Abstract
Context
Posttraumatic stress disorder (PTSD) is increasingly recognized as a cause of substantial disability. In addition to its tremendous mental health burden, PTSD has been associated with worse physical health status and an increased risk of cardiovascular disease.
Objective
To determine whether PTSD is associated with cardiovascular health status in patients with heart disease and whether this association is independent of cardiac function.
Design
Cross-sectional study.
Setting
The Heart and Soul Study, a prospective cohort study of psychological factors and health outcomes in adults with stable cardiovascular disease.
Participants
One thousand twenty-two men and women with coronary heart disease.
Main Outcome Measures
Posttraumatic stress disorder was assessed using the Computerized Diagnostic Interview Schedule for DSM-IV. Cardiac function was measured using left ventricular ejection fraction, treadmill exercise capacity, and inducible ischemia on stress echocardiography. Disease-specific health status was assessed using the symptom burden, physical limitation, and quality of life subscales of the Seattle Angina Questionnaire. We used ordinal logistic regression to evaluate the association of PTSD with health status, adjusted for objective measures of cardiac function.
Results
Of the 1022 participants, 95 (9%) had current PTSD. Participants with current PTSD were more likely to report at least mild symptom burden (57% vs 36%), mild physical limitation (59% vs 44%), and mildly diminished quality of life (62% vs 35%) (all P≤.001). When adjusted for cardiovascular risk factors and objective measures of cardiac function, PTSD remained independently associated with greater symptom burden (odds ratio, 1.9; 95% confidence interval, 1.2-2.9; P=.004); greater physical limitation (odds ratio, 2.2; 95% confidence interval, 1.4-3.6; P=.001); and worse quality of life (odds ratio, 2.5; 95% confidence interval, 1.6-3.9; P<.001). Results were similar after excluding participants with depression.
Conclusions
Among patients with heart disease, PTSD is more strongly associated with patient-reported cardiovascular health status than objective measures of cardiac function. Future studies should explore whether assessing and treating PTSD symptoms can improve function and quality of life in patients with heart disease.
With recent surges in global conflict and terrorism, post-traumatic stress disorder (PTSD) is increasingly being recognized as a cause of substantial disability in both civilian and military populations. The lifetime prevalence of PTSD in the general population is 8% to 12%,1,2 and the prevalence in military veterans is considerably higher, ranging from 13% to 31%.3-5 Posttraumatic stress disorder is not only the cause of tremendous mental health burden but is also a major risk factor for chronic physical illness, particularly cardiovascular disease (CVD).6-8 In the absence of a cure for PTSD, improving patients’ health status by reducing disease symptoms, maximizing function, and increasing quality of life is a major goal of treatment.
Health status, as measured by patients’ reports of symptoms, physical limitations, quality of life, and general health, is also widely recognized as an independent predictor of morbidity and mortality in patients with CVD.9,10 Studies of veterans from multiple eras have found that those with PTSD have significantly worse health status independent of demographics, military service characteristics, and health behaviors.11-14 Less information is available from nonmilitary populations, but an analysis of participants from 11 psychiatric treatment trials found that those with PTSD had more profound global deficits in health status than participants with other anxiety disorders.15 In addition, 59% of participants with PTSD had severely reduced quality of life, defined as 2 or more SDs less than population norms. Multiple studies have revealed that the association of PTSD with poor health status is independent of comorbid psychiatric conditions, such as depression.11,13 However, it is not known whether the association of PTSD with worse health status is independent of comorbid medical conditions.
We sought to compare the association of PTSD and cardiovascular function with patient-reported health status in a well-characterized cohort of participants with documented CVD. We evaluated the independent associations of PTSD and 3 objective measures of cardiovascular function (ejection fraction, exercise capacity, and ischemia) with a range of cardiovascular health status outcomes. We hypothesized that PTSD would predict health status independent of cardiovascular function and that PTSD would be a stronger predictor of cardiovascular health status than objective measures of CVD.
METHODS
PARTICIPANTS
The Heart and Soul Study is a prospective cohort study of psychological factors and health outcomes in adults with stable CVD. Detailed methods of the study have been previously described.16 Between September 2000 and December 2002, 1024 ambulatory men and women with established CVD were enrolled, including 438 from 2 Department of Veterans Affairs medical centers (San Francisco Veterans Affairs Medical Center and the Veterans Affairs Palo Alto Health Care System), 346 from a university medical center (University of California, San Francisco), and 238 from 9 public health clinics (Community Health Network of San Francisco). To be eligible, participants needed to have a history of a myocardial infarction, angiographic evidence of stenosis of 50% or greater in 1 or more coronary vessels, evidence of exercise-induced ischemia (by treadmill electrocardiogram or stress nuclear perfusion), or a history of coronary revascularization. Individuals unable to walk 1 block or those planning to leave the area within 3 years were excluded. Informed consent was obtained from all participants and appropriate institutional review boards approved the research protocol. Two participants who did not complete PTSD assessments were excluded from this analysis, yielding a total of 1022 participants.
