Abstract
Background
Falls are the number one cause of unintentional injury in older adults. The protective response of “breaking the fall” with the outstretched hand is often essential for avoiding injury to the hip and head. In this study, we compared the ability of young and older women to absorb the impact energy of a fall in the outstretched arms.
Methods
Twenty young (mean age = 21 years) and 20 older (M = 78 years) women were instructed to slowly lower their body weight, similar to the descent phase of a push-up, from body lean angles ranging from 15° to 90°. Measures were acquired of peak upper extremity energy absorption, arm deflection, and hand contact force.
Results
On average, older women were able to absorb 45% less energy in the dominant arm than young women (1.7 ± 0.5% vs 3.1 ± 0.4% of their body weight × body height; p < .001). These results suggest that, even when both arms participate equally, the average energy content of a forward fall exceeds by 5-fold the average energy that our older participants could absorb and exceeds by 2.7-fold the average energy that young participants could absorb.
Conclusions
During a descent movement that simulates fall arrest, the energy-absorbing capacity of the upper extremities in older women is nearly half that of young women. Absorbing the full energy of a fall in the upper extremities is a challenging task even for healthy young women. Strengthening of upper extremity muscles should enhance this ability and presumably reduce the risk for injury to the hip and head during a fall.
Keywords: Hip fracture, Wrist fracture, Falls, Biomechanics, Aging
FALLS are the number one cause of unintentional injury in older adults (1), and the act of arresting or “breaking a fall” with the outstretched hand or forearm is a common strategy for avoiding serious injury to the head, face, cervical spine, and hip. For example, clinical studies indicate that impact to the outstretched hands occurs in about 46% of falls in older women (2) and reduces risk for hip fracture by approximately threefold (2,3). Laboratory studies indicate that more than 90% of falls in young adults involve impact to one or both outstretched hands (4,5).
A reasonable goal in arresting a fall with the upper extremities is to absorb sufficient energy to prevent impact to the head and reduce to safe levels the residual energy that must be absorbed through contact to the trunk and pelvis. One’s ability to achieve this depends on (a) how quickly the hands can be moved into a protective position during descent and (b) the magnitude of energy that can be subsequently absorbed (through the generation of torques and deflections in the upper extremity joints) during contact. Previous studies have shown that healthy older women, although slower than young women in initiating hand movements, are generally able to move the hands quickly enough into an appropriate position for breaking a forward fall (6). Although, to our knowledge, no study has directly measured the effect of age on ability to subsequently absorb energy in the upper extremities during a fall, computer modeling suggests that age-related declines in muscle strength may prevent older individuals from halting the body’s downward movement during a fall from even a low height (7). Furthermore, clinical studies indicate that the strength of the triceps muscle, a major contributor to upper extremity energy absorption (8), is an important predictor of risk for hip fracture during a fall (2).
More direct evidence of age-related differences in the ability to safely arrest a fall should help to guide the design of exercise programs aimed at fracture prevention. Accordingly, the goal of the current study was to determine whether healthy older women are less able than young women to absorb energy in the upper extremities during a task that safely simulated a forward fall. We also examined whether peak energy absorption associates with peak hand contact force during descent, a marker of upper extremity strength.
METHODS
Participants included 20 young women who ranged in age from 18 to 31 years (M = 21 ± 2 [SD] years), in body mass from 39.8 to 80.0 kg (M = 58.1 ± 10.4 kg), and in height from 1.51 to 1.77 m (M = 1.64 ± 0.06 m) and 20 older women who ranged in age from 70 to 88 years (M = 78 ± 5 years), in body mass from 54.4 to 87.2 kg (M = 68.8 ± 8.6 kg), and in height from 1.45 to 1.74 m (M = 1.61 ± 0.07 m). Potential participants were screened initially for eligibility with a telephone interview. Those who seemed to meet our inclusion criteria were further screened on physical examination by an experienced physiotherapist. Exclusion criteria included (a) regular exercise averaging once a week or more for the past 3 months (because our intent in this study was to examine how normal aging influences ability to arrest a fall, without the confounding effect of varying levels of exercise), (b) impairment of neuromuscular function secondary to neurological disease (e.g., traumatic brain injury, Parkinson’s disease, cerebral palsy, multiple sclerosis, diabetic neuropathy), (c) amputation or other debilitating orthopedic conditions (e.g., joint replacements, rheumatoid arthritis), (d) inability to raise the arms to shoulder height, and (e) inability to follow simple instructions in English. Each participant provided written informed consent, and the experimental protocol was approved by the Office of Research Ethics at Simon Fraser University.
