Abstract
Neuropeptide Y (NPY) is a cotransmitter with norepinephrine (NE) and ATP in sympathetic nerves. There is evidence for increased activity of the sympathetic nervous system and the renin-angiotensin system (RAS), as well as a role for NPY in the development of hypertension in experimental animal models and in humans. Angiotensin II (ANG II) is known to facilitate sympathetic neurotransmission, an effect greater in spontaneously hypertensive rats (SHR) than normotensive Wistar-Kyoto (WKY) rats. A newly discovered product of the RAS is angiotensin-(1–7) [ANG-(1–7)]. There is evidence suggesting that ANG-(1–7) opposes the actions of ANG II, resulting in hypotensive effects. The objective of this study was to investigate the role of ANG-(1–7) on the nerve-stimulated overflow of NE and NPY from the mesenteric arterial bed of SHR and the mechanisms involved in mediating any effects produced. ANG-(1–7) (0.001, 0.01, 0.1 μM) decreased nerve-stimulated NE and NPY overflow, as well as perfusion pressure in preparations obtained from SHR. This effect was greater in preparations of SHR than WKY controls. In addition, ANG-(1–7) decreased NE overflow to a greater extent than NPY overflow. Administration of the Mas receptor antagonist, d-Ala7 ANG-(1–7), attenuated the decrease in both NE and NPY overflow due to ANG-(1–7) administration. However, the angiotensin type 2 receptor antagonist, PD-123391, attenuated the effect of ANG-(1–7) on NE overflow without affecting the decrease in NPY overflow. Moreover, in the presence of NG-nitro-l-arginine methyl ester, ANG-(1–7) decreased NPY overflow, but not NE overflow. ANG-(1–7) decreases the nerve-stimulated overflow of NE and NPY in preparations of SHR, whereas ANG II enhances it. Therefore, ANG-(1–7) may counteract the effects of ANG II by acting on ANG type 2 and Mas receptors.
Keywords: sympathetic neurotransmission, nitric oxide, bradykinin, mesenteric artery
sympathetic nerves synthesize and release the neurotransmitters norepinephrine (NE), neuropeptide Y (NPY), and adenosine triphosphate (ATP) (37, 42). Each neurotransmitter mimics a specific phase of the sympathetic nerve stimulation (NS) when administered to tissue preparations innervated by sympathetic nerves (37, 33). Postjunctionally, NE, NPY, and ATP produce contraction of vascular smooth muscle through the activation of α1, Y1, and P2X receptors, respectively. Prejunctionally, these mediators activate the α2, Y2, and P2Y receptors, respectively, resulting in feedback inhibition of their own release, as well as the release of each other (53, 57).
In addition to the sympathetic nervous system (SNS) and its cotransmitters, the renin-angiotensin system (RAS) is also an important modulator of vascular tone. The RAS was originally viewed solely as a hormonal circulating system involved in salt, water, and blood pressure homeostasis. However, current evidence recognizes distinct components of the RAS that are active locally in the vasculature, heart, and other tissues (6, 41). Although angiotensin (ANG) II is a key mediator of the actions of the RAS, it is now known that this system results in the synthesis of other peptides, which also have important physiological and biological actions. One of these is the heptapeptide ANG-(1–7). There are numerous studies demonstrating ANG-(1–7) to be a major physiologically active product of the RAS (12, 46, 48, 54). Ferrario and colleagues have suggested that ANG-(1–7) acts as an endogenous inhibitor of ANG II, therefore providing a negative feedback mechanism for the regulation of the hypertensive action of ANG II, and contributing to the antihypertensive effects of ANG converting enzyme (ACE) inhibitors and ANG type 1 (AT1) receptor blockers (ARB) (24). The receptor site of action of ANG-(1–7) is somewhat controversial. In some investigations, ANG-(1–7) has acted through non-AT1/AT2-receptor mediated mechanisms, whereas, in others, its effects have been blocked by either AT1- or AT2-receptor antagonists (17, 49). However, most evidence suggests that the heptapeptide is an endogenous ligand for the G-protein-coupled receptor Mas. The genetic deletion of this receptor abolishes the ANG-(1–7)-induced relaxation and antidiuretic responses in the mouse, suggesting that Mas is a functional receptor for ANG-(1–7) (47). ANG-(1–7) may oppose the actions of ANG II, either through direct activation of Mas receptors, or by stimulating the release of nitric oxide (NO), bradykinin, and prostaglandins through the activation of either Mas or AT2 receptors (2, 3, 15, 32).
ANG-(1–7) was reported to inhibit the evoked release of NE from hypothalamic preparations, with a greater effect in hypertensive rats than in normotensive rats (18, 19). A similar inhibitory effect of ANG-(1–7) was observed on the ANG I- and ANG II-induced facilitation of NE release from the perfused rat kidneys of both normotensive and hypertensive rats (54). On the contrary, ANG-(1–7) enhanced the evoked release of NE from rat atrial preparations in a manner similar to ANG II (17). Due to controversy about the effects and mechanism of action of ANG-(1–7), further research is needed to elucidate the role of this peptide in sympathetic neurotransmission modulation.
The perfused mesenteric arterial bed of the rat contains a dense sympathetic innervation and represents an excellent model of the vascular neuroeffector junction. Spontaneously hypertensive rats (SHR) have been extensively studied, and it is well established that these animals develop hypertension as they age (22, 38, 40, 45, 58, 62). In addition, the facilitating effect of the RAS on sympathetic neurotransmission in SHR has been shown to be increased compared with that in normotensive controls, suggesting a dysfunction in the interaction between RAS and the SNS in this model of hypertension (11, 25, 36, 39, 43).
The purpose of this study was to investigate the effects of ANG-(1–7) on the nerve NS-induced increase in perfusion pressure and NE and NPY overflow from the mesenteric arterial bed of 10- to 12-wk-old SHR and compare it to age-matched normotensive WKY controls. In our recently published data, we show that ANG II enhances sympathetic neurotransmission in SHR to a greater extent than WKY, even at a prehypertensive stage in their development, suggesting a possible mechanism for the development of hypertension in this model (4). In this study, we show that ANG-(1–7) does indeed modulate sympathetic neurotransmitter overflow in a manner that may oppose the effects of ANG II on sympathetic neurotransmission.
MATERIALS AND METHODS
Materials.
ANG-(1–7), captopril (ACE inhibitor), EMD66684 (AT1 receptor antagonist), PD-123319 (AT2 receptor antagonist), l-NAME (NG-nitro-l-arginine methyl ester, NO synthase inhibitor), bradyzine (B2 receptor antagonist), the protease inhibitor cocktail (for mammalian cell and tissue extracts), and Krebs' buffer salts were all purchased from Sigma (St. Louis, MO). (d-Ala7)-ANG-(1–7) (Mas-receptor antagonist) was purchased from Bachem. The NPY EIA kit was purchased from Peninsula Laboratories (San Carlos, CA).
Animals.
We used 10- to 12-wk-old age-matched male Wistar Kyoto (WKY) and SHR in all of our experiments. We used 10- to 12-wk-old rats because we consistently found in our studies that the blood pressure starts to rise around 8 wk of age in SHR compared with normotensive WKY, and they are fully hypertensive by 10–12 wk of age. Animals were housed two to four per cage, in constant temperature and 12:12 h light-dark cycle room. Rats were fed standard rat chow and water at will, and they were under the supervision of the Department of Comparative Medicine. All of the experimental procedures carried out were in accordance with the National Institutes of Health guidelines and were approved by the Institutional Animal Care and Use committee of St. Louis University Health Sciences Center.
Isolated, perfused mesenteric preparation of the rat: surgery.
