Abstract
Rationale: The Severe Asthma Research Program cohort includes subjects with persistent asthma who have undergone detailed phenotypic characterization. Previous univariate methods compared features of mild, moderate, and severe asthma.
Objectives: To identify novel asthma phenotypes using an unsupervised hierarchical cluster analysis.
Methods: Reduction of the initial 628 variables to 34 core variables was achieved by elimination of redundant data and transformation of categorical variables into ranked ordinal composite variables. Cluster analysis was performed on 726 subjects.
Measurements and Main Results: Five groups were identified. Subjects in Cluster 1 (n = 110) have early onset atopic asthma with normal lung function treated with two or fewer controller medications (82%) and minimal health care utilization. Cluster 2 (n = 321) consists of subjects with early-onset atopic asthma and preserved lung function but increased medication requirements (29% on three or more medications) and health care utilization. Cluster 3 (n = 59) is a unique group of mostly older obese women with late-onset nonatopic asthma, moderate reductions in FEV1, and frequent oral corticosteroid use to manage exacerbations. Subjects in Clusters 4 (n = 120) and 5 (n = 116) have severe airflow obstruction with bronchodilator responsiveness but differ in to their ability to attain normal lung function, age of asthma onset, atopic status, and use of oral corticosteroids.
Conclusions: Five distinct clinical phenotypes of asthma have been identified using unsupervised hierarchical cluster analysis. All clusters contain subjects who meet the American Thoracic Society definition of severe asthma, which supports clinical heterogeneity in asthma and the need for new approaches for the classification of disease severity in asthma.
Keywords: asthma phenotype, definition, cluster analysis, severe asthma
AT A GLANCE COMMENTAREY.
Scientific Knowledge on the Subject
Current classification and management approaches in asthma do not reflect the heterogeneous characteristics of this disease.
What This Study Adds to the Field
Using modeling approaches, this article describes five distinct clinical phenotypes of asthma that suggest differences in pathophysiologic mechanisms.
Asthma is defined as a clinical syndrome of intermittent respiratory symptoms triggered by viral upper respiratory infections, environmental allergens, or other stimuli, and is characterized by nonspecific bronchial hyperresponsiveness and airways inflammation (1, 2). An accurate assessment of asthma severity is essential to predict future risk and impairment and to guide asthma management. The National Asthma Education and Prevention Program and Global Initiative for Asthma guidelines divide asthma severity based on lung function (FEV1), daytime and nocturnal symptoms, and frequency of rescue bronchodilator use (1, 2). There is increasing evidence, however, that this approach does not reflect the heterogeneous characteristics of this disease that are observed in populations with asthma (3–5). Identification of heterogeneity and classification of asthma by phenotypes provides a foundation from which to understand disease causality and ultimately to develop management approaches that lead to improved asthma control while avoiding adverse effects and decreasing the risk of serious asthma outcomes (e.g., exacerbations and loss of pulmonary function) (6, 7).
Asthma heterogeneity and complex therapeutic management strategies are more easily recognized in severe asthma, where patients have diverse symptom profiles and altered responses to medications (7–11). The goal of the National Heart Lung and Blood Institute–sponsored Severe Asthma Research Program (SARP) is to identify and characterize not only a large number of subjects with severe asthma but also to compare these subjects with mild to moderate asthma. Initial data from SARP demonstrated persistent symptoms and high health care utilization (HCU) in severe asthma despite complex medication regimens, including high doses of inhaled or oral corticosteroids (11). These results suggested differences in the severe asthma phenotype stratified by age of onset with a group of later-onset, less atopic subjects that reported frequent sinopulmonary infections.
To expand on the previous report, an unsupervised modeling method was applied to the SARP dataset to identify unique groups or clusters of individuals with asthma and to evaluate the range of phenotypic heterogeneity. Five distinct clusters of asthma phenotypes were identified that differ in lung function, age of asthma onset and duration, atopy, sex, symptoms, medication use, and health care utilization. Some of the results of these studies have been previously reported in the form of an abstract (12).
METHODS
The Severe Asthma Research Program
Study participants underwent a detailed phenotypic characterization using established standard operating procedures as previously described (11). Briefly, investigators recruited nonsmoking subjects with asthma (less than 5 pack-years of tobacco use) who met the American Thoracic Society (ATS) definition of severe asthma and an additional group of subjects with asthma that did not meet these criteria (10). After informed consent was obtained, clinical staff administered questionnaires that assessed demographic information, asthma symptoms and medication use, medical history, and HCU. Physiologic testing of lung function included “Baseline” prebronchodilator spirometry with withholding of appropriate medications, responsiveness to two to eight puffs of short-acting β-agonists (“Maximal” lung function), and bronchial hyperresponsiveness to methacholine in subjects with a baseline FEV1 greater than 55%. Atopy was assessed by skin prick testing and measurement of serum total IgE and blood eosinophils. Exhaled nitric oxide was measured using ATS-approved on-line devices at a constant flow rate, and induced sputum was collected in a subset of subjects for evaluation of inflammatory cells. Some of the characteristics of a subset of these subjects have been reported in previous publications (11–20).
Variable Reduction/Data Transformation
The entire dataset provided 628 variables that required reduction in number before performance of a cluster analysis (see Figure E1 in the online supplement). Variables with missing data were excluded immediately. Variables that were clinically redundant (multiple pulmonary function assessments) were reduced by selection of variables chosen to reflect certain physiologic parameters (e.g., pre- and postbronchodilator FEV1). Categorical data from the questionnaires were excluded if the data were presented in text format (such as name of nasal steroid), if the data had been added later in the study (resulting in incomplete data), or if the information would be irrelevant for the current analysis (such as parental race).
Other questionnaire data were binary (yes/no questions) or a spectrum of responses (frequency of albuterol use), and these data were transformed into “composite variables” to capture multiple questions into a ranked ordinal scale. For example, HCU in the past year was queried in five separate yes/no questions on several forms. These questions were consolidated into one variable by generating a ranked “severity” scale ranging from no HCU to emergency department visit to hospitalization and ICU care (see Table E1 in the online supplement). Subjects were assigned a rank based on the most severe HCU reported by that individual. All composite variables were assigned a range of 0 to 10 so that they were equally weighted in the analysis. Similar transformation of data allowed reduction of 63 separate binary questions into 17 composite variables that reflect the information obtained from these individual questions.
Half of the 34 variables that were included in the cluster analysis were numeric variables, and the remaining half were transformed composite variables (Table E2). These variables were selected to cover a broad spectrum of routine assessments of asthma patients including demographic data (sex, race, age); additional variables previously reported to have an effect on disease severity (age of onset, asthma duration); elements of current classification schemes, including those indicative of impairment (symptoms, medication use) or risk (HCU); those that confound current asthma control (smoke exposure, sinopulmonary infections); and important physiologic measures (lung function, atopy). Subjects were required to have all 34 variables to be included in the cluster analysis.
