Abstract
The involvement of central nervous system is rare in acute promyelocytic leukemia (APL). We report a APL patient of a 41 yr-old Korean male who presented with fever and petechia. Complete molecular remission was achieved with all-trans retinoic acid (ATRA), idarubicin, and cytarabine. Ten months later, he complained of a mild headache. The results of the physical examination and the complete blood counts were normal. The examination of cerebrospinal fluid showed the presence of promyelocyte. Bone marrow studies showed cytogenetic remission but with molecular relapse. He was treated with intrathecal and systemic chemotherapy.
Keywords: Leukemia, Promyelocytic, Acute; Central Nervous System; Recurrence
INTRODUCTION
Acute promyelocytic leukemia (APL) is characterized by the presence of atypical promyelocytes in bone marrow and peripheral blood. APL is distinguished from other subtypes of acute myeloid leukemia (AML) by its distinctive morphology, younger patient age at presentation, specific chromosomal abnormality, associated coagulopathy, and unique response to treatment with retionic acid. All-trans retinoic acid (ATRA) and intensive chemotherapy with ara-C and anthracycline is recommended as the standard treatment for APL (1). Although ATRA has improved the outcome of APL, early bleeding diathesis and recurrence are main causes of death in patients with APL.
The involvement of central nervous system (CNS) in AML is an uncommon finding. Patients at the highest risk for developing the leukemia in CNS include those with a high circulating blast count, elevated lactate dehydrogenase activity, and one of the monocytic leukemic subtypes (2, 3). Moreover, leptomeningeal leukemic infiltration is rarely observed in patients with APL.
We report a case of leptomeningeal relapse in a patient with a variant APL who had achieved complete remission after ATRA, idarubicin and cytarabine therapy. Furthermore, we discuss the clinical manifestation and treatment of APL in CNS in comparison of the results from our patients with those of the previously reported cases.
CASE REPORT
A 41 yr-old man was presented with fever and generalized petechiae. The full blood count showed a hemoglobin level of 7.7 g/dL, a WBC count of 38.3×109/L consisting of 84% blasts, and a platelet count of 25×109/L. A coagulation test demonstrated severe disseminated intravascular coagulation (DIC), with a prothrombin time of 15 sec, a partial thromboplastin time of 81 sec, and a fibrinogen of 100 mg/dL. A bone marrow examination showed APL, which was confirmed by the presence of t(15;17)(q22;q21) on karyotypic analysis and PML/RARA on molecular analysis. Flow cytometry revealed leukemic cells positive for CD13 and CD33 expression, and negative for the expression of HLA-DR. Induction chemotherapy with idarubicin, ara-C (idarubicin 12 mg/m2/day intravenous i.v. on Days 1-3, ara-C100 mg/m2/day continuous iv for 24 hr on Days 1-7) and ATRA at 45 mg/m2, which was scheduled to be given until 30 days after complete remission, led to complete remission on Day 25 of the treatment. Analysis of bone marrow revealed a normal karyotype as well as absence of the PML/RARA rearrangement. The patient received a consolidation with three consecutive courses of idarubicin, and then a maintenance with ATRA (at 45 mg/m2 on Days 1-15, every other month for 2 yr).
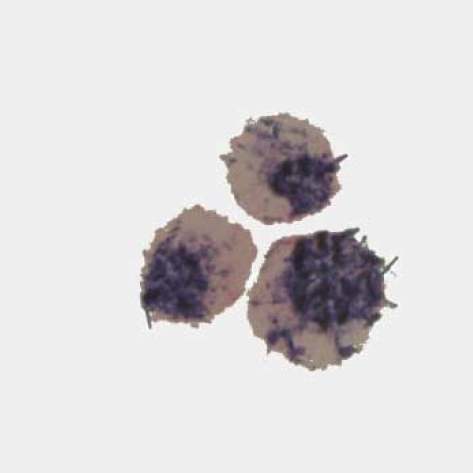
Ten months later, he complained of a mild non-specific headache for two weeks of duration. The physical examination was unremarkable. His complete blood counts were normal. Magnetic resonance imaging study showed multifocal leptomeningeal enhancement in both the frontal and parietal areas in enhanced T1-weighted image. Examination of cerebrospinal fluid (CSF) showed the presence of atypical promyelocytes (Fig. 1). The bone marrow smear showed a complete hematologic and cytogenetic remission, but molecular studies showed the presence of PML/RARA rearrangement in the bone marrow and in the CSF.