The experimental protocol simulated the descent phase of a push-up activity, with gradually increasing energy absorption demands, allowing for measurement of the participant’s maximum energy-absorbing capacity. In designing the protocol, we considered that real falls would create too great a risk for injury, especially for older participants, and that the task of breaking a forward fall is similar to the descent phase of a push-up. We also considered that there are several strategies available for arresting a fall with the upper extremities. In particular, DeGoede and Ashton-Miller (9) showed that a “stiff arm” approach can be used to break a fall, which produces a small amount of joint flexion over a short time interval. Our experiments simulated fall arrests involving much larger deflections of the upper extremity and downward movement of the torso during contact (via flexion at the elbow and shoulder). This arrest strategy mimics the “natural” or “minimal impact” condition of DeGoede and Ashton-Miller (9) much more closely than the stiff arm fall. In addition to safety considerations, we opted for this approach based on the expectation that this type of fall results in considerably greater energy absorption in the upper extremity (for a given force level) and thereby provides a more accurate measure of the true energy-absorbing capacity of the upper extremity.
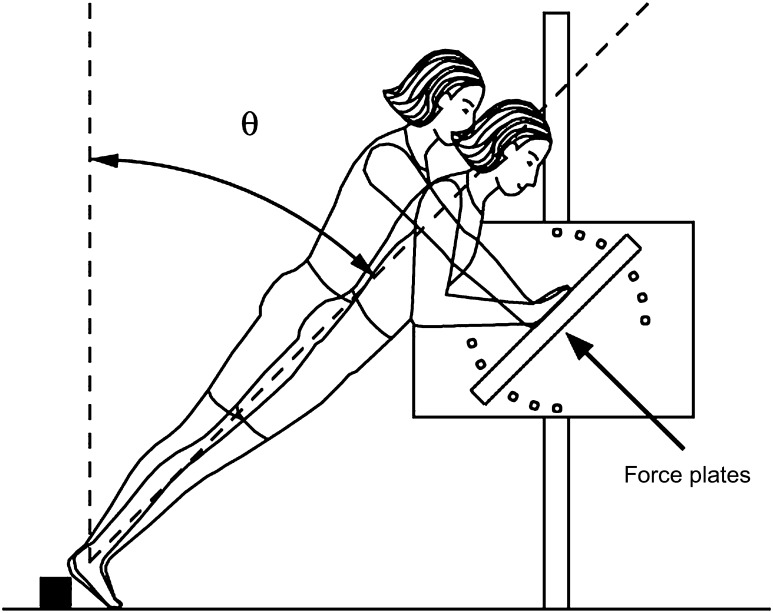
At the beginning of each trial, the participant stood with her body inclined at an angle θ from the vertical, with her elbows fully extended, shoulders flexed at 90°, and palms contacting two flush-mounted 25 × 35–cm force plates (MU2535; Bertec Corp., Columbus, OH) to acquire measures of hand contact force (Figure 1). Her hands were positioned with the middle fingers pointing superiorly and the wrists in the same sagittal plane as the shoulders. The platform was rotated to match the body lean angle θ, and the height was adjusted to allow the required upper extremity position (Figure 1).
Figure 1.
Experimental setup. At the start of the trial, the participant stood leaning at an angle θ from the vertical (initially set to 15°) with her arms fully extended and her hands contacting the force plates prior to the cue to slowly lower her body.