Statistical Analysis
SAS version 9.1 (SAS Institute Inc., Cary, NC) was used for the cluster and discriminant analyses. Ward's minimum-variance hierarchical clustering method was performed using an agglomerative (bottom-up) approach and Ward's linkage (see dendrogram in Figure E2). At each generation of clusters, samples were merged into larger clusters to minimize the within-cluster sum of squares or to maximize the between-cluster sum of squares. To compare differences between clusters, analysis of variance, Kruskal-Wallis, and chi-square tests were used for parametric continuous, nonparametric continuous, and categorical variables, respectively. Stepwise discriminant analysis was performed on the 34 variables to identify a subset of variables for the Tree analysis. Recursive partitioning and regression tree were used to generate binary trees (Rpart package [version 3.1-36] incorporated in R package [version 2.5.1]) and based on CART (Classification and Regression Trees) using the methods of Breiman and colleagues (21). The binary tree was pruned to minimize the cross-validation error.
RESULTS
Subject Demographics
The initial dataset included 856 subjects ranging in age from 6 to 80 years. Preliminary review of the results of this initial analysis by the SARP Steering Committee determined that participants under 12 years of age (n = 39) should not be included in this analysis based on previous reports suggesting important phenotypic differences in young children (14, 22, 23). The final analysis includes 726 subjects 12 years of age or older who had complete data for the 34 phenotypic variables; 304 of these subjects met the ATS workshop criteria for severe asthma. The demographics for the entire cohort are reported in the first column in Tables 1 and 2. The clinical characteristics for the cohort are presented with the sample divided into mild, moderate, and severe asthma in Table E3, similar to the univariate analysis of the first 450 subjects in SARP (11). Clinical characteristics of the SARP cohort have remained consistent over the 7-year period of patient recruitment.
TABLE 1.
DEMOGRAPHICS AND CLINICAL CHARACTERISTICS OF SUBJECTS
| Total Cohort | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 | P Value* | |
|---|---|---|---|---|---|---|---|
| Number of subjects | 726 | 110 | 321 | 59 | 120 | 116 | |
| Age at enrollment, years | 37 (14)† | 27 (8) | 33 (12) | 50 (8) | 38 (13) | 49 (11) | <0.0001 |
| Sex, % female | 66 | 80 | 67 | 71 | 53 | 63 | 0.0006 |
| Race, % White/AA/other | 64/28/8 | 62/29/9 | 63/30/7 | 73/22/5 | 62/33/5 | 68/20/12 | 0.17 |
| Body mass index (BMI) | 29 (8) | 27 (5) | 28 (8) | 33 (9) | 31 (9) | 31 (7) | <0.0001 |
| % with BMI >30 | 37 | 24 | 31 | 58 | 44 | 51 | <0.0001 |
| Age of asthma onset, years | 15 (14) | 11 (10) | 11 (11) | 42 (10) | 8 (10) | 21 (15) | <0.0001 |
| % with onset ≥ 12 years of age | 46 | 39 | 36 | 100 | 28 | 69 | |
| Asthma duration, years | 22 (14) | 15 (9) | 22 (12) | 9 (7) | 30 (14) | 29 (15) | <0.0001 |
| Baseline lung function‡ | |||||||
| FEV1 % predicted | 74 (22) | 102 (11) | 82 (11) | 75 (11) | 57 (12) | 43 (14) | <0.0001 |
| FVC % predicted | 86 (19) | 112 (10) | 93 (9) | 80 (8) | 72 (12) | 60 (13) | <0.0001 |
| FEV1/FVC | 0.70 (0.1) | 0.78 (0.1) | 0.74 (0.1) | 0.74 (0.1) | 0.64 (0.1) | 0.57 (0.1) | <0.0001 |
| Maximal lung function§ | |||||||
| FEV1 % predicted | 87 (20) | 113 (8) | 94 (9) | 84 (9) | 76 (12) | 58 (14) | <0.0001 |
| FVC % predicted | 96 (17) | 117 (10) | 100 (10) | 87 (8) | 89 (12) | 75 (15) | <0.0001 |
| Change in % predicted FEV1 | 13 (11) | 11 (9) | 12 (9) | 10 (7) | 19 (15) | 14 (11) | <0.0001 |
| Atopy status | |||||||
| Number of positive SPT | 3.4 (3.0) | 3.9 (3.0) | 3.6 (3.0) | 2.2 (2.5) | 4.0 (3.1) | 2.6 (2.7) | <0.0001 |
| Subjects with ≥ one positive SPT, % | 77 | 85 | 78 | 64 | 83 | 66 | 0.0008 |
Definition of abbreviation: SPT = skin prick test.
P value from analysis of variance or Chi-square analysis between five clusters.
Numeric data expressed as mean (SD).
Prebronchodilator values with greater than 6 hours withhold of bronchodilators.
Postbronchodilator values after six to eight puffs of albuterol.
TABLE 2.
MEDICATION USE AND HEALTH CARE UTILIZATION
| Total Cohort | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 | Cluster 5 | P Value* | |
|---|---|---|---|---|---|---|---|
| Number of subjects | 726 | 110 | 321 | 59 | 120 | 116 | |
| Corticosteroid use, % | <0.0001 | ||||||
| None | 25 | 45 | 31 | 14 | 15 | 5 | |
| Low- to moderate-dose ICS | 32 | 38 | 40 | 37 | 18 | 16 | |
| High-dose ICS† | 41 | 10 | 28 | 49 | 63 | 78 | |
| Oral or systemic CS† | 21 | 11 | 10 | 17 | 39 | 47 | |
| Total controllers, %‡ | <0.0001 | ||||||
| None | 21 | 41 | 26 | 10 | 12 | 4 | |
| ≤2 | 39 | 41 | 46 | 35 | 33 | 28 | |
| ≥3 | 40 | 19 | 29 | 54 | 56 | 67 | |
| Type of controllers, %‡ | <0.0001 | ||||||
| LTRA alone | 4 | 8 | 5 | 4 | 4 | 0 | |
| ICS alone | 14 | 15 | 18 | 13 | 8 | 8 | |
| ICS + LABA only | 42 | 46 | 42 | 36 | 40 | 44 | |
| ICS + LABA + LTRA | 36 | 26 | 30 | 45 | 43 | 40 | |
| Omalizumab | 7 | 3 | 6 | 6 | 10 | 10 | |
| Health care utilization past year, % | <0.0001 | ||||||
| None | 52 | 67 | 61 | 41 | 38 | 32 | |
| ED for asthma | 30 | 20 | 25 | 34 | 39 | 42 | |
| ≥ 3 OCS, burst/year | 28 | 11 | 19 | 36 | 46 | 42 | |
| Hospitalized for asthma | 14 | 7 | 9 | 15 | 23 | 28 | |
| Hospitalized in ICU | 7 | 5 | 4 | 7 | 11 | 12 | |
| Reported comorbidities, % | |||||||
| Pneumonia | 43 | 35 | 38 | 39 | 49 | 58 | 0.001 |
| Sinus disease | 45 | 40 | 41 | 63 | 45 | 53 | 0.0005 |
| Gastroesophageal reflux | 25 | 8 | 20 | 37 | 32 | 39 | <0.0001 |
| Hypertension, % | 13 | 6 | 8 | 23 | 14 | 29 | <0.0001 |
Definition of abbreviations: CS = corticosteroids; ICS = inhaled corticosteroids; ICU = intensive care unit; LABA = long-acting β-agonists; LTRA = leukotriene receptor antagonist; OCS = oral corticosteroids.
P value from Chi-square analysis of ranked ordinal composite variables between five clusters.