PREDICTOR VARIABLES
Posttraumatic Stress Disorder
Posttraumatic stress disorder was measured using the Computerized Diagnostic Interview Schedule for DSM-IV (CDIS), a validated computer-based interview administered by trained research personnel.17 The CDIS assesses current PTSD (symptoms meeting criteria in the last year) and past PTSD (symptoms meeting criteria prior to the last year) based on the criteria outlined in the DSM-IV.18 In our study population, only 35 participants met criteria for past (but not present) PTSD. Because our health status outcomes assessed current levels of symptoms and functioning, we used current vs noncurrent (past or never) PTSD for the primary analyses. However, we did conduct sensitivity analyses using the 3 separate PTSD categories (current vs past vs never). We also used the CDIS to assess history of military combat and exposure to combat-related trauma. The CDIS has a sensitivity of 88% and specificity of 73% compared with gold standard clinician interviews19 and has been widely used in previous large epidemiologic studies.20,21
Cardiac Function
We assessed 3 measures of cardiac function: left ventricular ejection fraction, exercise capacity, and inducible ischemia. Ejection fraction was measured on a resting echocardiogram using an Acuson Sequoia Ultrasound System (Mountain View, California) with a 3.5-MHz transducer. Following the resting echocardiogram, participants completed a symptom-limited, graded exercise treadmill test according to a standard Bruce protocol. To achieve maximum heart rate, participants who were unable to continue the standard Bruce protocol (for orthopedic or other reasons) were switched to slower settings on the treadmill and encouraged to exercise for as long as possible. Exercise capacity was calculated as the total number of metabolic equivalent tasks achieved at peak exercise (1 metabolic equivalent=3.5 mL/kg/min of oxygen consumption). At peak exercise, apical 2-chamber, 4-chamber, and precordial long-axis and short-axis views were obtained to evaluate right or left ventricular dilation or wall motion abnormalities that occurred with exercise. We calculated the wall motion score index at peak exercise as a measure of inducible ischemia.22
OUTCOME VARIABLE: HEALTH STATUS
To assess baseline cardiovascular health status, we used the Seattle Angina Questionnaire (SAQ), a well-validated and widely used questionnaire that was designed to measure the physical and emotional effects of CVD.23,24 We evaluated 3 domains of health status. Symptom burden was assessed with the 2-item angina frequency scale, which asks participants about frequency of “chest pain, chest tightness, or angina” and frequency of nitroglycerin use for these symptoms. Functional status was evaluated with the 9-item physical limitation scale. Participants rated limitation due to cardiovascular symptoms for 9 activities using a 5-point Likert scale from “not at all limited” to “severely limited.” Participants could also indicate if they were limited because of other reasons. Quality of life was assessed with the 3-item disease perception scale, which includes ratings of CVD-specific limitations in enjoyment in life, satisfaction with life if symptoms continued at the current level, and frequency of worrying about a heart attack or sudden death.25 In a validation study of 372 patients, scores were reproducible over a 3-month period in patients with stable coronary artery disease (intraclass correlation coefficients of 0.76 for angina frequency, 0.83 for physical limitation, and 0.78 for disease perception subscales). The SAQ also demonstrated responsiveness to change, with significant improvements in patients who underwent successful angioplasty (P<.001).
Standard scoring was used for the SAQ, with each subscale scored from 0 to 100 (higher scores indicated better health status). We used predefined cut points to divide subscale scores into categories.16 We divided symptom burden into daily (0-30), weekly (31-60), monthly (61-90), or no (91-100) angina; physical limitation into severe (0-24), moderate (25-49), mild (50-74), or minimal (75-100) limitation; and quality of life into severely diminished (0-24), moderately diminished (25-49), mildly diminished (50-74), or good to excellent (75-100) quality of life. In addition to the SAQ, we also asked participants to rate their overall health compared with people their age on a 5-point Likert scale (“poor,” “fair,” “good,” “very good,” or “excellent”).
COVARIATES
Participants completed questionnaires to determine age, sex, ethnicity, medical history, and smoking. Alcohol use was measured with the AUDIT-C, a validated screening questionnaire that uses 3 questions to assess frequency and amount of alcohol use and yields a total score of 0 to 12. Regular alcohol use was defined as a total score of 4 or more.26,27 We also examined “binge” drinking, defined using the third AUDIT-C question as a report of drinking 6 or more drinks on a single occasion at least once in the last year.27 Participants brought their medication bottles to the study visit, and a trained research assistant recorded all current medications. Medications were categorized using Epocrates Rx (San Mateo, California). Current depression was measured using the CDIS.17 Body mass index was calculated as weight in kilograms divided by height in meters squared. Fasting serum total cholesterol and high-density lipoprotein cholesterol concentrations were measured by enzymatic assays using a Synchron LX 20 (Beckman Coulter, Inc, Fullerton, California).28 Serum low-density lipoprotein cholesterol concentration was calculated using the Friedewald formula.29
STATISTICAL ANALYSIS
Our objectives were to evaluate the independent association of PTSD with health status and to compare the contributions of PTSD and objective measures of cardiac function with health status in patients with CVD. To describe differences in the characteristics of participants with and without current PTSD, we used t tests for continuous variables and χ2 tests for dichotomous variables. We used a χ2 test to compare the frequency of health status outcomes in participants with current vs past vs never PTSD.