We then instructed the participant to slowly lower her body weight while maintaining her knees and hips extended, similar to the descent phase of a push-up, until she reached 90° of elbow flexion. To prevent further descent, the participant wore a fall restraint harness, which was attached via a tether to an overhead support, and did not apply a restraining force until the elbow angle exceeded approximately 120°. Each participant started at a lean angle of 15°. If they were able to complete the lowering task three repeated times and achieve elbow flexions of approximately 90° in each trial with no assistance from the tether, the body lean angle was increased 15° (up to a maximum of 90°) and the experiment was repeated. For participants who were able to complete trials at 90°, a further set of trials were conducted at 90° with the addition of a 7 kg weight secured with a strap between the scapulae. We provided rest periods of 20 seconds between individual trials (in the inclined position) and 5 minutes between sets.
During each trial, we used a seven-camera, 60-Hz motion measurement system (Qualisys Inc., East Windsor, CT) to acquire the three-dimensional (3D) positions of 27 skin surface markers located at the top of the head, seventh cervical vertebra, sacrum and bilaterally at the acromion processes, lateral radial epicondyles, medial ulnar epicondyles, radial styloids, ulnar styloids, third metacarpal heads, anterior superior iliac spines, greater trochanters, lateral femoral epicondyles, lateral malleoli, and fifth metatarsal heads. We acquired simultaneous measures of hand contact force and center of pressure at 960 Hz from the force plates underlying the hands.
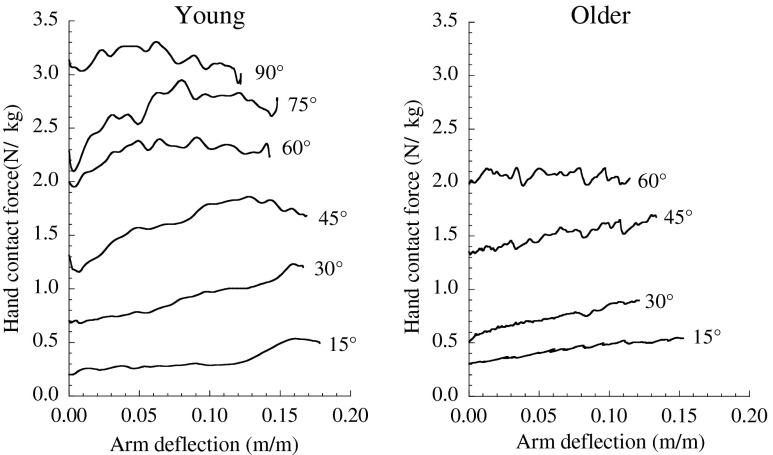
For each trial, we used custom MATLAB routines to calculate time-varying values of arm deflection, hand contact force, and energy absorbed by both upper extremities. Marker position data and force data were first filtered using low-pass, recursive, fourth-order Butterworth filters having cutoff frequencies of 6 and 10 Hz, respectively. Arm deflection was defined as the change in length of the arm position vector connecting the hand center of pressure (obtained from the force plate) and the skin surface marker at the acromion process. Hand contact force was calculated as the projection of the 3D force vector onto the arm position vector. Upper extremity total energy absorption was calculated by numerical integration using the trapezoid rule of the area under the hand contact force–arm deflection trace. Arm deflections were normalized by body height, and hand contact forces were normalized by body weight. Therefore, energy absorption was normalized by the product of body weight and body height. Figure 2 shows force–deflection traces at each completed body lean angle for a typical young participant and an older participant. We were unable to calculate upper extremity energy absorption in 25 of 372 trials (7%) due either to the marker on the acromion process dropping out of camera view (19 trials) or to equipment malfunction (6 trials), and these trials were excluded from analysis.
Figure 2.
Traces recorded during descent of hand contact force and arm deflection for one typical young participant and one typical older participant.
For each participant, we then identified the trial where the maximum energy was absorbed (which we will refer to as the peak energy absorption). In this trial, we identified peak values of hand contact force and arm deflection. We used independent samples t tests to determine whether there were differences between young and older participants in each of these outcome variables and paired t tests to determine whether there was a difference between results for the dominant and nondominant upper extremities. We also used Pearson correlations to examine the association between peak energy absorption, arm deflection, and hand contact force. We set the total significance level at .05 but applied a Bonferroni correction for multiple comparisons, resulting in a significance level of .01 for individual tests. All statistical analyses were performed using SPSS 15 (SPSS Inc., Chicago, IL).