High-dose ICS dose equivalent to 1,000 or greater fluticasone propionate daily; chronic OCS 20 mg or more daily or other systemic steroids in the past 3 months.
Controllers include LTRA, ICS, LABA, theophyllines, OCS, and omalizumab.
Cluster Analysis
Using the agglomerative cluster approach outlined in Methods, a dendrogram was generated (Figure E2). Six clusters were identified, but the sixth cluster was a small subgroup of Cluster 5 (n = 31), and the sample size of this group reduced the value of additional subdivision. The resulting five clusters differ significantly by age and sex but not by self-reported race, although Clusters 3 and 5 contain a greater percentage of non-Hispanic whites as compared with the other clusters (Table 1). Although some clinical sites enrolled a larger number of subjects, there was no significant difference in the distribution of the clusters at any given site (Table E4). Demographic and lung function results for each cluster are shown in Table 1, and medication use and HCU are reported in Table 2.
Cluster 1
Fifteen percent of subjects (n = 110) are grouped into Cluster 1. This cluster is characterized by younger, predominantly female subjects with childhood onset/atopic asthma and normal lung function. Forty percent of these subjects were receiving no controller medications, and those on asthma medications were most often on two or fewer controller therapies, with a combination of inhaled corticosteroids (ICS) and long-acting β-agonists most frequently reported. HCU was infrequent in this group, with nearly 70% reporting no need for any urgent physician or emergency department visits, oral corticosteroid bursts, or hospitalizations in the past year. Despite a lack of exacerbations requiring urgent evaluation, 30 to 40% of Cluster 1 subjects reported daily symptoms and rescue bronchodilator use (Figures E3A and E3B). This group contains the youngest and potentially most active subjects, suggesting that symptoms may be primarily exercise related.
Cluster 2
Cluster 2 is the largest group (n = 321; 44% of subjects). It consists of slightly older subjects, two-thirds female, with primarily childhood onset/atopic asthma. This group is distinguished by baseline prebronchodilator lung function that is relatively normal (65% with an FEV1 >80% predicted) or can be reversed to normal (>80% predicted) in nearly all of the subjects (94%). Medication use is more prevalent in this group, with fewer subjects not receiving controller medications (26%), a shift toward increased numbers of controllers (29% on three or more drugs), and higher doses of ICS (28% on high-dose ICS). HCU, asthma symptoms, and reported albuterol use were similar to those observed in Cluster 1, although Cluster 2 was treated with a greater number of asthma medications.
Cluster 3
Cluster 3 is the smallest cluster (n = 59; 8% of subjects). It is markedly different from the other clusters and consists mainly of older women (mean age, 50 years; range, 34–68 years) with the highest body mass index [BMI] (58% with BMI >30) and late-onset asthma (all older than 23 years of age), who are less likely to be atopic (64%). Despite a shorter reported duration of asthma, subjects in this cluster have decreased baseline pulmonary function (71% with FEV1 <80% predicted), and only 64% are able to attain this benchmark after bronchodilators. These subjects report complicated medical regimens, with more than half describing treatment with three or more asthma drugs (one of which is frequently high-dose ICS) and 17% receiving regular systemic corticosteroids. Despite this increased reliance on medications, they report more HCU (especially the need for oral corticosteroid bursts) and daily asthma symptoms that approach levels reported by subjects in Clusters 4 and 5. Subjects in Cluster 3 report symptoms and HCU that appear to be out of proportion to their degree of airflow obstruction. This result suggests an important relationship between obesity, level of symptoms, and HCU in this group of subjects.
Clusters 4 and 5
The remaining 33% of subjects are grouped in Clusters 4 and 5. Nearly 70% of subjects in Cluster 4 (n = 120) and 80% of subjects in Cluster 5 (n = 116) fulfill the ATS workshop criteria for severe asthma. Subjects are equally divided between these two clusters, but Cluster 4 is characterized by equal representation of both genders and many subjects with childhood onset (72%) and atopic disease (83%), whereas Cluster 5 consists of more women (63%) with mainly later-onset disease (69% late onset) and less atopy (66%). Clusters 4 and 5 are characterized by a long duration of disease, with those in Cluster 5 having the longest duration. Clusters 4 and 5 differ in the level of baseline lung function and the magnitude of response to bronchodilators. Subjects in Cluster 4 have severe reductions in pulmonary function at baseline (mean FEV1 57% predicted), but 40% of subjects are able to reverse to the near normal range (>80% predicted) after six to eight puffs of albuterol. In contrast, subjects in Cluster 5 have the most severe airflow limitation at baseline (mean FEV1 43% predicted), and, despite some response to maximum bronchodilator testing, 94% of subjects remain with a FEV1 <80% predicted. In both clusters, lung function is abnormal despite the use of multiple asthma medications; 55 to 70% are receiving three or more asthma drugs, and 60 to 80% are on high–dose ICS with subjects in Cluster 5 treated more frequently with systemic corticosteroids (47%) than were subjects in Cluster 4 (39%). HCU was similar in both Clusters 4 and 5, with nearly half of subjects reporting three or more oral CS bursts and an additional 25% reporting inpatient hospitalization in the past year for a severe exacerbation. Nearly 40% of subjects in Clusters 4 and 5 report a history of a prior ICU admission for asthma in their lifetime (P < 0.0001; data not shown). Not unexpectedly, 70% of subjects in these groups report daily symptoms and poor quality of life. A potential sixth cluster was a subset of Cluster 5 consisting of 31 subjects who showed a phenotype that was intermediate between Clusters 4 and 5. These individuals were somewhat younger, were more atopic, and showed more bronchodilator reversibility than the remaining 85 subjects in Cluster 5 (Table E5).
Comorbidities
In general, comorbidities tracked with increasing severity and age of the clusters (Table 2). The oldest subjects (Clusters 3 and 5) reported the highest prevalence of sinus disease, with nearly half of those in Cluster 5 reporting prior sinus surgery. Clusters 3 and 5 also have the highest frequency of hypertension when compared with the younger patients in other clusters. Pneumonia is reported more frequently in Clusters 4 and 5 (i.e., the subjects with the lowest lung function and highest exposure to corticosteroid treatment). Subjects in Clusters 3, 4, and 5 reported more symptoms of gastroesophageal reflux disease, suggesting that this comorbidity may be associated with asthma severity (Clusters 4 and 5) and increasing age with or without obesity (Clusters 3 and 5).
