramo DE. Clinical course of youth following treatment for alcohol and drug problems. In: Liddle HA, Rowe CL, editors. Adolescent substance abuse: Research and clinical advances. Cambridge University Press; New York, NY: 2006. pp. 79–103. [Google Scholar]
- Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addict Behav. 1989;14:291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Model selection and multimodel inference: A practical information-theoretic approach. Springer Science Business & Media, Inc.; New York, NY: 2002. [Google Scholar]
- Chassin L, Flora DB, King KM. Trajectories of alcohol and drug use and dependence from adolescence to adulthood: The effects of familial alcoholism and personality. J Abnorm Psychol. 2004;113:483–498. doi: 10.1037/0021-843X.113.4.483. [DOI] [PubMed] [Google Scholar]
- Chung T, Maisto SA. Relapse to alcohol and other drug use in treated adolescents: Review and reconsideration of relapse as a change point in clinical course. Clin Psychol Rev. 2006;26 doi: 10.1016/j.cpr.2005.11.004. [DOI] [PubMed] [Google Scholar]
- Chung T, Maisto SA, Cornelius JR, Martin CS. Adolescents' alcohol and drug use trajectories in the year following treatment. J Stud Alcohol. 2004;65:105–114. doi: 10.15288/jsa.2004.65.105. [DOI] [PubMed] [Google Scholar]
- Chung T, Maisto SA, Cornelius JR, Martin CS, Jackson KM. Joint trajectory analysis of treated adolescents' alcohol use and symptoms over 1 year. Addict Behav. 2005:1690–1701. doi: 10.1016/j.addbeh.2005.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung T, Martin C, Grella CE, Winters KC, Abrantes AM, Brown SA. Course of alcohol problems in treated adolescents. Alcohol Clin Exp Res. 2003;27:253–261. doi: 10.1097/01.ALC.0000053009.66472.5E. [DOI] [PubMed] [Google Scholar]
- Chung T, Martin CS, Clark DB. Concurrent change in alcohol and drug problems among treated adolescents over three years. JSAD. 2008;69:420–429. doi: 10.15288/jsad.2008.69.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung T, Martin CS. What were they thinking? Adolescents' interpretations of DSMIV alcohol dependence symptom queries and implications for diagnostic validity. Drug and Alcohol Depend. 2005;80:191–200. doi: 10.1016/j.drugalcdep.2005.03.023. [DOI] [PubMed] [Google Scholar]
- Clark DB, Jones BL, Wood DS, Cornelius JR. Substance use disorder trajectory classes: Diachronic integration of onset age, severity, and course. Addict Behav. 2006;31:995–1009. doi: 10.1016/j.addbeh.2006.03.016. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Maisto SA, Pollock NK, Martin CS, Salloum IM, Lynch KG, Clark DB. Rapid relapse generally follows treatment for substance use disorders among adolescents. Addict Behav. 2003 Mar;28:381–6. doi: 10.1016/s0306-4603(01)00247-7. [DOI] [PubMed] [Google Scholar]
- Eliason SR. Maximum likelihood estimation: Logic and practice. Sage Publications; Thousand Oaks, CA: 1993. [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, Buchner A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Godley SH, Dennis ML, Godley MD, Funk RR. Thirty-month relapse trajectory cluster groups among adolescents discharged from out-patient treatment. Addiction. 2004;99:129–139. doi: 10.1111/j.1360-0443.2004.00860.x. [DOI] [PubMed] [Google Scholar]
- Hastie TR, Tibshirani J, Friedman J. The elements of statistical learning: Data mining, inference, and prediction. Springer-Verlag; New York, NY: 2001. [Google Scholar]
- Hipp JR, Bauer DJ. Local solutions in the estimation of growth mixture models. Psychol Methods. 2006;11:36–53. doi: 10.1037/1082-989X.11.1.36. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Two-Factor Index of Social Position. Yale University Press; New Haven, CT: 1965. [Google Scholar]
- Holm S. A simple sequentially rejective multiple test procedure. Scand J Statist. 1979;6:65–70. [Google Scholar]
- Hosmer DW, Lemeshow S. Applied logistic regression. John Wiley and Sons; New York, NY: 2000. [Google Scholar]
- Jackson KM, Sher KJ, Schulenberg JE. Conjoint developmental trajectories of young adult alcohol and tobacco use. J Abnorm Psychol. 2005;114:612–626. doi: 10.1037/0021-843X.114.4.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, Abrantes A, Brown SA. Social Recovery Model: An 8-Year Investigation of Adolescent 12-Step Group Involvement Following Inpatient Treatment. Alcohol Clin Exp Res. 2008;32:1–11. doi: 10.1111/j.1530-0277.2008.00712.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Myers MG, Brown SA. A multivariate process model of adolescent 12-step attendance and substance use outcome following inpatient treatment. Psychol Addict Behav. 2000;14:376–389. [PMC free article] [PubMed] [Google Scholar]