To evaluate the independent association of PTSD with health status, we used multivariate ordinal logistic regression, a method that allows the outcome variable (health status) to have more than 1 category. These models calculate a single odds ratio (OR) for the association between a predictor variable (current vs noncurrent PTSD) and each combination of higher-risk vs lower-risk outcome categories (for example, daily angina vs other categories; daily or weekly angina vs other categories; daily, weekly, or monthly angina vs no angina). We adjusted for all patient characteristics that were associated with PTSD at a P value of <.20 (age entered as a continuous variable, sex, current smoking, history of diabetes mellitus, and recruitment site) and for the 3 cardiac function measures. We did not adjust for military combat exposure because it was highly collinear with recruitment site. The proportional odds assumption was verified for all models. We report our results as ORs with 95% confidence intervals (CIs) and P values.
We tested for interactions of PTSD with sex, ethnicity, and measures of cardiac function. Finally, to ensure that any associations of PTSD with health status were not due to comorbid depression, we added current depression (based on the CDIS) as a covariate and repeated the fully adjusted model stratifying by current depression. We also conducted sensitivity analyses using the 3 separate PTSD categories as predictors: current vs past vs never (reference category). All analyses were performed with Stata version 10 (StataCorp, College Station, Texas).
RESULTS
PATIENT CHARACTERISTICS
Of the 1022 participants, 95 (9%) had current PTSD. Of these participants, 34 (36%) reported trauma related to military combat. The frequency of combat-related trauma differed by sex, with 54% of the men with current PTSD reporting combat trauma vs 4% of the women with current PTSD reporting combat trauma. Compared with participants who did not have PTSD, those with current PTSD were on average 6 years younger and significantly more likely to smoke, report a history of diabetes, and have current depression (Table 1). We did not find significant differences in mean alcohol use scores, regular alcohol use, or binge drinking based on PTSD status. The 3 cardiac function measures were not significantly different in patients with vs without PTSD.
Table 1.
Characteristics of Participants With and Without PTSD
| No. (%) |
|||
|---|---|---|---|
| Variable | Current PTSD (n=95) | No Current PTSD (n=927) | P Value |
| Age, y, mean (SD) | 61 (11) | 67 (11) | <.001 |
| Male | 72 (76) | 766 (83) | .10 |
| White | 54 (57) | 561 (61) | .48 |
| Alcohol use score (AUDIT-C), mean (SD) | 2.1 (0.23) | 2.3 (0.08) | .40 |
| Regular alcohol use | 25 (26) | 268 (29) | .56 |
| Binge drinking | 21 (22) | 199 (21) | .89 |
| Current smoking | 32 (34) | 169 (18) | <.001 |
| History of military combat exposure | 34 (36) | 263 (28) | .13 |
| Recruitment site | |||
| Veterans Administration hospital | 39 (41) | 397 (43) | |
| University hospital/other (n=3) | 20 (21) | 326 (35) | .001 |
| Community health network | 36 (38) | 202 (22) | |
| Medical history | |||
| Hypertension | 72 (76) | 650 (70) | .26 |
| Myocardial infarction | 55 (58) | 492 (53) | .34 |
| Stroke | 15 (16) | 132 (14) | .69 |
| Diabetes mellitus | 33 (35) | 232 (25) | .04 |
| Depression | 58 (61) | 165 (18) | <.001 |
| Medication use | |||
| β-Blocker | 56 (59) | 536 (58) | .83 |
| Statin | 60 (63) | 595 (64) | .84 |
| Renin-angiotensin inhibitor | 46 (48) | 477 (51) | .57 |
| Aspirin | 76 (80) | 715 (77) | .52 |
| Cardiac measures, mean (SD) | |||
| Exercise capacity, METs | 7.5 (3.3) | 7.3 (3.4) | .58 |
| Left ventricular ejection fraction, % | 63 (9) | 62 (10) | .14 |
| Ischemia (wall motion score index) | 1.2 (0.38) | 1.2 (0.35) | .97 |
| Other measurements, mean (SD) | |||
| BMI | 29 (5) | 28 (5) | .82 |
| Total cholesterol level, mg/dL | 174 (35) | 178 (43) | .42 |
| LDL cholesterol level, mg/dL | 102 (27) | 105 (34) | .39 |
| HDL cholesterol level, mg/dL | 47 (14) | 46 (14) | .58 |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); HDL, high-density lipoprotein; LDL, low-density lipoprotein; METs, metabolic equivalent tasks; PTSD, posttraumatic stress disorder.