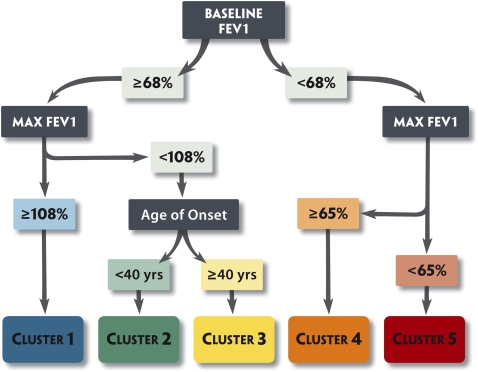
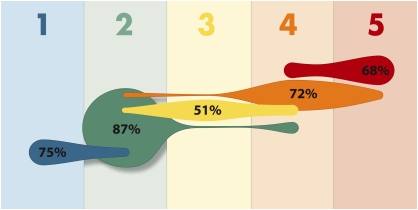
Discriminant Analysis and Tree Diagram
A discriminant analysis using the same 34 variables shows that the 11 strongest discriminatory variables for cluster assignment are pulmonary function measures, baseline (FEV1, FVC, and FEV1/FVC ratio) and after maximal bronchodilation with six to eight puffs of albuterol (maximal FEV1 and FVC, % change in FEV1), age of asthma onset and asthma duration, sex, frequency of β-agonist use, and dose of corticosteroids. A tree analysis was performed using subsets of these variables to assess classification of subjects (Figure 1). Using just pre- and postbronchodilator FEV1% predicted and age of onset, 80% of subjects in the current sample were assigned to the appropriate cluster (Figure 2). This suggests that a simple method for phenotyping of asthma subclasses can be based on these clinical variables.
Figure 1.
Tree analysis. Using three variables (baseline FEV1 [with a bronchodilator withhold], maximal “Max” FEV1 after six to eight puffs of albuterol, and age of onset of asthma), subjects can be assigned to the five clusters that range from milder asthma (Cluster 1) to more severe disease (Clusters 4 and 5).
Figure 2.
Tree performance. Using the algorithm generated by the tree analysis, 80% of subjects are assigned to the correct cluster of asthma severity. Colors are maintained from the tree diagram (blue = mild atopic asthma; green = mild to moderate atopic asthma; yellow = late-onset nonatopic asthma; orange = severe atopic asthma; red = severe asthma with fixed airflow). Individual figure size is proportional to the frequency of a specific cluster. The percentage of subjects from that cluster that are correctly assigned is indicated numerically within the shape.
Biomarkers
Noninvasive measures of airway inflammation are only available on a subset of subjects, and thus these variables could not be used in the cluster analysis. In this subset, blood eosinophils and fractional concentration of nitric oxide in exhaled air (FeNO) levels are similar in all clusters, but other biomarkers differ among clusters (Table 3). Serum total IgE levels are highest in atopic Clusters 1, 2, and 4 and lowest in Clusters 3 and 5. Clusters 4 and 5 are more hyperresponsive to methacholine, but less than half of these groups underwent testing because an FEV1 <55% precluded subjects from undergoing bronchial challenge. Cluster 3 has the lowest levels of bronchial hyperresponsiveness. Half of the subjects (n = 357) provided a sputum specimen for analysis, with similar numbers of subjects sampled in Clusters 1, 2, 3, and 4 but fewer subjects in Cluster 5 due to poor lung function in the latter group. Sputum inflammatory cell counts are greatest in Clusters 3, 4, and 5, but the cellular pattern differs among these clusters; eosinophils are elevated in Clusters 3, 4, and 5, whereas neutrophils are highest in Cluster 5.
TABLE 3.
BIOMARKERS IN SUBSET OF SUBJECTS*
| Cluster 1 |
Cluster 2 |
Cluster 3 |
Cluster 4 |
Cluster 5 |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Value | n | Value | n | Value | n | Value | n | Value | P Value | |
| PC20 methacholine†, mg/ml | 100 | 1.17 (0.73) | 268 | 1.12 (0.67) | 39 | 2.32 (0.60) | 64 | 0.73 (0.71) | 15 | 0.72 (0.86) | 0.007 |
| FeNO†, ppb | 90 | 32.8 (0.36) | 257 | 28.0 (0.37) | 47 | 24.8 (0.36) | 93 | 26.8 (0.37) | 84 | 29.3 (0.41) | 0.40 |
| Blood/serum | |||||||||||
| Total IgE†, IU/ml | 91 | 141 (0.71) | 257 | 125 (0.71) | 47 | 54 (0.82) | 90 | 132 (0.65) | 87 | 98 (0.62) | 0.008 |
| % Eosinophils† | 96 | 0.2 (0.42) | 272 | 0.2 (0.5) | 51 | 0.2 (0.42) | 106 | 0.3 (0.46) | 97 | 0.2 (0.6) | 0.29 |
| Sputum induction | 63 | 160 | 30 | 60 | 44 | ||||||
| % Eosinophils‡ | 0.7 (0.2–4.4) | 0.7 (0.1–3.7) | 1.9 (0.0–4.5) | 1.5 (0.3–7.9) | 1.2 (0.0–10.1) | 0.05 | |||||
| % Neutrophils‡ | 23.3 (7.4–42.9) | 33.0 (15.7–51.7) | 37.6 (12.7–66.4) | 34.7 (15.2–65.7) | 48.3 (25.7–80.3) | 0.001 | |||||
Definition of abbreviation: FeNO = fractional concentration of nitric oxide in exhaled air; PC20 = concentration of methacholine that causes a 20% fall in FEV1.
Subjects with FEV1 less than 55% predicted pretesting were excluded from methacholine challenge and sputum induction.
Data expressed as geometric mean (log 10 SD).
Data expressed as median (interquartile range).
DISCUSSION
Asthma is a clinical syndrome that is characterized by variability in disease expression and severity (4, 5, 11). Asthma severity classification in current and previous guidelines is based on four to six “steps” that range from intermittent to severe persistent asthma (1, 2). These classifications of asthma severity are based on clinical characteristics that include frequency of symptoms, short-acting bronchodilator use, pulmonary function, and medication requirements (1, 2). If an individual with asthma meets any one criterion in that “step,” he is then assigned to that severity despite potential disease heterogeneity within the level. The major assumption in these classification schemes is that all patients within a specific asthma severity level have similar disease characteristics and risk of future asthma exacerbations that should be managed with the same therapeutic regimen. This traditional approach ignores asthma subtypes within and across these levels of asthma severity. Furthermore, this classification approach assumes that patients with asthma who are classified as intermittent, mild, moderate, and severe respond similarly to specific therapies, although optimal management strategies may not always be achieved, specifically in the patients with more severe or “difficult to treat” asthma (3, 7, 24). Thus, the purpose of this study is to improve our understanding of the basis for severity classification and to develop an asthma classification algorithm using comprehensive phenotyping approaches that reflect pathophysiologic processes and disease heterogeneity. To accomplish this goal, data from the SARP cohort, which includes all levels of asthma severity, was analyzed using an unsupervised cluster approach to determine asthma subphenotypes.
Identification of asthma subphenotypes has generally been accomplished in two ways: (1) through a priori definitions of a phenotype based on clinical characteristics of subjects or (2) through pathobiologic differences in sputum or bronchoscopy specimens. The most studied clinical phenotypes have been related to age and atopy. Studies that have compared childhood with adult asthma have reported more atopy and preserved lung function in the former group (14, 25, 26). Other studies have described subsets of patients with adult asthma characterized by age of onset that differ clinically, suggesting different underlying pathophysiologic mechanisms of disease (11, 26–28).