RESULTS
There was no significant difference between the dominant and nondominant arms in peak arm deflection (young: p = .648; older: p = .309) or peak hand contact force (young: p = .165; older: p = .222). There was a significant but small difference in peak energy absorption between the dominant and nondominant arms (young: 0.3%, p = .001; older: 0.1%, p = .032), and thus, further statistical analysis focused only on dominant arm results.
Older individuals absorbed 45% less energy in their upper extremities than young participants (p < .001; Table 1). This reflected a 35% difference between young and older participants in peak hand contact force (p < .001) as there was no significant difference in peak arm deflection between young and older participants (p = .822; Table 1).
Table 1.
Mean Parameter Values and Results From t Tests
| Parameter | Young, n = 20, mean ± 1 SD (range) | Older n = 20, mean ± 1 SD (range) | Mean Difference (95% confidence interval) | p Value |
| Peak energy absorption, normalized (% body weight × body height) | 3.1 ± 0.4 (2.4–3.9) | 1.7 ± 0.5 (0.7–3.2) | 1.3 (1.0–1.6) | <.001 |
| Peak hand contact force, normalized (% body weight) | 36.5 ± 3.2 (30.0–44.0) | 23.8 ± 6.7 (13.9–36.5) | 12.6 (9.3–16.0) | <.001 |
| Peak arm deflection, normalized (% body height) | 13.7 ± 1.8 (11.0–17.0) | 13.6 ± 2.7 (9.7–22.1) | 0.1 (−1.3 to 1.6) | .822 |
| Maximum angle performed (°) | 87 ± 8 (60–90) | 67 ± 10 (45–90) | 20 (14–26) | <.001 |
| Angle of peak energy absorption (°) | 79 ± 11 (60–90) | 56 ± 12 (30–75) | 23 (16–30) | <.001 |
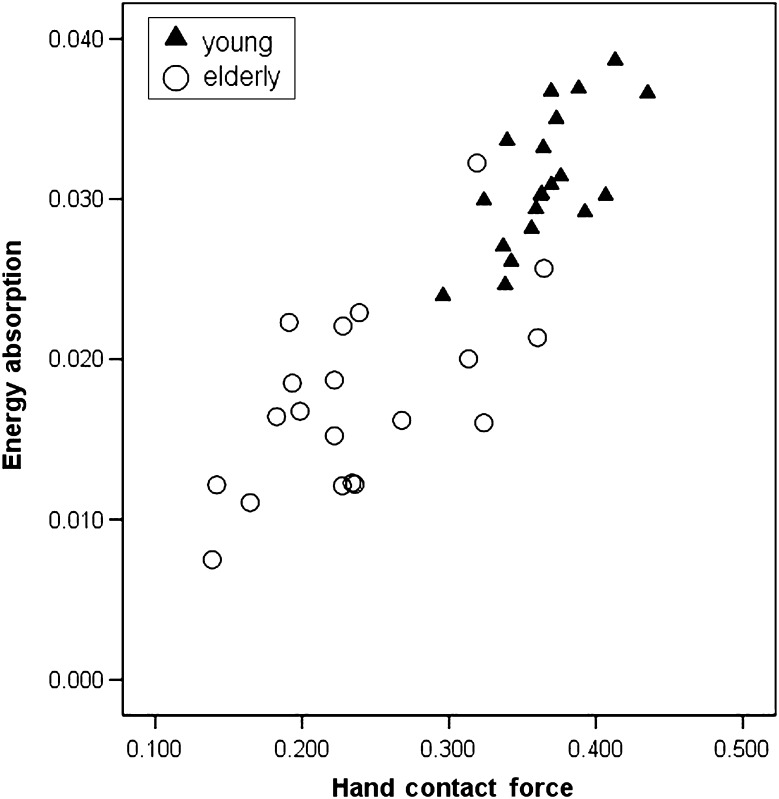
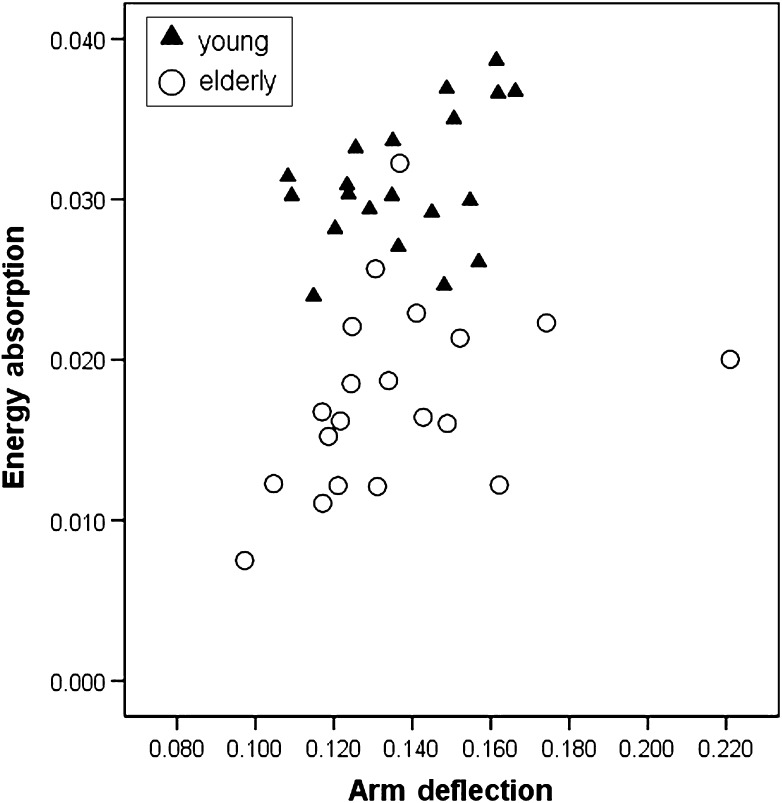