The rats were anesthetized with an intraperitoneal injection of pentobarbital sodium at a dose of 50 mg/kg. The abdomen was opened, and the intestine was excised by ligations of the descending colon proximal to the rectum, duodenum distal to the stomach, and the superior mesenteric artery distal to the abdominal aorta. The isolated intestine with the mesentery attached was than spread in a petri dish containing Krebs' physiological buffer (composed of, in mM: 120 NaCl, 5.0 KCl, 2.4 CaCl2, 1.2 MgSO4, 0.027 EDTA, 11 glucose, and 25 NaHCO3). The superior mesenteric artery was cannulated with a 20-gauge cannula, and 10% heparin solution was flushed through the mesenteric vascular bed. The four main branches of the mesenteric artery feeding the terminal ileum were located and left intact. The remaining branches were ligated and severed. The mesenteric vascular bed was then carefully detached from the intestine. The preparation was placed in an organ bath maintained at 37°C and perfused with aerated Krebs buffer (pH 7.4), by a Gilson minipuls pump at a rate of 2.5 ml/min, and superfused at a rate of 0.5 ml/min. The perfusion pressure was continuously monitored through a pressure transducer coupled with a Grass recorder. The preparation was allowed to equilibrate for 40 min before experimentation began. All drugs used were dissolved in the Krebs' buffer and delivered by continuous infusion. A protease inhibitor cocktail (50 μl/1 g tissue) was added to the Krebs buffer to ensure drug viability.
Isolated, perfused mesenteric preparation of the rat: periarterial NS.
Platinum ring electrodes were placed around the artery, and, when appropriate, the periarterial nerve was stimulated at 16 Hz for 30 s for catecholamine (CA) release, followed by 1.5-min stimulation 15 min later to elicit NPY release, using a Grass S-88 stimulator. The set of stimulations was than repeated 30 min later, in either the presence or absence of drugs. Perfusate effluents were collected continuously in 1-min time frames before, during, and after periarterial NS, into either 1 ml cold 0.4 N perchloric acid with 0.1% cysteine for CA studies, or 1% trifluoroacetic acid for NPY studies. A total collection time of 8 min was employed, with 2 min (basal) before and 6 min during and after stimulation for NPY. For NE, we collected for 6 min (basal) before and 6 min during and after stimulation, for a total collection time of 12 min. The collections were stored at −80°C for maximal stability until they were ready to be assayed.
NE measurement.
NE in acidified release medium, perfusate, and superperfusate samples was identified and quantified by high-pressure liquid chromatography with electrochemical detection. The system consists of a Varian Pro-Star solvent delivery system and a model 9090 autosampler (Varian, Walnut Creek, CA), coupled to a C18 column and an ESA Coulochem II detector. Separations were performed isocratically using a filtered and degassed mobile phase, consisting of 12% methanol, 0.1 M sodium phosphate, 0.2 mM sodium octyl sulfate, and 0.1 mM EDTA, adjusted to pH 2.8 with phosphoric acid. The high-pressure liquid chromatography system is coupled to a computer, where the chromatograms were recorded and analyzed with Varian Star workstation software.
NPY measurement.
The samples collected were pooled in groups of two to facilitate concentration assessment. NPY amounts in the perfusate samples were purified by use of C18 Sep-Pak columns and measured by a 96-well plate enzyme immunoassay kit (Peninsula Laboratories, San Carlos, CA). The 96-well plate was read by a Powerwave X plate reader (Biotek Instruments, Winooski, VT), and the calculation of sample value was analyzed by KC Junior Software (Biotek Instruments).
Statistical analysis of data.
Data are expressed as means ± SE. Statistical analysis was carried out by Student's t-test when comparing increase from basal (Table 1), or by one-way analysis of variance followed by Neuman-Keuls multiple statistical comparison tests when comparing changes across multiple groups (Figs. 1–7). Differences were accepted when P < 0.05.
Table 1.
The effect of NS (16 Hz) on perfusion pressure and NPY and NE overflow in the mesenteric arterial bed obtained from 10- to 12-wk-old WKY or SHR
| Strain | Basal | Nerve Stimulation | Increase (Nerve Stimulation-Basal) | |
|---|---|---|---|---|
| Perfussion pressure, mmHg | WKY | 16.86 ± 1.79 | 86 ± 9.09§ | 69.14 ± 9.6 |
| SHR | 36 ± 2.98 | 193 ± 5.69§ | 157 ± 7† | |
| NPY overflow, ng/ml | WKY | 0.1 ± 0.01 | 0.301 ± 0.049‡ | 0.201 ± 0.039 |
| SHR | 0.24 ± 0.035 | 0.665 ± 0.09‡ | 0.424 ± 0.069* | |
| NE overflow, ng/6 min | WKY | 5.28 ± 0.22 | 7.68 ± 0.22§ | 2.4 ± 0.38 |
| SHR | 7.68 ± 0.42 | 12.88 ± 1.08§ | 5.3 ± 0.84† |
Values are means ± SE; n = 7 Wistar-Kyoto (WKY) or n = 8 spontaneously hypertensive rats (SHR). NPY, neuropeptide Y; NE, norepinephrine. Values are given before (basal) and after nerve stimulation.
P < 0.01 and
P < 0.001 compared with WKY.
P < 0.01 and
P < 0.001 compared with basal.
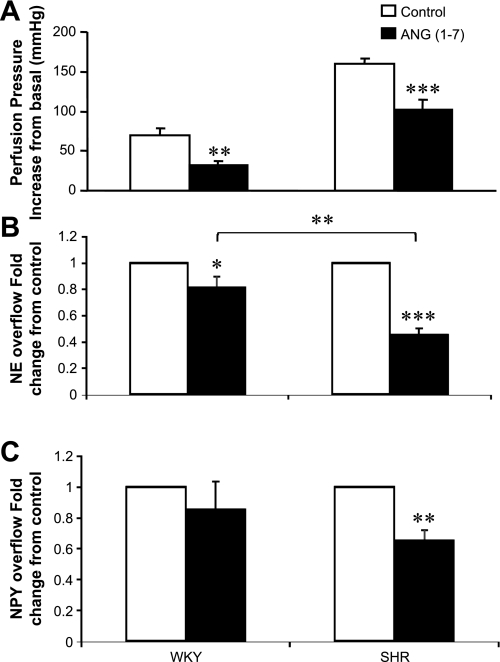
Fig. 1.
Effect of angiotensin (ANG)-(1–7) (0.01 μM) on the nerve stimulation (NS)-induced increase in perfusion pressure (A), norepinephrine (NE; B), and neuropeptide Y (NPY) overflow (C) from the mesenteric beds of 10- to 12-wk-old Wistar-Kyoto (WKY) and spontaneously hypertensive rats (SHR). Values are plotted as mmHg ± SE for perfusion pressure and fold change from control for neurotransmitter release (control set as 1). Each bar is the mean ± SE of 7–9 preparations. *P < 0.05, **P < 0.01, and ***P < 0.001 compared with control.
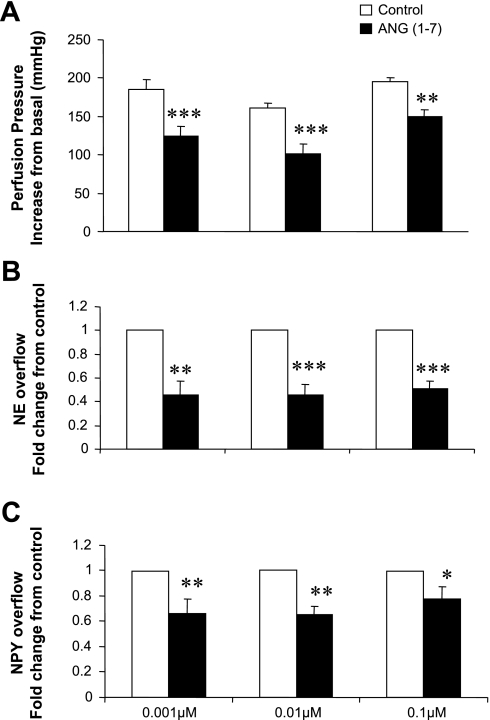
Fig. 2.