Several studies have demonstrated eosinophilic or noneosinophilic inflammation in asthma (28, 29) and have led to clinical approaches that use these cellular biomarkers to guide asthma management (30). Sputum eosinophilia is a biomarker that appears to be useful in guiding corticosteroid therapy (30), but analysis of induced sputum may not be available in most clinical settings because of the complexity of this technique and difficulty with accurate performance of this analysis. FeNO has been used clinically as a noninvasive biomarker to diagnose asthma and evaluate therapeutic responsiveness (31), but more recent studies suggest limitations of its predictive value (32). A recent study has shown better diagnostic and prognostic utility using a panel of several noninvasive inflammatory biomarkers (including FeNO), suggesting that a multidimensional approach may be more effective than single biomarker monitoring (33). As investigators continue to explore biomarkers that directly reflect airways inflammation and disease severity or guide therapy, more clinically available phenotyping approaches should be evaluated to assess their ability to characterize severity and provide insight into pathobiologic mechanisms in asthma.
The cluster analysis described in this paper is an unsupervised modeling approach to identify asthma phenotypes within the SARP cohort. This article describes five different groups of subjects with asthma who differ in clinical, physiologic, and inflammatory parameters. Of the 11 most important variables that determine assignment to individual clusters, six are pulmonary function tests, two are related to age (age of onset and duration of asthma), two are composite variables that reflect medication use (corticosteroids, β-agonists), and one is gender.
Pulmonary function is an important determinant of disease severity (17, 34). In the current cluster analysis, the combination of prebronchodilator and postbronchodilator measurements (baseline and best FEV1) best differentiates the mildest clusters (Cluster 1 from 2) and the most severe groups (Cluster 4 from 5). It is important to identify the patients with the mildest asthma with the lowest risk, and a prebronchodilator FEV1 ≥80% predicted identifies all subjects in Cluster 1. The patients with milder athma who do not meet that benchmark (Cluster 2) would appear to be at higher risk. The patients with the most severe asthma have a low prebronchodilator FEV1 (<68% predicted), but it is the postbronchodilator FEV1 that determines assignment to Clusters 4 and 5. Unfortunately, pulmonary function testing is usually performed without reference to recent bronchodilator use, and in that setting the reported values may represent the spectrum of prebronchodilator to postbronchodilator FEV1. The difference between those measurements determines phenotype in this cluster analysis, and the importance of having a true baseline FEV1 and a maximal postbronchodilator (four puffs of albuterol) FEV1 requires further evaluation.
Several clusters (Clusters 1, 2, and 4) consist of more atopic subjects with early or childhood onset of disease, which is consistent with the presence of an allergic phenotype in 76% of patients. Late-onset asthma (after the age of 12 years) and less atopy are more characteristic of the older subjects in Clusters 3 and 5, suggesting additional nonallergic disease mechanisms. Regardless of age of onset, the subjects with the longest duration of disease have the most severe asthma and lowest lung function (Clusters 4 and 5). These results suggest that patients with long-standing asthma are at risk for developing chronic airflow obstruction whether they have an allergic or nonallergic phenotype. Previous studies support this observation, with some groups reporting severe chronic airflow obstruction in patients with persistent airway eosinophilia and subjects with less atopy and late-onset asthma (27–29, 35).
Understanding the basis for persistent symptoms and reduced quality of life in Clusters 3 and 5 is confounded by a higher frequency of obesity in these older subjects, suggesting that impairment may be caused both by asthma and obesity. The interaction of asthma and obesity is complex because obesity may worsen asthma or represent a coexistent condition that increases respiratory symptoms (36–38). Obesity can be associated with reductions in FEV1 and FVC with a relatively preserved FEV1/FVC ratio, and recent studies have suggested dynamic hyperinflation as a possible etiology for dyspnea in these patients (39). Subjects in Cluster 3 show evidence of mild airways obstruction with symptoms somewhat out of proportion to their pulmonary impairment. All subjects in Cluster 3 had bronchial hyperresponsiveness to methacholine, which is consistent with their asthma diagnosis. Thus, Cluster 3 represents a difficult-to–manage, late-onset group of mostly older obese women with frequent exacerbations requiring oral corticosteroid therapies.
The frequency and intensity of HCU is greatest in the clusters with the lowest lung function (Clusters 4 and 5) despite therapy with high doses of inhaled and oral corticosteroids. It is possible that reduced lung function may predispose to severe exacerbations and frequent hospitalizations. The increased frequency of pneumonia in these groups, especially Cluster 5, may be related to higher exposure to corticosteroids and is similar to the more frequent history of pneumonia observed in patients with COPD who were treated with high doses of inhaled corticosteroids (40).
Biomarkers are not included in the cluster analysis because only a subset of subjects had these assessments. A post hoc analysis of this subset of subjects within the clusters provides potential insight into pathobiologic mechanisms that may be related to the different phenotypes observed, especially in Clusters 3, 4, and 5. Although eosinophils are present in the sputum of subjects in all three of these clusters, subjects in Cluster 4 are characterized by elevated clinical measures of atopy (skin testing, serum IgE), suggesting that allergic, IgE-mediated eosinophilic airways inflammation is important in this group. In contrast, sputum neutrophils are also elevated in Cluster 5, which contains subjects who are clinically less atopic with frequent sinopulmonary infections, suggesting complex mechanisms that may reflect allergic inflammation and other pathobiologic factors, including the systemic effects of obesity (37, 41). Persistent airway eosinophilia while receiving high doses of inhaled or oral corticosteroids in Clusters 3, 4, and 5 suggests the possibility of relative steroid insensitivity.
Other groups have reported statistical modeling approaches to investigate novel asthma phenotypes (5, 42–44). The overall purpose and methodology (factor or cluster), the size and demographics of the cohorts, and the number and type of variables used in these analyses differ. The cluster analysis reported by Haldar and colleagues has similarities to the current study but was performed in three smaller asthma cohorts (n = 187 in the largest cohort) and used fewer clinical variables to generate the disease clusters (5). Although some variables are the same as those used in this study (age of onset, BMI, sex, atopy, symptom scores), variables related to pulmonary function and bronchodilator reversibility were limited (only peak flow variability). Sputum eosinophil counts were used, however, which was not possible in the larger SARP multicenter network.
Although the clusters described by Haldar show overlap with the clusters described in this paper, there are important differences. Both cluster analyses identify a group of older obese patients (mostly women) with adult-onset asthma and less atopy (Cluster 3) that comprise approximately 10% of patients with severe asthma. Both analyses report a group of patients with severe asthma with late-onset asthma, less atopy, and decreased lung function, but the patients in Cluster 5 in this study are characterized by elevated sputum neutrophils and significant pulmonary function impairments. The Haldar analysis also describes two severe asthma atopic clusters that are differentiated by level of sputum eosinophilia and symptoms. The current analysis reveals three atopic clusters (Clusters 1, 2, and 4) that differ in baseline lung function, response to bronchodilators, medication requirements, HCU, and asthma symptoms. Clusters 1, 2, and 4 represent a continuum of allergic phenotype across three levels of disease severity, with the most severe patients assigned to Cluster 4. The ability to identify this severe subset of atopic asthma without assessment of sputum eosinophilia is a significant finding in the current analysis.
In conclusion, the five asthma clusters support the importance of disease heterogeneity in asthma and suggest differences in pathophysiologic mechanisms that determine cluster assignments. In retrospective and prospective population samples, the tree or algorithm can be used to evaluate the therapeutic implications of these clusters. The apparent divergent phenotypic characteristics observed, especially in Clusters 3, 4, and 5, suggest different pathophysiologic processes that may determine therapeutic responses and thus affect asthma control.