We observed a significant relationship between normalized peak energy absorption and hand contact force among both young (r = .69, p = .001) and older women (r = .61, p = .004; Figure 3). There was no significant relationship between normalized peak energy absorption and peak arm deflection for either young (r = .43, p = .055) or older women (r = .35, p = .123; Figure 4).
Figure 3.
Pearson correlations for normalized peak energy absorption (Joules/(body weight × body height)) and peak hand contact force (Newtons/body weight) for 20 young (r = .69, p = .001) and 20 older (r = .61, p = .004) participants.
Figure 4.
Pearson correlations for normalized peak energy absorption (Joules/(body weight × body height)) and peak arm deflection (Newtons/body height) for 20 young (r = .43, p = .055) and 20 older (r = .35, p = .123) participants.
We also found a significant difference between the maximum completed angle and angle of peak energy absorption between young and older participants (Table 1). The trial at which peak energy absorption occurred was not always the same as the last angle completed. This was due primarily to the observation that some participants were able to obtain greater joint flexions and contact forces at an angle smaller than the maximum angle performed. Of the young, the last angle completed was 90° plus weight for 3 participants, 90° for 14 participants, 75° for 2 participants, and 60° for 1 young participant. The angle of peak energy absorption for the young was 90° plus weight for 2 participants, 90° for 5 participants, 75° for 10 participants, and 60° for 3 participants. Of the older women, none completed 90° plus weight, 1 participant completed 90°, 4 participants completed 75°, 10 participants completed 60°, and 1 participant completed 45°. The angle of peak energy absorption for the older women was 75° for 3 participants, 60° for 12 participants, and 45° for 5 participants.