Effect of ANG-(1–7) on the NS-induced increase in perfusion pressure (A), NE (B), and NPY overflow (C) from the mesenteric beds of 10- to 12-wk-old SHR. Values are plotted as mmHg ± SE for perfusion pressure and fold change from control for neurotransmitter release [control set as 1; NS in the absence of ANG-(1–7)] in the presence of 0.001, 0.01, and 0.1 μM ANG-(1–7), administered 15 min before and during NS. Each bar is the mean ± SE of 7–9 preparations. *P < 0.05, **P < 0.01, and ***P < 0.001 compared with control.
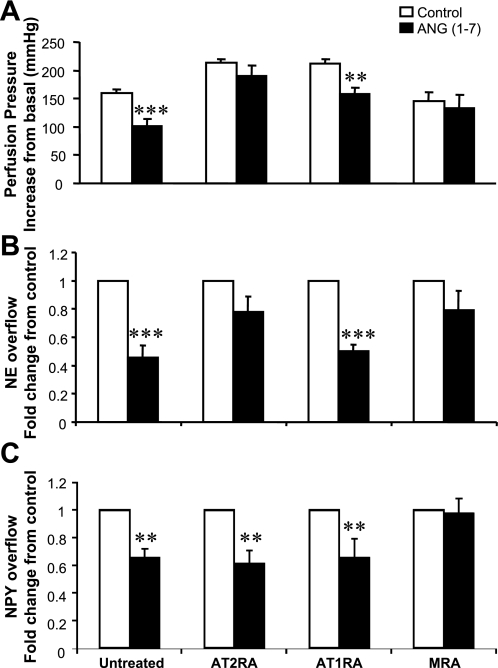
Fig. 3.
Effect of ANG-(1–7) (0.01 μM) on the NS-induced increase in perfusion pressure (A), NE (B), and NPY overflow (C) from the mesenteric beds of 12-wk-old SHR in the presence of the ANG type 2 (AT2) receptor antagonist (AT2RA) PD-123319 (0.1 μM), the AT1 receptor antagonist (AT1RA) EMD66684 (0.1 μM), or the Mas receptor antagonist (MRA) d-Ala7-ANG-(1–7) (0.1 μM). Each bar in A represents the NS-induced increase in perfusion pressure in mmHg ± SE alone (control) and in the presence of ANG-(1–7), or ANG-(1–7) plus an antagonist. In B and C, data are expressed as fold change from control (set as 1; NS in the absence of drugs) in the presence of ANG-(1–7) or in the presence of antagonists. Each bar is the mean ± SE of 7–9 preparations. **P < 0.01, and ***P < 0.001 compared with control.
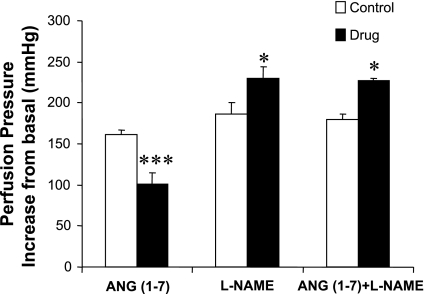
Fig. 4.
Effect of ANG-(1–7), NG-nitro-l-arginine methyl ester (l-NAME), and ANG-(1–7) in the presence of l-NAME on the NS-induced increase in perfusion pressure of the mesenteric arterial bed from 10- to 12-wk-old SHR. l-NAME was administered in a concentration of 30 μM for 45 min before and during NS alone or with ANG-(1–7) (0.01 μM; 15 min). Each bar is the mean increase in perfusion pressure ± SE of 6–7 preparations. *P < 0.05 and ***P < 0.001 compared with control.
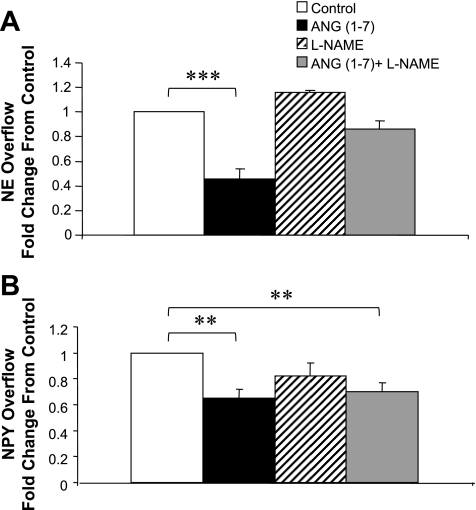
Fig. 5.
Effect of ANG-(1–7) (0.01 μM), l-NAME (30 μM), and ANG-(1–7) in the presence of l-NAME on the NS-induced increase in NE (A) and NPY (B) overflow from the mesenteric arterial bed of 10- to 12-wk-old SHR. Drugs were administered as described in Fig. 4. Data are plotted as the fold change from control (set as 1; NS in the absence of drugs) in the presence of ANG-(1–7), l-NAME, or ANG-(1–7) plus l-NAME. Each bar is the mean ± SE of 6–9 preparations. **P < 0.01 and ***P < 0.001 compared with control.
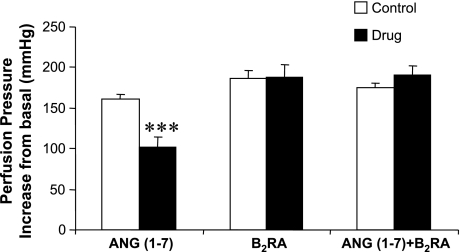
Fig. 6.
Effect of ANG-(1–7), the bradykinin B2 receptor antagonist (B2RA) bradyzine, or ANG-(1–7) plus bradyzine on the NS-induced increase in perfusion pressure in 10- to 12-wk-old SHR mesenteric preparations. Bradyzine was administered in a concentration of 0.1 μM for 15 min alone or in the presence of ANG-(1–7) (0.01 μM), before and during NS. Each bar is the mean increase in perfusion pressure ± SE of 6–7 preparations. ***P < 0.001 compared with control.
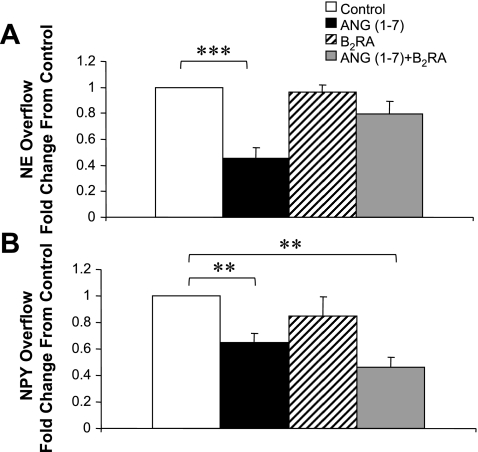
Fig. 7.
Effect of ANG-(1–7), the B2RA bradyzine, or ANG-(1–7) plus bradyzine on the NS-induced increase in NE (A) and NPY (B) overflow from 10- to 12-wk-old SHR mesenteric preparations. Drugs were administered as described in Fig. 4. Data are plotted as fold change from control (set as 1; NS in the absence of drugs) in the presence of ANG-(1–7) (0.01 μM), bradyzine (0.1 μM), or ANG-(1–7) plus bradyzine. **P < 0.01 and ***P < 0.001 compared with control.