An important question is how well this cluster approach can be applied to clinical settings. Algorithms have been used successfully for the differential diagnoses of asthma in research studies (45, 46) but have not been applied to different levels of asthma severity. In the current study, we developed an algorithm to assign subjects to asthma severity clusters using readily available clinical testing: the pre- and postbronchodilator FEV1 and an assessment of age of onset. This algorithm was successful in 80% of subjects. Future studies are needed to evaluate our ability to use this cluster analysis in a prospective manner to classify disease severity and improve asthma control by personalizing asthma management and identifying individuals at risk for adverse outcomes.
Supplementary Material
Acknowledgments
The authors thank Patricia Noel, Ph.D., at the National, Heart, Lung and Blood Institute who has guided the Severe Asthma Research Program from the beginning.
The Severe Asthma Research Program (SARP) is a multicenter asthma research group funded by the NHLBI and consisting of the following contributors (Principal Investigators are marked with an asterisk): Brigham and Women's Hospital—Elliot Israel*, Bruce D. Levy, Gautham Marigowda; Cleveland Clinic—Serpil C. Erzurum*, Raed A. Dweik, Suzy A.A. Comhair, Emmea Cleggett-Mattox, Deepa George, Marcelle Baaklini, Daniel Laskowski; Emory University—Anne M. Fitzpatrick, Eric Hunter, Denise Whitlock; Imperial College School of Medicine—Kian F. Chung*, Mark Hew, Patricia Macedo, Sally Meah, Florence Chow; University of Pittsburgh—Sally E. Wenzel*, Erin Aiken; University of Texas-Medical Branch—William J. Calhoun*, Bill T. Ameredes, Dori Smith; University of Virginia—Benjamin Gaston*, W. Gerald Teague*, Mike Davis; University of Wisconsin—William W. Busse*, Nizar Jarjour, Ronald Sorkness, Sean Fain, Erin Billmeyer, Cheri Swenson, Gina Crisafi, Laura Frisque, Dan Kolk; Wake Forest University—Eugene R. Bleecker*, Deborah Meyers, Wendy Moore, Stephen Peters, Annette Hastie, Gregory Hawkins, Jeffrey Krings, Regina Smith; Washington University in St Louis—Mario Castro*, Leonard Bacharier, Iftikhar Hussain, Jaime Tarsi; Data Coordinating Center—Douglas Curran-Everett*, Maura Robinson, Lori Silveira; NHLBI—Patricia Noel*.
Supported by National Institute of Health grants HL69116, HL69130, HL69149, HL69155, HL69167, HL69170, HL69174, HL69349, M01 RR018390, M01RR07122, M01 RR03186, and HL087665.
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Conflict of Interest Statement: W.C.M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. D.A.M. received $1,001–$5,000 from Centocor and $1,001–$5,000 from Aerovance in advisory board fees, $10,001–$50,000 from Centocor, and $10,001–$50,000 from Aerovance in industry sponsored grants (institutional – genetics research). S.E.W. received $5,001–$10,000 from Centocor, $10,001–$50,000 from GlaxoSmithKline, $1,001–$5,000 from AstraZeneca, $5,001–$10,000 from Wyeth, and $5,001–$10,000 from Genentech in consultancy fees; $1,001–$5,000 from Merck, $1,001–$5,000 from GlaxoSmithKline, $10,001–$50,000 from Amira, $10,001–$50,000 from Epigenesis, and $10,001–$50,000 from Novartis in advisory board fees; $1,001–$5,000 from Merck, $1,001–$5,000 from AstraZeneca, $1,001–$5,000 from Critical Therapeutics, and $1,001–$5,000 from Genentech in lecture fees; and $50,001–$100,000 from Centocor, $5,001–$10,000 from Amgen, $50,001–$100,000 from MedImmune, $50,001–$100,000 from Ception, and $10,001–$50,000 from AstraZeneca in industry-sponsored grants. W.G.T. received $5,001–$10,000 from Merck and Co. and up to $1,000 from Aerocrine in lecture fees. H.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. X.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. R.D. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. M.C. received $10,001–$50,000 from Asthmatx and $1,001–$5,000 from Ception in consultancy fees; $5,001–$10,000 from Genentech in advisory board fees; $50,001–$100,000 from AstraZeneca, $10,001–$50,000 from Boehringer Ingelheim, $10,001–$50,000 from Pfizer, $5,001–$10,000 from Genentech, and $1,001–$5,000 from Novartis in lecture fees; more than $100,001 from Asthmatx, more than $100,001 from Amgen, more than $100,001 from Centocor, more than $100,001 from Ception, and more than $100,001 from GlaxoSmithKline in industry-sponsored grants; $1,001–$5,000 from Elsevier in royalties; and $10,001–$50,000 from Pfizer, more than $100,001 from Genentech, more than $100,001 from MedImmune, more than $100,001 from Merck, and more than $100,001 from Novartis for contracted research. D.C-E. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. A.M.F. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. B.G. received $1,001–$5,000 as a consultant for Galleon Pharmaceuticals, $10,001–$50,000 from Galleon Pharmaceuticals in industry-sponsored grants, and holds $5,001–$10,000 as a minority shareholder for Respiratory Research, and controls a patent for inhibition of S-nitrosothiol breakdown to treat asthma. N.N.J. received $10,001–$50,000 from Asthmatx for review of CT scans, concept discussions, and advisory group meetings; $1,001–$5,000 from GlaxoSmithKline and $1,001–$5,000 from Genentech in advisory board fees; $1,001–$5,000 from Merck and Co. in lecture fees; and more than $100,001 from GlaxoSmithKline and more than $100,001 from Genentech in industry-sponsored grants. R.S.' spouse/life partner received $5,001–$10,000 from GlaxoSmithKline in advisory board fees, $5,001–$10,000 from GlaxoSmithKline, and $1,001–$5,000 from AstraZeneca in lecture fees. R.S. received more than $100,001 from Modus Biological Membranes in industry-sponsored grants. W.J.C. received $10,001–$50,000 from AstraZeneca and $5,001–$10,000 from Sepracor in consultancy fees, $5,001–$10,000 in advisory board fees from Merck, and more than $100,001 research grant from Alcon. K.F.C. received $1,001–$5,000 for ad hoc consulting from Gilead; $1,001–$5,000 from GlaxoSmithKline, $1,001–$5,000 from Chiesi, and $1,001 to $5,000 from Merck for serving on an advisory board; $1,001–$5,000 from AstraZeneca, $1,001–$5,000 from GlaxoSmithKline, and $1,001–$5,000 from Chiesi for nonpromotional lecture fees; $10,001–$50,000 from Novartis for a Phase 3 clinical trial; $1,001–$5,000 from Schering Plough for a Phase 3 clinical trial; $1,001–$5,000 from AstraZeneca for Phase 3 clinical research; and $50,001–$100,000 collaborative from GlaxoSmithKline in industry-sponsored grants. S.A.A.