DISCUSSION
Our results suggest that older women are substantially less able than young women to absorb energy in their upper extremities during a push-up task that simulates arresting a fall. This may contribute to the increase with age in the prevalence of fall-related hip fracture (10,11) and head and neck injury (12–15). To place these results in the context of the ability to safely arrest a fall, it is useful to compare our observed energy absorptions with measures of the average energy content of a forward fall (16). In a previous study, where forward falls from standing were initiated by means of a tether and electromagnet in an experimental study of forward falls from standing, the average energy content of the body at contact was 0.17 ± 0.09 J/(body weight × body height) (16), which exceeds the average energy that our older women could absorb in their upper extremities by 5-fold (0.017 J/(body weight × body height)) and exceeds by 2.7-fold the average energy that young women could absorb (0.031 J/(body weight × body height)). Thus, the task of absorbing all the energy of a forward fall in the upper extremities, and thereby completely avoiding contact to the trunk and head, presents a major challenge even for healthy young women. Of course, rather than being able to absorb all the energy of the fall in the upper extremities, a more reasonable goal is to absorb just enough energy to prevent impact to the head and reduce to safe levels the residual energy that must be absorbed through contact to the trunk and pelvis. Quantifying this value is a challenging but important goal for future research.
Our findings should inform the design of exercise programs aimed at enhancing fall protective responses, in particular resistance training, a treatment mode that is commonly used in the management of individuals who are at high risk of falls or those with osteoporosis (17). The reduced energy absorption capacity of our older participants was associated with reduced ability to generate force in the upper extremities, which is likely secondary to age-related loss of eccentric muscle strength (7,18) in the chest, scapular, shoulder, and arm muscles (19) that are required to decelerate the body mass as the shoulder horizontally abducts and the elbow flexes as in the descent phase of a push-up. Thus, training for this task should include eccentric pectoralis major and triceps brachii exercise, with adequate stabilization of the scapulae and thorax. These muscles and movements should be key targets in future studies of exercise therapy for the improvement of upper extremity energy absorption in falls.
Our results extend the findings of previous studies investigating age- and gender-related differences in the ability to break a fall with the hands. Nevitt and Cummings (2) reported that 49% of fallers aged 64–74 years and 33% of those aged 75 years or older reported landing on a hand during a fall. In contrast, Feldman and Robinovitch (4) found that 98% of young adults impacted one or both hands during unexpected falls in a laboratory setting. O’Neill and colleagues (21) found that older women were half as likely as young women to first impact the hand when falling. Finally, Vellas and colleagues (20) observed that 50% of older men but only 33% of older women reported absorbing the main impact of their fall with the hands.
To safely include older women in our study, we substituted an actual fall with the descent phase of a push-up task. On the one hand, the relevant muscle dynamics may be surprisingly similar because impact forces during falls on the outstretched hand are characterized by a higher frequency peak force (with little associated elbow and shoulder rotations) followed by a lower frequency oscillation. It is during this latter period, where force levels are considerably lower, and near the range used in the current study (7–9), where the great majority of elbow and shoulder rotations occur, allowing for energy absorption. On the other hand, the task we studied differs considerably from a fall in the rate of stretch of eccentrically contracting muscles. Although we did not record the time of descent in our trials, it was considerably longer than the ∼350 ms observed in DeGoede and Ashton-Miller’s (9) natural fall arrests, and thus, the rate of muscle stretch was considerably slower. It is well known that muscle force (and thus energy-absorbing capacity) increases with increasing rate of stretch and that there is a relative preservation of eccentric muscle strength with aging. In reviewing the literature, Thelen (22) concluded that, when compared with an isometric contraction, maximum muscle force during a rapidly lengthening contraction can be as much as 1.8-fold greater for older women and 1.4-fold greater for younger women. Although such differences would not affect our primary conclusions, they would reduce slightly the differences between young and older women and lessen the gap between the energy that can be absorbed in the upper extremities versus that available in a fall.