SI conversion factors: To convert total, LDL, and HDL cholesterol to millimoles per liter, multiply by 0.0259.
PTSD AND HEALTH STATUS
Participants with current PTSD had worse health status on all 4 measures (Table 2). Those with vs without current PTSD were more likely to report at least mild symptom burden (57% vs 36%), mild physical limitation (59% vs 44%), and mildly diminished quality of life (62% vs 35%). They were also significantly more likely to rate their overall health as fair or poor (54% vs 35%) (Figure). In unadjusted analyses, PTSD was significantly associated with worse health status on all 4 outcome measures (OR, 2.1; 95% CI, 1.4-3.1 for greater symptom burden; OR, 2.1; 95% CI, 1.4-3.1 for greater physical limitation; OR, 3.3; 95% CI, 2.2-4.9 for worse quality of life; and OR, 2.0; 95% CI, 1.4-3.1 for worse overall health; all P≤.001). When potential confounding variables and the 3 measures of cardiac function were also included in the models, PTSD remained independently associated with symptom burden, physical function, and quality of life (Table 3).
Table 2.
Associations of Current and Past PTSD With Measures of Health Status
| PTSD, No. (%) |
||||
|---|---|---|---|---|
| Health Status (Sample Size) | Current (n=95) | Past (n=35) | Never (n=892) | P Value |
| Symptom burden | ||||
| No angina (632) | 41 (43) | 21 (60) | 570 (64) | .001 |
| Monthly angina (279) | 39 (41) | 12 (34) | 228 (26) | |
| Weekly angina (101) | 15 (16) | 1 (3) | 85 (10) | |
| Daily angina (9) | 0 | 1 (3) | 8 (1) | |
| Physical function | ||||
| Minimal or no limitation (519) | 37 (41) | 13 (43) | 469 (56) | .003 |
| Mild limitation (270) | 24 (26) | 9 (30) | 237 (28) | |
| Moderate limitation (145) | 26 (29) | 7 (23) | 112 (13) | |
| Severe limitation (24) | 4 (4) | 1 (3) | 19 (2) | |
| Quality of life | ||||
| Good or excellent (636) | 36 (38) | 19 (54) | 581 (65) | <.001 |
| Mildly diminished (245) | 29 (31) | 8 (23) | 208 (23) | |
| Moderately diminished (103) | 18 (19) | 5 (14) | 80 (9) | |
| Severely diminished (36) | 12 (13) | 3 (9) | 21 (2) | |
| Overall health | ||||
| Excellent (75) | 6 (6) | 2 (6) | 67 (8) | .02 |
| Very good (220) | 12 (13) | 6 (17) | 202 (22) | |
| Good (354) | 26 (27) | 11 (31) | 317 (35) | |
| Fair (295) | 37 (39) | 12 (34) | 246 (28) | |
| Poor (78) | 14 (15) | 4 (11) | 60 (7) | |
Abbreviation: PTSD, posttraumatic stress disorder.
Figure.
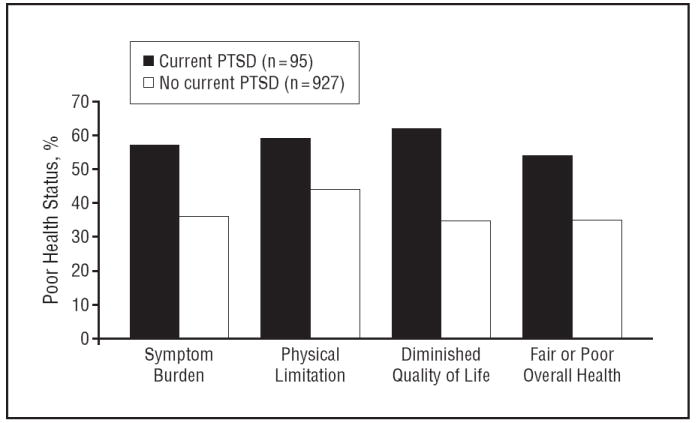
Health status in participants with vs without current posttraumatic stress disorder (PTSD). P<.001 for all comparisons.
Table 3.
Independent Association of Current PTSD and Cardiac Function With Worse Health Statusa
| Symptom Burden |
Physical Limitation |
Quality of Life |
Overall Health |
|||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| PTSD | 1.9 (1.2-2.9) | .004 | 2.2 (1.4-3.6) | .001 | 2.5 (1.6-3.9) | <.001 | 1.4 (0.91-2.3) | .12 |
| Exercise capacity | 1.5 (1.2-1.7) | <.001 | 2.8 (2.3-3.4) | <.001 | 1.6 (1.4-1.9) | <.001 | 2.0 (1.7-2.3) | <.001 |
| Ejection fraction | 1.0 (0.85-1.2) | .96 | 1.0 (0.86-1.2) | .84 | 0.98 (0.82-1.2) | .78 | 1.0 (0.86-1.2) | .95 |
| Wall motion score | 0.98 (0.83-1.2) | .80 | 1.0 (0.87-1.2) | .71 | 1.1 (0.89-1.2) | .52 | 1.1 (0.89-1.3) | .39 |
Abbreviations: CI, confidence interval; OR, odds ratio; PTSD, posttraumatic stress disorder.