- Kypri K, McCarthy DM, Coe MT, Brown SA. Transition to independent living and substance involvement of treated and high risk youth. J Child Adolescent Subst Abuse. 2004;13:85–100. [Google Scholar]
- Latimer WW, Winters KC, Stinchfield R, Travers RE. Demographic, individual, and interpersonal predictors of adolescent alcohol and marijuana use following treatment. Psychol Addict Behav. 2000;14:162–173. doi: 10.1037//0893-164x.14.2.162. [DOI] [PubMed] [Google Scholar]
- Luczak SE, Wall TL, Cook TAR, Shea SH, Carr LG. ALDH2 status and conduct disorder mediate the relationship between ethnicity and alcohol dependence in Chinese, Korean, and White college students. J Abnorm Psychol. 2004;113:271–278. doi: 10.1037/0021-843X.113.2.271. [DOI] [PubMed] [Google Scholar]
- McLachlan G, Peel . Finite mixture models. Wiley; New York: 2000. [Google Scholar]
- Muthén B. Latent variable mixture modeling. In: Marcoulides GA, Schumacker RE, editors. New Developments and Techniques in Structural Equation Modeling. Lawrence Erlbaum Associates; Philadelphia, PA: 2001. pp. 1–33. [Google Scholar]
- Muthén BO, Muthén LK. MPlus 4.2. Muthén & Muthén; Los Angeles, CA: 2007. [Google Scholar]
- Muthèn BO, Muthèn LK. Integrating person-centered and variable-centered analysis: Growth mixture modeling with latent trajectory classes. Alcohol Clin Exp Res. 2000;24:882–891. [PubMed] [Google Scholar]
- Muthèn LK, Muthèn B. MPlus User's Guide. Muthèn & Muthèn; Los Angeles, CA: 1998–2006. [Google Scholar]
- Nagin D. Analyzing developmental trajectories: A semiparametric, group-based approach. Psychol Methods. 1999;4:139–157. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- Nagin DS. Group-based Modeling of Development. Harvard University Press; Cambridge, MA: 2005. [Google Scholar]
- Piquero AR, Blumstein A, Brame R, Haapanen R, Mulvey EP, Nagin DS. Assessing the impact of exposure time and incapacitation on longitudinal trajectories of criminal offending. J Adolesc Res. 2001;16:54–74. [Google Scholar]
- Richter SS, Brown SA, Mott MA. The impact of social support and self-esteem on adolescent substance abuse treatment outcome. J Subst Abuse. 1991;3:371–385. doi: 10.1016/s0899-3289(10)80019-7. [DOI] [PubMed] [Google Scholar]
- Scales PC, Benson PL, Mannes M, Hintz NR, Roehlkepartain EC, Sullivan T. Other people's kids: Social expectations and American adults' involvement with children and adolescents. The Search Institute series on developmentally attentive community and society; New York, NY: 2003. [Google Scholar]
- Schulenberg J, O'Malley PM, Bachman JG, Wadsworth KN, Johnston LD. Getting drunk and growing up: Frequent binge drinking during the transition to young adulthood. J Stud Alcohol. 1996;57:289–304. doi: 10.15288/jsa.1996.57.289. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, Maggs JL. A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. J Stud Alcohol. 2002;14:54–70. doi: 10.15288/jsas.2002.s14.54. [DOI] [PubMed] [Google Scholar]
- Spear LP. Adolescence and the trajectory of alcohol use: Introduction to part VI. In: Dahl RE, Spear LP, editors. Adolescent brain development: Vulnerabilities and opportunities. New York Academy of Sciences; New York, NY: 2004. pp. 202–205. [DOI] [PubMed] [Google Scholar]
- Stewart DG, Brown SA. Withdrawal and dependency symptoms among adolescent alcohol and drug abusers. Addiction. 1995;90:627–635. doi: 10.1046/j.1360-0443.1995.9056274.x. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies . Treatment Episode Data Set (TEDS): 1995–2005. National Admissions to Substance Abuse Treatment Services; Rockville, MD: 2007. (DASIS Series: S-37). [Google Scholar]
- Wiesner M, Weichold K, Silbereisen RK. Trajectories of alcohol use among adolescent boys and girls: Identification, validation, and sociodemographic characteristics. Psychol Addict Behav. 2007;21:62–75. doi: 10.1037/0893-164X.21.1.62. [DOI] [PubMed] [Google Scholar]
- Winters KC, Stinchfield R, Latimer W, Lee S. Long-term outcome of substance-dependent youth following 12-step treatment. J Subst Abuse Treat. 2007;33:61–69. doi: 10.1016/j.jsat.2006.12.003. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. Am Psychol. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Chermack ST, Curran GM. Alcoholism: A life span perspective on etiology and course. In: Sameroff AJ, Lewis M, Miller SM, editors. Handbook of developmental psychopathology. second edition Kluwer Academic/Plenum Publishers; New York, NY: 2000. pp. 569–587. [Google Scholar]