RESULTS
Perfusion pressure increase in response to NS is higher in the mesenteric beds from SHR than WKY rats.
The mean basal perfusion pressures of mesenteric beds from WKY and SHR were 16.86 ± 1.79 and 36 ± 2.98 mmHg, respectively, as depicted in Table 1. Periarterial NS at 16 Hz increased the perfusion pressure to 86 ± 9.09 and 193 ± 5.69 mmHg for WKY and SHR, respectively. The increase in perfusion pressure was significantly greater in SHR preparations than WKY controls.
The overflow of NE and NPY from the SHR mesenteric beds is higher than WKY.
Table 1 depicts basal and nerve-stimulated NE and NPY overflow from the mesenteric beds of 10- to 12-wk-old WKY and SHR. Basal NE overflow was 5.28 ± 0.26 and 7.68 ± 0.42 ng/6 min for WKY and SHR, respectively. Upon NS, NE overflow increased to 7.68 ± 0.26 and 12.88 ± 1.08 ng/6 min for WKY and SHR, respectively. The NS-induced change was greater in SHR than WKY preparations. In addition, NS at 16 Hz also increased NPY overflow to 0.301 ± 0.049 and 0.665 ± 0.09 ng/ml in WKY and SHR preparations, respectively. Basal NPY overflow was 0.1 ± 0.01 ng/ml from WKY mesenteric preparations and 0.24 ± 0.035 ng/ml from SHR preparations. The increase in NPY overflow due to NS was also greater in SHR.
ANG-(1–7) attenuates the nerve-stimulated NE and NPY overflow and perfusion pressure responses to a greater extent in mesenteric beds of SHR compared with WKY.
ANG-(1–7) (0.01 μM) reduced the NS-induced increase in perfusion pressure from 69.14 ± 9.34 to 32.85 ± 4.2 mmHg in mesenteric preparations of WKY and from 160.6 ± 6.34 to 101.4 ± 13.2 mmHg in SHR preparations (Fig. 1A). In addition, ANG-(1–7) decreased NE overflow from mesenteric bed of SHR to a greater extent than WKY (e.g., to 0.45 ± 0.08-fold for SHR compared with 0.81 ± 0.05-fold for WKY) (Fig. 1B). ANG-(1–7) (0.01 μM) also decreased the NS-induced NPY overflow from the mesenteric beds of SHR (to 0.65 ± 0.07-fold of control), while it did not affect that from WKY preparations (Fig. 1C). ANG-(1–7) did not alter basal NE and NPY overflow values.
ANG-(1–7) attenuates the NS-induced increase in perfusion pressure, NE, and NPY overflow from SHR mesenteric arterial beds at three different concentrations.
ANG-(1–7) administration 15 min before and during NS resulted in a significant attenuation of the NS-induced increase in perfusion pressure of mesenteric preparations from 10- to 12-wk-old SHR (Fig. 2A). The increase in perfusion pressure was reduced from 185.7 ± 11.9 to 124.3 ± 12.7, 160.6 ± 6.34 to 101.4 ± 13.2, and 195.7 ± 5.3 to 150 ± 8.9 mmHg in the presence of 0.001, 0.01, and 0.1 μM ANG-(1–7), respectively. These changes are depicted as increase from basal, which represents the difference between the NS-induced peak increase in perfusion pressure and the basal perfusion pressure value. ANG-(1–7) did not affect basal perfusion pressure values.
In a similar way as perfusion pressure, ANG-(1–7) at all three concentrations (0.001, 0.01, and 0.1μM) significantly attenuated the NS-induced NE (Fig. 2B) and NPY (Fig. 2C) overflow from the mesenteric beds of 10- to 12-wk-old SHR. NS-induced increase in NE and NPY overflow in the absence of drug was set as one (control), and the fold change from this value in the presence of drug is plotted. NE overflow decreased to 0.45 ± 0.12-, 0.45 ± 0.08-, and 0.51 ± 0.06-fold of control in the presence of 0.001. 0.01, and 0.1 μM ANG-(1–7), respectively. Nerve-stimulated NPY overflow decreased to 0.66 ± 0.11-, 0.65 ± 0.07-, and 0.77 ± 0.1-fold of control due to administration of 0.001, 0.01, and 0.1 μM ANG-(1–7), respectively (Fig. 2C). ANG-(1–7) did not affect basal NE and NPY overflow. The inhibitory effect of ANG-(1–7) on the NS-induced overflow of NE was greater than the effect on NPY overflow.
The effect of ANG-(1–7) on NS-induced increases in perfusion pressure and neurotransmitter overflow from SHR preparations is attenuated in the presence of PD-123319 (AT2-receptor antagonist) and d-Ala7-ANG-(1–7) (Mas-receptor antagonist).
We proceeded to investigate whether the observed effects were the result of a receptor-mediated process, and, if so, which receptor was involved. The mesenteric preparations were pretreated with PD-123319 (AT2 receptor antagonist), EMD66684 (AT1 receptor antagonist), or d-Ala7-ANG-(1–7) (Mas-receptor antagonist) at a concentration of 0.1 μM for 15 min before the administration of ANG-(1–7) (0.01 μM). The results of these experiments are depicted in Fig. 3. Treatment with either antagonist did not alter basal perfusion pressure and neurotransmitter overflow values.
The ANG-(1–7) induced attenuation of the perfusion pressure increase upon periarterial NS was prevented by both the AT2-receptor antagonist PD-123319 and the Mas-receptor antagonist d-Ala7-ANG-(1–7) (Fig. 3A). In contrast, the AT1-receptor antagonist EMD66684 failed to prevent the attenuation by ANG-(1–7) of the NS-induced increase in perfusion pressure.
Similarly, both PD-123319 and d-Ala7-ANG-(1–7) also prevented the ANG-(1–7)-induced attenuation of the nerve-stimulated NE overflow from 10- to 12-wk-old SHR preparations (Fig. 3B). As with perfusion pressure, EMD66684 failed to alter the ANG-(1–7)-induced attenuation of nerve-stimulated NE overflow.
The effects of the three antagonists on the ANG-(1–7)-induced attenuation of nerve-stimulated NPY overflow are depicted in Fig. 3C. Neither the AT1- nor the AT2-receptor antagonist altered the ANG-(1–7)-induced attenuation of evoked NPY overflow in the concentrations utilized. In contrast, the Mas-receptor antagonist d-Ala7-ANG-(1–7) completely reversed the effect.
l-NAME attenuated the effect of ANG-(1–7) on nerve-stimulated perfusion pressure and NE overflow, but not NPY overflow.
We next investigated whether the attenuating effects of ANG-(1–7) on NS-induced increase in perfusion pressure as well as NE and NPY overflow involved the endogenous mediators NO and/or bradykinin.
l-NAME by itself resulted in a rise in the NS-induced increase in perfusion pressure (control = 186 ± 6.55 mmHg; l-NAME = 230 ± 13.6 mmHg) (Fig. 4). The ANG-(1–7)-induced decrease in NS-induced enhancement of perfusion pressure was prevented by l-NAME (Fig. 4). l-NAME by itself did not alter basal perfusion pressure or NE and NPY overflow values.
l-NAME alone did not alter the NS-induced increases in NE and NPY overflow from the mesenteric preparations of 10- to 12-wk-old SHR (1.15 ± 0.024-fold for NE and 0.82 ± 0.1-fold for NPY overflow). In contrast, l-NAME prevented the ANG-(1–7)-induced decrease in the evoked release of NE, but failed to alter the ANG-(1–7)-induced attenuation of the evoked NPY overflow (Fig. 5).