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. R.A.D. received more than $100,001 from Actelion in industry-sponsored grants. E.I. received $1,001–$5,000 from Amgen, $1,001–$5,000 from Astellas Pharma US, Inc., $10,001–$50,000 from Asthmatx, $10,001–$50,000 from Genentech, $5,001–$50,000 for Icagen, Inc., $10,001–$50,000 from MedImmune, $10,001–$50,000 from Merck & Co, Inc., $10,001–$50,000 from Novartis, $10,001–$50,000 from BioPharma, $5,001–$10,000 from Pfizer, $10,001–$50,000 from Schering Plough, $1,001–$5,000 from Sepracor, and $10,001–$50,000 from Teva Specialty Pharmaceuticals in consultancy fees; $10,001–$50,000 from Genentech, $10,001–$50,000 from Merck and Co., Inc., and $10,001–$50,000 from Novartis in lecture fees; $5,001–$10,000 from Ficksman & Conley, LLP and $1,001–$5,000 from Prince, Lobel, Glovsky & Tye, LLP for serving as an expert witness; and $50,001–$100,000 from Aerovance, $50,001–$100,000 from Asthmatx, $50,001–$100,000 from Boehringer Ingelheim, $50,001–$100,000 from Centocor, $50,001–$100,000 from Ception Therapeutics, $50,001–$100,000 from Genentech, $50,001–$100,000 from Icagen, Inc., $50,001–$100,000 from Johnson & Johnson, $50,001–$100,000 from MedImmune, $50,001–$100,000 from Merck & Co, Inc., $50,001–$100,000 from PDL BioPharma, and $50,001–$100,000 from Schering Plough in industry-sponsored grants. S.P.P. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. W.W.B. received up to $1,000 from Novartis, up to $1,000 from AstraZeneca, $1,001–$5,000 from Eisai, up to $1,000 from TEVA, $1,001–$5,000 from CompleWare, and $1,001–$5,000 from Schering Plough in consultancy fees; up to $1,000 from Altair, $1,001–$5,000 from GlaxoSmithKline, $5,001–$10,000 from Merck, $1,001–$5,000 from Wyeth, $5,001–$10,000 from Pfizer, up to $1,000 from Centocor, $1,001–$5,000 from Amgen, $1,001–$5,000 from UCB, $1,001–$5,000 from Johnson & Johnson, and up to $1,000 from Bristol-Myers Squib in advisory board fees; up to $1,000 from Merck in lecture fees, more than $100,001 from Novartis, $5,001–$10,000 from Centocor, $5,001–$10,000 from Ception, $10,00–$50,000 from MedImmune, and more than $100,001 from GlaxoSmithKline in industry-sponsored grants; and up to $1,000 from KaloBios in advisory board fees, up to $1,000 from Boehringer Ingelheim, up to $1,000 from Sandoz, up to $1,000 from Alexion, and up to $1,000 from Dainippion Sumitomo in consultancy fees. S.C.E. received more than $100,001 institutional grant from Asthmatx. E.R.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
- 1.National Asthma Education and Prevention Program. Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, MD: National Institutes of Health; National Heart, Lung, and Blood Institute; 2007. Publication no. 07-4051 [accessed June 8, 2009]. Available from: http://www.nhlbi.nih.gov/guidelines/asthma
- 2.Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention (GINA). National Institutes of Health; National Heart, Lung, and Blood Institute [accessed June 8, 2009; updated 2008]. Available at http://www.ginasthma.org)
- 3.Miller MK, Johnson C, Miller DP, Deniz Y, Bleecker ER, Wenzel SE for the TENOR Study Group. Severity assessment in asthma: an evolving concept. J Allergy Clin Immunol 2005;116:990–995. [DOI] [PubMed] [Google Scholar]
- 4.Wenzel SE. Asthma: defining of the persistent adult phenotypes. Lancet 2006;368:804–813. [DOI] [PubMed] [Google Scholar]
- 5.Haldar P, Pavord ID, Shaw DE, Berry MA, Thomas M, Brightling CE, Wardlaw AJ, Green RH. Cluster analysis and clinical asthma phenotypes. Am J Respir Crit Care Med 2008;178:218–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kiley J, Smith R, Noel P. Asthma phenotypes. Curr Opin Pulm Med 2007;13:19–23. [DOI] [PubMed] [Google Scholar]
- 7.Wenzel SE. Severe asthma in adults. Am J Respir Crit Care Med 2005;172:149–160. [DOI] [PubMed] [Google Scholar]
- 8.Busse WW, Banks-Schlegel S, Wenzel SE. Pathophysiology of severe asthma. J Allergy Clin Immunol 2000;106:1033–1042. [DOI] [PubMed] [Google Scholar]
- 9.Moore WC, Peters SP. Severe asthma: an overview. J Allergy Clin Immunol 2006;117:487–494. [DOI] [PubMed] [Google Scholar]
- 10.Proceedings of the ATS workshop on refractory asthma: current understanding, recommendations, and unanswered questions. American Thoracic Society. Am J Respir Crit Care Med 2000;162:2341–2351. [DOI] [PubMed] [Google Scholar]
- 11.Moore WC, Bleecker ER, Curran-Everett D, Erzurum SC, Ameredes BT, Bacharier L, Calhoun WJ, Castro M, Chung KF, Clark MP, et al. for the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. Characterization of the severe asthma phenotype by the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. J Allergy Clin Immunol 2007;119:405–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moore WC, Meyers DA, Li H, D'Agostino R, Peters SP, Bleecker ER for the NHLBI Severe Asthma Research Program (SARP). Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med 2009;179:A2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Comhair SA, Ricci KS, Arroliga M, Lara AR, Dweik RA, Song W, Hazen SL, Bleecker ER, Busse WW, Chung KF, et al. Correlation of systemic superoxide dismutase deficiency to airflow obstruction in asthma. Am J Respir Crit Care Med 2005;172:306–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fitzpatrick AM, Gaston BM, Erzurum SC, Teague WG for the National Institutes of Health/National Heart, Lung, and Blood Institute Severe Asthma Research Program. Features of severe asthma in school age children: atopy and increased exhaled nitric oxide. J Allergy Clin Immunol 2006;118:1218–1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wenzel SE, Balzar S, Ampleford EJ, Hawkins GA, Busse WW, Calhoun WJ, Castro M, Chung KF, Erzurum S, Gaston B, et al. Il-4Rα mutations are associated with asthma exacerbations, airway obstruction, tissue mast cells/IgE expression and racial background. Am J Respir Crit Care Med 2007;175:570–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lara AR, Khatri SB, Wang Z, Comhair SA, Xu W, Dweik RA, Bodine M, Levison BS, Hammel J, Bleecker ER, et al. for the National Heart, Lung, and Blood Institute's Severe Asthma Research Program. Alterations of the arginine metabolome in asthma. Am J Respir Crit Care Med 2008;178:673–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sorkness RL, Bleecker ER, Busse W, Calhoun WJ, Castor M, Chung KF, Curran-Everett D, Erzurum SC, Gaston BM, Israel E, et al. for the National Heart, Lung, Blood Institute Severe Asthma Research Program. Lung function in adults with stable but severe asthma: air trapping and incomplete reversal of obstruction with bronchodilation. J Appl Physiol 2008;104:394–403. [DOI] [PubMed] [Google Scholar]
- 18.Brasier AR, Victor S, Boetticher GD, Ju H, Lee C, Bleecker ER, Castro M, Busse WW, Calhoun WJ. Molecular phenotyping of severe asthma suing pattern recognition of bronchoalveolar lavage-derived cytokines. J Allergy Clin Immunol 2008;121:30–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aysola RS, Hoffman EA, Gierada D, Wenzel S, Cook-Granroth J, Tarsi J, Zheng J, Schechtman KB, Ramkumar TP, Cochran R, et al. Airway remodeling measured by multidetector CT is increased in severe asthma and correlates with pathology. Chest 2008;134:1183–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Busacker A, Newell JD Jr, Keefe T, Hoffman EA, Granroth JC, Castro M, Fain S, Wenzel S. A multivariate analysis of risk factors for the air-trapping asthmatic phenotype as measured by quantitative CT analysis. Chest 2009;135:48–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breiman L, Friedman J, Stone C, Olshen RA. Classification and regression trees. New York: Chapman & Hall; 1984.