Fig. 1.
Cells in cerebrospinal fluid with APL morphologic feature are noted (peroxidase stain, ×1,000).
The diagnosis of meningeal relapse of APL was made, and he was treated with intrathecal methotrexate and ara-C (methotrexate 12 mg and ara-C 100 mg administered twice a week for four weeks), followed by high-dose systemic chemotherapy (ara-C 3.0 g/m2 i.v. b.i.d. on Days 1-4, mitoxantrone 12 mg/m2/day i.v. on Days 3-5). At the end of the intrathecal chemotherapy his CSF analysis became normal, but blood and bone marrow evaluations at this time showed hematologic relapse. He died of neutropenic fever on Day 12 of his systemic therapy.
DISCUSSION
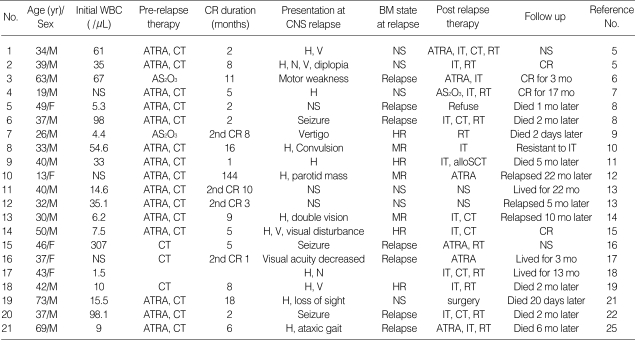
Extramedullary leukemic infiltration is rarely observed in patients with APL. The extramedullary sites reported are skin, CNS, middle ear, lung, lymph node, mediastinum, thymus, spine, breast, pelvis, and gingiva. The most common site is skin (4). To our knowledge, only 31 cases of APL in CNS have been reported (4-25). A summary of 21 cases of APL in CNS is listed in Table 1. Fourteen of those 19 patients were male. The age range of these patients was from 13 to 73 yr with a median age of 39. Twenty patients showed evidence of APL in CNS at the time of relapse. Only one case who had been treated for a non-Hodgkin's lymphoma with chemotherapy and radiotherapy ten months ago had an intracerebral leukemic mass at the onset of leukemia (18). Of the 20 relapsed patients, the duration of remission ranged from 1 to 144 months, with a median of five months. Four patients were in a secondary remission state. Magnetic resonance imaging study or CT scan was performed on ten patients; seven cases showed evidence of mass and three cases did not show any pathologic alteration. Magnetic resonance imaging study from our case showed leptomeningeal enhancement only without mass formation. Lumbar puncture was performed in all patients, and the result showed that all patients had leukemic cells in the CSF.
Table 1.
Reported cases of acute promyelocytic leukemia of the central nervous system
NS, not stated; CT, chemotherapy; CR, complete remission; H, headache; V, vomiting; N, nausea; Relapse hematologic relapse, HR, hematologic remission; MR, molecular remission; IT, intrathecal chemotherapy; RT, radiotherapy.
The symptoms of APL in CNS are headache, vertigo, nausea, vomiting, visual disturbance, motor weakness, and seizure. In our case, he complained of a non-specific, mild headache. Although CNS involvement of APL is rare, CSF studies should be performed when symptoms of CNS occur. Interestingly, recurrence in CNS did not coincide with a hematologic relapse. Hematologic remission was maintained in nine cases when a CNS relapse was found (5, 7, 9-12, 14, 15, 19). A molecular study to find the RARA rearrangement in the bone marrow was performed in five cases at the time of CNS relapse. Three cases sustained a molecular remission (10, 12, 14).