Model includes PTSD, exercise capacity, ejection fraction, ischemia (wall motion score), age, sex, smoking, history of diabetes mellitus, and recruitment site.
CARDIAC FUNCTION AND HEALTH STATUS
In adjusted models, decreased exercise capacity was significantly associated with greater symptom burden, greater physical limitation, worse quality of life, and worse overall health (Table 3). However, ejection fraction and wall motion score were not independent predictors of any of the health status outcomes. Posttraumatic stress disorder remained a significant predictor of symptom burden, physical limitation, and quality of life independent of the 3 cardiac function measures. There were no significant interactions between PTSD and sex, ethnicity, or cardiac function in any of the 4 health status models (all P for interaction >.05).
EFFECT OF CURRENT DEPRESSION
The association of PTSD with worse cardiovascular health status was similar after excluding 223 participants with major depression. As compared with the 762 remaining participants who did not have PTSD, the 37 participants with PTSD were more likely to report at least mild symptom burden (49% vs 34%), mild physical limitation (49% vs 41%), mildly diminished quality of life (59% vs 33%), and fair or poor overall health (59% vs 31%) (all P≤.01). Among patients without major depression, PTSD remained a strong predictor of health status, independent of cardiac function (Table 4).
Table 4.
Independent Association of Current PTSD and Worse Health Status in 799 Participants Without Major Depressiona
| Symptom Burden |
Physical Limitation |
Quality of Life |
Overall Health |
|||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | OR (95% CI) | P Value | |
| PTSD | 2.4 (1.2-4.8) | .02 | 2.8 (1.3-6.0) | .01 | 3.9 (2.0-7.6) | <.001 | 2.6 (1.3-5.5) | .01 |
| Exercise capacity | 1.4 (1.2-1.7) | .001 | 2.9 (2.3-3.7) | <.001 | 1.6 (1.3-2.0) | <.001 | 2.1 (1.8-2.5) | <.001 |
| Ejection fraction | 1.1 (0.88-1.3) | .58 | 1.1 (0.88-1.3) | .50 | 1.0 (0.85-1.2) | .78 | 1.0 (0.88-1.2) | .69 |
| Wall motion score | 1.0 (0.83-1.2) | .93 | 1.1 (0.89-1.3) | .52 | 1.1 (0.88-1.3) | .55 | 1.1 (0.85-1.3) | .39 |
Abbreviations: CI, confidence interval; OR, odds ratio; PTSD, posttraumatic stress disorder.
Model includes PTSD, exercise capacity, ejection fraction, ischemia (wall motion score), age, sex, smoking, history of diabetes mellitus, and recruitment site.
We also explored the effects of depression by simultaneously entering PTSD and depression in the fully adjusted model and by restricting the sample to include only those with current depression. When entered simultaneously, the independent associations of PTSD with the health status outcomes were symptom burden (OR, 1.6; 95% CI, 1.0-2.6; P=.03), physical limitation (OR, 1.6; 95% CI, 1.0-2.7; P=.05), quality of life (OR, 2.2; 95% CI, 1.4-3.4; P=.001), and overall health (OR, 1.1; 95% CI, 0.71-1.9; P=.58). In the same models, the independent associations of depression with the health status outcomes were symptom burden (OR, 1.4; 95% CI, 0.99-2.0; P=.05), physical limitation (OR, 2.1; 95% CI, 1.5-3.0; P<.001), quality of life (OR, 1.5; 95% CI, 1.1-2.2; P=.02), and overall health (OR, 1.8; 95% CI, 1.3-2.5; P=.001). In the subgroup of patients with depression, comorbid PTSD appeared to be associated with greater symptom burden (OR, 1.4; 95% CI, 0.76-2.7; P=.27), greater physical limitation (OR, 1.1; 95% CI, 0.59-2.1; P=.75), and worse quality of life (OR, 1.4; 95% CI, 0.75-2.6; P=.29). However, the small sample size resulted in wide CIs, and the P values were not statistically significant.
EFFECT OF CURRENT VS PAST PTSD
Using 3 categories of PTSD (current vs past vs never) did not change our results for the independent association of current PTSD with cardiovascular health status. Past PTSD was not independently associated with any of the health status outcomes, though the number of participants in this category was relatively small (n=35 for the full model, n=11 for participants without depression).