Bradyzine (B2-receptor antagonist) attenuated the effect of ANG-(1–7) on nerve-stimulated perfusion pressure and NE overflow, but not NPY overflow.
The decrease in nerve-stimulated perfusion pressure by ANG-(1–7) was attenuated in the presence of bradyzine (Fig. 6). In addition, pretreatment with the B2-receptor antagonist bradyzine attenuated the reduction in nerve-stimulated NE overflow by ANG-(1–7) (0.80 ± 0.09-fold of control) (Fig. 7). However, the effect of ANG-(1–7) on NPY overflow was not attenuated (0.46 ± 0.07-fold of control) (Fig. 7). The B2-receptor antagonist did not alter basal perfusion pressure or neurotransmitter overflow values. In the presence of bradyzine alone, NS-induced perfusion pressure and neurotransmitter overflow values were 188 ± 15.4 mmHg (control = 186 ± 9.7 mmHg), 0.96 ± 0.06-fold of control (NE overflow), and 0.85 ± 0.14-fold of control (NPY overflow). Data are expressed as previously described.
DISCUSSION
The aim of the present study was to investigate the effect of ANG-(1–7) on NS-induced perfusion pressure changes and neurotransmitter overflow from the perfused mesenteric arterial bed of rats and observe any differences between hypertensive and normotensive strains. In addition, we examined the mechanisms involved in the mediation of the observed effects.
Vascular tone is largely under the control of the SNS. The sympathetic neurotransmitters ATP, NE, and NPY are released from nerve terminals to result in direct postjunctional vasoconstriction, as well as prejunctional feedback inhibition of their own and each others' release (23, 33). We found that NS increases perfusion pressure to a greater extent in mesenteric arterial preparations of SHR than those of WKY controls (Table 1). This was accompanied by greater NE and NPY overflow from SHR preparations upon NS (Table 1). These results are consistent with reported evidence of dysfunction at both the pre- and postjunctional level of neurotransmission in hypertension, resulting in increased levels of neurotransmitter release and enhanced vasoconstriction (9, 16, 20, 21, 26, 52).
As mentioned, the RAS also regulates vascular tone. We have obtained evidence of a functional local RAS in the isolated, perfused mesenteric bed of the rat (4). ANG II has long been considered the main biologically active product of the RAS. ANG II produces multiple actions, including direct vasoconstriction and release of aldosterone from the adrenal cortex via activation of AT1 receptors. In addition, ANG II enhances sympathetic neurotransmission (5, 7, 8, 25, 31, 34–36, 44, 60, 61), which contributes to the vasopressor effects of the peptide. Our recently published data suggest that ANG II enhances both NE and NPY overflow from the mesenteric arterial beds of SHR to a greater extent than from WKY control, even at a prehypertensive stage, suggesting a possible mechanism contributing to the development of hypertension in these animals (4). The discovery of ANG-(1–7) by Ferrario et al. (12–14), of ACE2 by Tipnis et al. (55), and of a functional ANG-(1–7) receptor by Santos et al. (47) introduced a new operational axis in the RAS, which revolutionized the view of the function of this system. ANG-(1–7) is thought to act as an endogenous inhibitor of the actions of ANG II, therefore resulting in hypotensive effects (14, 27). In addition, ANG-(1–7) is thought to be a major contributor to the beneficial blood pressure lowering abilities of ACE inhibitors and ARBs (12, 24). Iyer et al. (24) confirmed that both ACE inhibitor and ARB treatment were associated with markedly elevated ANG-(1–7) levels in SHR, and that either neutralization of circulating ANG-(1–7) or blockade of ANG-(1–7) synthesis with a neprilysin inhibitor resulted in elevation of blood pressure in ACE inhibitor and ARB-treated groups. However, the data on the effects of ANG-(1–7) on sympathetic neurotransmission is controversial. ANG-(1–7) was found to enhance NE release in rat atria and kidney preparations (17, 54), as well as result in ANG II-like pressor effects when microinjected to the rostral ventral lateral medulla of the rat (49). Our laboratory has previously found that ANG II enhances the NS-induced increase in perfusion pressure NPY overflow and NE overflow (40). We, therefore, hypothesized that, as an endogenous inhibitor of ANG II, ANG-(1–7) would reduce the NS-induced increases in perfusion pressure and NE and NPY overflow. The data we obtained support this hypothesis. At three different concentrations, ANG-(1–7) significantly attenuated the NS-induced increase in perfusion pressure and NE and NPY overflow (Fig. 2) from SHR preparations. ANG-(1–7) also decreased the NS-induced increase in perfusion pressure of WKY preparations (Fig. 1A). However, the effect of ANG-(1–7) on the evoked NE and NPY overflow was greater in preparations from SHR than WKY (Fig. 1, B and C). As shown, SHR mesenteric beds have higher nerve-stimulated perfusion pressure and neurotransmitter overflow values than WKY; therefore, the observed reduction by ANG-(1–7) would be relatively greater in SHR. In addition, recent reports suggest that the production of ANG-(1–7) in SHR is impaired compared with that in WKY (10). Crackower et al. (10) reported that ACE2 mRNA and protein expression is markedly reduced in three different hypertensive rat models, suggesting a role for reduced ANG-(1–7) synthesis in hypertension development. In addition, ANG II was reported to downregulate ACE2 expression in hypertensive human heart and kidney tissue preparations and, therefore, result in a net increase in ANG II levels, propagating the ANG II hypertensive effects (30). Therefore, adding ANG-(1–7) to SHR preparations restores the balance between the ANG II and ANG-(1–7) arms of the RAS, resulting in decreased perfusion pressure and neurotransmitter overflow. On the other hand, WKY rats have an intact ANG-(1–7) synthesis pathway; therefore, addition of the heptapeptide would not result in further reductions in perfusion pressure and neurotransmitter overflow.
In the present studies, we observed that the modulation of perfusion pressure and neurotransmitter overflow by ANG-(1–7) in the mesenteric arterial bed of SHR is mediated by either AT2 or Mas receptors, or both. In contrast, we found no involvement of the AT1 receptor in the ANG-(1–7)-mediated effects. Both the AT2 and Mas receptor antagonists were able to attenuate the reduction of NS-induced increase in perfusion pressure and NE overflow by ANG-(1–7) (Fig. 3, A and B). However, the effect of ANG-(1–7) on NPY overflow appears to be mediated solely through the activation of the Mas receptors (Fig. 3C). It is important to consider that some of the effects observed in the presence of AT2-receptor antagonist could be due to the conversion of ANG II to ANG-(1–7) and its consequent action on Mas receptors or some other as yet unidentified receptor. Both the Mas and AT2 receptors are reported to activate pathways that lead to the release of NO. In conscious rats, activation of the RAS during sodium depletion increased renal NO through the stimulation of AT2 receptors (50). In addition, aortic explants from transgenic mice overexpressing the AT2 receptor showed increased cGMP production (56). These AT2-mediated effects were abolished by either removal of the endothelium or treatment with l-NAME (NO synthesis inhibitor), suggesting the involvement of NO. Our laboratory has previously shown that NO is able to deactivate CAs but not NPY and, therefore, alters perfusion pressure and neurotransmitter overflow patterns in rat mesenteric arterial preparations (28, 29). Therefore, it is reasonable to conclude that ANG-(1–7) acting on Mas and AT2 receptors stimulates the release of NO, which results in a direct vasodilator effect, as well as a net reduction in NE overflow without directly affecting NPY. We were able to further support the above contention with our results shown in Figs. 4 and 5A. In the presence of l-NAME, the effects of ANG-(1–7) on NS-induced increase in perfusion pressure and NE overflow were abolished. However, the effect on NPY overflow was not changed (Fig. 5B). This is consistent with reported data that ANG-(1–7) increases NO, either by acting on its Mas receptors (59), or by preventing the activation of NADPH oxidase, which results in reduced superoxide anion levels and increased bioavailable NO (1). Therefore, it is suggested that some of the beneficial effects of ANG-(1–7) on blood pressure and vascular function are NO mediated; however, other mechanisms of action are not to be excluded. In addition, ANG-(1–7) is reported to augment the vasodilator action of bradykinin (12, 32) and that some of its effects are attenuated in the presence of a bradykinin B2 receptor antagonist (19). We also observed that the ANG-(1–7) effect on nerve-stimulated perfusion pressure and NE overflow was attenuated in the presence of the bradykinin B2 receptor antagonist bradyzine (Figs. 6 and 7A). Similar to l-NAME, bradyzine did not attenuate the effect of ANG-(1–7) on nerve-stimulated NPY overflow (Fig. 7B). These findings are consistent with reports that bradykinin can result in hypotensive effects by stimulating NO release via activation of B2 receptors (51).