There are additional limitations of this study worth noting. The resolution of our reported peak energy absorptions may have been limited by performing trials at discreet increments of 15° in body lean angle. Although this was important to minimize participant fatigue, a participant’s maximum energy absorption may have been observed at a body lean angle between two performed levels or at a lean angle slightly larger than the maximum performed angle. However, the latter scenario is unlikely as 13 of 20 older participants absorbed greater energy at a lean angle smaller than their maximum performed angle. It is also possible that a participant may not have performed at her true maximum ability due to fatigue, lack of motivation, or fear of inability to halt downward movement of the body with her arms. We attempted to reduce these effects by providing a safety harness, frequent rest periods, and “coaching” to emphasize and encourage each participant to descend as far as possible. Although we did not calculate individual energy absorptions in the wrist, elbow, and shoulder, previous studies indicate the dominant role in energy absorption of the shoulder over the elbow (8,23). Furthermore, we calculated arm deflection based on the distance between the wrist and acromion markers and did not specifically measure and include shoulder retraction in our estimates of arm deflection. This may have contributed to an underestimation of energy absorption for both our young and older participants.
Finally, it is important to note that, although upper extremity impact is protective for reducing the risk for head injury and hip fracture, it obviously increases one’s risk for fracture or dislocation at the wrist, hand, or elbow during a fall. Thus, we recommend that exercise programs train individuals to “break the fall” in a way that also minimizes their risk for upper extremity injury. For example, DeGoede and Ashton-Miller (9) have shown that impact forces are reduced substantially by flexing the elbow just before descent, and Groen et al. (24) recently showed that older adults can be trained over a few sessions in using a martial arts falling technique.
FUNDING
This study was supported by grants from the Centers for Disease Control and Prevention (R49CCR019355), National Institutes of Health (R01AR46890), Canadian Institutes of Health Research, and the Michael Smith Foundation for Health Research. M.M.S. is a Canadian Institutes of Health Research and Michael Smith Foundation for Health Research postdoctoral fellow. S.N.R. holds a Canada Research Chair in Injury Prevention and Mobility Biomechanics.
References
- 1.The Economic Burden of Unintentional Injury in Canada. Toronto, Canada: SMARTRISK: 1998. [Google Scholar]
- 2.Nevitt MC, Cummings SR. Type of fall and risk of hip and wrist fractures: the study of osteoporotic fractures. The Study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 1993;41:1226–1234. doi: 10.1111/j.1532-5415.1993.tb07307.x. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz AV, Kelsey JL, Sidney S, et al. Characteristics of falls and risk of hip fracture in elderly men. Osteoporos Int. 1998;8:240–246. doi: 10.1007/s001980050060. [DOI] [PubMed] [Google Scholar]
- 4.Feldman F, Robinovitch SN. Reducing hip fracture risk during sideways falls: evidence in young adults of the protective effects of impact to the hands and stepping. J Biomech. 2007;40:2612–2618. doi: 10.1016/j.jbiomech.2007.01.019. [DOI] [PubMed] [Google Scholar]
- 5.Hsiao ET, Robinovitch SN. Common protective movements govern unexpected falls from standing height. J Biomech. 1998;31:1–9. doi: 10.1016/s0021-9290(97)00114-0. [DOI] [PubMed] [Google Scholar]
- 6.Robinovitch SN, Normandin SC, Stotz P, et al. Time requirement for young and elderly women to move into a position for breaking a fall with outstretched hands. J Gerontol A Biol Sci Med Sci. 2005;60:1553–1557. doi: 10.1093/gerona/60.12.1553. [DOI] [PubMed] [Google Scholar]