COMMENT
In this analysis of 1022 men and women with stable CVD, we found that PTSD was a strong and independent predictor of greater symptom burden, greater functional limitation, and worse quality of life. In contrast, 2 objective measures of cardiac function, ejection fraction and inducible ischemia, were not significantly associated with cardiovascular health status. These findings demonstrate that the association of PTSD with worse cardiovascular health status is not just due to greater medical comorbidity in patients with PTSD.
Previous studies have demonstrated an association between PTSD and self-reported health status,11-15,30,31 but it has been unclear whether this association is independent of objective measures of physical health. Our results build on these prior studies by examining the relative impact of PTSD and comorbid physical illness on health status. Determining the independent contributions of PTSD and comorbid medical disorders has been challenging for many reasons. First, most studies use self-reported history to define presence or absence of comorbid physical diseases, and such measures may be subject to diagnostic inaccuracies or reporting bias. Second, focusing on the role of comorbid physical illness requires health status measures that reflect the symptoms and functional limitations specific to that disease. Yet, validated disease-specific health status measures are available for only a limited number of physical illnesses. Lastly, no studies of PTSD and health status have examined the severity of physical illness or objective measures of disease-specific function, both of which may be important determinants of health status.
The availability of a validated, CVD-specific health status questionnaire and the detailed measures of CVD severity and cardiac function in the Heart and Soul Study allowed us to address these challenges. Of the 3 cardiac function measures examined, only exercise capacity, which has been used to validate the SAQ, was a significant predictor of health status.25 This is consistent with our prior finding that another psychiatric factor, level of depressive symptoms, was a more important determinant of function and quality of life in patients with CVD than expensive physiologic measures of cardiac function.16 In addition to their value as predictors of patient-centered health status outcomes, psychosocial factors are also strongly associated with cardiac events and mortality.32-34 In the INTERHEART study of 29 432 patients across 52 countries, psychosocial factors accounted for more than 30% of attributable risk of myocardial infarction.34 However, despite their importance, psychosocial factors are often overlooked in primary care and specialist medical practice, and mental health conditions such as PTSD may not be adequately diagnosed and treated in patients with chronic physical illness.35 Though PTSD symptoms are often chronic, trials of both behavioral and pharmacologic therapies have demonstrated that treating PTSD can improve patients’ function and quality of life.36-38 Indeed, our results suggest a dose response between PTSD and cardiovascular health status because participants with prior PTSD had health status outcomes that were intermediate between those with never and current PTSD. Though our sample size is too small to draw definitive conclusions about remitted PTSD, the cardiovascular status of this group deserves further study.
Posttraumatic stress disorder may affect cardiovascular health status through several pathways. Posttraumatic stress disorder is associated with biologic changes, including altered inflammation and sympathetic nervous system activity, which may adversely affect the cardiovascular system.39,40 In addition, patients with PTSD may have differences in health behaviors, such as smoking and physical activity, that could worsen health status by increasing symptoms and decreasing function.41 Therefore, PTSD may act both directly and indirectly to worsen cardiovascular health status.
Our findings should be interpreted in light of several limitations. First, this study included mostly older men, and our results may not generalize to other populations. Second, we focused on CVD because it is the leading cause of death in the world, and several recent studies have found that patients with PTSD have significantly increased risks of developing and dying of CVD.3,7,8,42 However, our findings about the relative influence of PTSD on health status may not extend to patients with other comorbid physical illnesses. Third, though CDIS yields diagnoses of current, past, or no PTSD, we could not determine the exact duration of PTSD symptoms nor could we evaluate the association of severity of PTSD symptoms with health status. In addition, our relatively small number of participants with past PTSD prevented us from fully exploring the association of remitted PTSD and health status. Finally, because our results are cross-sectional, we cannot determine whether the association between PTSD and worse health status is causal.
In summary, we found that PTSD was significantly associated with worse cardiovascular health status, independent of objective measures of cardiac function and comorbid depression. In contrast, 2 measures of cardiac function were not significantly associated with health status. Further study is needed to determine whether treating PTSD symptoms can improve function and quality of life in patients with heart disease.
Acknowledgments
Funding/Support: Dr Cohen was supported by National Institutes of Health/National Center for Research Resources University of California, San Francisco, Clinical and Translational Science grant UL1 RR024130 and Department of Defense/NCIRE grant WB1XWH-05-2-0094. The Heart and Soul Study was funded by the Department of Veterans Affairs, Washington, DC; grant R01 HL079235 from the National Heart, Lung, and Blood Institute, Bethesda, Maryland; the American Federation for Aging Research (Paul Beeson Scholars Program), New York, New York; the Robert Wood Johnson Foundation (Faculty Scholars Program), Princeton, New Jersey; the Ischemia Research and Education Foundation, South San Francisco, California, and the Nancy Kirwan Heart Research Fund, San Francisco.
Role of the Sponsors The funding organizations were not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: All authors had full access to all the data in the study. Drs Cohen and Ali conducted the statistical analyses. Drs Cohen and Whooley take responsibility for the integrity of the data and the accuracy of the analyses.