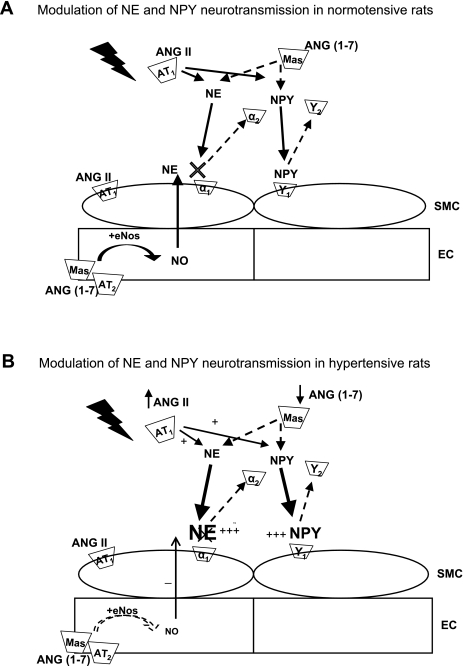
A schematic representation of the modulation by ANG II and ANG-(1–7) of NE and NPY neurotransmission from sympathetic nerves obtained from 10- to 12-wk old WKY and SHR is depicted in Fig. 8. Figure 8A depicts neurotransmission in normotensive rats. NS results in release of NE and NPY from the nerve varicosity, which, in turn, acts on their postjunctional receptors and results in vasoconstriction. ANG II augments the release of NE, NPY, and vasoconstriction. In contrast, ANG-(1–7) decreases NE and NPY release from the nerve varicosity and induces NO release, resulting in vasodilation and NE deactivation, therefore opposing the effect of ANG II. Figure 8B depicts the alterations that occur in blood vessels from hypertensive rats. The effect of ANG II is augmented in hypertension, resulting in increased NE and NPY overflow and enhanced vasoconstriction. Correspondingly, ANG-(1–7) levels are likely decreased in hypertensive rats, resulting in a decreased attenuation of the effects of ANG II. This results in an imbalance, which predisposes to increased NE and NPY levels and increased vasoconstriction supporting hypertension.
Fig. 8.
Depiction of the modulation by ANG II and ANG-(1–7) of NE and NPY neurotransmission from the perfused mesenteric arterial bed obtained from WKY (A) and SHR (B). Mas, ANG-(1–7) Mas receptor; α2, adrenergic A2 receptor; Y2, NPY Y2 receptor; SMC, smooth muscle cell; EC, endothelial cell; NO, nitric oxide; eNOS, endothelial NO synthase.
In conclusion, ANG-(1–7) decreases perfusion pressure and neurotransmitter overflow from the mesenteric beds of SHR to a greater extent than WKY. We have previously found that ANG II increases perfusion pressure and neurotransmitter overflow (4); therefore, the present data support the hypothesis that ANG-(1–7) is an endogenous inhibitor of the ANG II-mediated actions of the RAS. Our data suggest that the effects of ANG-(1–7) on NE overflow are mediated by the AT2 and Mas receptors, and that the mediators NO and bradykinin are also involved. Interestingly, the effect of ANG-(1–7) on NPY overflow was reversed only in the presence of the Mas receptor antagonist, suggesting that the modulation of NPY overflow by ANG-(1–7) is directly through the Mas receptors and does not involve the participation of the mediators NO or bradykinin. We have summarized our findings and our overall hypothesis about the effect of ANG II and ANG-(1–7) on NE and NPY neurotransmission and how it is altered in hypertension in Fig. 8. We believe that hypertension, in part, results from an imbalance between ANG II and ANG-(1–7) effects on sympathetic neurotransmission. As discussed, there is evidence to support that ANG-(1–7) levels are decreased in hypertensive models. There is also evidence to suggest that there is an increase in AT1-receptor subtypes in hypertensive models, resulting in augmented ANG II effects. The aforementioned findings suggest that a functional imbalance in the arms of the RAS, resulting in increased ANG II activity coupled with a decrease in ANG-(1–7) formation, may be at the heart of the development of hypertensive disease, and that restoring this balance by increasing ANG-(1–7) synthesis could be a valuable therapeutic target.
GRANTS
This work was supported by National Heart, Lung, and Blood Institute Grant HL60260 to T. C. Westfall and by the American Heart Association to M. Byku.
DISCLOSURES
I am not aware of financial conflict(s) with the subject matter or materials discussed in this manuscript with any of the authors, or any of the authors' academic institutions or employers.