- 7.DeGoede KM, Ashton-Miller JA. Biomechanical simulations of forward fall arrests: effects of upper extremity arrest strategy, gender and aging-related declines in muscle strength. J Biomech. 2003;36:413–420. doi: 10.1016/s0021-9290(02)00396-2. [DOI] [PubMed] [Google Scholar]
- 8.Chiu J, Robinovitch SN. Prediction of upper extremity impact forces during falls on the outstretched hand. J Biomech. 1998;31:1169–1176. doi: 10.1016/s0021-9290(98)00137-7. [DOI] [PubMed] [Google Scholar]
- 9.DeGoede KM, Ashton-Miller JA. Fall arrest strategy affects peak hand impact force in a forward fall. J Biomech. 2002;35:843–848. doi: 10.1016/s0021-9290(02)00011-8. [DOI] [PubMed] [Google Scholar]
- 10.Cummings SR, Black DM, Rubin SM. Lifetime risks of hip, Colles’, or vertebral fracture and coronary heart disease among white postmenopausal women. Arch Intern Med. 1989;149:2445–2448. [PubMed] [Google Scholar]
- 11.Jaglal SB, Weller I, Mamdani M, et al. Population trends in BMD testing, treatment, and hip and wrist fracture rates: are the hip fracture projections wrong? J Bone Miner Res. 2005;20:898–905. doi: 10.1359/JBMR.041231. [DOI] [PubMed] [Google Scholar]
- 12.Bouras T, Stranjalis G, Korfias S, et al. Head injury mortality in a geriatric population: differentiating an “edge” age group with better potential for benefit than older poor-prognosis patients. J Neurotrauma. 2007;24:1355–1361. doi: 10.1089/neu.2005.370. [DOI] [PubMed] [Google Scholar]
- 13.Malik SA, Murphy M, Connolly P, et al. Evaluation of morbidity, mortality and outcome following cervical spine injuries in elderly patients. Eur Spine J. 2008;17:585–591. doi: 10.1007/s00586-008-0603-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schrag SP, Toedter LJ, McQuay N., Jr Cervical spine fractures in geriatric blunt trauma patients with low-energy mechanism: are clinical predictors adequate? Am J Surg. 2008;195:170–173. doi: 10.1016/j.amjsurg.2007.09.029. [DOI] [PubMed] [Google Scholar]
- 15.Sharma OP, Oswanski MF, Sharma V, et al. An appraisal of trauma in the elderly. Am Surg. 2007;73:354–358. [PubMed] [Google Scholar]
- 16.Robinovitch SN, Inkster L, Maurer J, et al. Strategies for avoiding hip impact during sideways falls. J Bone Miner Res. 2003;18:1267–1273. doi: 10.1359/jbmr.2003.18.7.1267. [DOI] [PubMed] [Google Scholar]
- 17.Sran MM, Khan KM. Physiotherapy and osteoporosis: practice behaviors and clinicians’ perceptions—a survey. Man Ther. 2005;10:21–27. doi: 10.1016/j.math.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 18.Frischknecht R. Effect of training on muscle strength and motor function in the elderly. Reprod Nutr Dev. 1998;38:167–174. doi: 10.1051/rnd:19980203. [DOI] [PubMed] [Google Scholar]
- 19.Cogley RM, Archambault TA, Fibeger JF, et al. Comparison of muscle activation using various hand positions during the push-up exercise. J Strength Cond Res. 2005;19:628–633. doi: 10.1519/15094.1. [DOI] [PubMed] [Google Scholar]
- 20.Vellas BJ, Wayne SJ, Garry PJ, et al. A two-year longitudinal study of falls in 482 community-dwelling elderly adults. J Gerontol A Biol Sci Med Sci. 1998;53:M264–M274. doi: 10.1093/gerona/53a.4.m264. [DOI] [PubMed] [Google Scholar]
- 21.O’Neill TW, Varlow J, Silman AJ, et al. Age and sex influences on fall characteristics. Ann Rheum Dis. 1994;53:773–775. doi: 10.1136/ard.53.11.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thelen DG. Adjustment of muscle mechanics model parameters to simulate dynamic contractions in older adults. J Biomech Eng. 2003;125:70–77. doi: 10.1115/1.1531112. [DOI] [PubMed] [Google Scholar]
- 23.Robinovitch SN, Chiu J. Surface stiffness affects impact force during a fall on the outstretched hand. J Orthop Res. 1998;16:309–313. doi: 10.1002/jor.1100160306. [DOI] [PubMed] [Google Scholar]
- 24.Groen BE, Smulders E, de Kam D, Duysens J, Weerdesteyn V. Martial arts fall training to prevent hip fractures in the elderly. Osteoporosis Int. doi: 10.1007/s00198-009-0934-x. Published online 01 May 2009. [DOI] [PubMed] [Google Scholar]