Patients at increased genetic risk of breast or colorectal cancer who may benefit from screening can be identified from their family histories.1,2 For those at risk of colorectal cancer, colonoscopic surveillance reduces the incidence of disease.3 For those at risk of breast cancer, the results of mammographic screening are encouraging but more data are needed to confirm benefit.4
Currently, patients with indicative family histories who consult their general practitioners are often referred to clinics for cancer genetics. Others with similar family histories who are less aware of the familial nature of these cancers or of the availability of screening do not seek advice.
If improving knowledge about the genetics of familial cancers and other common diseases is to benefit all patients and not just those who are better informed, strategies need to be developed to identify those at risk. We investigated the feasibility of using a postal questionnaire to identify patients in a general practice at increased genetic risk of breast or colorectal cancer.
Subjects, methods, and results
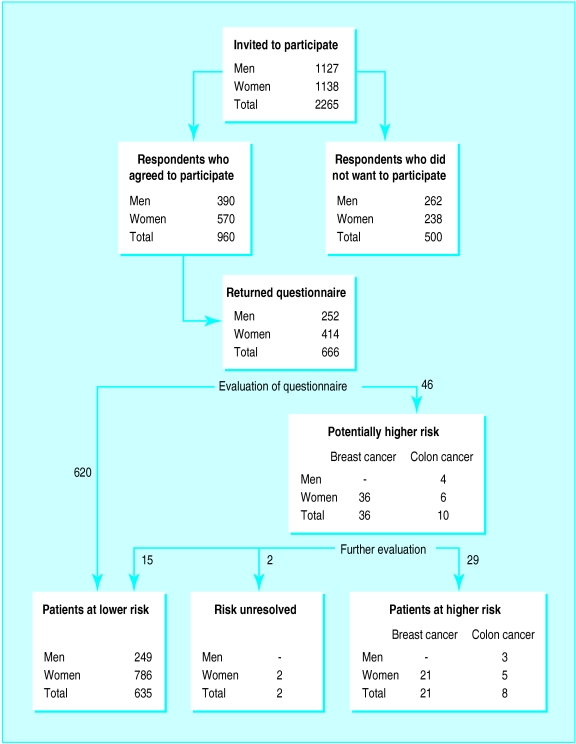
Information about the study was sent to all patients aged 35-65 years who were registered with one general practice. Altogether 1460 out of 2265 (64%) responded to the letter of invitation, but 500 (22%) declined to take part. The remaining 960 patients (42%) agreed to take part and were sent a questionnaire requesting details of first degree, second degree, and more distant relatives known to have had cancer and for their age at diagnosis; 666 patients (29%) completed the questionnaires. Compared with the practice population, a higher proportion of respondents were women (62.2% (414 out of 666) compared with 50.2% (1138 out of 2265), χ2=37.8; P<0.001) and a lower proportion were aged 35-44 (30.2% (201 out of 666) compared with 40.7% (921 out of 2265), χ2=30.3; P<0.001).
The completed questionnaires were assessed by a general practitioner (VL), applying criteria in use in local clinics for cancer genetics at the time of the study to identify patients at sufficiently increased risk of breast or colorectal cancer to offer screening (screening criteria available from us).
Six hundred and twenty patients not meeting these criteria (lower risk group) were informed of this by letter; 46 patients reporting potentially indicative family histories were evaluated further to confirm the details and validate diagnoses in relatives. Most were seen for interview, but in a few cases uncertainties were resolved by telephone. Finally, 29 patients were assessed to be at significantly increased risk (higher risk group): 18 met local screening criteria and 11 were deemed at sufficient risk to be offered screening after discussion with a clinical geneticist (JM or JRWY) (figure); of these patients 14 had previously received genetic advice.
The remaining 15 patients were offered referral to a clinic for cancer genetics, and one was found at screening to have an impalpable breast cancer. Twelve of those offered referral had never previously discussed their family history of cancer with their general practitioner.
Comment
An estimated 1.6% of women aged 35-49 years fulfil the screening criteria for breast cancer used in this study.5 The questionnaire identified 3 out of 198 (1.5%) female respondents in this age group meeting the criteria, which is in line with this prediction, but the numbers are too small to draw conclusions. Estimates of the proportion of the population fulfilling the screening criteria for colorectal cancer are not available.
This study shows that a self completed questionnaire is a useful instrument for obtaining family histories of cancer to identify patients at increased genetic risk. However, the response rate was only 29% when it was sent by post. A better response might be achieved if questionnaire was used in another setting, for example, during registration of new patients.
Figure.
Numbers, sex, and classification of cancer of patients at each stage of the study
Acknowledgments
We thank all the patients who participated in this study and the doctors and staff at East Barnwell Health Centre, Cambridge, for their support and encouragement. We thank Paul Pharoah for kindly allowing us to base the family history questionnaire on one that he had already developed. We thank Steve Jones for help with computing and Elaine Farrell for secretarial assistance. We thank Hilarie Bateman for help with planning the study and Chris Todd for statistical advice. We also thank Martin Bobrow, Ann Louise Kinmonth, and Fawzia Khan for their helpful comments.
Footnotes
Competing interests: None declared.
References
- 1.Pharoah PDP, Stratton JF, Mackay J. Screening for breast and ovarian cancer: the relevance of family history. Br Med Bull. 1998;54:823–828. doi: 10.1093/oxfordjournals.bmb.a011732. [DOI] [PubMed] [Google Scholar]
- 2.Dunlop MG. Colorectal cancer. BMJ. 1997;314:1882–1885. doi: 10.1136/bmj.314.7098.1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jarvinen HJ, Mecklin JP, Sistonen P. Screening reduces colorectal cancer rate in families with hereditary non-polyposis colorectal cancer. Gastroenterology. 1995;108:1405–1411. doi: 10.1016/0016-5085(95)90688-6. [DOI] [PubMed] [Google Scholar]
- 4.Lalloo F, Boggis CR, Evans DG, Shenton A, Threlfall AG, Howell A. Screening by mammography, women with a family history of breast cancer. Eur J Cancer. 1998;34:937–940. doi: 10.1016/s0959-8049(98)00005-7. [DOI] [PubMed] [Google Scholar]
- 5.Mackay J. The role of genetic testing in breast cancer by the year 2000. Cancer Treat Rev. 1997;23:S13–S22. doi: 10.1016/s0305-7372(97)90003-7. [DOI] [PubMed] [Google Scholar]