REFERENCES
- 1.Benter IF, Yousif MHM, Dhaunsi GS, Kaur J, Chappell MC, Diz DI. Angiotensin-(1–7) prevents activation of NADPH oxidase and renal vascular dysfunction in diabetic hypertensive rats. Am J Nephrol 28: 25–33, 2008 [DOI] [PubMed] [Google Scholar]
- 2.Brosnihan KB. Effect of the angiotensin-(1–7) peptide on nitric oxide release. Am J Cardiol 82: 17S–19S, 1998 [DOI] [PubMed] [Google Scholar]
- 3.Brosnihan KB, Li P, Tallant EA, Ferrario CM. Angiotensin-(1–7): a novel vasodilator of the coronary circulation. Biol Res 31: 227–234, 1998 [PubMed] [Google Scholar]
- 4.Byku M, Macarthur H, Westfall TC. Nerve stimulation induced overflow of neuropeptide Y and modulation by angiotensin II in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol 295: H2188–H2197, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campese VM, Ye S, Zhong H. Downregulation of neuronal nitric oxide synthase and interleukin-1 beta mediates angiotensin II-dependent stimulation of sympathetic nerve activity. Hypertension 39: 519–524, 2002 [DOI] [PubMed] [Google Scholar]
- 6.Carey RM, Siragy HM. Newly recognized components of the renin-angiotensin system: potential roles in cardiovascular and renal regulation. Endocr Rev 24: 261–271, 2003 [DOI] [PubMed] [Google Scholar]
- 7.Cavadas C, Grand D, Mosimann F, Cotrim MD, Fontes Ribeiro CA, Brunner HR, Grouzmann E. Angiotensin II mediates catecholamine and neuropeptide Y secretion in human adrenal chromaffin cells through the AT1 receptor. Regul Pept 111: 61–65, 2003 [DOI] [PubMed] [Google Scholar]
- 8.de Champlain J, Karas M, Toal C, Nadeau R, Larochelle P. Effects of antihypertensive therapies on the sympathetic nervous system. Can J Cardiol 15, Suppl A : 8A–14A, 1999 [PubMed] [Google Scholar]
- 9.de Champlain J. Pre- and postsynaptic adrenergic dysfunctions in hypertension. J Hypertens Suppl 8: S77–S85, 1990 [PubMed] [Google Scholar]
- 10.Crackower MA, Sarao R, Oudit GY, Yagil C, Kozieradzki I, Scanga SE, Oliveira-dos-Santos AJ, da Costa J, Zhang L, Pei Y, Scholey J, Ferrario CM, Manoukian AS, Chappell MC, Backx PH, Yagil Y, Penninger JM. Angiotensin-converting enzyme 2 is an essential regulator of heart function. Nature 417: 822–828, 2002 [DOI] [PubMed] [Google Scholar]
- 11.Dubinion JH, Mi Z, Jackson EK. Role of renal sympathetic nerves in regulating renovascular responses to angiotensin II in spontaneously hypertensive rats. J Pharmacol Exp Ther 317: 1330–1336, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Ferrario CM. Angiotension-(1–7) and antihypertensive mechanisms. J Nephrol 11: 278–283, 1998 [PubMed] [Google Scholar]
- 13.Ferrario CM, Mohara O, Ueno Y, Brosnihan KB. Hemodynamic and neurohormonal changes in the development of DOC hypertension in the dog. Am J Med Sci 295: 352–359, 1988 [DOI] [PubMed] [Google Scholar]
- 14.Ferrario CM, Trask AJ, Jessup JA. Advances in biochemical and functional roles of angiotensin-converting enzyme 2 and angiotensin-(1–7) in regulation of cardiovascular function. Am J Physiol Heart Circ Physiol 289: H2281–H2290, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ferrario CM, Jessup J, Gallagher PE, Averill DB, Brosnihan KB, Ann Tallant E, Smith RD, Chappell MC. Effects of renin-angiotensin system blockade on renal angiotensin-(1–7) forming enzymes and receptors. Kidney Int 68: 2189–2196, 2005 [DOI] [PubMed] [Google Scholar]
- 16.Flaa A, Mundal HH, Eide I, Kjeldsen S, Rostrup M. Sympathetic activity and cardiovascular risk factors in young men in the low, normal, and high blood pressure ranges. Hypertension 47: 396–402, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Gironacci MM, Adler-Graschinsky E, Pena C, Enero MA. Effects of angiotensin II and angiotensin-(1–7) on the release of [3H]norepinephrine from rat atria. Hypertension 24: 457–460, 1994 [DOI] [PubMed] [Google Scholar]
- 18.Gironacci MM, Valera MS, Yujnovsky I, Peña C. Angiotensin-(1–7) inhibitory mechanism of norepinephrine release in hypertensive rats. Hypertension 44: 783–787, 2004 [DOI] [PubMed] [Google Scholar]
- 19.Gironacci MM, Yujnovsky I, Gorzalczany S, Taira C, Peña C. Angiotensin-(1–7) inhibits the angiotensin II-enhanced norepinephrine release in coarcted hypertensive rats. Regul Pept 118: 45–49, 2004 [DOI] [PubMed] [Google Scholar]
- 20.Goldstein DS. Plasma norepinephrine in essential hypertension. A study of the studies. Hypertension 3: 48–52, 1981 [DOI] [PubMed] [Google Scholar]
- 21.Gradin KA, Li JY, Andersson O, Simonsen U. Enhanced neuropeptide Y immunoreactivity and vasoconstriction in mesenteric small arteries from spontaneously hypertensive rats. J Vasc Res 40: 252–265, 2003 [DOI] [PubMed] [Google Scholar]
- 22.Grobecker G, Roizen MF, Weise V, Saavedra JM, Kopin IJ. Letter: Sympathoadrenal medullary activity in young, spontaneously hypertensive rats. Nature 258: 267–268, 1975 [DOI] [PubMed] [Google Scholar]
- 23.Huidobro-toro J, Donoso MV. Sympathetic co-transmission: the coordinated action of ATP and noradrenaline and their modulation by neuropeptide Y in human vascular neuroeffector junctions. Euro Journal of Pharmacol 500: 27–35, 2004 [DOI] [PubMed] [Google Scholar]
- 24.Iyer SN, Ferrario CM, Chappell MC. Angiotensin-(1–7) contributes to the antihypertensive effects of blockade of the renin-angiotensin system. Hypertension 31: 356–361, 1998 [DOI] [PubMed] [Google Scholar]
- 25.Kawasaki H, Cline WH, Jr, Su C. Enhanced angiotensin-mediated facilitation of adrenergic neurotransmission in spontaneously hypertensive rats. J Pharmacol Exp Ther 221: 112–116, 1982 [PubMed] [Google Scholar]
- 26.Kawasaki H, Cline WH, Jr, Su C. Enhanced presynaptic beta adrenoceptor-mediated modulation of vascular adrenergic neurotransmission in spontaneously hypertensive rats. J Pharmacol Exp Ther 223: 721–728, 1982 [PubMed] [Google Scholar]
- 27.Kohara K, Brosnihan KB, Ferrario CM. Angiotensin(1–7) in the spontaneously hypertensive rat. Peptides 14: 883–891, 1993 [DOI] [PubMed] [Google Scholar]
- 28.Kolo LL, Westfall TC, Macarthur H. Nitric oxide decreases the biological activity of norepinephrine resulting in altered vascular tone in the rat mesenteric arterial bed. Am J Physiol Heart Circ Physiol 286: H296–H303, 2004 [DOI] [PubMed] [Google Scholar]
- 29.Kolo LL, Westfall TC, Macarthur H. Modulation of neurotransmitter release by NO is altered in mesenteric arterial bed of spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol 287: H1842–H1847, 2004 [DOI] [PubMed] [Google Scholar]
- 30.Koka V, Huang XR, Chung AC, Wang W, Truong LD, Lan HY. Angiotensin II up-regulates angiotensin I-converting enzyme (ACE), but down-regulates ACE2 via the AT1-ERK/p38 MAP kinase pathway. Am J Pathol 172: 1174–1183, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krum H, Lambert E, Windebank E, Campbell DJ, Esler M. Effect of angiotensin II receptor blockade on autonomic nervous system function in patients with essential hypertension. Am J Physiol Heart Circ Physiol 290: H1706–H1712, 2006 [DOI] [PubMed] [Google Scholar]