Because an increasing number of reports have been published on extramedullary localization in APL, at the time of relapse, following the advent ATRA treatment, the question arises as to whether treatment of APL with ATRA predisposes patients to the development of extramedullary relapse. There are two reports of CNS relapse after arsenic trioxide (AS2O3) treatment (7, 9). Several biologic effects, modulated by ATRA, have been suggested to play a role in extramedullary leukemic infiltration, such as increased expression of certain adhesion molecule (26, 27). It is possible that a similar differentiation and regulation of adhesion molecules, as seen with ATRA therapy, occurs with the use of AS2O3. The risk factors associated with extramedullary relapse are high WBC count on presentation and the ATRA syndrome (8, 13). A GIMEMA study compared the relapse pattern in APL patients enrolled into two consecutive large studies. Patients receiving ATRA, in addition to chemotherapy, have no increased risk of developing extramedullary disease at the time of relapse as compared with APL patients treated with chemotherapy alone. However, higher prevalence of CNS involvement was detected in patients receiving ATRA (28). In the literature review, only three among 21 cases with CNS relapse received systemic chemotherapy without ATRA.
Despite the impressive complete remission and survival results of APL, the prognosis for relapsed APL is generally poor. Treatment of CNS relapse consists of intrathecal chemotherapy, radiotherapy, systemic chemotherapy (with high-dose cytarabine which passes through the blood brain barrier), and agents for cytodifferentiation such as ATRA. Six cases with CNS relapse were treated with combination therapy including ATRA, and they achieved the complete remission as next (5, 6, 12, 16, 17, 25). Four of the six cases who were treated with ATRA for relapsed APL had received ATRA previously (5, 6, 12, 25). The durations of their first complete remission are 2, 6, 11 and 144 months. In our case, because he received ATRA for maintenance therapy when the CNS relapse was found, we treated him with intrathecal therapy and with high-dose systemic chemotherapy. Recently, AS2O3 has represented a useful salvage treatment for APL patients who relapsed after or refractory to ATRA and chemotherapy (29). AS2O3 may also be an option for patients with relapsed APL in the CNS.
In summary, we presented an APL case with meningeal relapse. CNS involvement of APL is rare, but CNS is a possible site of relapse in a patient with complete remission after treatment of APL. We think that it is necessary to do a complete evaluation and diagnostic approach, including CSF studies, if CNS symptoms occur in patients with APL, even though hematologic parameters sustain remission.
References
- 1.Fenaux P, Le Deley MC, Castaigne S, Archimbaud E, Chomienne C, Link H, Guerci A, Duarte M, Daniel MT, Bowen D, et al. Effect of all-trans-retinoic acid in newly diagnosed acute promyelocytic leukemia. Result of a multicenter randomized trial. European APL 91 Group. Blood. 1993;82:3241–3249. [PubMed] [Google Scholar]
- 2.Dekker AW, Elderson A, Punt K, Sixma JJ. Meningeal involvement in patients with acute nonlymphocytic leukemia. Incidence, management, and predictive factors. Cancer. 1985;56:2078–2082. doi: 10.1002/1097-0142(19851015)56:8<2078::aid-cncr2820560832>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 3.Cassileth PA, Sylvester LS, Bennett JM, Begg CB. High peripheral blast count in adult acute myelogenous leukemia is a primary risk factor for CNS leukemia. J Clin Oncol. 1988;6:495–498. doi: 10.1200/JCO.1988.6.3.495. [DOI] [PubMed] [Google Scholar]