Financial Disclosure: None reported.
Disclaimer: The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of any of the funding agencies.
References
- 1.Kessler RC. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61(suppl 5):4–14. [PubMed] [Google Scholar]
- 2.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 3.Boscarino JA. Posttraumatic stress disorder and mortality among U.S. Army veterans 30 years after military service. Ann Epidemiol. 2006;16(4):248–256. doi: 10.1016/j.annepidem.2005.03.009. [DOI] [PubMed] [Google Scholar]
- 4.Dohrenwend BP, Turner JB, Turse NA, Adams BG, Koenen KC, Marshall R. The psychological risks of Vietnam for U.S. veterans: a revisit with new data and methods. Science. 2006;313(5789):979–982. doi: 10.1126/science.1128944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Friedman MJ. Acknowledging the psychiatric cost of war. N Engl J Med. 2004;351(1):75–77. doi: 10.1056/NEJMe048129. [DOI] [PubMed] [Google Scholar]
- 6.Boscarino JA. Diseases among men 20 years after exposure to severe stress: implications for clinical research and medical care. Psychosom Med. 1997;59(6):605–614. doi: 10.1097/00006842-199711000-00008. [DOI] [PubMed] [Google Scholar]
- 7.Kang HK, Bullman TA, Taylor JW. Risk of selected cardiovascular diseases and posttraumatic stress disorder among former World War II prisoners of war. Ann Epidemiol. 2006;16(5):381–386. doi: 10.1016/j.annepidem.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Kubzansky LD, Koenen KC, Spiro A, III, Vokonas PS, Sparrow D. Prospective study of posttraumatic stress disorder symptoms and coronary heart disease in the Normative Aging Study. Arch Gen Psychiatry. 2007;64(1):109–116. doi: 10.1001/archpsyc.64.1.109. [DOI] [PubMed] [Google Scholar]
- 9.Bosworth HB, Siegler IC, Brummett BH, Barefoot JC, Williams RB, Clapp-Channing NE, Mark DB. The association between self-rated health and mortality in a well-characterized sample of coronary artery disease patients. Med Care. 1999;37(12):1226–1236. doi: 10.1097/00005650-199912000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Kleefstra N, Landman GW, Houweling ST, Ubink-Veltmaat LJ, Logtenberg SJ, Meyboom-de Jong B, Coyne JC, Groenier KH, Bilo HJ. Prediction of mortality in type 2 diabetes from health related quality of life (ZODIAC-4) Diabetes Care. 2008;31(5):932–933. doi: 10.2337/dc07-2072. [DOI] [PubMed] [Google Scholar]
- 11.Beckham JC, Moore SD, Feldman ME, Hertzberg MA, Kirby AC, Fairbank JA. Health status, somatization, and severity of posttraumatic stress disorder in Vietnam combat veterans with posttraumatic stress disorder. Am J Psychiatry. 1998;155(11):1565–1569. doi: 10.1176/ajp.155.11.1565. [DOI] [PubMed] [Google Scholar]
- 12.Barrett DH, Doebbeling CC, Schwartz DA, Voelker MD, Falter KH, Woolson RF, Doebbeling BN. Posttraumatic stress disorder and self-reported physical health status among U.S. Military personnel serving during the Gulf War period: a population-based study. Psychosomatics. 2002;43(3):195–205. doi: 10.1176/appi.psy.43.3.195. [DOI] [PubMed] [Google Scholar]
- 13.Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164(4):394–400. doi: 10.1001/archinte.164.4.394. [DOI] [PubMed] [Google Scholar]
- 14.Magruder KM, Frueh BC, Knapp RG, Johnson MR, Vaughan JA, III, Carson TC, Powell DA, Hebert R. PTSD symptoms, demographic characteristics, and functional status among veterans treated in VA primary care clinics. J Trauma Stress. 2004;17(4):293–301. doi: 10.1023/B:JOTS.0000038477.47249.c8. [DOI] [PubMed] [Google Scholar]
- 15.Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162(6):1171–1178. doi: 10.1176/appi.ajp.162.6.1171. [DOI] [PubMed] [Google Scholar]
- 16.Ruo B, Rumsfeld JS, Hlatky MA, Liu H, Browner WS, Whooley MA. Depressive symptoms and health-related quality of life: the Heart and Soul Study. JAMA. 2003;290(2):215–221. doi: 10.1001/jama.290.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Robins LN, Helzer JE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 2000. text revision. [Google Scholar]
- 19.Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan B, Marmar CR, Weiss DS. Contractual Report of Findings From the National Vietnam Veterans Read-justment Study Volume 1: Executive Summary, Description of Findings, and Technical Appendices. Research Triangle Park, NC: Research Triangle Park Institute; 1988. [Google Scholar]
- 20.Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam War Generation: Report of Findings From the National Vietnam Veterans Readjustment Study. New York, NY: Brunner Mazel; 1990. [Google Scholar]
- 21.Health status of Vietnam veterans, I: psychosocial characteristics. JAMA. 1988;259(18):2701–2707. [PubMed] [Google Scholar]