- 32.Li P, Chappell MC, Ferrario CM, Brosnihan KB. Angiotensin-(1–7) augments bradykinin-induced vasodilation by competing with ACE and releasing nitric oxide. Hypertension 29: 394–400, 1997 [DOI] [PubMed] [Google Scholar]
- 33.Lundberg JM. Pharmacology of cotransmission in the autonomic nervous system: integrative aspects on amines, neuropeptides, adenosine triphosphate, amino acids and nitric oxide. Pharmacol Rev 48: 113–178, 1996 [PubMed] [Google Scholar]
- 34.Majewski H, Hedler L, Schurr C, Starke K. Modulation of noradrenaline release in the pithed rabbit: a role for angiotensin II. J Cardiovasc Pharmacol 6: 888–896, 1984 [DOI] [PubMed] [Google Scholar]
- 35.Meldrum MJ, Xue CS, Badino L, Westfall TC. Angiotensin facilitation of noradrenergic neurotransmission in central tissues of the rat: effects of sodium restriction. J Cardiovasc Pharmacol 6: 989–995, 1984 [PubMed] [Google Scholar]
- 36.Meldrum MJ, Westfall TC. Angiotensin facilitation of 3H-norepinephrine release in central tissue of spontaneously hypertensive rats but not in Wistar-Kyoto rats: effects of sodium depletion. J Cardiovasc Pharmacol 8: 582–587, 1986 [PubMed] [Google Scholar]
- 37.Morris J, Gibbins IL. Co-transmission and Neuromodulation. In: Autonomic Neuroeffector Mechanisms, edited by Burnstock G, Hoyle CHV. Reading, PA: Hardwood Academic, 1992, p. 33–119 [Google Scholar]
- 38.Nagatsu T, Kato T, Numata Y, Keiko I, Umezawa H. Serum dopamine beta-hydroxylase activity in developing hypertensive rats. Nature 251: 630–631, 1974 [DOI] [PubMed] [Google Scholar]
- 39.Nap AB, Balt JC, Mathy MJ, van Zwieten PA. AT1-receptor blockade and sympathetic neurotransmission in cardiovascular disease. Auton Autacoid Pharmacol 23: 285–296, 2004 [DOI] [PubMed] [Google Scholar]
- 40.Palermo A, Costantini C, Mara G, Libretti A. Role of the sympathetic nervous system in spontaneous hypertension: changes in central adrenoceptors and plasma catecholamine levels. Clin Sci (Lond) 61, Suppl 7: 195s–198s, 1981 [DOI] [PubMed] [Google Scholar]
- 41.Paul M, Poyan Mehr A, Kreutz R. Physiology of local renin-angiotensin systems. Physiol Rev 86: 747–803, 2006 [DOI] [PubMed] [Google Scholar]
- 42.Potter E. Neuropeptide Y as an autonomic transmitter. In: Novel Peripheral Neurotransmitters, edited by Bell C. New York: Pergamon, 1991, p. 81–112 [Google Scholar]
- 43.Raizada MK, Lu D, Sumners C. AT1 receptors and angiotensin actions in the brain and neuronal cultures of normotensive and hypertensive rats. Adv Exp Med Biol 377: 331–348, 1995 [DOI] [PubMed] [Google Scholar]
- 44.Reinhart GA, Lohmeier TE, Hord CE., Jr Hypertension induced by chronic renal adrenergic stimulation is angiotensin dependent. Hypertension 25: 940–949, 1995 [DOI] [PubMed] [Google Scholar]
- 45.Roizen MF, Weise V, Grobecker H, Kopin IJ. Plasma catecholamines and dopamine-beta-hydroxylase activity in spontaneously hypertensive rats. Life Sci 17: 283–288, 1975 [DOI] [PubMed] [Google Scholar]
- 46.Roks AJ, van Geel PP, Pinto YM, Buikema H, Henning RH, de Zeeuw D, van Gilst WH. Angiotensin-(1–7) is a modulator of the human renin-angiotensin system. Hypertension 34: 296–301, 1999 [DOI] [PubMed] [Google Scholar]
- 47.Santos RA, Simoes e Silva AC, Maric C, Silva DM, Machado RP, de Buhr I, Heringer-Walther S, Pinheiro SV, Lopes MT, Bader M, Mendes EP, Lemos VS, Campagnole-Santos MJ, Schultheiss HP, Speth R, Walther T. Angiotensin-(1–7) is an endogenous ligand for the G protein-coupled receptor Mas. Proc Natl Acad Sci USA 100: 8258–8263, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Santos RA, Campagnole-Santos MJ, Andrade SP. Angiotensin-(1–7): an update. Regul Pept 91: 45–62, 2000 [DOI] [PubMed] [Google Scholar]
- 49.Santos RA, Campagnole-Santos MJ. Central and peripheral actions of angiotensin-(1–7). Braz J Med Biol Res 27: 1033–1047, 1994 [PubMed] [Google Scholar]
- 50.Siragy HM, Carey RM. The subtype 2 (AT2) angiotensin receptor mediates renal production of nitric oxide in conscious rats. J Clin Invest 100: 264–269, 1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siragy HM, Jaffa AA, Margolius HS. Bradykinin B2 receptor modulates renal prostaglandin E2 and nitric oxide. Hypertension 29: 757–762, 1997 [DOI] [PubMed] [Google Scholar]
- 52.Solt VB, Brown MR, Kennedy B, Kolterman OG, Ziegler MG. Elevated insulin, norepinephrine, and neuropeptide Y in hypertension. Am J Hypertens 3: 823–828, 1990 [DOI] [PubMed] [Google Scholar]
- 53.Starke K, Gothert M, Kilbinger H. Modulation of neurotransmitter release by presynaptic autoreceptors. Physiol Rev 69: 864–989, 1989 [DOI] [PubMed] [Google Scholar]
- 54.Stegbauer J, Oberhauser V, Vonend O, Rump LC. Angiotensin-(1–7) modulates vascular resistance and sympathetic neurotransmission in kidneys of spontaneously hypertensive rats. Cardiovasc Res 61: 352–359, 2004 [DOI] [PubMed] [Google Scholar]
- 55.Tipnis SR, Hooper NM, Hyde R, Karran E, Christie G, Turner AJ. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem 275: 33238–33243, 2000 [DOI] [PubMed] [Google Scholar]
- 56.Tsutsumi Y, Matsubara H, Masaki H, Kurihara H, Murasawa S, Takai S, Miyazaki M, Nozawa Y, Ozono R, Nakagawa K, Miwa T, Kawada N, Mori Y, Shibasaki Y, Tanaka Y, Fujiyama S, Koyama Y, Fujiyama A, Takahashi H, Iwasaka T. Angiotensin II type 2 receptor overexpression activates the vascular kinin system and causes vasodilation. J Clin Invest 104: 925–935, 1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Westfall TC, Carpentier S, Chen X, Beinfeld MC, Naes L, Meldrum MJ. Prejunctional and postjunctional effects of neuropeptide Y at the noradrenergic neuroeffector junction of the perfused mesenteric arterial bed of the rat. J Cardiovasc Pharmacol 10: 716–722, 1987 [DOI] [PubMed] [Google Scholar]
- 58.Westfall TC JMQ, Meldrum MJ, Zhang S, Carptentier S, Naes L. Central and peripheral alterations in noradrenergic transmission in experimental hypertension: modulation by prejunctional receptors. J Cardiovas Pharm 10: S62–S67, 1987 [Google Scholar]
- 59.Xu P, Costa-Goncalves AC, Todiras M, Rabelo LA, Sampaio WO, Moura MM, Santos SS, Luft FC, Bader M, Gross V, Alenina N, Santos RA. Endothelial dysfunction and elevated blood pressure in MAS gene-deleted mice. Hypertension 51: 574–580, 2008 [DOI] [PubMed] [Google Scholar]
- 60.Ye S, Zhong H, Yanamadala V, Campese VM. Renal injury caused by intrarenal injection of phenol increases afferent and efferent renal sympathetic nerve activity. Am J Hypertens 15: 717–724, 2002 [DOI] [PubMed] [Google Scholar]
- 61.Zimmerman BG, Gomez J. Increased response to sympathetic stimulation in the cutaneous vasculature in presence of angiotensin. Int J Neuropharmacol 4: 185–193, 1965 [DOI] [PubMed] [Google Scholar]
- 62.Zukowska-Grojec Z, Golczynska M, Shen GH, Torres-Duarte A, Haass M, Wahlestedt C, Myers AK. Modulation of vascular function by neuropeptide Y during development of hypertension in spontaneously hypertensive rats. Pediatr Nephrol 7: 845–852, 1993 [DOI] [PubMed] [Google Scholar]