- 4.Wiernik PH, De Bellis R, Muxi P, Dutcher JP. Extramedullary acute promyelocytic leukemia. Cancer. 1996;78:2510–2514. doi: 10.1002/(sici)1097-0142(19961215)78:12<2510::aid-cncr10>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 5.Colovic N, Bogdanovic A, Miljic P, Jankovic G, Colovic M. Central nervous system relapse in acute promyelocytic leukemia. Am J Hematol. 2002;71:60–61. doi: 10.1002/ajh.10158. [DOI] [PubMed] [Google Scholar]
- 6.Patriarca F, Fili C, Geromin A, Sperotto A, Prosdocimo S, Fanin R. Activity of all-trans-retinoic acid in a case of central nervous system extramedullary relapse of acute promyelocytic leukemia. Eur J Haematol. 2002;68:310–313. doi: 10.1034/j.1600-0609.2002.01660.x. [DOI] [PubMed] [Google Scholar]
- 7.Mathews V, Balasubramanian P, Shaji RV, George B, Chandy M, Srivastava A. Central nervous system relapse in a patient with acute promyelocytic leukaemia treated with arsenic tri-oxide. Br J Haematol. 2001;113:257–258. doi: 10.1046/j.1365-2141.2001.02673-4.x. [DOI] [PubMed] [Google Scholar]
- 8.Evans GD, Grimwade DJ. Extramedullary disease in acute promyelocytic leukemia. Leuk Lymphoma. 1999;33:219–229. doi: 10.3109/10428199909058422. [DOI] [PubMed] [Google Scholar]
- 9.Au WY, Ma SK, Ooi C, Liang R, Kwong YL. Unusual manifestations of acute leukemia. Case 1. CNS extramedullary relapse of acute promyelocytic leukemia after arsenic trioxide-induced remission. J Clin Oncol. 2000;18:3435–3437. doi: 10.1200/JCO.2000.18.19.3435. [DOI] [PubMed] [Google Scholar]
- 10.Anguita E, Villegas A, Gonzalez FA, Diaz-Mediavilla J, Lo Coco F. Acute promyelocytic leukemia relapse in the central nervous system during hematologic and molecular remission. Am J Hematol. 1999;60:170–171. doi: 10.1002/(sici)1096-8652(199902)60:2<170::aid-ajh21>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 11.Molero T, Valencia JM, Gomez-Casares MT. Central nervous system (CNS) infiltration in a case of promyelocytic leukemia. Haematologica. 1997;82:637. [PubMed] [Google Scholar]
- 12.Mesa JR, Espinosa E, Losada R, Hernandez C, Martinez G, Hernandez P. Parotid and central nervous system relapse during complete hematologic remission in acute promyelocytic leukemia. Haematologica. 1999;84:565–566. [PubMed] [Google Scholar]
- 13.Ko BS, Tang JL, Chen YC, Yao M, Wang CH, Shen MC, Tien HF. Extramedullary relapse after all-trans retinoic acid treatment in acute promyelocytic leukemia--the occurrence of retinoic acid syndrome is a risk factor. Leukemia. 1999;13:1406–1408. doi: 10.1038/sj.leu.2401495. [DOI] [PubMed] [Google Scholar]
- 14.Liso V, Specchia G, Pogliani EM, Palumbo G, Mininni D, Rossi V, Teruzzi E, Mestice A, Coppi MR, Biondi A. Extramedullary involvement in patients with acute promyelocytic leukemia: a report of seven cases. Cancer. 1998;83:1522–1528. [PubMed] [Google Scholar]
- 15.Martino B, Vincelli I, Marino A, Comis M, Ronco F, Nobile F. Meningeal relapse in a patient with acute promyelocytic leukaemia treated with all-trans retinoic acid. Br J Haematol. 1998;100:606–607. doi: 10.1046/j.1365-2141.1998.0636c.x. [DOI] [PubMed] [Google Scholar]