- 22.Bacharier LB, Strunk RC, Mauger D, White D, Lemanske RF, Sorkness CA. Classifying asthma severity in children: mismatch between symptoms, medication use and lung function. Am J Respir Crit Care Med 2004;170:426–432. [DOI] [PubMed] [Google Scholar]
- 23.Gelfand EW. Pediatric asthma: a different disease. Proc Am Thorac Soc 2009;6:278–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, Pedersen SE; GOAL Investigators Group. Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. Am J Respir Crit Care Med 2004;170:836–844. [DOI] [PubMed] [Google Scholar]
- 25.Panhuysen CIM, Vonk JM, Koeter GH, Schouten JP, Bleecker ER, Postma DS. Adult patients may outgrow their asthma: a 25 year follow-up study. Am J Respir Crit Care Med 1997;155:1267–1272. [DOI] [PubMed] [Google Scholar]
- 26.Jenkins HA, Cherniack R, Szefler SJ, Covar R, Gelfand EW, Spahn JD. A comparison of the clinical characteristics of children and adults with severe asthma. Chest 2003;124:1318–1324. [DOI] [PubMed] [Google Scholar]
- 27.ten Brinke A, Zwinderman AH, Sterk PJ, Rabe KF, Bel EH. Factors associated with persistent airflow limitation in severe asthma. Am J Respir Crit Care Med 2001;164:744–748. [DOI] [PubMed] [Google Scholar]
- 28.Miranda C, Busacker A, Balzar S, Trudeau J, Wenzel SE. Distinguishing severe asthma phenotypes: role of age of onset and eosinophilic inflammation. J Allergy Clin Immunol 2004;113:101–108. [DOI] [PubMed] [Google Scholar]
- 29.Wenzel SE, Schwartz LB, Langmack EL, Halliday JL, Trudeau J, Gibbs RL, Chu HW. Evidence that severe asthma can be divided pathologically into two inflammatory subtypes with distinct physiologic and clinical characteristics. Am J Respir Crit Care Med 1999;160:1001–1008. [DOI] [PubMed] [Google Scholar]
- 30.Green RH, Brightling CE, McKenna S, Hargadon B, Parker D, Bradding P, Wardlaw AJ, Pavord ID. Asthma exacerbations and sputum eosinophil counts: a randomized controlled trial. Lancet 2002;360:1715–1721. [DOI] [PubMed] [Google Scholar]
- 31.Smith AD, Cowan JO, Brassett KP, Herbison GP, Taylor DR. Use of exhaled nitric oxide measurements to guide treatment in chronic asthma. N Engl J Med 2005;352:2163–2173. [DOI] [PubMed] [Google Scholar]
- 32.Shaw DE, Berry MA, Thomas M, Green RH, Brightling CE, Wardlaw AJ, Pavord ID. The use of exhaled nitric oxide to guide asthma management: a randomized controlled trial. Am J Respir Crit Care Med 2007;176:231–237. [DOI] [PubMed] [Google Scholar]
- 33.Wedes S, Khatri S, Zhang R, W Wu, Comhair SAA, Wenzel SE, Teague WG, Israel E, Erzurum SC, Hazen SL. Noninvasive markers of airway inflammation in asthma. Clin Translational Sci 2009;2:112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fuhlbrigge AL, Kitch BT, Paltiel AD, Kuntz KM, Neumann PJ, Dockery DW, Weiss ST. FEV(1) is associated with risk of asthma attacks in a pediatric population. J Allergy Clin Immunol 2001;107:61–67. [DOI] [PubMed] [Google Scholar]
- 35.Bumbacea D, Campbell D, Nguyen L, Carr D, Barnes PJ, Robinson D, Chung KF. Parameters associated with persistent airflow obstruction in chronic severe asthma. Eur Respir J 2004;24:122–128. [DOI] [PubMed] [Google Scholar]
- 36.Beuther DA, Sutherland ER. Overweight, obesity and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med 2007;175:661–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shore SA. Obesity and asthma: possible mechanisms. J Allergy Clin Immunol 2008;121:1087–1093. [DOI] [PubMed] [Google Scholar]
- 38.Mosen DM, Schatz M, Magid DJ, Camargo CA. The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol 2008;122:507–511. [DOI] [PubMed] [Google Scholar]
- 39.Sutherland TJT, Cowan JO, Taylor DR. Dynamic hyperinflation with bronchoconstriction: differences between obese and nonobese women with asthma. Am J Respir Crit Care Med 2008;177:970–975. [DOI] [PubMed] [Google Scholar]
- 40.Calverley P, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, Yates JC, Vestbo J, for the TORCH investigators. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med 2007;356:775–789. [DOI] [PubMed] [Google Scholar]
- 41.Sutherland TJT, Cowan JO, Young S, Goulding A, Grant AM, Williamson A, Brassett K, Herbison GP, Taylor DR. The association between obesity and asthma: interactions between systemic and airway inflammation. Am J Respir Crit Care Med 2008;178:469–475. [DOI] [PubMed] [Google Scholar]
- 42.Rosi E, Ronchi MC, Grazzini M, Duranti R, Scano G. Sputum analysis, bronchial hyperresponsiveness, and airway function in asthma: results of a factor analysis. J Allergy Clin Immunol 1999;103:232–237. [DOI] [PubMed] [Google Scholar]
- 43.Pillai SG, Tang Y, van den Oord E, Klotsman M, Barnes K, Carlsen K, Gerritsen J, Lenney W, Silverman M, Sly P, et al. Factor analysis in the Genetics of Asthma International Network family study identifies five major quantitative asthma phenotypes. Clin Exp Allergy 2008;38:421–429. [DOI] [PubMed] [Google Scholar]
- 44.Weatherall M, Travers J, Shirtcliffe PM, Marsh SE, Williams MV, Nowitz MR, Aldington S, Beasley R. Distinct clinical phenotypes of airways disease defined by cluster analysis. Eur Respir J (In press) [DOI] [PubMed]
- 45.Panhuysen CIM, Bleecker ER, Koeter GH, Meyers DA, Postma DS. Characterization of obstructive airways disease in family members of probands with asthma: an algorithm for the diagnosis of asthma. Am J Respir Crit Care Med 1998;157:1734–1742. [DOI] [PubMed] [Google Scholar]
- 46.Celedon JC, Silverman EK, Weiss ST, Wand B, Fang Z, Xu X. Application of an algorithm for the diagnosis of asthma in Chinese families. Am J Respir Crit Care Med 2000;162:1679–1684. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.