- 22.Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I, Silverman NH, Tajik AJ. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography: American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr. 1989;2(5):358–367. doi: 10.1016/s0894-7317(89)80014-8. [DOI] [PubMed] [Google Scholar]
- 23.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD. Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol. 1994;74(12):1240–1244. doi: 10.1016/0002-9149(94)90555-x. [DOI] [PubMed] [Google Scholar]
- 24.Spertus JA, Jones P, McDonell M, Fan V, Fihn SD. Health status predicts long-term outcome in outpatients with coronary disease. Circulation. 2002;106(1):43–49. doi: 10.1161/01.cir.0000020688.24874.90. [DOI] [PubMed] [Google Scholar]
- 25.Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD. Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol. 1995;25(2):333–341. doi: 10.1016/0735-1097(94)00397-9. [DOI] [PubMed] [Google Scholar]
- 26.Bradley KA, Bush KR, McDonell MB, Malone T, Fihn SD Ambulatory Care Quality Improvement Project (ACQUIP) Screening for problem drinking: comparison of CAGE and AUDIT. J Gen Intern Med. 1998;13(6):379–388. doi: 10.1046/j.1525-1497.1998.00118.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158(16):1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 28.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20(4):470–475. [PubMed] [Google Scholar]
- 29.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18(6):499–502. [PubMed] [Google Scholar]
- 30.Holbrook TL, Hoyt DB, Stein MB, Sieber WJ. Perceived threat to life predicts post-traumatic stress disorder after major trauma: risk factors and functional outcome. J Trauma. 2001;51(2):287–293. doi: 10.1097/00005373-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Michaels AJ, Michaels CE, Moon CH, Smith JS, Zimmerman MA, Taheri PA, Peterson C. Posttraumatic stress disorder after injury: impact on general health outcome and early risk assessment. J Trauma. 1999;47(3):460–467. doi: 10.1097/00005373-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Friedmann E, Thomas SA, Liu F, Morton PG, Chapa D, Gottlieb SS. Relationship of depression, anxiety, and social isolation to chronic heart failure outpatient mortality. Am Heart J. 2006;152(5):940.e1–940.e8. doi: 10.1016/j.ahj.2006.05.009. [DOI] [PubMed] [Google Scholar]
- 33.Vaccarino V, Johnson BD, Sheps DS, Reis SE, Kelsey SF, Bittner V, Rutledge T, Shaw LJ, Sopko G, Bairey Merz CN National Heart, Lung, and Blood Institute. Depression, inflammation, and incident cardiovascular disease in women with suspected coronary ischemia: the National Heart, Lung, and Blood Institute-sponsored WISE study. J Am Coll Cardiol. 2007;50(21):2044–2050. doi: 10.1016/j.jacc.2007.07.069. [DOI] [PubMed] [Google Scholar]
- 34.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438):937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 35.Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, III, Hahn SR, Brody D, Johnson JG. Utility of a new procedure for diagnosing mental disorders in primary care: the PRIME-MD 1000 study. JAMA. 1994;272(22):1749–1756. [PubMed] [Google Scholar]
- 36.Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. J Consult Clin Psychol. 1999;67(2):194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- 37.Rapaport MH, Endicott J, Clary CM. Posttraumatic stress disorder and quality of life: results across 64 weeks of sertraline treatment. J Clin Psychiatry. 2002;63(1):59–65. doi: 10.4088/jcp.v63n0112. [DOI] [PubMed] [Google Scholar]
- 38.Tucker P, Zaninelli R, Yehuda R, Ruggiero L, Dillingham K, Pitts CD. Paroxetine in the treatment of chronic posttraumatic stress disorder: results of a placebo-controlled, flexible-dosage trial. J Clin Psychiatry. 2001;62(11):860–868. doi: 10.4088/jcp.v62n1105. [DOI] [PubMed] [Google Scholar]
- 39.Schnurr PP, Green BL. Understanding relationships among trauma, post-traumatic stress disorder, and health outcomes. Adv Mind Body Med. 2004;20(1):18–29. [PubMed] [Google Scholar]
- 40.von Känel R, Hepp U, Kraemer B, Traber R, Keel M, Mica L, Schnyder U. Evidence for low-grade systemic proinflammatory activity in patients with posttraumatic stress disorder. J Psychiatr Res. 2007;41(9):744–752. doi: 10.1016/j.jpsychires.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 41.Buckley TC, Mozley SL, Bedard MA, Dewulf AC, Greif J. Preventive health behaviors, health-risk behaviors, physical morbidity, and health-related role functioning impairment in veterans with post-traumatic stress disorder. Mil Med. 2004;169(7):536–540. doi: 10.7205/milmed.169.7.536. [DOI] [PubMed] [Google Scholar]
- 42.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349(9061):1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]