- 16.Lederman CA, Weisberger J, Seiter K, Feldman EJ. Differentiation of extramedullary acute promyelocytic leukemia by all-trans-retinoic acid. Leuk Lymphoma. 1995;18:189–193. doi: 10.3109/10428199509064942. [DOI] [PubMed] [Google Scholar]
- 17.Brown DM, Kimura AE, Ossoinig KC, Weiner GJ. Acute promyelocytic infiltration of the optic nerve treated by oral trans-retinoic acid. Ophthalmology. 1992;99:1463–1467. doi: 10.1016/s0161-6420(92)31783-x. [DOI] [PubMed] [Google Scholar]
- 18.Kanakura Y, Yonezawa T, Hamaguchi Y, Otsuka A, Matayoshi Y, Kondoh H, Tamaki T, Katagiri S, Kanayama Y, Nishiura T, Aozasa K, Tarui S. Acute promyelocytic leukemia with an intracerebral mass and meningeal involvement after treatment of non-Hodgkin's lymphoma. Cancer. 1987;59:94–98. doi: 10.1002/1097-0142(19870101)59:1<94::aid-cncr2820590121>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 19.Solano Vercet C, Escudero A, Fernandez-Ranada JM. Meningeal relapse in acute promyelocytic leukaemia. Acta Haematol. 1983;70:137–138. [PubMed] [Google Scholar]
- 20.Marra R, Stori S, Pagano L, Fioritoni G, Rabitti C, Sica S, Leone G, Torlontano G, Bizzi B. Central nervous system acute promyelocytic leukaemia: a report of three cases. Haematologia (Budap) 1989;22:195–199. [PubMed] [Google Scholar]
- 21.Lugassy G, Halperin Y. Pituitary relapse of acute promyelocytic leukemia after ATRA. Int J Hematol. 1998;68:101–102. [PubMed] [Google Scholar]
- 22.Currie J, Chee YL, Culligan DJ. Central nervous system relapse in acute promyelocytic leukaemia treated with ATRA. Br J Haematol. 1997;99:469. [PubMed] [Google Scholar]
- 23.Pogliani EM, Fowst C, Marozzi A, Salvatore M, Polli EE. Cerebral parenchymal involvement in acute promyelocytic leukemia. A case report. Haematologica. 1988;73:71–73. [PubMed] [Google Scholar]
- 24.Seldon M, Enno A. Central nervous system relapse in acute promyelocytic leukaemia treated with all-trans retinoic acid. Aust N Z J Med. 1998;28:462. doi: 10.1111/j.1445-5994.1998.tb02082.x. [DOI] [PubMed] [Google Scholar]
- 25.Burry LD, Seki JT. CNS relapses of acute promyelocytic leukemia after all-trans retinoic acid. Ann Pharmacother. 2002;36:1900–1906. doi: 10.1345/aph.1A471. [DOI] [PubMed] [Google Scholar]
- 26.Marchetti M, Falanga A, Giovanelli S, Oldani E, Barbui T. All-trans-retinoic acid increases adhesion to endothelium of the human promyelocytic leukaemia cell line NB4. Br J Haematol. 1996;93:360–366. doi: 10.1046/j.1365-2141.1996.4911029.x. [DOI] [PubMed] [Google Scholar]
- 27.Saiki I, Fujii H, Yoneda J, Abe F, Nakajima M, Tsuruo T, Azuma I. Role of aminopeptidase N (CD13) in tumor-cell invasion and extracellular matrix degradation. Int J Cancer. 1993;54:137–143. doi: 10.1002/ijc.2910540122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Specchia G, Lo Coco F, Vignetti M, Avvisati G, Fazi P, Albano F, Di Raimondo F, Martino B, Ferrara F, Selleri C, Liso V, Mandelli F. Extramedullary involvement at relapse in acute promyelocytic leukemia patients treated or not with all-trans retinoic acid: a report by the Gruppo Italiano Malattie Ematologiche dell'Adulto. J Clin Oncol. 2001;19:4023–4028. doi: 10.1200/JCO.2001.19.20.4023. [DOI] [PubMed] [Google Scholar]
- 29.Soignet SL, Frankel SR, Douer D, Tallman MS, Kantarjian H, Calleja E, Stone RM, Kalaycio M, Scheinberg DA, Steinherz P, Sievers EL, Coutre S, Dahlberg S, Ellison R, Warrell RP., Jr United States multicenter study of arsenic trioxide in relapsed acute promyelocytic leukemia. J Clin Oncol. 2001;19:3852–3860. doi: 10.1200/JCO.2001.19.18.3852. [DOI] [PubMed] [Google Scholar]